Abstract
Introduction
About 463 million adults aged 20–79 have diabetes globally. Mental disorders often exist in patients with diabetes as comorbidities, which can lead to aggravation of the diseases, increased difficulties in treatment, as well as elevated mortality rates. Music intervention has been applied in the treatment of comorbidities for 12 years now, but there are still no recommendations due to the lack of evidence. Thus, a meta-analysis is necessary to evaluate the effect of music intervention in treating mental disorders of patients with diabetes.
Methods and analysis
We will search the following nine online electronic databases from their inception until March 2020: PubMed, Web of Science, Embase, EBSCO, Cochrane Library, Chinese National Knowledge Infrastructure, Wanfang Database, Chinese Scientific Journal Database (VIP) and Chinese Biomedical and Medical Database. We also plan to search other relevant resources, including grey literature and the reference lists of relevant publications. Only randomised controlled trials of music intervention to treat depression or anxiety in patients with diabetes will be involved. The primary outcomes include the depression score and anxiety score measured on certain scales, and the secondary outcome is safety. Data extraction will be independently implemented by two researchers. The risk of bias will be evaluated through the Cochrane Collaboration’s Risk of Bias tool. Eventually, all the data will be analysed via the Review Manager V.5.3 software.
Ethics and dissemination
This meta-analysis will provide information about applying music intervention to treat depression or anxiety in patients with diabetes. No ethical approval is required because this meta-analysis is based on published data. The results of this systematic review will be published in a peer-reviewed journal.
PROSPERO registration number
CRD42019146439
Keywords: diabetes & endocrinology, mental health, complementary medicine
Strengths and limitations of this study.
This meta-analysis will be the first to provide evidence on the effectiveness and safety of applying music intervention to treat depression or anxiety in patients with diabetes.
Based on our comprehensive search strategy, the relevant original studies will be included.
Two authors will separately implement data extraction and estimation of the risk of bias.
We will only cover randomised controlled trials in this study.
A language bias may exist in this meta-analysis because it will include only the studies in English and Chinese due to the language barrier.
Introduction
According to the newest ‘IDF Diabetes Atlas (ninth edition)’ published by the International Diabetes Federation (IDF), about 463 million adults aged 20–79 have diabetes mellitus globally (1 in 11).1 Diabetes has a well-known significant influence on the patient’s quality of life due to its complications, such as retinopathy, cardiovascular, neurological or renal diseases, as well as foot ulcers, which may result in the amputation of lower extremity.2
In addition to the physical complications, patients with diabetes may also develop mental disorders as comorbidities. Some studies have indicated that depression is more prevalent in patients with diabetes compared with patients without diabetes.3 4 Meanwhile, depression could also increase the risk of diabetes,5–7 which suggests a bidirectional diabetes–depression relation; a similar relation has been confirmed between anxiety and diabetes: people with diabetes are more susceptible to concurrent anxiety,8 9 while anxiety is a risk factor of diabetes.10 Individuals with chronic diseases who have comorbid depression or anxiety have obviously higher healthcare utilisation, functional disability, work absence and mortality risk than healthy ones.11 12
When it comes to the treatment of diabetes with comorbid depression or anxiety, conventional glucose-lowering treatments combined with antidepressants, antianxiety medications or psychological intervention are the routine treatments.13 14 Music intervention is also a successful therapy, which can be divided into two major categories: music therapy and music medicine.15 The official definition of music therapy is the ‘clinical and evidence-based use of music interventions to accomplish individualised goals within a therapeutic relationship by a credentialed professional who has completed an approved music therapy programme’.16 Based on the patient’s condition, a trained music therapist conducts the treatment by choosing the type of music, the form of music presentation (prerecorded or live) and the treatment setting (singing, playing instruments, composing, etc), ultimately resulting in a therapeutic scheme that is best suited for the patient. On the other hand, music medicine is defined as passive listening to prerecorded music, which can be independently implemented by medical or healthcare professionals instead of music therapists.17 In brief, music therapy focuses on active music therapy and personalised treatments, while music medicine belongs to passive music listening and non-personalised therapy. It is important to emphasise the distinction between music therapy and music medicine because some studies suggest that the effect of the former is better than the latter with regard to many outcomes.18 19
A lot of studies suggested that music, with all its types, demonstrates a remarkable effect in alleviating depression and anxiety among patients with various diseases.20–22 As for diabetes, recent studies have shown that music intervention could improve fasting blood glucose and systolic blood pressure in patients with diabetes.23 24 Good control of blood glucose and blood pressure can effectively reduce the incidence of serious complications of diabetes.25
Previous research on music psychology showed the special potential of music. As a stimulus, music can not only trigger a variety of emotional experiences,26 27 but it can also strengthen the ability to deal with negative emotions in everyday life.28 The proposed mechanisms behind the effects of music intervention on depression and anxiety span across several domains. First, music intervention can exert neurophysiological and neurochemical effects, such as triggering the release of endorphin29 and stimulating cognitive functioning.30 Second, music intervention can promote positive self-conscious emotions including enhancing the sense of happiness31 and activating self-efficacy and self-confidence through experiencing success.32 Lastly, music intervention can enhance the sociable aspects, such as interaction skills33 and interpersonal relationships.34 Furthermore, many published studies indicated that music intervention combined with the diabetic routine treatments could improve the depression score, anxiety score and the values of fasting glucose and glycosylated haemoglobin (HbA1c).35 36
By searching the literature, it can be found that some reviews evaluated the effect of music intervention on the patients with mental disorders,37–39 while no related systematic reviews or meta-analyses can be found about the effect of music intervention on the mental health of patients with diabetes. Therefore, a review that can show music intervention to be both valid and with few side effects would be useful to indicate that this intervention is worth being promoted and clinically applied to benefit more people with this easy-operated method.
Objective
In this review, we present a meta-analysis to systematically assess the effect of music intervention and compare the effects of music therapy and those of music medicine on depression and anxiety of patients with diabetes. Additionally, it serves to establish an evidence reference for related guidelines.
Methods and analysis
Study registration
Our protocol for the meta-analysis has been registered in the International Prospective Register of Systematic Reviews (PROSPERO) with the registration ID of CRD42019146439. This protocol has been strictly planned based on the Preferred Reporting Items for Systematic Reviews and Meta-Analysis Protocols (PRISMA-P)40 statement guidelines. The results will be reported in accordance with the PRISMA Statement for Reporting Systematic Reviews and Meta-Analyses of Studies That Evaluate Healthcare Interventions.41
Eligibility criteria
Type of studies
This analysis will merely cover the randomised controlled trials (RCTs) in English or Chinese, except for Quasi-RCTs and cluster RCTs. The experiments on animals and non-randomised clinical trials will not be considered. The articles with a significant overlap with other articles through printing or e-publishing will not be included. Duplicate publications, in which the results originated from a single experiment but were measured by other standards and then published as disparate papers, will also be excluded. The main choice is original publications, regardless of the publication status.
Type of participants
Patients with Diabetes along with depression or anxiety symptoms, regardless of the type of diabetes, gender, age, race, economic ability and education level. Patients with other diseases or healthy persons will be excluded.
Type of interventions and controls
The interventions include music intervention (music therapy or music medicine, no restriction on the type of music) alone or combined with other interventions that refer to the following therapies: (1) routine treatments for diabetes, which mainly include pharmacologic approaches to glycaemic treatment, diabetes self-management education and support, and others, according to the newest guideline of the American Diabetes Association42 43; and (2) other therapies such as acupoint therapy,44 metabolic surgery,45 and so on. When the used intervention is the music intervention alone, the controls can be people with no treatment, placebo or other active therapies, while the same therapies should be used with the controls when the music intervention is used combined with active therapies.
Type of outcome measures
Since this review aims at the systematic assessment of the effect of music intervention on depression or anxiety in patients with diabetes, we will choose the depression and anxiety scores as the primary outcomes, which can indicate the degree of depression and anxiety on certain scales.
The depression score is measured using the self-rating depression scale (SDS), Hamilton depression scale (HAMD) or other validated scales for depression. The anxiety score is measured using the self-rating anxiety scale (SAS), Hamilton anxiety scale (HAMA) or other validated scales for anxiety.
The secondary outcome is the safety, measured via the incidence of adverse effects.
Search methods
Search resources
The following nine online electronic databases will be searched from their inception to March 2020: PubMed, Web of Science, Embase, EBSCO, Cochrane Library, Chinese National Knowledge Infrastructure (CNKI), Wanfang Database, Chinese Scientific Journal Database (VIP) and Chinese Biomedical and Medical Database. We also plan to search other relevant resources as far as possible, including: (1) grey literature (like conference literature and dissertations) from the following four sources—OpenGrey (www.opengrey.eu/), CNKI (www.cnki.net), Open Access Theses and Dissertations (oatd.org), and the British Library EThOS (ethos.bl.uk/); (2) the reference lists of relevant publications for additional studies.
Search strategies
The search strategy will include the MeSH terms of diabetes mellitus, depression, anxiety, music therapy, music and singing, combined with their respective free-text terms. The search details of PubMed are simplified in table 1.
Table 1.
Example of PubMed search strategy
| Number | Search terms |
| #1 | ‘Diabetes Mellitus’(MeSH) |
| #2 | ‘Depression’(MeSH) OR Depressions(Title/Abstract) OR Depressive Symptoms(Title/Abstract) OR Depressive Symptom(Title/Abstract) OR Symptom, Depressive(Title/Abstract) OR Symptoms, Depressive(Title/Abstract) OR Emotional Depression(Title/Abstract) OR Depression, Emotional(Title/Abstract) OR Depressions, Emotional(Title/Abstract) OR Emotional Depressions(Title/Abstract) |
| #3 | ‘Anxiety’(MeSH) OR Hypervigilance(Title/Abstract) OR Nervousness(Title/Abstract) |
| #4 | #2 OR #3 |
| #5 | ‘Music Therapy’(MeSH) OR Therapy, Music(Title/Abstract) |
| #6 | ‘Music’(MeSH) OR music intervention(Title/Abstract) OR music medicine(Title/Abstract) OR music listening(Title/Abstract) OR audio recording(Title/Abstract) OR mp3 hearing(Title/Abstract) |
| #7 | ‘Singing’(Mesh) OR sing(Title/Abstract) OR sings(Title/Abstract) OR song(Title/Abstract) OR compose(Title/Abstract) OR composing(Title/Abstract) |
| #8 | #5 OR #6 OR #7 |
| #9 | randomised controlled trial (Publication Type) OR randomised(Title/Abstract) OR placebo(Title/Abstract) |
| #10 | #1 AND #4 AND #8 AND #9 |
Data collection and analysis
Studies selection
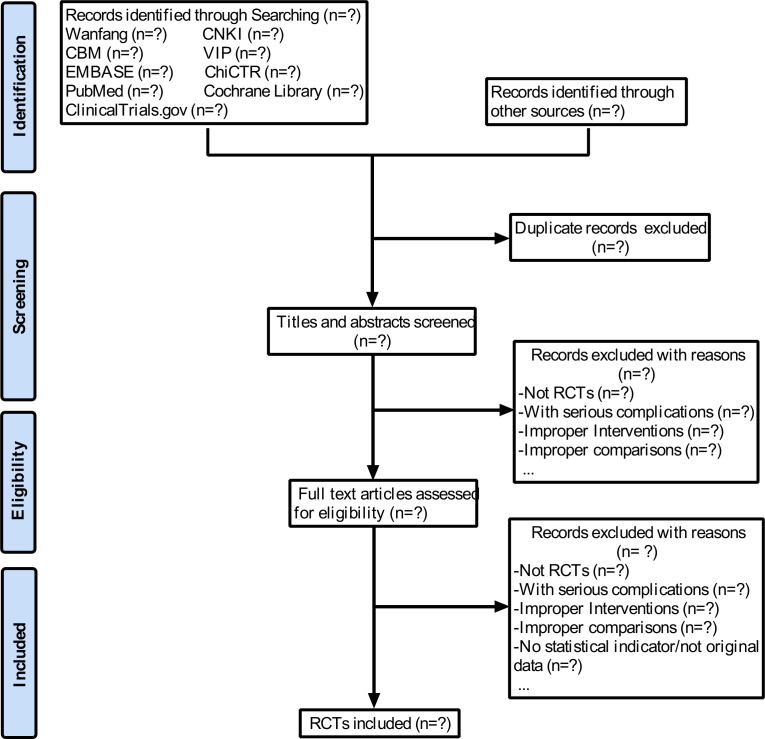
First, two researchers (L-yZ and YT) will respectively screen the keywords, titles and abstracts of all the obtained studies using the EndNote X9 software and determine whether the trials comply with the inclusion criteria. Then, we will also get access to the full text of all the studies with possible relevance for further assessment. Each of the excluded studies will be noted with the exclusion reasons. Any disagreements will be settled through consensus or referral to a third researcher (XF). The specific selection steps are presented in figure 1.
Figure 1.
Flowchart to present the search process. CBM, Chinese Biomedical and Medical Database; CNKI, Chinese National Knowledge Infrastructure; RCTs, randomised controlled trials.
Data extraction
Two researchers (L-yZ and YT) will independently extract and tabulate the following data items using the Microsoft Excel 2016 software:
General information (including the publication year and name of the first author).
Study design (including the random method, allocation concealment, and blinding).
Participants (including the sample size, gender, age, area, depression score, anxiety score and course of disease).
Treatment (including the interventions, controls, music type and the course of treatment).
Outcomes (including the depression score, anxiety score and safety).
In the case of different opinions, the final decision will be made by the third researcher (XF).
Assessment of risk of bias
In order to evaluate the risk of bias of all the included RCT studies, the Cochrane Collaboration’s Risk of Bias tool46 will be applied by two authors (L-zW and YZ). The assessed domains will be the following: sequence generation, allocation concealment, blinding of participants and personnel, blinding of outcome assessors, incomplete outcome data, selective reporting and other sources of bias. The assessments will be classified into ‘low’, ‘unclear’ or ‘high’ risk.
Measures of treatment effect
Considering that all the outcomes (depression score, anxiety score and safety) are continuous variables, when the quantitative data are from the same measurement method or a small data scale, the mean difference (MD) and 95% CI will be calculated. Otherwise, the standardised mean difference (SMD) and 95% CI will be calculated.
Unit of analysis issues
For the standard research that has one experimental group with one control group, the unit of analysis is the individual. For the multiarm study with more than two intervention groups, the recommended method is to create a single pairwise comparison by combining the groups.
Dealing with missing data
If the required data are unavailable from the literature, one researcher (YZ) will contact the corresponding author via email and ask for further information.
Assessment of heterogeneity
A meta-analysis will be implemented if the included studies are adequately homogenous. The p value and I² are used to assess the heterogeneity of the statistics. The heterogeneity is considered to be acceptable when p value >0.05 and I²≤50% and significant when p value <0.05 or I²>50%.
Assessment of reporting bias
The publication bias will be implemented if more than 10 studies are included through a funnel plot.
Data synthesis
The Review Manager V.5.3 software, provided by the Cochrane collaboration, will be used to analyse the data. If the included studies are adequately homogenous, then a fixed-effects model will be used for the statistical combination. Since all the outcomes are continuous variables in this meta-analysis, we will calculate the MD and 95% CI when the outcomes are from the same measurement method or a small data scale. Otherwise, we will calculate the SMD and 95% CI. If there is significant heterogeneity among the included studies, subgroup or sensitivity analyses will be performed. If a meta-analysis is unavailable, descriptive summaries will be provided.
Subgroup analysis
The subgroup analyses are planned as follows:
The type of music intervention (music therapy or music medicine).
The type of scales (SDS, HAMD, SAS, HAMA or other validated depression or anxiety scales).
The different age groups.
Sensitivity analysis
The sensitivity analyses will be performed by including or excluding a specific study, such as a study without clear allocation concealment or a randomization method, to observe whether the results change.
Evaluating the evidence
The Grading of Recommendations Assessment, Development and Evaluation (GRADE) guideline will be used to evaluate the quality of evidence.47 Based on the GRADE method, the quality of evidence can be assessed by four levels: ‘high’, ‘medium’, ‘low’ and ‘very low’. The GRADE profiler V.3.2 software will be applied for the analysis.
Patient and public involvement
No patients or volunteers from the public will be involved in this study.
Discussion
Depression and anxiety often occur independently or simultaneously during the development of many chronic diseases. In recent years, an increasing number of studies have been investigating the comorbid depression or anxiety in diabetics. This increased interest is not only because the bidirectional relationship between depression/anxiety and diabetes can lead to deterioration of the diseases, increased difficulties in treatment, as well as elevated mortality rates,48–51 but also because the therapeutic methods for treating the comorbidities are limited and unsatisfactory. On the one hand, some antidepressant drugs, such as nortriptyline and sertraline, may complicate the glycaemic control.52 On the other hand, psychotherapy that is based on verbal communication requires a professional psychiatrist and is expensive.
Music intervention has been proved by many studies to have a beneficial effect on depression and anxiety, as it strengthens the awareness and sensitiveness for positive emotions.53 Noticeably, a few studies also showed that music intervention can simultaneously reduce blood glucose and HbA1c levels.24 54 Therefore, music intervention is an applicable method to treat depression and anxiety in patients with diabetes. Additionally, this almost side effect-free intervention is safer than pharmacotherapy, easier to be operated and costs less than psychotherapy based on verbal communication; thus, it is conducive to clinical promotion and application.
Although music intervention has been applied in the treatment of depression and anxiety with diabetes for 12 years now,55 there is still no systematic review or meta-analysis to evaluate the potential pros and cons of this therapeutic method. Thus, this study intends to provide strong evidence on the benefits of applying music intervention to treat mental disorders in patients with diabetes and synchronously provide evidence to which related guidelines can refer.
However, a language bias may exist in this meta-analysis because it includes only the studies in English and Chinese due to the language barrier. Therefore, some related studies from the medical databases in other languages might be missed.
In conclusion, this meta-analysis will help to assess the underlying benefits and harms of music intervention on comorbid depression or anxiety in patients with diabetes. Moreover, the results of this study will represent a reference for the guidelines of relevant areas, attracting more attention to the music intervention, and facilitating its clinical application to benefit more patients.
Supplementary Material
Footnotes
Contributors: L-yZ and C-gX contributed to the conception of the study. The manuscript of the protocol was drafted by L-yZ and revised by XF and C-gX. L-yZ and YT will independently screen the potential studies and extract the data from the included studies. L-zW and YZ will assess the risk of bias and accomplish data synthesis. XF will arbitrate any disagreements. C-gX will ensure that no errors occur during the review. All the authors approved the publication of the protocol.
Funding: This study was supported by grants from the Science and Technology Project of Sichuan Province (2019YFS002), the Special Scientific and Technological Research Project of Administration of TCM of Sichuan Province (2018KF003) and the Foundation of Development of Science and Technology of Chengdu University of TCM (2016-D-YY-61).
Competing interests: None declared.
Patient and public involvement: Patients and/or the public were not involved in the design, or conduct, or reporting or dissemination plans of this research.
Patient consent for publication: Not required.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.International Diabetes Federation IDF diabetes atlas. 9th edition, 2019. http://www.diabetesatlas.org/ [Google Scholar]
- 2.World Health Organization Global report on diabetes, 2014. Available: https://www.who.int/news-room/fact-sheets/detail/diabetes [Accessed 9 Nov 2019].
- 3.Ali S, Stone MA, Peters JL, et al. The prevalence of co-morbid depression in adults with type 2 diabetes: a systematic review and meta-analysis. Diabet Med 2006;23:1165–73. 10.1111/j.1464-5491.2006.01943.x [DOI] [PubMed] [Google Scholar]
- 4.Anderson RJ, Freedland KE, Clouse RE, et al. The prevalence of comorbid depression in adults with diabetes: a meta-analysis. Diabetes Care 2001;24:1069–78. 10.2337/diacare.24.6.1069 [DOI] [PubMed] [Google Scholar]
- 5.Knol MJ, Twisk JWR, Beekman ATF, et al. Depression as a risk factor for the onset of type 2 diabetes mellitus. A meta-analysis. Diabetologia 2006;49:837–45. 10.1007/s00125-006-0159-x [DOI] [PubMed] [Google Scholar]
- 6.Cosgrove MP, Sargeant LA, Griffin SJ. Does depression increase the risk of developing type 2 diabetes? Occup Med 2008;58:7–14. 10.1093/occmed/kqm105 [DOI] [PubMed] [Google Scholar]
- 7.Mezuk B, Eaton WW, Albrecht S, et al. Depression and type 2 diabetes over the lifespan: a meta-analysis. Diabetes Care 2008;31:2383–90. 10.2337/dc08-0985 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Grigsby AB, Anderson RJ, Freedland KE, et al. Prevalence of anxiety in adults with diabetes: a systematic review. J Psychosom Res 2002;53:1053–60. 10.1016/s0022-3999(02)00417-8 [DOI] [PubMed] [Google Scholar]
- 9.Smith KJ, Béland M, Clyde M, et al. Association of diabetes with anxiety: a systematic review and meta-analysis. J Psychosom Res 2013;74:89–99. 10.1016/j.jpsychores.2012.11.013 [DOI] [PubMed] [Google Scholar]
- 10.Smith KJ, Deschênes SS, Schmitz N. Investigating the longitudinal association between diabetes and anxiety: a systematic review and meta-analysis. Diabet Med 2018;35:677–93. 10.1111/dme.13606 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Egede LE. Major depression in individuals with chronic medical disorders: prevalence, correlates and association with health resource utilization, lost productivity and functional disability. Gen Hosp Psychiatry 2007;29:409–16. 10.1016/j.genhosppsych.2007.06.002 [DOI] [PubMed] [Google Scholar]
- 12.Naicker K, Johnson JA, Skogen JC, et al. Type 2 diabetes and comorbid symptoms of depression and anxiety: longitudinal associations with mortality risk. Diabetes Care 2017;40:352–8. 10.2337/dc16-2018 [DOI] [PubMed] [Google Scholar]
- 13.van der Feltz-Cornelis CM, Nuyen J, Stoop C, et al. Effect of interventions for major depressive disorder and significant depressive symptoms in patients with diabetes mellitus: a systematic review and meta-analysis. Gen Hosp Psychiatry 2010;32:380–95. 10.1016/j.genhosppsych.2010.03.011 [DOI] [PubMed] [Google Scholar]
- 14.Komsuoglu Celikyurt I, Mutlu O, Ulak G, et al. Exenatide treatment exerts anxiolytic- and antidepressant-like effects and reverses neuropathy in a mouse model of type-2 diabetes. Med Sci Monit Basic Res 2014;20:112–7. 10.12659/MSMBR.891168 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Leubner D, Hinterberger T. Reviewing the effectiveness of music interventions in treating depression. Front Psychol 2017;8:1109. 10.3389/fpsyg.2017.01109 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.American Music Therapy Association What is music therapy? 2013. Available: https://www.musictherapy.org/about/musictherapy/ [Accessed 9 Jan 2020].
- 17.Dileo C. A classification model for music and medicine. Washington, DC: National Association of Music Therapy; 1999: 1–6. [Google Scholar]
- 18.Raglio A, Bellelli G, Mazzola P, et al. Music, music therapy and dementia: a review of literature and the recommendations of the Italian psychogeriatric association. Maturitas 2012;72:305–10. 10.1016/j.maturitas.2012.05.016 [DOI] [PubMed] [Google Scholar]
- 19.Dileo C. Effects of music and music therapy on medical patients: a meta-analysis of the research and implications for the future. J Soc Integr Oncol 2006;4:67–70. 10.2310/7200.2006.002 [DOI] [PubMed] [Google Scholar]
- 20.Thaut MH, Gardiner JC, Holmberg D, et al. Neurologic music therapy improves executive function and emotional adjustment in traumatic brain injury rehabilitation. Ann N Y Acad Sci 2009;1169:406–16. 10.1111/j.1749-6632.2009.04585.x [DOI] [PubMed] [Google Scholar]
- 21.Kim DS, Park YG, Choi JH, et al. Effects of music therapy on mood in stroke patients. Yonsei Med J 2011;52:977–81. 10.3349/ymj.2011.52.6.977 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Nwebube C, Glover V, Stewart L. Prenatal listening to songs composed for pregnancy and symptoms of anxiety and depression: a pilot study. BMC Complement Altern Med 2017;17:256. 10.1186/s12906-017-1759-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Lin XX, JM J, Zhou GY. Influence of listening to Jiao tune music on sleep quality and blood glucose in elderly patients with type 2 diabetes accompanied by insomnia. Journal of Fujian University of Traditional Chinese Medicine 2017;27:44–8. [Google Scholar]
- 24.Mandel SE, Davis BA, Secic M. Effects of music therapy and music-assisted relaxation and imagery on health-related outcomes in diabetes education: a feasibility study. Diabetes Educ 2013;39:568–81. 10.1177/0145721713492216 [DOI] [PubMed] [Google Scholar]
- 25.Centers for Disease Control and Prevention National diabetes statistics report, 2020. Available: https://www.cdc.gov/diabetes/data/statistics/statistics-report.html [Accessed 3 Jul 2020].
- 26.Gabrielsson A, Wik SL. Strong experiences related to music: Adescriptive system. Musicae Scientiae 2003;7:157–217. 10.1177/102986490300700201 [DOI] [Google Scholar]
- 27.Zentner M, Grandjean D, Scherer KR. Emotions evoked by the sound of music: characterization, classification, and measurement. Emotion 2008;8:494–521. 10.1037/1528-3542.8.4.494 [DOI] [PubMed] [Google Scholar]
- 28.Saarikallio S. Music as emotional self-regulation throughout adulthood. Psychol Music 2011;39:307–27. 10.1177/0305735610374894 [DOI] [Google Scholar]
- 29.Gök Ugur H, Yaman Aktaş Y, Orak OS, et al. The effect of music therapy on depression and physiological parameters in elderly people living in a Turkish nursing home: a randomized-controlled trial. Aging Ment Health 2017;21:1280–6. 10.1080/13607863.2016.1222348 [DOI] [PubMed] [Google Scholar]
- 30.Gómez Gallego M, Gómez García J. Music therapy and Alzheimer's disease: cognitive, psychological, and behavioural effects. Neurologia 2017;32:300–8. 10.1016/j.nrl.2015.12.003 [DOI] [PubMed] [Google Scholar]
- 31.Cheung DSK, Lai CKY, Wong FKY, et al. The effects of the music-with-movement intervention on the cognitive functions of people with moderate dementia: a randomized controlled trial. Aging Ment Health 2018;22:306–15. 10.1080/13607863.2016.1251571 [DOI] [PubMed] [Google Scholar]
- 32.Wang S-C, Yu C-L, Chang S-H. Effect of music care on depression and behavioral problems in elderly people with dementia in Taiwan: a quasi-experimental, longitudinal study. Aging Ment Health 2017;21:156–62. 10.1080/13607863.2015.1093602 [DOI] [PubMed] [Google Scholar]
- 33.Bieleninik L, Geretsegger M, Mössler K, et al. Effects of improvisational music therapy vs enhanced standard care on symptom severity among children with autism spectrum disorder: the TIME-A randomized clinical trial. JAMA 2017;318:525–35. 10.1001/jama.2017.9478 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Giovagnoli AR, Manfredi V, Parente A, et al. Cognitive training in Alzheimer's disease: a controlled randomized study. Neurol Sci 2017;38:1485–93. 10.1007/s10072-017-3003-9 [DOI] [PubMed] [Google Scholar]
- 35.Deng HX, Gao GS, ZM L, et al. Study of the effect of music therapy in the treatment of elderly patients with diabetes. China Health Care and Nutrition 2013;23:1186. [Google Scholar]
- 36.Zhang ZW. Study of the effect of music therapy and psychotherapy adjuvant therapy in the treatment of type 2 diabetes. China Medicine and Pharmacy 2011:150–1. [Google Scholar]
- 37.Solanki MS, Zafar M, Rastogi R. Music as a therapy: role in psychiatry. Asian J Psychiatr 2013;6:193–9. 10.1016/j.ajp.2012.12.001 [DOI] [PubMed] [Google Scholar]
- 38.Petrovsky D, Cacchione PZ, George M. Review of the effect of music interventions on symptoms of anxiety and depression in older adults with mild dementia. Int Psychogeriatr 2015;27:1661–70. 10.1017/S1041610215000393 [DOI] [PubMed] [Google Scholar]
- 39.Aalbers S, Fusar-Poli L, Freeman RE, et al. Music therapy for depression. Cochrane Database Syst Rev 2017;11:CD004517. 10.1002/14651858.CD004517.pub3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Shamseer L, Moher D, Clarke M, et al. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015: elaboration and explanation. BMJ 2015;350:g7647. 10.1136/bmj.g7647 [DOI] [PubMed] [Google Scholar]
- 41.Liberati A, Altman DG, Tetzlaff J, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: explanation and elaboration. BMJ 2009;339:b2700. 10.1136/bmj.b2700 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.American Diabetes Association 9. Pharmacologic Approaches to Glycemic Treatment: Standards of Medical Care in Diabetes-2020. Diabetes Care 2020;43:S98–110. 10.2337/dc20-S009 [DOI] [PubMed] [Google Scholar]
- 43.American Diabetes Association 5. Facilitating Behavior Change and Well-being to Improve Health Outcomes: Standards of Medical Care in Diabetes-2020. Diabetes Care 2020;43:S48–65. 10.2337/dc20-S005 [DOI] [PubMed] [Google Scholar]
- 44.Feng Y, Fang Y, Wang Y, et al. Acupoint therapy on diabetes mellitus and its common chronic complications: a review of its mechanisms. Biomed Res Int 2018;2018:1–9. 10.1155/2018/3128378 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Pérez-Pevida B, Escalada J, Miras AD, et al. Mechanisms underlying type 2 diabetes remission after metabolic surgery. Front Endocrinol 2019;10:641. 10.3389/fendo.2019.00641 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Higgins JPT, Thomas J, Chandler J, et al. Cochrane Handbook for systematic reviews of interventions version 6.0, 2019. Available: https://training.cochrane.org/handbook [Accessed 3 Jul 2020].
- 47.Balshem H, Helfand M, Schünemann HJ, et al. GRADE guidelines: 3. rating the quality of evidence. J Clin Epidemiol 2011;64:401–6. 10.1016/j.jclinepi.2010.07.015 [DOI] [PubMed] [Google Scholar]
- 48.Gonzalez JS, Peyrot M, McCarl LA, et al. Depression and diabetes treatment nonadherence: a meta-analysis. Diabetes Care 2008;31:2398–403. 10.2337/dc08-1341 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Trief PM, Foster NC, Chaytor N, et al. Longitudinal changes in depression symptoms and glycemia in adults with type 1 diabetes. Diabetes Care 2019;42:1194–201. 10.2337/dc18-2441 [DOI] [PubMed] [Google Scholar]
- 50.Novak M, Mucsi I, Rhee CM, et al. Increased risk of incident chronic kidney disease, cardiovascular disease, and mortality in patients with diabetes with comorbid depression. Diabetes Care 2016;39:1940–7. 10.2337/dc16-0048 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Lustman PJ, Anderson RJ, Freedland KE, et al. Depression and poor glycemic control: a meta-analytic review of the literature. Diabetes Care 2000;23:934–42. 10.2337/diacare.23.7.934 [DOI] [PubMed] [Google Scholar]
- 52.Roopan S, Larsen ER. Use of antidepressants in patients with depression and comorbid diabetes mellitus: a systematic review. Acta Neuropsychiatr 2017;29:127–39. 10.1017/neu.2016.54 [DOI] [PubMed] [Google Scholar]
- 53.Croom AM. Music, neuroscience, and the psychology of well-being: a précis. Front Psychol 2012;2:393. 10.3389/fpsyg.2011.00393 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Abd-Elshafy SK, Khalaf GS, Abo-Kerisha MZ, et al. Not all sounds have negative effects on children undergoing cardiac surgery. J Cardiothorac Vasc Anesth 2015;29:1277–84. 10.1053/j.jvca.2015.01.005 [DOI] [PubMed] [Google Scholar]
- 55.SJ Y, Sun ZY, Zhou J, et al. Study of the effect of music therapy and psychological intervention in the treatment of diabetic patients. Hebei med 2007;13:903–6. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.