Supplemental Digital Content is available in the text
Keywords: long birth interval, Short birth interval, sub-Saharan Africa
Abstract
Optimal birth spacing (defined as a birth spacing of 24–59 months) is incontrovertibly linked to better health outcomes for both mothers and babies. Using the most recent available Demographic and Health Survey data, we examined the patterns and determinants of short and long birth intervals among women in selected sub-Saharan African (SSA) countries.
Reproductive health and sociodemographic data of 98,934 women from 8 SSA countries were analyzed. Unadjusted and adjusted multinomial logistic regression models were used to examine the net relationship between all the independent variables and short and long birth intervals.
Overall, the majority of women in all the countries optimally spaced births. However, a significant proportion of women had short birth intervals in Chad (30.2%) and the Democratic Republic of Congo (Congo DRC) (27.1%). Long birth spacing was more common in Eastern and Southern African countries, with Zimbabwe having the highest rate of long term birth interval (27.0%). Women who were aged 35 years and above in Uganda (RRR = 0.72, CI = 0.60–0.87), Tanzania (RRR = 0.62, CI = 0.49–0.77), Zimbabwe (RRR = 0.52, CI = 0.31–0.85), Nigeria (RRR = 0.82, CI = 0.72–0.94) and Togo (RRR = 0.67, CI = 0.46–0.96) had significantly lower odds of having short birth intervals compared to women aged 15–24 years. Older women (above 34 years) had increased odds for long birth intervals in all countries studied (Chad (RRR = 1.44, CI = 1.18–1.76), Congo DRC (RRR = 1.73, CI = 1.33–2.15), Malawi (RRR = 1.54, CI = 1.23–1.94) Zimbabwe (RRR = 1.95, CI = 1.26–3.02), Nigeria (RRR = 1.85 CI = 1.56–2.20), Togo (RRR = 2.12, CI = 1.46–3.07), Uganda (RRR = 1.48, CI = 1.15–1.91), Tanzania RRR = 2.12, CI = 1.53–2.93).
The analysis suggested that the determinants of long and birth intervals differ and varies from country to country. The pattern of birth spacing found in this study appears to mirror the contraceptive use and fertility rate in the selected SSA countries. Birth intervals intervention addressing short birth intervals should target younger women in SSA, especially in Chad and Congo DRC, while intervention for long birth spacing should prioritize older, educated and wealthy women.
1. Introduction
Optimal birth spacing (defined as inter-birth interval length of 24–59 months) is incontrovertibly linked to better health outcomes for both mothers and babies.[1–4] There is a growing body of evidence associating short birth spacing (defined as inter-birth interval length of fewer than 24 months) with adverse maternal and child health outcomes.[1,3,5] Pregnancies that starts in less than 18 months after birth are linked with delayed prenatal care, increased risk of maternal mortality, and adverse birth outcomes, including miscarriages, preterm births, stillbirths, low birth weight, and neonatal morbidity.[6,7] Further, short birth spacing has longer-term effects on childhood nutrition status. Children that are spaced closely face the risk of under-nutrition and stunting. According to Gribble,[8] a birth spacing of fewer than 24 months is associated with increased odds of stunting. Short birth spacing suggests shorter breastfeeding duration, which indicates that the infant would miss out on the benefits of the WHO recommended two years of breastfeeding.[9–12] Consequently, the risk of dying and under-nutrition are higher among children that are spaced too closely.[13]
Likewise, long birth spacing (defined as inter-pregnancy interval greater than 60 months) is linked to adverse outcomes such as women's physiological regression, preterm birth, low birth-weight and an increased risk of labor dystocia and preeclampsia.[1,2,14] Very long birth interval (>75months) is linked to increased risk of maternal mortality.[7] Timæus and Moultrie[15] questioned whether very long birth interval should be viewed as “spacing” or “postponement”. They argued that a very long birth interval is not synonymous with birth spacing and should be considered to be birth postponement since the underlying reason for delaying subsequent birth for such a long interval might be unrelated to the age of the existing child. We posit that very long birth interval could be due to “birth postponement”, miscarriages, abortions and “secondary infertility”. It is also possible that women who delay or postpone having a subsequent birth for over 5 years got pregnant as teenagers or outside a committed relationship, which in most cases are unplanned pregnancy. As such, their subsequent births have nothing to do with the age of the existing child. While the proportion of women spacing births for over 5 years are increasing, the associated factors are less understood. This is important considering that very long birth interval is as deleterious as a short birth interval.
The affecting birth spacing could be categorized into two factors; “sociological” and “biological”.[16] The biological factors include differences in length of post-partum amenorrhea, pregnancy wastage and menstrual interval. According to Potter, variation in birth spacing is primarily determined by biological factors.[17] Lincoln and colleagues conducted a prospective study of birth spacing dynamics in rural Bangladesh and found that lengthy post-partum amenorrhea was primarily responsible for prolonged birth intervals and accounted for 45 percent of the variation in birth interval length.[16] The sociological factors affecting birth intervals included contraceptive use, breastfeeding length, the death of the previous child, gender of new-born, infrequent sex, and husband's occupation.[16,18–21] Baschieri and Hinde argued that birth intervals are determined mainly by the use of modern contraception.[22] However, the relationship between contraceptive use (both modern and traditional) and birth spacing is mixed.[23] While many studies reported that birth spacing is associated with contraceptive use,[24,25] some studies did not find such associations.[23] The socio-demographic factors which contribute to variation in birth spacing include; parity, age, residence type, wealth index, education, and religion.[16,18–21] The interaction between socio-demographic factors and birth spacing differ from society to society and change over time.
The deleterious consequences of long birth intervals are well known. Yet, recent evidence suggests an increasing trend towards longer inter-birth intervals in all regions of the world, and especially in sub-Saharan Africa (SSA).[26,27] Understanding the regional variation of long birth spacing and its demographic determinants could be crucial towards crafting policy that will address this phenomenon. This is currently missing in the literature. In addition, the determinants of short birth intervals are extensively documented in the literature; however, little is known about factors that determine long birth intervals. It is also unclear whether the factors that influence short birth intervals also influence long birth intervals in the SSA context. As such, we used the most recent demographic and health surveys to examine the patterns and the determinants of long and short birth intervals among childbearing women in 8 SSA countries.
2. Data and methods
The data for this present study was drawn from the Demographic and Health Survey (DHS) of eight purposively selected countries from the key regions of SSA. The choice was also informed by the availability of data in the past 5 years (from 2013–2018), geographical representation and variations in fertility and contraceptive prevalence rates. The child recode dataset of the following countries was used; Chad (2014–2015) and Congo DRC (2013–14) from the Central Africa region; Uganda (2016) and Tanzania (2015–16) from the East Africa region; Nigeria (2013) and Togo (2013–2014) from the West Africa region; and Malawi (2015–2016) and Zimbabwe (2015) from the Southern Africa region. To determine the proportion of women who had long, short and optimal birth spacing, only women who have had more than one birth are eligible. Women who had only one birth were dropped from the sample. The full analytic sample size has been presented in Supplementary Digital Content (Supplementary Digital Content, Table 1).
The DHS program is a nationally representative, cross-sectional survey that is collected every 5 years in participating countries. The child recode, which was used for this study, has one record for every child born in the 5 years preceding the survey of interviewed women. It contains the information relating to the mother's pregnancy, the child's delivery, postnatal care and immunization, among others. The data for the mothers of each of these children are included.
2.1. Outcome variable
The dependent variable for this study is birth spacing. This has been described as the duration between a preceding birth and index birth measured as the number of months between the birth of the child being studied and the immediately preceding child birth of the mother.[1,3,5] The objective of this study is to estimate the proportion of women who had short, optimal, and long birth spacing in the selected countries. This could only be achieved by focusing only on closed birth intervals. Although the limitations of using closed birth intervals have been well documented in demographic research,[15,27,28] there is public health and clinical relevance of studying the prevalence of short and long birth spacing. Although the World Health Organization (WHO) and other international organizations have suggested a waiting period of at least 2 to 3 years between pregnancies to reduce infant and child mortality, and also to benefit maternal health, recent studies supported by the United States Agency for International Development[29] have encouraged longer birth spacing, of 3 to 5 years, as possibly being more advantageous.[30] The variable measuring the self-reported length of time in months between the most recent birth (index birth) and the previous birth is continuous. This variable was based on the WHO and USAID definition of optimal birth spacing into: < 24 months “short birth spacing”, 24 to 60 months “optimal birth spacing” and >60 months “long birth spacing”. Optimal birth spacing was used as the reference interval for all analyses, based on previous literature reporting this interval as the best.
2.2. Independent variables
Based on the literature, we have included several covariates in our models that are likely to be associated with both short and long term birth intervals. The independent variables include age, sex of preceding child, survival of preceding birth, place of residence, marital status, educational level, employment status and wealth status, which is a proxy for household socioeconomic status captured through a wealth index based on household possessions and amenities. Detailed methodology on how the DHS constructs the wealth index has been discussed in the literature.[31] Age was defined as the age of the mother at the time of the index birth and was categorized as; “15 to 24”, “25 to 34” and “35+”. Due to the uncertainty associated with child survival in several countries in SSA, we controlled for sex and the survival of the preceding child. Educational attainment was classified as either no education, primary only, secondary and higher education. Employment status was categorized into women who were working and not working. The wealth quintile given in the DHS was regrouped into low (lowest and second quintiles), middle and high (fourth and highest quintiles) to examine the effect of socioeconomic status on the different birth intervals.
2.3. Statistical analysis
Three levels of analysis were employed in this paper, that is, univariate analysis, bivariate descriptive, unadjusted and adjusted multinomial logistic modeling. The univariate analysis presented the median birth-spacing according to socio-demographic characteristics. In the bivariate analysis, the percentage distributions of birth spacing were presented according to the selected demographic characteristics. Unadjusted and adjusted multinomial logistic regressions were then employed to examine the independent and net relationship between all the independent variables and the outcome variable due to the nature of the outcome.[32] The multinomial logistic regression was used because the outcome variable had three categories: < 24 months “short birth spacing”, 24 to 60 months “optimal birth spacing” and >60 months “long birth spacing”. Optimal birth spacing was used as the reference interval for all analyses. A P value < .05 was considered statistically significant. We used asterisk to indicate certain level of P value in tables as follows: ∗P < .05; ∗∗P < .01; ∗∗∗P < .001. Sampling weights were applied to adjust for differences in the probability of selection and to adjust for non-response in order to produce the proper representation. Individual weights were used for descriptive statistics in this study, using Stata 14 for Windows.
2.4. Ethical consideration
This study was exempted from ethical review by the committee because the study used deidentified publicly available datasets which are completely anonymous and do not contain any personal, confidential and identifying information or characteristics of the respondents. The study adhered to the ethical standards of the Helsinki Declaration by the World Medical Association. The DHS datasets can be downloaded online and are freely available for use by researchers upon request. In order to access the data from the website, a written request needed to be submitted to the measure DHS and permission was granted to use the data for this survey. Datasets are available from; https://dhsprogram.com/data/available-datasets.cfm.
3. Results
3.1. Descriptive results
Given that birth spacing length is not normally distributed, we estimated median birth spacing in place of mean birth spacing for all countries studied, and results were grouped by socio-demographic characteristics, the survival of preceding birth and sex of preceding birth (Table 1). The median birth spacing was highest in Malawi and Zimbabwe, but lowest in Chad and the Congo DRC. Women whose preceding child survived had higher median birth interval length compared those whose child did not survive. Women living in urban areas had higher median birth spacing length compared women residing in rural areas in all countries except in Chad and Congo DRC.
Table 1.
Median birth spacing by socio-demographic characteristics.
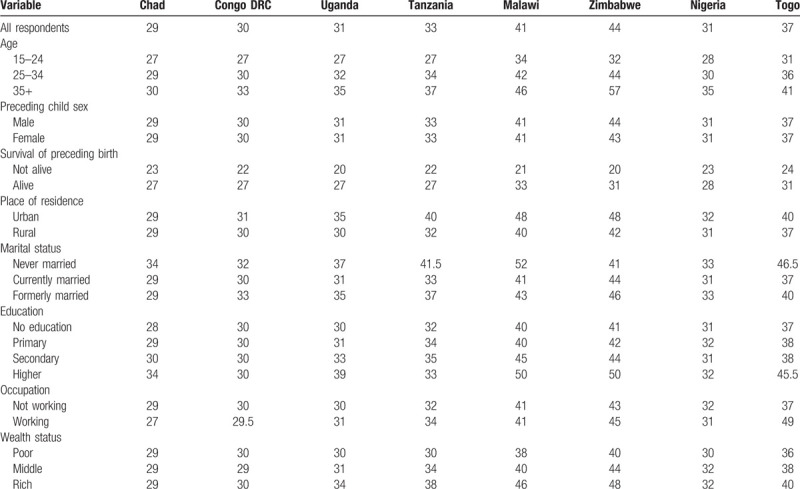
The median birth spacing of women is varied by age, education, and marital status. In all countries, women aged 35+ had higher median birth spacing length compared to women aged 15 to 24 years. For instance, the median birth spacing for women aged 35 and above was 57 months in Zimbabwe, compared to 32 months for their counterparts aged 15 to 24. Similar trends were seen in Tanzania (37 months for women aged 35+ vs 27 months for counterparts aged 15–24). The median birth spacing length was higher among never-married women compared to those currently married in all countries except in Zimbabwe. Median birth spacing was higher among women who had a higher education compared to women with no education in most of the countries studied. However, in Nigeria and Congo DRC, there was no difference in the median birth spacing of women by their educational status. In a number of the countries, the variations in the median birth spacing between women with secondary education and women with higher education were about 3 to 6 months.
3.2. Long and short birth spacing
We grouped the birth interval length into short, optimal and long and estimated the proportion of long, short and optimal birth spacing for all countries of interest. In all countries, the majority of women spaced their births optimally (see Supplementary Digital Content (Supplementary Digital Content, Table 2A–D). Nevertheless, the prevalence of short birth interval was highest in Chad (30.18%) and the Congo DRC (27.12%) (See Supplementary Digital Content, Table 2A). The prevalence of long-term birth spacing was highest among women in Zimbabwe (27%) (see Supplementary Digital Content, Table 2D) and lowest among women in Chad (6%). Percentage distribution of birth spacing differed by demographic characteristics in the different countries (see Supplementary Digital Content, Table 2A, 2B, 2C,2D). For example, there was a higher percentage of women aged 35 and above having short birth intervals in Central Africa (Chad 29.95%; Congo DRC 22.3%), compared to women in East Africa aged 35 and above (Uganda 18.8%, Tanzania 14.2%) (see Supplementary Digital Content Table 2B) and Southern Africa (Malawi 10.0%; Zimbabwe 6.7%). On the other hand, there were a higher proportion of women aged 35 and above having long birth intervals in Southern Africa (Malawi 31.6%; Zimbabwe 44.7%) compared to Western Africa (Nigeria 16.1%; Togo 22.98%) and Central Africa (Chad 9.2%; Congo DRC 14.1%). More women who were working in Eastern (Uganda 11.2%, Tanzania 17.8%) and Southern Africa (Zimbabwe 29.5%, Malawi 20.9%) had long birth intervals, compared working women in Central Africa (Chad 6.1%, Congo DRC 8.2%).
3.3. Determinants of short birth intervals
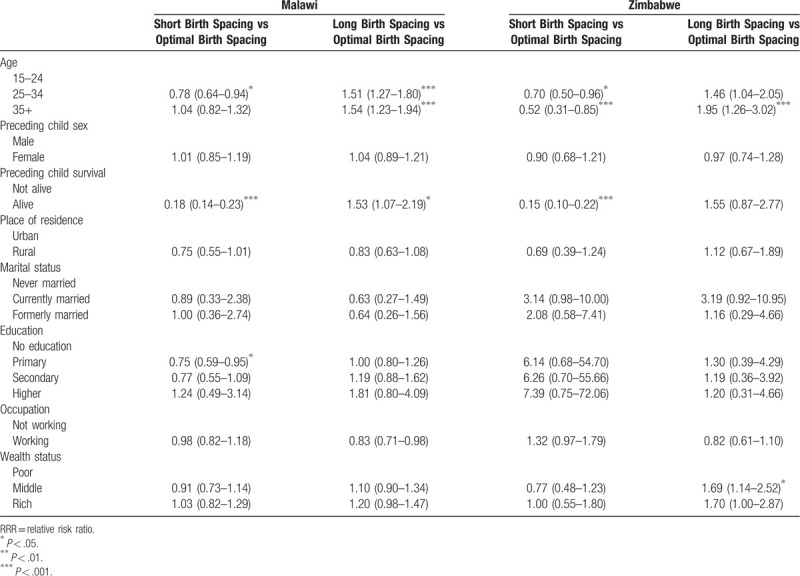
To examine the determinants of short birth intervals, we fitted both unadjusted and adjusted multinomial logistic regression models. The results of the unadjusted models are displayed in Tables 2–5, while the results of the adjusted model are presented in Tables 6–9. Age 35 years above, the survival of the preceding child, urban residence, higher education, and belonging to the rich quintile was significantly and independently associated with lower odds of short birth spacing among women in most of the countries. The direction of effect and the magnitude of effect remain in the adjusted model. Women who were 35 years and above in Uganda (RRR = 0.72, CI = 0.60–0.87), Tanzania (RRR = 0.62, CI = 0.49–0.77), Zimbabwe (RRR = 0.52, CI = 0.31–0.85), Nigeria (RRR = 0.82, CI = 0.72–0.94) and Togo (RRR = 0.67, CI = 0.46–0.96) had significantly lower odds of having short birth intervals compared to women aged 15 to 24 years. In all of the study countries, the survival of a preceding child was negatively associated with short birth intervals. However, there was no significant association between place of residence and short birth intervals except in Tanzania, where women in rural areas had significantly higher odds of having short birth intervals.
Table 2.
Unadjusted relative risks of association between selected characteristics, and birth spacing among women in Central Africa.
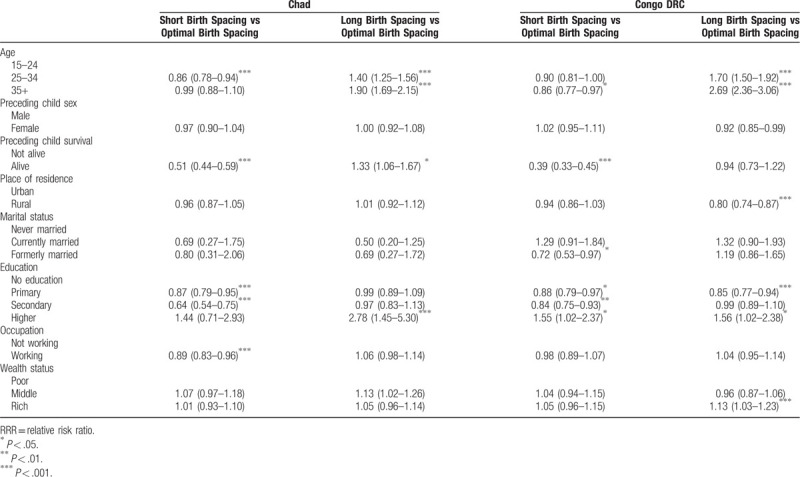
Table 5.
Unadjusted relative risks of association between contraceptive use, selected characteristics, and birth spacing among women in West Africa.
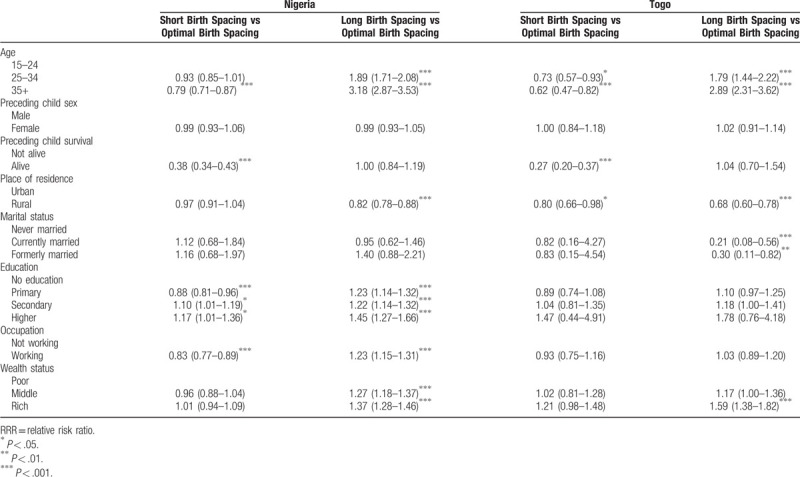
Table 6.
Adjusted Relative Risks of Association between Selected Characteristics, and Birth Spacing Among Women in Central Africa.
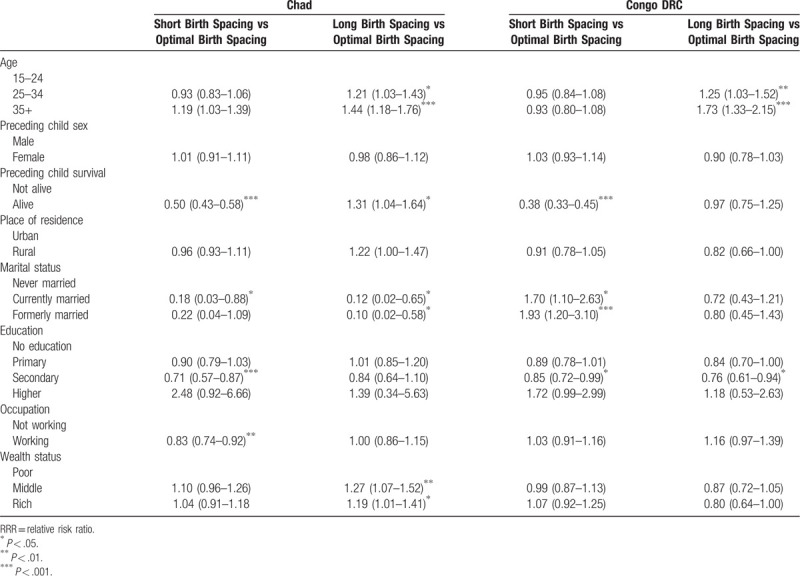
Table 9.
Adjusted relative risks of association between contraceptive use, selected characteristics, and birth spacing among women in West Africa.
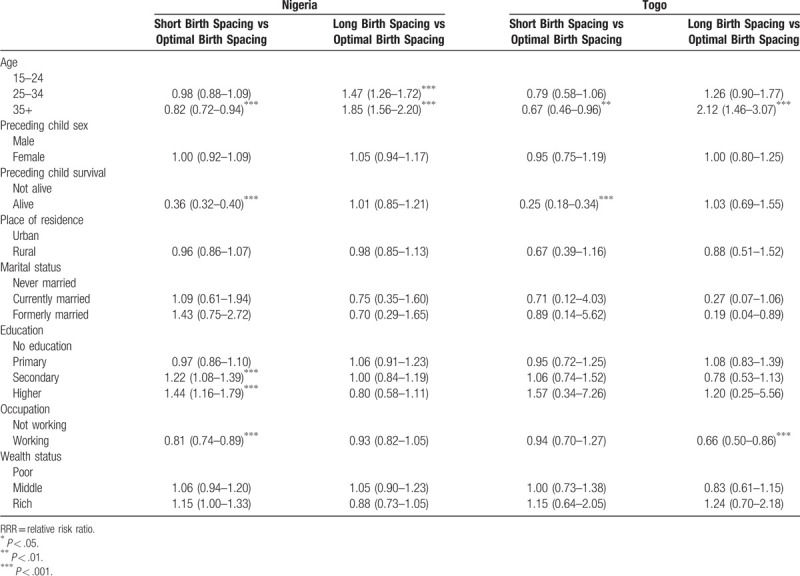
Table 3.
Unadjusted relative risks of association between selected characteristics, and birth spacing among women in East Africa.
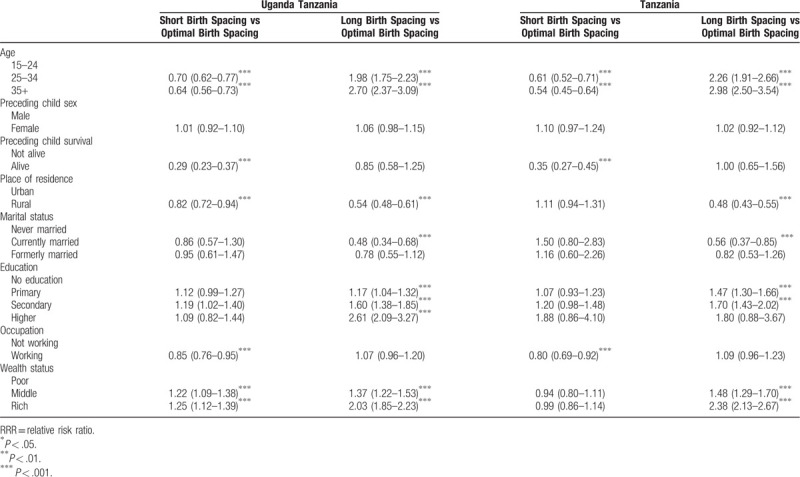
Table 4.
Unadjusted relative risks of association between selected characteristics, and birth spacing among women in Southern Africa.
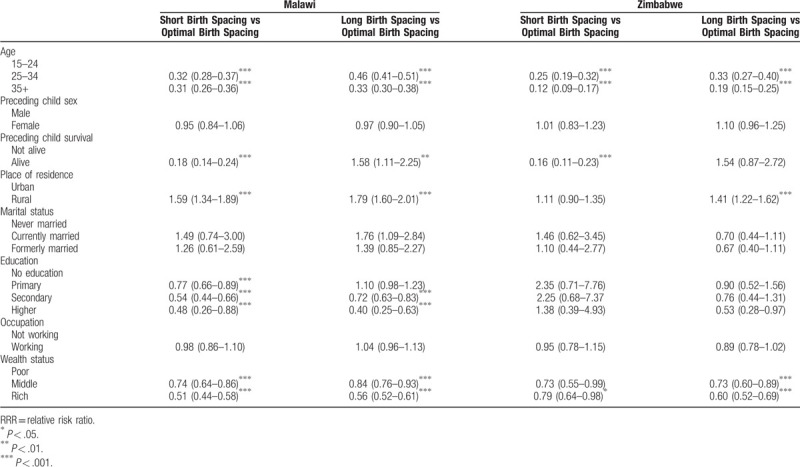
Table 7.
Adjusted relative risks of association between selected characteristics, and birth spacing among women in Eastern Africa.
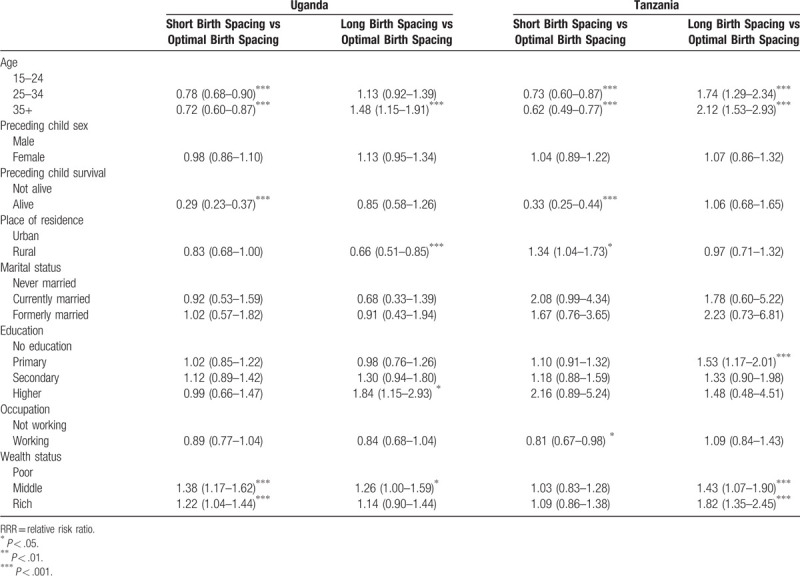
Table 8.
Adjusted relative risks of association between selected characteristics, and birth spacing among women in Southern Africa.
The findings on the association between education and birth spacing are mixed. There was no association between education and short birth spacing in Uganda, Tanzania, Togo, and Zimbabwe. However, in Nigeria, women with higher education (RRR = 1.44, CI = 1.16–1.79), and secondary education (RRR = 1.22, CI = 1.08–1.39) had significantly higher odds of having short birth intervals compared to women with no formal education. Compared to women who had no formal education, women who had secondary education had lower odds of having short birth spacing in Chad and Congo DRC. Women in Malawi (RRR = 0.75, CI = 0.59–0.95) with primary education had lower odds of having short birth intervals compared to their counterparts with no education.
Also, women who were working in Chad (RRR = 0.83, CI = 0.74–0.92) Tanzania (RRR = 0.81, CI = 0.67–0.98), and Nigeria (RRR = 0.81, CI = 0.74–0.89) had lower odds of having short birth intervals. Finally, women in the rich quintile had significantly higher odds of having short intervals in Uganda (RRR = 1.22, CI = 1.04–1.44).
Being married is associated with lesser odds of having short birth spacing in Chad while higher odds were observed in Congo DRC.
3.4. Determinants of long birth intervals
The adjusted and unadjusted multinomial regression models were used to examine the determinants of long birth intervals in all countries selected. The results are presented in Tables 2–9. The results of the unadjusted model indicate that age 35 and above, higher education, being employed and living in urban areas were associated with higher odds of having long birth spacing (P < .05). The results of the adjusted model were mixed in all countries studied. While older age is associated with long birth interval for all countries (P < .05), the survival of the preceding child was associated with long birth interval only in Chad (RRR = 1.31, CI = 1.04–1.64, P < .05) and Malawi (RRR = 1.53, CI = 1.07–2.19, P < .05). Also, sex of preceding child and work status were not significantly associated with long birth spacing in all countries studied. Similarly, place of residence was not significantly associated with long birth spacing in all selected countries except for Uganda (RRR = 0.66, CI = 0.51–0.85, P < .05). Women who were currently married had lower odds of having long birth intervals in Chad (RRR = 0.12, CI = 0.02–0.65, P < .05).
The findings on the association between women's education and long birth spacing are mixed. Education did not significantly influence long birth spacing in Chad, Malawi, Zimbabwe, Nigeria, and Togo. However, women who had secondary education in Congo DRC (RRR = 0.76, CI = 0.61–0.94, P < .05) had lower odds of having long birth intervals compared to their counterparts with no education. In contrast, women with tertiary education (RRR = 1.84, CI = 1.15–2.93, P < .05) were significantly more likely to have longer birth intervals compared to their counterparts with no formal education in Uganda while women with primary education (RRR = 1.53, CI = 1.17–2.01, P < .05) were significantly more likely to have longer birth intervals compared to their counterparts with no formal education in Tanzania.
Lastly, wealth status was not significantly associated with long birth spacing in Congo DRC, Nigeria, Togo and Malawi (P > .05). However, the wealth status increases the odds of having long birth spacing in Chad, Zimbabwe, Tanzania and Uganda. Women in the rich quintile in Tanzania (RRR = 1.82, CI = 1.35–2.45, P < .05), Chad (RRR = 1.19, CI = 1.01–1.41, P < .05) had significantly higher odds of having long birth intervals compared to women in the poorest quintile. In Uganda (RRR = 1.26, CI = 1.00–1.59, P < .05) and Zimbabwe (RRR = 1.69, CI = 1.14–2.52, P < .05), women in the middle-income quintile had higher odds of having a long birth spacing compared to those in the poorest quintile.
4. Discussion
This study examined the patterns of birth spacing and the determinants of long and short birth intervals among childbearing women in eight purposively selected SSA countries. We found a wide variation in the length of birth intervals among the countries. The median birth spacing length was significantly shorter in Western and Central Africa countries when compared to Eastern and Southern African countries. Overall, the majority of women optimally spaced births in all countries. However, the prevalence of short birth spacing was highest in Chad and the Congo DRC. Short birth spacing is common in these two countries and considering its associated adverse effects,[1–4] there is a need for intervention. Long birth interval, which is also associated with adverse maternal health outcomes,[1–3,7] is more common in Eastern and South African countries than other regions of SSA.
The determinants of long and short birth intervals varied from country to country. Some factors which influenced short birth spacing did not influence long birth spacing. This finding corroborates Timæus and Moultrie[15] assertion that very long birth interval is not synonymous with birth spacing and should be viewed as birth postponement since the underlying reason for delaying subsequent birth for such a long interval might be unrelated to the age of the existing child. Based on the findings of this study, it is clear that the factors that determine short birth spacing differ from those that influence long birth spacing. This study reveals that median birth interval length is longer among never-married women. It could be that women who experienced long birth interval purposely chose to postpone birth or they experienced secondary infertility. In contrast, most women who spaced birth closely have been reported to have experienced an unplanned pregnancy.[33]
Our study shows that age is an important determinant of both short and long birth intervals in all sub-Saharan countries. The finding that younger age is associated with short birth spacing is consistent with the literature.[20,21] Younger women tend to have shorter birth intervals, while older women are more prone to long birth intervals. The plausible explanation for this could be as a result of the difference in contraceptive use. There is an array of evidence showing that older women are more likely to use contraceptives compared to younger women.[34–36] There is also evidence that younger women are more likely to experience unplanned pregnancy compared to older women.[37] Studies have shown that older age is associated with fertility decline, increased time to conception and risk of spontaneous miscarriage.[38,39] All these could explain why longer birth intervals are prevalent in older age. It is also possible that older women are postponing births or experiencing an unplanned pregnancy after deciding to limit births. It could also be that women, with increasing age, understand better ways of achieving birth spacing.
Survival of the preceding child was associated with the decreased rate of short birth spacing in all countries studied but was not associated with long birth spacing. Our finding on the relationship between survival of preceding child and short birth spacing is consistent with previous studies.[16,18–21] The reason why women whose preceding child died have short birth spacing is apparent; however, what is less understood is whether their risk for adverse pregnancy outcomes is the same as those whose baby survived. While most births that are closely spaced reflect unplanned pregnancies, this is not the case among women whose preceding child had died.[33,40] Rather women whose prior child died may have more reason to become pregnant quickly and not wait for 2 years before having another child. It is unclear whether the elevated risks among women who spaced birth closely are due to women's bodies not having time to recover if they conceive soon after delivery or to factors associated with unplanned pregnancies such as delayed access to antenatal care.[40]
Our findings on the relationship between maternal education and long and short birth intervals are mixed. While women with higher education were more likely to have short birth spacing in Nigeria, this was not the case in other SSA countries included in this study. The Nigeria result is consistent with a study in India which found that higher maternal education was positively linked with short birth intervals.[21] Also, a study conducted in the United States shows that affluent women appear to deliberately spaced births closely.[41] Education is one of the reasons women delay childbearing. The Nigeria result is, however, not the norm in SSA given the results of other countries. Unlike the relationship between maternal education and short birth spacing, the findings on the link between education and long birth spacing are more consistent and show that education is positively associated with long birth spacing across countries in SSA. Women who are educated are more likely to favor long birth interval compare to those who are uneducated. This is not surprising given that educated women are more knowledgeable about contraceptives compared to uneducated women, which will help them to avoid unplanned pregnancy.
In contrast to previous studies in India and Nigeria,[42,43] our study did not find a significant association between sex of the preceding child and short birth spacing. One plausible explanation for this is that other factors, such as access to contraceptive, education, and survival of the preceding child, are more important determinants of short birth spacing than the sex of the preceding child. In patriarchal societies, the desire for a male child may make women with only female children to have a short birth interval. However, the overall effect of this compared to other factors seem negligible compared to proximate determinants of birth spacing.
Our study also showed that women in the rich quintile in Chad and Tanzania had significantly higher odds of having long birth intervals compared to women in the poor quintile. Intervention to prevent prolonged birth intervals should be targeted at these women. Similarly, the link between place of residence and birth spacing could be attributable to variations in access to contraceptives by place of residence.
The finding of this study has public health implications. Countries such as Nigeria, Togo, Chad, and Congo DRC have a high prevalence of adverse birth outcomes and infant mortality. As such, interventions aimed at addressing these adverse outcomes must include educating women on the risk of short birth intervals. Likewise, women in Southern Africa countries need to be informed of the risk of very long birth intervals as a matter of public health intervention.
The pattern of birth spacing found in this study appears to mirror the contraceptive use in the selected SSA countries.[44] For example, of all the selected countries, Zimbabwe has the highest contraceptive use prevalence (66.8%)[44] and also the longest birth spacing interval. The diffusion of contraceptives in Zimbabwe could be linked to the prolonged birth spacing observed in their context. An earlier study on birth intervals showed that Zimbabwean women are savvy about birth spacing and believe that too many children born close together will “burn” each other.[45] Similarly, Malawi has the second-highest rate of contraceptive use (59.2%)[44] of all the countries included, and likewise, the second-highest birth spacing length. This pattern is not a mere coincidence considering that contraception is crucial for achieving the desired birth spacing length. Access to contraceptives is an important contextual factor found to influence birth spacing.[46–48] A study on birth spacing in Zimbabwe shows that access to modern contraceptives was the main determinant of the birth spacing interval.[49] Since the adoption of modern contraceptives in Zimbabwe, birth spacing length has substantially increased. Another plausible reason for long birth spacing in Zimbabwe may perhaps be “birth postponement”, although this needs to be further investigated. There is at least evidence of this in a similar context where very long birth intervals were reported to be due to increasing “birth postponement”.[50] Contrastingly, Chad and the Congo DRC are among the lowest users of modern contraception[44] thus, it is not surprising that birth spacing length was lowest in these countries.
Interestingly, the pattern of birth spacing length found in this study also mirrors the rate of fertility decline in the selected countries.[51,52] Studies have shown that birth spacing is one of the main determinants of fertility. Sayi found that the increase in birth intervals from 28 months in the 1960s to 51 months in the year 2000 coincided with the period of fertility decline.[49] In other words, the changes in fertility and birth spacing are akin both in terms of timing and tempo. Chad and the Congo DRC have the highest fertility rates as well as the shortest birth spacing length of all the selected countries. Evidently, high fertility rate, low fertility decline, and low use of contraceptives suggest a shorter birth spacing interval, while high fertility decline, low fertility rate and high contraceptive prevalence connote long birth spacing intervals.
Our use of DHS data, which are mainly conducted, once in every 5 years), through verbal interviews with women and household heads, means that women have to recall past events. In our study, women had to recall the date of birth of their index baby as well as the preceding birth. While it is feasible to accurately recall the birth dates of the index and the preceding births, the methodology is subjected to recall and reporting biases. Also, due to the cross-sectional nature of the data, cause and effect relationships between independent variables and birth spacing length could not assume. Another limitation of this study is that we focused on only births in the past 5 years and not all births a woman experienced. As such, we could only examine the interval between the preceding birth and the index births. By analyzing only closed intervals, this sample is a selective sample of experiences of women and should be interpreted as such.
This study examined patterns of birth spacing and the determinants of long and short birth spacing in SSA. The findings showed that the length of birth intervals vary from country to country and regionally. While short birth intervals are common in West and Central Africa, long birth intervals are common in Southern and Eastern Africa. Factors that determine short and long birth spacing differ and also vary from country to country. Maternal age was the only factor influencing both long and short birth spacing in all countries. Intervention addressing short birth spacing should target younger women in SSA, while intervention for long birth spacing should prioritize older, educated and wealthy women.
Acknowledgments
The authors would like to acknowledge DHS for providing the data analyzed in this study. Anthony Idowu Ajayi would like to express gratitude to the Africa Population and Health Research Centre, which granted him the opportunity to work on this study by granting him a postdoctoral fellow position.
Author contributions
Anthony Idowu Ajayi and Oluwaseyi Dolapo Seyi both contributed to the conceptualization of the study and drafting of the manuscript. All authors read the final version of the manuscript.
Conceptualization: Anthony Idowu Ajayi, Oluwaseyi Dolapo Somefun.
Data curation: Oluwaseyi Dolapo Somefun.
Formal analysis: Oluwaseyi Dolapo Somefun.
Methodology: Oluwaseyi Dolapo Somefun.
Project administration: Anthony Idowu Ajayi.
Writing – original draft: Anthony Idowu Ajayi.
Writing – review & editing: Anthony Idowu Ajayi, Oluwaseyi Dolapo Somefun.
Supplementary Material
Supplementary Material
Supplementary Material
Supplementary Material
Supplementary Material
Footnotes
Abbreviations: CI = confidence interval, Congo DRC = Democratic Republic of Congo, DHS = demographic and health surveys, RRR = relative risk ratio, SSA = sub-Saharan Africa, USAID = The United States Agency for International Development, WHO = World Health Organization.
How to cite this article: Ajayi AI, Somefun OD. Patterns and determinants of short and long birth intervals among women in selected sub-Saharan African countries. Medicine. 2020;99:19(e20118).
The authors have no funding and conflicts of interest to disclose. Data analyzed in this study could be obtained for free on https://dhsprogram.com/data/available-datasets.cfm.
Supplemental Digital Content is available for this article.
The datasets generated during and/or analyzed during the current study are publicly available.
References
- [1].Conde-Agudelo A, Rosas-Bermúdez A, Kafury-Goeta AC. Effects of birth spacing on maternal health: a systematic review. Am J Obstet Gynecol 2007;196:297–308. [DOI] [PubMed] [Google Scholar]
- [2].Cecatti JG, Correa-Silva EP, Milanez H, et al. The associations between inter-pregnancy interval and maternal and neonatal outcomes in Brazil. Matern Child Health J 2008;12:275–81. [DOI] [PubMed] [Google Scholar]
- [3].Conde-Agudelo A, Rosas-Bermudez A, Castaño F, et al. Effects of birth spacing on maternal, perinatal, infant, and child health: a systematic review of causal mechanisms. Stud Fam Plann 2012;43:93–114. [DOI] [PubMed] [Google Scholar]
- [4].Ganatra B, Faundes A. Role of birth spacing, family planning services, safe abortion services and post-abortion care in reducing maternal mortality. Best Pract Res Clin Obstet & Gynaecol 2016;36:145–55. [DOI] [PubMed] [Google Scholar]
- [5].Ronsmans C, Campbell O. Short birth intervals don’t kill women: evidence from Matlab, Bangladesh. Studies in Family Planning. 1998; 29,3: 282–290. [PubMed] [Google Scholar]
- [6].Conde-Agudelo A, Belizán JM. Maternal morbidity and mortality associated with interpregnancy interval: cross sectional study. BMJ 2000;321:1255–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Marston C; (2006) Report of a technical consultation on birth spacing, Geneva, 13-15 June 2005. Technical Report. World Health Organization, Geneva. https://researchonline.lshtm.ac.uk/id/eprint/11717 [Google Scholar]
- [8].Gribble JN, Murray NJ, Menotti EP. Reconsidering childhood undernutrition: can birth spacing make a difference? An analysis of the 2002–2003 El Salvador National Family Health Survey. Matern Child Nutr 2009;5:49–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Kramer MS, Aboud F, Mironova E, et al. Breastfeeding and child cognitive development: new evidence from a large randomized trial. Arch Gen Psychiatry 2008;65:578–84. [DOI] [PubMed] [Google Scholar]
- [10]. Lamberti, L.M., Zakarija-Grković, I., Fischer Walker, C.L. et al. Breastfeeding for reducing the risk of pneumonia morbidity and mortality in children under two: a systematic literature review and meta-analysis. BMC Public Health 13, S18 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Rollins NC, Ndirangu J, Bland RM, Coutsoudis A, Coovadia HM, et al. (2013) Exclusive Breastfeeding, Diarrhoeal Morbidity and All-Cause Mortality in Infants of HIV-Infected and HIV Uninfected Mothers: An Intervention Cohort Study in KwaZulu Natal, South Africa. PLOS ONE 8(12): e81307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Chowdhury R, Sinha B, Sankar MJ, et al. Breastfeeding and maternal health outcomes: a systematic review and meta-analysis. Acta Paediatr 2015;104(S467):96–113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Rutstein S. Effects of preceding birth intervals on neonatal, infant and under-five years mortality and nutritional status in developing countries: evidence from the demographic and health surveys. International Journal of Gynecology & Obstetrics, 2005; 89: S7-S24. doi:10.1016/j.ijgo.2004.11.012 [DOI] [PubMed] [Google Scholar]
- [14].Conde-Agudelo A, Rosas-Bermúdez A, Kafury-Goeta AC. Birth spacing and risk of adverse perinatal outcomes: a meta-analysis. JAMA 2006;295:1809–23. [DOI] [PubMed] [Google Scholar]
- [15].Timæus IM, Moultrie TA. On postponement and birth intervals. Popul Dev Rev 2008;34:483–510. [Google Scholar]
- [16].Chen LC, Ahmed S, Gesche M, et al. Prospective study of birth interval dynamics in rural Bangladesh. Popul Stud 1974;28:277–97. [DOI] [PubMed] [Google Scholar]
- [17].Potter RG, Jr, Wyon JB, Parker M, et al. A case study of birth interval dynamics. Popul Stud 1965;19:81–96. [Google Scholar]
- [18]. Yohannes, S., Wondafrash, M., Abera, M. et al. Duration and determinants of birth interval among women of child bearing age in Southern Ethiopia. BMC Pregnancy Childbirth 11, 38 (2011). [DOI] [PMC free article] [PubMed] [Google Scholar]
- [19].Rodriguez G, Hobcraft J, McDonald J, et al. A comparative analysis of determinants of birth intervals. 1984. In, WFS comparative studies: cross-national summaries (World Fertility Surveys). Voorburg, Netherlands. International Statistical Institute:31. [Google Scholar]
- [20].Karkee R, Lee AH. Birth spacing of Pregnant Women in Nepal: a community-based study. Front Public Health 2016;4:205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21].Whitworth A, Stephenson R. Birth spacing, sibling rivalry and child mortality in India. Soc Sci Med 2002;55:2107–19. [DOI] [PubMed] [Google Scholar]
- [22].Baschieri A, Hinde A. The proximate determinants of fertility and birth intervals in Egypt: an application of calendar data. Demogr Res 2007;16:59–96. [Google Scholar]
- [23].Yeakey MP, Muntifering CJ, Ramachandran DV, et al. How contraceptive use affects birth intervals: results of a literature review. Stud Fam Plann 2009;40:205–14. [DOI] [PubMed] [Google Scholar]
- [24].Youssef RM. Duration and determinants of interbirth interval: community-based survey of women in southern Jordan. East Mediterr Health J 2005;11:559–72. [PubMed] [Google Scholar]
- [25].Janowitz Barbara, Nichols DJ. Child survivorship and pregnancy spacing in Iran. J Biosoc Sci 1983;15:35–46. [DOI] [PubMed] [Google Scholar]
- [26].Moultrie TA, Sayi TS, Timæus IM. Birth intervals, postponement, and fertility decline in Africa: a new type of transition? Popul Stud 2012;66:241–58. [DOI] [PubMed] [Google Scholar]
- [27].Casterline JB, Odden C. Trends in inter-birth intervals in developing Countries 1965–2014. Popul Dev Rev 2016;42:173–94. [Google Scholar]
- [28].Towriss CA, Timæus IM. Modelling period fertility: schooling and intervals following a birth in Eastern Africa. Popul Stud 2018;72:75–90. [DOI] [PubMed] [Google Scholar]
- [29].Santosh A, Zunjarwad G, Hamdi I, et al. Perinatal mortality rate as a quality indicator of healthcare in Al-Dakhiliyah Region, Oman. Sultan Qaboos Univ Med J 2013;13:545–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [30].World Health Organization. Report of a WHO technical consultation on birth spacing:. 2007;Geneva, Switzerland: World Health Organization, 13-15 June 2005. [Google Scholar]
- [31].Rutstein SO. Steps to constructing the new DHS Wealth Index. Rockville, MD: ICF International; 2015. [Google Scholar]
- [32].Hamilton LC, Seyfrit CL. Interpreting multinomial logistic regression. Stata Technical Bulletin 1993;13:24–8. [Google Scholar]
- [33].Cheslack Postava K, Winter AS. Short and long interpregnancy intervals: correlates and variations by pregnancy timing among US women. Perspect Sex Reprod Health 2015;47:19–26. [DOI] [PubMed] [Google Scholar]
- [34].Glei DA. Measuring contraceptive use patterns among teenage and adult women. Fam Plann Perspect 1999;31:73–80. [PubMed] [Google Scholar]
- [35].Achana F.S., Bawah A.A., Jackson E.F., et al. Spatial and socio-demographic determinants of contraceptive use in the Upper East region of Ghana. Reprod Health 12, 29 (2015). 10.1186/s12978-015-0017-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [36].Mostafa Kamal S, Aynul Islam M. Contraceptive use: socioeconomic correlates and method choices in rural Bangladesh. Asia Pac J Public Health 2010;22:436–50. [DOI] [PubMed] [Google Scholar]
- [37]. Ikamari, L., Izugbara, C. & Ochako, R. Prevalence and determinants of unintended pregnancy among women in Nairobi, Kenya. BMC Pregnancy Childbirth 13, 69 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- [38].Liu K, Case A, Cheung AP, et al. Advanced reproductive age and fertility. J Obstet Gynaecol Can 2011;33:1165–75. [DOI] [PubMed] [Google Scholar]
- [39].Andersen A-MN, Wohlfahrt J, Christens P, et al. Maternal age and fetal loss: population based register linkage study. BMJ 2000;320:1708–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [40].Schummers L, Hutcheon JA, Hernandez-Diaz S, et al. Association of short interpregnancy interval with pregnancy outcomes according to maternal age. JAMA Int Med 2018;178:1661–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [41].Gemmill A, Lindberg LD. Short interpregnancy intervals in the United States. Obstet Gynecol 2013;122:64–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [42].Fayehun O, Omololu O, Isiugo-Abanihe U. Sex of preceding child and birth spacing among Nigerian ethnic groups. Afr J Reprod Health 2011;15:79–89. [PubMed] [Google Scholar]
- [43].Verma J, Sachar R, Prakash V, et al. Effect of sex of preceding child on birth interval. Indian J Matern Child Health 1990;1:50. [PubMed] [Google Scholar]
- [44].Kaneda T, Bietsch K. World Population Data Sheet. Washington: Population Reference Bureau; 2015. [Google Scholar]
- [45].Lovel H, Mkandla M, Morley D. Birth spacing in Zimbabwe a generation ago. Lancet 1983;322:161–2. [DOI] [PubMed] [Google Scholar]
- [46].McGuire C, Stephenson R. Community factors influencing birth spacing among married women in Uganda and Zimbabwe. Afr J Reprod Health 2015;19:14–24. [PubMed] [Google Scholar]
- [47].Ajayi A.I., Nwokocha E.E., Akpan W., et al. Use of non-emergency contraceptive pills and concoctions as emergency contraception among Nigerian University students: results of a qualitative study. BMC Public Health 16, 1046 (2016). 10.1186/s12889-016-3707-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [48].Ajayi A.I., Nwokocha E.E., Adeniyi O.V., et al. Unplanned pregnancy-risks and use of emergency contraception: a survey of two Nigerian Universities. BMC Health Serv Res 17, 382 (2017). 10.1186/s12913-017-2328-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [49].Sayi T. Fertility, birth intervals, and their proximate determinants in Zimbabwe. University of Cape Town, Cape South Africa, 2009. [Google Scholar]
- [50].
- [51].World Bank, Fertility Rate, Total for Developing Countries in Sub-Saharan Africa [SPDYNTFRTINSSA], retrieved from FRED, Federal Reserve Bank of St. Louis; https://fred.stlouisfed.org/series/SPDYNTFRTINSSA, April 23, 2019. [Google Scholar]
- [52].United Nations. World Fertility Patterns 2015. In: United Nations., ed. http://wwwunorg/en/development/desa/population/publications/pdf/fertility/ world-fertility-patterns-2015pdf2015. Accessed on April 23, 2019 [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


