Abstract
Background:
Football has the highest number of nontraumatic fatalities of any sport in the United States.
Purpose:
To compare the incidence of nontraumatic fatalities with that of traumatic fatalities, describe the epidemiology of nontraumatic fatalities in high school (HS) and college football players, and determine the effectiveness of National Collegiate Athletic Association (NCAA) policies to reduce exertional heat stroke (EHS) and exertional sickling (ES) with sickle cell trait (SCT) fatalities in athletes.
Study Design:
Descriptive epidemiology study.
Methods:
We retrospectively reviewed 20 academic years (1998-2018) of HS and college nontraumatic fatalities in football players using the National Registry of Catastrophic Sports Injuries (NRCSI). EHS and ES with SCT fatality rates were compared before and after the implementation of the NCAA football out-of-season model (bylaw 17.10.2.4 [2003]) and NCAA Division I SCT screening (bylaw 17.1.5.1 [2010]), respectively. Additionally, we compiled incidence trends for HS and college traumatic and nontraumatic fatalities in football players for the years 1960 through 2018 based on NRCSI data and previously published reports.
Results:
The risk (odds ratio) of traumatic fatalities in football players in the 2010s was 0.19 (95% CI, 0.13-0.26; P < .0001) lower in HS and 0.29 (95% CI, 0.29-0.72; P = .0078) lower in college compared with that in the 1960s. In contrast, the risk of nontraumatic fatalities in football players in the 2010s was 0.7 (95% CI, 0.50-0.98; P = .0353) in HS and 0.9 (95% CI, 0.46-1.72; P = .7413) in college compared with that in the 1960s. Since 2000, the risk of nontraumatic fatalities has been 1.89 (95% CI, 1.42-2.51; P < .001) and 4.22 (95% CI, 2.04-8.73; P < .001) higher than the risk of traumatic fatalities at the HS and college levels, respectively. During the 20 years studied, there were 187 nontraumatic fatalities (average, 9.4 per year). The causes of death were sudden cardiac arrest (57.7%), EHS (23.6%), ES with SCT (12.1%), asthma (4.9%), and hyponatremia (1.6%). The risk of a nontraumatic fatality was 4.1 (95% CI, 2.8-5.9; P < .0001) higher in NCAA compared with HS athletes. There was no difference in the risk of an EHS fatality in NCAA athletes (0.86 [95% CI, 0.17-4.25]; P = .85) after implementation in 2003 of the NCAA football out-of-season model. The risk of an ES with SCT fatality in Division I athletes was significantly lower after the 2010 NCAA SCT screening bylaw was implemented (0.12 [95% CI, 0.02-0.95]; P = .04).
Conclusion:
Since the 1960s, the risk of nontraumatic fatalities has declined minimally compared with the reduction in the risk of traumatic fatalities. Current HS and college nontraumatic fatality rates are significantly higher than rates of traumatic fatalities. The 2003 NCAA out-of-season model has failed to significantly reduce EHS fatalities. The 2010 NCAA SCT screening bylaw has effectively prevented ES with SCT fatalities in NCAA Division I football.
Keywords: football, fatalities, cardiac, sickle cell trait, exertional heat illness, asthma, prevention
Football, one of the most popular team sports in the United States, has the highest number of fatalities of any high school (HS) or college sport.4,13 Over a 55-year period (1945-1999), a total of 718 fatalities were documented in football at the professional, college, HS, and recreational levels.6 In a report on fatalities due to trauma in young, competitive athletes in all sports over a 30-year span, football caused almost 60% of the fatalities.29 Football also had the highest number of nontraumatic sports-related deaths in HS and college athletes over a 10-year period (1983-1993).31 The most recent comprehensive report on fatalities in HS and college football players identified an average of 12 players dying annually because of traumatic and nontraumatic causes between 1990 and 2010.4
After high-profile out-of-season training deaths, in 2001, the National Collegiate Athletic Association (NCAA) enacted an out-of-season training model to ensure the health and safety of student-athletes engaging in these workouts.3 The model, effective in 2003, mandated acclimatization rules focusing on the first 5 days of the preseason and limited the number and duration of practices and equipment worn.3 There are no acclimatization guidelines outside of the preseason. The only restrictions during winter and summer sessions are a maximum of 8 hours per week of conditioning, weight training, reviews of game film, and walk-throughs.21,22 At the HS level, the National Federation of State High School Associations (NFHS) makes recommendations, but implementation is dependent on individual states. Since 2011, a total of 15 states have mandated heat-illness prevention guidelines.1,9
The settlement of litigation in an NCAA Division I member institution from a fatality due to exertional sickling (ES) with sickle cell trait (SCT) prompted the NCAA to mandate SCT screening, documentation of previous screening, or declination of testing with a signed written release during the preparticipation examination (PPE) for Division I football athletes, effective August 1, 2010.21 NCAA Divisions II23 and III24 adopted the SCT policy in 2012 and 2013, respectively. Associated guidelines promoted targeted education of SCT status inclusive of signs and symptoms of ES with SCT as well as settings presenting the risk for ES with SCT.20 Tailored precautions were recommended, such as allowing athletes with SCT to train at their own pace; receive adequate hydration; be excused from performance tests, such as serial sprints or timed miles; never to be urged to exercise at 100% beyond 2 or 3 minutes without offering a break; discontinue activity upon struggling or experiencing symptoms; and receive immediate medical attention if experiencing any symptoms.19,20 There are currently no legislated HS regulations regarding SCT screening education or precautions; however, the National Athletic Trainers’ Association has published a consensus statement recommending SCT guidelines for athletes.19
This is part 1 of a 2-part study. The purpose of part 1 was to compare the incidence of nontraumatic fatalities with that of traumatic fatalities, describe the epidemiology of nontraumatic fatalities in HS and college football players, and determine the effectiveness of NCAA policies to reduce exertional heat stroke (EHS) and ES with SCT fatalities. The aim of part 2 was to explore the characteristics of the training programs to determine the causes of nontraumatic deaths.5 After the causes of these fatalities are identified, prevention strategies can be developed and implemented.
Methods
Injury Definitions
This study was exempted from institutional review board approval. Exertion-related nontraumatic fatalities were classified as systemic compromise secondary to medical conditions, such as sudden cardiac arrest (SCA), EHS, ES with SCT, asthma, and hyponatremia. Athletes with pulmonary embolisms and infections secondary to a previous traumatic injury or surgery, as well as direct impact from lightning, were excluded from this study. Fatalities in football players were limited to HS and college athletes. College athletes not participating in an NCAA member institution were excluded from the 20-year review because EHS and ES with SCT guidelines for other leagues did not coincide with NCAA EHS and ES with SCT policies.
Injury Reports, Surveillance, and Statistics
Data on the number and incidence of nontraumatic fatalities in HS and college (NCAA and other college sports associations) football participants between 1960 and 20184,6,18,31 were compiled from previously published reports.4,6,18,31
Between July 1998 and June 2018, one of the authors (S.A.A.) collected football-related fatality case information (name, date of injury, diagnosis, and level of play) from organized, supervised school-sponsored sports at the HS and NCAA levels, compiling the data into the National Registry of Catastrophic Sports Injuries (NRCSI). Sources for event occurrence were extensive media reports and newspaper clippings, autopsy reports, certificates of death, case-related legal documents, depositions, school-sponsored investigations, published medical literature, and Freedom of Information Act reports. In 2017 and 2018, we retrospectively acquired additional investigative data (anthropometric data, game or practice, out-of-season vs in-season, and workout characteristics) on cause of death and treatment. Annual rates and incidences of fatalities, before and after NCAA bylaws for acclimatization (5/1/2003) and SCT (8/1/2010), were computed by a statistician (W.L.). The odds ratio, 95% CI, and P value were assessed for NCAA versus HS athletes per diagnosis, NCAA and HS before versus after NCAA bylaws, and HS EHS fatalities for the first versus second decade. ES with SCT fatalities were also analyzed separately for NCAA Division I African American football players.
Participation Numbers
During the study period, there were 23,681,497 HS (average, 1,184,075 annually) and 1,285,095 NCAA (average, 64,255 annually) football players.25,26 Participation numbers were based on data provided by the NCAA25 and the NFHS plus an additional 100,000 players (estimate based on the NFHS recommendation) each year for non-NFHS schools.26
Results
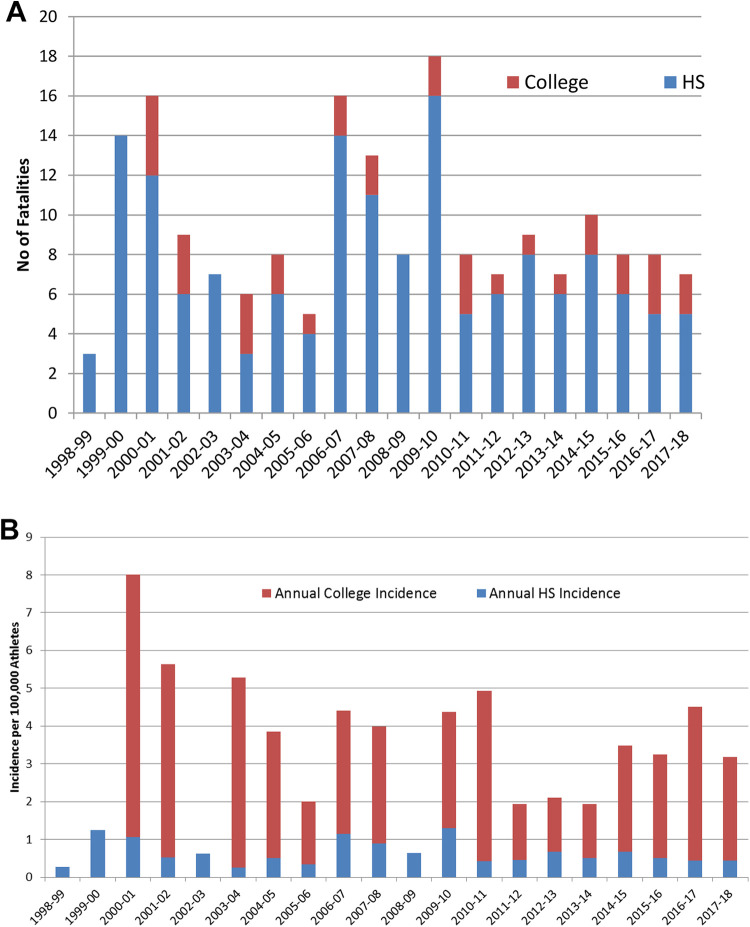
The risk of traumatic fatalities in football players in the 2010s was 0.19 (95% CI, 0.013-0.26; P < .0001) lower in HS (Figure 1A) and 0.29 (95% CI, 0.29-0.72; P = .0078) lower in college (Figure 1B) compared with that in the 1960s. In contrast, the risk of nontraumatic fatalities in football players in the 2010s was 0.7 (95% CI, 0.50-0.98; P = .0353) in HS and 0.9 (95% CI, 0.46-1.72; P = .7413) in college compared with that in the 1960s. Since 2000, the risk of nontraumatic fatalities has been 1.89 (95% CI, 1.42-2.51; P < .001) and 4.22 (95% CI, 2.04-8.73; P < .001) higher than the risk of traumatic fatalities at the HS and college levels, respectively.
Figure 1.
(A) Incidence of traumatic and nontraumatic deaths in high school football players by decade. (B) Incidence of traumatic and nontraumatic deaths in college football players by decade.
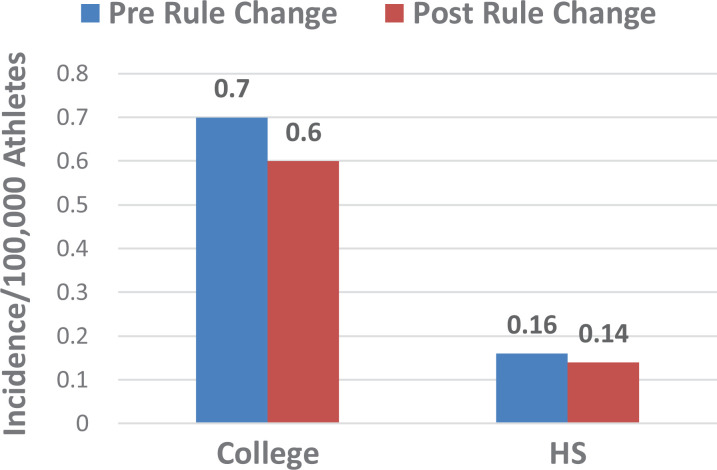
During the 20-year study period, there were 191 nontraumatic fatalities in football players; 4 fatalities (3 National Junior College Athletic Association and 1 National Association of Intercollegiate Athletics) were excluded for the comprehensive review. Of the remaining 187 fatalities (average, 9.4 annually), all cases involved male athletes: 153 (average, 7.7 annually) in HS and 34 (average, 1.7 annually) in NCAA athletes (Figure 2 and Table 1). The diagnosis was unknown in 5 cases. When known, the causes of nontraumatic fatalities were SCA (n = 105; 57.7%), EHS (n = 43; 23.6%), ES with SCT (n = 22; 12.1%), asthma (n = 9; 4.9%), and hyponatremia (n = 3; 1.6%) (Figure 3). The risk of a nontraumatic fatality was significantly higher in athletes at the college level compared with those at the HS level for all diagnoses (4.1) as well as individual diagnoses of ES with SCT (22.1), EHS (4.21), and SCA (2.6) (Table 1).
Figure 2.
(A) Number of fatalities in football players annually at the high school (HS) and college levels. (B) Fatality incidence per 100,000 football athletes at the HS and college levels.
Table 1.
Fatalities for Total and Specific Diagnoses at the HS and NCAA Levelsa
| Total | HS | NCAA | Per 100,000 Athletes | Odds Ratio (95% CI); P Value | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| No. | Annual Average | No. | Annual Average | No. | Annual Average | Total | HS | NCAA | ||
| All | 187 | 9.35 | 153 | 7.65 | 34 | 1.7 | 0.74 | 0.65 | 2.65 | 4.1 (2.8-5.9); P < .0001 |
| SCA | 105 | 5.3 | 92 | 4.6 | 13 | 0.7 | 0.42 | 0.39 | 1.01 | 2.6 (1.46-4.65); P = .0012 |
| EHS | 43 | 2.15 | 35 | 1.75 | 8 | 0.4 | 0.17 | 0.15 | 0.62 | 4.21 (1.95-9.08); P = .0002 |
| ES with SCT | 22 | 1.1 | 10 | 0.5 | 12 | 0.6 | 0.09 | 0.04 | 0.93 | 22.1 (9.6-51.2); P = .0001 |
| Asthma | 9 | 0.45 | 8 | 0.4 | 1 | 0.05 | 0.04 | 0.03 | 0.08 | 2.3 (0.3-19.4); P = .43 |
| Hyponatremia | 3 | 0.15 | 3 | 0.15 | 0 | 0.0 | 0.01 | 0.01 | 0.00 | |
| Unknown | 5 | 0.25 | 5 | 0.25 | 0 | 0.0 | 0.02 | 0.02 | 0.00 | |
aEHS, exertional heat stroke; ES, exertional sickling; HS, high school; NCAA, National Collegiate Athletic Association; SCA, sudden cardiac arrest; SCT, sickle cell trait.
Figure 3.
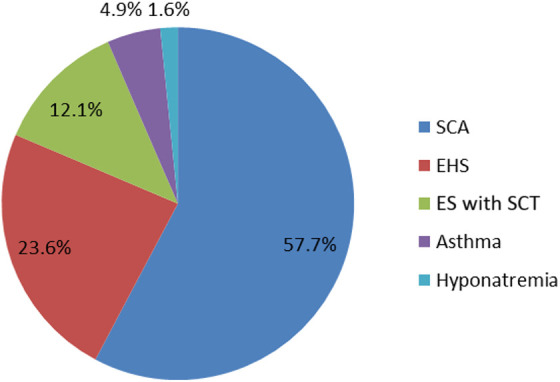
Percentage of fatalities in football players by diagnosis. EHS, exertional heat stroke; ES, exertional sickling; SCA, sudden cardiac arrest; SCT, sickle cell trait.
Causes
Sudden Cardiac Arrest
There were 105 deaths (average, 5.3 annually) due to cardiac causes: 92 in HS and 13 in NCAA athletes (Table 1 and Figure 3). A precise diagnosis could not be determined in 64 cases. For the remaining 41 cases, the diagnoses were hypertrophic cardiomyopathy (n = 22), myocardial infarction (n = 4), congenital heart defect (n = 4), arrhythmia (n = 4), coronary artery anomaly (n = 2), aortic aneurysm (n = 1), atrial myxoma (n = 1), long QT syndrome (n = 1), myocarditis (n = 1), and hypertensive heart disease (n = 1).
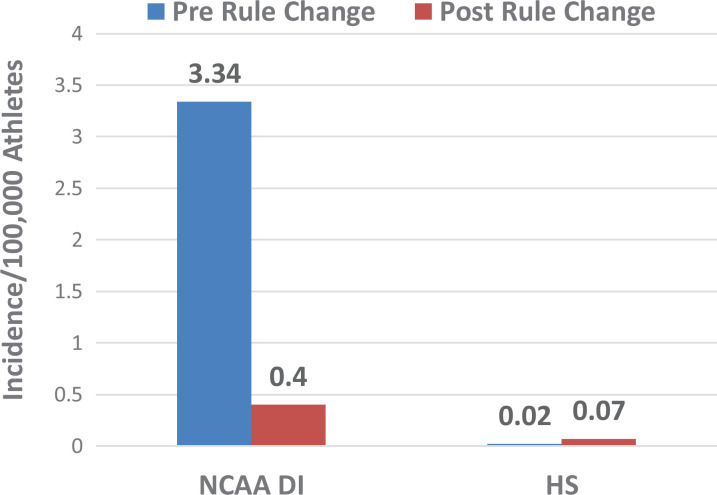
Exertional Heat Stroke
There were 43 deaths (average, 2.15 annually) secondary to complications from EHS: 35 in HS and 8 in NCAA players (Table 1). A total of 19 athletes were White, 15 were African American, 1 was Hispanic, and the race of 8 was unknown. The risk (0.86 [95% CI, 0.17-4.25]; P = .85), incidence (0.7 before and 0.6 after per 100,000 participants), and average annual rate (0.4 before and 0.4 after) of an EHS fatality in an NCAA player did not change significantly after implementation in 2003 of the NCAA football out-of-season model with its acclimatization period (Figure 4). Overall, 67% (4/6) of EHS fatalities in NCAA players after the 2003 bylaw occurred outside of the 5-day preseason acclimatization period. Before and after 2003, there was no difference in the risk (0.91 [95% CI, 0.42-1.93]; P = .80), incidence (0.16 before and 0.14 after per 100,000 participants), or average annual rate (2.0 before and 1.7 after) of EHS fatalities in HS players (Figure 4).
Figure 4.
The incidence of exertional heat stroke fatalities per 100,000 athletes before and after the 2003 National Collegiate Athletic Association acclimatization bylaw. HS, high school.
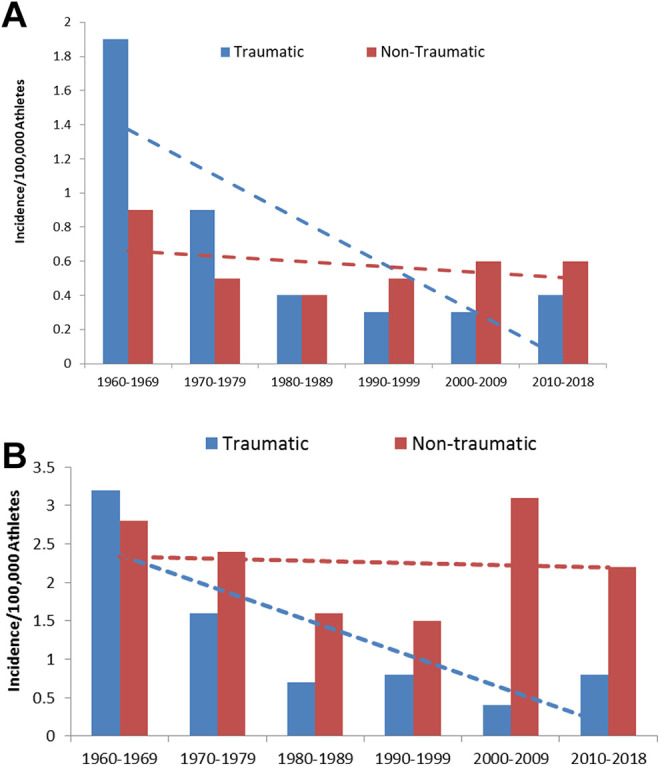
ES With SCT
There were 22 (average, 1.1 annually) deaths due to ES with SCT: 10 in HS and 12 in NCAA players (Table 1). A total of 21 (95%) athletes were African American, and 1 (5%) was White. The risk of an ES with SCT fatality in Division I athletes (0.12 [95% CI, 0.02-0.95]; P = .04) and Division I African American athletes (0.11 [95% CI, 0.01-0.86]; P = .04) was significantly lower after the 2010 NCAA SCT screening bylaw was implemented. In Division I football, there were 10 ES with SCT deaths in the 12 years before the 2010 NCAA screening bylaw and only 1 death in the 8 subsequent years. The average annual rate and incidence of Division I ES with SCT fatalities declined after the bylaw from 0.83 to 0.13 per year (85% reduction) and from 3.34 to 0.40 per 100,000 athletes (88% reduction), respectively (Figure 5). For Division I African American athletes, the average annual rate and incidence of ES with SCT fatalities declined after the bylaw from 0.83 to 0.25 per year and from 7.77 to 0.86 per 100,000 athletes, respectively. The risk of an ES with SCT fatality in all (Divisions I, II, and III) NCAA athletes (0.26 [95% CI, 0.06-1.16]; P = .08) was lower after implementation of the bylaw but did not reach statistical significance. Both deaths in NCAA athletes occurring after the bylaw implementation, 1 each in Divisions I and II, were due to noncompliance.
Figure 5.
The incidence of exertional sickling with sickle cell trait (SCT) fatalities per 100,000 athletes before and after the National Collegiate Athletic Association (NCAA) 2010 SCT screening bylaw. DI, Division I; HS, high school.
The risk of an ES with SCT fatality in HS players was 3.5 (95% CI, 0.8-16.3; P = .07) times higher after the NCAA bylaw was mandated in 2010 (Figure 5). The average annual rate and incidence of ES with SCT fatalities in HS players increased during the time span after the NCAA rule from 0.25 to 0.88 per year and from 0.02 to 0.07 per 100,000 athletes, respectively.
Asthma and Hyponatremia
A total of 9 deaths (average, 0.45 annually) resulted from asthma complications: 8 in HS and 1 in NCAA players (Table 1). Overall, 3 deaths (average, 0.15 annually) resulted from hyponatremia, all in HS players (Table 1).
Discussion
This study revealed a dramatic reduction in the incidence of traumatic fatalities in football players at the HS (81%) and college (71%) levels between the 1960s and 2010s. This decline is likely because of improved football helmets in the 1970s, which significantly reduced the number of skull fractures, the ban on spear tackling, and improved medical care.4,6,30 In contrast, this study demonstrated that the risk of nontraumatic fatalities has only declined minimally since the 1960s. Further, since 2000, the risk of nontraumatic fatalities has been 2 times higher than that of traumatic fatalities at the HS level and 4 times higher at the college level. The increased risk of nontraumatic fatalities requires further research into causation but may be because of the excessive intensity of conditioning drills.5
The incidence trends and number of nontraumatic fatalities identified by the NRCSI in this study concur with data from the National Center for Catastrophic Sport Injury Research (NCCSIR).13 The NCCSIR reported a similar reduction in nontraumatic fatalities since the 1960s but a constant rate of nontraumatic fatalities.13 The NCCSIR reported 203 nontraumatic (average, 10.2 per year) fatalities over a similar 20-year span between 1999 and 2018.13 The slightly higher number of fatalities in their database is likely because of the inclusion of middle school and junior college athletes as well as fatalities due to infections and pulmonary embolisms.4,13
Nontraumatic fatalities in this study were more numerous in HS athletes (82%) compared with NCAA athletes because of higher participation numbers; however, the overall risk of a fatality was 4.1 times higher at the NCAA level. This study concurs with a previous report that NCAA football athletes are at a higher risk for fatalities.4 This may be because of the excessive intensity of conditioning exercises at the college level. Therefore, an evaluation of existing NCAA rules and the development of improved guidelines for persistent problems should be a primary focus of prevention strategies.
Cardiac Fatalities
The data in this study concur with other reports that SCA is the leading cause of mortality in HS, college, and youth athletes, with hypertrophic cardiomyopathy being the most frequent diagnosis.4,10,14,15 However, the incidence of cardiac fatalities may be overestimated, as many of these cases, especially at the HS level, had limited data confirming the exact diagnosis.
Heat-Related Fatalities
Although the total number of EHS deaths in NCAA athletes was low and should be interpreted with caution, the results of this study demonstrated that the 5-day preseason acclimatization component of the NCAA out-of-season model, adopted in 2003, has not resulted in a significant reduction in the risk, incidence, or rate of EHS fatalities. One possible explanation is that some colleges may have adopted a similar preventive measure before it was mandated. A previous report4 has demonstrated a combined increased risk (1.5) of EHS fatalities in NCAA and HS athletes in the decade from 2000-2010 compared with 1990-1999. In another report,1 the authors stated that the 2003 bylaw was successful at reducing EHS fatalities in college athletes but only provided absolute numbers and not the risk or incidence. The authors identified 1 EHS fatality in an NCAA athlete since 2003 compared with 6 in this report.1 Additionally, 67% of the NCAA EHS fatalities since 2003 occurred outside of the 5-day preseason period, indicating that a brief preseason acclimatization period is inadequate at preventing EHS fatalities. The 5-day acclimatization period focuses on the football equipment worn, number of practices, and duration of practice sessions, with no regard for the intensity of conditioning drills or other risk factors. Despite the limitations in determining the effectiveness of the NCAA bylaw, fatalities are still occurring, and further preventive measures are required. Therefore, in addition to the NCAA bylaws, the focus should be on all 365 days of the year, inclusive of EHS risk factors, with exertion as a primary factor.5
The results revealed that the national risk of an EHS fatality in HS athletes declined slightly after 2003 but did not achieve statistical significance. This decline may be partially because of new preseason heat-related policies implemented in 15 states since 2011.1,9 These guidelines are similar to the NCAA bylaws and focus on environmental conditions as well as the frequency and duration of conditioning sessions, although there is no mention of exercise intensity or body habitus.5 We believe that the reason for the limited effectiveness of HS heat-related policies, similar to the NCAA, is that current guidelines focus on environmental causes of EHS, emphasizing acclimatization over excessive exertion and body habitus.5,8,9,11 We recommend a paradigm shift to prevent overexertion, which is the primary factor in EHS fatalities.5,27
ES With SCT
The 2010 NCAA bylaw 17.1.5.1, with targeted education and tailored precautions for the athlete with SCT, has successfully reduced the risk (0.12) and incidence (from 3.34 to 0.40 per 100,000) of ES with SCT deaths in Division I football athletes. Since its implementation in 2010 and through 2018, the bylaw has spared the life of an estimated 5 Division I football players. Compliance with the bylaw and associated precautions would have resulted in an estimated 7 lives spared through 2018. The bylaw did not have a significant effect on Division II or III deaths, as there were no deaths before the bylaw during our study period.
ES with SCT fatalities occur predominantly, but not exclusively, in African American athletes. An inherited condition, carrying 1 normal hemoglobin gene and 1 abnormal sickle gene, SCT is present in all populations and is most prominent in African Americans, in which 8% carry the trait.12 Athletes with SCT have been reported to have a 10- to 37-fold higher risk of sudden death compared with that of athletes without SCT.12,17 In this study, 95% of ES with SCT fatalities occurred in African American athletes. Assuming that 8% of the African American population in this study carried the sickle gene, the risk of death in Division I football athletes with presumed SCT was reduced 9-fold, from 1 in 1029 to 1 in 9315 athletes after the bylaw was implemented.
In both ES with SCT fatalities in NCAA athletes (2014 and 2016) occurring after the 2010 bylaw was implemented, there were noncompliance issues. In one case, the player signed a waiver, and the school was not aware of the athlete’s SCT status. This may be a flaw in the bylaw, as athletes decline testing based on how options are presented during the PPE. We recommend that awareness of SCT status be mandatory in the PPE. In the second case (see part 2,5 Appendix 2, case report 2), SCT precautions and the recommended medical response were not followed. There are no reported ES fatalities when SCT status was known, the athlete and staff were educated and there was compliance with ES precautions.
At the HS level in which there are no legislated SCT testing requirements, the risk (3.5) and incidence (from 0.02 to 0.07 per 100,000 participants) of ES with SCT fatalities has increased since 2010. It is possible that this rate of increase is falsely elevated because of improved recognition of ES with SCT in the second decade and the misdiagnosis of ES with SCT as a cardiac or EHS fatality in the first decade.4 Since 1995, all 50 states and the District of Columbia have required SCT screening at birth. However, communication of natal SCT status may not occur. Athletes entering athletic participation at the youth and HS levels often are unaware of their SCT status and thereby lack education of SCT signs and symptoms, settings of risk, and precautions. Based on the success of the NCAA bylaw and precautions, we recommend SCT status confirmation during the PPE be required for all sports, at all levels, granting pediatricians and family practice physicians the opportunity to counsel this population.28
Asthma and Hyponatremia
Exercise-induced asthma occurs in 8% to 10% of school-aged children. Our results concur with those of other studies that asthma-related fatalities in HS and college athletes are rare.4,7,31 In a comprehensive study of 61 asthma-related deaths in athletes between 1993 and 2000, most deaths occurred in athletes aged between 10 and 20 years.2 Basketball and track were the most frequent sports played, with football players representing 8% of fatalities.2 Exercise-associated hyponatremia has been reported in 10% to 20% of distance athletes.16 However, fatalities due to hyponatremia are rare in young athletes participating in team sports and were observed in only 3 athletes in this study.
Limitations
It is possible that all fatalities in organized HS and college football players were not identified; therefore, any flaw in the collection of data would have been one of underreporting. This is unlikely because these deaths are highly visible events with extensive reporting by the news media. In addition, the incidence trends and number of fatalities in this study closely mirror those of another national catastrophic injury database.4,13 The strength of this study is reliance on an abundance of investigative documentation to include autopsies, certificates of death, depositions, and school-sponsored independent reports. Limited case information, especially at the HS level, may confound the exact diagnosis, resulting in an overestimation of cardiac fatalities while underestimating other nontraumatic causes of death.
Conclusion
There has been a 71% (college) to 81% (HS) reduction in the risk of traumatic fatalities since the 1960s. In contrast, the risk of nontraumatic fatalities in football players has declined minimally since the 1960s, with rates since the 2000s being 2 (HS) to 4 (college) times higher than the risk of traumatic fatalities. The most common causes of nontraumatic fatalities in football players were SCA, EHS, ES with SCT, asthma, and hyponatremia. Although the number of heat-related fatalities was low, the NCAA out-of-season model, with a 5-day acclimatization period, implemented in 2003, did not appear to have had a significant effect on reducing EHS fatalities, and further preventive measures are recommended. The SCT screening bylaw adopted by the NCAA in 2010, with associated precautions, has successfully prevented ES with SCT fatalities in NCAA Division I football players. Similar SCT guidelines and enforced compliance should be mandated in all sports at all levels. The findings in this study indicate that further research is necessary to determine the causes and preventive strategies for nontraumatic fatalities in football players.
Footnotes
Accepted for presentation at the annual meeting of the AOSSM, July 2020.
Final revision submitted April 3, 2020; accepted April 23, 2020.
One or more of the authors has declared the following potential conflict of interest or source of funding: K.M.F. has received consulting fees from Flexion Therapeutics. AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
Ethical approval for this study was waived by the University of Oklahoma.
References
- 1. Adams WM, Casa DJ, Drezner JA. Sport safety policy changes: saving lives and protecting athletes. J Athl Train. 2016;51(4):358–360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Becker JM, Rogers J, Rossini G, Mirchandani H, D’Alonzo GE., Jr Asthma deaths during sports: report of a 7-year experience. J Allergy Clin Immunol. 2004;113(2):264–267. [DOI] [PubMed] [Google Scholar]
- 3. Blackwell C. Division I off-season football plan makes athlete safety first and goal. NCAA News. October 14, 2002:1–2. [Google Scholar]
- 4. Boden BP, Breit I, Beachler JA, Williams A, Mueller FO. Fatalities in high school and college football players. Am J Sports Med. 2013;41(5):1108–1116. [DOI] [PubMed] [Google Scholar]
- 5. Boden BP, Fine KM, Spencer TA, Breit I, Anderson SA. Nontraumatic exertional fatalities in football players, part 2: excess in conditioning kills. Orthop J Sports Med. 2020;8(8):2325967120943491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Cantu RC, Mueller FO. Brain injury-related fatalities in American football, 1945-1999. Neurosurgery. 2003;52(4):846–853. [DOI] [PubMed] [Google Scholar]
- 7. Carlsen KH, Hem E, Stensrud T. Asthma in adolescent athletes. Br J Sports Med. 2011;45(16):1266–1271. [DOI] [PubMed] [Google Scholar]
- 8. Casa DJ, Almquist J, Anderson SA, et al. The inter-association task force for preventing sudden death in secondary school athletics programs: best-practices recommendations. J Athl Train. 2013;48(4):546–553. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Casa DJ, Csillan D, Armstrong LE, et al. Preseason heat-acclimatization guidelines for secondary school athletics. J Athl Train. 2009;44(3):332–333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Endres BD, Kerr ZY, Stearns RL, et al. Epidemiology of sudden death in organized youth sports in the United States, 2007-2015. J Athl Train. 2019;54(4):349–355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Grundstein AJ, Hosokawa Y, Casa DJ. Fatal exertional heat stroke and American football players: the need for regional heat-safety guidelines. J Athl Train. 2018;53(1):43–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Harris KM, Haas TS, Eichner ER, Maron BJ. Sickle cell trait associated with sudden death in competitive athletes. Am J Cardiol. 2012;110(8):1185–1188. [DOI] [PubMed] [Google Scholar]
- 13. Kucera K, Klossner D, Colgate B, Cantu R. Annual survey of football injury research, 1931-2017. Accessed April 17, 2019 https://nccsir.unc.edu/files/2019/02/Annual-Football-2018-Fatalities-FINAL.pdf
- 14. Maron BJ. Sudden death in young athletes. N Engl J Med. 2003;349(11):1064–1075. [DOI] [PubMed] [Google Scholar]
- 15. Maron BJ, Doerer JJ, Haas TS, Tierney DM, Mueller FO. Sudden deaths in young competitive athletes: analysis of 1866 deaths in the United States, 1980-2006. Circulation. 2009;119(8):1085–1092. [DOI] [PubMed] [Google Scholar]
- 16. McDermott BP, Anderson SA, Armstrong LE, et al. National Athletic Trainers’ Association position statement: fluid replacement for the physically active. J Athl Train. 2017;52(9):877–895. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Mitchell BL. Sickle cell trait and sudden death: bringing it home. J Natl Med Assoc. 2007;99(3):300–305. [PMC free article] [PubMed] [Google Scholar]
- 18. Mueller FO, Cantu RC, Van Camp SP Catastrophic Injuries in High School and College Sports. Vol 8 Human Kinetics; 1996. [Google Scholar]
- 19. National Athletic Trainers’ Association. Consensus statement: sickle cell trait and the athlete. Accessed April 15, 2019 https://www.nata.org/sites/default/files/sicklecelltraitandtheathlete.pdf
- 20. National Collegiate Athletic Association. 2014-15 NCAA Sports Medicine Handbook. NCAA; 2014. [Google Scholar]
- 21. National Collegiate Athletic Association. 2018-19 NCAA Division I Manual. Bylaw 13.11.3.7.3: Mandatory Medical Examination. NCAA; 2018. [Google Scholar]
- 22. National Collegiate Athletic Association. 2018-19 NCAA Division I Manual. Bylaw 13.11.3.7.4: Strength and Conditioning Coach First Aid/CPR Certification and Authority of Sports Medicine Staff. NCAA; 2018. [Google Scholar]
- 23. National Collegiate Athletic Association. NCAA Division II Manual. Bylaw 17.1.5.1: Sickle Cell Solubility Test. NCAA; 2018. [Google Scholar]
- 24. National Collegiate Athletic Association. NCAA Division III Manual. Bylaw 17.1.6.4.1: Confirmation of Sickle Cell Trait Status. NCAA; 2018. [Google Scholar]
- 25. National Collegiate Athletic Association. Resources. Accessed November 17, 2018 http://www.ncaa.org/about/resources/research/ncaa-sports-sponsorship-and-participation-rates-database
- 26. National Federation of State High School Associations. Participation statistics. Accessed February 12, 2019 http://www.nfhs.org/ParticipationStatics/ParticipationStatics.aspx/
- 27. Rav-Acha M, Hadad E, Epstein Y, Heled Y, Moran DS. Fatal exertional heat stroke: a case series. Am J Med Sci. 2004;328(2):84–87. [DOI] [PubMed] [Google Scholar]
- 28. Taylor C, Kavanagh P, Zuckerman B. Sickle cell trait: neglected opportunities in the era of genomic medicine. JAMA. 2014;311(15):1495–1496. [DOI] [PubMed] [Google Scholar]
- 29. Thomas M, Haas TS, Doerer JJ, et al. Epidemiology of sudden death in young, competitive athletes due to blunt trauma. Pediatrics. 2011;128(1):e1–e8. [DOI] [PubMed] [Google Scholar]
- 30. Torg JS, Guille JT, Jaffe S. Injuries to the cervical spine in American football players. J Bone Joint Surg Am. 2002;84(1):112–122. [DOI] [PubMed] [Google Scholar]
- 31. Van Camp SP, Bloor CM, Mueller FO, Cantu RC, Olson HG. Nontraumatic sports death in high school and college athletes. Med Sci Sports Exerc. 1995;27(5):641–647. [PubMed] [Google Scholar]