Highlights
-
•
A larger number of ACEs predict substantial higher levels of PTSS and anxiety.
-
•
Experienced exposure and fear of exposure also predict more PTSS and anxiety.
-
•
Childhood abuse and neglect may exacerbate the impact of exposure on mental health.
Keywords: Covid-19, ACEs, Maltreatment, PTSS, Anxiety, Adolescents
Abstract
Background
Since the COVID-19 outbreak at the end of 2019, it has evolved into a global pandemic with tremendous mental health impact besides the threats to people’s physical health.
Objective
The aims were to examine whether exposure to COVID-19 predicts elevated levels of anxiety and post-traumatic stress symptoms and whether pre-pandemic maltreatment experiences exacerbate this impact on mental health in adolescents.
Participants and setting
The survey was conducted online from February 8 st to February 27th, 2020, and the questionnaires were distributed and retrieved through a web-based platform. This study includes a total of 6196 subjects, aged range from 11 to 18 years old.
Methods
Several multivariable linear regressions were used to analyse the data.
Results
The largest variance in PTSS and anxiety problems was explained by ACEs, with more pre-pandemic maltreatment experiences predicting more PTSS (effect size beta = 0.16∼0.27), and more anxiety (effect size beta = 0.32∼0.47). Experienced or subjective fear of exposure to COVID-19 predicted statistically significant variance in PTSS and anxiety, and standardized betas ranged from 0.04 to 0.09. Participants who had adverse childhood experiences and had experienced exposure to COVID-19 showed elevated PTSS.
Conclusions
After pre-pandemic maltreatment experiences the impact of exposure to COVID-19 on mental health may be stronger. Scars from the past seem to be vulnerabilities during societal upheaval. We therefore suggest that when exposed to COVID-19 rural adolescents should get prioritized professional family support and mental health counseling in particular when they have experienced family abuse and neglect in childhood, even though such support is more difficult to organize in rural areas.
1. Introduction
Since the COVID-19 outbreak at the end of 2019, it has evolved into a global pandemic with tremendous mental health impact besides the threats to people’s physical health (World Health Organization, 2020). Adolescents may be more vulnerable than adults to mental health problems, in particular during a lock down, because they are in a transition phase from growing up in a closely-knit family to a wider social network with increasing importance of peers, and struggling with their often brittle self-esteem (Crone et al., 2020). In particular, although spread of the virus was of greatest concern to populations in large urban centers, rural adolescents may bear more pressure due to difficulties in accessing technologies for distance learning, limited nearby physical and mental health services, and increasing unemployment rates for their family with the associated threat of poverty (FAO, 2020). Many rural adolescents are so-called ‘left-behind’ children raised by their grandparents and with their parents working in the city. These disadvantages could make rural adolescent more vulnerable to mental health issues during this difficult time, whereas they tend to be ignored in research and remain out of the spotlight in policy discussions. Furthermore, from a cumulative risk perspective rural adolescents with a history of child maltreatment experiences may be especially vulnerable to the negative consequences of the pandemic. They may lack a secure base to cope with the strains and stresses of a pandemic and its social consequences (Garber, 2000). In the current study we examine whether exposure to COVID-19 predicts elevated levels of anxiety and post-traumatic stress symptoms and whether pre-pandemic maltreatment experiences exacerbate this impact on mental health in Chinese rural adolescents.
Previous studies suggest that not only experienced exposure during the pandemic such as getting infected or facing family members’ deaths, increases mental health symptoms (Fegert, Vitiello, Plener, & Clemens, 2020; Sprang & Silman, 2013; Stikkelbroek, Bodden, Reitz, Vollebergh, & van Baar, 2016), but also fear of exposure and of becoming infected trigger stress, sometimes even traumatic stress (Braun-Lewensohn, Celestin-Westreich, Celestin, Verté, & Ponjaert-Kristoffersen, 2009). During the COVID-19 pandemic, 20–40 % Chinese adolescents were found to be prone to serious psychological problems in particular anxiety and posttraumatic stress disorder (PTSD) symptoms (Liang et al., 2020; Xie et al., 2020). Adverse childhood experiences (ACEs) including maltreatment experiences have been found to predict adolescents’ mental health outcomes in trauma contexts (Inoue et al., 2019; Rinne-Albers et al., 2017), but the relation between adverse childhood experiences and mental health consequences during the COVID-19 outbreak still is uncharted territory.
Defined by the World Health Organization (WHO), adverse childhood experiences refer to a series of intensive and frequently re-occurring stressors that people had in their childhood (World Health Organization, 2016). ACEs were measured in various ways across ACE studies in China. Some studies used questions adapted from life events or trauma scales(Wei & Yu, 2014; Xiao, Dong, Yao, Li, & Ye, 2008), others measured ACEs related to family, community, school, and personal adversity (Li, Cao, Cao, & Liu, 2015; Wong, Fong, & Chan, 2015), and one study conducted in Hong Kong translated and evaluated ACEs by the ACE-International Questionnaire (ACE-IQ) (Ho, Chan, Chien, Bressington, & Karatzias, 2019). ACEs have been found to predict physical health problems in later life such as cardiovascular diseases but also to foreshadow problems in socio-emotional development, including attachment and social cognition (Hughes et al., 2017; Schalinski, Teicher, Carolus, & Rockstroh, 2018), which might mediate various mental disorders (Vai et al., 2018).
Recent studies on adolescents have posited that ACEs were associated with increased risk of anxiety and PTSD (Lee, Kim, & Terry, 2020; van der Feltz-Cornelis et al., 2019). Moreover, studies on the relation between ACEs and adolescent’s mental health were most often inspired by a cumulative risk perspective, suggesting that a critical number of adversities experienced in childhood predicts later mental health problems (Bielas et al., 2016; Goldenson, Kitollari, & Lehman, 2020). Individuals reporting four or more ACEs had significantly more mental health outcomes than those endorsing less than four (Goldenson et al., 2020). However, the relation between ACEs and mental health problems may differ across countries (Merrick et al., 2017; Pietrek, Elbert, Weierstall, Müller, & Rockstroh, 2013). Studies on ACEs have been predominantly conducted in so-called WEIRD countries (Henrich, Heine, & Norenzayan, 2010) and to date, no empirical studies examined whether ACEs increased the risk of mental health problems among Chinese rural adolescents during the COVID-19 outbreak, and whether the same step-function of four or more ACEs holds in this (large) part of the world population.
Furthermore, ACEs may moderate the association between exposure to COVID-19 and mental health outcomes. From a cumulative risk model, the impact of exposure may be larger when individuals have experienced ACEs before the pandemic emerged (Evans, Li, & Whipple, 2013). Some previous studies point into the direction of elevated vulnerability to future adversities. For example, ACEs may enhance the risk of PTSD after exposure to later threatening events like natural disasters (Inoue et al., 2019). Furthermore, in a man-made life-threatening war, veterans with a greater number of ACEs were found to be at an increased risk of PTSD in some studies (Cabrera, Hoge, Bliese, Castro, & Messer, 2007; Fritch, Mishkind, Reger, & Gahm, 2010), but this result could not be replicated in some other studies (Rudenstine et al., 2015; Stein et al., 2005). Such differences in the relation between ACEs, exposure to a potentially traumatic event, and impact on mental health may vary according to the specific characteristics of the potentially traumatic event, and might differ across age, gender, and culture (Braun-Lewensohn et al., 2009; Schalinski et al., 2016). Thus, the cumulative stress perspective on ACEs should be examined in the Chinese pandemic context, with an emphasis on number and specific types of ACEs, in particular child abuse and neglect.
The standard measure for ACEs used in numerous studies (Hughes et al., 2017; Zhang et al., 2020) covers three dimensions related to child maltreatment and neglect. Some questions are asked about family abuse (physical, emotional, and sexual), and about family neglect (physical, emotional), whereas respondents are also asked about experiences of household dysfunctions such as growing up with substance abuse of a household member, suicide of a household member, mental illness, criminality, parental divorce, parental death). In the current study, we examine not only the impact of the number of ACEs but also the specific type of adversity, and test whether abuse, neglect or family dysfunctioning carries the weight of the moderating role.
Our first hypothesis proposes that adolescents with exposure to COVID-19 report more mental health issues than those without experienced exposure or fear of exposure. Our second hypothesis concerns the cumulative risk of ACEs, and whether in this large sample of Chinese rural adolescents the conventional step-function of four or more adversities predict mental health problems. Third, from the perspective of cumulative risk, we expect an interactive effect of exposure and ACEs on mental health symptoms, and posit that ACEs may increase the risk of PTSD and anxiety symptoms. Finally we explore which type of maltreatment or other adversity is responsible for the hypothesized moderating role.
2. Methods
2.1. Study design and population
The first case of a novel coronavirus was reported in Wuhan, China, in late December. On January 23th, Chinese authorities place the city of Wuhan under quarantine, and the rest of the Hubei province some days later. The current survey was conducted online from February 8st to February 27th, 2020, and the questionnaires were distributed and retrieved through a web-based platform (https://www.wjx.cn/app/survey.aspx). A two-stage cluster sampling method was used to choose participants from selected sites. In the first stage, three high school and seven middle schools in Zhenping County of Henan Province were selected for inclusion in the study. Henan located on the Central Plains in the mid-east of China, close to Hubei province. Then, all classes were selected from each grade of the selected school. There were 7208 subjects participate in the study. Due to the low response in two high schools and one middle school, they were excluded for this analyse. In total, 6345 rural students participated in the survey, while 149 were dropped because of incomplete information. Finally, a total of 6196 subjects from grade seven to twelve were included, age ranging from 11 to 18 years old. More details are presented in Table 1 .
Table 1.
Descriptive data on social-demographics, exposure, and mental health in the current sample (N = 6196).
| Total | Exposure = 0 | Exposure> = 1 | ||||||
|---|---|---|---|---|---|---|---|---|
| N | % | N | % | N | % | P | ||
| Ethnicity | Han | 5823 | 93.98 | 5490 | 94.3 | 333 | 5.7 | 0.110 |
| Else | 373 | 6.02 | 344 | 92.2 | 29 | 7.8 | ||
| Gender | Male | 2968 | 47.90 | 2794 | 94.1 | 174 | 5.9 | 0.957 |
| Female | 3228 | 52.10 | 3040 | 94.2 | 188 | 5.8 | ||
| Grade | Grade seven | 1237 | 19.96 | 1173 | 94.8 | 64 | 5.2 | 0.001 |
| Grade eight | 1020 | 16.46 | 975 | 95.6 | 45 | 4.4 | ||
| Grade nine | 658 | 10.62 | 623 | 94.7 | 35 | 5.3 | ||
| Grade ten | 1309 | 21.13 | 1203 | 91.9 | 106 | 8.1 | ||
| Grade eleven | 1179 | 19.03 | 1120 | 95.0 | 59 | 5.0 | ||
| Grade twelve | 793 | 12.80 | 740 | 93.3 | 53 | 6.7 | ||
| Father education | Primary and below | 1222 | 19.72 | 1143 | 93.5 | 79 | 6.5 | 0.049 |
| Junior high | 3752 | 60.56 | 3556 | 94.8 | 196 | 5.2 | ||
| Senior high | 911 | 14.70 | 843 | 92.5 | 68 | 7.5 | ||
| College and above | 311 | 5.02 | 292 | 93.9 | 19 | 6.1 | ||
| Mother education | Primary and below | 1582 | 25.53 | 1475 | 93.2 | 107 | 6.8 | 0.015 |
| Junior high | 3644 | 58.81 | 3460 | 95.0 | 184 | 5.0 | ||
| Senior high | 725 | 11.70 | 672 | 92.7 | 53 | 7.3 | ||
| College and above | 245 | 3.95 | 227 | 92.7 | 18 | 7.3 | ||
| Left behind status | No | 3264 | 52.68 | 3097 | 94.9 | 167 | 5.1 | 0.011 |
| Yes | 2932 | 47.32 | 2737 | 93.3 | 195 | 6.7 | ||
| Income | High | 417 | 6.73 | 385 | 92.3 | 32 | 7.7 | 0.125 |
| Medium | 4419 | 71.32 | 4175 | 94.5 | 244 | 5.5 | ||
| Low | 1360 | 21.95 | 1274 | 93.7 | 86 | 6.3 | ||
| Prior-exposure | Yes | 826 | 13.33 | 738 | 89.3 | 88 | 10.7 | <0.001 |
| None | 5370 | 86.67 | 5096 | 94.9 | 274 | 5.1 | ||
| Mean | SD | Mean | SD | Mean | SD | |||
| Fear exposure | Score | 7.45 | 1.92 | 7.51 | 1.92 | 7.35 | 1.87 | 0.136 |
| Anxiety | Score | 31.86 | 7.16 | 31.65 | 7.02 | 35.24 | 8.51 | <0.001 |
| PTSS | Score | 7.7 | 8 | 7.49 | 7.69 | 11.12 | 11.3 | <0.001 |
The Head teachers in each selected class helped us to distribute the questionnaires to each student through Wechat (a web communication tool in China). The teachers were being instructed about the concept of standardization and the use of standardized testing procedures. The teachers in their turn instructed the students about how to answer the questionnaires, and had them finish the questionnaire independently. However, if the students had some questions, they were able to ask the teacher or the research team. Generally, the items in the questionnaire took about 15−20 min in all to complete. Participants received a small gift (e.g., 1–3 RMB) as a token of appreciation at the end of the session. All participants gave consent after being informed about the aim of the survey and joined the study voluntarily. The study was approved by the Ethics Committee of Peking University Medical Center.
3. Measures
3.1. Outcomes variables
Post-traumatic stress symptoms(PTSS) were assessed with the self-report PTSD Checklist for DSM-5 (PCL-5) (Weathers et al., 2013), estimating the degree to which individuals had been struggling with DSM-5-related PTSS symptoms in the past month. Respondents answered the 20 items on a 4-point rating scale from 0 (not at all) to 4 (extremely). Items were summed for a total score ranging from 0 to 80, with higher scores indicating higher level of PTSS. In this study, Cronbach's alpha was 0.90.
Anxiety was assessed by the Zung self-rated anxiety scale (SAS) (Zung, 1971), a self-administered scale, with each response using a 4-point scale, from ‘none of the time” to “most of the time.” There were 20 questions with 15 questions about increasing anxiety level and 5 questions about decreasing anxiety. Although developed in 1971, the SAS continues to be extensively used in research. The SAS has satisfactory psychometric properties, and has been widely used with Chinese populations (Pang, Tu, & Cai, 2019; Zhou, Xu, Inglés, Hidalgo, & La Greca, 2008). Cronbach’s alpha for the SAS in this study was 0.83.
3.2. Independent variables
Adverse Childhood Experiences (ACE) is a measure based on previous ACE studies (Hughes et al., 2017; Zhang et al., 2020). The scale includes 14 items in three categories: three items about family abuse (physical abuse, emotional abuse, and sexual abuse), five items about family neglect (2 for emotional neglect including lack of communication and lack of attention; 3 for physical neglect including food difficulties, medical difficulties, and parental neglect), and six items about household dysfunctions (growing up with household member substance abuse, suicide among household members, mental illness among household members, criminality of household members, parental divorce, parental death). Response options for each question based on a 5-point Likert scale ranged from “never” to “always”. The scores for each item were summed to an overall ACE continuous score. We used the binary scoring method (World Health Organization, 2016) as follows: from five original response options, ACEs variable was dichotomized into individuals reporting that they never experienced this ACE (no exposure = 0) or that they rarely, sometimes, often or always had experienced it (exposure = 1) for family abuse, physical neglect, and household dysfunctions, while responses of “never” and “rarely” were recoded as “no exposure = 0”; “sometimes”, “often” or “always” were recoded as “exposure = 1” for emotional neglect. Then, the total numbers of ACE categories were summed to create an ACE score ranging from 0 to 14. Cronbach’s alpha for the overall continuous ACEs scale in this study was 0.78. For the three sub-scales Cronbach’s alpha was 0.67 for family abuse, 0.60 for family neglect, and 0.65 for household dysfunction.
Experienced exposure to COVID-19 was assessed with several questions about possibly having suffered or suffering from COVID-19, or someone in the family, or neighborhood or among friends, with “1” for COVID-19 of self, a member of the family, a friend, or someone in the neighborhood, and “0” referring to no exposure). Then, a total score was obtained by summing the scores of these items. In this study, the range of exposures was from 0 to 4.
Fear of exposure to COVID-19 were measured by two questions to estimate how they feared themselves the exposure to COVID-19, and how they feared their family members would be exposed to COVID-19. Response alternative for each item were as follows: 1—completely no fear, 2—no fear, 3—a little bit, 4—quite some fear; 5, a lot of fear. The total score was the sum of these two items. The Cronbach’s alpha was 0.69. In a previous study, fear of exposure was related to PTSS (Guo, He, Qu, Wang, & Liu, 2017).
3.3. Covariates
The following covariates were measured. Demographic variables included ethnicity (Han, else), grade (seven to twelve), father’s education (primary and below, junior high school, senior high school/technical school, college and above), mother’s education (primary and below, junior high school, senior high school/technical school, college and above), and family income (high, medium and low income), prior exposure to potential trauma (experience of a traumatic event in the last year (yes, no)), and left-behind status (Yes/No). Left-behind status was defined as “adolescents who have been left behind at their original residence while one or both parents migrated to other places for work and have been not living together with them for at least 6 months (Guo, Li, Wang, Ma, & Ma, 2020). These variables have been shown to be associated with PTSS and anxiety among adolescents (Fan, Zhang, Yang, Mo, & Liu, 2011; Zhang et al., 2012).
3.4. Statistical analyses
The main analyses consisted of multivariable linear regressions on PTSS or anxiety in three steps, and in each step the same covariates were used: gender, ethnicity, father’s educational level, mother’s education level, family income, prior exposure. In model 0 each of the predictors were included separately to estimate their ‘raw’ contribution to the prediction of PTSS, and anxiety, controlling for the covariates. In model 1 & 2 the three predictors of (potential) exposure (experienced exposure, fear of exposure, and ACE) were included to examine which component would be the most powerful predictor. To better estimate the relation between ACEs on the one hand and PTSS and anxiety on the other hand, ACEs were added to the model as a continuous variable. To refine this main analysis we also used the three dimensions of ACEs to differentiate child abuse from neglect and from family dysfunctions. We computed standardized betas that can be compared across models and predictors.
In the next two linear regression analyses, the interaction variables of the standardized continuous score for ACEs and standardized two types of exposure (experienced exposure, fear of exposure) were added to the model to examine their relation with PTSS and anxiety. In final exploratory analyses, several interaction variables for standardized scores of family abuse, family neglect, and household dysfunctions with standardized scores for exposure variables on PTSS and anxiety were examined in the linear regression models. The SPSS version 22.0 was used to carry out all analyses.
4. Results
4.1. Predicting PTSS and anxiety
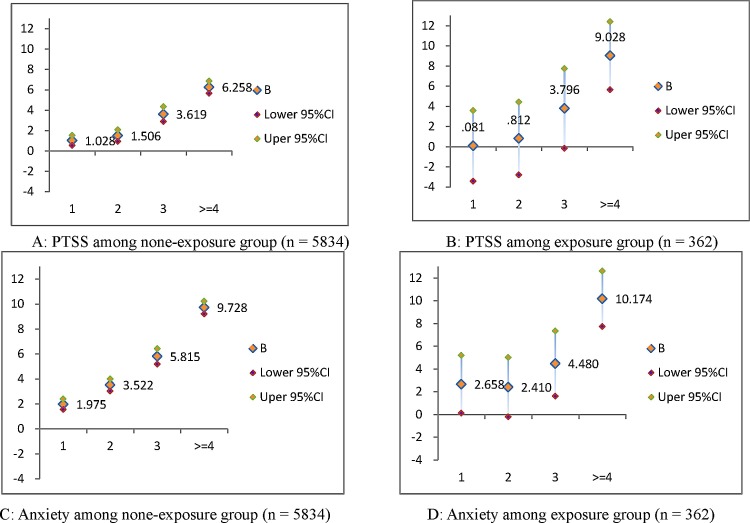
In Tables 2 and 3 the results of the linear regressions on PTSS and anxiety are presented. The largest variance in PTSS and anxiety problems was explained by ACEs, with more adverse childhood experience predicting more PTSS (effect size beta = 0.27), and more anxiety (effect size beta = 0.47). Furthermore, each of the ACE clusters (family abuse, family neglect, and household dysfunctions) also were associated with more PTSS and anxiety. Reported family neglect amounted to a substantial standardized beta of 0.15 for PTSS, while family neglect amounted to a standardized beta of 0.11 for anxiety. Finally, experienced or fear of exposure to COVID-19 predicted statistically significant variance in PTSS and anxiety. Standardized betas ranged from 0.06 to 0.09, thus considerably smaller effect sizes compared to those found for ACEs. Fear of exposure to the virus showed a standardized beta of 0.15 for PTSS, and 0.08 for anxiety. The expected dose-response effects of ACEs also are presented in Fig. 1 , with more ACEs predicting higher levels of PTSS and anxiety symptoms, in particular with 4 or more ACEs.
Table 2.
Multiple linear regressions with exposure, fear exposure, ACEs predicting PTSD.
| Model0 |
model1 |
model2 |
||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| B | Std. Error | Beta | Sig. | B | Std. Error | Beta | Sig. | B | Std. Error | Beta | Sig. | |
| Experienced exposure | 3.277 | .354 | .116 | <0.001 | 2.479 | .340 | .088 | .000 | 2.483 | .340 | .088 | <0.001 |
| Fear exposure | .572 | .052 | .137 | <0.001 | .639 | .050 | .153 | .000 | .638 | .050 | .153 | <0.001 |
| ACE count | 0.939 | .043 | .267 | <0.001 | .932 | .043 | .265 | .000 | <0.001 | |||
| Family abuse | 1.648 | .174 | .135 | <0.001 | 1.616 | .171 | .132 | <0.001 | ||||
| Family neglect | 1.036 | .099 | .151 | <0.001 | 1.050 | .097 | .153 | <0.001 | ||||
| Household dysfunctions | .411 | .119 | .051 | .001 | .395 | .117 | .049 | .001 | ||||
Notes: B: coefficient, Std Error: standard error; Control variables: Gender, ethnicity, grade, father education, mother education, family income, prior exposure. All the models were adjusted confounding.
Table 3.
Multiple linear regressions with exposure, fear exposure, ACEs predicting Anxiety.
| Anxiety | Model0 |
model1 |
model2 |
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| B | Std. Error | Beta | Sig. | B | Std. Error | Beta | Sig. | B | Std. Error | Beta | Sig. | |
| Experienced exposure | 2.854 | .318 | .113 | <0.001 | 1.502 | .283 | .059 | <0.001 | 1.506 | .282 | .059 | <0.001 |
| Fear exposure | .185 | .047 | .049 | <0.001 | .286 | .042 | .076 | <0.001 | .291 | .041 | .078 | <0.001 |
| ACE count | 1.495 | .036 | .474 | <0.001 | 1.486 | .036 | .471 | <0.001 | <0.001 | |||
| Family abuse | 1.242 | .142 | .113 | <0.001 | 1.223 | .142 | .112 | <0.001 | ||||
| Family neglect | 2.080 | .081 | .338 | <0.001 | 2.080 | .081 | .338 | <0.001 | ||||
| Household dysfunctions | .928 | .098 | .129 | <0.001 | .915 | .097 | .127 | <0.001 | ||||
Notes: B: coefficient, Std Error: standard error; Control variables: Gender, ethnicity, grade, father education, mother education, family income, prior exposure. All the models were adjusted confounding.
Fig. 1.
The dose-response effect of ACEs with PTSD and anxiety.
Notes: B: coefficient, CI: confidence interval; Control variables: Gender, ethnicity, grade, father education, mother education, family income, prior exposure, fear exposure. All the models were adjusted confounding.
4.2. Interactions between exposure and ACEs
Table 4 shows that there was an interaction between ACEs and exposure predicting PTSS, but not anxiety. Participants who reported more adverse childhood experiences and had experienced exposure to COVID-19 showed elevated PTSS (effect size beta = 0.03, p < 0.05). Interactions with fear of exposure were not significant, and no interaction predicted variance in anxiety symptoms.
Table 4.
Multiple linear regression for interaction effects of ACEs and exposure predicting mental health.
| Model 1 PTSD |
Model 2 Anxiety |
|||||||
|---|---|---|---|---|---|---|---|---|
| B | Std. Error | Beta | Sig. | B | Std. Error | Beta | Sig. | |
| Experienced exposure | 2.104 | .381 | .074 | <0.001 | 1.653 | .317 | .065 | <0.001 |
| Fear exposure | .640 | .050 | .153 | <0.001 | .284 | .042 | .076 | <0.001 |
| ACEs | .924 | .043 | .262 | <0.001 | 1.493 | .036 | .473 | <0.001 |
| ACEs*experienced exposure | .161 | .074 | .029 | .030 | −.064 | .062 | −.013 | .301 |
| ACEs*fear exposure | −.056 | .091 | −.007 | .540 | .132 | .076 | .019 | .083 |
Notes: B: coefficient, Std Error: standard error; Control variables: Gender, ethnicity, grade, father education, mother education, family income, prior exposure. All the models were adjusted confounding.
The significant interaction was further examined by testing the interactions of each of the three dimensions of ACEs (family abuse, family neglect and household dysfunctions) with experienced exposure on PTSS (see Table 5 ). The interaction of family neglect and experienced exposure significantly predicted PTSS (effect size beta = 0.04, p < 0.01). In particular participants with more adverse childhood experiences and with experienced exposure to COVID-19 showed elevated PTSS.
Table 5.
Multiple linear regression for interaction effects of Dimensions of ACEs and exposure predicting PTSD.
| Model1 |
Model2 |
Model3 |
||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| B | Std. Error | Beta | Sig. | B | Std. Error | Beta | Sig. | B | Std. Error | Beta | Sig. | |
| Experienced exposure | 2.492 | .358 | .088 | <0.001 | 1.975 | .373 | .070 | <0.001 | 2.223 | .371 | .079 | <0.001 |
| Fear exposure | .639 | .050 | .153 | <0.001 | .640 | .050 | .153 | <0.001 | .639 | .050 | .153 | <0.001 |
| Family abuse | 1.616 | .172 | .132 | <0.001 | 1.608 | .171 | .132 | <0.001 | 1.614 | .171 | .132 | <0.001 |
| Family neglect | 1.049 | .097 | .153 | <0.001 | 1.037 | .097 | .151 | <0.001 | 1.055 | .097 | .153 | <0.001 |
| Household dysfunctions | .395 | .117 | .049 | .001 | .387 | .117 | .048 | .001 | .377 | .118 | .047 | .001 |
| Family abuse*experienced exposure | −.006 | .070 | −.001 | .933 | ||||||||
| −.022 | .091 | −.003 | .810 | |||||||||
| Family neglect*experienced exposure | .283 | .086 | .043 | .001 | ||||||||
| −.112 | .093 | −.014 | .230 | |||||||||
| Household dysfunctions* experienced exposure | .122 | .070 | .023 | .082 | ||||||||
| .015 | .093 | .002 | .874 | |||||||||
Notes: B: coefficient, Std Error: standard error; Control variables: Gender, ethnicity, grade, father education, mother education, family income, prior exposure. All the models were adjusted confounding.
5. Discussion
The COVID-19 outbreak and resulting lockdown has been a major challenge for adolescents with a developing and often still brittle self-esteem and for whom peer relationships are of growing importance. In the current study we examined the associations between pre-pandemic adverse childhood experiences, exposure to COVID-19, and mental health among Chinese rural adolescents. We found that a larger number of ACEs predicted substantial higher levels of PTSS and anxiety, and to a lesser extent both experienced exposure and fear of exposure also predicted more PTSS and anxiety, controlling for several covariates. Furthermore, we found some evidence for cumulative risk as students with more adverse childhood experiences and with experienced exposure to COVID-19 showed elevated PTSS. Family abuse, family neglect, and household dysfunction were all associated with PTSS and anxiety levels but only neglect seemed to predict higher levels of PTSS in case adolescents were exposed to COVID-19.
Exposure to COVID-19 predicts higher levels of PTSS and anxiety with effect sizes ranging from 0.06 to 0.15 (standardized betas). The largest variance in PTSS and anxiety problems, however, was explained by ACEs, with more adverse childhood experience predicting more PTSS and more anxiety, with effect sizes ranging from 0.27 to 0.47 (standardized betas). Within the set of ACEs family abuse was the strongest predictor of PTSS (standardized beta = 0.17), whereas family neglect was the strongest predictor of anxiety levels (standardized beta = 0.34). As noted in previous studies, experienced exposure refers to direct harm from a traumatic event, and it is suggested to be a primary risk for elevated levels of adolescents’ subsequent anxiety and PTSS (Braun-Lewensohn et al., 2009; Schiff, Zweig, Benbenishty, & Hasin, 2007). The current study demonstrated that experienced exposure to COVID-19 leads to greater risk of adverse mental reactions such as PTSS and anxiety. Similarly, fear of exposure indicating fear and worries adolescents have about the safety of themselves and their families, are salient predictors of adverse mental health outcomes among adolescents (Braun-Lewensohn et al., 2009; Guo, Feng, Wang, & van IJzendoorn, 2020; Polimanti et al., 2019). However, effect sizes are not overwhelmingly large and the associations between ACEs and mental health problems seem to be comparably larger.
In the current study on Chinese rural adolescents the prevalence of ACEs was 58.8 %, and 14.2 % of the participants had experienced four adversities or more. In addition, the prevalence of each of the three types of adversities --family abuse, family neglect, and household dysfunction-- was 17.7 %, 45.4 %, and 30.1 % respectively. These rates are comparable to prevalence rates found in other studies (Bellis, Hughes, Leckenby, Perkins, & Lowey, 2014; Chan, 2013; Hughes et al., 2017; Walsh, McCartney, Smith, & Armour, 2019). A meta-analysis of 68 child maltreatment studies conducted in China estimated that 27 % of children suffered physical abuse, 20 % reported emotional abuse, 9% reported sexual abuse, and 26 % reported neglect (Fang et al., 2015). Studies in other countries also revealed a rather high prevalence of ACEs among adolescents (Afifi et al., 2020; Crouch, Probst, Radcliff, Bennett, & McKinney, 2019; Soares et al., 2016). In line with previous studies is also the prediction of PTSS and anxiety on the basis of cumulative ACEs (Sareen et al., 2013; Thomson & Jaque, 2017), in particular the accumulation of 4 or more ACEs.
One explanation for this predictive power of ACEs is the ‘kindling’ hypothesis, ACEs increase vulnerability to future life stresses and lower the threshold required to trigger depressive or anxious episodes (Monroe & Harkness, 2005; Shapero et al., 2017; Zuroff, Santor, & Mongrain, 2004), thus leading to a downward spiral in mental health problems (Crouch, Radcliff, Strompolis, & Srivastav, 2019; McLaughlin, Conron, Koenen, & Gilman, 2010; Walsh et al., 2019). Here we argue that we should look at the content of ACEs, in our study abuse and neglect being important predictors as well as moderators of the associations between exposure to COVID-19 and PTSS and anxiety symptoms. From studies of the influence of child abuse and neglect on the developing stress system and brain architecture it can be derived that dysregulation of the HPA-axis and atypical growth of hippocampal volume are among the negative consequences (van Hoof et al., 2019; van IJzendoorn et al., 2020). In normal circumstances such a dysregulation might not leave traces on adaptation of the individual but in chronic stressful conditions such as created by a pandemic the stress regulatory system might become overtaxed and successful adaptation out of reach (Dvir, Ford, Hill, & Frazier, 2014). Thus, child abuse and neglect may lead to changes of brain structure and functioning related to stress responses. Neural pathways processing threat would be more sensitized (Ramiro, Madrid, & Brown, 2010). In particular, neglect during childhood has been shown to stimulate stress sensitization, and individuals having experienced family neglect might become more vulnerable to subsequent stressful life events and suffer more intense traumatic feelings (McLaughlin et al., 2010; Ramiro et al., 2010).
6. Limitations and strengths
Some limitations of this study should be mentioned. A first limitation is the possible recall bias derived from retrospective reporting ACEs and other validity issues pertaining to self-reports based on a limited number of items and closed response categories. Indeed, there are valid reasons to question the use of the ACE questionnaires to assess separate types of adversities (McLennan, MacMillan, & Afifi, 2020). For example, in our study the Cronbach’s alpha for the three types of ACEs were borderline due to the small number of items for each of the dimensions. These issues might be exacerbated by the transfer of the instrument from the USA to China, and more cross-cultural psychometric studies are badly needed. Second, based on cross-sectional data this study cannot infer causality, although it seems plausible enough that in the temporal sequence ACEs are first, the potentially traumatic event of experiencing COVID-19second in line, and PTSS and anxiety being the outcome. Third, we found that a large number of rural adolescents were so-called ‘left-behind’ but the absence of their parents seemed not a crucial factor in their coping or lack thereof. Future studies should include measures of grandparental care for these youth. Finally, the study sample we collected was from adolescents in rural communities, not all of whom might have access to the internet. The non-response rate and reasons could not be estimated due to anonymity requirements.
The study was conducted online starting on February 8, 2020, just a short time after the city of Wuhan was placed under quarantine (January 23, 2020), and is probably one of the earliest studies focused on stress for youth caused by the pandemic. The results support our hypothesis that on top of both experienced exposure and fear of exposure a larger number of maltreatment experiences suffered before the pandemic predicted higher levels of PTSS and anxiety. Scars from the past seem to be vulnerabilities during societal upheaval. In addition, we focused on a rarely studied sample of rural adolescents whom are more difficult to reach but might nevertheless be impacted by a pandemic and even more so because of their being deprived of the same medical and social support available in the cities. Though COVID-19 spreads faster in big cities, rural adolescents’ mental health should not be neglected as they deserve the support of prevention and intervention strategies in particular when they have had adverse childhood experiences.
7. Conclusion
We found that adolescents with cumulative adverse childhood experiences such as family abuse and neglect are psychologically most at risk when exposed to infections during a pandemic that requires lockdown and social isolation. Therefore, we suggest that professional family support and mental health counseling for adolescents with a history of abuse and neglect, and current exposure to COVID-19 get prioritized.
Author contributions
J.G. and XW designed the study and conceived the paper. J.G. and M.H.v.I. extracted and analyzed the data. J.G. and M.H.v.I wrote the first draft. M.F., D.L., X.W., B.Z. and all authors commented on the manuscript and provided input in the final manuscript.
Funding
This work was supported by the National Social Science Fund of China (Number: 20VYJ042) to JG, and the Netherland’s Organization for Scientific Research (Spinoza Prize) to MHvIJ.
Declaration of Competing Interest
The authors report no declarations of interest.
References
- Afifi T.O., Taillieu T., Salmon S., Davila I.G., Stewart-Tufescu A., Fortier J.…MacMillan H.L. Adverse childhood experiences (ACEs), peer victimization, and substance use among adolescents. Child Abuse & Neglect. 2020;106 doi: 10.1016/j.chiabu.2020.104504. [DOI] [PubMed] [Google Scholar]
- Bellis M.A., Hughes K., Leckenby N., Perkins C., Lowey H. National household survey of adverse childhood experiences and their relationship with resilience to health-harming behaviors in England. BMC Medicine. 2014;12(1) doi: 10.1186/1741-7015-12-72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bielas H., Barra S., Skrivanek C., Aebi M., Steinhausen H.C., Bessler C., Plattner B. The associations of cumulative adverse childhood experiences and irritability with mental disorders in detained male adolescent offenders. Child and Adolescent Psychiatry and Mental Health. 2016;10(1) doi: 10.1186/s13034-016-0122-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Braun-Lewensohn O., Celestin-Westreich S., Celestin L.P., Verté D., Ponjaert-Kristoffersen I. Adolescents’ mental health outcomes according to different types of exposure to ongoing terror attacks. Journal of Youth and Adolescence. 2009;38(6):850–862. doi: 10.1007/s10964-008-9305-8. [DOI] [PubMed] [Google Scholar]
- Cabrera O.A., Hoge C.W., Bliese P.D., Castro C.A., Messer S.C. Childhood adversity and combat as predictors of depression and post-traumatic stress in deployed troops. American Journal of Preventive Medicine. 2007;33(2):77–82. doi: 10.1016/j.amepre.2007.03.019. [DOI] [PubMed] [Google Scholar]
- Chan K.L. Victimization and poly-victimization among school-aged Chinese adolescents: Prevalence and associations with health. Preventive Medicine. 2013;56(3–4):207–210. doi: 10.1016/j.ypmed.2012.12.018. [DOI] [PubMed] [Google Scholar]
- Crone E.A., Achterberg M., Dobbelaar S., Euser S., Bulk den, van B., Meulen der, van M.…van IJzendoorn M.H. Neural and behavioral signatures of social evaluation and adaptation in childhood and adolescence: The Leiden Consortium on Individual Development (L-CID) Developmental Cognitive Neuroscience. 2020;100805 doi: 10.1016/j.dcn.2020.100805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crouch E., Probst J.C., Radcliff E., Bennett K.J., McKinney S.H. Prevalence of adverse childhood experiences (ACEs) among US children. Child Abuse and Neglect. 2019;92:209–218. doi: 10.1016/j.chiabu.2019.04.010. [DOI] [PubMed] [Google Scholar]
- Crouch E., Radcliff E., Strompolis M., Srivastav A. Safe, stable, and nurtured: Protective factors against poor physical and mental health outcomes following exposure to adverse childhood experiences (ACEs) Journal of Child and Adolescent Trauma. 2019;12(2):165–173. doi: 10.1007/s40653-018-0217-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dvir Y., Ford J.D., Hill M., Frazier J.A. Childhood maltreatment, emotional dysregulation, and psychiatric comorbidities. Harvard Review of Psychiatry. 2014;22:149–161. doi: 10.1097/HRP.0000000000000014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Evans G.W., Li D., Whipple S.S. Cumulative risk and child development. Psychological Bulletin. 2013;139(6):1342–1396. doi: 10.1037/a0031808. [DOI] [PubMed] [Google Scholar]
- Fan F., Zhang Y., Yang Y., Mo L., Liu X. Symptoms of posttraumatic stress disorder, depression, and anxiety among adolescents following the 2008 Wenchuan earthquake in China. Journal of Traumatic Stress. 2011;24(1):44–53. doi: 10.1002/jts.20599. [DOI] [PubMed] [Google Scholar]
- Fang X., Fry D.A., Ji K., Finkelhor D., Chen J., Lannen P., Dunne M.P. La charge de la maltraitance des enfants en Chine: Une revue systématique. Bulletin of the World Health Organization. 2015;93(3):176–185. doi: 10.2471/BLT.14.140970. [DOI] [PMC free article] [PubMed] [Google Scholar]
- FAO (Nations Food and Agriculture Organization of the United) 2020. Rural youth and the COVID-19 pandemic. [Google Scholar]
- Fegert J.M., Vitiello B., Plener P.L., Clemens V. Challenges and burden of the Coronavirus 2019 (COVID-19) pandemic for child and adolescent mental health: A narrative review to highlight clinical and research needs in the acute phase and the long return to normality. Child and Adolescent Psychiatry and Mental Health. 2020;14 doi: 10.1186/s13034-020-00329-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fritch A.M., Mishkind M., Reger M.A., Gahm G.A. The impact of childhood abuse and combat-related trauma on postdeployment adjustment. Journal of Traumatic Stress. 2010;23(2):248–254. doi: 10.1002/jts.20520. [DOI] [PubMed] [Google Scholar]
- Garber J. Handbook of attachment. In: Cassidy J., Shaver P.R., editors. Vol. 61. 2000. (The journal of clinical psychiatry). [DOI] [Google Scholar]
- Goldenson J., Kitollari I., Lehman F. The relationship between ACEs, trauma-related psychopathology and resilience in vulnerable youth: Implications for screening and treatment. Journal of Child and Adolescent Trauma. 2020 doi: 10.1007/s40653-020-00308-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guo J., He H., Qu Z., Wang X., Liu C. Post-traumatic stress disorder and depression among adult survivors 8 years after the 2008 Wenchuan earthquake in China. Journal of Affective Disorders. 2017;210:27–34. doi: 10.1016/j.jad.2016.12.009. [DOI] [PubMed] [Google Scholar]
- Guo J., Feng X.L., Wang X.H., van IJzendoorn M.H. Coping with COVID-19: Exposure to covid-19 and negative impact on livelihood predict elevated mental health problems in Chinese adults. International Journal of Environmental Research and Public Health. 2020;17(11):1–18. doi: 10.3390/ijerph17113857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guo J., Li M., Wang X., Ma S., Ma J. Being bullied and depressive symptoms in Chinese high school students: The role of social support. Psychiatry Research. 2020:284. doi: 10.1016/j.psychres.2019.112676. [DOI] [PubMed] [Google Scholar]
- Henrich J., Heine S.J., Norenzayan A. The weirdest people in the world? The Behavioral and Brain Sciences. 2010;33:61–83. doi: 10.1017/S0140525X0999152X. [DOI] [PubMed] [Google Scholar]
- Ho G.W.K., Chan A.C.Y., Chien W.T., Bressington D.T., Karatzias T. Examining patterns of adversity in Chinese young adults using the Adverse Childhood Experiences—International Questionnaire (ACE-IQ) Child Abuse and Neglect. 2019;88:179–188. doi: 10.1016/j.chiabu.2018.11.009. [DOI] [PubMed] [Google Scholar]
- Hughes K., Bellis M.A., Hardcastle K.A., Sethi D., Butchart A., Mikton C.…Dunne M.P. The effect of multiple adverse childhood experiences on health: A systematic review and meta-analysis. The Lancet Public Health. 2017;2(8):e356–e366. doi: 10.1016/S2468-2667(17)30118-4. [DOI] [PubMed] [Google Scholar]
- Inoue Y., Stickley A., Yazawa A., Aida J., Kawachi I., Kondo K., Fujiwara T. Adverse childhood experiences, exposure to a natural disaster and posttraumatic stress disorder among survivors of the 2011 Great East Japan earthquake and tsunami. Epidemiology and Psychiatric Sciences. 2019;28(1):45–53. doi: 10.1017/S2045796017000233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee H., Kim Y., Terry J. Adverse childhood experiences (ACEs) on mental disorders in young adulthood: Latent classes and community violence exposure. Preventive Medicine. 2020:134. doi: 10.1016/j.ypmed.2020.106039. [DOI] [PubMed] [Google Scholar]
- Li Y., Cao F., Cao D., Liu J. Nursing students’ post-traumatic growth, emotional intelligence and psychological resilience. Journal of Psychiatric and Mental Health Nursing. 2015;22(5):326–332. doi: 10.1111/jpm.12192. [DOI] [PubMed] [Google Scholar]
- Liang L., Ren H., Cao R., Hu Y., Qin Z., Li C., Mei S. The effect of COVID-19 on youth mental health. The Psychiatric Quarterly. 2020 doi: 10.1007/s11126-020-09744-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McLaughlin K.A., Conron K.J., Koenen K.C., Gilman S.E. Childhood adversity, adult stressful life events, and risk of past-year psychiatric disorder: A test of the stress sensitization hypothesis in a population-based sample of adults. Psychological Medicine. 2010;40(10):1647–1658. doi: 10.1017/S0033291709992121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McLennan J.D., MacMillan H.L., Afifi T.O. Questioning the use of adverse childhood experiences (ACEs) questionnaires. Child Abuse & Neglect. 2020;101 doi: 10.1016/j.chiabu.2019.104331. [DOI] [PubMed] [Google Scholar]
- Merrick M.T., Ports K.A., Ford D.C., Afifi T.O., Gershoff E.T., Grogan-Kaylor A. Unpacking the impact of adverse childhood experiences on adult mental health. Child Abuse & Neglect. 2017;69:10–19. doi: 10.1016/j.chiabu.2017.03.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Monroe S.M., Harkness K.L. Life stress, the “kindling” hypothesis, and the recurrence of depression: Considerations from a life stress perspective. Psychological Review. 2005;112(2):417–445. doi: 10.1037/0033-295X.112.2.417. [DOI] [PubMed] [Google Scholar]
- Pang Z., Tu D., Cai Y. Psychometric properties of the SAS, BAI, and S-AI in Chinese university students. Frontiers in Psychology. 2019;10(January) doi: 10.3389/fpsyg.2019.00093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pietrek C., Elbert T., Weierstall R., Müller O., Rockstroh B. Childhood adversities in relation to psychiatric disorders. Psychiatry Research. 2013;206(1):103–110. doi: 10.1016/j.psychres.2012.11.003. [DOI] [PubMed] [Google Scholar]
- Polimanti R., Carvalho C.M., Wendt F., Belangero S., Nievergelt C., Koenen K., Gelernter J. Causal inference using different phenotypic traits related to trauma exposure, trauma response, and posttraumatic stress disorder. European Neuropsychopharmacology. 2019;29:S42–S43. doi: 10.1016/j.euroneuro.2019.07.084. [DOI] [Google Scholar]
- Ramiro L.S., Madrid B.J., Brown D.W. Adverse childhood experiences (ACE) and health-risk behaviors among adults in a developing country setting. Child Abuse and Neglect. 2010;34(11):842–855. doi: 10.1016/j.chiabu.2010.02.012. [DOI] [PubMed] [Google Scholar]
- Rinne-Albers M.A., Pannekoek J.N., van Hoof M.J., van Lang N.D., Lamers-Winkelman F., Rombouts S.A.…Vermeiren R.R. Anterior cingulate cortex grey matter volume abnormalities in adolescents with PTSD after childhood sexual abuse. European Neuropsychopharmacology. 2017;27(11):1163–1171. doi: 10.1016/j.euroneuro.2017.08.432. [DOI] [PubMed] [Google Scholar]
- Rudenstine S., Cohen G., Prescott M., Sampson L., Liberzon I., Tamburrino M.…Galea S. Adverse childhood events and the risk for new-onset depression and post-traumatic stress disorder among U.S. national guard soldiers. Military Medicine. 2015;180(9):972–978. doi: 10.7205/MILMED-D-14-00626. [DOI] [PubMed] [Google Scholar]
- Sareen J., Henriksen C.A., Bolton S.L., Afifi T.O., Stein M.B., Asmundson G.J.G. Adverse childhood experiences in relation to mood and anxiety disorders in a population-based sample of active military personnel. Psychological Medicine. 2013;43(1):73–84. doi: 10.1017/S003329171200102X. [DOI] [PubMed] [Google Scholar]
- Schalinski I., Teicher M.H., Carolus A.M., Rockstroh B. Defining the impact of childhood adversities on cognitive deficits in psychosis: An exploratory analysis. Schizophrenia Research. 2018;192:351–356. doi: 10.1016/j.schres.2017.05.014. [DOI] [PubMed] [Google Scholar]
- Schalinski I., Teicher M.H., Nischk D., Hinderer E., Müller O., Rockstroh B. Type and timing of adverse childhood experiences differentially affect severity of PTSD, dissociative and depressive symptoms in adult inpatients. BMC Psychiatry. 2016;16(1) doi: 10.1186/s12888-016-1004-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schiff M., Zweig H.H., Benbenishty R., Hasin D.S. Exposure to terrorism and Israeli youths’ cigarette, alcohol, and cannabis use. American Journal of Public Health. 2007;97(10):1852–1858. doi: 10.2105/AJPH.2006.090514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shapero B.G., Weiss R.B., Burke T.A., Boland E.M., Abramson L.Y., Alloy L.B. Kindling of life stress in bipolar disorder: Effects of early adversity. Behavior Therapy. 2017;48(3):322–334. doi: 10.1016/j.beth.2016.12.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Soares A.L.G., Howe L.D., Matijasevich A., Wehrmeister F.C., Menezes A.M.B., Gonçalves H. Adverse childhood experiences: Prevalence and related factors in adolescents of a Brazilian birth cohort. Child Abuse and Neglect. 2016;51:21–30. doi: 10.1016/j.chiabu.2015.11.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sprang G., Silman M. Posttraumatic stress disorder in parents and youth after health-related disasters. Disaster Medicine and Public Health Preparedness. 2013;7(1):105–110. doi: 10.1017/dmp.2013.22. [DOI] [PubMed] [Google Scholar]
- Stein A.L., Tran G.Q., Lund L.M., Haji U., Dashevsky B.A., Baker D.G. Correlates for posttraumatic stress disorder in Gulf War veterans: A retrospective study of main and moderating effects. Journal of Anxiety Disorders. 2005;19(8):861–876. doi: 10.1016/j.janxdis.2004.09.006. [DOI] [PubMed] [Google Scholar]
- Stikkelbroek Y., Bodden D.H.M., Reitz E., Vollebergh W.A.M., van Baar A.L. Mental health of adolescents before and after the death of a parent or sibling. European Child and Adolescent Psychiatry. 2016;25(1):49–59. doi: 10.1007/s00787-015-0695-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thomson P., Jaque S.V. Adverse childhood experiences (ACE) and adult attachment interview (AAI) in a non-clinical population. Child Abuse and Neglect. 2017;70:255–263. doi: 10.1016/j.chiabu.2017.06.001. [DOI] [PubMed] [Google Scholar]
- Vai B., Riberto M., Ghiglino D., Bollettini I., Falini A., Benedetti F., Poletti S. Mild adverse childhood experiences increase neural efficacy during affective theory of mind. Stress. 2018;21(1):84–89. doi: 10.1080/10253890.2017.1398231. [DOI] [PubMed] [Google Scholar]
- van der Feltz-Cornelis C.M., Potters E.C., van Dam A., Koorndijk R.P.M., Elfeddali I., van Eck van der Sluijs J.F. Adverse Childhood Experiences (ACE) in outpatients with anxiety and depressive disorders and their association with psychiatric and somatic comorbidity and revictimization. Cross-sectional observational study. Journal of Affective Disorders. 2019;246:458–464. doi: 10.1016/j.jad.2018.12.096. [DOI] [PubMed] [Google Scholar]
- van Hoof M.J., Riem M., Garrett A., Pannekoek N., van der Wee N., van IJzendoorn M., Vermeiren R. Unresolved–disorganized attachment is associated with smaller hippocampus and increased functional connectivity beyond psychopathology. Journal of Traumatic Stress. 2019;32(5):742–752. doi: 10.1002/jts.22432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van IJzendoorn M.H., Bakermans-Kranenburg M.J., Duschinsky R., Fox N.A., Goldman P.S., Gunnar M.R.…Sonuga-Barke E.J.S. Institutionalisation and deinstitutionalisation of children 1: A systematic and integrative review of evidence regarding effects on development. The Lancet Psychiatry. 2020 doi: 10.1016/S2215-0366(19)30399-2. [DOI] [PubMed] [Google Scholar]
- Walsh D., McCartney G., Smith M., Armour G. Relationship between childhood socioeconomic position and adverse childhood experiences (ACEs): A systematic review. Journal of Epidemiology and Community Health. 2019;73(December):1087–1093. doi: 10.1136/jech-2019-212738. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weathers F.W., Litz B.T., Keane T.M., Palmieri P.A., Marx B.P., Schnurr P.P. The PTSD checklist for DSM-5 (PCL-5) National Center for PTSD. 2013;5(August) doi: 10.1037/t02622-000. 2002. [DOI] [Google Scholar]
- Wei W., Yu X. China: Adverse childhood experience as a risk factor for adolescent pregnancy. Adolescence and Sexuality: International Perspectives. 2014:103–115. [Google Scholar]
- Wong J.Y.H., Fong D.Y.T., Chan K.K.W. Anxiety and insomnia as modifiable risk factors for somatic symptoms in Chinese: A general population-based study. Quality of Life Research. 2015;24(10):2493–2498. doi: 10.1007/s11136-015-0984-9. [DOI] [PubMed] [Google Scholar]
- World Health Organization . 2016. Adverse childhood experiences international questionnaire (ACE-IQ)http://www.who.int/violence_injury_prevention/violence/activities/adverse_childhood_experiences/en/ Retrieved from. [Google Scholar]
- World Health Organization . World Health Organization; 2020. Mental health and psychosocial considerations during COVID-19 outbreak; pp. 1–6. (January) [Google Scholar]
- Xiao Q., Dong M.X., Yao J., Li W.X., Ye D.Q. Parental alcoholism, adverse childhood experiences, and later risk of personal alcohol abuse among Chinese medical students. Biomedical and Environmental Sciences. 2008;21(5):411–419. doi: 10.1016/S0895-3988(08)60062-8. [DOI] [PubMed] [Google Scholar]
- Xie X., Xue Q., Zhou Y., Zhu K., Liu Q., Zhang J., Song R. Mental Health Status among Children in Home Confinement during the Coronavirus Disease 2019 Outbreak in Hubei Province, China. JAMA Pediatrics. 2020 doi: 10.1001/jamapediatrics.2020.1619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang L., Fang J., Wan Y., Gong C., Su P., Tao F., Sun Y. The patterns of adverse childhood experiences among Chinese children: Four-year longitudinal associations with psychopathological symptoms. Journal of Psychiatric Research. 2020;122:1–8. doi: 10.1016/j.jpsychires.2019.12.009. [DOI] [PubMed] [Google Scholar]
- Zhang Z., Ran M.S., Li Y.H., Ou G.J., Gong R.R., Li R.H.…Fang D.Z. Prevalence of post-traumatic stress disorder among adolescents after the Wenchuan earthquake in China. Psychological Medicine. 2012;42(8):1687–1693. doi: 10.1017/S0033291711002844. [DOI] [PubMed] [Google Scholar]
- Zhou X., Xu Q., Inglés C.J., Hidalgo M.D., La Greca A.M. Reliability and validity of the chinese version of the social anxiety scale for adolescents. Child Psychiatry and Human Development. 2008;39(2):185–200. doi: 10.1007/s10578-007-0079-0. [DOI] [PubMed] [Google Scholar]
- Zung W.W.K. A rating instrument for anxiety disorders. Psychosomatics. 1971;12(6):371–379. doi: 10.1016/S0033-3182(71)71479-0. [DOI] [PubMed] [Google Scholar]
- Zuroff D.C., Santor D.A., Mongrain M. Conceptualizing and measuring personality vulnerability to depression: Comment on Coyne and Whiffen (1995) Psychological Bulletin. 2004;130(May):489–511. doi: 10.1037/0033-2909.130.3.489. [DOI] [PubMed] [Google Scholar]