Graphical abstract
Keywords: Coronaviruses, COVID-19, SARS-CoV-2, Transmission, Reproduction number, Pathogenesis
Abstract
As the new cases of COVID-19 are growing every daysince January 2020, the major way to control the spread wasthrough early diagnosis. Prevention and early diagnosis are the key strategies followed by most countries. This study presents the perspective of different modes of transmission of coronavirus,especially during clinical practices and among the pediatrics. Further, the diagnostic methods and the advancement of the computerized tomography have been discussed. Droplets, aerosol, and close contact are thesignificantfactors to transfer the infection to the suspect. This study predicts the possible transmission of the virus through medical practices such as ophthalmology, dental, and endoscopy procedures. With regard to pediatric transmission, as of now, only afew child fatalities had been reported. Childrenusually respond to the respiratory virus; however, COVID-19 response ison the contrary. The possibility of getting infected is minimal for the newborn. There has been no asymptomatic spread in children until now. Moreover, breastfeedingwould not transmit COVID-19, which is encouraging hygiene news for the pediatric. In addition, the current diagnostic methods for COVID-19 including Immunoglobulin M (IgM) and Immunoglobulin G (IgG)and chest computed topography(CT) scan, reverse transcription-polymerase chain reaction (RT-PCR) andimmunochromatographic fluorescence assay, are also discussed in detail. The introduction of artificial intelligence and deep learning algorithmhas the ability to diagnose COVID-19 in precise. However, the developments of a potential technology for the identification of the infection, such as a drone with thermal screening without human intervention, need to be encouraged.
1. Introduction
Coronavirus disease (COVID-19) is initially identified as a pneumonia virus in Wuhan, and it is named as SARS-CoV-2 by the World health organization (WHO) on 12th Jan 2020. This disease originated from a local seafood market in Huanan, Wuhan city, China [1]. The common symptoms of early infections are fever, cough, and other respiratory issues. Some patients have not reported any symptoms. Among the infected patient, 68 % reported dry cough and the 33 % observed with wet cough (mucus production). Cough is a major transmission route of CoV-2. To avoid the cough the inflected patients were treated with lidocaine during intubation and extubation. Lidocaine reduces the cough without major side effects [52]. In addition, 82.1 % of patients had lymphopenia, and 33.7 % had leukopenia. As the infection increases, the infected patient faces severe respiratory syndrome, lung issues, and kidney failure in some cases. Clinical observations stated no response for treatment with conventionalantibiotics. The patients still lost their blood cells and had an uncontrollable body temperature. COVID-19 looks similar to the severe acute respiratory syndrome-related coronavirus (SARS-CoV) that originated from bats [2,3]. However, few samples revealed that the spike protein content of SARS-CoV-2 is not a bat beta-coronavirus nor the pangolin beta-coronavirus [4,5].Further, no animal virus looked the same as CoV-2. Besides, the mutations in the spike protein make the CoV-2 bind with the human angiotensin-converting enzyme 2 (ACE2). The progenitor of CoV-2 jumped to humans without being detected, and it was transmitted rapidly from human to human. Similar to CoV-1, CoV-2 acquired receptor-binding domain (RBD) mutations during transmission in the cell, where the study revealed that CoV-2 is not a purposefully modified virus. However, at the moment, it cannot be proved or disproved with the available data [6,7].
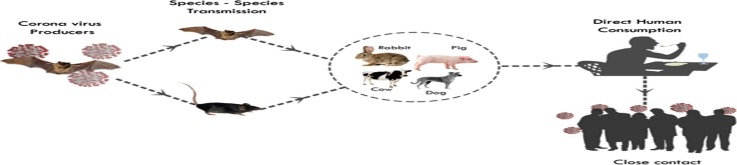
CoV-2 is a Ribonucleic acid (RNA) virus, which can infect animals and humans. The infection with coronavirus leads to respiratory, gastrointestinal, and neurologic syndromes [8]. It has been believed that wild animals and bats are the natural hosts. Wuhan reported that the patients are suffering from viral pneumonia fever in the city starting from December 2019. It wasidentified as a CoV virus and later named as SARS-CoV-2. CoV-2 virus consists of a structured protein such as spike (S), membrane (M), envelope (E), hemagglutinin esterase (HE), and nucleocapsid (N). Electron microscopy revealed that compared to other proteins, the content of M is higher. Thus, the M protein determines the shape of COVID-19 [9,10].
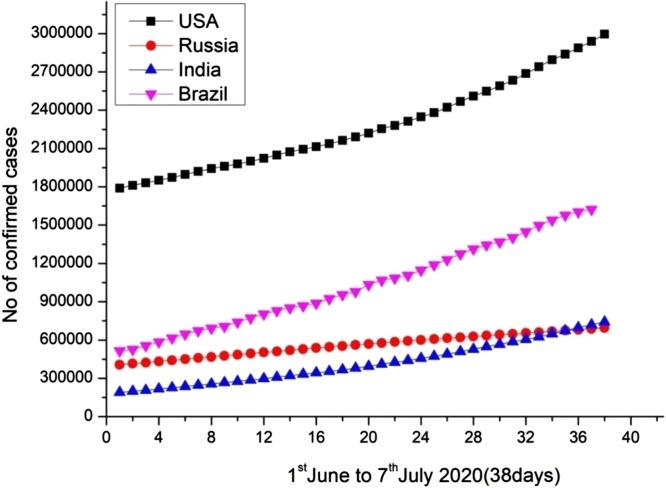
Further, the coronavirus is zoonotic in origin [11]. Hence, it can evolve into a strain to infect humans. The primary symptoms are fever (88 %), fatigue (38 %), dry cough (68 %), sore throat (15 %), sputum production (33 %), muscle pain (15 %) and respiratory problems (19 %) [12]. As of now (January 10 to March 30, 2020), there were 752,263 reported COVID-19 cases and 36,204 deaths around the world as per the record of worldometers with the mortality rate of 15 %. The mortality rates were high in April 2020. As the treatment procedure was aggravated, the mortality rates were reduced significantly. The current mortality is 10 %, which is a positive note. However, the report on new cases is growing. In the last few months (April 2020- June 2020), the report of fresh cases of COVID-19 increased by 54 %, which needs extensive attention. As of 10 June 2020, the total cases were approximately 7,451,900, with reported deaths of 418,891. Fig. 1 indicates the total number of COVID-19 cases identified in the major countries.
Fig. 1.
Total number of COVID-19 cases identified in the major countries between June 1∼ July 07, 2020 [European CDC].
2. Transmission of COVID-19
The transmission takes place mainly through human to human during intimate contact with each other. In the early period, it was reported that coronavirus affected 72 % of resident people, and 31 % had a travel history to Wuhan [13]. Recent researches have pointed out that human proximity and social interaction increase the transmission of the virus. Finding the transmission link is very tedious. Thus, mathematical modeling patterns are applied to predict infectious transmission. Although there are several methods to predict the rate of spread, the uncertainty is high [14,15]. Among the several rates of transmission,thedropletsaretheprimary sources(Fig. 2 ). Picking the contaminated surfaces and touching face increases the risk of getting infected. The recent spread of infection through stool has been confirmed [16]. The latest investigation reveals the possibility of transmission through the ocular surface [17]. Studies showed the impact of handwashing and transmission of the virus after hand sanitizing. They identified that washing hands at least 5 times per day would reduce the overall risk of infection [Incidence rate ratios (IRR) = 0.35, P = 0.02]. Further, washing hands after cough or sneeze minimize the risk of transmission via household objects [IRR = 3.35 & P = 0.02] [18]. The importance of the mask and the social distancing were discussed in detail. In general the particles (60−100 μm) emitted by the infected person fall to the ground within 6 feet. However, in some rare cases stimulated cough and sneeze droplets (> 0.1 mm) of the person can travel more than 12 feet. Since the average person aerosol transmission occurs between 4.5–6 feet, the social distance of 6 feet rule has been strictly followed. Besides, the social distancing rules differ from countries to countries based on the rules imposed by the regional authorities guidelines. For instance, Australia follows 5 feet whereas the Denmark, France and Lithuania follow 3 feet rules. Notable study concluded the 13 % of the risk of getting infected takes place within 1 m. Beyond 1 m, the risk rate drastically reduced to 3 %. Further, for every increase in 3 feet reduces the risk by half.
Fig. 2.
Transmission of COVID-19 to the susceptible individual.
To avoid transmission of the virus wearing mask and the social distancing are the effective tool. Based on the current evidence the proper mask reduces the transmission of droplets on both clinical and laboratory environment. Despite the several types of mask, N95 offers higher protection followed by surgical mask against COVID-19. Due to the limitation of N95, the non-health care people are recommended to use handmade cloth mask with adequate social distancing guidelines and recommendations. A notable article made a natural study on the mandate face mask and the growth rate of infection. Wearing the mask reduces the growth rate of COVID-19, which became obvious. Decline in the growth rate were reported after the US state government mandates the face mask. For instance after 5th date of mandate face mask the growth rate dropped by 1.1 % and it is increased to 2 % after couple of weeks. From this significance finding, role of face mask and social distancing was apparent [51].
Identifications of the infection at the early stages are possible by developing superior technology. For instance, the drone with a thermal camera can detect the infected person without any human intervention. Further, it can be useful to identify the person not wearing mask through artificial intelligence technology. Few notable works reveal the reproduction number (R0) can be changed from 1.5–6.49 based geographic locations. Further, the key studies reveal the R0 of CoV-2 to be 3.28, which is higher than the early prediction by the WHO. Further, based on the current reproduction rate,the median is 2.79, and the interquartile range (IQR) was 1.16 [1]. Several guidelines have been proposed for both medical personnel and infected patients to ensure high safety such as,
For medical personnel,
-
•
The medical staff treating the patient should be isolated
-
•
Their routine activities must be monitored
-
•
If they witness any problems such as fever, cold, and cough, they need to be quarantined
-
•
The team officials must check whether the medical personnel are following the preventive measures.
Recent studies showed thatCoV-2 could live in the air for several hours, and it can remain intact on the surface for more than 2–3 days. Further, the findings observed that the virus could live up to 4 h in copper and 2–3 days in steel. Moreover, the virus stays on plastic longer than any other host. However, there is no evidence of cloth exposure still [19]. Meanwhile, they also observed that the virus could spread through droplets in air medium, by human contact and surface contact. Some myths indicated that COVID-19 couldnotlive in hot temperatures. However, there is no adequate proof ofthe same. Thus, isolating infected patients is very crucial. As per the WHO situation report 64, European regions and northern America have been confirmed with the highest number of cases [4]. This denotes the crucial role of temperature on transmission. The patients must be identified before they transmit the disease. It can be made possible by the screening criteria.
Some preliminary countermeasures are,
-
•
Finding the history of the travel and quarantine
-
•
Monitoring the temperature of the people
-
•
Observing the movement of people who are in-home quarantine.
-
•
Alerting the society by pasting the warning symbols on the respective walls of home quarantine person
-
•
Identifying the premature sickness (If the patients are infected, they are treated with oxygen therapy, intravenous immunoglobulin, antiviral therapy, and empirical antimicrobial therapy).
From the previous lessons learned through the management of several diseases, prevention is the best cure to fight against this new novel virus to reduce the mortality rate. Four key features can avoid fatalities, such as prevention, response, transmission, and treatment.
2.1. Transmission of COVID-19 through eyes
Sun et al. reported the transmission of novel coronavirus through the eyes. The role of the eye in transmitting the SARS-CoV and COVID-19 is scarce. Nevertheless, the entry of CoV is tested through the exposure of tears and conjunctival secretions from infected patients. Further, the viral transmissions during the practice of ophthalmicdiagnosis are possible. Thus, medical personnel are strictly advised to maintain hand hygiene and personnel protection [20].As perthe previous infections of SARS-CoV, exposure of the virus to ultraviolet irradiation and heating can control infection. Further, sterilization at 56 °C for 30 min with lipid solvents can make the ophthalmic instrument safe from transmitting.
2.2. Transmission of COVID-19 through dental procedures
The possibility of transmission through dental practice is higher owing to close communication, exposure of saliva, blood, and body fluids. Thus, the dentist has to be very cautious being injected. To prevent transmission through dental practices, some essential countermeasures are necessary.
There are different types of transmission, such as airborne, contact spread, and surface spread. Hence, there must be precautions before handling patients [21]. The crucial key points are
-
•
Hand hygiene
-
•
Use of personal protective measures
-
•
Mouth rinse before dental procedures
-
•
Knowing the travel history of the patient
-
•
Rubber dam isolation
-
•
Antiretractionhand piece
-
•
Disinfection of the clinical settings
-
•
Handling the medical wastes
-
•
By managing the above things, the spread through the dentistry can be avoided.
2.3. Transmission of COVID-19 through endoscopy
Endoscopy health care personnel will mostly not be working with COVID-19 patients. However, it is essential to know the critical things to stop the transmission during endoscopy treatments in the case of COVID-19 patients. During the treatment procedure, the distance between the patient and medical personnel is very short, which risks the spread of infection. Every patient undergoing the endoscopic treatment procedures, including 14 days track record examination such as travel history, body temperature, and other symptoms need to be checked. By doing the above method, the risk factor can be reduced. Further, the patient having any contact with the CoV-2 person or asymptomatic COVID-19 person willhavea high risk of executing the endoscopy procedure by the doctors [22]. Onthe contrary, wearing personal protective equipment’s such as mask, gloves, goggles, gowns, shields and other respiratory equipment’s are essential, which must be followed during this outbreak, especially and also the rapid testing method of COVID-19 can be used to evaluate the infection prior to endoscopy. The key ways of possible transmission during endoscopy are human to human, droplets, air, and body fluids [23].
If any of the patients werefound to be suffering from CoV-2 after the procedure, the entire room, including all the equipments must be sterilized and sanitized to avoid potential transmission.
2.4. Transmission of COVID-19 in pregnant women and infants
The incubation periods of COVID-19 are approximately 14 days [24]. The first child case was reported in Shenzhen. As of now, there are more than 230 children being affected by the coronavirus with no fatality [25].Similar to SARS, there is no mortality for COVID-19. However, the transmission of disease from neonates and children are possible. Thus, wearing protective equipments such as hats, gloves, suits, goggles, and mask are essential [26,27].Chen et al. reported a clinical course of four live-born infants whose mother infected with the virus at trimester and witnessed fever, cough, headache at the time of admission in the hospital. After the necessary test, it is observed lymphocytes were below the normal range for all patients. After performing CT, there are some abnormalities seen among all. Three patients underwent caesarean, and one patient with vaginal delivery. After the full-term birth of infants, they are isolated. A few days later, all mothers successfully recovered from COVID-19 infection. Although the mother possesses positive COVID-19 during pregnancy, their infant tested negative. So there is no transmission from mother to infant [28].
In another notable study, Liu et al. studied the reason for pregnant women being more susceptible to COVID-19. They reported no vertical transmission of the virus. Further, they found the virus to have the capacity to alter the immune response [29,30]. Hung et al. studied clinical and vertical transmission in nine pregnant women for novel pneumonia fever (COVID-19). Among the nine, seven suffered fever, including cough, sore throat, and malaise. Further, five patients experienced lymphopenia. The delivery of the newborn was successful. There was no vertical transmission, and breast milk samples tested negative for the virus [31].This denoted that breastfeeding can be done to the infants, even the mother is infected.
3. Diagnostic methods and procedures
COVID-19 can be detected using various diagnostic procedures such as chest CT scan, acid detection, epidemiological history, and clinical treatment. Since COVID-19 is highly contagious, finding a rapid and reliable diagnosis technique is significant. Although the origin of the virus took place in Wuhan, now under control there due to the effective utilization of diagnostic tests to identify the individual before the reproduction rates of infection were increased [32]. At the time of origin, the test procedures are different when compared to the latest clinical practices. For instance, the patients are subjected to a CT scan to find the infection. However, nowadays, the rapid test kits are used to predict the infection though uncertainty is a problem.
IgM and IgG is a simple technique performed to diagnosis the infected person. The test performed on 57 individuals. On comparing, IgG reported 72.7 % of the detection rate. Besides, the nucleic acid test report 87.5 %. Moreover, high-sensitivity C-reactive protein (hs-CRP) nucleic acid negative group observed higher test results compared to the positive group [33,34].To sum up, the use of IgM and IgG over nucleic acid detection is highly recommended. Furthermore, a combination of all these to predict COVID-19 leads to high reliability and precision. Zhang et al. diagnosed the presence of COVID-19 by identifying the presence of the spike protein. They evaluated six recombinant nucleocapsid and spike proteins using IgM and IgG. They found that rs1 and rs-receptor binding domain-mFc are highly suitable to diagnose theHCoV-19. In the same way, gold immunochromatography assay (GICA) can be used to identify the antibodies [34,35].
Unlike the above method, the chest CT is widely used to find the infected person through diagnostic imaging. The CT is performed only on the person who has been infected severely. In many positive patients, pulmonary consolidation is observed, and based on that, the infected patients are quarantined. In addition, few patients were observed with a decrease in WBC and lymphocytes. The effects of infection in Hubei patients were compared with those from other countries. This comparative determination has aidedin correlating the transmission of the virus from one geographic location to another. All patients, irrespective of their origin, suffered from fever, cough, and other respiratory issues. Likewise, the decrease in WBC and lymphocyte count was also seen [36].In traditional clinical procedures, X-ray imaging is performed to identify pulmonary diseases. However, in the case of COVID-19, using X-ray will not help due to the poor imaging characteristics, as shown in Table 1 . Thus, CT is used to identify the infected person. Generally, the uncertainty in determination exists owing to false-negative ground-glass opacification (GGO) detection. Moreover, the imaging differs from case to case based on age, infection seriousness, and health status. To identify the infection, a comprehensive diagnosis must be made using distribution pattern, quantity and range, density, shape, interface, internal features of the lesion and adjacent structural changes, CT staging, quantitative CT, and artificial intelligence (AI). The determination of CoV-2 using CT is not very clear. Furthermore, using CT on children is not specific [37,38].Thus, advanced computer-aided CT and AI are required urgently for screening patients and conducting virus surveillance.Further, analyzing the CT images by AI using deep learning reduces the uncertainty in the confirmation of the positive new case. Few notable works incorporated the neuro-network through a deep learning model, which has achieved 82 % accuracy on findings. Song et al. proposed a framework to predict COVID-19 with minimum time using AI technology engines. The designed framework was made of simple Smartphone sensor measurements. The designed framework was comprised ofa series of layers, such as input, measurement, sensing, computing, and predicting layers. The implementation of the proposed AI increased the mobility of diagnosis. The reliability was higher since the framework used multiple readings to diagnose. Another reliable method is deep learning. Deep learning was proposed based on the CT diagnosis system to detect patients with COVID-19 using radiograph imaging. The model was built based on 88 patients' CT images. The DREnet architecture used ground-glass opacity in CT images to assist doctors in determining the infected persons [39].
Table 1.
Comparison of diagnostic imaging technique for COVID-19.
| Type of diagnostic imaging | ||
|---|---|---|
| X-radiation | Computed Tomography | Ultrasound |
|
|
|
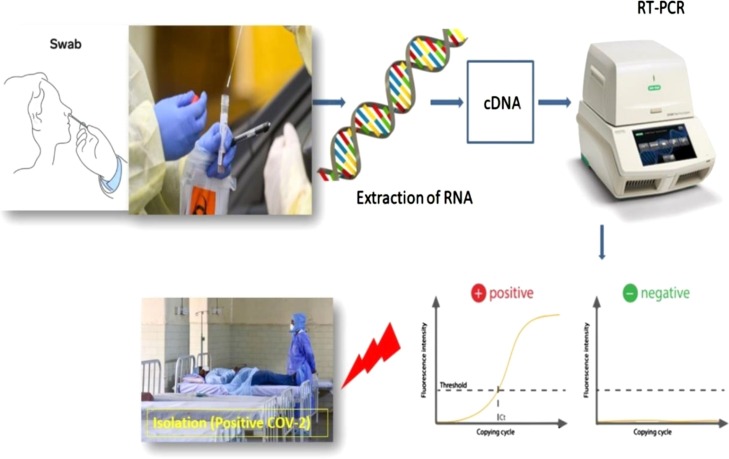
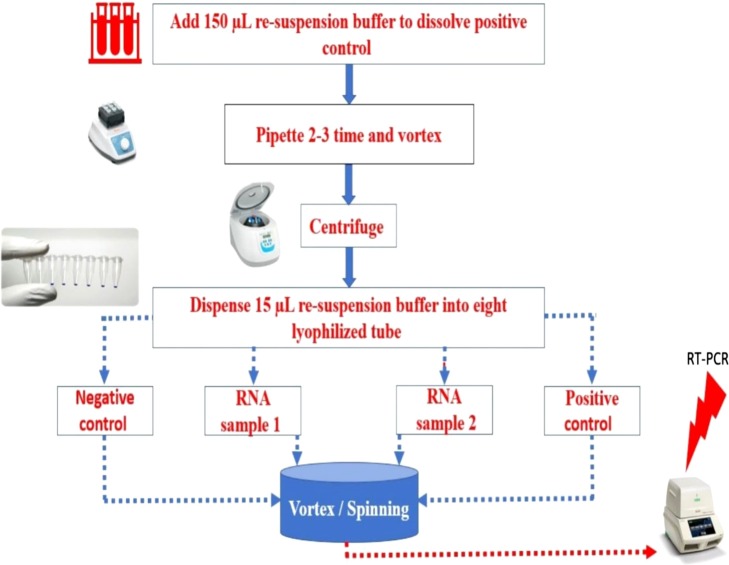
Another technique involves the use of real-time fluorescent RT-PCR to identify the virus [40]. Figs. 3 and 4 shows the diagnostic techniques to determine the infection using PCR kits. Initially, the duration of the test took two minimum days. After the upgrade, the reports are available within 6 h. Based on the accumulated experience, the PCR is replaced with a CT scan for the confirmed person. Based on the early prediction, the patient would receive special attention to fight COVID-19 [41]. Despite the above, a determination of the CoV-2 is possible by using immunochromatographic fluorescence assay. The fluorescence would be applied to the samples to detect the presence ofthenucleocapsid protein of CoV-2. 239 patients were diagnosed with nucleocapsid protein using anucleic acid test. All the patients underwent the acid test repeatedly for three times. On the whole, 208 patients tested positive for nucleic acid and 31 negatives for nucleic acid. Besides,thenucleic acid test is unstable, and the uncertainties in the test are high. Thus, the double-blind evaluation of the test is mandatory [42].
Fig. 3.
Diagnostic procedures of COVID-19.
Fig. 4.
Test sample preparation for the analysis of COVID-19 for reverse transcription polymerase chain reaction (RT-PCR).
3.1. Comparative analysis of CT and RT-PCR
The CT diagnosis employed to the COVID-19 positive patients based on the RT-PCR results. CT imaging is done based on a 4-day interval to monitor the function of the respiratory syndrome. CT scans are usually conducted on a single respiratory phase. To reduce the uncertainties, the patients are advised to hold breath during CT imaging [40,41]. The distribution of the abnormalities are recorded and evaluated by the digital database and the radiologist. The patients are evaluated based on the ground glass opacity, crazy paving, and consolidation. A notable studied derived CT scanobservations based on the seriousness of infections. All the patients were hospitalized and discharged after recovery with the mean days of 18. Based on imaging, the infection can be categorized into 4 stages. Further, the CT scan classified the different lobes such as left upper, left lower, right middle, and right lower. During stage 1, the maximum numbers of patients were observed with GGO (75 %), lesions in single lobe (42 %), and Consolidation (42 %). At stage II, consolidation (47 %), GGO (82 %), Crazy paving (53 %), multilobe (77 %), and peripheral lesion (59 %).Followed by at stage III, peripheral (70 %), bilateral multilobe (86 %), GGO (71 %), and consolidation (91 %). At stage IV, peripheral (70 %), bilateral multilobe (80 %), GGO (65 %), consolidation (75 %), and crazy paving pattern (0 %) [38]. As the patients getting cured, the GGO is decreased and the null observation for crazing paving patterns. From the above distribution frequency, it is evident COVID-19 can be diagnosed using GGO, consolidation, and crazy paving pattern. Further, the distribution of pulmonary lesion and the involvement of lesions also helped to detect the COVID-19 with the least precision since many patients were not observed with lesions [41].
Some studies revealed the effectiveness of PCR on CT. To understand this, comparative analysis between both is mandatory. A case report had been generated for 1014 confirmed cases in China. Based on the test dataof1014 suspected cases, the comparison of RT-PCR and CT is prepared. Nevertheless, the time interval between the RT-PCR and CT is approximately 5 days. Ai et al. reported a basic comparison of CT and PCR for 167 patients in China. Based on the comparison they revealed, 155 patients were confirmed with COVID-19 infection by testing using both. Onthe contrary, 12 patients were tested with false results in PCR compared to CT [42,43]. Further, the usage of PCR led to false negatives owing to insufficient viral material and laboratory errors. Yet again, immature nucleic acid, insufficient viral load, improper clinical sampling, low detection rate, and manufacturing defects were the other possibilities of errors in RT-PCR. By concluding all, CT is considered as more reliable for comprehensive evaluation and screening. Another study performed a statistical analysis using SPSS version 21.0. 95 % of the confidence interval was observed by the Wilson score method. Some patients with negative RT-PCR wereconfirmed with the infection by CT scans [43,44]. Thus, CT is preferred over RT-PCR when the patients carry clinical symptoms such as shortness of breath, cold, fever, and diarrhea.On the other end, the correlation between RT-PCR and CT was done to make sure the infected patients after complete recovery.
In summary, COVID-19 can be identified with higher precision using CT than RT-PCR. Further, the diagnosis of infection is possible by identifying the GGO and consolidation along the subpleural area of the lung. Identification of infected patients using CT can be more efficient to enable the prevention ofinfection transmission.
3.2. Molecular assays for COVID-19 diagnosis
Recently, there are various molecular assay methods that can detect 2019-nCoV, and some are under research and development to increase the testing feasibility to identify COVID-19 patients. Few assay methodsselectively detect the novel CoV,and some assays also detect other CoVstrains (e.g., SARS-CoV),which are genetically identical. Most countries shared their molecular assay protocols (Table 2 ). The list is not exhaustive and is being updated based on the current research. United States of America and China, Center for disease control and prevention(CDC)are extensively working on the assays by targeting the genes such as open reading frame 1ab (ORF1ab), RNA dependent RNA polymerase (RdRp) and nonstructural protein 14 (nsp14) for the detection of CoV-2 with high accuracy [45,47].
Table 2.
Summary of available molecular assays protocols for COVID-19 diagnosis as per WHO [[43], [44], [45], [46], [47], [48], [49]].
| Gene targets | Institute | Country |
|---|---|---|
| ORF1ab and N | China CDC | China |
| RdRP, E, N | Charité | Germany |
| ORF1b-nsp14, N | University of Hong Kong | Hong Kong |
| Pancorona and multiple targets, Spike protein | National Institute of Infectious Diseases, Department of Virology III | Japan |
| N | National Institute of Health | Thailand |
| Three targets in N gene | United States CDC | US |
| Two targets in RdRP | Institut Pasteur, Paris | France |
Recently, Abbott came up with ID NOW™ COVID-19, which can deliver the results in 5 min targeting theRdRpgene. The sampling types are throat, nasal, oropharyngeal swabs, and nasopharyngeal. The company decided to make a largebatch production, which helps to diagnose the COVID-19 at a very early stage. This will create a critical change in the current scenario (Table 3 ).
Table 3.
Major vaccine candidates in preclinical stages of development and research [56].
| Candidate | Sponsor/Firm | Trial Phase |
|---|---|---|
| Inactivated vaccine | Wuhan Institute of Biological Products; China National Pharmaceutical Group (Sinopharm) | Phase 3 |
| CoronaVac | Sinovac | Phase 3 |
| Bacillus Calmette-Guerin (BCG) live-attenuated vaccine | University of Melbourne and Murdoch Children’s Research Institute; Radboud University Medical Center; Faustman Lab at Massachusetts General Hospital | Phase 2/3 |
| AZD1222 | The University of Oxford; AstraZeneca; IQVIA | Phase 2/3 |
| mRNA-1273 | Moderna | Phase 2 |
| Ad5-nCoV | CanSino Biologics | Phase 2 |
| BNT162 | Pfizer, BioNTech | Phase 1/2 |
4. Outlook of clinical procedures and treatment
Wei et al. made a study on the clinical characteristics of CoV-2 in china. More than a thousand patient data were extracted. The majority of the infected persons were treated with antibiotic therapy (58 %), oseltamivir (36 %), oxygen therapy (41.3 %), and mechanical ventilation (6.1 %). Mechanical ventilation is used in patients who are incritical condition. Among all the patients, 204 patients are hospitalized for a minimum of 12 days [13].
Han et al. reported the clinical treatment procedure for a 47-year-old man in Wuwei. The patient tested positive, and the test results indicated that the patient suffered from decreased lymphocytes, increased C-reactive protein, high fibrinogen, and elevated lactic dehydrogenase [45]. Further, CT reported a multiple patchy high-density shadow, similar to other patients reported in the notable literature [46]. To handle the respiratory issue, oxygen inhalation therapy was used. In addition, rehydration therapy was performed. Blood glucose and blood pressure were closely monitored. In addition, the patient was treated with lopinavir and ritonavir tablets. After a day’s treatment, the patient faced shortness in breath and chest tightness, occasionally. On the following day, methylprednisolone was advised for 5 days. The patient was discharged on day 10 without any symptoms. The detailed procedure on medication is available in the literature [48,49]. Although the treatment was continuous, the patient’s body temperature, blood pressure, and respiratory rate were on fluctuations [50].
Based on the response of the infected patients, 15 drugs were initially identified as the potential break through for the treatment of the COVID-19 are chloroquine-hydroxychloroquine, lopinavir-ritonavir, nafamostat-camostat, famotidine, umifenovir, nitazoxanide, ivermectin, corticosteroids, tocilizumab-sarilumab, bevacizumab and Fluvoxamine [53]. Besides, based on the recent reports dexamethasone and remdesivir drugs are widely considered as the life saving drug. Based on the study on 1063 patents it was convinced that, remdesivir performed significantly in reducing the symptoms and the recovery time of the adults with the COVID-19 infection [54]. However use of the remdesivir in the developing countries like India was questionable due to its cost and availability. Dexamethasone is a cheap steroid used to fight the inflammation in the moderate and severely infected patient. Based on the current progress the dexamethasone cut the mortality rate by one-third of the patients in the ventilator [55]. In the other end, the studies predicted use of the drug is safe since it carries fewer side effects based on the short exposure. On the contrary, the long term side effects of the drug are still under progress. With regard to the potential COVID vaccines, the top three candidates are Oxford-AstraZeneca, Pfizer-BioNtech & Moderna. Based on the phase 1 results, Oxford-AstraZeneca trials were promising compared to other competitors. Oxford-AstraZeneca AZD1222 vaccine based on the chimpanzee ChAdOx1 adenovirus. As on July 2020, the phase II/III trials were undergoing in the countries like UK, Brazil and South Africa. Based on the outcome of phase 1 results, the vaccine generates the dual immune response to the people range between 18–55 years. AZD1222 develops the protective neutralising antibodies to target the coronavirus. In August 2020 the phase III trials to be started in India, and the vaccine available in the market as early as November with estimated cost below $13. In the other hand, the US supported Moderna’s mRNA-1273 vaccine available in the end of December with the cost of $50−60. Moderna uses the RNA messenger to nudge the immune system to combat the virus. Pfizer (US)-BioNtech (German) BNT162b2 is on phase II/III trials, based on the results from the trials two doses of vaccines are necessary to neutralise the virus. In the major advantage of the Pfizer vaccine is its proce, the expected estimated cost were $3−4 per dose [56].
5. Conclusion
The incubation period of COVID-19 is 14 days in the host, and the possible outliner is expected to be 27 days. Besides, the average incubation period is 5.2 days, with a 95 % confidence interval level. Notable studies concluded that they could live in plastic longer than 2 days compared to copper or steel. Further, the transmission of COVID-19 from the patients to the medical personnel is vulnerable. Despite the field of general medicine, the possibility of transmission through eyes and dental practices are probable. Perhaps, washing the hands at least 5 times in the day and wearing the protective shields would reduce the transmission of COVID-19 to others, significantly. Pregnant women are more susceptible than the general population. Findings denoted no trace of intrauterine vertical transmission. Infants are not asymptomatic. None of the mothers has developed severe COVID-19 after giving birth. Further, there is no trace of the virus in breast milk until now. All infants of the infected mother were tested negative for COVID-19. In addition,lymphopenia is commonly seen in pregnant women. Early diagnosis of CoV-2 is an effective way to reduce the reproduction ratio. Although there are many ways to identify the infected person, CT- AI is aneffective way with high accuracy. In addition, RT-PCR can be used to detect the infection in a rapid way. Besides, IgM and IgGare also very effective,and they are coupled with the nucleic acid test.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgements
The authors are thankful to the Ministry of Science and Technology-Taiwan (MOST107-2113-M-037-007-MY2), and NSYSU-KMU collaboration research project (109KN007)-Taiwan for research grant supports. This work was also financially supported by the Research Center for Environmental Medicine, Kaohsiung Medical University, Kaohsiung, Taiwan from The Featured Areas Research Center Program within the framework of the ‘Higher Education Sprout Project’ by the Ministry of Education (MOE) in Taiwan. This study is supported partially by Kaohsiung Medical University Research Center Grant (KMU-TC108A01). The authors are thankful to Sathyabama Institute of Science and Technology-Chennai city, India, and Duy Tan University, Da Nang, Vietnam, for supporting the work.
References
- 1.Novel C.P.E.R.E. The epidemiological characteristics of an outbreak of 2019 novel coronavirus diseases (COVID-19) in China. Zhonghua liu xing bing xue za zhi= Zhonghua liuxingbingxue zazhi. 2020;41(2):145. doi: 10.3760/cma.j.issn.0254-6450.2020.02.003. [DOI] [PubMed] [Google Scholar]
- 2.Yang P., Wang X. COVID-19: a new challenge for human beings. Cell. Mol. Immunol. 2020;17(5):555–557. doi: 10.1038/s41423-020-0407-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Zhou P., Yang X.-L., Wang X.-G., Hu B., Zhang L., Zhang W., Si H.-R., Zhu Y., Li B., Huang C.-L. A pneumonia outbreak associated with a new coronavirus of probable bat origin. Nature. 2020;579(7798):270–273. doi: 10.1038/s41586-020-2012-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.W.H. Organization . Vol. 72. 2020. (Coronavirus Disease 2019 (COVID-19): Situation Report). [Google Scholar]
- 5.Liu Q., Liu Z., Zhu J., Zhu Y., Li D., Gao Z., Zhou L., Tang Y., Zhang X., Yang J. Assessing the global tendency of COVID-19 outbreak. MedRxiv. 2020 [Google Scholar]
- 6.Burkle F.M. Declining public health protections within autocratic regimes: impact on global public health security, infectious disease outbreaks, epidemics, and pandemics. Prehosp. Disaster Med. 2020;35(3):237–246. doi: 10.1017/S1049023X20000424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Cyranoski D. This scientist hopes to test coronavirus drugs on animals in locked-down Wuhan. Nature. 2020;577(7792):607. doi: 10.1038/d41586-020-00190-6. [DOI] [PubMed] [Google Scholar]
- 8.Weiss S.R., Leibowitz J.L. Elsevier; 2011. Coronavirus Pathogenesis, Advances in Virus Research; pp. 85–164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Chen Y., Liu Q., Guo D. Emerging coronaviruses: genome structure, replication, and pathogenesis. J. Med. Virol. 2020;92(4):418–423. doi: 10.1002/jmv.25681. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Zhu N., Zhang D., Wang W., China Novel Coronavirus Investigating and Research Team A novel coronavirus from patients with pneumonia in China. N. Engl. J. Med. 2019 [published January 24, 2020] [Google Scholar]
- 11.Millán-Oñate J., Rodriguez-Morales A.J., Camacho-Moreno G., Mendoza-Ramírez H., Rodríguez-Sabogal I.A., Álvarez-Moreno C. A new emerging zoonotic virus of concern: the 2019 novel Coronavirus (SARS CoV-2) Infection. 2020;24(3):187–192. [Google Scholar]
- 12.Cui J., Li F., Shi Z.-L. Origin and evolution of pathogenic coronaviruses. Nat. Rev. Microbiol. 2019;17(3):181–192. doi: 10.1038/s41579-018-0118-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Byrareddy H.A.R.N. The epidemiology and pathogenesis of coronavirus disease (COVID-19) outbreak. J. Autoimmun. 2020 doi: 10.1016/j.jaut.2020.102433. Available online 26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kucharski A.J., Russell T.W., Diamond C., Liu Y., Edmunds J., Funk S., Eggo R.M., Sun F., Jit M., Munday J.D. Early dynamics of transmission and control of COVID-19: a mathematical modelling study. Lancet Infect. Dis. 2020 doi: 10.1016/S1473-3099(20)30144-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Guan W.-j., Ni Z.-y., Hu Y., Liang W.-h., Ou C.-q., He J.-x., Liu L., Shan H., Lei C.-l., Hui D.S. Clinical characteristics of coronavirus disease 2019 in China. N. Engl. J. Med. 2020;382(18):1708–1720. doi: 10.1056/NEJMoa2002032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hosoda T., Sakamoto M., Shimizu H., Okabe N. SARS-CoV-2 enterocolitis with persisting to excrete the virus for approximately two weeks after recovering from diarrhea: a case report. Infect. Control Hosp. Epidemiol. 2020;41(6):753–754. doi: 10.1017/ice.2020.87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Lu C.-w., Liu X.-f., Jia Z.-f. 2019-nCoV transmission through the ocular surface must not be ignored. Lancet (London, England) 2020;395(10224):e39. doi: 10.1016/S0140-6736(20)30313-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Beale S., Johnson A.M., Zambon M., Hayward A.C., Fragaszy E.B. 2020. Hand and Respiratory Hygiene Practices and the Risk and Transmission of Human Coronavirus Infections in a UK Community Cohort, Flu Watch, Hand and Respiratory Hygiene Practices and the Risk and Transmission of Human Coronavirus Infections in a UK Community Cohort. (3/8/2020) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Van Doremalen N., Bushmaker T., Morris D., Holbrook M., Gamble A., Williamson B., Lloyd-Smith J.O. Aerosol and surface stability of SARS-CoV-2 as compared with SARS-CoV-1. N. Engl. J. Med. 2020 doi: 10.1056/NEJMc2004973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Sun C.-b., Wang Y.-y., Liu G.-h., Liu Z. Role of the eye in transmitting human coronavirus: what we know and what we do not know. Front. Public Health. 2020;8:155. doi: 10.3389/fpubh.2020.00155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Peng X., Xu X., Li Y., Cheng L., Zhou X., Ren B. Transmission routes of 2019-nCoV and controls in dental practice. Int. J. Oral Sci. 2020;12(1):1–6. doi: 10.1038/s41368-020-0075-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Repici A., Maselli R., Colombo M., Gabbiadini R., Spadaccini M., Anderloni A., Carrara S., Fugazza A., Di Leo M., Galtieri P.A. Coronavirus (COVID-19) outbreak: what the department of endoscopy should know. Gastrointest. Endosc. 2020 doi: 10.1016/j.gie.2020.03.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Ong J., Cross G.B., Dan Y.Y. The prevention of nosocomial SARS-CoV2 transmission in endoscopy: a systematic review of recommendations within gastroenterology to identify best practice. medRxiv. 2020 [Google Scholar]
- 24.Jiang X., Niu Y., Li X., Li L., Cai W., Chen Y., Liao B., Wang E. Is a 14-day quarantine period optimal for effectively controlling coronavirus disease 2019 (COVID-19)? medRxiv. 2020 [Google Scholar]
- 25.Bi Q., Wu Y., Mei S., Ye C., Zou X., Zhang Z., Liu X., Wei L., Truelove S.A., Zhang T. Epidemiology and Transmission of COVID-19 in Shenzhen China: analysis of 391 cases and 1,286 of their close contacts. MedRxiv. 2020 doi: 10.1016/S1473-3099(20)30287-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Lee P.-I., Hu Y.-L., Chen P.-Y., Huang Y.-C., Hsueh P.-R. Are children less susceptible to COVID-19? J. Microbiol. Immunol. Infect. 2020 doi: 10.1016/j.jmii.2020.02.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Lu Q., Shi Y. Coronavirus disease (COVID‐19) and neonate: what neonatologist need to know. J. Med. Virol. 2020;92(6):564–567. doi: 10.1002/jmv.25740. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Chen Y., Peng H., Wang L., Zhao Y., Zeng L., Gao H., Liu Y. Infants born to mothers with a new coronavirus (COVID-19) Front. Pediatr. 2020;8:104. doi: 10.3389/fped.2020.00104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Liu H., Wang L.-L., Zhao S.-J., Kwak-Kim J., Mor G., Liao A.-H. Why are pregnant women susceptible to viral infection: an immunological viewpoint? J. Reprod. Immunol. 2020 doi: 10.1016/j.jri.2020.103122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Li Y., Zhao R., Zheng S., Chen X., Wang J., Sheng X., Zhou J., Cai H., Fang Q., Yu F. Lack of vertical transmission of severe acute respiratory syndrome coronavirus 2. China. 2020 doi: 10.3201/eid2606.200287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Chen H., et al. Clinical characteristics and intrauterine vertical transmission potential of COVID-19 infection in nine pregnant women: a retrospective review of medical records. Lancet. 2020 doi: 10.1016/S0140-6736(20)30360-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Sugishita Y., Kurita J., Sugawara T., Ohkusa Y. Preliminary evaluation of voluntary event cancellation as a countermeasure against the COVID-19 outbreak in Japan as of 11 March, 2020. medRxiv. 2020 doi: 10.1371/journal.pone.0239455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Jia X., Zhang P., Tian Y., Wang J., Zeng H., Wang J., Jiao L., Chen Z., Zhang L., He H. Clinical significance of IgM and IgG test for diagnosis of highly suspected COVID-19 infection. medRxiv. 2020 doi: 10.3389/fmed.2021.569266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Zhang P., Gao Q., Wang T., Ke Y., Mo F., Jia R., Liu W., Liu L., Zheng S., Liu Y. Evaluation of recombinant nucleocapsid and spike proteins for serological diagnosis of novel coronavirus disease 2019 (COVID-19) MedRxiv. 2020 [Google Scholar]
- 35.Konrad R., Eberle U., Dangel A., Treis B., Berger A., Bengs K., Fingerle V., Liebl B., Ackermann N., Sing A. Rapid establishment of laboratory diagnostics for the novel coronavirus SARS-CoV-2 in Bavaria, Germany. Eurosurveillance. 2020;25(9) doi: 10.2807/1560-7917.ES.2020.25.9.2000173. February 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Andersen K.G., Rambaut A., Lipkin W.I., Holmes E.C., Garry R.F. The proximal origin of SARS-CoV-2. Nat. Med. 2020;26(4):450–452. doi: 10.1038/s41591-020-0820-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Fan L., Li D., Xue H., Zhang L., Liu Z., Zhang B., Zhang L., Yang W., Xie B., Duan X. Progress and prospect on imaging diagnosis of COVID-19. Chin. J. Acad. Radiol. 2020:1–10. doi: 10.1007/s42058-020-00031-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.H.S. Maghdid, K.Z. Ghafoor, A.S. Sadiq, K. Curran, K. Rabie, A novel ai-enabled framework to diagnose coronavirus covid 19 using smartphone embedded sensors: design study, arXiv preprint arXiv:2003.07434 (2020).
- 39.Song Y., Zheng S., Li L., Zhang X., Zhang X., Huang Z., Chen J., Zhao H., Jie Y., Wang R. Deep learning enables accurate diagnosis of novel coronavirus (COVID-19) with CT images. medRxiv. 2020 doi: 10.1109/TCBB.2021.3065361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Ai T., Yang Z., Hou H., Zhan C., Chen C., Lv W., Tao Q., Sun Z., Xia L. Correlation of chest CT and RT-PCR testing in coronavirus disease 2019 (COVID-19) in China: a report of 1014 cases. Radiology. 2020;10 doi: 10.1148/radiol.2020200642. [published online ahead of print February 26, 2020] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Cheng Z., Lu Y., Cao Q., Qin L., Pan Z., Yan F., Yang W. Clinical features and chest CT manifestations of coronavirus disease 2019 (COVID-19) in a single-center study in Shanghai, China. Am. J. Roentgenol. 2020:1–6. doi: 10.2214/AJR.20.22959. [DOI] [PubMed] [Google Scholar]
- 42.Xie X., Zhong Z., Zhao W., Zheng C., Wang F., Liu J. Chest CT for typical 2019-nCoV pneumonia: relationship to negative RT-PCR testing. Radiology. 2020 doi: 10.1148/radiol.2020200343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Chung M., Bernheim A., Mei X., Zhang N., Huang M., Zeng X., Cui J., Xu W., Yang Y., Fayad Z.A., Jacobi A., Li K., Li S., Shan H. CT imaging features of 2019 novel coronavirus (2019-NCoV) Radiology. 2020 doi: 10.1148/radiol.2020200230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Corman V.M., Landt O., Kaiser M., Molenkamp R., Meijer A., Chu D.K., Bleicker T., Brünink S., Schneider J., Schmidt M.L. Detection of 2019 novel coronavirus (2019-nCoV) by real-time RT-PCR. Eurosurveillance. 2020;25(3) doi: 10.2807/1560-7917.ES.2020.25.3.2000045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Han W., Quan B., Guo Y., Zhang J., Lu Y., Feng G., Wu Q., Fang F., Cheng L., Jiao N. The course of clinical diagnosis and treatment of a case infected with coronavirus disease 2019. J. Med. Virol. 2020;92(5):461–463. doi: 10.1002/jmv.25711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Bischof E., Chen G., Ferretti M.T. Understanding COVID-19 new diagnostic guidelines–a message of reassurance from an internal medicine doctor in Shanghai. Swiss Med. 2020;150(0910) doi: 10.4414/smw.2020.20216. [DOI] [PubMed] [Google Scholar]
- 47.Organization W.H. World Health Organization; 2020. Laboratory Testing for Coronavirus Disease (COVID-19) in Suspected Human Cases: Interim Guidance. 19 March 2020. [Google Scholar]
- 48.Hirotsu Y., Mochizuki H., Omata M. Double-quencher probes improved the detection sensitivity of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) by one-step RT-PCR. medRxiv. 2020 doi: 10.1016/j.jviromet.2020.113926. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Casto A.M., Huang M.-L., Nalla A., Perchetti G.A., Sampoleo R., Shrestha L., Wei Y., Zhu H., Greninger A.L., Jerome K.R. Comparative performance of SARS-CoV-2 detection assays using seven different Primer/Probe sets and one assay kit. medRxiv. 2020 doi: 10.1128/JCM.00557-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Fadel M., Salomon J., Descatha A. Coronavirus outbreak: the role of companies in preparedness and responses. Lancet Public Health. 2020;5(4):e193. doi: 10.1016/S2468-2667(20)30051-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Lyu Wei, Wehby George L. Community use of face masks and COVID-19: evidence from a natural experiment of state mandates in the US: study examines impact on COVID-19 growth rates associated with state government mandates requiring face mask use in public. Health Aff. 2020:10–1377. doi: 10.1377/hlthaff.2020.00818. [DOI] [PubMed] [Google Scholar]
- 52.Aminnejad Reza, Salimi Alireza, Saeidi Mohammad. Lidocaine during intubation and extubation in patients with coronavirus disease (COVID-19) Canad. J. Anesthesia. 2020 doi: 10.1007/s12630-020-01627-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Shaffer L. 15 drugs being tested to treat COVID-19 and how they would work. Nat. Med. 2020 doi: 10.1038/d41591-020-00019-9. https://www.nature.com/articles/d41591-020-00019-9 [DOI] [PubMed] [Google Scholar]
- 54.Beigel John H., Tomashek Kay M., Dodd Lori E., Mehta Aneesh K., Zingman Barry S., Kalil Andre C., Hohmann Elizabeth, et al. Remdesivir for the treatment of Covid-19—preliminary report. N. Engl. J. Med. 2020 doi: 10.1056/NEJMc2022236. [DOI] [PubMed] [Google Scholar]
- 55.Moon Chang. 2020. Dexamethasone to the Rescue; p. 1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.2020. COVID-19 vaccine tracker RAPS. n.d. https://www.raps.org/news-and-articles/news-articles/2020/3/covid-19-vaccine-tracker (accessed July 30, 2020) [Google Scholar]