Abstract
Discoid lateral meniscus is one of the most common knee problems in clinical practice. Several radiographic findings have been reported to screen discoid lateral meniscus, but the diagnostic value of those signs varies.
We introduce a new method of measurement on plain radiograph for initial screening discoid lateral meniscus and describe its efficacy and correlation to symptomatic discoid lateral meniscus.
This is a retrospective case-control study.
Seventy-eight arthroscopic proven symptomatic discoid lateral meniscus adult patients plus 73 patients of matched control group were retrospectively reviewed at our institution between 2012 and 2017. We studied their standardized non-weight-bearing knee radiograph anterior-posterior view and measured the following parameters: lateral joint space height, lateral tibia spine height, fibular head height, lateral tibia plateau obliquity (LTPO), and lateral condyle convex angle (LCCA).
Significant statistical differences were found in the lateral joint space height, lateral tibia spine height, fibular head height, LTPO and LCCA measurements between the 2 groups (P < .05). Also, we found the phenomenon that angle parameters such as LTPO and LCCA had high sensitivities with relatively low specificities compared with height parameters.
We propose that LCCA is a new measurement which is statistically larger in discoid meniscus patients. Furthermore, it can be useful for screening discoid lateral meniscus on plain radiograph with its relative high sensitivity.
Level of Evidence: Level III, Case-control study.
Keywords: adult, discoid lateral meniscus, knee radiograph measurement
1. Introduction
Discoid meniscus is a common variation of lateral meniscus. In Asian population, the incidence is especially high in literature, ranging from 17% to 33.2%.[1,2] Discoid lateral meniscus is known as one of the most common knee problems in clinical practice. It can cause several symptoms such as pain, clicking, and extension limitation, which is of clinical importance to deal with. Both arthroscopy examination and magnetic resonance imaging (MRI) are the 2 definitive diagnostic tools. Arthroscopy is often associated with several surgical risks, so it is not the first choice to make the diagnosis. MRI is a noninvasive technique, but it also has several disadvantages. First, it is relatively expensive and inconvenient. Second, it has contraindications for patients with magnetic metallic implants or claustrophobia.
Although several radiographic findings have been reported, such as lateral joint space widening, squaring of the lateral femoral condyle, high fibula head,[3–6] some authors believe that plain radiography has little value in the detection of a discoid lateral meniscus.[7,8] The diagnostic value of current signs is still questionable. For example, some authors[3,4] reported that height of the lateral tibia spine in discoid lateral meniscus group is lower than normal control group while other authors[6] reported complete opposite results. Therefore, we analyzed and compared several radiographic signs, including lateral joint space height (LJSH), lateral tibia spine height (LTSH), fibular head height (FHH), and lateral tibia plateau obliquity (LTPO), of adult symptomatic discoid lateral meniscus with matched controls to determine whether the diagnosis of discoid lateral meniscus on radiograph is possible and reliable.
Since lateral discoid meniscus is generally considered as developmental problem since childhood,[9] we hypothesis that it can also affect the development of lateral condyle which may lead to more flat appearance. Thus, we also developed 1 sign of our own which to our knowledge has not been reported before. We name it lateral condyle convex angle (LCCA) (Fig. 1).
Figure 1.

The radiographic assessments on anterorposterior view. First of all, the imaginary tibia joint line (red line) was established as a baseline, which was approximately defined as from the most medial edge of the tibial plateau to the most lateral edge of the plateau, as it is demonstrated in the Figure 1. The main parameters are listed as below: (A) LJSH is the distance from the lowest point of lateral condyle to the imaginary tibia joint line. (B) LTSH is the distance from the tip of the lateral tibia spine to the imaginary tibia joint line. (C) FHH is the distance from the tip of the fibular head to the imaginary tibia joint line. (D) Width of the distal femur at the level of interepicondylar line. α LTPO is the angle formed by imaginary tibia joint line and articular line of the lateral tibia plateau. β LCCA is the angle formed by the imaginary line through the lowest point of the lateral condylar and the highest point of inter-condylar fossa and the imaginary line through the lowest point of the lateral condylar and the most lateral point of the lateral femoral articular surface. FHH = fibular head height, LCCA = lateral condyle convex angle, LJSH = lateral joint space height, LTPO = lateral tibia plateau obliquity, LTSH = lateral tibia spine height.
2. Materials and methods
We retrospectively reviewed records of patients who underwent arthroscopic surgery at our institution between 2012 and 2017. Patients who had been proven discoid lateral meniscus by both MRI and arthroscopy were enrolled. All together there were 78 patients with 83 limbs in the study group. For the control group, 73 patients with 84 limbs who were proven normal lateral meniscus by MRI and matched by gender and age in out-patient practice were included. The exclusion criteria contained following:
-
(1)
patients who had surgery or trauma history before of the same knee joint;
-
(2)
patients who were under 16 years or over 65 years of age, who were most likely skeletal immature or articular degenerative respectively;
-
(3)
patients whose X-ray radiographic films showed clear osteophytic signs (grade 3 and 4 according to the Kellgren and Lawrence classification).[10]
This study was approved by the institutional Review Board of our hospital.
2.1. Radiographic analysis
All patients and controls underwent a standardized nonweight-bearing knee radiograph from anterior-posterior (AP) view with a tube to film distance of 110 cm. The following variables were evaluated: LJSH, LTSH, FHH, LTPO, and LCCA (Fig. 1). Considering the difference of knee dimensions, width of the distal femur at the level of inter-epicondylar line as Kim et al[4] had described before was also evaluated to calculate the relative value. All the measurements were performed by 2 independent and well-trained orthopedic surgeons who were unaware of the MRI or arthroscopic findings, using a computer calculation software for the distance and angle (Centricity∗5.0 Sp7.1, GE Healthcare, Barrington IL USA). Two weeks later, all images were reviewed and measured again by the same 2 surgeons.
2.2. Statistical analysis
All analyses were performed using SPSS version 17.0 (SPSS Inc., Chicago, IL). The Chi-square test was used to compare gender and involved side ratio. Independent sample t test analysis was used to compare all variables (LJSH, LTSH, FHH, LTPO, and LCCA) between each group. The threshold points for the parameters were determined using the receiver operating characteristic (ROC) curve. The cut off value derived from ROC curves at the point of highest accuracy was used to determine the mean sensitivity, specificity. The sensitivity refers to the proportion of true lateral discoid meniscus patients who are correctly identified as having those predictors. The specificity measures the proportion of normal discoid meniscus whose relative variables are negative. The intra- and interobserver reliability was also analyzed by interclass and intraclass correlation coefficients (ICC). The P-values of <.05 were considered to be significant.
3. Results
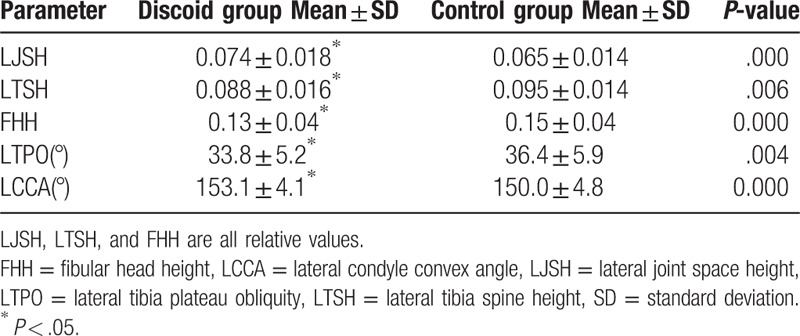
The Institutional Review Board number of our hospital is S-K686. There were no statistical differences between the 2 groups in sex, age, and involved side (Table 1). All 5 variables in tables (LJSH, LTSH, FHH, LTPO, and LCCA) were listed by categorical order, which the first 3 (LJSH, LTSH, and FHH) were ratio variables and the rest 2 (LTPO and LCCA) were numerical variables. Table 2 showed the interobserver ICC for each parameter in both groups as measured ranged from 0.75 to 0.93 while the intra-observer ICC ranged from 0.75 to 0.96, indicating a significantly high agreement between the 2 observers and high repeating consistency of observer himself among the 2 groups for measurement of radiographic parameters. Table 3 showed the mean and standard deviation of all parameters as measured in both groups. There were significant statistical differences in the LJSH, LTSH, FHH, LTPO, and LCCA.
Table 1.
Comparison of demographics between discoid lateral meniscus group and control group.
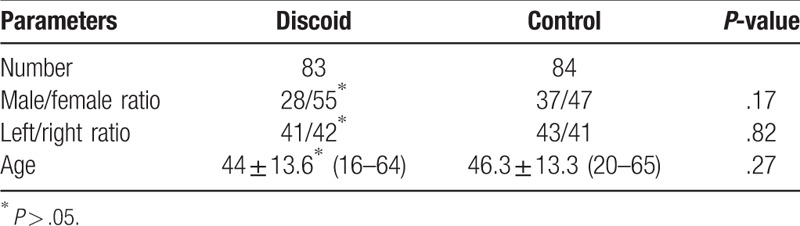
Table 2.
Intraclass correlation coefficient for the intraobserver and interobserver reliabilities of each parameter as measured.
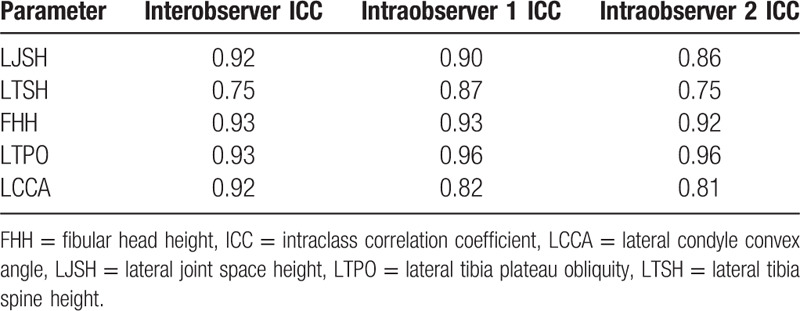
Table 3.
Mean and standard deviation of all parameters as measured in both groups.
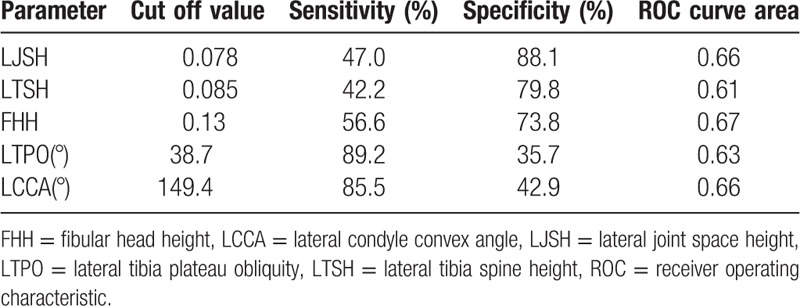
The ROC curves of all these 5 parameters were show in Figure 2. The sensitivity, the specificity and the ROC curve area according to the cut off values, which corresponded to Youden index (maximum of sensitivity + specificity − 1), in diagnosing discoid lateral meniscus are also shown in Table 4.
Figure 2.
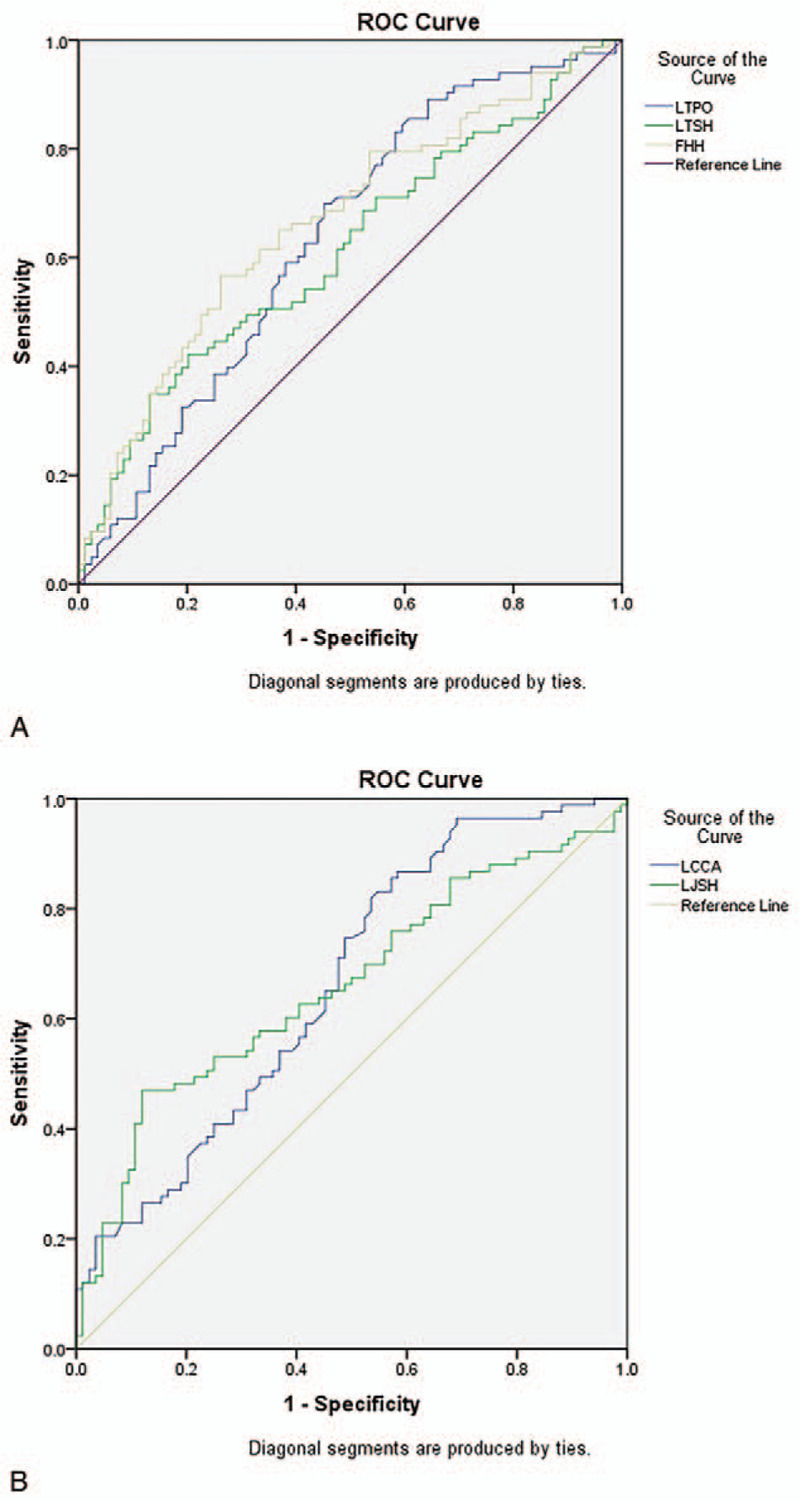
(A) ROC curve area of all parameters as measured (LTPO, LTSH, FHH). (B) ROC curve area of all parameters as measured (LCCA, LJSH). FHH = fibular head height, LCCA = lateral condyle convex angle, LJSH = lateral joint space height, LTPO = lateral tibia plateau obliquity, LTSH = lateral tibia spine height, ROC = receiver operating characteristic.
Table 4.
Sensitivity, specificity, and ROC curve area of all parameters in diagnosing discoid lateral meniscus as measured.
4. Discussion
Discoid lateral meniscus is one of the most common types of anatomic variant in the knee, with a higher incidence rate in Asian populations in literature, ranging from 17% to 33.2%.[1,2] Early literatures described some findings of plain radiography,[1,11,12] including widened lateral joint space, hypoplasia of lateral femoral condyle, soft tissue swelling and early osteoarthritis. Kim et al[4] compared discoid meniscus patients with normal controls. They used non-weight bearing AP and lateral views of plain radiography. The height of fibular head, the lateral tibia-femoral joint space, the height of lateral intercondylar spine, the obliquity and cupping of lateral tibia plateau, notching and squaring of lateral femoral condyle were measured. Only the lateral joint space and the height of fibular head showed statistical differences between the 2 groups. As for discoid meniscus, there were no statistical differences between complete and incomplete groups for all parameters. Song et al[5] also carried out a study which is similar to Kim's. They showed different results. There were statistically significant differences in the FHH and lateral joint space between the complete versus incomplete discoid meniscus groups. However, there were no statistically significant differences in all parameters between the incomplete discoid meniscus groups versus the normal groups. Interestingly, there were statistically significant differences for both lateral joint space and condylar cut-off sign between the “thick” and “thin” types of complete discoid meniscus groups. They concluded that thinner complete discoid meniscus was closer to incomplete discoid meniscus radiographically. One possible reason for the different results of both Kim and Song's studies is the different percentage of “thick” type discoid lateral meniscus in the groups. Furthermore, Song used a weight bearing films and the 45° flexion posteroanterior view instead of the standard nonweight bearing anteroposterior view radiographs used by Kim. This might also explain the difference between these 2 studies.
Ha et al[13] measured a new parameter called condylar cut-off sign. The results showed high sensitivity and specificity which were 76% and 96%, respectively. Unfortunately, the author used a specific film called tunnel view radiograph,[14] which means extra X-ray exposure and cost. Furthermore, the measurement of cut-off sign is relatively complicated and all cases in the study group are complete discoid meniscus patients without degeneration changes. Those strict criteria restricted the interpreting of their conclusions. Choi et al[6] compared radiographic findings of symptomatic discoid lateral meniscus in children instead of adults with those of matched controls. A significant difference in the FHH, lateral joint space, LTSH, and obliquity of the lateral tibia plateau distinguished the 2 groups. However, the children's age in the study ranged from 3 to 15. The cut-off values of those numerical parameters were questionable due to high variation of personal dimensions such as height and weight. The measurement of obliquity of the lateral tibia plateau was not affected by the personal dimensions. But the author showed poor interobserver ICC result (0.594). Since children's tibia plateau has more round shape on plain radiograph, we suppose that different observer might draw different baseline of tibia plateau. It would directly lead to poor interobserver ICC result whiling measuring the obliquity. Jiang et al[3] developed new parameters using relative values of height of the fibular head/lateral joint space distance and lateral joint space distance/height of the lateral tibial spine. They claimed it could eliminate the influence of body dimensions such as height and weight and lead to better ROC curve area and higher specificity and sensitivity. We question that those higher specificity and sensitivity results might also be affected by sample selection instead of relative values itself. Interestingly, the author found the mean height of lateral intercondylar spine of discoid group was statistically lower than that of normal control. This result was consistent with that of Kim and Song but contrary to that of Choi et al.[6] The reason is still unclear.
In our opinion, arthroscopy and MRI are still the gold standard for diagnosis. The main purpose of plain radiograph is for screening instead of definitive diagnosing, due to the variety of race, gender, age, extent of the degeneration of each patient. Therefore, it is quite unreliable to use the radiographic finding solely to diagnose discoid meniscus, which is in accordance with other studies.[3,4,6] On the other hand, although extra radiography checks may help to increase the sensitivity and specificity for diagnosing discoid meniscus on plain radiograph. It also leads to extra X-ray exposure and cost. Thus, we only choose the basic non-weight bearing AP view radiograph in our study. All parameters including LJSH, LTSH, FHH, LTPO, and LCCA showed significant statistical differences between the 2 groups. LCCA, 1 new type of measurement proposed by us, was significantly larger in discoid meniscus group than normal control. This result proved our hypothesis that discoid meniscus could also affect the development of lateral condyle, leading to more flat appearance. This parameter also showed high interobserver and intraobserver ICC. Giving the cut off value of 149.4°, the sensitivity and specificity were 85.5% and 42.9%, respectively. We found an interesting phenomenon in our study. Height parameters such as LJSH, LTSH, and FHH had high specificities with relatively low sensitivities. However, angle parameters such as LTPO and LCCA had high sensitivities with relatively low specificities. The reason is still unknown.
Considering that the definitive diagnosis of discoid lateral meniscus depends on arthroscopy and MRI, the main purpose of plain radiograph is for screening. Thus, parameter sensitivity is more important than specificity. Angle parameters with high sensitivities including LTPO and LCCA are more useful for screening discoid lateral meniscus than height parameters including LJSH, LTSH, and FHH. As for other parameters, different studies have different and sometime controversial conclusions, which we think may be affected by many factors including the degeneration of the joint, the exact radiography method, patient body weight, height, thick or thin type, complete discoid or incomplete, meniscus tear or not, and other factors. The retrospective, single-center design is the major and obvious limitation of this study, which may cause bias. Hence, a large randomized multi-center study or real-world research is needed before the final convincing conclusion.
As concluded, LCCA, a new type of measurement proposed by us, is statistically larger in discoid meniscus group than normal control. This high sensitivity makes it very useful for screening discoid lateral meniscus on plain radiograph. Discoid group has more widened lateral joint space and higher fibular head than that of normal control.
Author contributions
Conceptualization: Xin Lu, Jun Qian.
Data curation: Xin Lu, Jun Qian, Bo Yang, Yu Fan, Zheng Li.
Formal analysis: Xin Lu, Jun Qian, Bo Yang, Yu Fan.
Funding acquisition: Jun Qian.
Investigation: Xin Lu, Jun Qian, Bo Yang, Zheng Li.
Methodology: Xin Lu, Yu Fan, Zheng Li.
Project administration: Jun Qian.
Resources: Xin Lu, Jun Qian, Yu Fan, Zheng Li, Bo Jiang.
Software: Xin Lu, Jun Qian, Bo Jiang.
Supervision: Jun Qian, Bo Yang.
Validation: Jun Qian, Yu Fan.
Writing – original draft: Xin Lu.
Writing – review & editing: Xin Lu.
Jun Qian orcid: 0000-0001-9132-9829.
Footnotes
Abbreviations: AP view = anterior-posterior view, FHH = fibular head height, ICC = intraclass correlation coefficient, LCCA = lateral condyle convex angle, LJSH = lateral joint space height, LTPO = lateral tibia plateau obliquity, LTSH = lateral tibia spine height, ROC curve = receiver operating characteristic curve.
How to cite this article: Lu X, Qian J, Yang B, Li Z, Fan Y, Jiang B. A new radiographic finding of adult symptomatic discoid lateral meniscus. Medicine. 2020;99:14(e19646).
JQ and BY contributed equally to this work.
The authors have no conflicts of interest to disclose.
References
- [1].Ikeuchi H. Arthroscopic treatment of the discoid lateral meniscus. Technique and long-term results. Clin Orthop Relat Res 1982;167:19–28. [PubMed] [Google Scholar]
- [2].Kato Y, Oshida M, Aizawa S, et al. Discoid lateral menisci in Japanese cadaver knees. Mod Rheumatol 2004;14:154–9. [DOI] [PubMed] [Google Scholar]
- [3].Jiang W, Li X, Su H, et al. A new method to diagnose discoid lateral menisci on radiographs. Knee Surg Sports Traumatol Arthrosc 2016;24:1519–24. [DOI] [PubMed] [Google Scholar]
- [4].Kim SJ, Moon SH, Shin SJ. Radiographic knee dimensions in discoid lateral meniscus: comparison with normal control. Arthroscopy 2000;16:511–6. [DOI] [PubMed] [Google Scholar]
- [5].Song JG, Han JH, Kwon JH, et al. Radiographic evaluation of complete and incomplete discoid lateral meniscus. Knee 2015;22:163–8. [DOI] [PubMed] [Google Scholar]
- [6].Choi SH, Ahn JH, Kim KI, et al. Do the radiographic findings of symptomatic discoid lateral meniscus in children differ from normal control subjects? Knee Surg Sports Traumatol Arthrosc 2015;23:1128–34. [DOI] [PubMed] [Google Scholar]
- [7].Nathan PA, Cole SC. Discoid meniscus. A clinical and pathologic study. Clin Orthop Relat Res 1969;64:107–13. [PubMed] [Google Scholar]
- [8].Ogut T, Kesmezacar H, Akgun I, et al. Arthroscopic meniscectomy for discoid lateral meniscus in children and adolescents: 4.5 year follow-up. J Pediatr Orthop B 2003;12:390–7. [DOI] [PubMed] [Google Scholar]
- [9].Clark CR, Ogden JA. Development of the menisci of the human knee joint. Morphological changes and their potential role in childhood meniscal injury. J Bone Joint Surg Am 1983;65:538–47. [PubMed] [Google Scholar]
- [10].Kohn MD, Sassoon AA, Fernando ND. Classifications in brief: Kellgren-Lawrence classification of osteoarthritis. Clin Orthop Relat Res 2016;474:1886–93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Jeannopoulos CL. Observations on discoid menisci. J Bone Joint Surg Am 1950;32-A:649–52. [PubMed] [Google Scholar]
- [12].Jordan MR. Lateral meniscal variants: evaluation and treatment. J Am Acad Orthop Surg 1996;4:191–200. [DOI] [PubMed] [Google Scholar]
- [13].Ha CW, Lee YS, Park JC. The condylar cutoff sign: quantifying lateral femoral condylar hypoplasia in a complete discoid meniscus. Clin Orthop Relat Res 2009;467:1365–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Hing C, Raleigh E, Bailey M, et al. A prospective study of the diagnostic potential of the knee tunnel view radiograph in assessing anterior knee pain. Knee 2007;14:29–33. [DOI] [PubMed] [Google Scholar]


