Supplemental Digital Content is available in the text
Keywords: chronic obstructive pulmonary disease, continuous nursing care, IKAP theory, quality of life
Abstract
Objective:
To explore the effect of continuous nursing care based on the Information, Knowledge, Attitude, and Practice (IKAP) theory on the quality of life of patients with chronic obstructive pulmonary disease (COPD).
Methods:
This study is a randomized control trial. COPD patients attending the Affiliated Hospital of Inner Mongolia Medical University, China between July 1 and October 31, 2017 were eligible. Following random assignment of participants to either the intervention group or control group, 70 patients (35 in each group) were included in the final sample. The intervention group received nursing care based on the Information, Knowledge, Attitude, and Practice theory, while the control group received standard nursing care. Data were collected before the intervention, 1 month after the intervention, and three months after the intervention. The St. George's Respiratory Questionnaire (SGRQ) was used to measure quality of life.
Results:
Three months after the intervention, there were significant differences in the total SGRQ score (20.29 ± 10.03 vs 30.14 ± 12.52) and in the three SGRQ dimensions between the intervention group and the control group (P < .05). A repeated-measures analysis of variance showed that the total SGRQ score and the scores for impact and symptoms had a significant time effect (P < .001), that the total SGRQ score and the score for symptoms had a significant interaction effect (P < .05), and that the impact dimension had a significant group effect (P = .042). Pairwise comparisons of the data for the intervention group showed that there were significant differences between the pre-intervention and 1 month after intervention scores as well as between pre-intervention and three months after intervention, for the total SGRQ scores and the scores for impact and symptoms(P < .001). In terms of the impact dimension, there was a significant difference in the intervention group between 1 month after intervention and 3 months after intervention (P = .016).
Conclusion:
Continuous nursing care based on Information, Knowledge, Attitude, and Practice theory improved quality of scores at 3 months after intervention among COPD patients. Given limitations of the study, future large-scale studies are needed to validate our results.
1. Introduction
The Global Initiative for Chronic Obstructive Lung Disease (GOLD) has defined chronic obstructive pulmonary disease (COPD) as a common preventable and treatable disease that is characterized by persistent airflow limitation that is usually progressive and is associated with an enhanced chronic inflammatory response in the airways and the lungs to noxious particles or gases. Exacerbations and comorbidities contribute to its overall severity in individual patients.[1] COPD affects a wide range of people in high, middle, and low-income countries and can cause death and disability.[2–4] COPD is therefore a major global public health problem, and can seriously affect the quality of life (QoL) of patients.[5] It is estimated that approximately 210 million people worldwide have COPD[6] and, if its trend of increasing prevalence continues, the disease will become the third leading cause of death in the world by 2030.[7] At present, COPD remains an incurable disease, and the corresponding treatment process—involving measures such as repeated hospitalization—leads to high economic costs for countries.[8–10] Hospitalization costs account for approximately 70% of COPD-related direct medical costs which, on a global scale, cumulatively exceed $US 18 billion.[11–14] Thus, implementing effective management of COPD patients is becoming increasingly important. Notably, there are a growing number of reports from around the world of methods of effectively managing COPD. For example, one study found that hospitals can promote the rehabilitation of COPD patients and reduce medical costs by providing continuous care.[15] Similarly, in the United States, Australia, and other countries,[16] transitional management models and projects have been established to meet the discharge needs of COPD patients, and some positive results have been achieved in these cases.
The Information, Knowledge, Attitude, and Practice theory (IKAP) theory is a relational theory that has been applied by many scholars since the 1960s.[17–21] The implementation of this theoretical system is mainly divided into 4 continuous processes: information collection, knowledge acquisition, attitude generation, and practice formation. There are gradual relationships among information, knowledge, attitude, and practice, and the basis of the IKAP theory is that information and knowledge are the foundations of practical change, while beliefs and attitudes are the driving forces of practical change. The IKAP theory has been applied to the nursing of patients with acute pancreatitis, essential hypertension, coronary heart disease, and bladder perfusion, and has shown good results[22–24]; however, it has seldom been used in the care of patients with COPD.
2. Methods
2.1. Ethics
This study was approved by the Ethics Committee of the Affiliated Hospital of the Inner Mongolia Medical University (approval number: 2019006). Informed written consent was obtained from each participant. Before the study, the patients were informed of the purpose of this research and were assured of their right to refuse to participate or to withdraw from the study at any stage. The anonymity and confidentiality of all participants were guaranteed.
2.2. Design
This research is randomized controlled trial. Participants were recruited from the inpatient pulmonary ward at Affiliated Hospital of Inner Mongolia Medical University, which is in the Inner Mongolia Autonomous Region of China. All 70 patients were diagnosed with COPD according to the criteria of GOLD.[25] Six researchers were involved in the project; of these, 4 were Registered Nurses, and held a bachelor's degree and had at least three years’ experience in clinical care. Registered Nurses were IKAP nurses (ie, nurses who have received group training in the form of lectures, including how to standardize the intervention and supporting patients through using standardized tools based on the IKAP theory. Such nurses also receive training related to diseases, smoking-cessation counseling, medication management, etc). These nurses administered the intervention. The remaining 2 researchers were master's candidates and were responsible for data collection and analysis.
Participants were divided into 2 groups: a control group, which received routine care, and an intervention group, which received continuous care based on IKAP theory in addition to routine care. The participants were administered paper-based questionnaires, which they completed within 20 minutes. Data were collected and analyzed at baseline and at 1 and 3 months thereafter.
2.3. Participants and randomization
Overall, among the original 76 recruited patients, 3 did not meet the inclusion criteria, 1 refused to participate, 1 participant in the control group passed away during the study, and 1 participant in the intervention group was lost to follow-up. Of the original 76 participants, 35 patients in each group were included in the final analysis.
A random number table was used for sampling and assigning participants to the groups, which was conducted by a professional statistician. The allocation sequence was stored in numbered, opaque, sealed envelopes. Once group allocation was completed, the IKAP nurses received a copy of the participants’ ID numbers and allocations. Participants and the master's candidates were blinded to group allocation. To maintain observer blinding throughout the study period, participants were requested not to discuss the intervention with the master's candidates. IKAP nurses and master's candidates were trained separately on how to control bias. There was no communication between the IKAP nurses and the master's candidates, because the former are registered nurses and the latter are students (they are in 2 institutions).
The inclusion criteria were as follows:
-
(1)
Satisfying the spirometry criteria for GOLD severity class 1, 2, 3, or 4.[25]
-
(2)
The GOLD 2017 diagnostic criteria for COPD was applied:
Symptoms such as dyspnea, chronic cough, or expectoration;
a history of exposure to host factors (genetic factors, congenital developmental abnormalities, etc), tobacco, indoor/outdoor pollution, biofuels, occupational pollution, and other risk factors;
incompletely reversible air flow obstruction, defined as a forced expiratory volume in the first second (FEV1)/forced vital capacity (FVC) ratio of below 70 after bronchodilation.
-
(3)
Capable of communicating in Chinese.
-
(4)
Willing to voluntarily participate in this study.
-
(5)
Cognitively capable of completing questionnaires and participating in interviews.
-
(6)
Having access to a smart mobile phone.
-
(7)
Living in the Hohhot area, so that subsequent follow ups would be possible.
The exclusion criteria were:
-
(1)
Having an unstable medical condition such as recent myocardial infarction, congestive cardiac failure, cor pulmonale in the decompensatory stage, active malignancy, or acute cerebrovascular accidents.
-
(2)
Having bronchiectasis, bronchial asthma, or similar diseases.
-
(3)
An inability to adequately communicate due to language barriers or cognitive disorders.
-
(4)
Having severe limb dysfunction.
-
(5)
Unwilling to provide informed consent to participate in the study.
The sample size was calculated by considering the effect value of improving the health status of COPD patients, which was δ/σ = 0.74[26] (determined by consulting existing literature regarding long-term health education of COPD patients). Based on one-sided α = 0.05, β = 0.1, and taking a 10% attrition rate into consideration, the total sample size was determined to be 35 patients in each group. The sample size was calculated using the following formula for 2 sample comparisons:
 |
2.4. Implementation of the study
2.4.1. Control group
Patients in the control group were provided with routine care, which included a COPD education session every 2 weeks (20–30 minutes each). This included topics such as guidance regarding the discharge process, information regarding factors that influence the disease and induce acute attacks, home oxygen therapy, lung rehabilitation, and telephone follow-ups.
2.4.2. Intervention group
Details are shown in the Supplementary Table. The intervention group received 20 to 30 minutes of IKAP-theory-based continuous nursing every 2 weeks along with the routine nursing care. (Information collection takes 10–15 minutes, Knowledge acquisition takes 10–15 minutes, and changes in patients’ attitudes generation and practice formation were assessed after intervention.) In accordance with the IKAP theory, the tenets of the nursing intervention mainly included:
Information collection: This involved nurses identifying information sought by the patients. The nurses also collected information regarding the patients’ health status and psychological status. Further, the nurses also answered patients’ questions, encouraged and comforted patients and their families, and sought to establish a healthy psychological and social environment.
Knowledge acquisition: This stage involved providing healthcare-related knowledge to the patients. Other topics included attempting to modify patients’ unhealthy lifestyles or habits, clarifying the significance of respiratory function exercises, and giving demonstrations of such exercises.
Attitude generation: In this stage, nurses aimed to encourage the patients to develop a positive attitude concerning the importance of their health. The nursing staff also continued to consolidate the content of the health education provided before discharge through telephone follow-ups, e-mails, WeChat (WeChat is a popular messaging application, with over a billion users monthly) and QQ (Tencent QQ is another popular messaging service). The nursing staff continuously assessed patients’ knowledge and daily behavior to track and collect behavioral change data, identified key factors that hinder changes in patients’ behaviors, and implemented targeted guidance measures designed to encourage patients to believe that their treatment is beneficial and to make plans for long-term treatment.
Practice formation: In the final stage, the nurses encouraged the patients to develop habits to maintain and restore their health. The IKAP nursing team discussed a nursing plan with each patient and then implemented it. This involved the application of targeted individual intervention measures for patients, helping patients develop an appropriate understanding of their disease, providing adequate ideological preparation, ensuring patients had the ability to consciously implement their health-education plan, performing periodic reviews, helping patients maintain a good mental outlook, and promoting a change towards healthy behavior, thereby improving the patients’ health.
2.5. Outcome measurements
The outcome measure for this study was the St. George's Respiratory Questionnaire (SGRQ).[27] This questionnaire contains 70 items, grouped into 3 dimensions[28]: symptoms,[29] activity (measuring negative effects on or limitations to activities of daily living), and impact (lifestyle, changes at the social and psychological levels).[30] A total score (0–100) is obtained from the sum of the 3 categories, with higher scores indicating lower QoL. The validity and reliability of the scale were reported by Tao Liu,[31] who translated SGRQ into Chinese, and demonstrated its suitability for the Chinese culture and society.[32]
2.6. Statistical analysis
Data were analyzed using SPSS 19.0 (SPSS Inc., IL). The general data between the 2 groups were tested using a chi-squared test and t tests. The Shapiro-Wilk test and a Q-Q plot were used to test the normal distribution of the SGRQ total score and impact score. The results of the Shapiro-Wilk test showed that P > .05 and that the degree of coincidence among the data points and theoretical straight lines in the Q-Q graph was high. The above data follow a normal distribution and can be described by (x̄ ± s). Therefore, t tests, a repeated measure analysis of variance (ANOVA), and pairwise comparisons could be used for statistical analysis. For the Shapiro-Wilk test of the symptom and activity scores P < .05, and the degree of coincidence among the data points and theoretical straight lines in the Q-Q chart was low. This indicated that the data did not follow a normal distribution pattern. Therefore, median and quartile spacing were used to describe the data in this study. Meanwhile, the Mann–Whitney U test, a repeated-measures ANOVA, and pairwise comparisons were used for statistical analysis.
3. Results
3.1. Participants’ characteristics
Table 1 shows the baseline characteristics of the 2 groups. No significant difference was observed between the 2 groups in terms of the GOLD grade. Further, the analyses did not reveal any significant differences between the two groups regarding pulmonary function variables, such as Forced Vital Capacity Predicted, Forced Expiratory Volume in the First Second Predicted, and FEV1/FVC ratio. There were also no statistically significant differences between the 2 groups regarding medication, such as Long-Acting Beta Agonist, Long-Acting Muscarinic Antagonist, inhaled steroids, systemic steroids, and antibiotics. Finally, no significant differences were observed between the 2 groups regarding their baseline demographic characteristics, including gender, age, education, marital status, family caregivers, smoking years, home oxygen therapy, and regular medication (P > .05).
Table 1.
Characteristics of the participants of intervention vs control group.

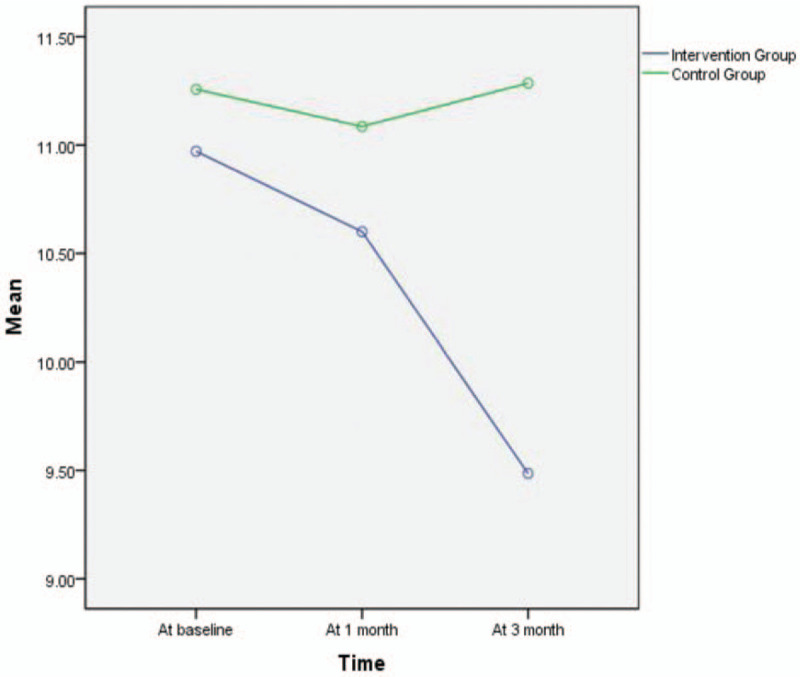
3.2. Results of statistical analysis of total SGRQ score
The specifics of these results are provided in Table 2 and in Figure 1. The data for the total SGRQ score were normally distributed and were tested using 2 independent samples t tests. The results showed that 3 months after the intervention, there were significant differences in the total SGRQ score between the intervention group and the control group (20.29 ± 10.03 vs 30.14 ± 12.52; P = .001). The repeated-measures ANOVA showed a Time effect (P < .001), the differences in SGRQ scores at each time point were statistically significant. The group effect (P = .055) indicated that there was no statistical difference between the intervention group and the control group. A significant interaction effect (P = .010) showed that time and grouping had an interaction, and the effects of time factors (before intervention, 1 month after intervention, and 3 months after intervention) varied by group (intervention group and control group).
Table 2.
Comparison of patients in the 2 groups before intervention, 1 month after intervention and 3 months after intervention.

Figure 1.
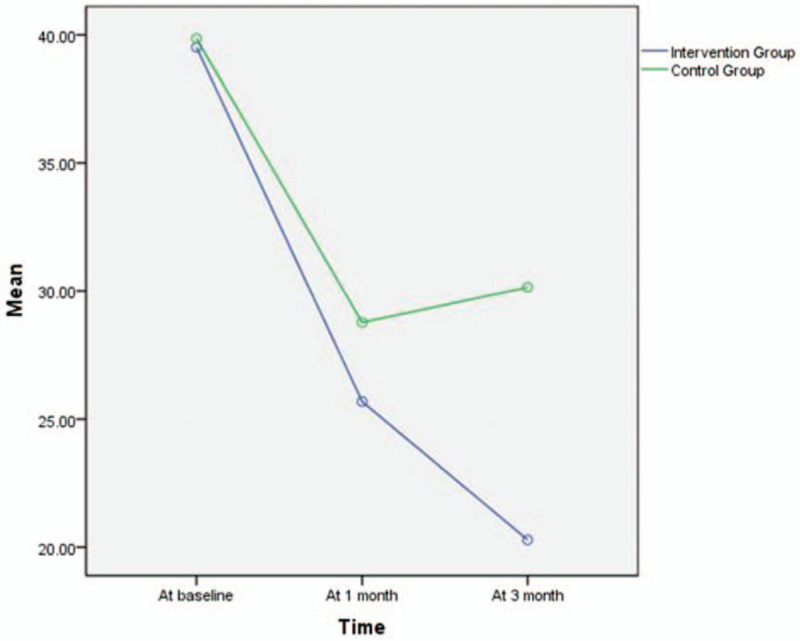
Comparison of the 2 groups on SGRQ total scores at 3 time points. The graph of the comparison of the 2 groups on SGRQ total scores at 3 time points was illustrated according to time as abscissa and the total scores mean as ordinate. The green line is the control group and the blue line is the intervention group.
Details are shown in Table 3, pairwise comparisons across time for the intervention group showed that there was a significant difference in the total SGRQ score between pre-intervention and 1 month after intervention (difference,12.457 [95%CI,10.429–14.485]; P < .001) and between pre-intervention and 3 months after intervention (difference,14.471[95%CI,11.281–17.662]; P < .001).
Table 3.
Pairwise comparison of SGRQ total mean in the intervention group.

3.3. Results of statistical analyses of the impact scores
The specifics of these results are provided in Table 2 and in Figure 2. The data for the impact scores followed a normal distribution and were tested using 2 independent samples t tests. The results indicated that there was a significant difference in the impact score between the intervention group and the control group 3 months after the intervention (7.09 ± 4.65 vs 11.00 ± 6.03; P = .003). The repeated-measures ANOVA showed a main effect for time (P < .001): The difference in data at each time point was statistically significant. A significant group effect (P = .042) indicated that there was a statistical difference between the intervention group and the control group. The interaction effect (P = .059): showed that time and grouping had not interactions, the effects of time factors did not vary with grouping.
Figure 2.
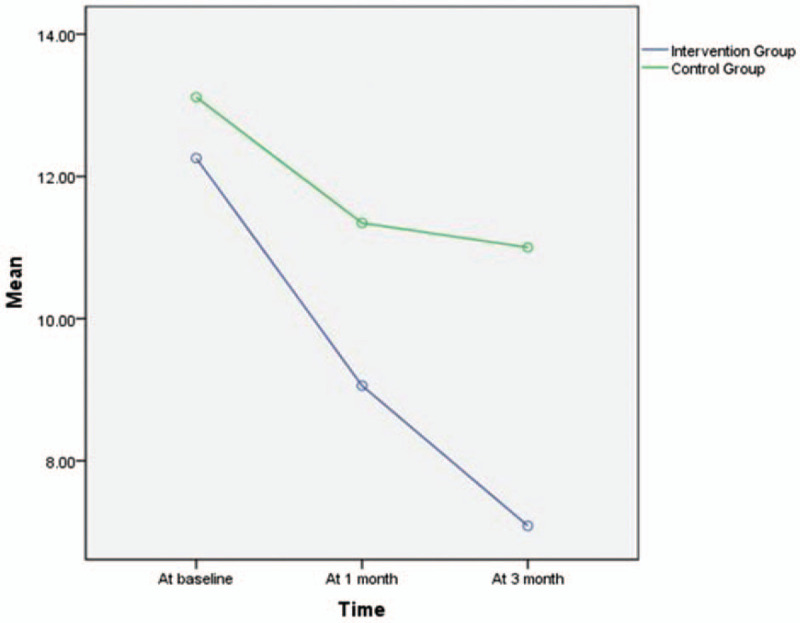
Comparison of the 2 groups of Impact scores at 3 time points. The graph of the comparison of the 2 groups on Impact scores at 3 time points was illustrated according to time as abscissa and the Impact scores mean as ordinate. The green line is the control group and the blue line is the intervention group.
Details are shown in Table 4, pairwise comparisons of the intervention group showed that all three time points significantly differed regarding the dimension of impact: between pre-intervention and one month after intervention (difference, 2.486 [95%CI, 1.765–3.207]; P < .001), between pre-intervention and 3 months after intervention (difference, 3.643 [95%CI, 2.374–4.912]; P < .001), and between 1 month after intervention and 3 months after intervention (difference, 1.157 [95%CI, 0.220–2.095]; P = .016).
Table 4.
Pairwise comparison of Impact scores means in the intervention group.

3.4. Results of statistical analyses of the symptom scores
The specifics of these results are shown in Table 2 and in Figure 3. When data did not follow a normal distribution pattern, the Mann–Whitney U test was applied. The results showed that, for the patients’ symptom scores, at three months after the intervention there was a statistically significant difference between the intervention group and the control group [1.00 (0,5) vs 5.00 (3,9); P < .001]. The repeated-measures ANOVA showed a significant difference between the 2 groups regarding the time effect (P < .001). Regarding the group effect (P = .171), findings indicated that there was no significant difference between the intervention group and the control group. The interaction effect between the intervention group and the control group was statistically significant (P = .018), this result shows that the role of the time effect factors changes with the different groups.
Figure 3.
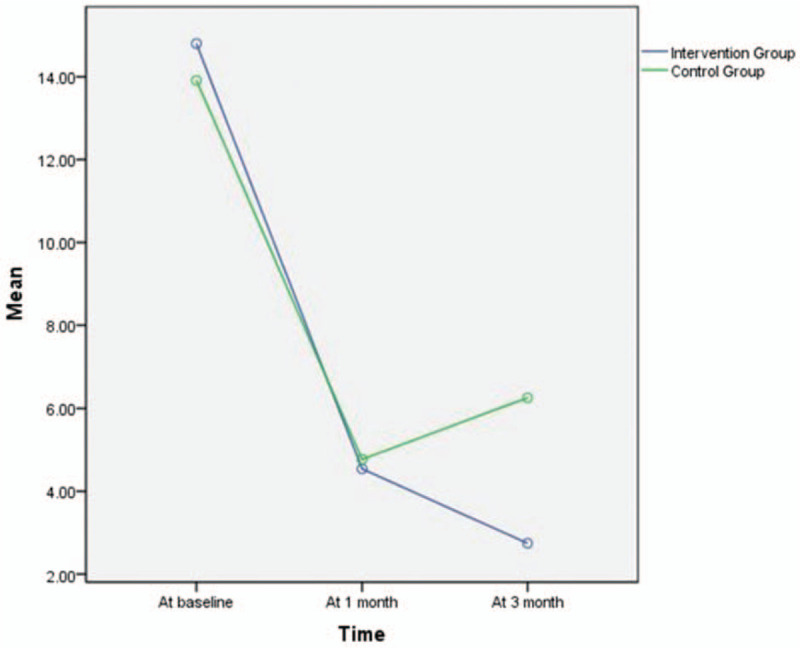
The comparison of the 2 groups of Symptom scores at 3 time points. The graph of the comparison of the 2 groups of Symptom scores at 3 time points was illustrated according to time as abscissa and the Symptom scores mean as ordinate. The green line is the control group and the blue line is the intervention group.
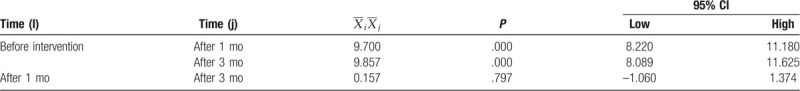
Details are shown in Table 5, pairwise comparisons of the intervention group showed that there was a significant difference in the dimension of symptoms between pre-intervention and 1 month after intervention (difference, 9.700 [95%CI, 8.220–11.180]; P < .001) and between pre-intervention and 3 months after intervention (difference, 9.857 [95%CI,8.089–11.625]; P < .001).
Table 5.
Pairwise comparison of Symptom scores means in the intervention group.
3.5. Results of statistical analyses of activity scores
The specific results in this regard are shown in Table 2 and in Figure 4. A comparison of the data on the activity scores showed that the trend of the data distribution did not follow normal distribution patterns. Therefore, the Mann–Whitney U test was used to analyze the data. The results showed that there was a statistically significant difference in the activity score between the intervention group and the control group at 3 months after the intervention [11.00 (8,11) vs 12.00 (9,14); P = .010]. Statistical analysis of the time effect and grouping effect of all data showed that P > .05, meaning there was no significant difference. Similarly, there was no statistically significant difference for the interaction effect (P = .088). These results show that the effect of the time factor did not vary between the groups.
Figure 4.
Comparison of the 2 groups of Activity scores at 3 time points. The graph of the comparison of the 2 groups of Activity scores at 3 time points was illustrated according to time as abscissa and the Activity scores mean as ordinate. The green line is the control group and the blue line is the intervention group.
Details are shown in Table 6, the time point of the intervention was used as a factor for comparing the activity ability of the patients in the intervention group. The results of the comparative analysis showed that there was no significant difference in activity ability pre-intervention, at 1 month after intervention, or at three months after intervention (P > .05).
Table 6.
Pairwise comparison of activity scores means in the intervention group.

4. Discussion
Mood disorders, lower levels of exercise tolerance, and dyspnea have previously been shown to affect the QoL and health status of COPD patients.[33] The IKAP theory can be beneficial with regard to all of these issues. The implementation of the IKAP theoretical system is mainly divided into four continuous processes: information collection, knowledge acquisition, attitude generation, and practice formation that encourage patients to consciously adhere to health-education programs and promote changes in their health behaviors.
4.1. Effectiveness of the total SGRQ scores
This study showed that continuous nursing based on the IKAP theory can improve the QoL of patients with COPD. Several previous studies have reported the benefits of education programs regarding the improvement of the QoL of patients with COPD [34–45]; however, some other studies found that there are no significant improvements after implementing education programs for COPD patients.[46–51]The implementation of education interventions can be influenced by differences among individual patients, which may be the cause of previous inconsistent results. Furthermore, the QoL of patients with severe or extremely severe COPD is relatively low.[52] Therefore, differences in lung function between patients may also account for the different outcomes. Future studies should explore the implementation of interventions for patients with differing levels of lung function.
4.2. Effect of IKAP-based continuous care on the different dimensions of QoL
The results showed that for patients with COPD, continuous care based on the IKAP theory had a positive impact on each dimension of QoL. Wakabayashi et al[53] reported results similar to our findings. However, other existing studies have found the opposite.[47,50] In this study, dimensions of symptoms and impact have been reported to benefit from education programs. The findings of Soler et al and other studies [35,40,42,53] are consistent with the results of this study. This research shows that the implementation of health education does not improve the activity ability of COPD patients. In contrast, the studies of Lan et al,[54] Jácome and Marques,[55] Chen et al,[56] and Zhou et al[57] reported that health education can improve the activity ability of patients. This discrepancy may be explained by the fact that the health conditions of the patients differed in these studies. For example, the Jácome and Marques study mainly studied patients with mild COPD.
5. Conclusion
The innovations of this study can be summarized as the application of IKAP theory to the continuous nursing care of COPD patients. The research team consequently developed a continuous, comprehensive, and planned nursing intervention that could help patients obtain knowledge regarding the etiology, symptoms, and treatment of their condition in a comprehensive and real-time manner. This intervention strengthens patients’ attitude and confidence regarding their ability to adhere to healthy behaviors and can lead to the emergence of behaviors that are conducive to rehabilitation. This study showed that IKAP-theory-based continuous nursing interventions have a significantly positive effect on the QoL of COPD patients.
5.1. Research limitations and future research ideas
This study has several limitations. First, the number of hospitalizations and emergency visits and readmission rates of COPD patients may be important sensitive indicators for monitoring; this should be considered in future research. Second, although this was a representative sample of COPD patients, sampling errors may exist due to the relatively small sample size. Third, the study was conducted in only one hospital, meaning that certain categories of patients may have been missed. Efforts were made during the questionnaire survey to minimize the possibility of observer bias. For example, data entry and analysis were not conducted by the IKAP nurse to prevent the nurse from speculating about the results of the study.
5.2. Relevance to clinical practice
The main contribution of this study is that continuous nursing intervention based on the IKAP theory was applied to patients with COPD, which has seldom been done in previous studies. COPD patients constitute a major portion of the population in need of nursing and support from health-care systems. Continuous care based on the IKAP theory was found to have a positive effect on patient's QoL. This continuous care intervention can help patients with COPD take a more active role in self-management by developing self-regulation skills.
Acknowledgments
We are grateful to our participants. We would like to thank Editage (www.editage.com) for English language editing.
Author contributions
Data curation: Wennv Hao.
Formal analysis: Xuewei Du, Wennv Hao.
Funding acquisition: Xinxia Li.
Investigation: Xinxia Li.
Methodology: Wennv Hao.
Project administration: Xinxia Li.
Resources: Xinxia Li, Wen Song, Chang Lu.
Software: Wen Song, Chang Lu.
Supervision: Xinxia Li, Wennv Hao.
Validation: Xuewei Du, Wennv Hao.
Visualization: Xuewei Du.
Writing – original draft: Wennv Hao.
Writing – review & editing: Xuewei Du, Wennv Hao.
Supplementary Material
Footnotes
Abbreviations: ANOVA = analysis of variance, COPD = Chronic Obstructive Pulmonary Disease, GOLD = Global Initiative for Chronic Obstructive Lung Disease, IKAP theory = Information, Knowledge, Attitude, and Practice theory, QoL = quality of life, SGRQ = St. George's Respiratory Questionnaire.
How to cite this article: Li XX, Du XW, Song W, Lu C, Hao WN. Effect of continuous nursing care based on the IKAP theory on the quality of life of patients with chronic obstructive pulmonary disease: a randomized controlled study. Medicine. 2020;99:11(e19543).
XXL and XWD contributed equally to this work and are co-first authors.
Funding for this study was provided by the Inner Mongolia Medical University Science and Technology Million Project, Inner Mongolia, China (YKD2015KJBW021).
The authors report no conflicts of interest.
Trial registry: Chinese Clinical Trial Registry (No. ChiCTR1900024383).
Supplemental Digital Content is available for this article.
References
- [1]. Global initiative for chronic obstructive lung disease: Global strategy for the diagnosis, management and prevention of chronic obstructive pulmonary disease updated; 2015:2. [Google Scholar]
- [2].Pauwels RA, Rabe KF. Burden and clinical features of chronic obstructive pulmonary disease (COPD). Lancet 2004;364:613–20. [DOI] [PubMed] [Google Scholar]
- [3].Hillas G, Perlikos F, Tsiligianni I, et al. Managing comorbidities in COPD. Int J Chron Obstruct Pulmon Dis 2015;10:95–109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Gershon AS, Warner L, Cascagnette P, et al. Lifetime risk of developing chronic obstructive pulmonary disease: a longitudinal population study. Lancet 2011;378:991–6. [DOI] [PubMed] [Google Scholar]
- [5].Sunde S, Walstad RA, Bentsen SB, et al. The development of an integrated care model for patients with severe or very severe chronic obstructive pulmonary disease (COPD): the COPD-Home model. Scand J Caring Sci 2013;28:469–77. [DOI] [PubMed] [Google Scholar]
- [6].2009;Franchi M. EFA Book on Chronic Obstructive Pulmonary Disease in Europe: Sharing and Caring Brussels: European Federation of Allergy and Airways Disease. [Google Scholar]
- [7]. World Health Organization. World health statistics 2008. Geneva: World Health Organization; 2008. Available at: https://www.who.int/whosis/whostat/EN_WHS08_Full.pdf?ua=1. (Accessed on April, 2017). [Google Scholar]
- [8].Asia Pacific COPD Roundtable Group. Global initiative for chronic obstructive lung disease strategy for the diagnosis, management and prevention of chronic obstructive pulmonary disease: an Asia-Pacific perspective. Respirology 2005;10:9–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Guarascio AJ, Ray SM, Finch CK, et al. The clinical and economic burden of chronic obstructive pulmonary disease in the USA. Clinicoecon Outcomes Res 2013;5:235–45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10]. Global Initiative for Chronic Obstructive Lung Disease (GOLD). (2013). 2013 reports, global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease (updated 2013). [Cited12Mar2013.]. Available at: http://www.goldcopd.org/uploads/users/files/GOLD_Report_2013_Feb20.pdf. (Accessed on April, 2017). [Google Scholar]
- [11].Seemungal TA, Donaldson GC, Paul EA, et al. Effect of exacerbation on quality of life in patients with chronic obstructive pulmonary disease. Am J Respir Crit Care Med 1998;157:1418–22. [DOI] [PubMed] [Google Scholar]
- [12].Garcia-Aymerich J, Monsó E, Marrades RM, et al. Risk factors for hospitalization for a chronic obstructive pulmonary disease exacerbation: EFRAM study. Am J Respir Crit Care Med 2001;164:1002–7. [DOI] [PubMed] [Google Scholar]
- [13].Hurst JR, Wedzicha JA. Chronic obstructive pulmonary disease: the clinical management of an acute exacerbation. Postgrad Med J 2004;80:497–505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Chenna PR, Mannino DM. Outcomes of severe COPD exacerbations requiring hospitalization. Semin Respir Crit Care Med 2010;31:286–94. [DOI] [PubMed] [Google Scholar]
- [15].Morrison J, Palumbo MV, Rambur B. Reducing preventable hospitalizations with two models of transitional care. J Nurs Scholarsh 2016;48:322–9. [DOI] [PubMed] [Google Scholar]
- [16].Pearson M, Hunt H, Cooper C, et al. Providing effective and preferred care closer to home: a realist review of intermediate care. Health Soc Care Community 2015;23:577–93. [DOI] [PubMed] [Google Scholar]
- [17].2016;Wang X. Study on the effect of IKAP theory continuous nursing mode applied to patients with bladder perfusion Xinxiang medical college. [Google Scholar]
- [18].Cheng X. Application of IKAP theory in health education of patients with acute. J Qi Lu Nurs 2007;(7):19–20. [Google Scholar]
- [19].Liu J, Liu X, Wu Y. IKAP theory in patients with coronary heart disease health education application. China Foreign Med 2007;(3):47–8. [Google Scholar]
- [20].Jiang H. The use of IKAP theory for pregnant women with gestational diabetes health education effect analysis. Jiangsu Health Care 2011;13:41–2. [Google Scholar]
- [21].Liu J, Zhang Q, Yan T. IKAP theory in patients with coronary heart disease health education application. China Foreign Med 2008;14:84–5. [Google Scholar]
- [22].Wu H, Fu X, Wang D, et al. Application of IKAP management model in elderly patients with hypertension. Chin J Gerontol 2019;39:1458–60. [Google Scholar]
- [23].Fu H, Song D, Wang D. The clinical effect of IKAP continuous nursing mode on bladder perfusion chemotherapy. J Nurses Train 2019;234:1005–8. [Google Scholar]
- [24].Li GG. Effects of IKAP health education on self-efficacy and quality of life in patients with acute pancreatitis. Int Med 2016;11:489–91. [Google Scholar]
- [25].Vogelmeier CF, Criner GJ, Martinez FJ, et al. Global strategy for the diagnosis, management, and prevention of chronic obstructive lung disease 2017 report. GOLD executive summary. Am J Respir Crit Care Med 2017;195:557–82. [DOI] [PubMed] [Google Scholar]
- [26]. Zhang Xr. Design and Application of Transitional Care Model Based on Omaha System in Elderly Malnourished Patients with Chronic Diseases. College of nursing, Southern Medical University, 2014. [Google Scholar]
- [27].Moezy A, Erfani A, Mazaherinezhad A, et al. Downhill walking influence on physical condition and quality of life in patients with COPD: a randomized controlled trial. Med J Islam Repub Iran 2018;32:49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [28].Vestbo J, Hurd SS, Agustí AG, et al. Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease: GOLD executive summary. Am J Respir Crit Care Med 2013;187:347–65. [DOI] [PubMed] [Google Scholar]
- [29].Soriano JB, Miravitlles M. Epidemiological data of COPD in Spain (in Spanish). Archivos de Bronconeumología 2007;43(Sup 1):2–9. [Google Scholar]
- [30].Schols AMWJ, Soeters PB, Dingemans AMC, et al. Prevalence and characteristics of nutritional depletion in patients with stable COPD eligible for pulmonary rehabilitation. Am Rev Respir Dis 1993;147:1151–6. [DOI] [PubMed] [Google Scholar]
- [31]. Liu T. Comprehensive study on pathogenesis and quality of life of chronic obstructive pulmonary disease. Union Medical College of China, 2004. [Google Scholar]
- [32].Liu H, Zhao A, Li X. Study on the continuous nursing effect of chronic obstructive pulmonary disease. Chin Gen Med 2013;16:867–9. [Google Scholar]
- [33].Lamers F, Jonkers CC, Bosma H, et al. Improving quality of life in depressed COPD patients: effectiveness of a minimal psychological intervention. COPD 2010;7:315–22. [DOI] [PubMed] [Google Scholar]
- [34].Ding M, Su Q, Yang P-R. Effect of continuous nursing intervention on the quality of life of COPD patients. Qilu Nurs J 2014;20:17–9. [Google Scholar]
- [35].Soler JJ, Martínez-García MÁ, Román P, et al. Effectiveness of a specific program for patients with chronic obstructive pulmonary disease and frequent exacerbations. Archivos de Bronconeumología (English edition) 2006;42:501–8. [DOI] [PubMed] [Google Scholar]
- [36].Khdour MR, Agus AM, Kidney JC, et al. Cost-utility analysis of a pharmacy-led self-management programme for patients with COPD. Int J Clin Pharm 2011;33:665–73. [DOI] [PubMed] [Google Scholar]
- [37].Wedzicha JA, Brill SE, Allinson JP, et al. Mechanisms and impact of the frequent exacerbator phenotype in chronic obstructive pulmonary disease. BMC Med 2013;11:181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [38].Koff P, Jones RH, Cashman JM, et al. Proactive integrated care improves quality of life in patients with COPD. Eur Respir J 2009;33:1031–8. [DOI] [PubMed] [Google Scholar]
- [39].Hoogendoorn M, van Wetering CR, Schols AM. Rutten-van Mölken MPMH. Is INTER disciplinary community-based COPD management (INTERCOM) cost-effective? Eur Respir J 2010;35:79–87. [DOI] [PubMed] [Google Scholar]
- [40].Bourbeau J, Collet J-P, Schwartzman K, et al. Economic benefits of self-management education in COPD. Chest 2006;130:1704–11. [DOI] [PubMed] [Google Scholar]
- [41].Taylor SJC, Sohanpal R, Bremner SA, et al. Self-management support for moderate-to-severe chronic obstructive pulmonary disease: a pilot randomized controlled trial. Br J Gen Pract 2012;62:e687–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [42].Efraimsson EÖ, Hillervik C, Ehrenberg AJ. Effects of COPD self-care management education at a nurse-led primary health care clinic. Scand J Caring Sci 2008;22:178–85. [DOI] [PubMed] [Google Scholar]
- [43].Chavannes NH, Grijsen M, van den Akker M, et al. Integrated disease management improves one-year quality of life in primary care COPD patients: a controlled clinical trial. Prim Care Respir J 2009;18:171–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [44].Billington J, Coster S, Murrells T, et al. Evaluation of a nurse-led educational telephone intervention to support self-management of patients with chronic obstructive pulmonary disease: a randomized feasibility study. COPD 2015;12:395–403. [DOI] [PubMed] [Google Scholar]
- [45].Rice KL, Dewan N, Bloomfield HE, et al. Disease management program for chronic obstructive pulmonary disease: a randomized controlled trial. Am J Respir Crit Care Med 2010;182:890–6. [DOI] [PubMed] [Google Scholar]
- [46].Coultas D, Frederick J, Barnett B, et al. A randomized trial of two types of nurse-assisted home care for patients with COPD. Chest 2005;128:2017–24. [DOI] [PubMed] [Google Scholar]
- [47].Theander K, Jakobsson P, Jörgensen N, et al. Effects of pulmonary rehabilitation on fatigue, functional status and health perceptions in patients with chronic obstructive pulmonary disease: a randomized controlled trial. Clin Rehabil 2009;23:125–36. [DOI] [PubMed] [Google Scholar]
- [48].Monninkhofe E, Van der valk P, Schermer T, et al. Economic evaluation of a comprehensive self-management programme in patients with moderate to severe chronic obstructive pulmonary disease. Chron Respir Dis 2004;1:7–16. [DOI] [PubMed] [Google Scholar]
- [49].Watson PB, Town GI, Holbrook N, et al. Evaluation of a self-management plan for chronic obstructive pulmonary disease. Eur Respir J 1997;10:1267–71. [DOI] [PubMed] [Google Scholar]
- [50].Hesselink AE, Penninx BWJH, van der Windt DAWM, et al. Effectiveness of an education programme by a general practice assistant for asthma and COPD patients: results from a randomized controlled trial. Patient Educ Couns 2004;55:121–8. [DOI] [PubMed] [Google Scholar]
- [51].Monteagudo M, Rodriguez-Blanco T, Llagostera M, et al. Effect of health professional education on outcomes of chronic obstructive pulmonary disease in primary care: a non-randomized clinical trial. Respirology 2013;18:718–27. [DOI] [PubMed] [Google Scholar]
- [52].Kangovi S, Mitra N, Grande D, et al. Patient-centered community health worker intervention to improve posthospital outcomes: a randomized clinical trial. JAMA Intern Med 2014;174:535–43. [DOI] [PubMed] [Google Scholar]
- [53].Wakabayashi R, Motegi T, Yamada K, et al. Efficient integrated education for older patients with chronic obstructive pulmonary disease using the Lung Information Needs Questionnaire. Geriatr Gerontol Int 2011;11:422–30. [DOI] [PubMed] [Google Scholar]
- [54].Lan C-C, Huang H-C, Yang M-C, et al. Pulmonary rehabilitation improves subjective sleep quality in COPD. Respir Care 2014;59:1569–76. [DOI] [PubMed] [Google Scholar]
- [55].Jácome C, Marques A. Impact of pulmonary rehabilitation in subjects with mild COPD. Respir Care 2014;59:1577–82. [DOI] [PubMed] [Google Scholar]
- [56].Chen L, Chen X, Lu Q. Effects of health care cooperative health education combined behavioral intervention on COPD patients. Electron J Clin Med Lit 2017;4:11434–5. [Google Scholar]
- [57].Zhou A, Yuan W. Application of health education model of knowledge, faith and action in COPD patients with stable period. Qilu Nurs J 2013;19:15–7. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


