Abstract
This study aimed to investigate diabetes distress, happiness, and its associated factors of patients with type 2 diabetes mellitus (T2DM) treated by different therapies, and to analyze the related impact factors. A total of 1512 patients with T2DM were randomly selected from 18 tertiary hospitals in Hunan province from January 2016 to April 2016 who has been treated with oral antidiabetics monotherapy, insulin monotherapy, and combination therapy. Use the general information questionnaire, WHO-5 (the World Health Organization 5 well-being index) and PAID (the problem areas in diabetes scale) to collect the data. There are 846 (55.95%) patients that have serious emotional disorders, and the diabetes related distress in insulin treatment group was higher than that in combination treatment group (P < .05). Happiness of T2DM patients in combination therapy was higher than oral antidiabetic drug monotherapy and insulin monotherapy (P < .05). There was a negative correlation between diabetic suffering and happiness in patients with different treatments (R ranged from –0.335 to –0.436, P < .001). Age and happiness experience could explain 14.8% of the variance. Acute and chronic complications, controlled blood glucose level, lifestyle, therapies, and school education can explain 18.3% variance. Under different therapies, the suffering and happiness of T2DM patients differed from each other. The suffering and happiness of T2DM were related to different therapies, age, complications, glycaemic control, lifestyle, school education, and so on.
Keywords: diabetes distress, happiness, insulin, oral antidiabetic drug, type 2 diabetes mellitus
1. Introduction
Diabetes mellitus (DM) is a chronic lifelong disease especially type 2 diabetes mellitus (T2DM) which needs comprehensive, long-term, and strict self-management. The disease can inevitably affect the original life of patients, produce a variety of negative emotional experience and psychological pressure, and even can evolve into emotional and psychological disorders.[1] T2DM can increase the risk of both serious physical and mental health issues. Diabetes mellitus suffering (diabetes distress [DD]) refers to the suffering emotion caused by excessive anxiety in disease management, treatment approach, emotional burden, emotional support, and so on.[2] It was found that diabetic suffering was significantly associated with poor glycemic control, negatively affecting treatment compliance, self-management behavior, and risky lifestyle behavior.[3,4] Happiness is an individual's overall assessment of the quality of life according to self-determined criteria, and it is a comprehensive psychological index to measure the quality of life of individuals.[5] Epidemiological studies suggest that the prevalence of diabetes in China will double between 2000 and 2030 with the acceleration of population aging and urbanization,[6,7] and will be a major social and public health problem affecting people's livelihood,[8] the mental health status, and burden of patients are paid more attention.[9] Influenced by cultural tradition, economic development background and family structure, the suffering and happiness of T2DM in China are particular. In order to further understand the mental and spiritual world state of patients with T2DM and seek more scientific and perfect intervention measures, we used questionnaires to investigate and analyze DM treated by different methods.
2. Participants and methods
2.1. Study subjects
This study was approved by the ethics committee of all research institutes. T2DM patients were recruited from 18 tertiary hospitals in 7 cities of Hunan Province (Changsha, Yongzhou, Xiangtan, Zhuzhou, Yueyang, Hengyang, and Loudi).
All participates met the inclusion criteria: male or female sex, diabetes diagnosis at least 1 year before the recruitment in the study, signed informed consent; the only exclusion criterion was the incapability to fill in the study questionnaire according to the investigator judgment.
In this study, patients were divided into oral antidiabetic drug monotherapy (group A), insulin monotherapy (group B), combined therapy (group C, combination of oral antidiabetic drugs and insulin injection) according to the different therapies.
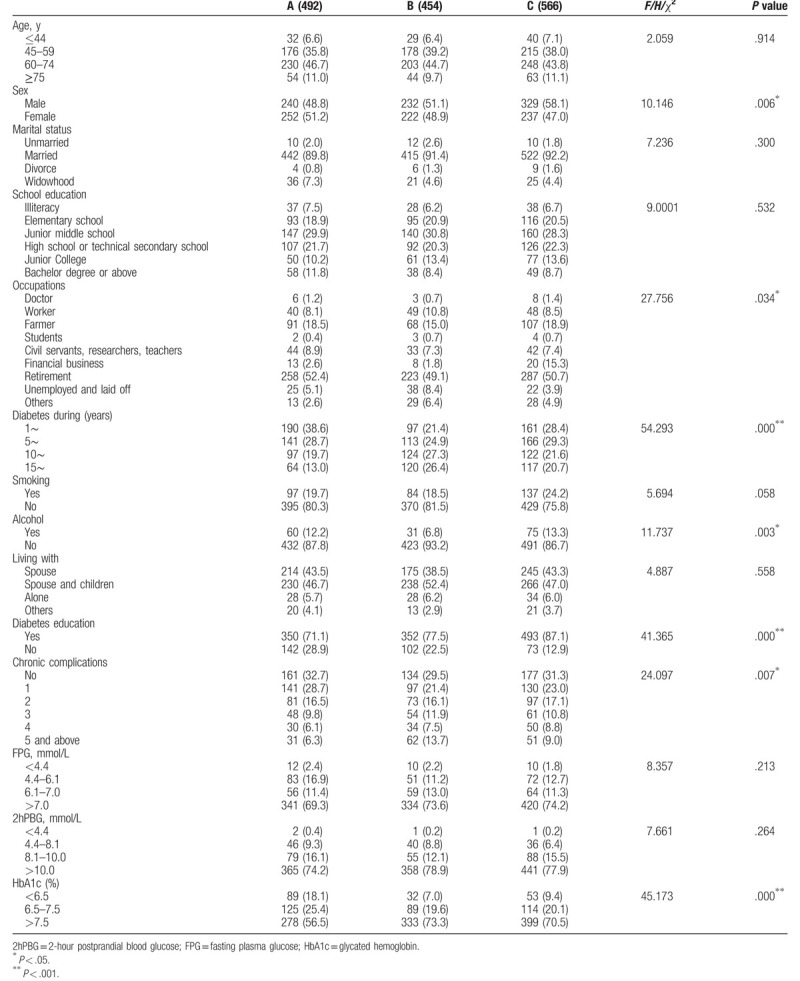
According to pre-survey feedback, the demographic data (age, sex, alcohol consumption, smoking, marital status, solitary living, school education, occupational type, and lifestyle) and chronic complications of the patients were obtained from questionnaires and medical records (Table 1).
Table 1.
General information and blood glucose control in each group (%).
2.2. Questionnaires
The questionnaires used in the study included standardized instruments for the evaluation of emotions.
We used the World Health Organization 5 well-being index (WHO-5) which is a self-rated questionnaire with high sensitivity and specificity[10,11] to assess the psychological well-being of diabetic patients. It can effectively reflect the happiness of patients in the past 2 weeks.[12] It is also a valid and reliable risk assessment measure for mild, moderate, and severe depression. It includes 5 items with responses on a 6-point Likert scale. A score <50 indicates poor psychological well-being, a score ≤28 indicates likely depression.
The problem areas in diabetes scale (PAID) has been widely used in various countries and has good reliability and validity in measuring the emotional disorders of patients.[3,4,11,13,14] In this study, a simplified version of the scale PAID-5 (consisting of items 3, 6, 12, 16, 19 of PAID) was used to conduct a questionnaire survey. PAID-5 is more suitable for large-scale investigation and application.
PAID-5 scores are transformed into a 0 to 100 scale, with higher scores indicating greater emotional distress. A cutoff of ≥40 was used to indicate the probable existence of a diabetes-related emotive impact. This cutoff score represents one standard deviation above the mean of the studied populations need psychological intervention urgently.[11]
The WHO-5 and PAID-5 scores were used as dependent variables, and the variables with statistical differences between univariate analysis groups were used as independent variables for multivariate linear regression analysis. Individual variables were assigned: age, duration of DM, recent blood glucose control (fasting plasma glucose [FPG], 2-hour postprandial blood glucose [2hPBG], and glycated hemoglobin [HbA1c]) using the original observation values; binary variables were assigned by “0–1,” including sex (female = 1, male = 0), smoking (is = 1, is = 0), drinking (is = 1, is = 0), diabetes education (is = 1, is = 0). Chronic complications and acute complications (with = 1, no = 0); multiple classified variables were dummy processed and converted into N–1 column dummy variables, including marital status, school education, occupational type, and lifestyle. The independent variable inclusion method was stepwise entry method (“STEPWISE”), and the test level was set as alpha entry = 0.05, alpha exit = 0.10.
2.3. Procedures
Questionnaire survey was used. The investigators of each research institute were trained uniformly before questionnaire survey. All the patients who participated in the study were required to sign the informed consent. Before the start of the survey, the investigators of every hospital briefly introduced the purpose and methods of this study. After obtaining the consent of the respondents, they used unified instructions and avoided inductive language to fill in the questionnaire anonymously. After filling in the questionnaire, the investigators checked the questionnaire and point out the missing items and errors to correct immediately. After the questionnaires were collected, researchers checked the questionnaires one by one and rejected the invalid questionnaires (missing value >10%, regular answers).
2.4. Statistical analysis
Data analysis was carried out by SPSS 18 software package (IBM Corp, Armonk, US). The counting data were described by example, percentage (%), and chi-square test or rank sum test, and the measurement data were described by mean (±s). t Test, one-way Analysis of Variance (LSD), Kruskal-Wallis H test, Spearman correlation analysis, and multiple stepwise regression analysis were used for statistical analysis. The test level was set at α = 0.05, and the difference was statistically significant at P < .05.
3. Results
3.1. Clinical characteristics of T2DM patients
The sample characteristics of the participants are listed in Table 1. We recruited 1512 patients, and all agreed to take part in the study. There were 801 men and 711 women, mean age (60.63 ± 11.294). Chronic complications: 729 cases of hypertension, 311 cases of cardiovascular disease, 239 cases of cerebrovascular disease, 226 cases of diabetic peripheral vascular disease, 254 cases of diabetic nephropathy, 440 cases of diabetic peripheral neuropathy, 370 cases of diabetic ophthalmopathy, 88 cases of diabetic foot. Acute complications: hyperglycemia hyperosmotic syndrome 29 cases, diabetic lactic acidosis 11 cases, diabetic ketoacidosis 86 cases, hypoglycemia 435 cases.
3.2. Happiness and diabetes distress in T2DM patients with different therapies
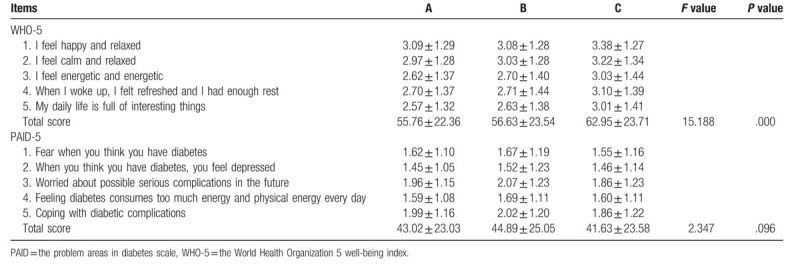
The mean score of WHO-5 in T2DM patients was (58.71 ± 23.44) >50, and that of 230 (15.21%) patients was <30. The happiness experience of T2DM patients in oral antidiabetic drug treatment group and insulin treatment group was lower than that of combined treatment group (P < .05). There was no significant difference in happiness between the oral antidiabetic treatment group and insulin treatment group (P > .05). The average score of PAID-5 was (43.06). The suffering level of DM in insulin treatment group was higher than that in combination treatment group (P < .05), and there was no significant difference between the other groups (P > .05) (Table 2).
Table 2.
Score and total score of WHO-5 and PAID-5 items in each group  .
.
3.3. Correlation analysis of happiness and diabetes suffering in T2DM patients with different treatments
Happiness and diabetes suffering were classified into different kinds based on WHO-5 and PAID-5 scores in 3 groups. It was found that the number of persons with possible depression, diminished happiness, and severe emotional disorder was deceased while the number of persons with happy, no or low emotional disorder was increased in Group C (Table 3). Spearman correlation coefficient fluctuated from R = –0.436 to –0.335, P < .001, indicating that there was a moderate negative correlation between happiness and diabetic suffering in T2DM patients with different treatment methods (Table 4). The stepwise regression equation model of overall happiness of T2DM patients was statistically significant (F = 18.817, P = .000), R2 = 0.193, and R2 = 0.183 after correction. The stepwise regression model of diabetic suffering in T2DM patients was statistically significant (F = 22.874, P = .000), R2 = 0.155, and R2 = 0.148 after correction. The variables for entering the equation model are shown in Table 5. The stepwise regression equation model of happiness of T2DM patients in oral antidiabetic group was statistically significant (F = 5.589, P = .000), R2 = 0.192, and R2 = 0.157 after correction. The stepwise regression equation model of diabetic suffering in the oral antidiabetic group was statistically significant (F = 23.619, P = .000), R2 = 0.127, and R2 = 0.121 after correction. The variables for entering the equation model are shown in Table 6. The stepwise regression equation model of happiness of T2DM patients in insulin treatment group was statistically significant (F = 10.182, P = .000), R2 = 0.171, and R2 = 0.154 after correction. The stepwise regression equation model of diabetic suffering in T2DM patients in insulin treatment group was statistically significant (F = 8.050, P = .000), R2 = 0.140, and R2 = 0.123 after correction. The variables for entering the equation model are shown in Table 7. The stepwise regression equation model of happiness of T2DM patients in the combined treatment group was statistically significant (F = 39.721, P = .000), R2 = 0.221, and R2 = 0.215 after correction. The stepwise regression equation model of diabetic suffering in T2DM patients in the combined treatment group was statistically significant (F = 69.318, P = .000), R2 = 0.198, and R2 = 0.195 after correction. The variables for entering the equation model are shown in Table 8.
Table 3.
Happiness and diabetic suffering classification in each group (%).
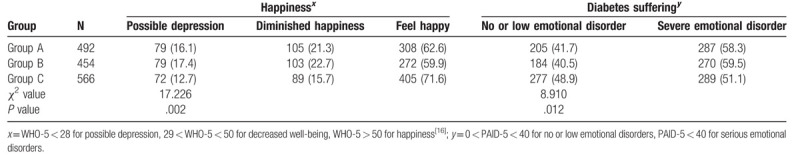
Table 4.
Correlation analysis between WHO-5 and PAID-5 scores in each group.
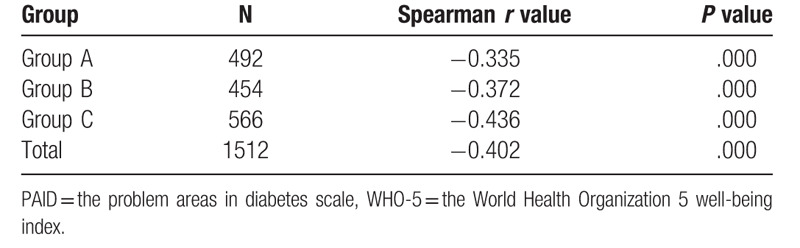
Table 5.
Multiple linear regression analysis of happiness and diabetic distress in T2DM patients (n = 1512).
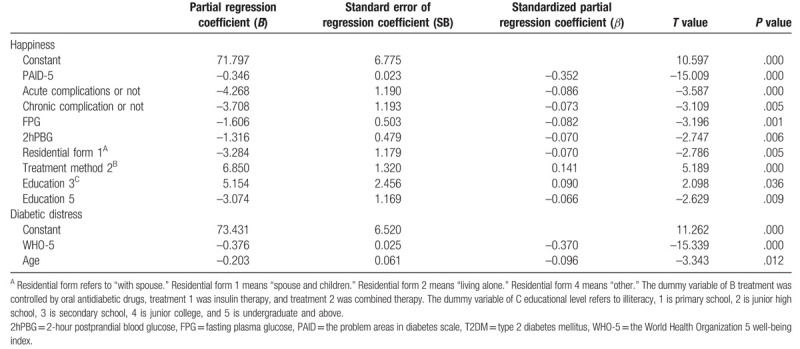
Table 6.
Multiple linear regression analysis of happiness and diabetic suffering in oral antidiabetic drugs group (n = 492).
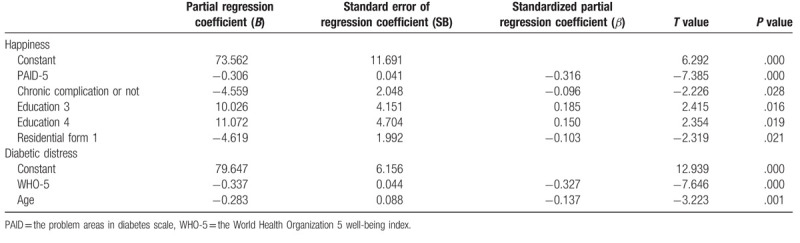
Table 7.
Multiple linear regression analysis of happiness and diabetic suffering in insulin treatment group (n = 454).
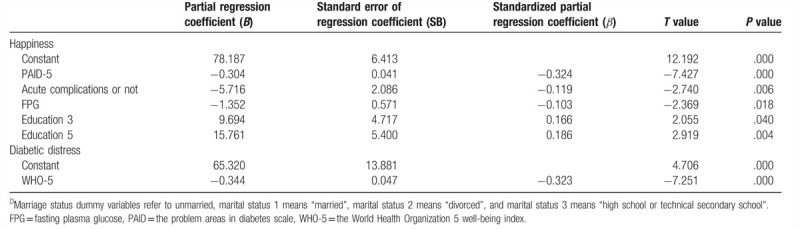
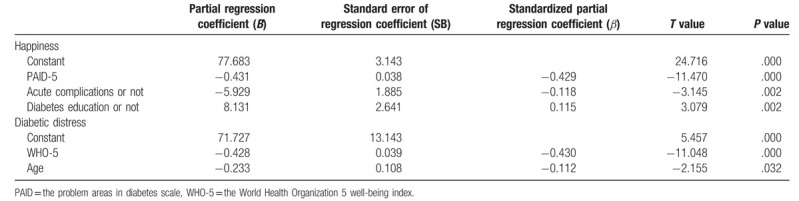
Table 8.
Multiple linear regression analysis of happiness and diabetic suffering in combined treatment group (n = 566).
4. Discussion
There were differences in happiness and diabetes distress among T2DM patients with different therapies.
The study showed that 55.95% of the patients had serious emotional disorders and suffered from diabetes-related psychological distress, which was slightly lower than other studies by Wang et al[15] (58.89%) and other scholars of China, but higher than the global survey incidence of the American Diabetes Association (18%–45%)[16] and DAWN2 (Diabetes Attitudes, Wishes, and Needs) study (46%). In addition, 34.85% of the patients reported a decrease in happiness, of which 15.21% had the possibility of concurrent depression, which was in close agreement with Fisher et al[17] view that 70% of the patients with diabetes depression were actually suffering from diabetes and 30% of the patients with high diabetes distress score were suffering from depression. The happiness of T2DM patients treated with combination of oral antidiabetic drugs and insulin injection was higher than that of monotherapy group (oral antidiabetic drugs or insulin treatment group), and the suffering level of DM in combination treatment group was lower than that of insulin treatment group. The reason may be that the subjects in this study have a longer course of disease (111.67 ± 83.190) months, more difficulty to control blood glucose and poor hypoglycemic effect and tolerance, while insulin combined with oral antidiabetic drug group is relatively satisfactory, it can relatively better control the disease to a certain extent, reduce the negative emotional experience of patients.
Our study showed that the combined treatment group had better happiness experience than monotherapy group which is inconsistent with Makine et al.[18] The reason may be that the T2DM patients investigated in this group have a longer course of disease (111.67 ± 83.190) months, more difficulty to control blood glucose, and more complicated with chronic complications, so the effect on emotion was not effective using a single treatment. Insulin combined with oral antidiabetic drugs can control the disease more effectively. Therefore, to a certain extent, combined therapies could improve happiness and decrease diabetes distress with patient's diet, exercise, and so on.
We showed that age was a protective factor for diabetes distress, which means older patients experienced lower levels of diabetes distress than younger patients, which are consistent with those of Zhou et al[19] and Wardian et al.[20] The reason may be that the patients in our study are older and have lower self-perception of disease-related distress than the young and middle-aged, so they are more optimistic. Older patients have more leisure time and can better adhere to exercise, diet, blood glucose monitoring, and other self-management programs. Therefore, we also remind the specialist doctors, nurses, and community health managers to help elderly patients with T2DM to establish regular lifestyle and implement various diabetes management plans, while not neglecting the guidance, supervision, and psychological counseling of young patients and to urge them to do a good job of time management, to cultivate, and enhance their good self-management so as to reduce psychological suffering and improve the quality of life.
The results of this study showed that the occurrence and existence of acute and chronic diabetic complications will negatively affect the happiness of patients in varying degrees which was consistent with the results of Baek et al[21] and Papathanasiou et al.[22] The reason of this condition may be physical suffering or inconvenience to patients with diabetes-related complications, which also increase the financial burden of treatment, and reduce the happiness of patients. Therefore, in addition to strictly controlling blood glucose levels, diabetic patients should also actively prevent and decrease the risk of diabetes-related chronic complications, reduce the psychological suffering of patients.
Our study showed that fasting plasma glucose and 2-hour postprandial blood glucose negatively affected the happiness of the patients which was in consistent with those of Fisher et al[17] and Graue et al.[23] Fasting blood glucose, 2-hour postprandial blood glucose, and other simple tests are indicators of blood glucose control. Intuitive and unsatisfactory blood glucose values will affect the emotional state of patients, affect disease-related management behavior, reduce the happiness experience of patients, and then aggravate their psychological distress. Therefore, it is suggested that DM suffering may already exist in patients with poor blood glucose control. In addition to helping patients improve blood glucose control, active psychological intervention should be taken as soon as possible to improve patients’ well-being experience and avoid developing into more serious psychological and emotional disorders.
The results of this study showed that the happiness of patients with higher education level (“high school or secondary school,” “college,” and “undergraduate and above”) was better than those with lower education level, which was in accordance with the results of Pintaudi et al[24] and Panagi et al.[25] The former is better than the latter in integrating various information channels and acquiring disease management related knowledge. It is easy to have a higher sense of responsibility in the process of disease management and is handier in dealing with the changes of diabetes and complications. The latter, because of the poor understanding of the disease and new knowledge acceptance, cognitive deficiencies, their awareness of diabetes self-management is weak. Therefore, in the process of diabetes self-management guidance, more practical individual guidance measures should be provided according to the education of different patients to help them to control blood glucose effectively and process various types of problems that may arise in the process of diabetes management.
Patients living with “spouse and children” had poorer happiness experience than those living with other living styles. Most of the patients living with “spouse and children” are middle-aged and young people. They not only need to carry out complex self-management of diabetes, but also have pressure from society, the workplace, children, and so on. Psychological and economic pressure is greater than that of the solitary people, which affects their well-being. The results of this study showed that patients in the combined treatment group who had received diabetes health education had better happiness experience. It may be that combination therapy is used only when a single treatment does not achieve the goal of good blood glucose control, and combination therapy requires more detailed and professional knowledge of the disease. Standardized, structured, quality, continuous education can more effectively guide patients to fully understand the disease and improve self-management.[26] Therefore, T2DM patients should actively carry out multi-form diabetes self-management education including psychological and emotional management, carry out comprehensive prevention, and monitoring of physical and mental health care projects, such as emotional relaxation skills (such as mindfulness meditation, progressive relaxation training, breathing control, etc). In the process of management, all kinds of negative emotional experience can enhance happiness, and establish a positive and optimistic attitude towards life and reduce the distress of T2DM patients.
5. Conclusion
Patients with T2DM generally suffer from diabetes and high levels of distress were particularly common. The happiness of T2DM patients who were treated with combination therapy (oral antidiabetic drugs and insulin injection) was higher than that of monotherapy group (oral antidiabetic drugs or insulin treatment group), and the diabetes distress level of diabetic patients treated with combination was lower than that of insulin treatment group. In addition, the suffering and happiness of T2DM were also related to treatment, age, complications, blood glucose control, lifestyle, school education. We will further pay more attention to the emotion of T2DM patients to investigate different influence factors.
Acknowledgments
The authors would like to thanks all of the colleagues who helped contribute to this study.
Author contributions
Conceptualization: Shun-Ying Liu, Jin Huang, Qiao-Liang Dong, Bei Li, Xue Zhao, Rong Xu, Hong-Fang Yin.
Data curation: Shun-Ying Liu, Jin Huang, Qiao-Liang Dong, Bei Li, Xue Zhao, Rong Xu, Hong-Fang Yin.
Formal analysis: Shun-Ying Liu, Jin Huang, Qiao-Liang Dong, Bei Li, Xue Zhao, Rong Xu, Hong-Fang Yin.
Funding acquisition: Shun-Ying Liu, Jin Huang, Qiao-Liang Dong, Bei Li, Xue Zhao, Rong Xu, Hong-Fang Yin.
Investigation: Shun-Ying Liu, Jin Huang, Qiao-Liang Dong, Bei Li, Xue Zhao, Rong Xu, Hong-Fang Yin.
Methodology: Shun-Ying Liu, Jin Huang, Qiao-Liang Dong, Bei Li, Xue Zhao, Rong Xu, Hong-Fang Yin.
Project administration: Shun-Ying Liu, Jin Huang, Qiao-Liang Dong, Bei Li, Xue Zhao, Rong Xu, Hong-Fang Yin.
Resources: Shun-Ying Liu, Jin Huang, Qiao-Liang Dong, Bei Li, Xue Zhao, Rong Xu, Hong-Fang Yin.
Software: Shun-Ying Liu, Jin Huang, Qiao-Liang Dong, Bei Li, Xue Zhao, Rong Xu, Hong-Fang Yin.
Supervision: Shun-Ying Liu, Jin Huang, Qiao-Liang Dong, Bei Li, Xue Zhao, Rong Xu, Hong-Fang Yin.
Validation: Shun-Ying Liu, Jin Huang, Qiao-Liang Dong, Bei Li, Xue Zhao, Rong Xu, Hong-Fang Yin.
Visualization: Shun-Ying Liu, Jin Huang, Qiao-Liang Dong, Bei Li, Xue Zhao, Rong Xu, Hong-Fang Yin.
Writing – original draft: Shun-Ying Liu, Jin Huang, Qiao-Liang Dong, Bei Li, Xue Zhao, Rong Xu, Hong-Fang Yin.
Writing – review & editing: Shun-Ying Liu, Jin Huang, Qiao-Liang Dong, Bei Li, Xue Zhao, Rong Xu, Hong-Fang Yin.
Footnotes
Abbreviations: 2hPBG = 2-hour postprandial blood glucose, FPG = fasting plasma glucose, HbA1c = glycated hemoglobin, PAID = the problem areas in diabetes scale, T2DM = type 2 diabetes mellitus, WHO-5 = the World Health Organization 5 well-being index.
How to cite this article: Liu SY, Huang J, Dong QL, Li B, Zhao X, Xu R, Yin HF. Diabetes distress, happiness and its associated factors among type 2 diabetes mellitus patients with different therapies. Medicine. 2020;99:11(e18831).
This work was supported by Project of Chinese Nursing Association (ZHKY201416).
The authors have no conflicts of interest to disclose.
References
- [1].Huang CJ, Hsieh HM, Tu HP, et al. Major depressive disorder in patients with type 2 diabetes mellitus: prevalence and clinical characteristics. J Affect Disord 2018;227:141–8. [DOI] [PubMed] [Google Scholar]
- [2].Mathiesen AS, Egerod I, Jensen T, et al. Psychosocial interventions for reducing diabetes distress in vulnerable people with type 2 diabetes mellitus: a systematic review and meta-analysis. Diabetes Metab Syndr Obes 2018;12:19–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].Wong EM, Afshar R, Qian H, et al. Diabetes distress, depression and glycemic control in a Canadian-based specialty care setting. Can J Diabetes 2017;41:362–5. [DOI] [PubMed] [Google Scholar]
- [4].Berry E, Lockhart S, Davies M, et al. Diabetes distress: understanding the hidden struggles of living with diabetes and exploring intervention strategies. Postgrad Med J 2015;91:278–83. [DOI] [PubMed] [Google Scholar]
- [5].Medvedev ON, Landhuis CE. Exploring constructs of well-being, happiness and quality of life. PeerJ 2018;6:e4903. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Han K, Yao J, Yin X, et al. Review on the prevalence of diabetes and risk factors and situation of disease management in floating population in China. Glob Health Res Policy 2017;2:33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Hu C, Jia W. Diabetes in China: epidemiology and genetic risk factors and their clinical utility in personalized medication. Diabetes 2018;67:3–11. [DOI] [PubMed] [Google Scholar]
- [8].Ma RCW. Epidemiology of diabetes and diabetic complications in China. Diabetologia 2018;61:1249–60. [DOI] [PubMed] [Google Scholar]
- [9].Alberti KG, Zimmet PZ. Definition, diagnosis and classification of diabetes mellitus and its complications. Part 1: diagnosis and classification of diabetes mellitus. Provisional report of a WHO Consultation. Diabet Med 1998;15:539–53. [DOI] [PubMed] [Google Scholar]
- [10].de Wit M, Pouwer F, Gemke RJ, et al. Validation of the WHO-5 Well-Being Index in adolescents with type 1 diabetes. Diabetes Care 2007;30:2003–6. [DOI] [PubMed] [Google Scholar]
- [11].Forbes A, Hermanns N, Holt R, et al. Diabetes Attitudes Wishes and Needs 2 (DAWN2): a multinational, multi-stakeholder study of psychosocial issues in diabetes and person-centred diabetes care. Diabetes Res Clin Pract 2013;99:174–84. [DOI] [PubMed] [Google Scholar]
- [12].Topp CW, Østergaard SD, Søndergaard S, et al. The WHO-5 Well-Being Index: a systematic review of the literature. Psychother Psychosom 2015;84:167–76. [DOI] [PubMed] [Google Scholar]
- [13].Aljuaid MO, Almutairi AM, Assiri MA, et al. Diabetes-related distress assessment among type 2 diabetes patients. J Diabetes Res 2018;2018:7328128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Welch GW, Jacobson AM, Polonsky WH. The problem areas in diabetes scale. An evaluation of its clinical utility. Diabetes Care 1997;20:760–6. [DOI] [PubMed] [Google Scholar]
- [15].Wang W, McGreevey WP, Fu C, et al. Type 2 diabetes mellitus in China: a preventable economic burden. Am J Manag Care 2009;15:593–601. [PubMed] [Google Scholar]
- [16].American Diabetes Association. Standards of medical care in diabetes-2014. Diabetes Care 2014;37: suppl: S14–80. [DOI] [PubMed] [Google Scholar]
- [17].Fisher L, Glasgow RE, Mullan JT, et al. Development of a brief diabetes distress screening instrument. Ann Fam Med 2008;6:246–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18].Makine C, Karşidağ C, Kadioğlu P, et al. Symptoms of depression and diabetes-specific emotional distress are associated with a negative appraisal of insulin therapy in insulin-naive patients with Type 2 diabetes mellitus. A study from the European Depression in Diabetes [EDID] Research Consortium. Diabet Med 2009;26:28–33. [DOI] [PubMed] [Google Scholar]
- [19].Zhou H, Zhu J, Liu L, et al. Diabetes-related distress and its associated factors among patients with type 2 diabetes mellitus in China. Psychiatry Res 2017;252:45–50. [DOI] [PubMed] [Google Scholar]
- [20].Wardian J, Sun F. Factors associated with diabetes-related distress: implications for diabetes self-management. Soc Work Health Care 2014;53:364–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21].Baek RN, Tanenbaum ML, Gonzalez JS. Diabetes burden and diabetes distress: the buffering effect of social support. Ann Behav Med 2014;48:145–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [22].Papathanasiou A, Koutsovasilis A, Shea S, et al. The Problem Areas in Diabetes (PAID) scale: psychometric evaluation survey in a Greek sample with type 2 diabetes. J Psychiatr Ment Health Nurs 2014;21:345–53. [DOI] [PubMed] [Google Scholar]
- [23].Graue M, Haugstvedt A, Wentzel-Larsen T, et al. Diabetes-related emotional distress in adults: reliability and validity of the Norwegian versions of the Problem Areas in Diabetes Scale (PAID) and the Diabetes Distress Scale (DDS). Int J Nurs Stud 2012;49:174–82. [DOI] [PubMed] [Google Scholar]
- [24].Pintaudi B, Lucisano G, Gentile S, et al. BENCH-D Study Group. Correlates of diabetes-related distress in type 2 diabetes: findings from the benchmarking network for clinical and humanistic outcomes in diabetes (BENCH-D) study. J Psychosom Res 2015;79:348–54. [DOI] [PubMed] [Google Scholar]
- [25].Panagi L, Poole L, Hackett RA, et al. Happiness and inflammatory responses to acute stress in people with type 2 diabetes. Ann Behav Med 2018;53:309–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [26].Adam L, O’Connor C, Garcia AC. Evaluating the impact of diabetes self-management education methods on knowledge, attitudes and behaviours of adult patients with type 2 diabetes mellitus. Can J Diabetes 2018;42:470.e2–7.e2. [DOI] [PubMed] [Google Scholar]


