Abstract
Background:
The optimal treatment for symptomatic, nontraumatic rotator cuff tear is unknown. The primary aim of this randomized controlled trial is to compare functional improvement after surgical and conservative treatment of nontraumatic rotator cuff tears.
Methods:
This is a single-centre, randomized clinical trial with a follow-up of 12 months. Patients older than 18 years with magnetic resonance imaging – confirmed nontraumatic rotator cuff tears that are suitable for either surgery or nonsurgery treatment is enrolled. The primary outcome is Constant score. Secondary outcome measures include visual analog scale (VAS) score, patient satisfaction, and American Shoulder and Elbow Surgeons (ASES) score. All scores are assessed by an independent observer who is blinded to the allocation of groups.
Results:
The study will provide much needed data on surgical vs nonsurgical treatment for nontraumatic rotator cuff tears. Results of this study may help patients, clinicians, and policy makers assess the pivotal question on comparative effectiveness of surgery vs nonsurgical for rotator cuff tears.
Trial registration:
This study protocol was registered in Research Registry (researchregistry5442).
Keywords: nonsurgery, nontraumatic rotator cuff tear, randomized controlled trial, study protocol, surgery
1. Introduction
Rotator cuff tear is a common shoulder disorder that lacks a consensus treatment algorithm. It is present in 20% to 54% of persons aged between 60 and 80 years.[1] It has been estimated that rotator cuff tear accounts for 4.5 million patient visits per year and a $3 to $5 billion annual economic burden in the U.S.[2] With increases in the number of physically active aging persons, rotator cuff disease is quickly becoming a major medical and economic burden.
Despite this wide prevalence, controversy exists over the optimal treatment. Nonoperative treatment and surgery are offered to patients with rotator cuff tears with good outcomes for both.[3] However, the evidence base to support surgical versus nonsurgical treatment is quite small and conflicting. Those who favor surgical repair worry that tear progression over time will lead to increased disability with conservative treatment of full-thickness tears.[4] The rotator cuff has limited capabilities for healing without repair, yet conservative treatment often yields an acceptable outcome. Recently, 3 recent prospective randomized controlled trials have compared operative repair to nonoperative treatment in older patients with chronic, degenerative tears of the rotator cuff.[5–7] These studies have generally shown small, nonsignificant differences in favour of surgical repair, and have been unable to provide clear conclusions regarding the preferred treatment. These conflicting results can make decision making regarding the optimal treatment for rotator cuff tears difficult.
The paucity of evidence for operative vs nonoperative treatments for rotator cuff tears is highlighted in the 2012 American Academy of Orthopedic Surgeons Clinical Practice Guidelines, Cochrane reviews, a report by the Agency for Health care Research and Quality, and expert reviews. Thus, a well-conducted randomized clinical trial with an adequate sample size is urgently needed. We undertake a randomized controlled trial to compare outcomes in patients who undertake surgical or nonsurgical treatment for nontraumatic rotator cuff tears. We hypothesize that surgical repair and conservative treatment of nontraumatic rotator cuff tears provide comparable outcomes. Our primary aim is to compare functional outcome after surgical and conservative treatment.
2. Materials and methods
This study is performed and reported in accordance with the principles of the Declaration of Helsinki (2000). This study design is a prospective, surgeon- and observer-blinded, randomized controlled trial. Research Ethics Board approval was obtained by the Institutional Review Board in our hospital (JN200213). The study was registered in the Research Registry (researchregistry5442). After written informed consent, all patients are randomized into a surgical and a nonsurgical group.
2.1. Patients
Patients with degenerative, nontraumatic full-thickness rotator cuff tears are included in this study from May 2020 to December 2021. Patients should be over 18 years old and can cooperate with us for treatment and postoperative observation. Exclusion criteria are traumatic onset of complaints, previous surgical treatment of the shoulder, frozen shoulder, radiologic and symptomatic osteoarthritis of the glenohumeral or acromioclavicular joint, arthritis/rheumatoid arthritis, diabetes mellitus, cognitive disorders, neurologic disease affecting function of the upper extremity, and language barriers impairing participation (Fig. 1).
Figure 1.
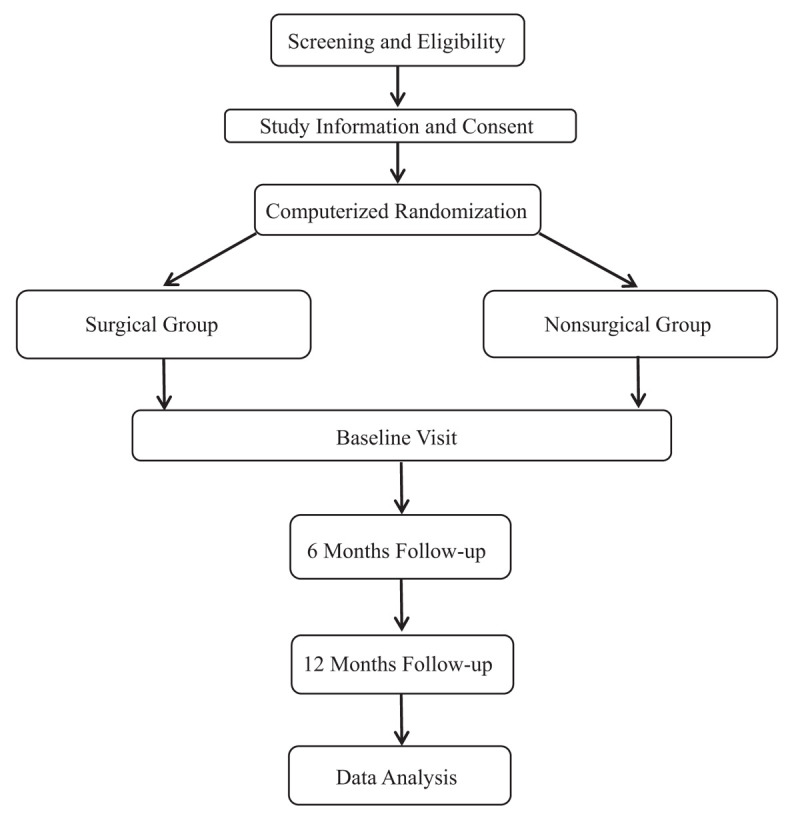
Flow diagram of the study.
2.2. Randomization
All patients who met these criteria during the enrollment period are approached about enrollment during a preoperative visit. A computer-generated randomization table is used for patient allocation to 1 of the 2 study groups: the surgical group or the nonsurgical group. Each time a patient is included in the trial, the generated randomized number is assigned accordingly. The randomization assignments are placed in opaque envelopes by research coordinators and then opened after patient enrollment. All staff, including surgeons, nurses and anesthesia staff, are blinded to the contents of the envelope prior to opening, so that patient enrollment cannot be based on group assignment. Demographic information is presented in Table 1.
Table 1.
Patient baseline demographics.
2.3. Interventions
2.3.1. Surgical group
Procedures in the surgery group are performed by 2 qualified and experienced surgeons. Surgery is scheduled within 6 weeks of inclusion and is done with the patient under general anesthesia, supplement with an interscalene brachial plexus block. The operation is performed in beach chair position using an anterolateral miniopen approach. The coracoacromial ligament is detached from its insertion, and the subacromial bursa is excised. The anteroinferior part of the acromion is removed. The footprint of the rotator cuff on the greater tuberosity is debrided, and a bleeding bony bed is created. Side-to-side repair and repair augmented with bone anchors are performed depending on the shape of the rupture. The deltoid muscle is reattached to the acromion by transosseous refixation.
2.3.2. Nonsurgical group
Treatment in the nonsurgical group consists of subacromial steroid infiltration, physiotherapy, and analgesic medication. After inclusion, patients are given an infiltration in the subacromial space by a posterior approach. If the first infiltration gives no pain relief, a second infiltration will be performed under radiologic or ultrasound guidance. The number of subacromial infiltrations is limited to a maximum of 3. Further conservative treatment options consist of analgesic medication with nonsteroidal anti-inflammatory drugs, paracetamol, or tramadol.
2.4. Outcome evaluation
Outcome was assessed in both study groups at 6 and 12 months postoperatively. The Constant score was used as the primary outcome measure. It is a shoulder-specific outcome instrument. Its inter-observer reliability was established in the original paper and a more complete assessment of its reliability in patients with shoulder pathology has been performed by Conboy et al.[8] The system uses a combination of subjective and examiner-derived components to assess shoulder function. A maximal score of 100 points is achievable.
Secondary outcome measures include visual analog scale (VAS) score, patient satisfaction, and American Shoulder and Elbow Surgeons (ASES) score. Pain was evaluated on a VAS with 0 = no pain, and 100 = worst imaginable pain. At the control visits, patients were also asked to grade whether the shoulder was better or worse compared with its preoperative state and if the patients were satisfied or dissatisfied with the treatment outcome. Satisfaction levels are rated using a 100 mm horizontal VAS, for which 0 mm represent completely dissatisfied and 100 mm represent completely satisfied. The self-report section of the ASES score consists of parts for pain and shoulder function, each contributing 50 points to a maximum score of 100. The system's validity, reliability, and responsiveness have been demonstrated.
2.5. Statistical analysis
Statistical analyses are conducted using SPSS v22.0 software (IBM, Chicago, IL). All patients in the study are analyzed on the basis of an intention-to-treat principle. This means that for patients in the nonsurgical group who changed treatment, the final score before secondary surgery is carried forward to the 6- and 12-month analyses. Patient characteristics at baseline are compared between groups by t tests, chi-squared tests and Mann–Whitney U tests. Testing of our null hypothesis (no difference in treatment benefit between groups) is performed by a linear mixed model with an unstructured covariance matrix. The time of follow-up and choice of treatment are used as categorical variables, and an interaction term between time and treatment is included.
2.6. Power analysis
With regard to the sample size calculations, the power calculations are based on the assumed changes in the Constant score. On the basis of previous study, the mean score at baseline is assumed to be 50 ± 10 points. At the time of 1-year follow-up, the score is assumed to be 70 points in the best treatment group and 60 points in the worst treatment group. The mean correlation between the measurements during the follow-up is assumed to be 0.40 to 0.50 and the standard deviation of the measurements is assumed to be 20. In an analysis of variance (ANOVA) test with an alpha of 0.05 and a power of 85%, we expect the findings to be significant if the number of subjects per group is 51. Significance is set at P < .05. The drop-out rate is assumed to be 15%, and thus the number of subjects per group was 60.
3. Discussion
Which patients with rotator cuff tears should have surgical treatment and which should have physiotherapy remains unclear. Early surgical repair is essential for younger, active patients with acute tears, and severe functional deficit.[9–11] In other cases, however, surgery is not indicated and nonoperative treatment may be recommended.[12] This has the advantage of less treatment-related morbidity, but should only be preferred if the short- and long-term results are comparable to those of surgical repair.
Earlier studies regarding either tendon repair or physiotherapy have shown benefit for both approaches.[13–15] However, the studies are difficult to compare because of differing study populations, methods of treatment and evaluation, and periods of follow-up. Most studies of nonoperative treatment are retrospective, present pre-selected groups, and exclude from analysis those patients who were operated upon after failed conservative treatment, the effect of which may have been overestimated.[16,17] This randomized controlled trial is designed to compare outcomes after surgical or nonsurgical treatment of nontraumatic rotator cuff tears.
This trial has some limitations. The results of this study need to be viewed in light of certain limitations. Most importantly, our sample size was small, with 120 patients. Inclusion of patients in this trial may be difficult because most patients have already received conservative treatment or are specifically referred for surgical treatment. Second, the subjects may be exclusively Chinese. Therefore, the data from this clinical trial cannot be applied to other ethnic groups. A third limitation of this study is the follow-up period of only 1 year. Further follow-up is necessary and is underway. However, the study will provide much needed data on surgical vs nonsurgical treatment for nontraumatic rotator cuff tears. Results of this study may help patients, clinicians, and policy makers assess the pivotal question on comparative effectiveness of surgery vs nonsurgical for rotator cuff tears.
Author contributions
Ding-gen Huang and Ya-li Wu conceived, designed, and planed the study. Ding-gen Huang, Peng-fei Chen, and Ya-li Wu are recruiting the study participants and performing the interventions. Cui-lan Xia and Ze-jin Lin supervised the study. Ding-gen Huang, Ya-li Wu, and Jin-qi Song will interpret and analyze the data. Jin-qi Song drafted the manuscript. Jin-qi Song critically revised the manuscript for important intellectual content. All authors have full access to the manuscript and take responsibility for the study design. All authors have approved the manuscript and agree with submission.
Footnotes
Abbreviations: ASES = American Shoulder and Elbow Surgeons, VAS = visual analog scale.
How to cite this article: Huang Dg, Wu Yl, Chen Pf, Xia Cl, Lin Zj, Song Jq. Surgical or nonsurgical treatment for nontraumatic rotator cuff tears: Study protocol clinical trial. Medicine. 2020;99:18(e20027).
This study is supported by National Health Commission of Shenzhen (2017039).
The authors have no conflicts of interest to disclose.
Data sharing not applicable to this article as no datasets were generated or analyzed during the current study.
References
- [1].Li S, Sun H, Luo X, et al. The clinical effect of rehabilitation following arthroscopic rotator cuff repair: a meta-analysis of early versus delayed passive motion. Medicine (Baltimore) 2018;97:e9625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2].Boileau P, Brassart N, Watkinson DJ, et al. Arthroscopic repair of full-thickness tears of the supraspinatus: does the tendon really heal? J Bone Joint Surg Am 2005;87:1229–40. [DOI] [PubMed] [Google Scholar]
- [3].Fuchs B, Gilbart MK, Hodler J, et al. Clinical and structural results of open repair of an isolated one-tendon tear of the rotator cuff. J Bone Joint Surg Am 2006;88:309–16. [DOI] [PubMed] [Google Scholar]
- [4].Huijsmans PE, Pritchard MP, Berghs BM, et al. Arthroscopic rotator cuff repair with double-row fixation. J Bone Joint Surg Am 2007;89:1248–57. [DOI] [PubMed] [Google Scholar]
- [5].Kukkonen J, Joukainen A, Lehtinen J, et al. Treatment of non-traumatic rotator cuff tears: a randomised controlled trial with one-year clinical results. Bone Joint J 2014;96-B:75–81. [DOI] [PubMed] [Google Scholar]
- [6].Lambers Heerspink FO, van Raay JJ, Koorevaar RC, et al. Comparing surgical repair with conservative treatment for degenerative rotator cuff tears: a randomized controlled trial. J Shoulder Elbow Surg 2015;24:1274–81. [DOI] [PubMed] [Google Scholar]
- [7].Moosmayer S, Lund G, Seljom U, et al. Comparison between surgery and physiotherapy in the treatment of small and medium-sized tears of the rotator cuff: a randomised controlled study of 103 patients with one-year follow-up. J Bone Joint Surg Br 2010;92-B:83–91. [DOI] [PubMed] [Google Scholar]
- [8].Conboy VB, Morris RW, Kiss J, et al. An evaluation of the Constant-Murley shoulder assessment. J Bone Joint Surg Br 1996;78-B:229–32. [PubMed] [Google Scholar]
- [9].van Kampen DA, van Beers LW, Scholtes VA, et al. Validation of the Dutch version of the Simple Shoulder Test. J Shoulder Elbow Surg 2012;21:808–14. [DOI] [PubMed] [Google Scholar]
- [10].Moosmayer S, Lund G, Seljom US, et al. Tendon repair compared with physiotherapy in the treatment of rotator cuff tears: a randomized controlled study in 103 cases with a five-year follow-up. J Bone Joint Surg Am 2014;96:1504–14. [DOI] [PubMed] [Google Scholar]
- [11].Teng A, Liu F, Zhou D, et al. Effectiveness of 3-dimensional shoulder ultrasound in the diagnosis of rotator cuff tears: a meta-analysis. Medicine (Baltimore) 2018;97:e12405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Nho SJ, Shindle MK, Adler RS, et al. Prospective analysis of arthroscopic rotator cuff repair: subgroup analysis. J Shoulder Elbow Surg 2009;18:697–704. [DOI] [PubMed] [Google Scholar]
- [13].Zhang T, Duan Y, Chen J, et al. Efficacy of ultrasound-guided percutaneous lavage for rotator cuff calcific tendinopathy: a systematic review and meta-analysis. Medicine (Baltimore) 2019;98:e15552. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Koubaa S, Ben Salah FZ, Lebib S, et al. Conservative management of full-thickness rotator cuff tears. A prospective study of 24 patients. Ann Readapt Med Phys 2006;49:62–7. [DOI] [PubMed] [Google Scholar]
- [15].Kukkonen J, Kauko T, Vahlberg T, et al. Investigating minimal clinically important difference for Constant score in patients undergoing rotator cuff surgery. J Shoulder Elbow Surg 2013;22:1650–5. [DOI] [PubMed] [Google Scholar]
- [16].Lambers Heerspink FO, Dorrestijn O, van Raay JJ, et al. Specific patient-related prognostic factors for rotator cuff repair: a systematic review. J Shoulder Elbow Surg 2014;23:1073–80. [DOI] [PubMed] [Google Scholar]
- [17].Levy O, Venkateswaran B, Even T, et al. Mid-term clinical and sonographic outcome of arthroscopic repair of the rotator cuff. J Bone Joint Surg Br 2008;90:1341–7. [DOI] [PubMed] [Google Scholar]


