Abstract
African American men have the highest prostate cancer incidence and mortality rates worldwide, but have lower screening rates compared with Caucasian men. The purpose of the study was to identify social ecological factors that affect screening behaviors in African American men, knowledge that could be integral to the design of culturally appropriate interventions. The exploratory study included 60 African American males recruited from the greater Detroit metropolitan area. Social ecological variables examined included age, marital status, presence of health insurance, education, health values and behaviors, physician trust, and perceived stress coping (John Henryism). Analyses included descriptives, chi-square tests, one-way ANOVAs, and logistic regression. Findings concluded that a parsimonious model consisting of two variables (age and health values) was predictive. African American males, ≥50 years, with higher positive health values were more likely to obtain screening. Findings imply the importance of health values and targeted educational and screening interventions for younger African American men.
Keywords: health-screening behaviors, Black, statistical analysis
Prostate cancer is the most common malignancy and the second leading cause of cancer death for men in the United States (Jemal et al., 2009). Importantly, prostate cancer is also a disease characterized by striking racial/ethnic differences in incidence and mortality. African American men have the highest disease rates and are close to 2.5 times more likely to die from prostate cancer when compared to White men, the second racial/ethnic group most affected (Jemal et al., 2009). Importantly, prostate cancer is amenable to early detection, and more than 75% of prostate cancer cases are diagnosed when the disease is locally confined and curable (Lim, Sherin, & ACPM Prevention Practice Committee, 2008). Although routine screening for prostate cancer is a contentious issue, prostate cancer screening offers the only possibility of early detection for individuals at high risk (Lim et al., 2008). Thus, it is essential for health care providers to recognize factors that determine whether high-risk individuals such as African American men are screened. The purpose of the study was to identify socioecological factors including personal attributes (age, education level, presence of health care insurance, and health-related values and behaviors), relations between people and the environment (health provider trust), and interdependence of environment and life domains (marital status and John-Henryism, e.g., perceived stress coping) that may influence prostate cancer–screening behaviors in African American men.
African American men have lower screening rates for prostate cancer as compared to Caucasian men, a factor that is associated with advanced disease presentation and lowered treatment success (Lim et al., 2008; Woods, Montgomery, Herring, Gardner, & Stokois, 2006). Furthermore, African American men are significantly more likely to be diagnosed with prostate cancer at a younger age (<45 years) compared with White men, a factor that is also associated with more aggressive disease and poorer treatment outcomes (Karami, Young, & Henson, 2007). Despite recognition that prostate cancer is curable when detected early, screening for the disease is controversial (Lim et al., 2008). Results from a large randomized multicenter European study that examined prostate cancer screening and mortality found that screening reduced the rate of death from prostate cancer by 20%, but was also associated with significant risk for overdiagnosis (Schröder et al., 2009). Although the study controlled for age, the published findings did not provide information about the racial identity of the respective participants pooled from the countries of the Netherlands, Finland, Sweden, Belgium, Spain, Italy, and Switzerland (Schröder et al., 2009). Thus, we do not know the representation of men of color in this important large-scale study.
Prostate-specific antigen (PSA) serum levels and digital rectal examination (DRE), the most frequently used strategies for identifying individuals with early disease, can also reflect noncancerous conditions (Lim et al., 2008). Given the economic costs, the limited evidence of reduced mortality, the potential for false negatives and positives, and potential mental health stressors associated with prostate cancer screening, the American College of Preventive Medicine (ACPM) does not recommend routine screening with PSA or DRE in the general population at this time (Lim et al., 2008). At the same time, the lowered screening rates coupled with the more severe disease presentation among African American men, the highest-risk group for morbidity and mortality, are reflective of a lack of knowledge about prostate cancer and the benefits of early detection and treatment for aggressive disease (Lim et al., 2008). Thus, the ACPM does recommend that individuals at high risk for prostate cancer, such as African American men, be provided with information about prostate cancer screening by their physicians so that they can make informed personal health care decisions (Lim et al., 2008).
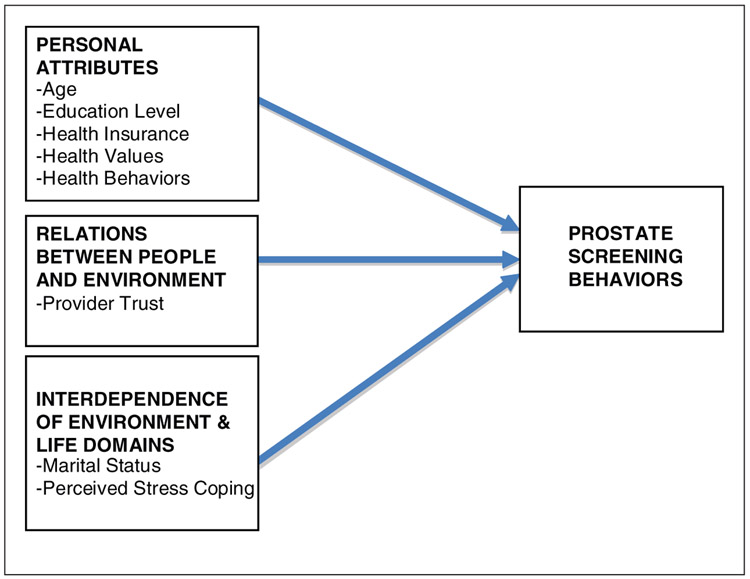
The social ecological perspective uses a broad multidisciplinary systems approach to investigate multiple levels of influence and their interrelatedness in the environment that motivate human behavior. The social ecological framework of health promotion and education emphasizes the roles of social, cultural, and institutional contexts and the dynamic interaction among person–environment factors within these contexts as important for understanding African American men’s behavioral outcomes (Woods et al., 2006). Included in the social ecological framework are (a) environment dimensions (physical, social, cultural information), (b) personal attributes (values, sociodemographic information, behaviors), (c) relations between people and the environment (positive and negative feedback), (d) interdependence of environment and life domains (environmental conditions, family relations, group interactions), and (e) interdisciplinary approach (health system policy) to assessing health and well-being of environments and individuals (Woods et al., 2006). The goal of this article is to identify person–environment interaction factors stemming from a social ecologic approach that may potentially influence prostate cancer–screening behaviors in African American men. Personal attributes include age, education level, presence of health care insurance, and health-related values and behaviors. Relations between people and the environment factors include health provider trust. Interdependence of environment and life domains include marital status and perceived coping with stressful environments. Environment dimensions and interdisciplinary approach constructs are not included in this study (see Figure 1).
Figure 1.
Social ecological factors influencing prostate cancer screening behavior examined in the study
Prostate cancer screening has been shown to increase with age (Tanner & Ross, 2006). Younger African American men who were college educated were more likely to report perceived higher prostate cancer risk and recent participation in screening (Bloom, Stewart, Oakley-Girvans, Banks, & Chang, 2006). Other research has found that African American men with some college or technical school education are more likely to have been screened for prostate cancer (Tanner & Ross, 2006).
Little research has examined if presence of health care insurance and intrapersonal factors such as health values and positive health behaviors relate to prostate cancer screening among African American men. Prostate cancer–screening differences between White and African American men have been explained by presence of health care insurance (Parker et al., 2006). In focus groups, African American men have identified a lack of health care insurance as a barrier to seeking screening (Ford, Vernon, Havstad, Thomas, & Davis, 2006). Studies have found that older African American men adopted a few health behaviors, but were also likely to engage in high-risk activities such as cigarette smoking and alcohol use and were less likely to exercise (Weaver & Gary, 1996). More information is needed as to whether positive health values and behaviors provide a context for preventive health activities among African American men.
Research is limited on how trust in providers relate to African American men’s prostate cancer–screening behaviors. However, negative personal experiences and perceived racism are reported to lead to perceptions of mistrust in the health care system among African American men (Adegbembo, Tomar, & Logan, 2006; Benkert, Peters, Clark, & Keves-Foster, 2006; Boulware, Cooper, Ratner, LaVeist, & Powe, 2003). In focus group feedback, distrust in physicians was cited as a potential barrier to preventive screening for prostate cancer (Forrester-Anderson, 2005). Furthermore, other research conducted among focus groups reported that support from health care providers was associated with prostate cancer–screening decision making (Sanchez, Bowen, Hart, & Spigner, 2007). Less continuity with primary physicians and distrust may be obstacles to prostate cancer screening (Sanchez et al., 2007). More research is needed that examines the role that trust in health care providers plays in African American prostate cancer–screening behaviors.
Interpersonal factors such as support from family and health providers have also been associated with African American men’s prostate cancer behavior. African American males have identified partners as motivational for screening behaviors (Webb, Kronheim, Williams, & Hartman, 2006). In a qualitative study, African American men reported that family involvement was an important factor in their decision to obtain screening for prostate cancer (Jones, Steeves, & Williams, 2009). A large study found that single and unmarried African American men were significantly less likely to have had a PSA test (Tanner & Ross, 2006).
African American adults may develop unique patterns of coping with sustained environmental stress that can impact negatively on health status. John Henryism is a construct that is defined as active, determined, high-effort coping with chronic stressors, and is associated with negative health in different ethnic groups, especially in African Americans (Bennett et al., 2004). One study found a relationship between John Henryism and prostate cancer risk in older African American and Caucasian men (Coker, Sanderson, Ellison, & Fadden, 2006). Evidence of how personal experiences and coping contribute to African American men’s prostate cancer–screening behaviors is lacking.
The purpose of the exploratory study was to determine whether certain social ecological dimensions, including personal attributes (e.g., age, education level, presence of health insurance, and health values and behaviors), person–environment relationship factors (provider trust), and interdependence of environment and life domains factors (marital status and perceived coping with stressful environments), affect African American men’s prostate cancer screening. Proposed hypotheses included that higher age, higher education level, marital status, and positive presence of health care insurance would be related to prostate cancer screening with a PSA test. Furthermore, lowered trust in physicians and high-effort stress coping would be associated with less prostate cancer–screening behaviors.
Method
Sample
The descriptive cross-sectional study was approved by the ethics committee and institutional review board (IRB) at the associated Midwestern University. Using convenience sampling, 60 African American adults were recruited from the larger metropolitan Detroit area. Flyers promoting the study were approved by the IRB and were posted on church bulletins prior to the data collection date following discussions and consent from the respective pastors. Testing of the participants occurred in a private community church classroom away from distractions and disturbances. Timing of the data collection coincided with times that congregants would be participating in church activities to bolster potential volunteer availability.
Potential volunteers were included if they reported good health, had no previous history of cancer, and were able to read and write English. Prior to data collection, the study was fully explained and participants provided written, informed consent, of which they were provided a copy. Participants received a modest monetary incentive for completing the interview.
Measures
Participants completed a sociodemographic survey that elicited information about age, educational background, marital and family status, health and medication history, employment status, presence of insurance, and history of prostate cancer screening via PSA; questions related to health values and health behaviors; a trust in providers’ survey; and a stress-coping survey.
Health values were measured with four Likert-type scale statements about perceived importance of good health with responses that range from strongly disagree to strongly agree with a possible range of 4 to 28 (Lau, Hartman, & Ware, 1986). The health values short survey has been shown to have solid test–retest reliability with consistent and acceptable alpha reliabilities ranging from .62 to .73, credible values for a four-item measure (Lau et al., 1986). Less is known about health values in African American men. The initial testing of the health values survey identified that 30% of the participants were non-White, but it did not describe their racial/ethnic makeup (Lau et al., 1986). Similar to what has been reported in the literature, the Cronbach’s alpha for the health values survey was .62 in this study.
Health behaviors were measured with seven Likert-type scale items eliciting degree of endorsement for questions that included smoking, maintenance of a nutritious diet, sleep regularity, stress management, medical checkup regularity, alcohol use, and exercise frequency (Berkman & Breslow, 1983; Hooker & Kaus, 1994). The scale ranged from 7 to 35. The Cronbach’s alpha reliabilities for the Health Behaviors Questionnaire range from .62 to .69 (Hooker & Kaus, 1994). Given that the one-item summed health behaviors are augmented via accretion and are not correlational, the reported reliability coefficients are acceptable (Hooker & Kaus, 1994). Similar to what has been reported in the literature, the Cronbach’s alpha was .61 for this sample of African American men.
The Trust in Physician Scale (TIPS), an 11-item 1- to 5-point Likert-type scale with responses from totally disagree to totally agree (range 11 to 55), was used to measure health care provider trust. This scale has high internal consistency and good test–retest reliability, and has been used in African American populations (Benkert et al., 2006; Thom, Ribisi, Stewart, Luke, & The Stanford Trust Study Physicians, 1999). The Cronbach’s alpha for the TIPS was .75.
Stress coping with the environment was measured with the John Henryism Scale for Active Coping (JHAC12; Bennett et al., 2004). The JHAC12 is a 12-item 1- to 5-point survey (responses range from completely false to completely true; range 12 to 60) that measures behavioral tendencies to cope actively with psychosocial environmental stressors. Three important themes of John Henryism are tapped with this measure and include mental and physical vigor, committedness to hard work, and single-minded determination to succeed (Bennett et al., 2004). The instrument has satisfactory reliability and validity (Bennett et al., 2004). The Cronbach’s alpha in this study was .77.
Analysis
Descriptive statistics were obtained on all variables. Age was dichotomized into a binary variable (≤50 vs. >50 years of age). Marital status, education level, insurance status, and screening status were coded into dichotomous variables (e.g., married vs. not married, high school education or less vs. at least some college). Chi-square tests and one-way ANOVA were conducted to screen the potential variables that were significantly related to the prostate cancer–screening behaviors. Logistic regression analyses using the backward stepwise method were used to achieve the research aim using SPSS version 16.0. An alpha level of .05 was used for all statistical tests and r was calculated as the effect size.
Results
Most of the men were more than 50 years old (M = 54.8 ± 10.13, range 38 to 79). About 63% were married and the majority had at least some post–high school education (see Table 1 for characteristics of the study sample). About 70% of the men were employed, and the majority (92%) had health insurance. Half of the participants reported health problems such as hypertension or arthritis. Compared to those who did not have prostate cancer screening, men who obtained screening were more likely to be married (χ2 = 3.95, df = 1, p < .05), 50 years or older (χ2 = 21.93, df = 1, p < .00), and to have health insurance (χ2 = 6.49, df = 1, p < .05). Education and employment status were not related to screening behaviors.
Table 1.
Demographic and Health Characteristics of the Sample (N = 60)
| Demographic Variables | Data, n (%) |
|---|---|
| Age distribution, years | |
| <40 | 4 (6.7) |
| 40-49 | 11 (18.3) |
| 50-59 | 28 (46.7) |
| 60-69 | 11 (18.3) |
| 70-79 | 6 (10.0) |
| Education background | |
| <12 years | 4 (6.7) |
| 12 years/GED | 7 (11.7) |
| Some college/trade school | 26 (43.3) |
| College graduate | 12 (20.0) |
| Graduate school | 11 (18.3) |
| Marital status | |
| Married | 38 (63.3) |
| Widowed | 1 (1.7) |
| Divorced | 15 (25.0) |
| Never married | 6 (10.0) |
| Health conditions | |
| Hypertension/cardiac | 17 (28.3) |
| Diabetes mellitus | 4 (6.7) |
| Arthritis | 2 (3.3) |
| Combinationa | 5 (8.3) |
| Otherb | 3 (5.0) |
| None | 29 (48.3) |
| Prostate screening | |
| Yes | 42 (70.0) |
| No | 18 (30.0) |
A combination of hypertension and/or cardiac disease, diabetes mellitus, and arthritis.
Included back spasms and sarcoidosis.
Health values scores tended to be positive in this group (M = 20.33 ± 4.06, range 12 to 28). Similarly, mean scores for health behaviors (M = 22.83 ± 3.86, range 9 to 34) demonstrate that the group generally reported more positive health care behaviors, although there were findings on the low end of the health behavior scale. The overall mean and standard deviation of the TIPS (40.42 ± 5.35, range 28 to 54) are similar to results reported in other research conducted among African American adults (Benkert et al., 2006). However, the range was less broad in this study, with all participants reporting at least 28, which suggests that there were at least moderate levels of trust in physicians in the reported sample. The group mean and standard deviation for the JHAC12 (47.18 ± 6.39, range 32 to 59) indicates moderate to high scores on the John Henryism construct. Scores in the 50s that were found in this study reflect higher levels of John Henryism (Bennett et al., 2004). Findings from this study indicate John Henryism scores that are slightly lower but similar to other studies conducted among African American groups (Bennett et al., 2004; Fernander et al., 2005). One-way ANOVA results showed that participants who had prostate cancer screening tended to report higher scores on both positive health values and behaviors questions, F = 3.18, df = 1, p < .05, and F = 6.87, df = 1, p < .01, respectively. Trust in Physician and the John Henryism scales were not related to African American men’s prostate cancer–screening behaviors (F = 0.08, df = 1, p > .05, and F = 0.58, df = 1, p > .05, respectively).
Logistic regression analyses were done with statistically significant variables from the above-mentioned descriptive analyses ( age, health insurance, positive health values and behaviors, marital status). Men who were 50 years and older and who had higher scores on the health values survey were more likely to have prostate cancer screening in the past year. Specifically, the odds of men 50 years and older having obtained PSA screening were about 16 times higher than those younger than 50 years of age (odds ratio [OR] = 15.72, 95% confidence interval [CI] = 3.45 to 71.64). The odds of men having had PSA testing also increased by about 26% for those who had 1 unit increase in their health behaviors and values measure (OR = 1.26, CI = 1.02 to 1.54). Although being married and having health insurance and higher scores on the Health Behaviors Questionnaire also seemed to increase the likelihood of African American men obtaining PSA screening in the previous year, such findings were statistically insignificant (Table 2). These variables were thus excluded from the final model. The statistically significant parsimonious model (Table 2) consisting of two variables (age and health values, χ2 = 22.71, p < .000) replaced the full model with all the variables of interest. The overall rate of correct classification of prostate cancer screening was 81.7% in the sample.
Table 2.
Factors Influencing the Prostate Cancer–Screening Behavior in African American Men (Full and Parsimonious Models)
| β | Wald | Odds Ratio | 95% Confidence Interval |
|
|---|---|---|---|---|
| Full model variables | ||||
| Age (≥50 years of age) | 2.56 | 8.81** | 12.88 | 2.38-69.62 |
| Marital status (married) | 0.139 | 0.03 | 0.88 | 0.20-6.50 |
| Health behaviors | 0.11 | 1.09 | 1.11 | 0.91-1.52 |
| Health values | 0.21 | 3.80* | 1.23 | 1.0-1.52 |
| Insurance (with insurance) | 1.16 | 0.71 | 3.18 | 0.22-47.38 |
| Constant | −1.79 | 1.33 | 0.17 | |
| −2 log likelihood | 48.69 | |||
| Model chi-square (df = 6) | 24.61 | |||
| p | .000 | |||
| Overall rate of correct classification | 83.3% | |||
| Parsimonious model variables | ||||
| Age (≥50 years of age) | 2.78 | 12.67** | 15.72 | 3.45-71.63 |
| Health values | 0.23 | 4.82* | 1.26 | 1.01-1.53 |
| Constant | −0.87 | 1.94 | 0.42 | |
| −2 log likelihood | 50.60 | |||
| Model chi-square (df = 2) | 22.71 | |||
| p | .000 | |||
| Overall rate of correct classification (parsimonious model) | 81.7% | |||
p ≤ .05.
p ≤ .001.
Discussion
Despite the lack of uniform consensus relative to the merits of prostate cancer screening, preventive screening is the primary modality of early detection and thus opportunity for cure among African American men, a group disproportionately affected by prostate cancer (Woods et al., 2006). Thus, the purpose of the exploratory study were to determine whether certain social ecological dimensions including personal attributes, person–environment relationship factors, and interdependence of environment and life domains factors affect African American men’s prostate cancer–screening behavior.
As hypothesized, African American men were most likely to report having obtained the PSA screening if they were older than 50 years of age. Furthermore, older men with higher positive health value scores were more likely to have received prostate cancer screening. Contrary to study expectations, screening behaviors were not influenced by marital status, education level, health insurance, stress coping, and provider trust. African American men reporting high health values may be more health conscious. These individuals may be more likely to be exposed to health maintenance information and more interested in preventive health services. Familiarity and exposure to health-related information, including prostate cancer information from health providers, may increase the likelihood of prostate cancer screening. Self-awareness of health and well-being has been identified as a major prostate cancer screening-related theme (Sanchez et al., 2007). Familiarity with the illness and more general exposure to prostate cancer information have also been shown to be enabling factors for prostate cancer–screening participation (Nivens, Herman, Pweinrich, & Weinrich, 2001; Odedina et al., 2004), whereas a lack of knowledge regarding prostate cancer has been negatively related to cancer screening (Ford et al., 2006). Thus, individuals with higher health values may also possess heightened drive to be knowledgeable of personal health risks and to engage in preventive health behaviors.
The inclusion of stress coping in the analysis is novel in studying prostate cancer–screening behavior among African American men. Although research has shown that higher John Henryism scores indicating high-effort coping may be associated with an increase in prostate cancer risk (Coker et al., 2006), there has been little research on how John Henryism scores affect men’s prostate cancer–screening behaviors. This pilot research, to our knowledge, is the first to examine such a relationship. John Henryism scores tended to be moderate to high. High John Henryism scores reflective of active engagement with the environment may be buffered by higher socioeconomic status, a finding that may reduce the negative effects on health (Bennett et al., 2004) and would coincide with a social ecological interpretation. Furthermore, high scores may reflect social desirability biases in the scale as the items may reflect core American values of determination and hard work (Bennett et al., 2004). Although this study did not find relationships between screening and stress coping, research examining potential relationships with a larger, more diverse sample is warranted.
In this study, provider trust had no significant effect on prostate cancer–screening behavior. This result was divergent from focus group reports that identified distrust in physicians as a potential barrier to preventive screening (Forrester-Anderson, 2005). Trust is a fundamental component of the patient–physician relationship and is significantly related to the continuity with the physician and positive behaviors such as medication adherence (Thom et al., 1999). Physician distrust, on the contrary, has been identified as one of the major obstacles to timely diagnosis and appropriate care for prostate cancer patients, especially among African American men (Talcott et al., 2007). The deviation of this study’s findings from expected directions may stem from the homogeneous sample that suggested an overall higher socioeconomic status. Our research participants were mostly older, better educated, married, employed, and insured. Higher trust combined with the presence of health care insurance may reflect more autonomy in provider choice, a finding that would be justified from a social ecological interpretation.
The study is not without limitations. The small convenience sample that tended to better educated is likely less representative of healthy African American men at large. Furthermore, most of the men participating in this study had been previously screened for prostate cancer with a PSA test. Better educated men may be more informed about important health issues and more likely to access preventive health services. There was no information related to the ethnicity of the participants’ health providers, a factor that could affect levels of perceived trust and communication. Furthermore, given the small scale of the study, other socioecological factors such as culture (Parchment, 2004), health beliefs (Odedina et al., 2004), and income (Chiu, Anderson, & Corbin, 2005) that have been shown to be associated with preventive screening in African Americans were not examined. The study did not examine the pivotal role that a church environment may also play in the promotion of positive health values and behaviors. African Americans have identified the church as playing a key role in disseminating health care information and the advocacy of positive health behaviors (Webb et al., 2006). Importantly, the data is based solely on self-report, and medical record data were not available to validate the correctness of the prostate cancer–screening history. Furthermore, the health values and behavior surveys have had limited use in an African American population. More testing of health values and health behaviors among African American men is needed before findings can be generalized.
Early detection of prostate cancer decreases the risk for advanced disease and improves the probability of long-term survival (Woods et al., 2006). Findings from this study incorporating a social ecological perspective demonstrate the positive effects of having health care insurance and access to services among African American men. Furthermore, findings from this research provide preliminary evidence useful to the design of further research and the development of interventions to promote positive health promotion behaviors in African American men. Programs that promote prostate cancer awareness among African Americans not only must target younger adults but also could devote efforts to improve general health behaviors (e.g., smoking, alcohol use, balanced diet, and exercise). Given that newly diagnosed African American men with prostate cancer are often younger, less often married, and more likely to report less education and poorer medical insurance coverage compared to their White counterparts (Talcott et al., 2007), such emphasis is sorely needed.
Acknowledgments
Funding
The authors disclosed receipt of the following financial support for the research and/ or authorship of this article: The authors received financial support for the research and/or authorship of this article from the MESA Center for Health Care Disparities, National Institute for Nursing Research, administered by the University of Michigan School of Nursing, NINR T32 NR 0704, and support from the Mary Margaret Walther Program for Cancer Care Research.
Footnotes
Declaration of Conflicting Interests
The authors declared no conflicts of interests with respect to the authorship and/or publication of this article.
References
- Adegbembo AO, Tomar SL, & Logan HL (2006). Perception of racism explains the difference between Blacks’ and Whites’ level of healthcare trust. Ethnicity & Disease, 16, 792–798. [PubMed] [Google Scholar]
- Benkert R, Peters RM, Clark R, & Keves-Foster K (2006). Effects of perceived racism, cultural mistrust and trust in providers on satisfaction with care. Journal of the National Medical Association, 98, 1532–1540. [PMC free article] [PubMed] [Google Scholar]
- Bennett GG, Merritt MM, Sollers JJ III, Edwards CL, Whitfield KE, & Brandon DT (2004). Stress, coping, and health outcomes among African-Americans: A review of the John Henryism hypothesis. Psychology & Health, 19, 369–383. [Google Scholar]
- Berkman L, & Breslow L (1983). Health and ways of living: The Alameda County study. New York, NY: Oxford University Press. [Google Scholar]
- Bloom JR, Stewart SL, Oakley-Girvans I, Banks PJ, & Chang S (2006). Family history, perceived risk, and prostate cancer screening among African American men. Cancer Epidemiology, Biomarkers & Prevention, 15, 2167–2173. [DOI] [PubMed] [Google Scholar]
- Boulware LE, Cooper LA, Ratner LE, LaVeist TA, & Powe NR (2003). Race and trust in the health care system. Public Health Reports, 118, 358–365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chiu BC, Anderson JR, & Corbin D (2005). Predictors of prostate cancer screening among health fair participants. Public Health, 119, 686–693. [DOI] [PubMed] [Google Scholar]
- Coker AL, Sanderson M, Ellison GL, & Fadden MK (2006). Stress, coping, social support, and prostate cancer risk among older African American and Caucasian men. Ethnicity & Disease, 16, 978–987. [PubMed] [Google Scholar]
- Fernander AF, Patten CA, Schroeder DR, Stevens SR, Eberman KM, & Hurt RD (2005). Exploring the association of John Henry active coping and education on smoking behavior and nicotine dependence among Blacks in the USA. Social Science & Medicine, 60, 491–500. [DOI] [PubMed] [Google Scholar]
- Ford ME, Vernon SW, Havstad SL, Thomas SA, & Davis SD (2006). Factors influencing behavioral intention regarding prostate cancer screening among older African-American men. Journal of the National Medical Association, 98, 505–514. [PMC free article] [PubMed] [Google Scholar]
- Forrester-Anderson IT (2005). Prostate cancer screening perceptions, knowledge and behaviors among African American men: Focus group findings. Journal of Health Care for the Poor & Underserved, 16(4 Suppl. A), 22–30. [DOI] [PubMed] [Google Scholar]
- Hooker K, & Kaus CR (1994). Health-related possible selves in young and middle adulthood. Psychology and Aging, 9, 126–133. [DOI] [PubMed] [Google Scholar]
- Jemal A, Siegel R, Ward E, Hao Y, Xu J, & Thun J (2009). Cancer statistics, 2009. CA: A Cancer Journal for Clinicians. doi: 10.3322/caac.20006 [DOI] [PubMed] [Google Scholar]
- Jones RA, Steeves R, & Williams I (2009). How African American men decide whether or not to get prostate cancer screening. Cancer Nursing: An International Journal, 32, 166–172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Karami S, Young HA, & Henson DE (2007). Earlier age at diagnosis: Another dimension in cancer disparity? Cancer Detection and Prevention, 31, 29–34. [DOI] [PubMed] [Google Scholar]
- Lau RR, Hartman KA, & Ware JE (1986). Health as a value: Methodological and theoretical considerations. Health Psychology, 5, 25–43. [DOI] [PubMed] [Google Scholar]
- Lim LS, Sherin K, & ACPM Prevention Practice Committee. (2008). Screening for prostate cancer in U.S. men: ACPM position statement on preventive practice. American Journal of Preventive Medicine, 34, 164–170. [DOI] [PubMed] [Google Scholar]
- Nivens AS, Herman J, Pweinrich S, & Weinrich MC (2001). Cues to participation in prostate cancer screening: A theory for practice. Oncology Nursing Forum, 28, 1449–1456. [PubMed] [Google Scholar]
- Odedina FT, Scrivens J, Emanuel A , LaRose-Pierre M, Brown J, & Nash R (2004). A focus group study of factors influencing African-American men’s prostate cancer screening behavior. Journal of the National Medical Association, 96, 780–788. [PMC free article] [PubMed] [Google Scholar]
- Parchment YD (2004). Prostate cancer screening in African American and Caribbean males: Detriment in delay. The Association of Black Nursing Faculty Journal, 15, 116–120. [PubMed] [Google Scholar]
- Parker PA, Cohen L, Bhadkamkar VA, Babaian RJ, Smith MA, Gritz ER, & Basen-Engquist KM (2006). Demographic and past screening behaviors of men attending a free community screening program for prostate cancer. Health Promotion Practice, 7, 213–220. [DOI] [PubMed] [Google Scholar]
- Sanchez MA, Bowen DJ, Hart A, & Spigner C (2007). Factors influencing prostate cancer screening decisions among African American men. Ethnicity & Disease, 17, 374–380. [PubMed] [Google Scholar]
- Schröder FH, Hugosson J, Roobol MJ, Tammela TL, Ciatto S, Nelen V, … Auvinen A; ERSPC Investigators. (2009). Screening and prostate cancer mortality in a randomized European study. New England Journal of Medicine, 360, 1320–1328. [DOI] [PubMed] [Google Scholar]
- Talcott JA, Spain P, Clark JA, Carpenter WR, Do YK, Hamilton RJ, … Godley PA (2007). Hidden barriers between knowledge and behavior: The North Carolina prostate cancer screening and treatment experience. Cancer, 109, 1599–1606. [DOI] [PubMed] [Google Scholar]
- Tanner BB, & Ross L (2006). Physician-patient discussions about prostate-specific antigen test use among African-American men. Journal of the National Medical Association, 98, 532–538. [PMC free article] [PubMed] [Google Scholar]
- Thom DH, Ribisi KM, Stewart AL, Luke DA, & The Stanford Trust Study Physicians. (1999). Further validation and reliability testing of the Trust in Physician Scale. Medical Care, 37, 510–517. [DOI] [PubMed] [Google Scholar]
- Weaver GD, & Gary LE (1996). Correlates of health-related behaviors in older African American adults: Implications for health promotion. Community Health, 19, 43–57. [Google Scholar]
- Webb CR, Kronheim L, Williams JE, & Hartman TJ (2006). An evaluation of the knowledge, attitudes, and beliefs of African-American men and their female significant others regarding prostate cancer screening. Ethnicity & Disease, 16, 234–238. [PubMed] [Google Scholar]
- Woods VD, Montgomery SB, Herring RP, Gardner RW, & Stokois D (2006). Social ecological predictors of prostate-specific antigen blood test and digital rectal examination in Black American men. Journal of the National Medical Association, 98, 492–504. [PMC free article] [PubMed] [Google Scholar]