Abstract
This study estimates the association between the fall experience in the last 2 years and cognitive function and further evaluate the differences in this association between men and women and across different age groups. Data from the Korean Longitudinal Study of Ageing from 2006 to 2016 was used and 9279 research samples were included at baseline in 2006. To analyze the association between fall experience for the last 2 years and cognitive function, generalized estimating equation model and chi-square test were used. After adjusting for all confounders, those with fall experience were significantly associated with cognitive decline. With non-fall experience as reference: fall experience, B = −0.013 (P = .017). In the 64 years or less group, fall experience was significantly associated with cognitive decline (P-value: 0.006) to those with non-fall experience. In male group, with non-fall experience as reference: fall experience, B = −0.017 (P = .041). Fall experience in the last 2 years is associated with cognitive decline, especially in those 64 years or less and male group. Therefore, self-reported screening for fall experience might aid population-based prevention strategies for cognitive decline, especially in 64 years or less and male.
Keywords: economic activity, elderly, health, restriction
1. Introduction
Due to the increasing longevity in the lifespan of our population, a noticeable increase in multimorbidity is of much concern, with falls being a source of both morbidity and mortality. In the community-dwelling aged population, about a third experience at least one fall each year.[1] Furthermore, these falls could lead to problems such as cognitive impairment and possibly increase the risk of institutionalization or mortality.[2]
In most cases, the occurrence of falling is caused by more than one problem.[3] This is supported by findings of previous studies that show associations between multiple risk factors (e.g., weakness in muscle, gait and balance, cognitive impairment, previous history of falls, arthritis, depression, poor visual acuity, chronic diseases, postural hypotension, or psychotropic medication) and increased risk of falls.[4–6] Also, the presence of these risk factors have shown association with adverse physical consequences (e.g., facture, restriction of activity), deterioration of health, increased social isolation as well as increased risk of institutionalization.[7,8] Subsequently, various adverse outcomes such as disability, quality of life and mortality and effected.[9,10]
Even though it was evident that falls, depression and cognitive impairment share common risk factors,[11,12] it is yet unclear which risk factors need more attention in regards to community interventions.[13] Furthermore, although a number of studies have indicated physical and functional outcomes of falls (e.g., fractures, soft-tissue injury, premature institutionalization, and deaths), the same cannot be said in regards to long-term emotional and cognitive outcomes.[11,14] In this regard, understanding the fall-cognition pathway is a crucial aspect in order to design interventions targeted to address potential pathways to cognition as well as falls. Additionally, it is important to understand how fall experience affects cognitive function, because such understanding would further assist in terms of designing interventions for physical disability as well as fall-related mental health. These relationships still seem unexplored for Korean middle-aged and elderly population. In particular, the effects of fall experiences by gender (male and female) and age (elderly group and non-elderly group) on cognitive decline are less known, so our study performed stratification analysis on gender and age group.
The objectives of our study was to examine the association between experience of falls and subsequent change in cognitive function over a 10-year follow-up in a community sample of middle aged and elderly population. Furthermore, the differences between male and female elderly population were evaluated.
2. Methods
2.1. Data source
The data used for the following analyses were derived from the Korean Longitudinal Study of Ageing (KLoSA) from 2006 to 2016. KLoSA was constructed by repeatedly surveying the identical content for the same respondents every year and repeatedly measured from the 2006 (1st wave) to 2016 (6th wave) to collect observation cases at multiple points in time. This survey involves multistage stratified randomly probability sampling to create a nationally representative sample of community-dwelling Koreans 45 years of age and older based on geographical areas and housing types across Korea.
In the first baseline survey (2006), 10,254 individuals in 6171 households were interviewed. The second survey, in 2008, followed up with 8675 subjects, who represented 86.6% of the original panel. The third survey, in 2010, followed up with 8229 subjects, who represented 81.7% of the original panel, the fourth survey, in 2012, followed up with 7813 subjects, who represented 80.1% of the original panel and the fifth survey, in 2014, followed up with 8387 subjects (including 920 new participated sample), who represented 80.4% of the original panel. The sixth survey, in 2016, followed up with 9913 subjects (including 878 new participated sample), who represented 79.6% of the original panel.
We excluded individuals for whom we had incomplete data: 33 individuals who lacked information on socioeconomic factors and one individual who lacked information on health status and risk factors, 74 individuals who lacked information on Center for Epidemiologic Studies Depression, 791 individuals who lacked information on grip strength, and 76 individuals who lacked information on MMSE in 2006. Finally, 9279 research samples were included. This study does not need ethical approval because it is not a study using human derivatives, and all subjects are encrypted and cannot be identified
2.2. Independent variables
Fall experience in the last 2 years was assessed by self-reported response to the question: “Have you ever had a fall experience since the last survey?” the responses were assigned to “Yes” or “No.”
2.3. Dependent variables
The study considered a two-fold dependent variable, which was measured by using the Korean Mini-Mental State Examination (K-MMSE) as cognitive impairment and grip strength. The K-MMSE included 11 items in seven categories of cognitive functions, including orientation for time and place, registration, attention & calculation, recall, language, and visual construction.[15,16] The total score of the measure ranges from 0 to 30; higher the score, better the cognitive function. The validity of the K-MMSE was reported elsewhere.[15]
2.4. Control variables
2.4.1. Socioeconomic and demographic factors
Age groups were divided into three categories: 45 to 54, 55 to 64 and ≥65 years of age. Education level was categorized into four groups: elementary school or lower, middle school, high school, and college or higher. Gender was categorized as male and female. Residential regions were categorized as Metropolitan (Seoul), urban (Daejeon, Daegu, Busan, Incheon, Kwangju, or Ulsan) or rural (not classified as a city). Marital status was divided into three groups: married, separated or divorced, and single. Health insurance was categorized into national health insurance and medical aid.
2.4.2. Health status and behavioral factors
Grip strength was measured by a handgrip dynamometer (Model number: NO6103, TANITA, Japan). The test was performed in a sitting position with the elbow flexed at 90° on both the right and left sides. The mean strength was calculated from grip strength on both sides.[17] Grip strength in each year was divided into three groups: low, middle, and high using SAS Rank function. Economic activity and regular exercise more than once a week was categorized into Yes and No. Smoking status was categorized into three groups: current smoker, former smoker, and never smoker. Alcohol use also was divided into three groups: current drinker, former drinker, and never drinker. Self-rated health was categorized into three groups: very good, good, normal, bad, and worst. Finally, the number of chronic diseases (consisting of hypertension, diabetes, osteoarthritis, rheumatoid arthritis, cancer, chronic pulmonary disease, liver disease, cardiovascular disease, and cerebrovascular disease) and year dummies were included as covariates in our analyses.
2.4.3. Analytical approach and statistics
Chi-square test and a generalized estimating equation (GEE) model were used to investigate the association between fall experience in the last 2 years and cognitive function. The use of a GEE model was required in order to handle the unbalanced data with correlated outcomes over time. To determine whether cognitive function changed over time, we included time (year) in the model as a continuous covariate; the regression coefficient was used to estimate both the change in cognitive function and independent variables, annually.[18] For all analyses, statistical significance was set to P ≤ .05, two-tailed. All analyses were conducted using the SAS statistical software package, version 9.4 (SAS Institute Inc., Cary, NC).
3. Results
3.1. Prevalence of cognitive function
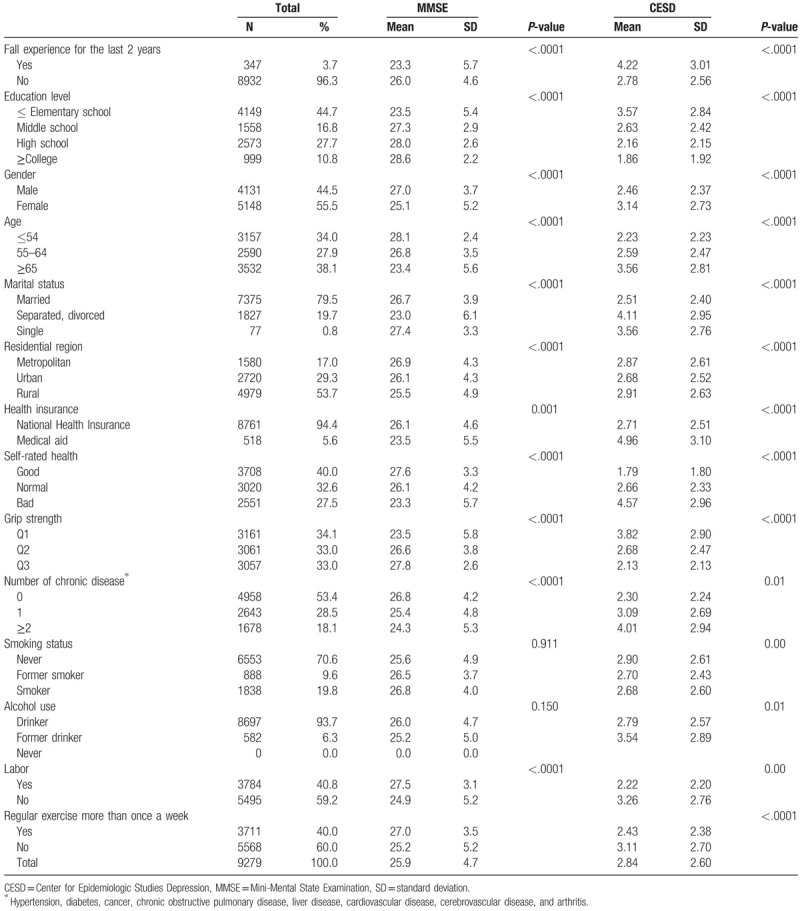
Table 1 displays the descriptive statistics of all variables at baseline (2006). Of the 9279 research subjects included in our study, mean of cognitive function (MMSE) 2.84 points standard deviation (SD: 2.60). Of the total sample population, mean of cognitive function in those with fall experience in the last 2 years had 23.3 points (SD: 5.7).
Table 1.
General characteristics of subjects included for analysis.
3.2. Association between fall experience in the last 2 years and cognitive function
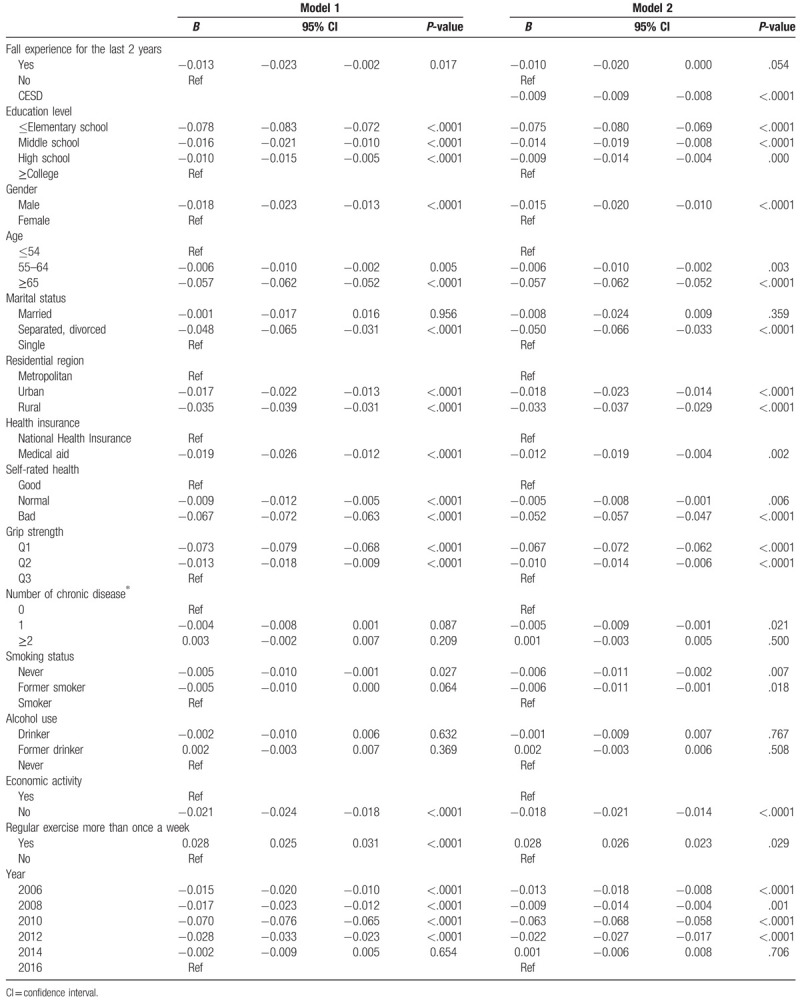
Table 2 shows the relationship between fall experience in the last 2 years and cognitive function adjusted for socioeconomic status and health risk and status behavior factors. After adjusting for all of these confounders, estimate of cognitive function in those with fall experience was −0.013 lower (95% confidence interval [CI]: −0.023 to −0.002 P-value: .017) compared with those with non-fall experience.
Table 2.
Adjusted effect between fall experience and mental health.
3.3. Association between fall experience in the last 2 years and cognitive function by age and gender
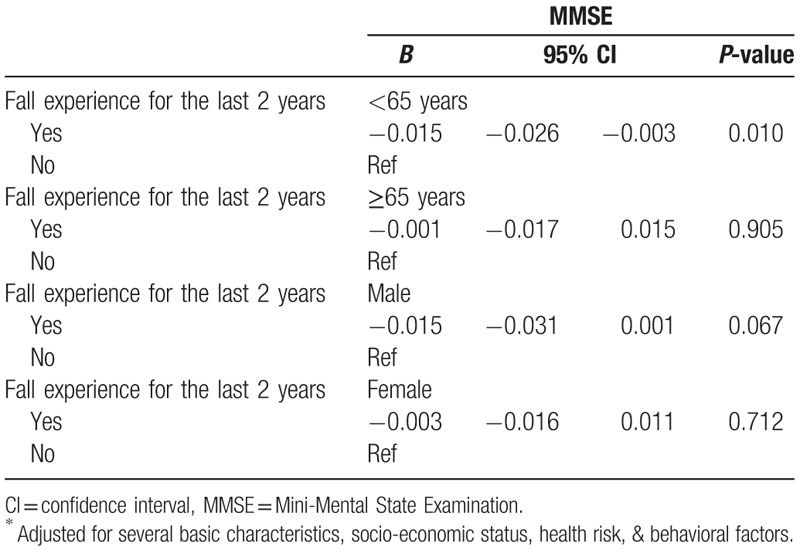
Table 3 shows subgroup analysis according to age (64 years or less and 65 years or more) and gender (male and female). In 64 years or less, estimate of cognitive function in those with fall experience was −0.016 lower (95% CI: −0.027 to −0.005 P-value: .006) and in male, estimate of those with fall experience was −0.017 (95% CI: −0.033 to −0.001 P-value: .041) compared with those with non-fall experience.
Table 3.
Adjusted effect between grip strength and mental health by age and gender.
4. Discussion
In this population-based prospective study of 9279 middle aged and older adults at baseline, our primary purpose was to investigate whether fall experience in the last 2 years was responsible for the cognitive function after adjusting all covariates including socioeconomic status, health risk, and behavior factors using nationally representative database in South Korea.
There are two major findings in this study. First, a significant association between fall accidents and cognitive function, among middle-aged and elderly Korean people, was found. Second, in the subgroup analyses, the association in those 64 years or less was more statistically significant than others.
Despite the efforts of previous studies to reveal the mechanism of the association between fall accidents and cognitive decline, the underlying mechanisms are still undetermined. One possible explanation for these complex relationships between falls, depression, and cognitive decline may be due to the subsequent event following one of these conditions. Considering the evidence regarding this relationship, a vicious cycle could be considered. For instance, a fall accident has been associated with fear of falling,[19,20] which then could lead to reduced levels of physical activity, walking as well as social participation, further leading to loneliness and social isolation.[19,21–24] This then could reduce stability or balance control, bring the cycle back to the increased risk of falling. Furthermore, reduced social and physical activity could also lead to onset of depression and cognitive decline.[25–27] In other cases, cognitive factors have shown mediating effect on the association between depression and falling.[28] Our findings are also consistent with the results from Biderman et al, showing an association between fall accident and depression, with subsequent cognitive decline.[29] Another similar finding was found in a 12-year longitudinal study of 2425 cognitively intact adults, which showed an association between high depressive symptoms and cognitive decline in the memory domain.[30]
Worldwide, fall accident is a major public health issue among the elderly. About a third of community dwelling elderly people will fall at least once a year, and of those 5% consequently suffer fractures, which then could lead to subsequent disability and even loss of independence.[5] Notably, preventive interventions against falls, which often focus on functional status, have shown to be more effective for those relatively less cognitively impaired in advance.[31] Therefore, identifying the future risk of falls in those with less severe cognitive impairment could be more beneficial in terms of primary intervention.
There are several limitations to this study that should be taken into consideration. First, although our study was based on a longitudinal design, it may not fully acknowledge the causality between the variables of interest and cannot be ascertained. Therefore, prospective studies targeting this issue are required to further investigate the causal relationship between fall experience and cognitive function. Second, because the fall history was assessed by interview, there could be a possible recall bias. A prospective study incorporating a daily record of fall experience is needed to overcome the possible recall bias. Third, although our research is based on a large sample size (N = 9279), which strengthens the precision in the odds ratio estimation, the fact that individuals with missing values on the critical information were not included need to be taken into consideration. The excluded individuals could have changed our results to overestimate the association between fall experience and cognitive function. Finally, information regarding health status and risky health behaviors was not sufficient. Furthermore, there might have been unobserved confounders. However, the lack of such information might have resulted in an underestimation of our results in the present study. Nevertheless, despite the underestimation, we found a significant association between fall experience in the last 2 years and cognitive function.
Despite these limitations, this study has various strengths, particularly with its use of a population-based representative sample and the 10-year follow-up database. We also prospectively analyzed a large number of individuals from longitudinal data of a well-defined and comprehensively studied sample of middle aged and older adults to examine the association between fall experience in the last 2 years and cognitive function. Therefore, with the rapidly aging population in Korea, fall experience in the last 2 years may be a reasonably good predictor of cognitive function in middle aged and elderly population.
In conclusion, having fall history in the last 2 years was independently associated with cognitive decline over 10 years compared to having no history of falls, with a mediating effect of depression on the association between falls and cognitive decline, especially in those 64 years or less. The findings suggest that screening for cognitive decline problems in those with fall history might help stem the onset of falls-related physical and cognitive disability.
Footnotes
Abbreviations: CES-D = Center for Epidemiologic Studies Depression, CI = confidence interval, GEE = generalized estimating equation, KLoSA = Korean Longitudinal Study of Ageing, K-MMSE = Korean Mini-Mental State Examination, SD = standard deviation.
How to cite this article: Kim JH. Fall experience and cognitive function in middle aged and elderly population. Medicine. 2020;99:18(e19203).
The authors have no conflicts of interest to disclose.
References
- [1].Formiga F, Ferrer A, Duaso E, et al. Falls in nonagenarians living in their own homes: the Nonasantfeliu study. J Nutr Health Aging 2008;12:273–6. [DOI] [PubMed] [Google Scholar]
- [2].Salva A, Bolibar I, Pera G, et al. Incidence and consequences of falls among elderly people living in the community. Med Clin (Barc) 2004;122:172–6. [DOI] [PubMed] [Google Scholar]
- [3].Tinetti ME, Speechley M, Ginter SF. Risk factors for falls among elderly persons living in the community. N Engl J Med 1988;319:1701–7. [DOI] [PubMed] [Google Scholar]
- [4].Kannus P, Sievanen H, Palvanen M, et al. Prevention of falls and consequent injuries in elderly people. Lancet 2005;366:1885–93. [DOI] [PubMed] [Google Scholar]
- [5].Rubenstein LZ, Josephson KR. The epidemiology of falls and syncope. Clin Geriatr Med 2002;18:141–58. [DOI] [PubMed] [Google Scholar]
- [6].Uemura K, Shimada H, Makizako H, et al. Effects of mild cognitive impairment on the development of fear of falling in older adults: a prospective cohort study. J Am Med Dir Assoc 2015;16:1104.e9–13. [DOI] [PubMed] [Google Scholar]
- [7].Lopes K, Costa D, Santos L, et al. Prevalence of fear of falling among a population of older adults and its correlation with mobility dynamic balance, risk and history of falls. Braz J Phys Ther 2009;13:223–9. [Google Scholar]
- [8].Veras R. Population aging today: demands, challenges and innovations. Rev Saude Publica 2009;43:548–54. [DOI] [PubMed] [Google Scholar]
- [9].Finlayson ML, Peterson EW. Falls, aging, and disability. Phys Med Rehabil Clin N Am 2010;21:357–73. [DOI] [PubMed] [Google Scholar]
- [10].Thiem U, Klaassen-Mielke R, Trampisch U, et al. Falls and EQ-5D rated quality of life in community-dwelling seniors with concurrent chronic diseases: a cross-sectional study. Health Qual Life Outcomes 2014;12:2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Delbaere K, Kochan NA, Close JC, et al. Mild cognitive impairment as a predictor of falls in community-dwelling older people. Am J Geriatr Psychiatry 2012;20:845–53. [DOI] [PubMed] [Google Scholar]
- [12].Wang YC, Lin FG, Yu CP, et al. Depression as a predictor of falls amongst institutionalized elders. Aging Ment Health 2012;16:763–70. [DOI] [PubMed] [Google Scholar]
- [13].Cameron ID, Murray GR, Gillespie LD, et al. Interventions for preventing falls in older people in nursing care facilities and hospitals. Cochrane Database Syst Rev 2010;CD005465. [DOI] [PubMed] [Google Scholar]
- [14].Hartholt KA, van Beeck EF, Polinder S, et al. Societal consequences of falls in the older population: injuries, healthcare costs, and long-term reduced quality of life. J Trauma 2011;71:748–53. [DOI] [PubMed] [Google Scholar]
- [15].Kang Y, Na DL, Hahn S. A validity study on the Korean Mini-Mental State Examination (K-MMSE) in dementia patients. J Korean Neurol Assoc 1997;15:300–8. [Google Scholar]
- [16].Thomas F, Bean K, Pannier B, et al. Cardiovascular mortality in overweight subjects: the key role of associated risk factors. Hypertension 2005;46:654–9. [DOI] [PubMed] [Google Scholar]
- [17].Min JY, Lee KJ, Park JB, et al. Social engagement, health, and changes in occupational status: analysis of the Korean Longitudinal Study of Ageing (KLoSA). PLoS One 2012;7:e46500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18].Arrandale VH, Koehoorn M, MacNab Y, et al. Longitudinal analysis of respiratory symptoms in population studies with a focus on dyspnea in marine transportation workers. Int Arch Occup Environ Health 2009;82:1097–105. [DOI] [PubMed] [Google Scholar]
- [19].Li F, Fisher KJ, Harmer P, et al. Fear of falling in elderly persons: association with falls, functional ability, and quality of life. J Gerontol B Psychol Sci Soc Sci 2003;58:283–90. [DOI] [PubMed] [Google Scholar]
- [20].Harada K, Oka K, Shibata A, et al. Relationships between foot problems, fall experience and fear of falling among Japanese community-dwelling elderly. Nihon Koshu Eisei Zasshi 2010;57:612–23. [PubMed] [Google Scholar]
- [21].Iaboni A, Flint AJ. The complex interplay of depression and falls in older adults: a clinical review. Am J Geriatr Psychiatry 2013;21:484–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [22].Painter JA, Allison L, Dhingra P, et al. Fear of falling and its relationship with anxiety, depression, and activity engagement among community-dwelling older adults. Am J Occup Ther 2012;66:169–76. [DOI] [PubMed] [Google Scholar]
- [23].van Haastregt JC, Zijlstra GA, van Rossum E, et al. Feelings of anxiety and symptoms of depression in community-living older persons who avoid activity for fear of falling. Am J Geriatr Psychiatry 2008;16:186–93. [DOI] [PubMed] [Google Scholar]
- [24].Zijlstra GA, van Haastregt JC, van Eijk JT, et al. Prevalence and correlates of fear of falling, and associated avoidance of activity in the general population of community-living older people. Age Ageing 2007;36:304–9. [DOI] [PubMed] [Google Scholar]
- [25].Dias RC, Freire MT, Santos EG, et al. Characteristics associated with activity restriction induced by fear of falling in community-dwelling elderly. Rev Bras Fisioter 2011;15:406–13. [PubMed] [Google Scholar]
- [26].Buchman AS, Boyle PA, Yu L, et al. Total daily physical activity and the risk of AD and cognitive decline in older adults. Neurology 2012;78:1323–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [27].Bassuk SS, Glass TA, Berkman LF. Social disengagement and incident cognitive decline in community-dwelling elderly persons. Ann Intern Med 1999;131:165–73. [DOI] [PubMed] [Google Scholar]
- [28].Kvelde T, McVeigh C, Toson B, et al. Depressive symptomatology as a risk factor for falls in older people: systematic review and meta-analysis. J Am Geriatr Soc 2013;61:694–706. [DOI] [PubMed] [Google Scholar]
- [29].Biderman A, Cwikel J, Fried AV, et al. Depression and falls among community dwelling elderly people: a search for common risk factors. J Epidemiol Community Health 2002;56:631–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [30].Zahodne LB, Stern Y, Manly JJ. Depressive symptoms precede memory decline, but not vice versa, in non-demented older adults. J Am Geriatr Soc 2014;62:130–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [31].Montero-Odasso M, Verghese J, Beauchet O, et al. Gait and cognition: a complementary approach to understanding brain function and the risk of falling. J Am Geriatr Soc 2012;60:2127–36. [DOI] [PMC free article] [PubMed] [Google Scholar]


