Abstract
Background
Little is known about the trend of incidence and mortality of specific organ dysfunction among sepsis patients at the population level. This study aimed to examine the trend and mortality of organ dysfunction in patients with sepsis using a nationwide database in Taiwan.
Methods
We conducted a study using 2002–2012 data from the nationwide health insurance database of Taiwan. Sepsis hospitalizations were identified by Angus algorithm to include all cases with ICD-9-CM codes for specific sepsis diagnosis and both an infectious process and a diagnosis of acute organ dysfunction. The primary outcome was the trend of incidence and in-hospital mortality of specific type of organ dysfunction in sepsis patients.
Results
We identified 1,259,578 adult patients with sepsis. Acute respiratory dysfunction, cardiovascular dysfunction/shock, and renal system dysfunction were the leading three types of acute organ dysfunction, accounting for 65.6, 30.5, and 18.3% of all sepsis patients, respectively. All types of organ dysfunction increased over time, except for hepatic and metabolic systems. Renal system (annual increase: 13.5%) and cardiovascular system dysfunction (annual increase: 4.3%) had the fastest increase. Mortality from all sources of infection has decreased significantly in the study period (trend p < 0.001).
Conclusions
This is the first true nationwide population-based data showing the trend and outcome of acute organ dysfunction in sepsis patients. Renal and cardiovascular systems dysfunction are increasing at an alarming rate.
Keywords: sepsis, organ dysfunction, sepsis-related mortality
Introduction
Sepsis is a clinical syndrome that develops when a human’s host immune system responds to infection.[1] This response may cause collateral injury to affect organs or systems, leading to a life-threatening condition.[2] Before 2016, sepsis was traditionally defined as the presence of infection and the systemic inflammatory response syndrome (SIRS). In addition, two severe forms of sepsis: severe sepsis and septic shock were also defined.[1] Many large-scale or population-based studies[3-6] regarding the incidence, trends, and outcomes of sepsis or severe sepsis were reported based on the SIRS definition. However, the new clinical definition of sepsis that is termed as Sepsis-3 was proposed in 2016 by the Society of Critical Care Medicine and the European Society of Intensive Care Medicine.[7] Sepsis-3 is based on the presence of infection and organ dysfunction. Operationally, acute organ dysfunction is defined by an increase of more than 2 points in the total sequential organ failure assessment (SOFA) score in the intensive care unit (ICU) settings or quick SOFA score outside the ICU settings. Although several studies[3,8-10] have assessed the burden of sepsis at the national level, studies that examine the trends of incidence and outcomes of organ function in sepsis, which is an important component of the Sepsis-3 definition, are still lacking.
Moreover, organ replacement therapies, comprised of evidence-based hemodynamic optimization and organ protection devices, have been introduced and widely adopted for the management of patients with sepsis in the last few decades. These therapies include invasive or non-invasive mechanical ventilation (MV) for respiratory failure, intra-aortic balloon pumps for cardiac dysfunction, dialysis for renal injury, and extracorporeal membrane oxygenation for cardiopulmonary failure. The development of new management approaches, such as the protective-ventilation strategy,[11] conservative strategy of fluid management,[12] and restrictive transfusion[13] have also significantly changed clinical practice. It is, therefore, interesting to know the temporal trend of the incidence and outcome of acute organ dysfunctions in patients with sepsis. Thus, the aim of this study is to investigate the incidence and outcomes of different types of organ dysfunction among patients with sepsis over time.
Methods
Study Cohort
The entire National Health Insurance (NHI) claims database of Taiwan between January 1, 2002 and December 31, 2012 was used for this study. Because the NHI of Taiwan was a government-operated and mandatory health insurance system with a 99.7% coverage rate, using such database allowed us to obtain information for almost all 23 million residents of Taiwan. The database was developed as part of the National Health Informatics Project sponsored by the Ministry of Health and Welfare of Taiwan. The NHI Research Database contained complete outpatient and inpatient electronic claim records, individual diagnoses, procedures, and medications prescribed. Available information on all prescription drugs included brand name, route of administration, quantity, and number of days supplied. Since this was an anonymized administrative database study, patient consent was not required. Our study was approved by the institutional review board of National Taiwan University Hospital (no. 201402032RINA).
Following the publication of the surviving sepsis campaign in 2004, a nationwide educational program was launched by the joint Taiwan Critical Care Medicine Committee, which consisted of three medical societies: Critical Care Medicine, Emergency and Critical Care Medicine, and Pulmonary and Critical Care Medicine (total board-certified specialists = 2,102). This educational program included at least 10-hours of training for physicians who work in the ICU.[14] During the study period, there was no financial incentive that encouraged physicians to follow the guideline.
Case Selection and Definitions
According to sepsis-3, sepsis is defined as lifethreatening organ dysfunction caused by a dysregulatedhost response to infection.[7] We only includedadult patients for this analysis and patients under 18 years of age were excluded. The cases with sepsiswas identified by the ICD-9 coding strategy proposed by Angus that identified sepsis cases by combining ICD-9-CM codes for both a bacterial or fungal infectionand a diagnosis of acute organ dysfunction in the hospital or emergency department records.[15] The organs/systems dysfunctions used for this study included cardiovascular/shock, respiratory, central nervous, hematologic, hepatic, renal and metabolic dysfunctions. The ICD-9 codes used for identificationof acute organ dysfunction were shown in the Appendix 1. Index date was defined as the first day of emergency department visit or hospital admission of sepsis. We also included patients with an explicit codeof sepsis, severe sepsis, and septic shock (ICD-9 CM: 995.92, 785.52). Angus implementation15 is the most common administrative implementations for severe sepsis and has been cited more than 2,000 times as of December 2011. This implementation was validated by demonstrating that it identifies a population of patients similar in aggregate to one identified by nursing-led prospective assessment[16,17] or physician review.[18] We used the Angus implementation of identify sepsis cases in this study to ensure the comparability with international sepsis epidemiology. The followinginformation including demographic, presence of pre-existing comorbidity, and outcome were collected. Other information was abstracted from the index hospitalizationclaims records. We defined the mortality as the 30-day all-cause mortality verified by a linkednational death certificate database.
Statistical Analysis
We compared the characteristics and outcomes of organ dysfunction among patients with sepsis across the study period. Categorical variables were presented as frequency and percentage, and continuous variables were presented as mean ± standard deviation. The annual incidence of sepsis was calculated as the number of sepsis patients divided by the number of population in a given year. When there were multiple episodes of sepsis in one patient, we only counted the first episode in a given year. The mortality rate was calculated by the number of deaths divided by the total number of sepsis patients. The temporal trends were all presented with line graphs. Our nationwide database allowed for the capture of all cases of sepsis and there was minimal possibility of chance variation. Therefore, confidence intervals were not presented in all estimates. All analyses were performed using SAS Version 9.3 (SAS Institute Inc., Cary, NC, USA), and a two sided p-value of 0.05 was deemed as statistical significance.
Results
Demographics
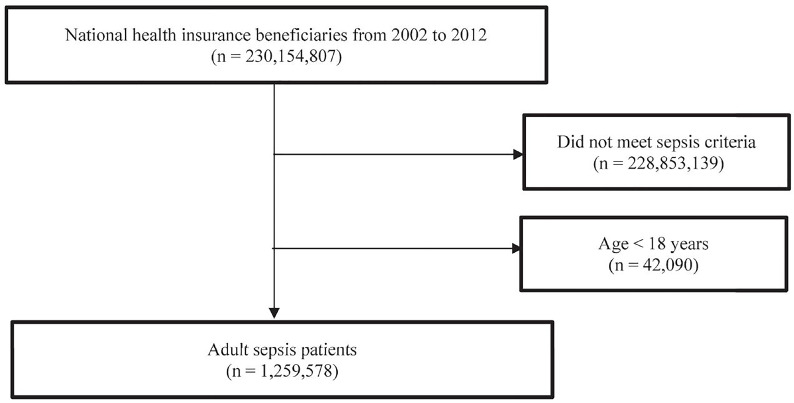
In total, we identified 1,259,578 episodes of sepsis between 2002 and 2012 (Figure 1). Overall, acute respiratory failure was the most common organ dysfunction (65.6%, n = 827,078) among sepsis patients, followed by cardiovascular dysfunction/shock (30.5%), renal dysfunction (18.3%), hepatic dysfunction (11.2%), metabolic dysfunction (5.1%), hematologic system dysfunction (5.0%), and central nervous system dysfunction (4.1%). We divided the study periods into three subperiods: 2002–2005, 2006–2009, and 2010–2012 for further analysis (Table 1). Male comprised more than half of sepsis cases, and the ratio of male patients increased from 56.69% first subperiod to 58.47% in last subperiod. The average age of sepsis patients also gradually increased over time, from 67.93 years in the first subperiod to 69.70 years in the last subperiod. In all subperiods, acute respiratory failure remained the most common type of organ dysfunction, but the percentage of acute respiratory failure among patients with sepsis declined from 70.10% in first subperiod to 60.34% in last subperiod. The decreasing trends of organ dysfunction over time were also noted for hepatic system dysfunction, and metabolic dysfunction. In contrast, the trends of renal system dysfunction, hematologic systemic dysfunction, and central nervous system dysfunction appeared increasing with time. For cardiovascular dysfunction/ shock—the second most common type of organ dysfunction, the ratio was lowest in first subperiod (27.51%), and highest in second subperiod (39.10%). Finally, the 30-day all-cause mortality rate decreased from 26.52% in the first subperiod to 22.95% in the last subperiod.
Figure 1. Flowchart for patient enrollment.
Table 1. Characteristics of patients with sepsis according to three subperiods spanning 2002 to 2012.
n = total number of severe sepsis and septic shock patients.
| Characteristic | 2002–2005
n = 380,343 |
2006–2009
n = 471,489 |
2010–2012
n = 407,746 |
|---|---|---|---|
| Male sex (%) | 227,020 (56.69) | 278,826 (58.78) | 238,422 (58.47) |
| Age | 67.93 ± 16.45 | 69.03 ± 16.50 | 69.70 ± 16.68 |
| Acute organ/system dysfunction | |||
| Acute respiratory failure (%) | 266,614 (70.10) | 314,445 (66.69) | 246,019 (60.34) |
| Cardiovascular dysfunction/shock(%) | 104,620 (27.51) | 148,730 (39.10) | 130,796 (34.39) |
| Renal system dysfunction (%) | 51,579 (13.56) | 87,101 (18.47) | 91,941 (22.55) |
| Hepatic system dysfunction (%) | 45,735 (12.02) | 51,868 (11.00) | 43,259 (10.61) |
| Metabolic system dysfunction (%) | 22,174 (5.83) | 23,111 (4.90) | 19,309 (4.74) |
| Hematologic system dysfunction (%) | 18,682 (4.91) | 22,677 (4.81) | 22,186 (5.44) |
| Central nervous system dysfunction (%) | 13,919 (3.66) | 19,208 (4.07) | 18,183 (4.46) |
| Outcome | |||
| All-cause mortality (30 days) (%) | 100,866 (26.52) | 114,582 (24.30) | 93,560 (22.95) |
Incidence
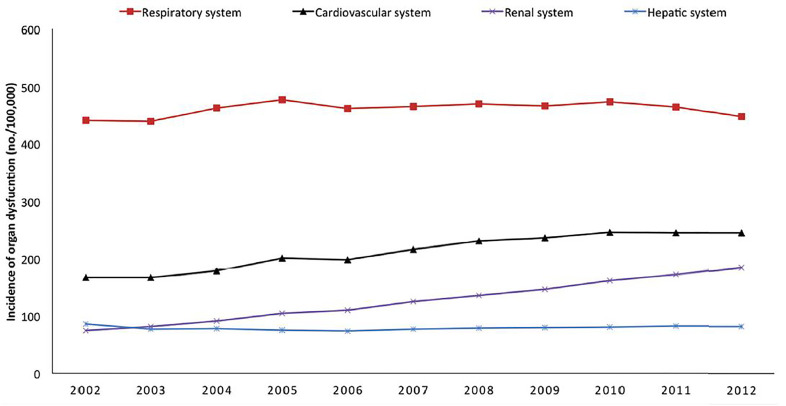
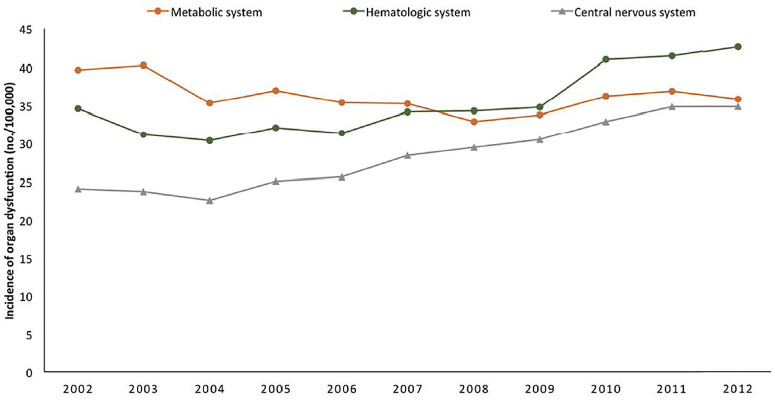
Figures 2A‒B and Table 2 showed annual incidence (per 100,000 persons) of sepsis-related organ dysfunction over the 11-year period. The incidence of patients with renal dysfunction (annual increase of 13.51%), cardiovascular dysfunction/shock (annual increase of 4.31%), central nervous system dysfunction (annual increase of 4.10%), hematologic dysfunction (annual increase of 2.10%) and respiratory dysfunction (annual increase of 0.14%) were found to increase from year 2002 to year 2012. In contrast, the incidence of sepsis patients with hepatic dysfunctions (annual decrease of 0.42%) and metabolic dysfunctions (annual decrease of 0.88%) were found to decrease in number during the study period.
Table 2. Changes in population incidence of specific organ dysfunction among patients with sepsis, from 2002 to 2012: incidence of all the organ dysfunctions, presented by events per 100,000 population.
| 2002 | 2003 | 2004 | 2005 | 2006 | 2007 | 2008 | 2009 | 2010 | 2011 | 2012 | Annual change | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Cardiovascular system dysfunction | 166 | 167 | 179 | 201 | 198 | 216 | 231 | 236 | 246 | 246 | 245 | 4.31% |
| Respiratory system dysfunction | 441 | 440 | 463 | 477 | 463 | 465 | 470 | 466 | 473 | 465 | 448 | 0.14% |
| Renal system dysfunction | 74 | 81 | 91 | 104 | 109 | 125 | 135 | 146 | 161 | 172 | 185 | 13.51% |
| Hepatic system dysfunction | 86 | 76 | 77 | 75 | 73 | 77 | 78 | 79 | 80 | 82 | 82 | -0.42% |
| Metabolic system dysfunction | 40 | 40 | 35 | 37 | 35 | 35 | 33 | 34 | 36 | 37 | 36 | -0.88% |
| Central nervous system dysfunction | 24 | 24 | 23 | 25 | 26 | 28 | 29 | 30 | 33 | 35 | 35 | 4.10% |
| Hematologic system dysfunction | 35 | 31 | 30 | 32 | 31 | 34 | 34 | 35 | 41 | 41 | 43 | 2.1% |
Figure 2A. Changes in population incidence of specific organ dysfunction among patients with sepsis, from 2002 to 2012. (A) High to moderate incidence trends.
Figure 2B. (B) Low incidence trends.
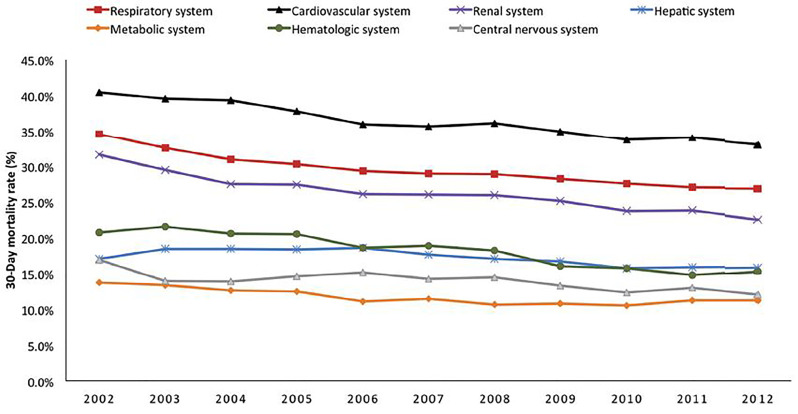
The Mortality of Septic Patients With Specific Organ Dysfunction and Mortality
Figure 3 and Table 3 illustrated the 30-day all-causes mortality of different types of organ dysfunctions. The mortality rates for all kinds of organ dysfunctions were trending downward in general. The mortality of central nervous system dysfunction decreased at the fastest rate (annual mortality decrease: -2.61%), followed by renal system (-2.59%), hematologic system (-2.37%), respiratory system (-1.99%), metabolic system (-1.65%), cardiovascular system (-1.63%), and hepatic system dysfunction (-0.58%).
Figure 3. Changes in mortality rate of specific organ dysfunction among patients with sepsis, from 2002 to 2012: temporal trend of mortality rate.
Table 3. Changes in mortality rate of specific organ dysfunction among patients with sepsis, from 2002 to 2012: mortality rates.
| 2002 | 2003 | 2004 | 2005 | 2006 | 2007 | 2008 | 2009 | 2010 | 2011 | 2012 | Annual change | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Cardiovascular system dysfunction | 40.5% | 39.6% | 39.3% | 37.8% | 36.0% | 35.7% | 36.1% | 35.0% | 33.8% | 34.1% | 33.2% | -1.63% |
| Respiratory system dysfunction | 34.5% | 32.6% | 30.9% | 30.3% | 29.4% | 29.0% | 28.9% | 28.3% | 27.6% | 27.1% | 27.0% | -1.99% |
| Renal system dysfunction | 31.6% | 29.5% | 27.5% | 27.5% | 26.1% | 26.0% | 25.9% | 25.2% | 23.8% | 23.8% | 22.6% | -2.59% |
| Hepatic system dysfunction | 17.1% | 18.4% | 18.5% | 18.4% | 18.6% | 17.6% | 17.1% | 16.7% | 15.7% | 15.8% | 16.0% | -0.58% |
| Metabolic system dysfunction | 13.8% | 13.4% | 12.6% | 12.5% | 11.1% | 11.5% | 10.7% | 10.8% | 10.5% | 11.2% | 11.3% | -1.65% |
| Central nervous system dysfunction | 16.9% | 13.9% | 13.9% | 14.6% | 15.2% | 14.2% | 14.5% | 13.3% | 12.4% | 13.0% | 12.1% | -2.61% |
| Hematologic system dysfunction | 20.7% | 21.5% | 20.6% | 20.5% | 18.6% | 18.9% | 18.2% | 16.0% | 15.7% | 14.8% | 15.3% | -2.37% |
Discussion
After the development of sepsis-3 consensus, acute organ dysfunction has become an essential part of sepsis diagnosis. By using a large database encompassing the population of an entire nation for eleven years, we were able to determine the true population- based incidence and mortality trend of organ dysfunctions among patients with sepsis. We determined respiratory system (65.6%), cardiovascular system (30.5%), and renal system dysfunctions (18.3%) were the leading three organ dysfunctions associated with sepsis. However, renal system dysfunction (annual increase: 13.35%), cardiovascular dysfunction (4.31%), and central nervous system (4.10%) were the three organ dysfunctions that increased at a fastest rate during the study period. Meanwhile, the annual incidence of sepsis increased by 18.7%, from 28,023 in 2002 to 35,650 in 2012.[10] In a previous work,[10] we have shown the incidence of sepsis increased from 600.5 per 100,000 persons in 2002 to 712.9 per 100,000 in 2012 after adjusting for the change of population age and gender structure of over the study period. This work is an extension of previous work, in which we aimed to describe the change of incidence of mortality of different organ dysfunction among patients with sepsis. The knowledge on the epidemiological change of organ dysfunction in sepsis patients will have important public health implications.
Compared with prior studies, Kumar et al.[19] analyzed the US Nationwide Inpatient Sample study showing that respiratory, renal and cardiovascular dysfunction were the most common organ system dysfunctions. In addition, except for the acute respiratory failure showing a downward trend between 2000 and 2007 (from 52.8 to 47.6%), other organ dysfunctions increased with time, especially for renal failure (from 33.4 to 48.6%) and cardiovascular dysfunctions (from 30.3 to 41.7%). Rhee et al.[3] analyzed electronic medical record database and found acute kidney injury (AKI), shock, and acute respiratory failure requiring MV were the leading three organ dysfunctions among sepsis patients, with a prevalence of 43.5, 28.4 and 26.0% respectively. In a national study of Norwegian hospitals during the years 2011 and 2012,[20] cardiovascular dysfunction was the most common organ dysfunction (48.5%), followed by respiratory system dysfunction (32.0%) and renal dysfunction (24.8%). Another nationwide population-based analysis of severe sepsis in Spain from 2006 to 2011 showed that respiratory failure was the most common dysfunctional organ (50.5%), followed by cardiovascular system (44.7%) and renal system (40.5%).[21] Among the change of different organ dysfunction, only renal failure had considerable increase with time (from 36.5 to 46.5%).
Taken together, the results of our study were consistent with previous findings. Acute respiratory, cardiovascular, and renal systems dysfunctions were the three most common types of organ dysfunctions in patients with sepsis. In addition, all of these studies showed an upward trend for incidence or prevalence of renal system dysfunction. This rise might be partially explained by increased awareness of AKI, improved ascertainment in administrative data and greater sensitivity of consensus diagnostic and classification schemes. Furthermore, an increasing aging population, a growing percentage with chronic kidney disease, and an expanding characterization of modifiable risk factors, such as administration of contrast media and exposure to nephrotoxins and broad-spectrum antibiotic,[22] had contributed to the increase incidence of renal system dysfunction.
Furthermore, we observed a decreasing trend of sepsis-related mortality similar to previous studies conducted.[3,14,19,20] The causes should, therefore, be multifactorial. The improving outcome of sepsis could be due to implementation of several Surviving Sepsis Campaign recommended interventions such as the use of vasopressor and hemodynamic monitor, conservative transfusion strategy, early and appropriate antibiotic uses, early goal directed therapy.[23,24] In Taiwan, Chen et al. demonstrated that a national education program could cause a significant impact on clinical practice and lead to significant reduction of severe sepsis mortality rate.[14] In addition, we also noted that organ dysfunction specific mortality was gradually decreasing during the study period. These could be benefit from the improvement of various organ supports such as lung protection strategy for acute respiratory distress syndrome,8 the choice and amount of fluids,[12,25] appropriate type and intensity of hemodynamic monitoring,[26] role of adjunctive vasoactive agents for septic shock,[27] and transfusion strategy for hematologic organ dysfunction.[13]
In addition to the decline of overall mortality over time, we observed different trends of mortality decrease for various types of organ dysfunctions. Excluding hepatic dysfunction with an annual mortality decrease of 0.58%, other organ dysfunctions were associated with a more pronounced mortality reduction during the study period with annual mortality decrease of more than 1%. Except for liver transplant, there was limited evidence-based practice with proved benefits to improve liver function during sepsis. This trend indicated that liver support treatment would be an important area for research in improving the outcome of sepsis. Rhee et al.[28] noted the increased awareness of AKI after risk, injury, failure, loss of kidney function, and end-stage kidney disease definition was one of the major causes for the observed increased prevalence of AKI and probable pseudo-improvement of AKI or sepsis related mortality. Hence, there was a strong debate that the incidence of sepsis based on the administrative database was artificially inflated by the code abstraction strategy for renal system dysfunction. We could not totally completely exclude the possibility in our study due to the national education activity of Surviving Sepsis Campaign and several organ dysfunction guidelines increasing the awareness of sepsis, which might lead to improved documentation of sepsis and organ dysfunction. However, we did not have any incentive for quality improvement from the insurance agency to promote the upcoding of sepsis. We also observed that acute renal dysfunction had the sharpest increase during the past decade. Moreover, we did not see the AKI-specific mortality rate decreasing at a similar pace. Therefore, the increase of sepsis could not be entirely explained by the upcoding practice or increased diagnosis of AKI in our database.
Results of this study should be interpreted in light of both strength and weakness. We are the first in literature that estimate the burden of sepsis in a true population based database that could totally avoid the sampling variability. Although we used the most widely validated Angus implementation to identify sepsis cases, previous validation study showed a 71% positive predictive value. The sensitivity was estimated at 50%, but with other coding implementations had even poor sensitivity. We acknowledged that Angus implementation does identify a population predominantly comprised of patients with severe sepsis, but not a pure sample. The burden of sepsis patients may be underestimated given the suboptimal sensitivity.
Conclusions
Respiratory, cardiovascular, and renal system dysfunctions were the three most common and deadly types of organ dysfunctions for patients with sepsis. The different types did not increase in parallel with renal system dysfunction increasing at the sharpest rate and posing a great public health concern. Findings of our study should inform the allocation of research and healthcare resource for different types of organ dysfunctions and also warrant the search of underlying cause for the rapid increase of acute renal dysfunction among sepsis patients for future prevention.
Acknowledgments
We thank the staff of the Core Labs at the Department of Medical Research in National Taiwan University Hospital for technical support, Medical Wisdom Consulting Group for technical assistance in statistical analysis, and National Taiwan University Hospital Health Data Science Research Group for advice on study design.
Funding
This work was supported by Taiwan Ministry of Science and Technology Grants, MOST-104-2314-B- 002-039-MY3 and MOST 107-2314-B-002-196., the research grant of National Taiwan University Hospital Yunlin Branch, NTUHYL108. S006, and the research grant of Far Eastern Memorial Hospital, FEMH- 2019-C-038. No funding bodies had any role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Availability of Data and Materials
The datasets used during the current study are available from the corresponding author upon reasonable request.
Authors’ Contributions
(1) Chien-Chang Lee designed the study, obtained funding, drafted the analytical plan, guided the statistical analysis, interpreted the data, and wrote the draft. (2) Tzu-Chun Hsu, Alvaro E. Galvis, Debra Yen, Wan-Ting Hsu, and Jason Wang helped to collect data in this study. (3) Alvaro E. Galvis and Debra Yen helped with language editing and provided critical comments. (4) Wan-Ting Hsu and Jason Wang conducted statistical analysis. (5) Chia-Hung Yo, Chih- Cheng Lai, Cheng-Yi Wang, and Chien-Chang Lee analyzed the data, provided critical feedback, and authorized the final manuscript. (6) Chia-Hung Yo and Chih-Cheng Lai contributed equally to the work.
Ethics and Consent
This study was approved by the institutional review board of National Taiwan University Hospital (no. 201402032RINA).
Conflicts of Interest Statement
The authors declare that they had no competing interests when conducting the research.
Appendix 1.ICD-9-CM/procedure codes of organ dysfunction associated with sepsis.
Cardiovascular dysfunction/shock
785.5, Shock
458, Hypotension
Acute respiratory dysfunction
96.7, Mechanical ventilation
57001B, 57002B, 57023B, 57029C, Use of ventilators
Central nervous system dysfunction
348.3, Neurologic encephalopathy
293, Transient organic psychosis
348.1, Anoxic brain damage
Hematologic system dysfunction
287.4, Hematologic secondary thrombocytopenia
287.5, Thrombocytopenia, unspecified
286.9, Other/unspecified coagulation defect
286.6, Defibrination syndrome
Hepatic system dysfunction
570, Hepatic acute and subacute necrosis of liver
572.2, Hepatic encephalopathy
572.4, Hepatorenal syndrome
572.8, Other squeal of chronic liver disease
573.4, 573.8, Hepatic infarction
V42.7, Liver replaced by transplant
Renal system dysfunction
584, Acute renal failure
58014C, Use of CVVH
Metabolic system dysfunction
250.1, Diabetic ketoacidosis
250.2, Hyperosmolar hyperglycemic state
References
- 1.Angus Derek C., van der Poll Tom. Severe Sepsis and Septic Shock. New England Journal of Medicine. 2013 Aug 29;369(9) doi: 10.1056/nejmra1208623. [DOI] [PubMed] [Google Scholar]
- 2.Russell James A. Management of Sepsis. New England Journal of Medicine. 2006 Oct 19;355(16) doi: 10.1056/nejmra043632. [DOI] [PubMed] [Google Scholar]
- 3.Rhee Chanu, Dantes Raymund, Epstein Lauren, Murphy David J., Seymour Christopher W., Iwashyna Theodore J., Kadri Sameer S., Angus Derek C., Danner Robert L., Fiore Anthony E., Jernigan John A., Martin Greg S., Septimus Edward, Warren David K., Karcz Anita, Chan Christina, Menchaca John T., Wang Rui, Gruber Susan, Klompas Michael. Incidence and Trends of Sepsis in US Hospitals Using Clinical vs Claims Data, 2009-2014. JAMA. 2017 Oct 03;318(13) doi: 10.1001/jama.2017.13836. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Gaieski David F., Edwards J. Matthew, Kallan Michael J., Carr Brendan G. Benchmarking the Incidence and Mortality of Severe Sepsis in the United States*. Critical Care Medicine. 2013 May;41(5) doi: 10.1097/ccm.0b013e31827c09f8. [DOI] [PubMed] [Google Scholar]
- 5.Page David B., Donnelly John P., Wang Henry E. Community-, Healthcare-, and Hospital-Acquired Severe Sepsis Hospitalizations in the University HealthSystem Consortium. Critical Care Medicine. 2015 Sep;43(9) doi: 10.1097/ccm.0000000000001164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Shen Hsiu-Nien, Lu Chin-Li, Yang Hsi-Hsing. Epidemiologic Trend of Severe Sepsis in Taiwan From 1997 Through 2006. Chest. 2010 Aug;138(2) doi: 10.1378/chest.09-2205. [DOI] [PubMed] [Google Scholar]
- 7.Singer Mervyn, Deutschman Clifford S., Seymour Christopher Warren, Shankar-Hari Manu, Annane Djillali, Bauer Michael, Bellomo Rinaldo, Bernard Gordon R., Chiche Jean-Daniel, Coopersmith Craig M., Hotchkiss Richard S., Levy Mitchell M., Marshall John C., Martin Greg S., Opal Steven M., Rubenfeld Gordon D., van der Poll Tom, Vincent Jean-Louis, Angus Derek C. The Third International Consensus Definitions for Sepsis and Septic Shock (Sepsis-3) JAMA. 2016 Feb 23;315(8) doi: 10.1001/jama.2016.0287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Shankar-Hari M., Harrison D.A., Rubenfeld G.D., Rowan K. Epidemiology of sepsis and septic shock in critical care units: comparison between sepsis-2 and sepsis-3 populations using a national critical care database. British Journal of Anaesthesia. 2017 Oct;119(4) doi: 10.1093/bja/aex234. [DOI] [PubMed] [Google Scholar]
- 9.Churpek Matthew M., Snyder Ashley, Sokol Sarah, Pettit Natasha N., Edelson Dana P. Investigating the Impact of Different Suspicion of Infection Criteria on the Accuracy of Quick Sepsis-Related Organ Failure Assessment, Systemic Inflammatory Response Syndrome, and Early Warning Scores*. Critical Care Medicine. 2017 Nov;45(11) doi: 10.1097/ccm.0000000000002648. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lee Chien-Chang, Yo Chia-Hung, Lee Meng-tse Gabriel, Tsai Kuang-Chau, Lee Shih-Hao, Chen Yueh-Sheng, Lee Wan-Chien, Hsu Tzu-Chun, Lee Sie-Hue, Chang Shy-Shin. Adult sepsis – A nationwide study of trends and outcomes in a population of 23 million people. Journal of Infection. 2017 Nov;75(5) doi: 10.1016/j.jinf.2017.08.012. [DOI] [PubMed] [Google Scholar]
- 11.Amato Marcelo Britto Passos, Barbas Carmen Silvia Valente, Medeiros Denise Machado, Magaldi Ricardo Borges, Schettino Guilherme Paula, Lorenzi-Filho Geraldo, Kairalla Ronaldo Adib, Deheinzelin Daniel, Munoz Carlos, Oliveira Roselaine, Takagaki Teresa Yae, Carvalho Carlos Roberto Ribeiro. Effect of a Protective-Ventilation Strategy on Mortality in the Acute Respiratory Distress Syndrome. New England Journal of Medicine. 1998 Feb 05;338(6) doi: 10.1056/nejm199802053380602. [DOI] [PubMed] [Google Scholar]
- 12.Wiedemann HP, Wheeler AP, Bernard GR, et al Comparison of Two Fluid-Management Strategies in Acute Lung Injury. New England Journal of Medicine. 2006 Jun 15;354(24) doi: 10.1056/nejmoa062200. [DOI] [PubMed] [Google Scholar]
- 13.Holst Lars B., Haase Nicolai, Wetterslev Jørn, Wernerman Jan, Guttormsen Anne B., Karlsson Sari, Johansson Pär I., Åneman Anders, Vang Marianne L., Winding Robert, Nebrich Lars, Nibro Helle L., Rasmussen Bodil S., Lauridsen Johnny R.M., Nielsen Jane S., Oldner Anders, Pettilä Ville, Cronhjort Maria B., Andersen Lasse H., Pedersen Ulf G., Reiter Nanna, Wiis Jørgen, White Jonathan O., Russell Lene, Thornberg Klaus J., Hjortrup Peter B., Müller Rasmus G., Møller Morten H., Steensen Morten, Tjäder Inga, Kilsand Kristina, Odeberg-Wernerman Suzanne, Sjøbø Brit, Bundgaard Helle, Thyø Maria A., Lodahl David, Mærkedahl Rikke, Albeck Carsten, Illum Dorte, Kruse Mary, Winkel Per, Perner Anders. Lower versus Higher Hemoglobin Threshold for Transfusion in Septic Shock. New England Journal of Medicine. 2014 Oct 09;371(15) doi: 10.1056/nejmoa1406617. [DOI] [PubMed] [Google Scholar]
- 14.Chen Yu-Chun, Chang Shih-Chieh, Pu Christy, Tang Gau-Jun. Salluh Jorge IF., editor. The Impact of Nationwide Education Program on Clinical Practice in Sepsis Care and Mortality of Severe Sepsis: A Population-Based Study in Taiwan. PLoS ONE. 2013 Oct 04;8(10) doi: 10.1371/journal.pone.0077414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Angus Derek C., Linde-Zwirble Walter T., Lidicker Jeffrey, Clermont Gilles, Carcillo Joseph, Pinsky Michael R. Epidemiology of severe sepsis in the United States: Analysis of incidence, outcome, and associated costs of care. Critical Care Medicine. 2001 Jul;29(7) doi: 10.1097/00003246-200107000-00002. [DOI] [PubMed] [Google Scholar]
- 16.Angus Derek C. The Lingering Consequences of Sepsis. JAMA. 2010 Oct 27;304(16) doi: 10.1001/jama.2010.1546. [DOI] [PubMed] [Google Scholar]
- 17.Sands Kenneth E. Epidemiology of Sepsis Syndrome in 8 Academic Medical Centers. JAMA: The Journal of the American Medical Association. 1997 Jul 16;278(3) doi: 10.1001/jama.1997.03550030074038. [DOI] [PubMed] [Google Scholar]
- 18.Iwashyna Theodore J., Odden Andrew, Rohde Jeffrey, Bonham Catherine, Kuhn Latoya, Malani Preeti, Chen Lena, Flanders Scott. Identifying Patients With Severe Sepsis Using Administrative Claims. Medical Care. 2014 Jun;52(6) doi: 10.1097/mlr.0b013e318268ac86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kumar Gagan, Kumar Nilay, Taneja Amit, Kaleekal Thomas, Tarima Sergey, McGinley Emily, Jimenez Edgar, Mohan Anand, Khan Rumi Ahmed, Whittle Jeff, Jacobs Elizabeth, Nanchal Rahul. Nationwide Trends of Severe Sepsis in the 21st Century (2000–2007) Chest. 2011 Nov;140(5) doi: 10.1378/chest.11-0352. [DOI] [PubMed] [Google Scholar]
- 20.Knoop Siri Tandberg, Skrede Steinar, Langeland Nina, Flaatten Hans Kristian. Brakenridge Scott., editor. Epidemiology and impact on all-cause mortality of sepsis in Norwegian hospitals: A national retrospective study. PLOS ONE. 2017 Nov 17;12(11) doi: 10.1371/journal.pone.0187990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Bouza Carmen, López-Cuadrado Teresa, Saz-Parkinson Zuleika, Amate-Blanco José María. Epidemiology and recent trends of severe sepsis in Spain: a nationwide population-based analysis (2006-2011) BMC Infectious Diseases. 2014 Dec;14(1) doi: 10.1186/s12879-014-0717-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Rewa Oleksa, Bagshaw Sean M. Acute kidney injury—epidemiology, outcomes and economics. Nature Reviews Nephrology. 2014 Jan 21;10(4) doi: 10.1038/nrneph.2013.282. [DOI] [PubMed] [Google Scholar]
- 23.Dellinger R. Phillip, Carlet Jean M., Masur Henry, Gerlach Herwig, Calandra Thierry, Cohen Jonathan, Gea-Banacloche Juan, Keh Didier, Marshall John C., Parker Margaret M., Ramsay Graham, Zimmerman Janice L., Vincent Jean-Louis, Levy Mitchell M. Surviving Sepsis Campaign guidelines for management of severe sepsis and septic shock. Critical Care Medicine. 2004 Mar;32(3) doi: 10.1097/01.ccm.0000117317.18092.e4. [DOI] [PubMed] [Google Scholar]
- 24.Dellinger R. Phillip, Levy Mitchell M., Rhodes Andrew, Annane Djillali, Gerlach Herwig, Opal Steven M., Sevransky Jonathan E., Sprung Charles L., Douglas Ivor S., Jaeschke Roman, Osborn Tiffany M., Nunnally Mark E., Townsend Sean R., Reinhart Konrad, Kleinpell Ruth M., Angus Derek C., Deutschman Clifford S., Machado Flavia R., Rubenfeld Gordon D., Webb Steven A., Beale Richard J., Vincent Jean-Louis, Moreno Rui. Surviving Sepsis Campaign Critical Care Medicine. 2013 Feb;41(2) doi: 10.1097/ccm.0b013e31827e83af. [DOI] [Google Scholar]
- 25.Rochwerg Bram, Alhazzani Waleed, Sindi Anees, Heels-Ansdell Diane, Thabane Lehana, Fox-Robichaud Alison, Mbuagbaw Lawrence, Szczeklik Wojciech, Alshamsi Fayez, Altayyar Sultan, Ip Wang-Chun, Li Guowei, Wang Michael, Wludarczyk Anna, Zhou Qi, Guyatt Gordon H., Cook Deborah J., Jaeschke Roman, Annane Djillali. Fluid Resuscitation in Sepsis. Annals of Internal Medicine. 2014 Sep 02;161(5) doi: 10.7326/m14-0178. [DOI] [PubMed] [Google Scholar]
- 26.Shah Monica R., Hasselblad Vic, Stevenson Lynne W., Binanay Cynthia, O’Connor Christopher M., Sopko George, Califf Robert M. Impact of the Pulmonary Artery Catheter in Critically Ill Patients. JAMA. 2005 Oct 05;294(13) doi: 10.1001/jama.294.13.1664. [DOI] [PubMed] [Google Scholar]
- 27.Hammond Drayton A., Ficek Oktawia A., Painter Jacob T., McCain Kelsey, Cullen Julia, Brotherton Amy L., Kakkera Krishna, Chopra Divyan, Meena Nikhil. Prospective Open-label Trial of Early Concomitant Vasopressin and Norepinephrine Therapy versus Initial Norepinephrine Monotherapy in Septic Shock. Pharmacotherapy: The Journal of Human Pharmacology and Drug Therapy. 2018 Apr 30;38(5) doi: 10.1002/phar.2105. [DOI] [PubMed] [Google Scholar]
- 28.Rhee Chanu, Murphy Michael V., Li Lingling, Platt Richard, Klompas Michael. Improving documentation and coding for acute organ dysfunction biases estimates of changing sepsis severity and burden: a retrospective study. Critical Care. 2015 Sep 14;19(1) doi: 10.1186/s13054-015-1048-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets used during the current study are available from the corresponding author upon reasonable request.