Abstract
Objective
Polypharmacy occurs in approximately 30% of older adults aged 65 years or more, particularly among those with multimorbidity. With polypharmacy, there is an associated risk of potentially inappropriate prescribing (PIP). The aims of this scoping review were to (1) identify the intervention elements that have been adopted to reduce PIP in the outpatient setting and (2) determine the behaviour change wheel (BCW) intervention functions performed by each of the identified intervention elements.
Design
Scoping review
Data sources
PubMed, Cumulative Index to Nursing and Allied Health Literature, EMBASE, Web of Science and Cochrane Library databases, grey literature sources, six key geriatrics journals and the reference lists of review papers.
Study selection
All studies reporting an intervention or strategy that addressed PIP in the older adult population (age ≥65) with multimorbidity in the outpatient setting and in which the primary prescriber is the physician.
Data extraction
Data extracted from the included studies can be broadly categorised into (1) publication details, (2) intervention details and (3) results. This was followed by data synthesis and analysis based on the BCW framework.
Results
Of 8195 studies yielded, 80 studies were included in the final analysis and 14 intervention elements were identified. An average of two to three elements were adopted in each intervention. The three most frequently adopted intervention elements were medication review (70%), training (26.3%) and tool/instrument(s) (22.5%). Among medication reviews, 70% involved pharmacists. The 14 intervention elements were mapped onto five intervention functions: ‘education’, ‘persuasion’, ‘training’, ‘environmental restructuring’ and ‘enablement’.
Conclusion
PIP is a multifaceted problem that involves multiple stakeholders. As such, interventions that address PIP require multiple elements to target the behaviour of the various stakeholders. The intervention elements and their corresponding functions identified in this scoping review will serve to inform the design of complex interventions that aim to reduce PIP.
Keywords: geriatric medicine, primary care, quality in health care
Strengths and limitations of this study.
This is the first attempt to map the extent and nature of information on elements of care interventions that address potentially inappropriate prescribing among older adults in the outpatient setting in both peer-reviewed and grey literature.
The results from this review can be used to guide the design of complex interventions to reduce potentially inappropriate prescribing among older adults.
Consultation with experts and stakeholders was initiated at the time of writing and will be reported in a separate work.
The effectiveness or outcomes of interventions were not examined in the present study.
This review may not be fully comprehensive due to the time period and language restrictions imposed during the literature search and study selection.
Introduction
Polypharmacy, commonly defined as the use of five or more medications daily, is a widespread phenomenon among older adults as they tend to develop multiple chronic diseases or multimorbidity with age.1 Polypharmacy among community-dwelling older people is a global problem, with its prevalence ranging from 11.5% among rural residents of China to 43.3% in Australia, according to a 2019 WHO report.2 Furthermore, the prevalence of polypharmacy has been increasing worldwide.3 A longitudinal, cohort study of over 2000 community-dwelling older adults aged 62–85 years in the USA showed that the prevalence of polypharmacy increased from 30.6% to 35.8% between 2005 and 2011.4 Similar trends have also been observed in other countries, including the UK, Netherlands, Belgium, Japan, South Korea and New Zealand.5–10 Polypharmacy is a cause for concern as it predisposes older adults to potentially inappropriate prescribing (PIP), which occurs when medicines prescribed confer more harm than benefit.11 Current clinical guidelines are designed to be disease-specific, but many in so doing fail to take into consideration drug-disease and drug–drug interactions in their treatment recommendations.12 13 In older adults, adverse drug events (ADE) are made even more unpredictable by age-related changes in pharmacokinetics and pharmacodynamics.14 15 This problem is further exacerbated by the fact that clinical trials often exclude older adults, which means approved drug doses may not be appropriate for geriatric patients.16
It is estimated that up to 50% of older adults receive at least one unnecessary medication, and the incidence of PIP increases significantly with polypharmacy.17 18 Older adults with at least two PIP indicators based on the Screening Tool of Older Person’s Potentially Inappropriate Prescriptions (STOPP) criteria were shown to be two times as likely to experience ADE.19 Apart from drug-related problems, older adults with PIP also reported poorer functional status, reduced health-related quality of life and increased healthcare utilisation, including more frequent emergency department visits and hospitalisations.20–22 Given the high prevalence of PIP and its adverse outcomes, it is therefore imperative for appropriate measures to be implemented to improve prescribing for older adults. With rising concern on suboptimal prescribing both internationally and at home, a three-phase implementation research project aiming to reduce PIP among older adults is underway. The first phase includes a literature review to examine interventions to reduce PIP among older adults with multimorbidity receiving outpatient care. While there have been several systematic reviews performed to explore interventions that address PIP, these reviews included a limited number of studies as they focused only on specific study types (eg, randomised controlled trials23) or specific intervention types (eg, computerised decision support systems24 and pharmacist-led medication reviews25). Moreover, systematic reviews often restrict inclusion to studies that fulfil a certain standard of methodological rigour and reporting, which might result in the omission of a significant number of potentially relevant studies.26
In addition, reviews of complex interventions can be challenging as there is currently no formal methodology for the synthesis of data from these studies.27 There is also great variability among complex interventions in terms of their components and modes of delivery, which makes it even harder to perform comparative analyses.27 To overcome this problem, a theoretical framework could be applied to organise and make sense of the data extracted. In this scoping review, the behaviour change wheel (BCW) framework28 was used. The BCW was developed by Michie et al28 as a framework to systematically guide the development of interventions using theory. In the BCW framework, evidence-based principles of behaviour change are represented in the core model of behaviour: capability, opportunity, motivation and behaviour (COM-B).29 COM-B identifies sources of behaviour that could bring about a change, which are mapped onto nine intervention functions: education, persuasion, incentivisation, coercion, training, restriction, environmental restructuring, modelling and enablement. This approach offers a systematic method of characterising and analysing intervention content. As such, in order to capture the breadth of intervention studies that have been conducted to address PIP, we adopted a scoping review methodology to identify all relevant information irrespective of study type and quality of their sources.
The aims of our scoping review were thus to: (1) identify intervention elements and within-element variations that have been adopted to reduce inappropriate prescribing among older adults in the outpatient setting and (2) map the intervention elements onto the BCW intervention functions for synthesis. The findings will contribute to the knowledge base to inform the development of a collaborative care intervention to reduce PIP, which will be tested in subsequent study phases. To our knowledge, there have been no scoping reviews published that map information on the extent and nature of care interventions to reduce PIP from both peer-reviewed and grey literature.
Methods
The methodological framework developed by Arksey and O’Malley30 was adopted, with the application of recommendations proposed by Levac et al31 and the Joanna Briggs Institute (JBI).32 Five of the six stages outlined in the framework were performed: (1) identifying the research question; (2) identifying relevant studies; (3) selecting studies; (4) charting data and (5) summarising and reporting the results.
Identifying the research question
This scoping review was guided by the research question: ‘What intervention elements have been adopted to reduce inappropriate prescribing among older adults with multimorbidity in outpatient care?’ The research question was formulated after several rounds of discussion within the study team (one physician (YYD), two pharmacists (KTT and WA) and three researchers (KY, JQL, PL). Following the recommendation by JBI,32 the research question incorporated the elements ‘Population, Concept and Context’.
Identifying the relevant studies
We started with five articles that are relevant to our research question and identified the keywords and Medical Subject Headings (MeSH) terms that were used to describe these articles. These search terms were then categorised into ‘Population’, ‘Concept’ and ‘Context’ and additional keywords and MeSH terms were identified through searching their synonyms and the MeSH browser, respectively. The final list of search terms can be found in online supplementary file 1.
bmjopen-2020-039543supp001.pdf (98.7KB, pdf)
We conducted a pilot search in Ovid MEDLINE. Using the five articles as a test of sensitivity and specificity, the search strategy was refined after several iterative searches. The eventual search strategy was then adapted for the remaining databases using the appropriate syntax. The following six electronic databases were searched on 28 January 2019: PubMed, Cumulative Index to Nursing and Allied Health Literature (CINAHL), Web of Science, Embase (Ovid), The Cochrane Library and Scopus. Our searches were limited to English Language only with a publication date from January 1998 to the date performed (January 2019). The full electronic search strategy for PubMed is provided in online supplementary file 2.
bmjopen-2020-039543supp002.pdf (53.7KB, pdf)
We also performed a search for grey literature in February 2019 in 13 resources, including ClinicalTrials.gov, OpenGrey, Science.gov and WorldCat. In addition, six key geriatrics and gerontology journals were searched electronically: Journal of the American Geriatrics Society, Age and Ageing, The Journals of Gerontology Series A, Archives of Gerontology and Geriatrics, BMC Geriatrics and European Geriatric Medicine. Various combinations of the following keywords were used: ‘intervention’ and ‘inappropriate prescribing’, combined with ‘multimorbidity’, ‘comorbidity’ and ‘polypharmacy’. Where possible, language and publication date limits were imposed (as above).
Screening and study selection procedures
The eligibility criteria were developed based on the research question and further refined along the way as the reviewers became more familiar with the evidence base. Our inclusion criteria were: (1) original publications that describe an intervention or strategy that addresses PIP in a population that includes older adults (age ≥65 years); (2) intervention was carried out in the outpatient setting; (3) physicians were the prescribers and (4) prescribing was not restricted to specific diseases or conditions, for example, hypertension, chronic obstructive pulmonary disease or specific medications, for example, opioids.
The screening was conducted in the web-based systematic review software Covidence and consisted of two stages. The first stage involved title and abstract screening, which was performed independently by two reviewers (KY and JQL). Reviewers met at the beginning, middle and end stages of the abstract review process to clarify doubts and establish a common understanding of the inclusion criteria, as recommended by Levac et al.31 In the second stage, the same reviewers similarly reviewed the full-text articles independently, before meeting to discuss and resolve conflicts. A third reviewer (YYD) was involved in resolving conflicts where necessary. During the screening process, systematic reviews that were relevant to the research question were also identified, and their reference lists were searched to garner additional primary studies for inclusion. The systematic review papers were not included in data extraction and synthesis.
Charting the data
A data charting form was developed and used to extract data from the included studies. The extracted information included: (1) publication details: author(s), year of publication, country of origin; (2) intervention details: study type, participants, description of intervention and (3) results: outcome measures. Charting of the first three studies was performed together by the two reviewers (KY and JQL) to establish a standardised method of extraction. Each reviewer then charted half of the remaining studies.
Collating, summarising and reporting of results
The first step of data synthesis involved identifying the intervention elements present in each study. During full-text screening of the 80 articles, a provisional list of common intervention elements implemented in the reported studies was identified by the reviewers (eg, medication reviews, education and training, case conference, medication reconciliation, etc) and the list was expanded and refined along the way. Coding of the intervention elements was performed independently by the two reviewers (KY and JQL), before meeting to compare, discuss and reach a consensus on the coding.
Application of behaviour change framework
The intervention elements were then mapped onto the BCW intervention functions: education, persuasion, incentivisation, coercion, training, restriction, environmental restructuring, modelling and enablement. The definitions and examples of the BCW intervention functions are outlined in online supplementary file 3. Two reviewers (KY and JQL) performed the mapping independently before discussing and finalising the synthesis.
bmjopen-2020-039543supp003.pdf (72.2KB, pdf)
Patient and public involvement
Patients and/or members of the public were not involved in this scoping review.
Results
Study selection and characteristics of included studies
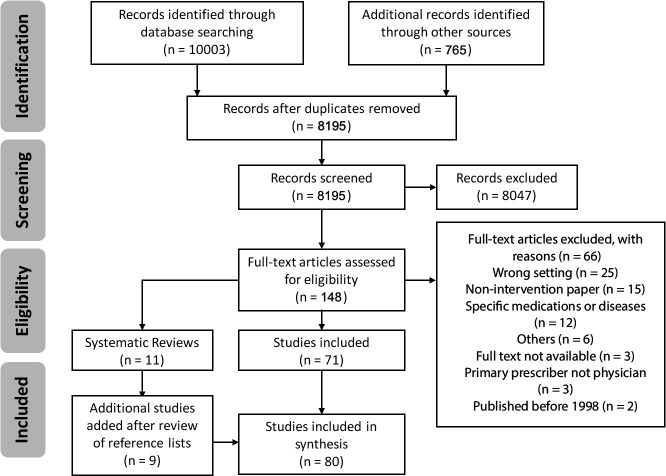
The review selection process is summarised in figure 1 using a Preferred Reporting Items for Systematic Reviews and Meta-Analyses flow diagram. The initial search yielded 8195 abstracts after removal of duplicates. After title and abstract screening and full-text review, 71 studies were included. Eleven systematic review papers relevant to our research question were identified, and their reference lists were searched, adding another nine studies. A total of 80 studies were included for data extraction and synthesis (references to the included studies are provided in online supplementary file 4). They comprised 40 interventional studies, 13 observational studies, 13 study protocols, 13 conference abstracts and 1 report. The characteristics of the included studies are summarised in table 1. The studies originated from 19 countries, with the majority from the USA (n=25, 32%). More than 60% of the included studies were published in the last 5 years, that is, 2014 to present.
Figure 1.
Preferred Reporting Items for Systematic Reviews and Meta-Analyses flow diagram of study selection process.
Table 1.
Characteristics of included studies
| Characteristics | Frequency count (%) |
| Study type | |
| Interventional studies | 40 (50.0) |
| Randomised controlled trial | 17 (21.3) |
| Pre–post study | 9 (11.3) |
| Cluster randomised controlled trial | 7 (8.8) |
| Non-randomised trial | 6 (7.5) |
| Randomised trial | 1 (1.3) |
| Observational studies | 13 (16.3) |
| Prospective cohort study | 10 (12.5) |
| Retrospective cohort study | 2 (2.5) |
| Cross-sectional study | 1 (1.3) |
| Others | 27 (33.8) |
| Study protocol | 13 (16.3) |
| Conference abstract | 13 (16.3) |
| Report | 1 (1.3) |
| Publication year | |
| 1998 – 2003 | 8 (10.0) |
| 2004 – 2008 | 8 (10.0) |
| 2009 – 2013 | 15 (18.8) |
| 2014 – 2019 | 49 (61.3) |
| Country of origin | |
| USA and Canada | 31 (38.8) |
| UK and Ireland | 5 (6.3) |
| Scandinavia | 9 (11.3) |
| Western Europe | 25 (31.3) |
| Asia | 6 (7.5) |
| Australia | 3 (3.8) |
| Others | 1 (1.3) |
bmjopen-2020-039543supp004.pdf (131KB, pdf)
Intervention elements identified
Fourteen intervention elements were identified from the included studies. Within each intervention element, variations were noted and coded separately to capture the differences in which the elements were performed (eg, medication review performed by pharmacist or physician or both physician and pharmacist). The definitions of the 14 intervention elements are outlined in tables 2–4. Medication review was found to be the most frequently adopted intervention element (n=56; 70%), followed by training (n=21; 26.3%), tool/instrument(s) (n=18; 22.5%), feedback and audit (n=15; 18.8%) and medication therapy management (n=14; 17.5%). Of all medication reviews, 69.6% involved pharmacists (n=39; MR1, 2, 3 and 4), 26.8% were performed by physicians alone (n=15; MR5) and 3.6% were performed by physicians and medical assistants (n=2; MR6). Case conference and peer support were the least frequently adopted intervention elements (n=3 and n=2, respectively). Interventions have an average of 2.5 elements, with more than 80% (n=65) consisting of more than 1 element. The highest number of elements present in a single intervention is 8.33
Table 2.
Descriptions and examples of medication review, training, tool/instrument(s) and feedback and audit
| Intervention element | Definition | Subtypes | Code | Example | BCW intervention function(s) |
| Medication review | ‘Structured evaluation of patient‘s medicines with the aim of optimising medicines use and improving health outcomes’.42 | Pharmacist-led with feedback to physician | MR1 | Clinical pharmacists performed drug therapy reviews for patients identified with a high risk of polypharmacy and suggested drug therapy changes to the physicians by telephone, fax or in person. Physicians reviewed and endorsed recommendations.43 |
|
| Performed by pharmacist and physician | MR2 | Clinical pharmacist reviewed patient charts to determine patients at greatest risk for MRPs and worked side by side with physicians to consult patient and resolve MRPs.44 |
|
||
| Performed by an external team of pharmacist(s) and/or physician(s) | MR3 | A panel of five experts (physicians and pharmacists) not affiliated with the MCO or the academic medical centre performed a peer review of the drugs to be included in the intervention and their corresponding alternative medications.45 |
|
||
| Performed by pharmacist (but not the one conveying feedback) | MR4 | A clinical pharmacologist performed a thorough medication review of the selected patients, which was sent to the medication consultant. The medication consultant offered a visit to the general practitioner to discuss potential changes to the individual patient’s medication.46. |
|
||
| Performed by physician | MR5 | A letter was sent to selected patients to encourage them to make an appointment with their primary care physician for a medication review. Physicians were provided with patient-specific medication management report and clinical practice guidelines for managing polypharmacy.47 |
|
||
| Performed by physician and medical assistant | MR6 | MA performed brown bag review and GPs reviewed the medication systematically using tools (PRISCUS list or MAI) to reduce potentially inappropriate medications.48 |
|
||
| Training | Imparting skills required to carry out intervention to improve prescribing.28 | For pharmacists | TG1 | Pharmacists attended tutorial by the study pharmacist to ensure standardised method of medication review.49 |
|
| For physicians | TG2 | 20 GPs were trained to use STOPP criteria.50 |
|
||
| For medical assistants | TG3 | MAs were trained to perform brown bag reviews.48 |
|
||
| Tool/instrument (s) | Checklist/guideline(s) used to identify medication-related problems or measure medication appropriateness. | – | TI1 | Pharmacist identified potential MRPs using START/STOPP criteria to be addressed with the provider.51 |
|
| Feedback and audit | Monitoring and evaluation of physician’s prescribing patterns. | Feedback only | FA1 | Retrospective DUR identified patients at risk of drug injury. Main prescribing GP of the identified patient received a personalised feedback letter containing patient-specific information and clinical practice guidelines.52 |
|
| Feedback with the discussion of improvement strategies | FA2 | A quality improvement tool was used to track PIP and individualised feedback were mailed to PCPs monthly. A geriatrician and geriatric clinical pharmacist met face-to-face with each PCP to review his/her first feedback form and discuss improvement strategies.53 |
|
BCW, behaviour change wheel; DUR, drug utilisation review; GP, general practitioner; MA, medical assistant; MAI, medication appropriateness index; MCO, managed care organisation; MRP, medication-related problem; PCP, primary care provider; PIP, potentially inappropriate prescribing; START, screening tool to alert to right treatment; STOPP, screening tool of older person’s potentially inappropriate prescriptions.
Table 3.
Descriptions and examples of medication therapy management, shared decision-making, clinical decision support, education and patient interview
| Intervention element | Definition | Subtypes | Code | Example | BCW intervention function(s) |
| Medication therapy management | ‘Providing verbal education and training designed to enhance patient understanding and appropriate use of his/her medications’.54 | – | MTM1 | Patients will be provided with comprehensive counselling and specific adherence strategies (information about medications and administration) by the pharmacist.55 |
|
| Shared decision-making | Narrative-based dialogue between doctor and patient to discuss treatment targets and priorities of the patient.56 | – | SDM1 | GPs met with patients three times within 12 months. The first session was aimed at identifying patients’ priorities in life (including non-medical goals) and carving out treatment targets based on this information. The second session involved a ‘brown bag review’. On the third session, GPs discussed with patients about goal attainment, changes in medication and treatment targets for the future.56 |
|
| Clinical decision support | ‘Technological applications that provide clinicians, staff, patients or other individuals with knowledge and person-specific information, intelligently filtered or presented at appropriate times, to enhance health and healthcare’.57 | – | CDS1 | GP recorded medication and diagnoses in STRIPA and performed a structured drug review using the software. STRIPA is a Dutch software-based tool that 1) highlights predictable adverse medication effects, 2) advises safe and appropriate therapy using STOPP/START criteria, 3) monitors for interactions and 4) provides appropriate dosing in accordance with renal function.58 |
|
| Education | Increasing knowledge or understanding about PIP.28 | For physicians | ED1 | Physicians in the intervention group received: (1) a detailed educational brochure listing potentially inappropriate medications, (2) a list of suggested alternative medications (independently suggested and reviewed by five geriatricians and pharmacists not affiliated with the MCOs).45 |
|
| For physicians and nurses | ED2 | PCPs and nurses underwent tutorial on PIP.59 |
|
||
| Patient interview | ‘Asking patient about how, when and why the patient takes each medication, as well as about any adverse reactions, allergies or issues with medication cost the patient may have experienced’.60 | Performed by physician | PI1 | During the consultation, patients were interviewed on drugs currently being taken, dosage and frequency and the condition for which the medication had been prescribed.61 |
|
| Performed by healthcare professional other than physician | PI2 | Patients received a 30–60 minute face-to-face consultation with the pharmacist at the clinic. Prior to the consultation, pharmacist reviewed patient's medical records. During the consultation, pharmacists interviewed patients for medication history, adherence and knowledge.62 |
|
BCW, behaviour change wheel; GP, general practitioner; MCO, managed care organisation; PCP, primary care provider; PIP, potentially inappropriate prescribing; START, screening tool to alert to right treatment; STOPP, screening tool of older person’s potentially inappropriate prescriptions; STRIPA, systematic tool to reduce inappropriate prescribing-assistant.
Table 4.
Descriptions and examples of medication reconciliation, multidisciplinary team, comprehensive geriatric assessment, case conference and peer support
| Intervention element | Definition | Code | Example | BCW intervention function(s) |
| Medication reconciliation | ‘The process of creating the most accurate list possible of all medications a patient is taking, including drug name, dosage, frequency, and route’.63 | MRC1 | HCA reconciled all medications, which the patient was instructed to bring in their original packaging.64 |
|
| Multidisciplinary team | Involvement of healthcare professionals from more than two disciplines to address PIP in a patient. | MT1 | Patient attended a shared medical appointment co-facilitated by a pharmacist, health psychologist, nurse practitioner, and physician, which consisted of interactive discussions about polypharmacy, adherence, and patients’ beliefs about medications.65 |
|
| Comprehensive geriatric assessment | ‘A multidimensional, multidisciplinary process, which identifies medical, social and functional needs’.66 | CGA1 | Complete geriatric assessment was carried out by geriatrician at geriatric day clinic.67 |
|
| Case conference | Meeting of a multidisciplinary team of healthcare professionals to discuss an individual patient’s case or multiple patients’ cases.68 | CC1 | Two physicians, a pharmacist and a nurse reviewed the list of drugs and the diagnoses of a subgroup of the experimental group in a case conference.68 |
|
| Peer support | Discussions between physicians for decision-making.69 | PS1 | GPs engaged in a group discussion about their prescribing behaviours facilitated by a peer academic detailer.70 |
|
BCW, behaviour change wheel; GP, general practitioner; HCA, health care assistant.
Mapping of intervention elements to BCW intervention functions
The 14 intervention elements were mapped onto five of the nine BCW intervention functions, namely education, persuasion, training, environmental restructuring and enablement. Tables 2–4 summarise the 14 intervention elements and their corresponding intervention functions. No intervention elements were mapped onto the remaining four intervention functions (incentivisation, coercion, restriction, modelling).28 Environmental restructuring and enablement were the two functions that were most commonly identified among the intervention elements and their subtypes (n=11 and n=16 out of 24).
Medication review
Pharmacist-led medication reviews (MR1), medication reviews conducted by an external team of pharmacist(s) and/or physician(s) (MR3) and medication reviews conducted by pharmacist(s) without communicating recommendations to the physician directly (MR4) were mapped onto the same three functions. The first function persuasion was performed as the pharmacist communicated their recommendations to the physician, prompting them to reconsider their prescription for the respective patients. Environmental restructuring was also served, when the presence of a pharmacist changed the social context of the physician.28 The third function was enablement, as the physicians’ means to prescribe appropriately could increase with the pharmacist’s review of the medications for drug-related problems. The function persuasion was not identified in medication reviews that were performed together by a pharmacist and a physician (MR2), as the pharmacist and physician worked together to reach a decision to resolve medication-related problems for the patient. Medication review that was performed solely by a physician (MR5) served the function of enablement, as the medication review provided an opportunity for the physician to review and rethink the prescription, after having an overview of the patient’s medications and health records. Medication review that was performed by a physician and a medical assistant (MR6) served two functions. First, involving a medical assistant in the medication review process (eg, brown bag review or medication reconciliation) changed the social context of the physician, which indicates environment restructuring.28 Second, by providing a complete medication review or reconciliation list of medication to the physicians, medical assistants enabled them to review and make changes to patient’s medication when necessary.
Training
All three types of training (targeted at pharmacists (TG1), physicians (TG2) and medical assistants (TG3)) were mapped onto the function training, as they served to equip healthcare professionals with practical skills to support the reduction of PIP.
Tool/instrument(s)
Tool and instrument(s) were mapped onto the function of enablement, as they served as guidelines to increase the means and capability of prescribers to prescribe more appropriately. Among the 18 studies that involved tool/instrument(s), the most commonly employed tools/instruments were the STOPP criteria (n=7; 38.9%), followed by Screening Tool to Alert to Right Treatment (START) (n=5; 27.8%) and Beers criteria (n=4; 22.2%).
Feedback and audit
Both types of feedback and audit (feedback only (FA1) and feedback with a discussion of improvement strategies (FA2)) served the function of persuasion, since they prompted physicians to prescribe more appropriately through monitoring and feedback of their prescribing behaviour. FA2 also served the function of environmental restructuring, as having someone to discuss strategies to improve prescribing changed the social context of the physician.28
Medication therapy management and education
Both medication therapy management and education were mapped onto the function of education, since they served to increase patients’ knowledge and understanding about their medication regimen and educate healthcare professionals about PIP, respectively.
Shared decision-making, patient interview, medication reconciliation and comprehensive geriatric assessment
The intervention elements shared decision-making, patient interview, medication reconciliation and comprehensive geriatric assessment performed the function of enablement, as they increased the means or capability of physicians to prescribe more appropriately by providing in-depth and holistic information about the patient.
Clinical decision support
As an intervention element, clinical decision support served the function of environmental restructuring by providing infrastructural support (changing physical context) and the function of enablement by increasing physicians’ means to prescribe appropriately.
Multidisciplinary team, case conference and peer support
The intervention elements multidisciplinary team, case conference and peer support all performed the functions of environmental restructuring and enablement. Environmental restructuring through involvement of other physicians and healthcare professionals changed the social context of the physician, whereas enablement by support from coworkers increased the physician’s means to prescribe more appropriately.
Discussion
Our results indicate that more than 80% of the interventions identified were complex, with multimodal approaches that comprise an average of 2.5 elements. This corroborates with past systematic reviews that also identified most interventions as being complex.34 35 Furthermore, the intervention elements were targeted at various stakeholders. For instance, medication therapy management aimed to educate patients, training served to equip healthcare providers with skills to improve prescribing, while clinical decision support provided infrastructural support. Taken together, these highlight the fact that PIP is a multifaceted problem and multipronged approaches have been adopted to change the behaviour of stakeholders at the patient, healthcare provider and organisation levels. Medication review is the most frequently adopted intervention element, much more so than tool/instrument and clinical decision support. This could be attributed to the fact that PIP is a highly dynamic problem that varies according to the individual clinical context. The determination of medication appropriateness, therefore, requires not only theoretical knowledge, but also clinical judgement and experience. As such, the involvement of a pharmacist and physician in the medication review process is crucial for sound decisions to be made to achieve optimal outcomes for patients.
On the other hand, medication reviews are often time-consuming, making them a challenge to implement in busy clinical practice.36 37 While physicians generally appreciated support from pharmacists, some studies have also noted that the collaboration between pharmacists and physicians required trust and rapport, which would take time to develop.38 39 Therefore, although medication review was widely adopted as a strategy to reduce PIP, a systems-oriented approach to its implementation is needed for it to function as intended. Case conference and peer support were found to be the least frequently adopted intervention elements. It is likely that physicians were already seeking advice from their peers when they encounter more complex cases, although on an informal and ad hoc basis. Notably, the 13 studies that adopted the element shared decision-making were all published in the last 5 years, that is, 2014 to January 2019. This could be attributed to the shift in recent years towards patient-centred care, where emphasis is placed on prioritising individual patient’s needs and expectations.40 This is particularly relevant in the context of PIP, where stopping medications can be challenging for patients, and they tend to heed the advice of healthcare professionals only if they trust the latter.41 In order to establish trust, it is essential for healthcare professionals to consider their concerns, thoughts and expectations.
Environmental restructuring and enablement were the two BCW intervention functions most frequently mapped onto the 14 intervention elements. Environmental restructuring constitutes a change in either the physical or social context.28 This suggests that inadequate infrastructure and social support for prescribers were being addressed. Enablement, on the other hand, involves increasing prescribers’ opportunities or capabilities to prescribe appropriately by addressing the barriers that limit their ability to prescribe optimally, such as incomplete information about patients.
Our findings will be useful in informing the development of a care intervention that will undergo feasibility testing in the second of three phases of the wider project. The anticipated product will be an effective, feasible and scalable physician–pharmacist collaborative care intervention to improve prescribing for older adults receiving outpatient care at public hospitals in Singapore.
Strengths and limitations
We aimed to achieve methodological rigour by adhering closely to the scoping review framework proposed by Arksey and O’Malley30 and applying the recommendations outlined by Levac et al31 and JBI.32 A comprehensive search in both peer-reviewed and grey literature was performed, and the final search strategy was developed after several rounds of iteration. We documented all search iterations attempted and systematic decisions made along the way, in order to keep an accurate record of how the eventual search strategy was finalised. Following recommendations proposed by JBI, a step-by-step protocol was developed prior to undertaking the scoping review and our research question were clearly outlined in the format of ‘Population, Concept, Context’. These steps helped to provide a clear direction and focus throughout the review process. The reviewers also met frequently to clarify doubts, as recommended by Levac et al.
Our initial search yielded a substantial number of titles and abstracts, which could suggest that our search strategy lacked specificity. However, given the lack of standardised terms and definitions (eg, for the concept of ‘polypharmacy’) available on this subject, a broad array of search terms was used to capture as many studies relevant to our research question as possible. Due to feasibility reasons, language restrictions were imposed during literature search and study selection, which could result in the omission of relevant studies and underrepresentation of available literature. A limit was also placed on the year of publication of included studies, but this was to ensure that interventions identified were relevant to current healthcare contexts. Intervention elements and functions were only coded when explicitly stated or observed. Thus, coding was limited by the extent of intervention and methodological details reported. We also did not perform the sixth stage of the Arksey and O’Malley framework, that is, the consultation exercise. This stage will be replaced by a separate Delphi study, where findings from this scoping review will be presented to a panel of clinical experts to elicit their opinions on the relevance of our findings in local prescribing contexts.
As the intention for conducting our scoping review was to mainly focus on identifying all the intervention elements that have been implemented in the outpatient settings, interactions between intervention elements within an intervention package and the effectiveness or outcomes of these interventions were not examined. It would be interesting to explore the intervention elements that are most often grouped together and the effect these elements have on one another and on the eventual outcome in a separate work. This could provide valuable evidence on the effectiveness of separate intervention elements when combined.
Conclusion
This review represents the first scoping review performed to identify elements of care interventions that address PIP among older adults in the outpatient setting. The wide range of intervention elements found was characterised based on the functions they perform using the BCW intervention functions adapted from Michie et al.28 The findings from this review would thus provide valuable information and guidance when designing a theory-based and evidence-based complex intervention to reduce PIP. Furthermore, a theoretical framework is applied in the synthesis and analysis of data, which could be regarded as an adaptation of the scoping review methodology given that there is currently no formalised approach to data synthesis. Further investigation could involve exploring the interactions between different elements within an intervention and how they influence effectiveness in improving prescribing quality for older patients.
Supplementary Material
Footnotes
Correction notice: This article has been corrected for fonts and alignment in Table 2, 3 and 4.
Contributors: KY and JQL conducted the scoping review, performed the data extraction and synthesis, and wrote the first draft of the paper for submission. JQL is the corresponding author and has taken the primary responsibility of communicating with the journal during the manuscript submission, peer review and publication process, and has ensured that all the journal’s administrative requirements, such as providing details of authorship, and gathering conflict of interest forms and statements, are properly completed. YYD, KTT, WA and PL provided specific content clinical expertise to inform the discussion and implications of the study results (from the perspectives of geriatrician, pharmacists and researcher respectively). YM was the study librarian on the study and contributed to the search strategy as well as the draft and review of the methods of the manuscript. All seven authors reviewed the accuracy and integrity of the work.
Funding: Intramural Grant Award (GERI1622) from Geriatric Education and Research Institute, Singapore.
Competing interests: None declared.
Patient and public involvement: Patients and/or the public were not involved in the design, conduct, reporting, or dissemination plans of this research.
Patient consent for publication: Not required.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data availability statement: Data are available upon reasonable request. Readers interested in using our database for specific purposes related to their respective research are invited to do so by contacting the first author through their corresponding email address.
References
- 1.Masnoon N, Shakib S, Kalisch-Ellett L, et al. What is polypharmacy? A systematic review of definitions. BMC Geriatr 2017;17:230. 10.1186/s12877-017-0621-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.World Health Organization Medication safety in polypharmacy. technical report; 2019: 11–14.
- 3.Wastesson JW, Morin L, Tan ECK, et al. An update on the clinical consequences of polypharmacy in older adults: a narrative review. Expert Opin Drug Saf 2018;17:1185–96. 10.1080/14740338.2018.1546841 [DOI] [PubMed] [Google Scholar]
- 4.Qato DM, Wilder J, Schumm LP, et al. Changes in prescription and over-the-counter medication and dietary supplement use among older adults in the United States, 2005 vs 2011. JAMA Intern Med 2016;176:473. 10.1001/jamainternmed.2015.8581 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Oktora MP, Denig P, Bos JHJ, et al. Trends in polypharmacy and dispensed drugs among adults in the Netherlands as compared to the United States. PLoS One 2019;14:e0214240. 10.1371/journal.pone.0214240 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.van den Akker M, Vaes B, Goderis G, et al. Trends in multimorbidity and polypharmacy in the Flemish-Belgian population between 2000 and 2015. PLoS One 2019;14:e0212046. 10.1371/journal.pone.0212046 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Zhang F, Mamtani R, Scott FI, et al. Increasing use of prescription drugs in the United Kingdom. Pharmacoepidemiol Drug Saf 2016;25:628–36. 10.1002/pds.3947 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Onoue H, Koyama T, Zamami Y, et al. Trends in polypharmacy in Japan: a nationwide retrospective study. J Am Geriatr Soc 2018;66:2267–73. 10.1111/jgs.15569 [DOI] [PubMed] [Google Scholar]
- 9.Baek Y-H, Shin J-Y. Trends in polypharmacy over 12 years and changes in its social gradients in South Korea. PLoS One 2018;13:e0204018. 10.1371/journal.pone.0204018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Nishtala PS, Salahudeen MS. Temporal trends in polypharmacy and Hyperpolypharmacy in older new Zealanders over a 9-year period: 2005–2013. Gerontology 2015;61:195–202. 10.1159/000368191 [DOI] [PubMed] [Google Scholar]
- 11.Gallagher P, Barry P, O'Mahony D. Inappropriate prescribing in the elderly. J Clin Pharm Ther 2007;32:113–21. 10.1111/j.1365-2710.2007.00793.x [DOI] [PubMed] [Google Scholar]
- 12.Moßhammer D, Haumann H, Mörike K, et al. Polypharmacy-an upward trend with unpredictable effects. Dtsch Arztebl Int 2016;113:627–33. 10.3238/arztebl.2016.0627 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Dumbreck S, Flynn A, Nairn M, et al. Drug-disease and drug-drug interactions: systematic examination of recommendations in 12 UK national clinical guidelines. BMJ 2015;350:h949. 10.1136/bmj.h949 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Corsonello A, Pedone C, Incalzi RA. Age-Related pharmacokinetic and pharmacodynamic changes and related risk of adverse drug reactions. Curr Med Chem 2010;17:571–84. 10.2174/092986710790416326 [DOI] [PubMed] [Google Scholar]
- 15.Corsonello A, Abbatecola AM, Fusco S, et al. The impact of drug interactions and polypharmacy on antimicrobial therapy in the elderly. Clin Microbiol Infect 2015;21:20–6. 10.1016/j.cmi.2014.09.011 [DOI] [PubMed] [Google Scholar]
- 16.Cho S, Lau SWJ, Tandon V, et al. Geriatric drug evaluation. Arch Intern Med 2011;171:937–40. 10.1001/archinternmed.2011.152 [DOI] [PubMed] [Google Scholar]
- 17.Maher RL, Hanlon J, Hajjar ER. Clinical consequences of polypharmacy in elderly. Expert Opin Drug Saf 2014;13:57–65. 10.1517/14740338.2013.827660 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Bradley MC, Motterlini N, Padmanabhan S, et al. Potentially inappropriate prescribing among older people in the United Kingdom. BMC Geriatr 2014;14:72. 10.1186/1471-2318-14-72 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Cahir C, Bennett K, Teljeur C, et al. Potentially inappropriate prescribing and adverse health outcomes in community dwelling older patients. Br J Clin Pharmacol 2014;77:201–10. 10.1111/bcp.12161 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Peron EP, Gray SL, Hanlon JT. Medication use and functional status decline in older adults: a narrative review. Am J Geriatr Pharmacother 2011;9:378–91. 10.1016/j.amjopharm.2011.10.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Wallace E, McDowell R, Bennett K, et al. Impact of potentially inappropriate prescribing on adverse drug events, health related quality of life and emergency Hospital attendance in older people attending general practice: a prospective cohort study. J Gerontol A Biol Sci Med Sci 2017;72:271–7. 10.1093/gerona/glw140 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Varga S, Alcusky M, Keith SW, et al. Hospitalization rates during potentially inappropriate medication use in a large population-based cohort of older adults. Br J Clin Pharmacol 2017;83:2572–80. 10.1111/bcp.13365 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Clyne B, Fitzgerald C, Quinlan A, et al. Interventions to address potentially inappropriate prescribing in primary care: a systematic review of randomised control trials. Int J Pharm Pract 2015;23:8–9. [Google Scholar]
- 24.Scott IA, Pillans PI, Barras M, et al. Using EMR-enabled computerized decision support systems to reduce prescribing of potentially inappropriate medications: a narrative review. Ther Adv Drug Saf 2018;9:559–73. 10.1177/2042098618784809 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Jokanovic N, Tan ECK, van den Bosch D, et al. Clinical medication review in Australia: a systematic review. Res Social Adm Pharm 2016;12:384–418. 10.1016/j.sapharm.2015.06.007 [DOI] [PubMed] [Google Scholar]
- 26.Riordan DO, Walsh KA, Galvin R, et al. The effect of pharmacist-led interventions in optimising prescribing in older adults in primary care: a systematic review. SAGE Open Med 2016;4:205031211665256. 10.1177/2050312116652568 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Craig P. Developing and evaluating complex interventions. Available: www.mrc.ac.uk/complexinterventionsguidance [Accessed 17 Jun 2019].
- 28.Michie S, van Stralen MM, West R. The behaviour change wheel: a new method for characterising and designing behaviour change interventions. Implement Sci 2011;6:42. 10.1186/1748-5908-6-42 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Tombor I, Michie S, Tombor I, et al. Methods of health behavior change. In: Oxford Research Encyclopedia of Psychology, 2017. [Google Scholar]
- 30.Arksey H, O’Malley L. Scoping studies: towards a methodological framework. Int J Soc Res Methodol Theory Pract 2005. [Google Scholar]
- 31.Levac D, Colquhoun H, O'Brien KK. Scoping studies: advancing the methodology. Implement Sci 2010;5:69. 10.1186/1748-5908-5-69 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Peters M, Godfrey C, McInerney P, et al. The Joanna Briggs Institute reviewers’ manual 2015: Methdology for JBI scoping reviews 2015.
- 33.Gardner AL, Thomas JM, Mecca MC, et al. Initiative to minimize pharmaceutical risk in older veterans (improve) polypharmacy clinic. Fed Pract 2018;35:40-47. [PMC free article] [PubMed] [Google Scholar]
- 34.Johansson T, Abuzahra ME, Keller S, et al. Impact of strategies to reduce polypharmacy on clinically relevant endpoints: a systematic review and meta-analysis. Br J Clin Pharmacol 2016;82:532–48. 10.1111/bcp.12959 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Rankin A, Cadogan CA, Patterson SM, et al. Interventions to improve the appropriate use of polypharmacy for older people. Cochrane Database Syst Rev 2018;9:CD008165. 10.1002/14651858.CD008165.pub4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Brandt M, Hallas J, Graabæk T, et al. Description of a practice model for pharmacist medication review in a general practice setting. Pharm Pract 2014;12:420. 10.4321/S1886-36552014000300005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Campins L, Serra-Prat M, Gózalo I, et al. Randomized controlled trial of an intervention to improve drug appropriateness in community-dwelling polymedicated elderly people. Fam Pract 2017;34:36–42. 10.1093/fampra/cmw073 [DOI] [PubMed] [Google Scholar]
- 38.Benson H, Lucas C, Kmet W, et al. Pharmacists in general practice: a focus on drug-related problems. Int J Clin Pharm 2018;40:566–72. 10.1007/s11096-018-0617-9 [DOI] [PubMed] [Google Scholar]
- 39.Blakey SA, Hixson-Wallace JA. Clinical and economic effects of pharmacy services in geriatric ambulatory clinic. Pharmacotherapy 2000;20:1198–203. 10.1592/phco.20.15.1198.34581 [DOI] [PubMed] [Google Scholar]
- 40.Reynolds A. Patient-Centered care. Radiol Technol 2009;81:133–47. [PubMed] [Google Scholar]
- 41.Hazen ACM, Zwart DLM, Poldervaart JM, et al. Non-dispensing pharmacists' actions and solutions of drug therapy problems among elderly polypharmacy patients in primary care. Fam Pract 2019;36:544–51. 10.1093/fampra/cmy114 [DOI] [PubMed] [Google Scholar]
- 42.Pharmaceutical Care Network Medication review definition approved - Pharmaceutical Care Network Europe, 2016. Available: https://www.pcne.org/news/35/medication-review-definition-approved
- 43.Zarowitz BJ, Stebelsky LA, Muma BK, et al. Reduction of high-risk polypharmacy drug combinations in patients in a managed care setting. Pharmacotherapy 2005;25:1636–45. 10.1592/phco.2005.25.11.1636 [DOI] [PubMed] [Google Scholar]
- 44.Harris IM, Westberg SM, Frakes MJ, et al. Outcomes of medication therapy review in a family medicine clinic. J Am Pharm Assoc 2009;49:623–7. 10.1331/JAPhA.2009.08069 [DOI] [PubMed] [Google Scholar]
- 45.Fick DM, Maclean JR, Rodriguez NA, et al. A randomized study to decrease the use of potentially inappropriate medications among community-dwelling older adults in a southeastern managed care organization. Am J Manag Care 2004;10:761–8. [PubMed] [Google Scholar]
- 46.Dalin DA, Vermehren C, Jensen AK, et al. 107 systematic medication review in general practice–a collaboration between clinical pharmacology and general practice. BMJ Evidence-Based Medicine 2018;23:1–2. [Google Scholar]
- 47.Fillit HM, Futterman R, Orland BI, et al. Polypharmacy management in Medicare managed care: changes in prescribing by primary care physicians resulting from a program promoting medication reviews. Am J Manag Care 1999;5:587–94. [PubMed] [Google Scholar]
- 48.Jäger C, Freund T, Steinhäuser J, et al. Impact of a tailored program on the implementation of evidence-based recommendations for multimorbid patients with polypharmacy in primary care practices-results of a cluster-randomized controlled trial. Implement Sci 2017;12:8. 10.1186/s13012-016-0535-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Milos V, Rekman E, Bondesson Åsa, et al. Improving the quality of pharmacotherapy in elderly primary care patients through medication reviews: a randomised controlled study. Drugs Aging 2013;30:235–46. 10.1007/s40266-013-0057-0 [DOI] [PubMed] [Google Scholar]
- 50.Gibert P, Cabaret M, Moulis M, et al. Optimizing medication use in elderly people in primary care: impact of STOPP criteria on inappropriate prescriptions. Arch Gerontol Geriatr 2018;75:16–19. 10.1016/j.archger.2017.10.022 [DOI] [PubMed] [Google Scholar]
- 51.Kiel WJ, Phillips SW. Impact of Pharmacist-Conducted comprehensive medication reviews for older adult patients to reduce medication related problems. Pharmacy 2017;6:2. 10.3390/pharmacy6010002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Woodward MC, Streeton CL, Guttmann A, et al. Polypharmacy management among Australian veterans: improving prescribing through the Australian department of Veterans' Affairs' prescriber feedback programme. Intern Med J 2008;38:95–100. 10.1111/j.1445-5994.2007.01453.x [DOI] [PubMed] [Google Scholar]
- 53.Vandenberg AE, Echt KV, Kemp L, et al. Academic detailing with provider audit and feedback improve prescribing quality for older veterans. J Am Geriatr Soc 2018;66:621–7. 10.1111/jgs.15247 [DOI] [PubMed] [Google Scholar]
- 54.Bluml BM. Definition of medication therapy management: development of Professionwide consensus. Available: www.japha.org [Accessed 6 Jun 2019]. [DOI] [PubMed]
- 55.Dauphinot V, Jean-Bart E, Krolak-Salmon P, et al. A multi-center, randomized, controlled trial to assess the efficacy of optimization of drug prescribing in an elderly population, at 18 months of follow-up, in the evolution of functional autonomy: the OPTIM study protocol. BMC Geriatr 2017;17:195. 10.1186/s12877-017-0600-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Schäfer I, Kaduszkiewicz H, Mellert C, et al. Narrative medicine-based intervention in primary care to reduce polypharmacy: results from the cluster-randomised controlled trial MultiCare AGENDA. BMJ Open 2018;8:e017653. 10.1136/bmjopen-2017-017653 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.The Office of the National Coordinator for Health Information Technology (ONC) Clinical decision support, 2018. Available: https://www.healthit.gov/topic/safety/clinical-decision-support
- 58.Streit S, Rozsnyai Z, Al B, et al. Optimising Pharmaco therapy in the multimorbid elderly in primary care a cluster randomized trial 2011;2012. [Google Scholar]
- 59.Schmidt-Mende K, Andersen M, Wettermark B, et al. Educational intervention on medication reviews aiming to reduce acute healthcare consumption in elderly patients with potentially inappropriate medicines-A pragmatic open-label cluster-randomized controlled trial in primary care. Pharmacoepidemiol Drug Saf 2017;26:1347–56. 10.1002/pds.4263 [DOI] [PubMed] [Google Scholar]
- 60.Lauster CD, Srivastava SB. Fundamental skills for patient care in pharmacy practice, 2014. Available: www.jblearning.com [Accessed 6 Jun 2019].
- 61.McKinnon M, Townsend J, Cooper J, et al. Systematic review and clinical governance in repeat prescribing in general practice. Prim Heal Care Res Dev 2001;2:235–40. 10.1191/146342301682157719 [DOI] [Google Scholar]
- 62.Tan ECK, Stewart K, Elliott RA, et al. Pharmacist consultations in general practice clinics: the pharmacists in practice study (PIPS). Res Social Adm Pharm 2014;10:623–32. 10.1016/j.sapharm.2013.08.005 [DOI] [PubMed] [Google Scholar]
- 63.Institute for Healthcare Improvement Institute for healthcare improvement: medication reconciliation to prevent adverse drug events. Available: http://www.ihi.org/Topics/ADEsMedicationReconciliation/Pages/default.aspx [Accessed 6 Jun 2019].
- 64.Muth C, Uhlmann L, Haefeli WE, et al. Effectiveness of a complex intervention on Prioritising Multimedication in Multimorbidity (PRIMUM) in primary care: results of a pragmatic cluster randomised controlled trial. BMJ Open 2018;8:e017740. 10.1136/bmjopen-2017-017740 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Thomas J, Zapatka S, Brienza R, et al. Mastering the art of deprescribing: an interprofessional outpatient polypharmacy program for older veterans using the shared medical appointment model. J Am Geriatr Soc 2014:1–331. [Google Scholar]
- 66.Parker SG, McCue P, Phelps K, et al. What is comprehensive geriatric assessment (CGA)? An umbrella review. Age Ageing 2018;47:149–55. 10.1093/ageing/afx166 [DOI] [PubMed] [Google Scholar]
- 67.Frankfort SV, Tulner LR, van Campen JPCM, et al. Evaluation of pharmacotherapy in geriatric patients after performing complete geriatric assessment at a diagnostic day clinic. Clin Drug Investig 2006;26:169–74. 10.2165/00044011-200626030-00007 [DOI] [PubMed] [Google Scholar]
- 68.Allard J, Hébert R, Rioux M, et al. Efficacy of a clinical medication review on the number of potentially inappropriate prescriptions prescribed for community-dwelling elderly people. CMAJ 2001;164:1291–6. [PMC free article] [PubMed] [Google Scholar]
- 69.Sinnott C, Mercer SW, Payne RA, et al. Improving medication management in multimorbidity: development of the multimorbidity collaborative medication review and decision making (my COMRADE) intervention using the behaviour change wheel. Implement Sci 2015;10:132. 10.1186/s13012-015-0322-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Rognstad S, Brekke M, Gjelstad S, et al. Potentially Inappropriate Prescribing to Older Patients: Criteria, Prevalence and an Intervention to Reduce It: The Prescription Peer Academic Detailing (Rx-PAD) Study - A Cluster-Randomized, Educational Intervention in Norwegian General Practice. Basic Clin Pharmacol Toxicol 2018;123:380–91. 10.1111/bcpt.13040 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjopen-2020-039543supp001.pdf (98.7KB, pdf)
bmjopen-2020-039543supp002.pdf (53.7KB, pdf)
bmjopen-2020-039543supp003.pdf (72.2KB, pdf)
bmjopen-2020-039543supp004.pdf (131KB, pdf)