Abstract
COVID-19 is causing a major once-in-a-century global pandemic. The scientific and clinical community is in a race to define and develop effective preventions and treatments. The major features of disease are described but clinical trials have been hampered by competing interests, small scale, lack of defined patient cohorts and defined readouts. What is needed now is head-to-head comparison of existing drugs, testing of safety including in the background of predisposing chronic diseases, and the development of new and targeted preventions and treatments. This is most efficiently achieved using representative animal models of primary infection including in the background of chronic disease with validation of findings in primary human cells and tissues. We explore and discuss the diverse animal, cell and tissue models that are being used and developed and collectively recapitulate many critical aspects of disease manifestation in humans to develop and test new preventions and treatments.
Introduction
There is currently a major human pandemic caused by the novel severe acute respiratory syndrome (SARS)- coronavirus-2 (SARS-CoV-2) that leads to coronavirus-induced disease (COVID-19).1 It is primarily a viral-induced inflammatory disease of the airways and lungs that causes severe respiratory issues. SARS-CoV-2 uses the angiotensin converting enzyme-II receptor (ACE2) to bind and infect cells leading to internalization and proliferation.2, 3 Inflammatory, innate and adaptive immune responses are induced to clear the virus but also cause host tissue damage.4, 5 Consequent hypoxia leads to systemic involvement particularly of the vasculature that leads to vasoconstriction reduced perfusion and organ failure.6 Much remains to be understood of the inflammatory and immune responses that are induced by the infection and how they induce pathogenesis. Ventilation and oxygen therapy are primary treatments and it is emerging that those with severe disease who survive develop lung fibrosis.7 The most effective pharmacological treatments remain ill-defined with varying results with hydroxychloroquine8 but more promising results with dexamethasone.9
Elucidating the mechanisms of pathogenesis will enable the identification of the most effective therapies. Animal models of SARS-CoV-2 infection and COVID-19 that recapitulate the hallmark features of the human disease will undoubtedly be valuable in elucidating pathogenic mechanisms, identifying new therapeutic targets and developing and testing new and effective treatments.
Human infection and disease
SARS-CoV-2 is a beta-coronavirus closely related to SARS-CoV that caused a relatively small outbreak in the early 2000s.2, 10 Similar to SARS-CoV, SARS-CoV-2 binds the ACE2 receptor and requires proteases such as serine TMPRSS2 to cleave the viral spike (S) protein required for SARS-CoV and SARS-CoV-211, 12 cell entry.2 This step may be facilitated by endosomal proteases such as cathepsin-L and enhanced by the protein furin,13 the virus then enters the host cell by endocytosis.
A critical element of SARS-CoV-2 tropism in humans is the abundance of ACE2 in the upper respiratory tract (URT) especially the nasopharynx.14 The molecular configuration of the SARS-CoV-2 membrane binding component of the S protein binds with greater affinity to ACE2 than does SARS-CoV, which likely contributes to the higher infectivity of the former.15 The clinical course commences with an incubation period with a median of 5.1 days, with illness typically developing by 11 days.16 This phase is characterized by mild symptoms, with most people remaining asymptomatic and infection thought to be confined to the URT, although they are capable of transmitting infection. Symptoms when they do occur are typically acute viral respiratory illness with fever, cough, dyspnoea, fatigue, anosmia, myalgia and confusion.17 In ~80% of people, the course remains mild and disease does not extend to the lower respiratory tract (LRT). However, ~20% develop more severe symptoms, with diffuse widespread pneumonia, with 5% having severe gas exchange problems, acute lung injury and progress onto acute respiratory distress syndrome (ARDS).18, 19 The clearest predictor of mortality is age, with the case fatality rate rising dramatically over 60 years of age.20 Other predisposing factors for heightened mortality are male sex, social deprivation, and chronic disease particularly chronic obstructive pulmonary disease (COPD), cardiovascular disease (CVD), obesity and diabetes.21
A key issue is why some individuals progress to more severe lower respiratory disease but others do not. One factor is the ability of the inflammatory and immune responses to confine the infection to the URT. ACE2 is expressed in the LRT, but at lower levels than in the nasopharynx.22 Also, while ciliated airway epithelial cells are readily infected and transmit to surrounding cells, the reduction in ACE2 may be a barrier to LRT infection. In those that progress severe systemic inflammatory response or “cytokine storm” develop. The pneumonia associated with severe infection bears all the pathological features of ARDS, with diffuse alveolar damage, interstitial pneumonitis and lymphocytic infiltrates.23, 24 Unique features of critical disease are extravascular fibrin deposition, neutrophil trapping, microvascular thrombosis and large vessel pulmonary emboli.24 Widespread thrombosis and microangiopathy in critical COVID-19 occurs at higher rates than in ARDS associated with influenza, and dysregulated coagulation and angiogenesis are also features.25
Increased and dysregulated Th-1 and Th-17 responses were present in ARDS in Middle Eastern respiratory syndrome (MERS-CoV) and influenza.26, 27 The occurrence of severe lung disease at 5–10 days post-infection (dpi) reflects the dual features of spread of infection to the LRT and coincident development of adaptive immune responses with heightened activation of virus-specific T-effector cells. This coincides with lymphopenia associated with severe disease, and is a predictive marker earlier in disease with worse outcome.28 There is also evidence that T-cells are dysfunctional with increased expression of exhaustion molecules related to heightened systemic inflammation.29 The role of elevated systemic immune dysregulation is supported by analysis of the transcriptomic responses in 50 people with SARS-CoV-2 infection, demonstrating that impaired interferon (IFN) responses were related to persistent viremia and increased systemic inflammation, with elevated TNF-α, IL-6 and IL-10.30 Elevated systemic levels of IL-17 are also present in critical illness with ARDS and heightened inflammation, and it is plausible that increased Th-17 responses drive ongoing inflammation.31 While interesting, these are observations, often performed with limited patient numbers where ARDS and disease severity are associated with heightened inflammatory and immune activation, and a causative role cannot be established.27, 32 Interrogation of representative animal models is needed to define cause and effect, elucidate mechanisms of pathogenesis and test treatments.
Small animal models
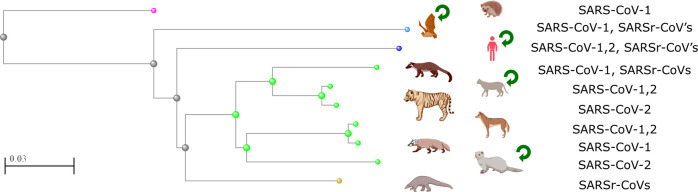
A range of animal models have been used to study COVID-19 with varying susceptibility likely dependent on species specific make-up for ACE2 (Fig. 1 ).
Fig. 1.

ACE2 protein phylogenetic divergence and in vivo model severity. Left panel, fast minimum evolution distance tree for ACE2 protein sequences using Griphin for evolutionary distance, unsorted. Species included are Gallus gallus (Chicken), Anas platyrhynchos (Duck), Cavia porcellus (Guinea Pig), Mustela putoris furo (Ferret), Canis lupus familiaris (Dog), Felis catus (Cat), Sus scrofa (Pig), Rousettus aegyptiacus (fruitbat), Mesocricetus auratus (Golden hamster), Mus musculus (Mouse), Callithrixjacchus (Common Marmoset), Macaca mulatta (Rhesus macaque), Macaca fascicularis (Cynomolgus Macaque), Chlorocebus aethiops (African Green Monkey) and Homo sapiens. Macaques are represented as one image due to close divergence. Severity of disease is color-coded from refractory to infection (BLUE, no virus detected) to severe (RED, shedding). Common Marmoset and Guinea Pig have only been assessed for SARS-CoV, all others with SARS-CoV-2. Scale indicates 10% amino acid divergence.
Mouse models
Small animal models are widely used to study emerging viruses, but often they need to be genetically modified or the virus needs to be adapted for different species to be susceptible and this is the case for SARS-CoV-2. In most studies to date the mouse strains have been incompletely or incorrectly described and should be included in future publications.
Genetically modified mice
Several inbred mouse strains were used to model SARS-CoV infection including BALB/c,33 C57BL/634 and “129SvEv” (incorrectly reported name),35 as well as factor-deficient (−/−) mice such as Cd1 −/−, Rag1 −/− and Stat1 −/−.34, 35, 36, 37 The identification of ACE2 as the host receptor for SARS-CoV38 initiated considerable global interest in developing murine models that are representative of human disease. This led to the generation of transgenic mice that express human (h)ACE2, K18-hACE2, in the epithelia of tissues and organs including lungs, liver, kidney, spleen, heart and gut. K18-hACE2 mice still express the mouse (m)ACE2, however this is primarily localised in the ileum.39 They are highly susceptible to SARS-CoV infection and experience high viral lung titres, significant weight loss and morbidity from 4 dpi.39 Viral dissemination to the brain was the main cause of death.40 Similar results were obtained in another transgenic strain expressing hACE2 under the control of the mACE2 promoter.41
With the MERS outbreak in 2012 and identification of that virus' entry receptor dipeptidyl peptidase-4 (DPP4, CD26), it was found that neither wild-type (WT) nor immuno-deficient mice were susceptible to MERS-CoV infection.42 Transgenic mice expressing human (h)DPP4 in epithelial and endothelial cells in the lung, brain, heart, liver, kidney, spleen and intestine were generated.43 They were highly susceptible to MERS-CoV infection, with significant weight loss, high viral lung titres and inflammatory cytokine production from 2 dpi, and mortality from day 5.43 In other studies, exons 10–12 of the mDPP4 locus were modified to resemble hDPP4 expression,44, 45, 46 which led to MERS-CoV lung replication but not disease development.47, 48
With the discovery of SARS-CoV-2/ACE2 interactions2, 12, 49 global interest in hACE2 mouse models re-emerged. However, due to falling interest with the resolution of the SARS outbreak, most labs ceased maintaining hACE2 mice. To satisfy the global demand for hACE2 mice, the Jackson Laboratory re-animated K18-hACE2 mice, which are becoming available. The lag-time has slowed the understanding of disease mechanisms in COVID-19 and the identification of effective drug and vaccine candidates to progress to clinical trials.
The first live SARS-CoV-2 infection model used transgenic mice expressing hACE2 under the control of the mACE2 promoter.41, 50 Mice had significant weight loss over a 14-day infection period, and high viral lung titres 1–5 dpi. Histological lung examination revealed moderate interstitial pneumonia, infiltration of lymphocytes, mucus accumulation and desquamation of bronchoepithelial cells from day 3.50 There were no detectable viral titres or pathology in other tissues or organs, except on day 1 in the intestine, suggesting that infection is localized almost exclusively to the lungs.
Similarly, transgenic mice overexpressing hACE2 under the control of HFH4/FOXJ1 lung ciliated epithelial cell-specific promoters are also susceptible to SARS-CoV-2 infection.51, 52 Most infected HFH4-hACE2 mice had minimal weight loss over 7-days of infection. However mice that later became moribund showed significant weight loss from day 4 and significant lymphopenia and neutrophilia in peripheral blood at day 6, which recapitulates severe human disease.28, 31 Lung histology showed initial macrophage and lymphocyte infiltration and fibrin exudation from 1 dpi, which steadily progressed to severe pneumonia, blockage of terminal bronchioles, extensive fibroplasia and alveolar necrosis by day 7.51 In contrast to previous findings of lung tissue specificity,50 HFH4-hACE2 infected mice had detectable viral titres in the lung, eyes, brain and heart suggesting that the virus may have additional tissue tropisms following initial lung infection.50, 51 Re-infection following recovery from initial SARS-CoV-2 infection resulted in reduced weight loss and viral titres and improved survival indicating the development of protective immunity following initial challenge.
Recently, the first K18-hACE2 SARS-CoV-2 infection was examined.53 Mice exhibited no clinical symptoms or weight loss until 4 dpi. By day 5, mice had 10% weight loss with variable clinical presentation, ranging from reduced activity to increased respiration and lethargy. Infected mice also had moderate viral lung titres, suggesting productive infection. Bronchoalveolar lavage revealed increased infiltrating granulocytes, monocytes and eosinophils accompanied by alveolar debris and septal thickening on histopathology analysis. While these results are encouraging, the study only examined five mice up until 5 dpi. In agreement with these initial finding,53 a recent pre-print paper similarly shows that SARS-CoV-2 infected K18-hACE2 mice lost ~10–15% weight by 5 dpi, which steadily decreased to 25% body weight by 7 dpi.54 They had high viral lung titres from 2 dpi, accompanied by modest viral titres in the heart, brain, kidney and spleen. Declines in pulmonary function were notable at 7 dpi evidenced by reduced inspiratory capacity and increased tissue resistance and elastance. RNA-sequencing analysis of infected lung tissues identified the upregulation of innate immune signatures, particularly NF-kB-dependent, type I and II IFN signalling and leucocyte activation pathways. Another pre-print paper shows that SARS-CoV-2 infected K18-hACE2 mice produce a robust Th1/2/17 cytokine storm in the lungs and spleens from 2 dpi,55 highlighting the relevance of this mouse model that recapitulates critical human clinical features of COVID-19. Importantly, multiple reports have shown that SARS-CoV-2 infection of K18-hACE2 mice is dose-dependently fatal from 5 dpi,55, 56, 57 suggesting that it is similarly lethal as SARS-CoV39 in these transgenic mice.
Adenoviral systems
Adenovirus vector-based systems can be used to insert human receptors into mouse genomes and are valuable for use with already factor-deficient or transgenic mice. Replication-defective adenovirus vectors have been used to insert hDDP4 into WT mice rendering them susceptible to MERS-CoV infection.58 Infected mice developed pneumonia with extensive pulmonary immune cell infiltration and viral clearance by 6 dpi58 but were less affected than fully hDPP4 transgenic mice.
Similarly, transduction of BALB/c mice with adenovirus containing hACE2 (AdV-hACE2) led to stable hACE2 expression in the lungs from 10 h post-transfection.59 SARS-CoV-2 infected AdV-hACE2 mice had ~10% weight loss over 8 days, high viral lung titres and modest titres in the heart, brain, liver and spleen, extensive neutrophil accumulation in perivascular and alveolar locations and vascular congestion upon histological examination. Administration of anti-IFNAR1 monoclonal antibodies to transiently inhibit type-I IFN signalling resulted in up to 20% weight loss and more severe lung inflammation, compared to infection alone. In this system, neutralizing antibodies against SARS-CoV-2 S protein (1B07) were protective against severe disease. Mice lost less body weight and had lower viral titres in the lung, heart and spleen at 4 dpi, and reduced expression of pro-inflammatory cytokines and chemokines (Ifnb, Il6, Cxcl10, Cxcl1, Ccl2, Ccl5) and immune cell infiltrates in the lungs at 6 dpi.
CRISPR systems
Using CRISPR/Cas9, an alternative humanised hACE2 mouse model was developed where the mACE2 was disrupted by inserting hACE2 linked to the red fluorescent protein TdTomato.60 hACE2 expression is under the control of the mACE2 promoter in the native locus, with expression predominantly in the lungs and kidneys, similar to mACE2 in WT mice. SARS-CoV-2 infected humanized hACE2 mice had high viral titres in the brain, trachea and lungs with no differences between young and aged mice. However, infected aged mice had lung neutrophilia and extensive alveolar thickening, vascular injury and focal hemorrhaging compared to young mice. Intragastric infection resulted in high viral titres in the trachea and lungs, suggesting that the oral administration route can lead to productive pulmonary infection.
Mouse-adapted viruses
Viruses can be adapted to infect WT mice through serial passaging or targeted mutation. Their use is advantageous as they reduce biological risks to researchers and may more closely resemble natural host-pathogen interactions in mice. However, they are limited due to mouse adaptation that may result in infection that does not recapitulate all aspects of human disease.
This approach was applied to SARS-CoV, which was serially passaged in the respiratory tracts of young BALB/c mice. This led to the generation of a mouse-adapted SARS-CoV strain (MA15) which was lethal to mice from 3 dpi.61 Infection resulted in high viral titres in the lungs from 1 dpi, followed by viremia and diffusion to extra-pulmonary sites including the brain, liver and spleen, significant lymphopenia and neutrophilia, mild and focal pneumonitis and necrotic cellular debris in the airways and alveoli. Another mouse-adapted SARS-CoV strain (v2163) was produced by serial passage in 6-week-old BALB/c mice.62 Infection resulted in more severe symptoms and higher mortality rate than with MA15, with greater immune responses and lung pathology. Mouse-adapted SARS-CoV strains lacking the critical viral envelope I protein induce varying degrees of protection against re-infection with virulent strains, highlighting the potential for live-attenuated vaccines.63, 64
Serial passage of MERS-CoV through the lungs of mice with human modified exons 10–12 of DPP4 resulted in a virus that induced significant weight loss and mice became moribund from 4 dpi. Mice had high stable viral titres in the lungs and blood, inflammatory cell infiltrates, and oedema, necrotic debris and vascular permeabilization in lungs.47
Mouse-adapted SARS-CoV-2 has been reported in a preprint, with mutations in the receptor binding domain (RBD) of the spike protein following serial passage, inducing productive infection of both young and aged WT BALB/c mice.65 Infected mice had high viral lung loads up to 7 dpi, and displayed mild pneumonia with inflammatory cell infiltration, alveolar damage, focal exudation and haemorrhage and endothelial cell denaturation. The efficacy of a RBD-Fc based vaccine was examined in this model, which induced the production of neutralizing antibodies which potently inhibited the infection. A similar preprint describes the modification of the RBD of the SARS-CoV-2 S protein, which facilitated the efficient binding of the S protein to mACE2 for host cell entry.66 Infection with this virus resulted in viral replication in the upper and lower airways of young and aged BALB/c mice. Aged mice had greater weight loss and pulmonary function decline compared to young mice, reproducing important aspects of human disease.
A summary of the different mouse models that are permissive to SARS-CoV-2 infection (Table 1 ) and a comparison of features between mouse models and human COVID-19 (Fig. 2 ) are shown.
Table 1.
Summary of available mouse models used to examine SARS-CoV-2 pathogenesis.
| Mouse line | Promoter | hACE2 expression and localisation | Infectious doses | Disease outcome | Reference |
|---|---|---|---|---|---|
| hACE2-HB-01 | mACE2 promoter | High expression in intestine and kidney. Moderate expression in heart. Low expression in lungs. |
Up to 1 × 106 TCID50 | Mice lost ~10% body weight but all recovered. High viral titres in the lung, no obvious clinical signs. No morbidity. | 42,51 |
| HFH4-hACE2 | Forkhead transcription factor (HFH4/FOXJ1) | High expression in lungs, gut and brain. Low expression in liver and kidneys. | 3 × 104 PFU | Proportion of mice lost >20% body weight and died. Moribund mice had neutrophilia and severe lung damage evidenced by histopathology. | 52,53 |
| K18-hACE2 | Cytokeratin 18 (K18) High expression in lungs and colon. Moderate expression in small intestine, spleen, kidney, liver and heart. Low expression in brain. |
8 × 104 TCID50 | ~10% weight loss and symptomatic disease by 5 dpi. High viral titres and inflammatory cell counts in lungs. Extensive lung inflammation and histopathology. | 40,54 | |
| Up to 2 × 104 PFU | ~30% weight loss by 7 dpi. High viral lung titres by 3 dpi. Extensive lung and brain inflammation and histopathology. | 40,57 | |||
| 2.5 × 104 PFU | ~25% weight loss by 7 dpi. High viral titres in the lungs, and modest viral titres in the heart, brain, kidney and spleen from 2 dpi. Reduced respiratory capacity from 7 dpi. RNA-seq of infected lung tissue shows high upregulation for innate immune response pathways. | 40,55 | |||
| 1 × 105 PFU | ~20% weight loss by 5 dpi, with uniform mortality by 6 dpi. High viral titres in the lung from 2 dpi, as well as moderate viral titres in the nasal turbinates and brain from 2–4 dpi. Cytokine storm observed in lungs and spleen from 2 dpi. | 40,56 | |||
| AdV-hACE2 | HFH4 under control of cytomegalovirus promoter in incompetent adenoviral vector | High expression in lungs. Expression in other tissues not reported. | 105 FFU | Mice lost ~10% body weight over 8 days. High viral lung titres reported. No reported mortality. | 56 |
| Humanised ACE2 | Native mACE2 promoter | High expression in lungs, small intestine, spleen and kidney. Low expression in brain, ovary and heart. | 4 × 105 PFU | Mice had high viral titres in brain, trachea and lung. Aged mice lost 10% body weight. No obvious clinical signs. | 57 |
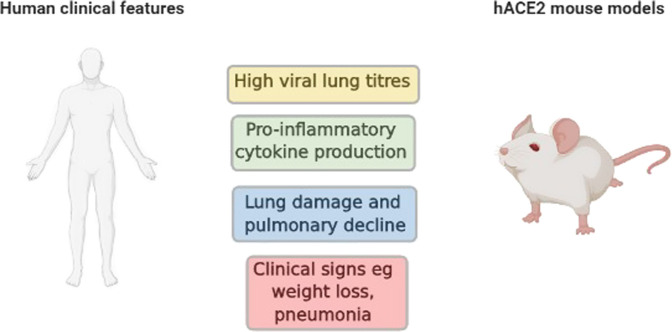
Fig. 2.
Comparison of disease features shared between humans with COVID-19 and mouse models of SARS-CoV-2. Both humans and mice display similar clinical signs such as weight loss and pneumonia. Severe infections are often associated with increased pro-inflammatory cytokine production, accompanied by high viral lung titres which correlates with extensive lung damage and significant pulmonary decline.
Diversified models
The immediate aim of producing infection-permissive mice or mouse-adapted viruses is to generate models with high respiratory viral titres and lung lesions resembling those observed in humans. Host factors are associated with increased risk of severe complications including age and obesity67 and comorbidities like COPD, CVD and diabetes.68 Human genetic variants likely modulate susceptibility to COVID-19.69
In mice, the impact of host genetic variations were investigated in SARS-CoV using the collaborative cross (CC), a collection of mouse inbred strains produced by crossing eight founder inbred strains, including five classic laboratory strains (A/J, C57BL/6J, 129S1/SvImJ, NOD/ShiLtJ and NZO/HiLtJ) and three wild-derived (CAST/EiJ, PWK/PhJ and WSB/EiJ) strains.70 CC strains segregate ~45 million polymorphisms and have more genetic diversity than the human population.71 This resource is ideally suited for investigating the role of host genetic variants in the pathophysiology of infectious diseases.72 MA15 infected CC mice had a broad range of phenotypes including weight loss and increased lung viral titres and lung pathology.73 Susceptibility varied from absence of symptoms to 100% mortality with normal lung parenchyma and lung viral titres at 4 dpi that varied over 6 log units. Genetic analysis of CC strains identified Trim55 and Ticam2 as host susceptibility genes.73, 74 This shows that the genetic background of mice is important in replicating distinct human clinical presentations. Investigating multiple genetic backgrounds is possible using adenovirus-transduced hACE2 or mouse-adapted viruses.
Predisposing risk factors and mouse models
Chronic diseases like COPD, asthma, lung fibrosis, CVD, diabetes mellitus as well as obesity, male sex and old age are associated increased susceptibility to SARS-CoV-2 infection and severe COVID-19.18, 75, 76, 77, 78, 79 Animal models that combine these risk factors with infection will be invaluable in elucidating mechanisms of increased susceptibility and severity.80, 81
Chronic respiratory diseases
Both cigarette smoking (CS) and COPD are strong independent risk factors for severe COVID-19 with extensive lung damage and increased mortality.82 CS upregulates ACE2 expression in the airways, which may increase infection risk.83 The use of short-term murine models that replicate CS-induced COPD has greatly increased our understanding of disease and identified and tested novel therapeutic interventions.80, 81, 84, 85, 86, 87, 88
Early data from China showed asthma prevalence in COVID-19 patients were lower than the general population suggesting that asthma may be protective.89 However, emerging reports show that asthma is one of the most prevalent comorbidities in hospitalized COVID-19 patients90 and is associated with higher risk of death, especially in severe asthma based on oral corticosteroid use.21 Elucidating how severe asthma predisposes to severe COVID-19 is needed and can be achieved using preclinical animal models of severe asthma that recapitulate the human disease,91, 92, 93 K18-hACE2 mice, and SARS-CoV-2 infection.
Lung fibrosis is the most severe sequelae of COVID-19 in up to 45% of the patients after 6 months.94, 95, 96, 97 The mechanisms are unclear but inflammation and cytokine storm likely contribute.7 SARS-CoV-2 infection of human alveolar epithelial cells results in altered profibrotic gene expression similar to pulmonary fibrosis, including ACE2, TGF-β, connective tissue growth factor, tissue inhibitor of metalloproteinase-3 and fibronectin.98 Fibrotic sequalae can be assessed in mouse models with long rest periods after infection.86, 99 Bleomycin-induced experimental pulmonary fibrosis could be combined with SARS-CoV-2 infection to investigate sequalae.86, 99
Obesity, diabetes and CVD
Mouse models of genetic or dietary modifications to induce features of human disease are widely available.86, 87, 100, 101 Inbred mouse strains such as C57BL/B6 have genetic susceptibility to obesity and diabetes, while male mice and rats are more prone compared to females.101, 102, 103 ACE2 is highly expressed in heart tissues and so it is expected that CVD models will increased susceptibility to SARS-CoV-2 infection.104 The link between type 1 and/or 2 diabetes and ACE2 expression is unknown with conflicting reports on the levels of expression in diabetes progression and severity.105, 106 There are numerous mouse models of type 1 and 2 diabetes that are chemically or genetically induced and, for type 2 diabetes, typically incorporate obesity.107 SARS-CoV and SARS-CoV-2 infection has not yet been explored in these models but these mice will likely be highly susceptible to infection with pulmonary decline and increased mortality as observed in humans.
Age-related susceptibility
Old age is the main risk factor for severe COVID-19,108 which is attributed to comorbidity, immunosenescence, malnutrition, residential care and biological aging changes.109 ACE2 expression in human lungs may either be unchanged83 or decreased104 with old age, while expression is increased in the olfactory epithelium, which may contribute to susceptibility to SARS-CoV-2 infection.110 The significance of age is exemplified in murine models where infection of young BALB/c and C57BL/B6 mice with SARS-CoV resulted in high viral titres in the upper and lower airways, but with no disease or mortality.33 However, aged BALB/c mice had significant weight loss and severe disease with extensive alveolar damage and bronchiolitis.111 ACE2 levels are decreased in aged compared to younger mice which may explain differences in disease severity.112 It is unknown whether aged mice are susceptible to SARS-CoV-2 infection, however evidence from humanised ACE2 mice shows that aged mice display greater disease severity.60 Aged mice showed a reduced response to experimental vaccination for SARS-CoV, with lower levels of neutralizing antibodies than young mice,113 similar to responses to many vaccines in older people. Thus, studying aged mice is likely to be pivotal for developing treatments and vaccines for older people.
Ferrets
Ferrets have been extensively used to study influenza A virus (IAV) pathogenesis and transmission, since their respiratory tract is anatomically comparable to humans.114 ACE2 is most abundantly expressed on type-II alveolar and glandular epithelial cells in the trachea and bronchi of ferrets.115 Ferrets are susceptible to SARS-CoV infection with replication in the URT and LRT, increased body temperature, sneezing and alveolar damage.115, 116, 117
Recently, ferret ACE2 was shown to contain the critical residues required for binding by SARS-CoV-2 RBD.118 The animals were susceptible to SARS-CoV-2 infection with viral replication in the URT, however, only low levels of virus were detected in lungs.119, 120 Viral loads in the lung and nasal turbinates peaked at 4 dpi with clearance by 8 and 12 dpi, respectively. While infectious virus was not detected outside the respiratory tract, viral RNA was found in the intestine, saliva, urine, rectal swabs and faeces up to 8dpi. This suggests that SARS-CoV-2 preferentially replicates in the URT of ferrets. In line with this, disease is mild with reduced activity and occasional cough from days 2–6. In most studies, elevated body temperatures are observed from 2 dpi, returning to baseline by day 8 with no change in body weight.119, 121 Shi et al.,120 reported only 1 out of 3 ferrets developed fever and loss of appetite following intranasal inoculation with different SARS-CoV-2 isolates, suggesting isolate variability and dose may alter disease outcomes. Limited studies have examined immune responses to SARS-CoV-2 in ferrets. Intranasal infection induced serum neutralizing antibodies.119, 121 Another study compared transcriptional responses in cells from nasal washes of IAV and SARS-CoV-2-infected ferrets.122 The magnitude of antiviral and IFN responses were higher with IAV compared to SARS-CoV-2 infection, with unique enrichment for cell death and leucocyte activation in the latter. Kim et al.,119 used the ferret model to study SARS-CoV-2 transmission. Viral RNA was detectable in nasal washes from ferrets 48 h after direct contact with intranasally inoculated animals, suggesting transmission is rapid and can be transmitted prior to the peak of disease 4 dpi. All six ferrets that had direct contact developed elevated body temperatures. In contrast to direct contact, airborne transmission was less efficient with low levels of viral antigen detectable in nasal washes from two of six ferrets and infection was mild with no changes in body temperature. Overall, the ferret model of SARS-CoV-2 is limited as the infection is mild with little LRT involvement and no reported characteristics of severe disease in humans such as oedema or ARDS. They may provide a model to study SARS-CoV-2 transmission.
Golden hamster
Syrian Golden hamsters have been used to model a broad range of viral infections,123 and genetically modified animals have been generated.124, 125, 126 Hamsters are susceptible to SARS-CoV infection with comparable viral replication in the URT and LRT, but no clinical signs of disease other than reduce activity.111, 127, 128
In silico structural analysis predicts that SARS-CoV-2 S protein RBD effectively binds hamster ACE2.129, 130 Infection of hamsters with SARS-CoV-2 resulted in clinical signs such as ruffled fur, rapid breathing and weight loss from day 2 with recovery by 10–12 dpi.129 High levels of infectious virus were detected in the lung and nasal turbinates on days 2 and 4 and significant histological changes were observed including protein-rich lung fluid exudate, mononuclear cell infiltration, severe cell death and haemorrhage and alveolar damage. Transmission studies revealed efficient virus spread via direct contact between co-housed infected hamsters.129 Infectious virus was detectable in the lungs and nasal turbinates, accompanied by lung histology changes. Co-housed hamsters did not lose significant body weight suggesting the infection was less severe than with intranasally inoculation, likely due to differences in inoculum dose. This suggests that SARS-CoV-2 infection of hamsters is not dissimilar to humans and may be a model to study pathogenesis, and transmission and test potential therapeutics.
Non-human primates (NHPs)
NHP experiments account for only 5% of all animal research. Nevertheless, clinical translation of NHP studies is much greater than for other animal models, as they are closest to human pathophysiology and comply with FDA approvals.131 Consequently, several NHP species were investigated in SARS-CoV infection, including Cynomolgus and Rhesus Macaques, African Green Monkeys (AGMs, old-world monkeys) and Common Marmosets, Squirrel Monkeys and Mustard Tamarins (new-world monkeys).132, 133, 134, 135, 136, 137, 138, 139 Initial studies were performed in Cynomolgus Macaques and virus was isolated from nasal secretions and detected in lung samples.133 Pulmonary pathology indicative of interstitial pneumonia was confirmed and representative of mild human disease. They presented with a spectrum of clinical illness ranging from no symptoms to skin rash, decreased activity, cough and respiratory distress with old animals more likely to develop disease.134, 136, 139 Pulmonary inoculation of these Macaques caused infection of type-1 and -2 bronchoepithelial cells from 1–4 dpi, followed by extensive type-2 pneumocyte hyperplasia from 4–6 dpi.132, 137 Comparing Cynomolgus and Rhesus Macaques and AGMs infected with SARS-CoV, all had viral replication in nasal throat swabs and tracheal lavage but did not develop clinical disease. Viral replication was highest in AGM, followed by Cynomolgus then Rhesus Macaques. Neutralizing antibodies correlated with viral titres that peaked at day 2 and cleared in the upper and LRT by 8–10 dpi. AGMs had interstitial pneumonia and inflammation and lung oedema.135 In infected Rhesus Macaques, virus was detected from day 5 in nasopharyngeal swabs and different degrees of interstitial pneumonia occurred over 60 dpi. Changes were less marked at later time points, indicative of active healing and resolution of acute inflammation.140 Infection of Common Marmosets caused only mild disease, but led to both pulmonary and hepatic pathology at 2–7 dpi, including early interstitial pneumatosis and hepatic lesions, including multifocal hepatitis.141
NHP models were used to investigate MERS-CoV infection and develop remedial measures. Infected Rhesus Macaques developed mild-to-moderate respiratory disease142, 143, 144 representative of milder MERS cases, whereas infected Marmosets developed moderate-to-severe disease as observed in severe patients.145, 146
With the occurrence of COVID-19, learning from NHP models of SARS-CoV and MERS-CoV has been applied. A pathogenesis study compared historical reports of SARS-CoV infections with results from MERS-CoV or SARS-CoV-2 inoculated Rhesus Macaques. SARS-CoV infection induced severe lung lesions. With MERS-CoV infection, virus was detected mainly in type-II pneumocytes and there were mild lung lesions. In SARS-CoV-2 infection, virus was excreted from the nose and throat without clinical signs and was detected in ciliated epithelial cells of nasal, bronchial, and bronchiolar mucosae and in type-I and -II pneumocytes in foci of diffuse alveolar damage. It was concluded that SARS-CoV-2 causes COVID-19–like disease in Macaques and provides a model to test preventions and treatments.139 A preprint confirmed that SARS-CoV-2 causes respiratory disease lasting 8–16 days in Rhesus Macaques. Nose and throat swabs confirmed high viral loads, similar to those in human bronchoalveolar lavage; in one animal, prolonged rectal shedding occurred. Pulmonary infiltrates were visible in pulmonary X-rays. Thus, collectively, Macaques developed moderate disease similar to most human cases.147 As in humans, age matters in Rhesus Macaques. Three 3–5-year old and two 15-year old Macaques were intratracheally infected with SARS‐CoV‐2. Viral replication in nasopharyngeal and anal swabs and lung was higher in old compared to young monkeys over 14 dpi. Animals developed typical interstitial pneumonia characterized by inflammation and oedema with thickened alveolar septa. Only old Macaques exhibited diffuse severe interstitial pneumonia. Viral antigens were detected mainly in alveolar epithelial cells and macrophages.148 Others reported similar findings, where viral RNA was detected at higher levels and for longer in older Macaques, though none presented with severe symptoms observed in older human patients.139 Thus, as in humans SARS-CoV-2 is more infectious in older NHP.
Susceptibility of other NHP to SARS-CoV-2 is mostly unknown. A preprint reports comparison of infected old-world monkeys (12 Rhesus, 6 Long-tailed Macaques) and new-world monkeys (6 Common Marmoset) and found increased body temperatures in 12/12 Rhesus and 2/6 Long-tailed Macaques, but no fever in Marmosets. Only Macaques had chest radiographic abnormalities, although viral loads in blood, nasal, throat and anal swabs of all three species could be detected. Post-mortem, Rhesus and Long-tailed Macaques had viral loads in lung, bronchus and spleen, whereas none were detected in Marmosets. Thus, Rhesus Macaques appear to be most susceptible to SARS-CoV-2 infection, followed by Long-tailed Macaques and Marmosets.149
Another report of investigations of SARS-CoV-2 susceptibility among Apes compared ACE2 sequences in Chimpanzees, Bonobos, Gorillas, and Orangutans, and all African and Asian monkeys (Catarrhines). All species have the same set of 12 key amino acid residues similar to hACE2. Monkeys of the Americas, and some Tarsiers, Lemurs and Lorises, differed at significant contact residues, and protein modelling predicted these differences should greatly reduce the binding affinity of SARS-CoV-2 to ACE2, hence moderating susceptibility to infection. Other Lemurs are predicted to be closer to Catarrhines in susceptibility, suggesting that Apes, African and Asian monkeys and some Lemurs are likely to be susceptible to SARS-CoV-2, representing a critical threat to their survival.150
It is important to understand protective immunity in NHPs. In SARS-CoV-2 infected Rhesus Macaques high viral loads in the upper and LRT, pathologic evidence of viral pneumonia, and humoral and cellular immune responses were observed. After initial viral clearance, Macaques were re-challenged and presented with a 5 log10 reduction in viral loads in bronchoalveolar lavage and nasal mucosa compared to primary infection. These findings suggest that SARS-CoV-2 re-infections are mild due to protective immunity.151 Another study assessed SARS-CoV-2 DNA vaccine candidates consisting of six different forms of S proteins in 35 Rhesus Macaques. Vaccinated animals had similar humoral and cellular immune responses, including neutralizing antibody titres to those in convalescent humans and Macaques infected with SARS-CoV-2.151, 152 Single vaccination with the adenovirus-vectored vaccine ChAdOx1 COVID-19 induced humoral and cellular immune responses in Rhesus Macaques.153 Viral load was significantly reduced in bronchoalveolar lavage fluid and respiratory tract tissue and pneumonia was absent compared to unvaccinated infected controls. This vaccine is currently in phase I trials.154
Thus, while no NHP model fully reproduces all COVID-19 features observed in humans, AGMs are similar with respect to primary infection. However, little work has been done with AGMs on antibody and treatment responses. Most important aspects of disease are observed with NHP models and these can be used to evaluate preventions and treatments for COVID-19.
Other infected animals
Bats
While SARS-CoV-2 is clearly a suitable human virus, its origins remains elusive with a common ancestor of bat SARS-Like CoVs and SARS-CoV-2 existing ~40–70 years prior to emergence.155 Scientists are now searching for further evidence in wild bats and have performed infection studies with a non-native host bat species, Rousettus aegyptiacus. 156 While this species is divergent from the predicted host bat families, Rhinolophidae/Hipposideridae, 157 intranasal inoculation resulted in URT infection with shedding of live virus and bat-to-bat transmission although somewhat limited. Oral swabs were positive for nucleic acid from 2–12 dpi and nasal epithelium, trachea, lung, lung lymphatic tissue and faeces were positive, including from non-inoculated contact animals. Infection occurred to a lower extent in heart, skin, duodenum and adrenal glands in some animals. Live virus was cultivated from oral swabs, trachea and nasal epithelium only, indicating stronger URT than enteric infection. Bats developed weak antibody responses from 8 dpi. While tissue viral loads were similar between side-by-side bat and ferret infections, ferrets developed stronger neutralizing antibody responses. Fitting with known viral tolerance in bats, no clinical signs, weight loss, fever or respiratory signs were detected throughout infection. This matches observations in wild bats infected with SARS-like viruses, or experimentally infected bats with MERS-CoV158 and a HKU-9-like β-CoV.159 Antigens but only minor, transient inflammation with minor immune cell infiltration were detected at 4 dpi. In vivo bat infections, coupled with in vitro infection in cell lines and intestinal enteroids is possible160 but is logistically difficult and bats do not develop disease. Homology studies show that, particularly for immune genes and cytokines, bats are close to humans.161
Cats
SARS-CoV has been detected in wild cats,162 and cats can contract SARS-CoV-2 from their owners.163, 164, 165 Cats are susceptible to experimental infection120 and shed virus in nasal turbinates, soft palates, tonsils, tracheas, lungs, and small intestines with live virus in these tissues except intestines or faeces, suggesting minimal shedding of virus via that route. Viral RNA was cleared by 6 dpi from the lungs while remaining in other tissues. Juvenile cats had lower URT viral loads but prolonged viral RNA shedding in lung tissue. Concordant with this, there were varying degrees of respiratory illness in wild-infected cats. Cats are a suitable model for droplet transmission with 1/3 naïve cats in contact with infected cats developing infection and shedding viral RNA in tissue and faeces. Higher shedding was observed in juvenile cats, though sub-adult cats developed higher antibody titres. One study suggested minimal antibody seroprevalence in domestic cats166 and random sampling in Wuhan, China, revealed 14.7% seroprevalence in domestic cats post-outbreak.167 This suggests that spill-over from humans to cats may be frequent. Thus, cats as an animal model for infection reveal suitable infection and transmission dynamics. There is little information on inflammation and how this mirrors human disease.
Animals minimally infected: pig, dog, chicken, tree shrew
Other infections with SARS-CoV-2 of pig, dog, chicken and tree shrew have yielded limited results with none showing signs of disease, and only dogs displaying shedding in faeces only but not tissue.120 Another study confirmed no detectable infection in pigs or their cell lines.156 PCR positive domestic dogs were reported, though there was no evidence of respiratory disease.168 Viral RNA was detected from nasal swabs for almost whole genome sequencing and also live virus isolation in one canine. High Ct values were recorded from rectal swabs in one animal though there was no transmission to another dog in the same household. Chickens are sources of viral zoonotic diseases, like Newcastle disease and avian IAV.169, 170 Since IAVs replicate efficiently in chickens, infection of embryonated eggs is a common, cheap and efficient way of propagating them.171 However, chickens are largely resistant to SARS-CoV, MERS-CoV and SARS-CoV-2. Chickens inoculated intravenously, intranasally, ocularly and orally with SARS-CoV did not develop signs of disease or display pathological organ changes. Viral RNA was detected in blood, trachea, lung and kidney up to 14 dpi, but isolation of replicating viruses was unsuccessful.172 Chickens inoculated intranasally did not transmit the virus to co-housed, unchallenged counterparts.120 SARS-CoV, MERS-CoV and SARS-CoV-2 injected into embryonating eggs do not replicate.172, 173 Recently, the tree shrew (Tupaia belangeris) was examined for susceptibility to SARS-CoV-2 infection.174 Following infection, Shrews displayed no clinical signs except for increasing body temperature particularly in females. Moderate levels of viral shedding and tissue replication were consistent across all age groups, but was higher in kidney, pancreas and spinal cord. Histopathology revealed mild pulmonary abnormalities with inflammatory cell infiltration, airway obstruction and necrosis. Thus, none of these animals appear to be suitable for SARS-CoV-2 research.
Wild-caught positive animals
Whilst many animal species are infected with IAV175 and SARS-CoV infection, only a few are so far associated with SARS-CoV-2, many are likely susceptible that may depend on their phylogeny (Fig. 3 ). To date all are apparently anthropo-zoonotic infections from human to animal, including dog, cat, mink, tiger and lion.176 Studies of mink in farms in the Netherlands suggest a strain passed from an infected handler, actively transmitted amongst the mink population and infected another human, and viral RNA was detected in inhalable dust.177 Infected mink had respiratory disease with lung inflammation and interstitial pneumonia and mortality in some. This suggests that mink may be a better model then ferrets, though controlled studies are needed. Tigers and lions infected with SARS-CoV-2 had respiratory symptoms and loss of appetite though all recovered.176, 178 The genome of SARS-CoV-2 from a tiger in Bronx zoo shows close relationships to human strains, and various tissues and swabs were positive.179 Other SARS-CoV's including SARS-CoV have been detected in various Rhinolophus and Hipposideros species of bats, pangolins, Bamboo Rat, Palm Civet, Hog Badger, Hedgehog and Racoon Dog.12, 157, 180, 181, 182, 183, 184 A recent study suggests increasing coronavirus prevalence associated with the wildlife trade with increased disease along the trade route.185 Palm Civets and Racoon Dogs previously detected with SARS-CoV infection exhibited symptoms and signs of distress. Similarly, this was observed for smuggled Sunda Pangolins in China that were positive for the closely related Pangolin-CoV.186 They had respiratory distress with frothing at the lips and blood in their lungs. These studies show that a broad range of wild animals carry coronaviruses.
Fig. 3.
Phylogeny of observed wild infections. Left panel, fast minimum evolution distance tree for ACE2 protein sequences using Grishin for evolutionary distance, unsorted. Species included are Erinaceous europaeus (in place of Erinaceous amurensis, Hedgehog), Rhinolophus sinicus (representative microbat), Nyctereutes procyonoides (Racoon Dog), Manisjavanica (Sunda Pangolin), Paguma larvata (Masked Palm Civet), Mustela putoris furo (representative ferret), Panthera tigris altaica (Siberian Tiger, in place of Bengal Tiger), Canis lupus familiaris (Dog), Neovison vison (in place of European Mink). The closest species was used where applicable due to a lack of sequence for ACE2. Right side indicates whether infection was observed for SARS-CoV, SARS-CoV-2 or SARSr-CoV (Bat SARS-Like CoVs), as indicated. Green arrows indicate where animal-animal transmission has been reported to occur.
Translational models to humans
Analysis of the combination of complementary in vivo animal models and ex vivo human studies are powerful ways to better under disease and test preventions and treatments.
Cell models
Cell models for in vitro/ex vivo examination of SARS-CoV-2 are valuable for understanding viral replication and pathogenesis. They can be high-throughput systems for evaluating therapeutics and vaccine candidates. Vero and VeroE6 are kidney epithelial-derived cell lines commonly used for viral propagation.187 VeroE6 cells were used to identify ACE2 as the host cell receptor for SARS-CoV entry via binding the S protein.38 They are highly permissive to SARS-CoV and SARS-CoV-2 infection due to high expression of ACE2, however, TMPRSS2 is expressed at low levels.2, 3 Propagation of SARS-CoV-2 in VeroE6 cells abundantly expressing TMPRSS2 greatly exceeds standard VeroE6 propagation.3 Moreover, camostat mesylate, a clinically approved serine protease inhibitor of TMPRSS2, partially inhibits SARS-CoV-2 entry into Caco2 and VeroE6/TMPRSS2-expressing cells,2 reinforcing the applicability of cell culture models for drug discovery.
A broad screen of human cell lines showed that SARS-CoV-2 replication was most robust in Calu-3 (pulmonary), followed by Caco2 (intestinal), Huh7 (hepatic), HEK293T (renal), and U251 (neuronal) cells.11 Commonly used human cell lines such as HeLa (cervical cancer) and A549 (alveolar epithelial cancer) express low levels of ACE2188, 189 and are non-permissive to SARS-CoV-2 infection unless exogenously expressing ACE2.12, 13, 190 Furthermore, SARS-CoV-2 was able to efficiently replicate in a broad range of non-human cell lines such as FRhK4, LLCMK2 (both Rhesus Macaque kidney), CRFK (feline kidney) and RK-13 (Rabbit kidney), suggesting broad host and tissue susceptibility.11
Human minimally immortalised or primary bronchoepithelial cells are clearly human relevant and express ACE2. They can be cultured submerged191 or at the air-liquid interface (ALI) where they differentiate into pseudostratified mucociliary epithelium, grow cilia, produce mucus and maintain their disease phenotype.192, 193 They are the gold standard in vitro models of the upper, large and small airways. They can be infected with SARS-CoV-2 that replicates and inflammatory and immune responses, pathogenesis and treatments assessed.80, 81, 194, 195, 196 However, they have limited life spans (2–4 passages) so cells that resemble primary cell features but can be expanded are used for high-throughput screening. Growing primary cells co-cultured with irradiated fibroblast feeder cells and a Rho kinase inhibitor propagates these cells indefinitely in vitro and can be differentiated at ALI.197
Patrolling immune cells are critical host defences against pathogens and are important in protecting against COVID-19.198, 199 They may also be important infectious niches for SARS-CoV-2. THP-1 human monocytes are permissive to SARS-CoV infection,200, 201 however, current evidence suggests they are not susceptible to SARS-CoV-2.202 Nevertheless, THP-1 cells exposed to SARS-CoV-2 S protein produce IL-6,203 suggesting that macrophages have roles in COVID-19 pathogenesis independent of promoting SARS-CoV-2 infection. MT-2 T-lymphoid cells are also permissive to SARS-CoV-2 entry but not replication202, 204 similar to MERS-CoV.205 Whole blood infections can be used to assess mechanisms of pathogenesis and test treatments.206
Organoids
Organoids are three-dimensional tissue models derived from embryonic stem (ES), induced pluripotent (iPSCs)207, 208 or multi-potent adult tissue stem cells.209 Their strength is the ability to self-arrange into tissue structures that have the cytoarchitecture, cellular complexity and some functions of the organ they resemble.210 They include cell-to-cell interactions and organization, allowing for accurate representations of infection patterns, and improved resolution to determine cell-specific drug targets and toxicity. Benefits over 2D cell cultures are the ability to study SARS-CoV-2 tissue infectivity and effects on cell function. SARS-CoV-2 is primarily a respiratory infection which can lead to multi-organ failure and organoids can be used to investigate the causes and rapid testing of potential therapies. Importantly, human lung organoids have been developed211, 212 and used to study respiratory infections including IAV and tuberculosis,213 and will be important for investigating COVID-19 pathogenesis. One study used pluripotent stem cell-derived lung organoids and identified drug candidates including imatinib and mycophenolic acid, that inhibited SARS-CoV-2 entry.214 Organoids do present challenges in modelling the complex structure of the lung. They do not generally express vascularity and do not expand and contract during gas exchange as viable lungs do. However, when combined with animal models and other systems, organoids expand technical capabilities in investigating disease pathogenesis. COVID-19 patients also suffer severe endothelial, kidney, liver and neurological damage showing direct effects on these tissues.25, 215, 216, 217, 218 Recent organoids studies show that vascular, intestinal, kidney, brain and liver tissues are all permissive to SARS-CoV-2 and may be viral reservoirs.160, 219, 218, 219, 220, 221, 222 Soluble hACE2 could significantly reduce SARS-CoV-2 load in vascular and kidney organoids, and is in a multicentre clinical trial for COVID-19 therapy.223 Cholangiocytes in liver ductal organoids express ACE2 and TMPRSS2 that enable SARS-CoV-2 infection that impairs their barrier and bile acid transporting functions.222 Enterocytes, express high levels of ACE2, can be infected and show a generic viral response program, including type-I and -III IFNs.219, 222, 224 Bat enteroids can also be generated and infected with SARS-CoV-2, indicating animal tissues may be suitable for organoid-derived studies enabling validation and translation.160 SARS-CoV-2 infection of human brain organoids shows viral tropism for cortical neurons but not neuronal stem cells.225, 226 The virus co-localized with phosphorylated Tau, suggesting early neurodegeneration-like effects.
Tissue explants
Whole primary host-derived tissues that can be manipulated are ex vivo system for understanding tissue-specific responses and pre-clinical drug screening. Precision cut lung slices (PCLS) are used to assess immunology, toxicology and airway reactivity as they maintain lung architecture, cell–cell, cell-matrix and tissue interactions. They enable investigation of whole tissue immune responses to a virus from airway, vascular, parenchymal and resident immune cells, without confounding effects from systemic cells that migrate to the lung following challenge in vivo. Multiple sections can be obtained from a single lung, including human,227 Rhesus Macaques,228 marmosets229 and mice.230, 231, 232 SARS-CoV-2 replication in PCLS has not been established, but other viruses such as Adenovirus Type-7 can replicate in human,233 swine IAV can replicate in pig234 and respiratory syncytial virus can replicate in mouse PCLS.235 The complexity of PCLS maintaining all cell types in their in vivo configuration is an advantage other culture techniques and the ability to directly compare between species is translational.
Translating findings
The clinical relevance of individual animal models and ex vivo systems for translation of preventive and therapeutic interventions into clinical practice will depend on their characteristics.
Anti-viral efficacy
Although antiviral activity may be demonstrated in cell cultures, efficacy against infection must be confirmed in animal models prior to human studies. Remdesivir (GS-5734) that inhibits viral RNA-dependent RNA polymerase was confirmed to be active in murine236 and Rhesus Macaque145 models of SARS-CoV and MERS-CoV infection before evaluation in a recent randomized controlled trial showing clinical benefit against SARS-CoV-2.237 This is also relevant for testing passive antibody therapy. A recombinant human monoclonal antibody showed prophylactic and therapeutic efficacy against SARS-CoV-2 in infected hACE2 mice,238 while another neutralizing antibody controlled SARS-CoV2 in golden hamsters.239 These models also provide pharmacokinetic data on drug dosing, and permit rapid translation to human studies through established conversions.240
Vaccine-induced protective immunity
Animal models are essential for developing SARS-CoV-2 vaccines. A variety of protein, RNA and viral vaccines have been tested in mice and NHPs to induce anti-SARS-CoV-2 antibodies that are neutralizing against infection of human cell lines in vitro.241, 242, 243 This provides a rapid screen for potential protective efficacy but these must be tested in challenge models. Recent studies with Chimpanzee adenovirus (ChAdOx1 nCoV-19)153 and vesicular stomatitis virus (rVSV-ΔG)244 vaccines expressing the S protein showed protection against SARS-CoV-2 lung disease and inhibited viral replication in NHP and golden hamsters, respectively. Similarly, S protein bearing nanoparticles induced a broad range of antibody and CD4+ and CD8+ T cell responses in mice and protected against SARS-CoV-2 infection.243 There are >130 SARS-CoV-2 vaccines in development and it is important to compare their efficacy in multiple models to select those most likely to provide durable immunity in humans.
Modifying lung inflammation
The critical determinant of clinical outcome in COVID-19 is the excessive lung inflammation that develops in 15–20% and progresses to severe disease in the 4% requiring ICU care. Animal models of infection will provide insights into the pathophysiology of this inflammation and the relative contributions of innate immune and adaptive T-cell responses, and provide a platform to test anti-inflammatories. In MERS-CoV infection of DPP4 transgenic mice, C5a receptor neutralization alleviated lung inflammation, confirming important roles for complement activation.245
Treating vascular damage
Emerging studies show extensive vascular inflammation in the lung and other organs in COVID-19 patients. This includes extensive endothelial cell inflammation and small and large vessel thrombosis in the lungs in fatal COVID-19,25 and widespread brain inflammation and vascular damage post-mortem.246 It is unknown if these findings are replicated in different animal models and this will be an important area of future investigation.
Conclusions
Interrogation of representative animal models is needed to define cause and effect and elucidate mechanisms of pathogenesis that are validated and translated in human studies (Fig. 4 ). They need to replicate human disease features individually and collectively. Mice that are modified genetically or with adenoviruses or CRISPR, or WT mice infected with mouse-adapted viruses will undoubtedly be the most widely used due to ease and costs but also because they replicate human features of pulmonary inflammation, histopathology and pneumonia. New studies will define additional features and refine models to achieve these, and also incorporate representative models of chronic diseases to define and treat mechanisms of increased susceptibility to infection and COVID-19. Other animal models may be useful but pose substantial logistical issues. NHPs are closer to humans and can be used to test interventions prior to human treatment. Wild animals such as bats are important natural reservoirs of coronavirus and should be avoided. Refined translational in vitro/ex vivo platforms enable validation and translation of animal model findings including primary cells cultured at ALI, organoids and primary tissue explants that can be infected and immune responses and interventions assessed. Translation of findings to humans will enable us to elucidate the mechanisms of pathogenesis and develop and test preventions and interventions and combat COVID-19 to return the world to a semblance of normality.
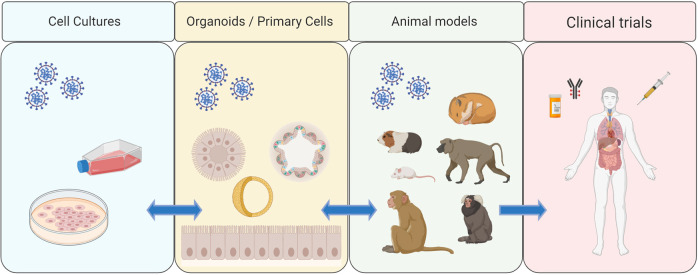
Fig. 4.
Overview of the different translational model systems used to interrogate disease mechanisms of SARS-CoV-2. Cell culture and organoid/primary cell infection studies are critical for deciphering the cellular mechanisms of SARAS-CoV-2 pathogenesis and for high-throughput identification of leading drug candidates. In vitro findings can then be directly translated to animal models such as mice, hamsters, guinea pigs and non-human primates to assess the safety and efficacy of drugs and vaccines before progressing to human clinical trials.
ADDITIONAL INFORMATION
Publisher's note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Acknowledgments
P.M.H. is funded by a Fellowship from the National Health and Medical Research Council (NHMRC) of Australia (1175134), the Rainbow Foundation and UTS. M.D.T. is funded by a Fellowship from the NHMRC (1181522).
Footnotes
Published online: 20 August 2020
Author contributions
All authors contributed to the writing of this manuscript.
Competing interests
The authors declare no competing interests.
References
* Publications that have not been peer-reviewed and are available on pre-publication servers.
- 1.WHO. WHO Coronavirus Disease (COVID-19) Dashboard, https://covid19.who.int/ (2020).
- 2.Hoffmann M, et al. SARS-CoV-2 cell entry depends on ACE2 and TMPRSS2 and is blocked by a clinically proven protease inhibitor. Cell. 2020;181:271–280. doi: 10.1016/j.cell.2020.02.052. 1:CAS:528:DC%2BB3cXktl2qtb8%3D, 7102627, 32142651. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Matsuyama S, et al. Enhanced isolation of SARS-CoV-2 by TMPRSS2-expressing cells. Proc. Natl Acad. Sci. USA. 2020;117:7001–7003. doi: 10.1073/pnas.2002589117. 1:CAS:528:DC%2BB3cXmt1Gju7w%3D, 7132130, 32165541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Berlin, D. A., Gulick, R. M. & Martinez, F. J. Severe Covid-19. N. Engl. J. Med. NEJMcp2009575 (2020, in press). [DOI] [PubMed]
- 5.Ong EZ, et al. A dynamic immune response shapes COVID-19 progression. Cell Host Microbe. 2020;27:879–882. doi: 10.1016/j.chom.2020.03.021. 1:CAS:528:DC%2BB3cXovVCgs70%3D, 7192089, 32359396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Gibson PG, Qin L, Puah SH. COVID-19 acute respiratory distress syndrome (ARDS): clinical features and differences from typical pre-COVID-19 ARDS. Med. J. Aust. 2020;213:54–56. doi: 10.5694/mja2.50674. 32572965. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.George PM, Wells AU, Jenkins RG. Pulmonary fibrosis and COVID-19: the potential role for antifibrotic therapy. Lancet Resp. Med. 2020;8:807–815. doi: 10.1016/S2213-2600(20)30225-3. 1:CAS:528:DC%2BB3cXpsFCgu7g%3D. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Gautret, P. et al. Hydroxychloroquine and azithromycin as a treatment of COVID-19: results of an open-label non-randomized clinical trial. Int. J. Antimicrob. Agents, 105949 (2020). [DOI] [PMC free article] [PubMed] [Retracted]
- 9.Horby, P. et al. Dexamethasone in Hospitalized Patients with Covid-19 — Preliminary Report. N. Engl. J. Med. NEJMoa2021436 (2020, in press).
- 10.Zhu N, et al. A novel coronavirus from patients with pneumonia in China, 2019. N. Engl. J. Med. 2020;382:727–733. doi: 10.1056/NEJMoa2001017. 1:CAS:528:DC%2BB3cXjslGmsrc%3D, 7092803, 31978945. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Chu H, et al. Comparative tropism, replication kinetics, and cell damage profiling of SARS-CoV-2 and SARS-CoV with implications for clinical manifestations, transmissibility, and laboratory studies of COVID-19: an observational study. Lancet Microbe. 2020;1:e14–e23. doi: 10.1016/S2666-5247(20)30004-5. 1:CAS:528:DC%2BB3cXit1Kms73M, 7173822, 32835326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Zhou P, et al. A pneumonia outbreak associated with a new coronavirus of probable bat origin. Nature. 2020;579:270–273. doi: 10.1038/s41586-020-2012-7. 1:CAS:528:DC%2BB3cXksFKlsLg%3D, 7095418, 32015507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ou X, et al. Characterization of spike glycoprotein of SARS-CoV-2 on virus entry and its immune cross-reactivity with SARS-CoV. Nat. Commun. 2020;11:e1620. doi: 10.1038/s41467-020-15562-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Xu, H. et al. High expression of ACE2 receptor of 2019-nCoV on the epithelial cells of oral mucosa. Int. J. Oral Sci.12 (2020, in press). [DOI] [PMC free article] [PubMed]
- 15.Wang Y, Liu M, Gao J. Enhanced receptor binding of SARS-CoV-2 through networks of hydrogen-bonding and hydrophobic interactions. Proc. Natl Acad. Sci. USA. 2020;117:13967–13974. doi: 10.1073/pnas.2008209117. 1:CAS:528:DC%2BB3cXhsVCgsrrN, 7322019, 32503918. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lauer SA, et al. The incubation period of coronavirus disease 2019 (COVID-19) from publicly reported confirmed cases: estimation and application. Ann. Intern. Med. 2020;172:577–582. doi: 10.7326/M20-0504. 32150748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Guan W-j, et al. Clinical characteristics of coronavirus disease 2019 in China. N. Engl. J. Med. 2020;382:1708–1720. doi: 10.1056/NEJMoa2002032. 1:CAS:528:DC%2BB3cXovVSjsb8%3D, 32109013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Wu C, et al. Risk factors associated with acute respiratory distress syndrome and death in patients with coronavirus disease 2019 pneumonia in Wuhan, China. JAMA Intern. Med. 2020;180:934–943. doi: 10.1001/jamainternmed.2020.0994. 1:CAS:528:DC%2BB3cXhsVWjs77M, 32167524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Chen T, et al. Clinical characteristics of 113 deceased patients with coronavirus disease 2019: retrospective study. BMJ. 2020;368:m1091. doi: 10.1136/bmj.m1091. 7190011, 32217556. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Du R-H, et al. Predictors of mortality for patients with COVID-19 pneumonia caused by SARS-CoV-2: a prospective cohort study. Eur. Respiratory J. 2020;55:2000524. doi: 10.1183/13993003.00524-2020. 1:CAS:528:DC%2BB3cXhvFelsrvF. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Williamson, E. J. et al. OpenSAFELY: factors associated with COVID-19 death in 17 million patients. Nature, s41586-020-2521-4 (2020, in press).
- 22.Sungnak W, et al. SARS-CoV-2 entry factors are highly expressed in nasal epithelial cells together with innate immune genes. Nat. Med. 2020;26:681–687. doi: 10.1038/s41591-020-0868-6. 1:CAS:528:DC%2BB3cXotVCjurY%3D, 8637938, 32327758. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Xu Z, et al. Pathological findings of COVID-19 associated with acute respiratory distress syndrome. Lancet Respir. Med. 2020;8:420–422. doi: 10.1016/S2213-2600(20)30076-X. 7164771, 1:CAS:528:DC%2BB3cXjsValtbk%3D, 32085846. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Buja LM, et al. The emerging spectrum of cardiopulmonary pathology of the coronavirus disease 2019 (COVID-19): report of 3 autopsies from Houston, Texas, and review of autopsy findings from other United States cities. Cardiovasc. Pathol. 2020;48:107233. doi: 10.1016/j.carpath.2020.107233. 1:CAS:528:DC%2BB3cXpsFCrtbw%3D, 7204762, 32434133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ackermann M, et al. Pulmonary vascular endothelialitis, thrombosis, and angiogenesis in Covid-19. N. Engl. J. Med. 2020;383:120–128. doi: 10.1056/NEJMoa2015432. 1:CAS:528:DC%2BB3cXhsVeis7jK, 7412750, 32437596. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Li C, et al. IL-17 response mediates acute lung injury induced by the 2009 pandemic influenza A (H1N1) virus. Cell Res. 2012;22:528–538. doi: 10.1038/cr.2011.165. 1:CAS:528:DC%2BC38Xjt1Wjurs%3D, 22025253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Mahallawi WH, Khabour OF, Zhang Q, Makhdoum HM, Suliman BA. MERS-CoV infection in humans is associated with a pro-inflammatory Th1 and Th17 cytokine profile. Cytokine. 2018;104:8–13. doi: 10.1016/j.cyto.2018.01.025. 1:CAS:528:DC%2BC1cXisVSltb8%3D, 7129230, 29414327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Tan L, et al. Lymphopenia predicts disease severity of COVID-19: a descriptive and predictive study. Signal Transduct. Tar. Ther. 2020;5:e33. doi: 10.1038/s41392-020-0148-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Diao B, et al. Reduction and functional exhaustion of T cells in patients with coronavirus disease 2019 (COVID-19) Front. Immunol. 2020;11:e827. doi: 10.3389/fimmu.2020.00827. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Hadjadj, J. et al. Impaired type I interferon activity and inflammatory responses in severe COVID-19 patients. Science, eabc6027 (2020). [DOI] [PMC free article] [PubMed]
- 31.Qin C, et al. Dysregulation of immune response in patients with COVID-19 in Wuhan, China. Clin. Infect. Dis. 2020;71:762–768. doi: 10.1093/cid/ciaa248. 1:CAS:528:DC%2BB3cXhsF2mt7fF, 32161940. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Pacha O, Sallman MA, Evans SE. COVID-19: a case for inhibiting IL-17? Nat. Rev. Immunol. 2020;20:345–346. doi: 10.1038/s41577-020-0328-z. 1:CAS:528:DC%2BB3cXosVersb0%3D, 7194244, 32358580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Subbarao K, et al. Prior infection and passive transfer of neutralizing antibody prevent replication of severe acute respiratory syndrome coronavirus in the respiratory tract of mice. J. Virol. 2004;78:3572–3577. doi: 10.1128/JVI.78.7.3572-3577.2004. 1:CAS:528:DC%2BD2cXis1Klur4%3D, 371090, 15016880. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Glass WG, Subbarao K, Murphy B, Murphy PM. Mechanisms of host defense following severe acute respiratory syndrome-coronavirus (SARS-CoV) pulmonary infection of mice. J. Immunol. 2004;173:4030–4039. doi: 10.4049/jimmunol.173.6.4030. 1:CAS:528:DC%2BD2cXnsVWktL0%3D, 15356152. [DOI] [PubMed] [Google Scholar]
- 35.Hogan RJ, et al. Resolution of primary severe acute respiratory syndrome-associated coronavirus infection requires Stat1. J. Virol. 2004;78:11416–11421. doi: 10.1128/JVI.78.20.11416-11421.2004. 1:CAS:528:DC%2BD2cXotlKisbk%3D, 521834, 15452265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Frieman MB, et al. SARS-CoV pathogenesis is regulated by a STAT1 dependent but a type I, II and III interferon receptor independent mechanism. PLOS Pathog. 2010;6:e1000849. doi: 10.1371/journal.ppat.1000849. 2851658, 20386712. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Gretebeck LM, Subbarao K. Animal models for SARS and MERS coronaviruses. Curr. Opin. Virol. 2015;13:123–129. doi: 10.1016/j.coviro.2015.06.009. 4550498, 26184451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Li W, et al. Angiotensin-converting enzyme 2 is a functional receptor for the SARS coronavirus. Nature. 2003;426:450–454. doi: 10.1038/nature02145. 1:CAS:528:DC%2BD3sXpt1GlsLs%3D, 7095016, 14647384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.McCray PB, Jr., et al. Lethal infection of K18-hACE2 mice infected with severe acute respiratory syndrome coronavirus. J. Virol. 2007;81:813–821. doi: 10.1128/JVI.02012-06. 1:CAS:528:DC%2BD2sXms1Smsw%3D%3D, 17079315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Netland J, Meyerholz DK, Moore S, Cassell M, Perlman S. Severe acute respiratory syndrome coronavirus infection causes neuronal death in the absence of encephalitis in mice transgenic for human ACE2. J. Virol. 2008;82:7264–7275. doi: 10.1128/JVI.00737-08. 1:CAS:528:DC%2BD1cXovVSltr4%3D, 2493326, 18495771. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Yang XH, et al. Mice transgenic for human angiotensin-converting enzyme 2 provide a model for SARS coronavirus infection. Comp. Med. 2007;57:450–459. 1:CAS:528:DC%2BD2sXht1SjtrbK, 17974127. [PubMed] [Google Scholar]
- 42.Coleman CM, Frieman MB. Coronaviruses: important emerging human pathogens. J. Virol. 2014;88:5209–5212. doi: 10.1128/JVI.03488-13. 4019136, 24600003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Agrawal AS, et al. Generation of a transgenic mouse model of Middle East respiratory syndrome coronavirus infection and disease. J. Virol. 2015;89:3659–3670. doi: 10.1128/JVI.03427-14. 1:CAS:528:DC%2BC2MXkvFKgu7Y%3D, 4403411, 25589660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Barlan A, et al. Receptor variation and susceptibility to Middle East respiratory syndrome coronavirus infection. J. Virol. 2014;88:4953–4961. doi: 10.1128/JVI.00161-14. 3993797, 24554656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Cockrell AS, et al. Mouse dipeptidyl peptidase 4 is not a functional receptor for Middle East Respiratory syndrome coronavirus infection. J. Virol. 2014;88:5195–5199. doi: 10.1128/JVI.03764-13. 3993820, 24574399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.van Doremalen N, et al. Host species restriction of Middle East respiratory syndrome coronavirus through its receptor, dipeptidyl peptidase 4. J. Virol. 2014;88:9220–9232. doi: 10.1128/JVI.00676-14. 4136254, 24899185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Cockrell AS, et al. A mouse model for MERS coronavirus-induced acute respiratory distress syndrome. Nat. Microbiol. 2016;2:e16226. doi: 10.1038/nmicrobiol.2016.226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Li K, et al. Mouse-adapted MERS coronavirus causes lethal lung disease in human DPP4 knockin mice. Proc. Natl Acad. Sci. USA. 2017;114:E3119–E3128. doi: 10.1073/pnas.1619109114. 1:CAS:528:DC%2BC2sXkvF2iur8%3D, 5393213, 28348219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Letko M, Marzi A, Munster V. Functional assessment of cell entry and receptor usage for SARS-CoV-2 and other lineage B betacoronaviruses. Nat. Microbiol. 2020;5:562–569. doi: 10.1038/s41564-020-0688-y. 1:CAS:528:DC%2BB3cXjvFyitL0%3D, 32094589. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Bao L, et al. The pathogenicity of SARS-CoV-2 in hACE2 transgenic mice. Nature. 2020;583:830–833. doi: 10.1038/s41586-020-2312-y. 1:CAS:528:DC%2BB3cXhsVCisrnM, 32380511. [DOI] [PubMed] [Google Scholar]
- 51.Jiang R-D, et al. Pathogenesis of SARS-CoV-2 in transgenic mice expressing human angiotensin-converting enzyme 2. Cell. 2020;182:50–58. doi: 10.1016/j.cell.2020.05.027. 1:CAS:528:DC%2BB3cXhtFWks7vJ, 7241398, 32516571. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Menachery VD, et al. SARS-like WIV1-CoV poised for human emergence. Proc. Natl Acad. Sci. USA. 2016;113:3048–3053. doi: 10.1073/pnas.1517719113. 1:CAS:528:DC%2BC28XktV2msr8%3D, 4801244, 26976607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Moreau, G. B. et al. Evaluation of K18-hACE2 Mice as a Model of SARS-CoV-2 Infection. Am. J. Tropical Med. Hygiene, ajtmh.20-0762 (2020, in press). [DOI] [PMC free article] [PubMed]
- 54.*Winkler, E. S. et al. SARS-CoV-2 infection in the lungs of human ACE2 transgenic mice causes severe inflammation, immune cell infiltration, and compromised respiratory function. Preprint at 10.1101/2020.07.09.196188 (2020). [DOI]
- 55.*Oladunni, F. S. et al. Lethality of SARS-CoV-2 infection in K18 human angiotensin converting enzyme 2 transgenic mice. Preprint at 10.1101/2020.07.18.210179 (2020). [DOI] [PMC free article] [PubMed]
- 56.*Golden, J. W. et al. Human angiotensin-converting enzyme 2 transgenic mice infected with SARS-CoV-2 develop severe and fatal respiratory disease. Preprint at 10.1101/2020.07.09.195230 (2020). [DOI] [PMC free article] [PubMed]
- 57.*Perlman, S. & McCray, P. B. K18-hACE2 mice develop dose-dependent disease, https://www.jax.org/strain/034860 (2020).
- 58.Zhao J, et al. Rapid generation of a mouse model for Middle East respiratory syndrome. Proc. Natl Acad. Sci. USA. 2014;111:4970–4975. doi: 10.1073/pnas.1323279111. 1:CAS:528:DC%2BC2cXjsFGrsb4%3D, 3977243, 24599590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Hassan AO, et al. A SARS-CoV-2 infection model in mice demonstrates protection by neutralizing antibodies. Cell. 2020;182:744–753.e4. doi: 10.1016/j.cell.2020.06.011. 1:CAS:528:DC%2BB3cXhtFyktLzJ, 7284254, 32553273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Sun SH, et al. A mouse model of SARS-CoV-2 infection and pathogenesis. Cell Host Microbe. 2020;28:124–133. doi: 10.1016/j.chom.2020.05.020. 1:CAS:528:DC%2BB3cXhtVKmtrrE, 7250783, 32485164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Roberts A, et al. A mouse-adapted SARS-coronavirus causes disease and mortality in BALB/c mice. PLoS Pathog. 2007;3:e5. doi: 10.1371/journal.ppat.0030005. 1769406, 17222058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Day CW, et al. A new mouse-adapted strain of SARS-CoV as a lethal model for evaluating antiviral agents in vitro and in vivo. Virology. 2009;395:210–222. doi: 10.1016/j.virol.2009.09.023. 1:CAS:528:DC%2BD1MXhsV2gs7vM, 19853271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Fett C, DeDiego ML, Regla-Nava JA, Enjuanes L, Perlman S. Complete protection against severe acute respiratory syndrome coronavirus-mediated lethal respiratory disease in aged mice by immunization with a mouse-adapted virus lacking E protein. J. Virol. 2013;87:6551–6559. doi: 10.1128/JVI.00087-13. 1:CAS:528:DC%2BC3sXptlKksbo%3D, 3676143, 23576515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Netland J, et al. Immunization with an attenuated severe acute respiratory syndrome coronavirus deleted in E protein protects against lethal respiratory disease. Virology. 2010;399:120–128. doi: 10.1016/j.virol.2010.01.004. 1:CAS:528:DC%2BC3cXis1WlsLY%3D, 20110095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.*Gu, H. et al. Rapid adaptation of SARS-CoV-2 in BALB/c mice: Novel mouse model for vaccine efficacy. Preprint at 10.1101/2020.05.02.073411 (2020). [DOI]
- 66.*Dinnon, K. H. et al. A mouse-adapted SARS-CoV-2 model for the evaluation of COVID-19 medical countermeasures. Preprint at 10.1101/2020.05.06.081497 (2020). [DOI]
- 67.Pettit, N. N. et al. Obesity is associated with increased risk for mortality among hospitalized patients with COVID-19. Obesity, oby.22941 (2020, in press). [DOI] [PMC free article] [PubMed]
- 68.Wu, Z. H., Tang, Y. & Cheng, Q. Diabetes increases the mortality of patients with COVID-19: a meta-analysis. Acta Diabetol, s00592-020-01546-0 (2020, in press). [DOI] [PMC free article] [PubMed]
- 69.Casanova, J.-L., Su, H. C. & COVID Human Genetic Effort. A global effort to define the human genetics of protective immunity to SARS-CoV-2 infection. Cell181, 1194–1199 (2020). [DOI] [PMC free article] [PubMed]
- 70.Genetics CCC. The genome architecture of the collaborative cross mouse genetic reference population. Genetics. 2012;190:389–401. doi: 10.1534/genetics.111.132639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Keane TM, et al. Mouse genomic variation and its effect on phenotypes and gene regulation. Nature. 2011;477:289–294. doi: 10.1038/nature10413. 1:CAS:528:DC%2BC3MXhtFOlsL7N, 3276836, 21921910. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Noll KE, Ferris MT, Heise MT. The collaborative cross: a systems genetics resource for studying host-pathogen interactions. Cell Host Microbe. 2019;25:484–498. doi: 10.1016/j.chom.2019.03.009. 1:CAS:528:DC%2BC1MXntFOntrw%3D, 6494101, 30974083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Gralinski LE, et al. Genome wide identification of SARS-CoV susceptibility loci using the collaborative cross. PLOS Genet. 2015;11:e1005504. doi: 10.1371/journal.pgen.1005504. 4599853, 26452100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Gralinski LE, et al. Allelic variation in the toll-like receptor adaptor protein Ticam2 contributes to SARS-coronavirus pathogenesis in mice. G3 (Bethesda) 2017;7:1653–1663. doi: 10.1534/g3.117.041434. 1:CAS:528:DC%2BC1cXitFOqs7nF. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Jordan RE, Adab P, Cheng KK. Covid-19: risk factors for severe disease and death. BMJ. 2020;368:m1198. doi: 10.1136/bmj.m1198. 32217618. [DOI] [PubMed] [Google Scholar]
- 76.Yang J, et al. Prevalence of comorbidities and its effects in patients infected with SARS-CoV-2: a systematic review and meta-analysis. Int. J. Infect. Dis. 2020;94:91–95. doi: 10.1016/j.ijid.2020.03.017. 1:CAS:528:DC%2BB3cXnslOgsrY%3D, 7194638, 32173574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Mehra MR, Desai SS, Kuy SR, Henry TD, Patel AN. Cardiovascular disease, drug therapy, and mortality in Covid-19. N. Engl. J. Med. 2020;382:e102. doi: 10.1056/NEJMoa2007621. 1:CAS:528:DC%2BB3cXht1GmsbrM, 32356626. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 78.Rubino, F. et al. New-Onset Diabetes in Covid-19. N. Engl. J. Med. NEJMc2018688 (2020, in press). [DOI] [PMC free article] [PubMed]
- 79.Clark A, et al. Global, regional, and national estimates of the population at increased risk of severe COVID-19 due to underlying health conditions in 2020: a modelling study. Lancet Glob. Health. 2020;8:e1003–e1017. doi: 10.1016/S2214-109X(20)30264-3. 7295519, 32553130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Hsu AC, et al. Targeting PI3K-p110alpha suppresses influenza virus infection in chronic obstructive pulmonary disease. Am. J. Respir. Crit. Care Med. 2015;191:1012–1023. doi: 10.1164/rccm.201501-0188OC. 1:CAS:528:DC%2BC2MXpsFGiurk%3D, 25751541. [DOI] [PubMed] [Google Scholar]
- 81.Hsu ACY, et al. MicroRNA-125a and -b inhibit A20 and MAVS to promote inflammation and impair antiviral response in COPD. JCI Insight. 2017;2:e90443. doi: 10.1172/jci.insight.90443. 5374076, 28405612. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Alqahtani JS, et al. Prevalence, severity and mortality associated with COPD and smoking in patients with COVID-19: a rapid systematic review and meta-analysis. PLoS ONE. 2020;15:e0233147. doi: 10.1371/journal.pone.0233147. 1:CAS:528:DC%2BB3cXhtVeks7fO, 7213702, 32392262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Smith JC, et al. Cigarette smoke exposure and inflammatory signaling increase the expression of the SARS-CoV-2 receptor ACE2 in the respiratory tract. Dev. Cell. 2020;53:514–529. doi: 10.1016/j.devcel.2020.05.012. 1:CAS:528:DC%2BB3cXhtVGgsrjE, 7229915, 32425701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Beckett EL, et al. A new short-term mouse model of chronic obstructive pulmonary disease identifies a role for mast cell tryptase in pathogenesis. J. Allergy Clin. Immunol. 2013;131:752–762. doi: 10.1016/j.jaci.2012.11.053. 1:CAS:528:DC%2BC3sXitFKntbs%3D, 4060894, 23380220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Jones B, et al. Animal models of COPD: what do they tell us? Respirology. 2017;22:21–32. doi: 10.1111/resp.12908. 27731525. [DOI] [PubMed] [Google Scholar]
- 86.Liu G, et al. Fibulin-1 regulates the pathogenesis of tissue remodeling in respiratory diseases. JCI Insight. 2016;1:e86380. doi: 10.1172/jci.insight.86380. 4936823, 27398409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Hansbro PM, et al. Importance of mast cell Prss31/transmembrane tryptase/tryptase-γ in lung function and experimental chronic obstructive pulmonary disease and colitis. J. Biol. Chem. 2014;289:18214–18227. doi: 10.1074/jbc.M114.548594. 1:CAS:528:DC%2BC2cXhtVGjsL3K, 4140286, 24821729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Tay HL, et al. Antagonism of miR-328 increases the antimicrobial function of macrophages and neutrophils and rapid clearance of non-typeable haemophilus influenzae (NTHi) from infected lung. PLOS Pathog. 2015;11:e1004549. doi: 10.1371/journal.ppat.1004549. 4404141, 25894560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Li X, et al. Risk factors for severity and mortality in adult COVID-19 inpatients in Wuhan. J. Allergy Clin. Immunol. 2020;146:110–118. doi: 10.1016/j.jaci.2020.04.006. 1:CAS:528:DC%2BB3cXotFCgu7Y%3D, 7152876, 32294485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Garg S, et al. Hospitalization rates and characteristics of patients hospitalized with laboratory-confirmed coronavirus disease 2019—COVID-NET, 14 States, March 1–30, 2020. Morbidity Mortal. Wkly. Rep. (MMWR) 2020;69:458–464. doi: 10.15585/mmwr.mm6915e3. 1:CAS:528:DC%2BB3cXnvFWhsbg%3D. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Hansbro PM, et al. Mechanisms and treatments for severe, steroid-resistant allergic airway disease and asthma. Immunol. Rev. 2017;278:41–62. doi: 10.1111/imr.12543. 1:CAS:528:DC%2BC2sXhtVKqtbjM, 28658552. [DOI] [PubMed] [Google Scholar]
- 92.Kim RY, et al. MicroRNA-21 drives severe, steroid-insensitive experimental asthma by amplifying phosphoinositide 3-kinase-mediated suppression of histone deacetylase 2. J. Allergy Clin. Immunol. 2017;139:519–532. doi: 10.1016/j.jaci.2016.04.038. 1:CAS:528:DC%2BC28Xht1SlurjO, 27448447. [DOI] [PubMed] [Google Scholar]
- 93.Kim RY, et al. Role for NLRP3 Inflammasome-mediated, IL-1beta-Dependent Responses in Severe, Steroid-Resistant Asthma. Am. J. Respir. Crit. Care Med. 2017;196:283–297. doi: 10.1164/rccm.201609-1830OC. 1:CAS:528:DC%2BC1cXitVShsr3E, 28252317. [DOI] [PubMed] [Google Scholar]
- 94.Hui DS, et al. Impact of severe acute respiratory syndrome (SARS) on pulmonary function, functional capacity and quality of life in a cohort of survivors. Thorax. 2005;60:401–409. doi: 10.1136/thx.2004.030205. 1:STN:280:DC%2BD2M3is1egtQ%3D%3D, 1758905, 15860716. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Venkataraman T, Frieman MB. The role of epidermal growth factor receptor (EGFR) signaling in SARS coronavirus-induced pulmonary fibrosis. Antivir. Res. 2017;143:142–150. doi: 10.1016/j.antiviral.2017.03.022. 1:CAS:528:DC%2BC2sXms1CgtLs%3D, 28390872. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Xie L, et al. Follow-up study on pulmonary function and lung radiographic changes in rehabilitating severe acute respiratory syndrome patients after discharge. Chest. 2005;127:2119–2124. doi: 10.1378/chest.127.6.2119. 15947329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Zhang P, et al. Long-term bone and lung consequences associated with hospital-acquired severe acute respiratory syndrome: a 15-year follow-up from a prospective cohort study. Bone Res. 2020;8:8. doi: 10.1038/s41413-020-0084-5. 1:CAS:528:DC%2BB3cXktlGjsb4%3D, 7018717, 32128276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Xu R, et al. SARS-CoV-2 induced transcriptional signatures in human lung epithelial cells that promote lung fibrosis. Respiratory Res. 2020;21 doi: 10.1186/s12931-020-01445-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Liu G, et al. Fibulin-1c regulates transforming growth factor-β activation in pulmonary tissue fibrosis. JCI Insight. 2019;5:e124529. doi: 10.1172/jci.insight.124529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Camacho P, Fan H, Liu Z, He JQ. Small mammalian animal models of heart disease. Am. J. Cardiovasc Dis. 2016;6:70–80. 1:CAS:528:DC%2BC1cXotlyqsLc%3D, 5030387, 27679742. [PMC free article] [PubMed] [Google Scholar]
- 101.Kleinert M, et al. Animal models of obesity and diabetes mellitus. Nat. Rev. Endocrinol. 2018;14:140–162. doi: 10.1038/nrendo.2017.161. 29348476. [DOI] [PubMed] [Google Scholar]
- 102.Surwit RS, Kuhn CM, Cochrane C, McCubbin JA, Feinglos MN. Diet-induced type II diabetes in C57BL/6J mice. Diabetes. 1988;37:1163–1167. doi: 10.2337/diab.37.9.1163. 1:CAS:528:DyaL1cXls12gsr0%3D, 3044882. [DOI] [PubMed] [Google Scholar]
- 103.Winzell MS, Ahrén B. The high-fat diet-fed mouse: a model for studying mechanisms and treatment of impaired glucose tolerance and type 2 diabetes. Diabetes. 2004;53(Suppl 3):S215–S219. doi: 10.2337/diabetes.53.suppl_3.s215. 15561913. [DOI] [PubMed] [Google Scholar]
- 104.Chen L, Li X, Chen M, Feng Y, Xiong C. The ACE2 expression in human heart indicates new potential mechanism of heart injury among patients infected with SARS-CoV-2. Cardiovasc. Res. 2020;116:1097–1100. doi: 10.1093/cvr/cvaa078. 1:CAS:528:DC%2BB3cXhtFGrtLjF, 32227090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Cristelo C, Azevedo C, Marques JM, Nunes R, Sarmento B. SARS-CoV-2 and diabetes: New challenges for the disease. Diabetes Res Clin. Pr. 2020;164:108228. doi: 10.1016/j.diabres.2020.108228. 1:CAS:528:DC%2BB3cXhtVSjsbjN. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Roca-Ho H, Riera M, Palau V, Pascual J, Soler MJ. Characterization of ACE and ACE2 Expression within Different Organs of the NOD Mouse. Int. J. Mol. Sci. 2017;18:e563. doi: 10.3390/ijms18030563. 28273875. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Hulme KD, Gallo LA, Short KR. Influenza virus and glycemic variability in diabetes: a killer combination? Front. Microbiol. 2017;8:e861. doi: 10.3389/fmicb.2017.00861. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Petrilli CM, et al. Factors associated with hospital admission and critical illness among 5279 people with coronavirus disease 2019 in New York City: prospective cohort study. BMJ. 2020;369:m1966. doi: 10.1136/bmj.m1966. 7243801, 32444366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Mueller AL, McNamara MS, Sinclair DA. Why does COVID-19 disproportionately affect older people? Aging. 2020;12:9959–9981. doi: 10.18632/aging.103344. 1:CAS:528:DC%2BB3cXisVWht7jM, 7288963, 32470948. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Bilinska K, Jakubowska P, Von Bartheld CS, Butowt R. Expression of the SARS-CoV-2 entry proteins, ACE2 and TMPRSS2, in cells of the olfactory epithelium: identification of cell types and trends with age. ACS Chem. Neurosci. 2020;11:1555–1562. doi: 10.1021/acschemneuro.0c00210. 1:CAS:528:DC%2BB3cXoslOmu78%3D, 32379417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Roberts A, et al. Severe acute respiratory syndrome coronavirus infection of golden Syrian hamsters. J. Virol. 2005;79:503–511. doi: 10.1128/JVI.79.1.503-511.2005. 1:CAS:528:DC%2BD2MXhslertg%3D%3D, 538722, 15596843. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.*Booeshaghi, A. S. & Pachter, L. Decrease in ACE2 mRNA expression in aged mouse lung. Preprint at 10.1101/2020.04.02.021451 (2020). [DOI]
- 113.Deming D, et al. Vaccine efficacy in senescent mice challenged with recombinant SARS-CoV bearing epidemic and zoonotic spike variants. PLoS Med. 2006;3:e525. doi: 10.1371/journal.pmed.0030525. 1716185, 17194199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Enkirch T, von Messling V. Ferret models of viral pathogenesis. Virology. 2015;479-480:259–270. doi: 10.1016/j.virol.2015.03.017. 1:CAS:528:DC%2BC2MXks1aksrc%3D, 25816764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.van den Brand JM, et al. Pathology of experimental SARS coronavirus infection in cats and ferrets. Vet. Pathol. 2008;45:551–562. doi: 10.1354/vp.45-4-551. 18587105. [DOI] [PubMed] [Google Scholar]
- 116.Chu YK, et al. The SARS-CoV ferret model in an infection-challenge study. Virology. 2008;374:151–163. doi: 10.1016/j.virol.2007.12.032. 1:CAS:528:DC%2BD1cXks12gsb4%3D, 18234270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Martina BE, et al. Virology: SARS virus infection of cats and ferrets. Nature. 2003;425:e915. doi: 10.1038/425915a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Wan Y, Shang J, Graham R, Baric RS, Li F. Receptor recognition by the novel coronavirus from Wuhan: an analysis based on decade-long structural studies of SARS coronavirus. J. Virol. 2020;94:e00120–e00127. doi: 10.1128/JVI.00127-20. 7081895, 31996437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Kim YI, et al. Infection and rapid transmission of SARS-CoV-2 in ferrets. Cell Host Microbe. 2020;27:704–709. e702. doi: 10.1016/j.chom.2020.03.023. 1:CAS:528:DC%2BB3cXmsl2qsLs%3D, 7144857, 32259477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Shi J, et al. Susceptibility of ferrets, cats, dogs, and other domesticated animals to SARS-coronavirus 2. Science. 2020;368:1016–1020. doi: 10.1126/science.abb7015. 1:CAS:528:DC%2BB3cXhtVCntbnK, 7164390, 32269068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Park SJ, et al. Antiviral efficacies of FDA-approved drugs against SARS-CoV-2 infection in ferrets. mBio. 2020;11:e01114–e01120. doi: 10.1128/mBio.01114-20. 7244896, 32444382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Blanco-Melo D, et al. Imbalanced host response to SARS-CoV-2 drives development of COVID-19. Cell. 2020;181:1036–1045. e1039. doi: 10.1016/j.cell.2020.04.026. 1:CAS:528:DC%2BB3cXps1yjtrk%3D, 7227586, 32416070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Miao J, Chard LS, Wang Z, Wang Y. Syrian hamster as an animal model for the study on infectious diseases. Front Immunol. 2019;10:e2329. doi: 10.3389/fimmu.2019.02329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Li R, et al. Production of genetically engineered golden Syrian hamsters by pronuclear injection of the CRISPR/Cas9 complex. J. Vis. Exp. 2018;131:e56263. doi: 10.3791/56263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Miao J, et al. Characterization of an N-terminal non-core domain of RAG1 gene disrupted Syrian Hamster model generated by CRISPR Cas9. Viruses. 2018;10:e243. doi: 10.3390/v10050243. 29734775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Toth K, et al. STAT2 knockout Syrian hamsters support enhanced replication and pathogenicity of human adenovirus, revealing an important role of type I interferon response in viral control. PLoS Pathog. 2015;11:e1005084. doi: 10.1371/journal.ppat.1005084. 4546297, 26291525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Roberts A, et al. Therapy with a severe acute respiratory syndrome-associated coronavirus-neutralizing human monoclonal antibody reduces disease severity and viral burden in golden Syrian hamsters. J. Infect. Dis. 2006;193:685–692. doi: 10.1086/500143. 1:CAS:528:DC%2BD28XitF2htLw%3D, 16453264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Schaecher SR, et al. An immunosuppressed Syrian golden hamster model for SARS-CoV infection. Virology. 2008;380:312–321. doi: 10.1016/j.virol.2008.07.026. 1:CAS:528:DC%2BD1cXht1egtbfF, 18760437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Chan, J. F. et al. Simulation of the clinical and pathological manifestations of Coronavirus Disease 2019 (COVID-19) in golden Syrian hamster model: implications for disease pathogenesis and transmissibility. Clin. Infect. Dis. ciaa325 (2020, in press). [DOI] [PMC free article] [PubMed]
- 130.Luan J, Lu Y, Jin X, Zhang L. Spike protein recognition of mammalian ACE2 predicts the host range and an optimized ACE2 for SARS-CoV-2 infection. Biochem. Biophys. Res. Commun. 2020;526:165–169. doi: 10.1016/j.bbrc.2020.03.047. 1:CAS:528:DC%2BB3cXlsFaksLk%3D, 7102515, 32201080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.(FDA), F. a. D. A. Product development under the animal rule: Guidance for Industry. (2015).
- 132.Kuiken T, et al. Newly discovered coronavirus as the primary cause of severe acute respiratory syndrome. Lancet. 2003;362:263–270. doi: 10.1016/S0140-6736(03)13967-0. 1:CAS:528:DC%2BD3sXlvVSmsLs%3D, 7112434, 12892955. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Fouchier RA, et al. Aetiology: Koch's postulates fulfilled for SARS virus. Nature. 2003;423:240. doi: 10.1038/423240a. 1:CAS:528:DC%2BD3sXjs1yntb0%3D, 7095368, 12748632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Lawler JV, et al. Cynomolgus macaque as an animal model for severe acute respiratory syndrome. PLoS Med. 2006;3:e149. doi: 10.1371/journal.pmed.0030149. 1435788, 16605302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.McAuliffe J, et al. Replication of SARS coronavirus administered into the respiratory tract of African Green, rhesus and cynomolgus monkeys. Virology. 2004;330:8–15. doi: 10.1016/j.virol.2004.09.030. 1:CAS:528:DC%2BD2cXpsFentb8%3D, 15527829. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Rowe T, et al. Macaque model for severe acute respiratory syndrome. J. Virol. 2004;78:11401–11404. doi: 10.1128/JVI.78.20.11401-11404.2004. 1:CAS:528:DC%2BD2cXotlKisbo%3D, 521815, 15452262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Haagmans BL, et al. Pegylated interferon-alpha protects type 1 pneumocytes against SARS coronavirus infection in macaques. Nat. Med. 2004;10:290–293. doi: 10.1038/nm1001. 1:CAS:528:DC%2BD2cXhs1WntbY%3D, 7095986, 14981511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Smits SL, et al. Exacerbated innate host response to SARS-CoV in aged non-human primates. PLoS Pathog. 2010;6:e1000756. doi: 10.1371/journal.ppat.1000756. 2816697, 20140198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Rockx B, et al. Comparative pathogenesis of three human and zoonotic SARS-CoV strains in cynomolgus macaques. PLoS ONE. 2011;6:e18558. doi: 10.1371/journal.pone.0018558. 1:CAS:528:DC%2BC3MXlt12ht7k%3D, 3080360, 21533129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Qin C, et al. An animal model of SARS produced by infection of Macaca mulatta with SARS coronavirus. J. Pathol. 2005;206:251–259. doi: 10.1002/path.1769. 7167940, 15892035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Greenough TC, et al. Pneumonitis and multi-organ system disease in common marmosets (Callithrix jacchus) infected with the severe acute respiratory syndrome-associated coronavirus. Am. J. Pathol. 2005;167:455–463. doi: 10.1016/S0002-9440(10)62989-6. 1603565, 16049331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.de Wit E, et al. Middle East respiratory syndrome coronavirus (MERS-CoV) causes transient lower respiratory tract infection in rhesus macaques. Proc. Natl Acad. Sci. USA. 2013;110:16598–16603. doi: 10.1073/pnas.1310744110. 3799368, 24062443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Munster VJ, de Wit E, Feldmann H. Pneumonia from human coronavirus in a macaque model. N. Engl. J. Med. 2013;368:1560–1562. doi: 10.1056/NEJMc1215691. 1:CAS:528:DC%2BC3sXmsFKgtbY%3D, 23550601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Yao Y, et al. An animal model of MERS produced by infection of rhesus macaques with MERS coronavirus. J. Infect. Dis. 2014;209:236–242. doi: 10.1093/infdis/jit590. 1:CAS:528:DC%2BC2cXit1Sgug%3D%3D, 24218506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.de Wit E, et al. Prophylactic and therapeutic efficacy of mAb treatment against MERS-CoV in common marmosets. Antivir. Res. 2018;156:64–71. doi: 10.1016/j.antiviral.2018.06.006. 29885377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Falzarano D, et al. Infection with MERS-CoV causes lethal pneumonia in the common marmoset. PLoS Pathog. 2014;10:e1004250. doi: 10.1371/journal.ppat.1004250. 4140844, 25144235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.*Munster, V. J. et al. Respiratory disease and virus shedding in rhesus macaques inoculated with SARS-CoV-2. Preprint at 10.1101/2020.03.21.001628 (2020). [DOI] [PMC free article] [PubMed]
- 148.Yu P, et al. Age-related rhesus macaque models of COVID-19. Anim. Model Exp. Med. 2020;3:93–97. doi: 10.1002/ame2.12108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.*Lu, S. et al. Comparison of SARS-CoV-2 infections among 3 species of non-human primates. Preprint at 10.1101/2020.04.08.031807 (2020). [DOI]
- 150.*Melin, A. D., Janiak, M. C., Marrone, F., 3rd, Arora, P. S. & Higham, J. P. Comparative ACE2 variation and primate COVID-19 risk. Preprint at 10.1101/2020.04.09.034967 (2020). [DOI] [PMC free article] [PubMed]
- 151.Chandrashekar, A. et al. SARS-CoV-2 infection protects against rechallenge in rhesus macaques. Science, eabc4776 (2020). [DOI] [PMC free article] [PubMed]
- 152.Yu J, et al. DNA vaccine protection against SARS-CoV-2 in rhesus macaques. Science. 2020;369:806–811. doi: 10.1126/science.abc6284. 1:CAS:528:DC%2BB3cXhsF2qsrrN, 7243363, 32434945. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153.van Doremalen, N. et al. ChAdOx1 nCoV-19 vaccination prevents SARS-CoV-2 pneumonia in rhesus macaques. Nature. s41586-020-2608-y (2020, in press). [DOI] [PubMed]
- 154.Health, N. I. O. COVID-19 vaccine (ChAdOx1 nCoV-19) trial in South African adults with and without HIV-infection, https://www.clinicaltrials.gov/ct2/show/NCT04444674 (2020).
- 155.Boni, M. F. et al. Evolutionary origins of the SARS-CoV-2 sarbecovirus lineage responsible for the COVID-19 pandemic. Nat. Microbiol. s41564-020-0771-4 (2020, in press). [DOI] [PubMed]
- 156.Schlottau, K. et al. SARS-CoV-2 in fruit bats, ferrets, pigs, and chickens: an experimental transmission study. Lancet Microbe. S2666-5247(20)30089-6 (2020, in press). [DOI] [PMC free article] [PubMed]
- 157.Anthony SJ, et al. Global patterns in coronavirus diversity. Virus Evolution. 2017;3:vex012. doi: 10.1093/ve/vex012. 5467638, 28630747. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158.Munster VJ, et al. Replication and shedding of MERS-CoV in Jamaican fruit bats (Artibeus jamaicensis) Sci. Rep. 2016;6 doi: 10.1038/srep21878. 1:CAS:528:DC%2BC28XivFGrsL8%3D, 4761889, 26899616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 159.Watanabe S, et al. Bat coronaviruses and experimental infection of bats, the Philippines. Emerg. Infect. Dis. 2010;16:1217–1223. doi: 10.3201/eid1608.100208. 1:CAS:528:DC%2BC3cXhtVOnsbnE, 3298303, 20678314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160.Zhou J, et al. Infection of bat and human intestinal organoids by SARS-CoV-2. Nat. Med. 2020;26:1077–1083. doi: 10.1038/s41591-020-0912-6. 1:CAS:528:DC%2BB3cXpt1Kmt7c%3D, 32405028. [DOI] [PubMed] [Google Scholar]
- 161.Shaw TI, et al. Transcriptome Sequencing and Annotation for the Jamaican Fruit Bat (Artibeus jamaicensis) PLOS ONE. 2012;7:e48472. doi: 10.1371/journal.pone.0048472. 1:CAS:528:DC%2BC38XhvVShs7vL, 3499531, 23166587. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 162.W. H. O. Consensus document on the epidemiology of severe acute respiratory syndrome (SARS). Department of Communicable Disease Surveillance and Response, 1–44 (2003).
- 163.Halfmann, P. J. et al. Transmission of SARS-CoV-2 in Domestic Cats. N. Engl. J. Med. NEJMc2013400 (2020, in press). [DOI] [PMC free article] [PubMed]
- 164.Sailleau, C. et al. First detection and genome sequencing of SARS-CoV-2 in an infected cat in France. Transbound Emerg. Dis. tbed.13659 (2020, in press). [DOI] [PMC free article] [PubMed]
- 165.Newman A, et al. First Reported Cases of SARS-CoV-2 Infection in Companion Animals - New York, March-April 2020. MMWR Morb. Mortal. Wkly Rep. 2020;69:710–713. doi: 10.15585/mmwr.mm6923e3. 1:CAS:528:DC%2BB3cXht1Shtr3N, 7315787, 32525853. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 166.IDEXX. Leading Veterinary Diagnostic Company Sees No COVID-19 Cases in Pets, https://www.idexx.com/en/about-idexx/news/no-covid-19-cases-pets/ (2020).
- 167.*Zhang, Q. et al. SARS-CoV-2 neutralizing serum antibodies in cats: a serological investigation. Preprint at 10.1101/2020.04.01.021196 (2020). [DOI]
- 168.Sit, T. H. C. et al. Infection of dogs with SARS-CoV-2. Nature. s41586-020-2334-5 (2020, in press). [DOI] [PMC free article] [PubMed]
- 169.MacMahon KL, et al. Protecting poultry workers from exposure to avian influenza viruses. Public Health Rep. 2008;123:316–322. doi: 10.1177/003335490812300311. 2289984, 19006973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 170.Yang Y, Halloran ME, Sugimoto JD, Longini IM., Jr. Detecting human-to-human transmission of avian influenza A (H5N1) Emerg. Infect. Dis. 2007;13:1348–1353. doi: 10.3201/eid1309.07-0111. 2857285, 18252106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 171.Brauer, R. & Chen, P. Influenza virus propagation in embryonated chicken eggs. J. Vis. Exp. 52421 (2015). [DOI] [PMC free article] [PubMed]
- 172.Weingartl HM, et al. Susceptibility of pigs and chickens to SARS coronavirus. Emerg. Infect. Dis. 2004;10:179–184. doi: 10.3201/eid1002.030677. 3322906, 15030680. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 173.Swayne DE, et al. Domestic poultry and SARS coronavirus, southern China. Emerg. Infect. Dis. 2004;10:914–916. doi: 10.3201/eid1005.030827. 3323233, 15200830. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 174.*Zhao, Y. et al. Susceptibility of tree shrew to SARS-CoV-2 infection. Preprint at, 10.1101/2020.04.30.029736 (2020). [DOI] [PMC free article] [PubMed]
- 175.Hansbro PM, et al. Surveillance and analysis of avian influenza viruses, Australia. Emerg. Infect. Dis. 2010;16:1896–1904. doi: 10.3201/eid1612.100776. 3294589, 21122219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 176.Society, W. C. Bronx Zoo Tigers and Lions Recovering from COVID-19, https://newsroom.wcs.org/News-Releases/articleType/ArticleView/articleId/14084/Update-Bronx-Zoo-Tigers-and-Lions-Recovering-from-COVID-19.aspx (2020).
- 177.Oreshkova N, et al. SARS-CoV-2 infection in farmed minks, the Netherlands, April and May 2020. Eurosurveillance. 2020;25:2001005. doi: 10.2807/1560-7917.ES.2020.25.23.2001005. 7403642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 178.Geographic, N. Seven more big cats test positive for coronavirus at Bronx Zoo, https://www.nationalgeographic.com/animals/2020/04/tiger-coronavirus-covid19-positive-test-bronx-zoo/ (2020).
- 179.Wang L, et al. Complete genome sequence of SARS-CoV-2 in a tiger from a U.S. zoological collection. Microbiol. Resour. Announcements. 2020;9:e00420–e00468. doi: 10.1128/MRA.00468-20. 1:CAS:528:DC%2BB3cXht1GlsbvK. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 180.Li W, et al. Bats are natural reservoirs of SARS-like coronaviruses. Science. 2005;310:676–679. doi: 10.1126/science.1118391. 1:CAS:528:DC%2BD2MXhtFChsLjO, 16195424. [DOI] [PubMed] [Google Scholar]
- 181.Wahba L, et al. An extensive meta-metagenomic search identifies SARS-CoV-2-homologous sequences in pangolin lung viromes. mSphere. 2020;5:e00120–e00160. doi: 10.1128/mSphere.00160-20. 1:CAS:528:DC%2BB3cXhtFeqsr3P, 7203451, 32376697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 182.*Wong, M. C., Javornik Cregeen, S. J., Ajami, N. J. & Petrosino, J. F. Evidence of recombination in coronaviruses implicating pangolin origins of nCoV-2019. Preprint at 10.1101/2020.02.07.939207 (2020). [DOI]
- 183.Zhao J, et al. Detection of SARS-coronavirus in both human and animals by RT-PCR. Wei Sheng Yan Jiu. 2005;34:412–415. 1:CAS:528:DC%2BD28XntlOlurg%3D, 16229261. [PubMed] [Google Scholar]
- 184.Zhou H, et al. A novel bat coronavirus closely related to SARS-CoV-2 contains natural insertions at the S1/S2 cleavage site of the spike protein. Curr. Biol. 2020;30:2196–2203. doi: 10.1016/j.cub.2020.05.023. 1:CAS:528:DC%2BB3cXps1yjt7o%3D, 7211627, 32416074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 185.McIver DJ, et al. Coronavirus surveillance of wildlife in the Lao People's Democratic Republic detects viral RNA in rodents. Arch. Virol. 2020;165:1869–1875. doi: 10.1007/s00705-020-04683-7. 1:CAS:528:DC%2BB3cXhtVOjt7nN, 7265875, 32488616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 186.Liu P, Chen W, Chen J-P. Viral Metagenomics revealed sendai virus and coronavirus infection of Malayan Pangolins (Manis javanica) Viruses. 2019;11:e979. doi: 10.3390/v11110979. 31652964. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 187.Ammerman NC, Beier-Sexton M, Azad AF. Growth and maintenance of Vero cell lines. Curr. Protoc. Microbiol. 2008;Appendix 4:4E. doi: 10.1002/9780471729259.mca04es11. 19016439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 188.Jia HP, et al. ACE2 receptor expression and severe acute respiratory syndrome coronavirus infection depend on differentiation of human airway epithelia. J. Virol. 2005;79:14614–14621. doi: 10.1128/JVI.79.23.14614-14621.2005. 1:CAS:528:DC%2BD2MXht1Cgsb%2FO, 1287568, 16282461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 189.Mossel EC, et al. Exogenous ACE2 expression allows refractory cell lines to support severe acute respiratory syndrome coronavirus replication. J. Virol. 2005;79:3846–3850. doi: 10.1128/JVI.79.6.3846-3850.2005. 1:CAS:528:DC%2BD2MXit1ehtrw%3D, 1075706, 15731278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 190.Harcourt J, et al. Severe acute respiratory syndrome coronavirus 2 from patient with 2019 novel coronavirus disease, United States. Emerg. Infect. Dis. 2020;26:1266–1273. doi: 10.3201/eid2606.200516. 1:CAS:528:DC%2BB3cXhtlarurvN, 7258473, 32160149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 191.Hsu AC, et al. Critical role of constitutive type I interferon response in bronchial epithelial cell to influenza infection. PLoS ONE. 2012;7:e32947. doi: 10.1371/journal.pone.0032947. 1:CAS:528:DC%2BC38XjvFWqt74%3D, 3292582, 22396801. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 192.Heijink IH, Postma DS, Noordhoek JA, Broekema M, Kapus A. House dust mite-promoted epithelial-to-mesenchymal transition in human bronchial epithelium. Am. J. Respir. Cell Mol. Biol. 2010;42:69–79. doi: 10.1165/rcmb.2008-0449OC. 1:CAS:528:DC%2BC3cXksFSjsA%3D%3D, 19372245. [DOI] [PubMed] [Google Scholar]
- 193.Faiz, A. et al. Effect of long-term corticosteroid treatment on microRNA and gene-expression profiles in Chronic Obstructive Pulmonary Disease. Eur. Resp. J. 1801202 (2019). [DOI] [PubMed]
- 194.Hu M, et al. Respiratory syncytial virus co-opts host mitochondrial function to favour infectious virus production. Elife. 2019;8:e42448. doi: 10.7554/eLife.42448. 6598784, 31246170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 195.Kedzierski L, et al. Suppressor of cytokine signaling (SOCS)5 ameliorates influenza infection via inhibition of EGFR signaling. Elife. 2017;6:e20444. doi: 10.7554/eLife.20444. 5354519, 28195529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 196.*Mulay, A. et al. SARS-CoV-2 infection of primary human lung epithelium for COVID-19 modeling and drug discovery. Preprint at 10.1101/2020.06.29.174623 (2020). [DOI] [PMC free article] [PubMed]
- 197.Horani A, Nath A, Wasserman MG, Huang T, Brody SL. Rho-associated protein kinase inhibition enhances airway epithelial basal-cell proliferation and lentivirus transduction. Am. J. Resp. Cell Mol. Biol. 2013;49:341–347. doi: 10.1165/rcmb.2013-0046TE. 1:CAS:528:DC%2BC3sXhtlyqu7vN. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 198.Huang I, Pranata R. Lymphopenia in severe coronavirus disease-2019 (COVID-19): systematic review and meta-analysis. J. Intensive Care. 2020;8 doi: 10.1186/s40560-020-00453-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 199.Zhao Q, et al. Lymphopenia is associated with severe coronavirus disease 2019 (COVID-19) infections: a systemic review and meta-analysis. Int J. Infect. Dis. 2020;96:131–135. doi: 10.1016/j.ijid.2020.04.086. 1:CAS:528:DC%2BB3cXpsFCmsrk%3D, 7196544, 32376308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 200.Yen YT, et al. Modeling the early events of severe acute respiratory syndrome coronavirus infection in vitro. J. Virol. 2006;80:2684–2693. doi: 10.1128/JVI.80.6.2684-2693.2006. 1:CAS:528:DC%2BD28Xis1CqsL0%3D, 1395447, 16501078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 201.Ng LFP, et al. A human in vitro model system for investigating genome-wide host responses to SARS coronavirus infection. BMC Infect. Dis. 2004;4 doi: 10.1186/1471-2334-4-34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 202.Banerjee, A. et al. Isolation, sequence, infectivity and replication kinetics of SARS-CoV-2. Emerg Infect Dis. eid2609.201495 (2020, in press). [DOI] [PMC free article] [PubMed]
- 203.*Chen, Y. et al. The novel severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) directly decimates human spleens and lymph nodes. Preprint at 10.1101/2020.03.27.20045427 (2020). [DOI]
- 204.Wang, X. et al. SARS-CoV-2 infects T lymphocytes through its spike protein-mediated membrane fusion. Cell. Mol. Immunol. s41423-020-0424-9 (2020, in press). [DOI] [PMC free article] [PubMed]
- 205.Chu H, et al. Middle East respiratory syndrome coronavirus efficiently infects human primary T lymphocytes and activates the extrinsic and intrinsic apoptosis pathways. J. Infect. Dis. 2015;213:904–914. doi: 10.1093/infdis/jiv380. 26203058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 206.Ragan I, Hartson L, Pidcoke H, Bowen R, Goodrich R. Pathogen reduction of SARS-CoV-2 virus in plasma and whole blood using riboflavin and UV light. PLOS ONE. 2020;15:e0233947. doi: 10.1371/journal.pone.0233947. 1:CAS:528:DC%2BB3cXhtVygtrjJ, 7259667, 32470046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 207.Lancaster MA, et al. Cerebral organoids model human brain development and microcephaly. Nature. 2013;501:373–379. doi: 10.1038/nature12517. 1:CAS:528:DC%2BC3sXhtlCntb3F, 23995685. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 208.Wimmer RA, et al. Human blood vessel organoids as a model of diabetic vasculopathy. Nature. 2019;565:505–510. doi: 10.1038/s41586-018-0858-8. 1:CAS:528:DC%2BC1MXlvFSntLc%3D, 7116578, 30651639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 209.Sato T, et al. Single Lgr5 stem cells build crypt-villus structures in vitro without a mesenchymal niche. Nature. 2009;459:262–265. doi: 10.1038/nature07935. 1:CAS:528:DC%2BD1MXjslartrg%3D, 19329995. [DOI] [PubMed] [Google Scholar]
- 210.Elbadawi M, Efferth T. Organoids of human airways to study infectivity and cytopathy of SARS-CoV-2. Lancet Resp. Med. 2020;S2213-2600(2220):30231–30238. doi: 10.1016/S2213-2600(20)30238-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 211.Dye BR, et al. In vitro generation of human pluripotent stem cell derived lung organoids. Elife. 2015;4:e05098. doi: 10.7554/eLife.05098. 4370217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 212.Miller AJ, et al. Generation of lung organoids from human pluripotent stem cells in vitro. Nat. Protoc. 2019;14:518–540. doi: 10.1038/s41596-018-0104-8. 1:CAS:528:DC%2BC1MXmtFGrurk%3D, 6531049, 30664680. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 213.Li Y, Wu Q, Sun X, Shen J, Chen H. Organoids as a powerful model for respiratory diseases. Stem Cells Int. 2020;2020:5847876. doi: 10.1155/2020/5847876. 7086445, 32256609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 214.*Han, Y. et al. Identification of candidate COVID-19 therapeutics using hPSC-derived lung organoids. Preprint at 10.1101/2020.05.05.079095 (2020). [DOI]
- 215.Varga Z, et al. Endothelial cell infection and endotheliitis in COVID-19. Lancet. 2020;395:1417–1418. doi: 10.1016/S0140-6736(20)30937-5. 1:CAS:528:DC%2BB3cXnslektbs%3D, 7172722, 32325026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 216.Yang X, et al. Prevalence and impact of acute renal impairment on COVID-19: a systematic review and meta-analysis. Crit. Care. 2020;24 doi: 10.1186/s13054-020-03065-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 217.Huang C, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395:497–506. doi: 10.1016/S0140-6736(20)30183-5. 1:CAS:528:DC%2BB3cXhs1Kqu7c%3D, 7159299, 31986264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 218.Helms J, et al. Neurologic Features in Severe SARS-CoV-2 Infection. N. Engl. J. Med. 2020;382:2268–2270. doi: 10.1056/NEJMc2008597. 32294339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 219.Lamers MM, et al. SARS-CoV-2 productively infects human gut enterocytes. Science. 2020;369:50–54. doi: 10.1126/science.abc1669. 1:CAS:528:DC%2BB3cXhtlCmt7jO, 32358202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 220.Monteil V, et al. Inhibition of SARS-CoV-2 infections in engineered human tissues using clinical-grade soluble human ACE2. Cell. 2020;181:905–913. doi: 10.1016/j.cell.2020.04.004. 1:CAS:528:DC%2BB3cXotVCnsLY%3D, 7181998, 32333836. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 221.Zang R, et al. TMPRSS2 and TMPRSS4 promote SARS-CoV-2 infection of human small intestinal enterocytes. Sci. Immunol. 2020;5:eabc3582. doi: 10.1126/sciimmunol.abc3582. 1:CAS:528:DC%2BB3cXhtVCnu7nM, 7285829, 32404436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 222.Zhao, B. et al. Recapitulation of SARS-CoV-2 infection and cholangiocyte damage with human liver ductal organoids. Protein Cell, s13238-020-00718-6 (2020, in press). [DOI] [PMC free article] [PubMed]
- 223.Health, N. I. O. Recombinant Human Angiotensin-converting Enzyme 2 (rhACE2) as a Treatment for Patients With COVID-19 (APN01-COVID-19), https://clinicaltrials.gov/ct2/show/NCT04335136 (2020).
- 224.Stanifer, M. L. et al. Critical role of type III interferon in controlling SARS-CoV-2 infection in human intestinal epithelial cells. Cell Rep. 107863 (2020). [DOI] [PMC free article] [PubMed]
- 225.*Ramani, A. et al. SARS-CoV-2 targets cortical neurons of 3D human brain organoids and shows neurodegeneration-like effects. Preprint at 10.1101/2020.05.20.106575 (2020). [DOI]
- 226.Bullen, C. K. et al. Infectability of human BrainSphere neurons suggests neurotropism of SARS-CoV-2. Altex. altex.2006111 (2020, in press). [DOI] [PubMed]
- 227.Prihandoko, R. et al. Pathophysiological regulation of lung function by the free fatty acid receptor FFA4. Preprint at 10.1101/2020.05.18.101170 (2020). [DOI] [PubMed]
- 228.Joad JP, Kott KS, Bric JM, Peake JL, Pinkerton KE. Effect of perinatal secondhand tobacco smoke exposure on in vivo and intrinsic airway structure/function in non-human primates. Toxicol. Appl. Pharm. 2009;234:339–344. doi: 10.1016/j.taap.2008.10.018. 1:CAS:528:DC%2BD1MXhtlCltrs%3D. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 229.Schlepütz M, et al. Neurally mediated airway constriction in human and other species: a comparative study using precision-cut lung slices (PCLS) PLOS ONE. 2012;7:e47344. doi: 10.1371/journal.pone.0047344. 3467211, 23056631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 230.Ali MK, et al. Critical role for iron accumulation in the pathogenesis of fibrotic lung disease. J. Pathol. 2020;251:49–62. doi: 10.1002/path.5401. 1:CAS:528:DC%2BB3cXot12qurs%3D, 32083318. [DOI] [PubMed] [Google Scholar]
- 231.Donovan C, Seow HJ, Bourke JE, Vlahos R. Influenza A virus infection and cigarette smoke impair bronchodilator responsiveness to β-adrenoceptor agonists in mouse lung. Clin. Sci. 2016;130:829–837. doi: 10.1042/CS20160093. 1:CAS:528:DC%2BC28XmsVamtLk%3D. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 232.Liu G, et al. Airway remodelling and inflammation in asthma are dependent on the extracellular matrix protein fibulin-1c. J. Pathol. 2017;243:510–523. doi: 10.1002/path.4979. 1:CAS:528:DC%2BC2sXhvVeqtrzN, 28862768. [DOI] [PubMed] [Google Scholar]
- 233.Booth JL, Coggeshall KM, Gordon BE, Metcalf JP. Adenovirus type 7 induces interleukin-8 in a lung slice model and requires activation of Erk. J. Virol. 2004;78:4156–4164. doi: 10.1128/JVI.78.8.4156-4164.2004. 1:CAS:528:DC%2BD2cXjtFWlt7s%3D, 374302, 15047831. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 234.Meng F, et al. Replication characteristics of swine influenza viruses in precision-cut lung slices reflect the virulence properties of the viruses. Vet. Res. 2013;44:110. doi: 10.1186/1297-9716-44-110. 3840634, 24225030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 235.Ebsen M, et al. Infection of murine precision cut lung slices (PCLS) with respiratory syncytial virus (RSV) and chlamydophila pneumoniae using the Krumdieck technique. Pathol. Res. Pr. 2002;198:747–753. doi: 10.1078/0344-0338-00331. 1:STN:280:DC%2BD3s%2FitlKnsw%3D%3D. [DOI] [PubMed] [Google Scholar]
- 236.Sheahan TP, et al. Broad-spectrum antiviral GS-5734 inhibits both epidemic and zoonotic coronaviruses. Sci. Transl. Med. 2017;9:eaal3653. doi: 10.1126/scitranslmed.aal3653. 5567817, 28659436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 237.Beigel, J. H. et al. Remdesivir for the Treatment of Covid-19 — Preliminary Report. N. Engl. J. Med. NEJMoa2007764 (2020, in press). [DOI] [PubMed]
- 238.Cao Y, et al. Potent neutralizing antibodies against SARS-CoV-2 identified by high-throughput single-cell sequencing of convalescent patients' B cells. Cell. 2020;182:73–84. doi: 10.1016/j.cell.2020.05.025. 1:CAS:528:DC%2BB3cXhtVyiu7fP, 7231725, 32425270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 239.Rogers, T. F. et al. Isolation of potent SARS-CoV-2 neutralizing antibodies and protection from disease in a small animal model. Science, eabc7520 (2020). [DOI] [PMC free article] [PubMed]
- 240.Reagan-Shaw S, Nihal M, Ahmad N. Dose translation from animal to human studies revisited. Faseb j. 2008;22:659–661. doi: 10.1096/fj.07-9574LSF. 1:CAS:528:DC%2BD1cXjtVaqsrY%3D, 17942826. [DOI] [PubMed] [Google Scholar]
- 241.*Erasmus, J. H. et al. Single-dose replicating RNA vaccine induces neutralizing antibodies against SARS-CoV-2 in nonhuman primates. Preprint at 10.1101/2020.05.28.121640 (2020). [DOI]
- 242.*Routhu, N. K. et al. Modified vaccinia Ankara based SARS-CoV-2 vaccine expressing full-length spike induces strong neutralizing antibody response. Preprint at 10.1101/2020.06.27.175166 (2020). [DOI]
- 243.*Tian, J.-H. et al. SARS-CoV-2 spike glycoprotein vaccine candidate NVX-CoV2373 elicits immunogenicity in baboons and protection in mice. Preprint at 10.1101/2020.06.29.178509 (2020). [DOI] [PMC free article] [PubMed]
- 244.*Yahalom-Ronen, Y. et al. A single dose of recombinant VSV-ΔG-spike vaccine provides protection against SARS-CoV-2 challenge. Preprint at 10.1101/2020.06.18.160655 (2020). [DOI] [PMC free article] [PubMed]
- 245.Jiang Y, et al. Blockade of the C5a-C5aR axis alleviates lung damage in hDPP4-transgenic mice infected with MERS-CoV. Emerg. Microbes Infect. 2018;7 doi: 10.1038/s41426-018-0063-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 246.von Weyhern CH, Kaufmann I, Neff F, Kremer M. Early evidence of pronounced brain involvement in fatal COVID-19 outcomes. Lancet. 2020;395:e109. doi: 10.1016/S0140-6736(20)31282-4. [DOI] [PMC free article] [PubMed] [Google Scholar]