Abstract
Patient: Female, 45-year-old
Final Diagnosis: Multiple splanchnic artery aneurysms secondary to median arcuate ligament syndrome • occlusion of the coeliac trunk • significant stenosis of the superior mesenteric artery
Symptoms: Abdominal pain • postprandial abdominal pain • weight loss
Medication:—
Clinical Procedure: Aorto-hepatic bypass • endovascular aneurysm embolization
Specialty: Surgery
Objective:
Rare disease
Background:
Median arcuate ligament syndrome (MALS) is a rare and often misdiagnosed condition affecting about 0.4% of the population, typically ages 20–50 years old, and more frequently females. Caused by the compression of the celiac artery and adjacent nervous structures by the median arcuate ligament, it is typically manifested by postprandial abdominal pain, nausea or vomiting, and loss of weight. This condition also results in compensatory increased blood flow in peripancreatic arcades, facilitating formation of true aneurysms of the visceral vessels.
Case Report:
A 45-year-old woman with hypertension and left inferior renal pole cysts was referred to our department due to chronic, recurrent postprandial abdominal pains, nausea, and weight loss of approximately 15 kg in 1 year. A computed tomography (CT) scan demonstrated complete occlusion of the celiac trunk, significant stenosis of the superior mesenteric artery, and multiple aneurysms up to 17 mm in collateral circulatory vessels. Surgical decompression of the median arcuate ligament was performed and venous bypass was implanted between the aorta and the common hepatic artery, resulting in restoration of proper blood in the visceral circulation. Subsequently, 2 endovascular embolizations of visceral aneurysms were successfully performed. In the 48-month follow-up period, there was resolution of symptoms and no aneurysm formation was observed.
Conclusions:
Endovascular methods should be the treatment of choice in patients with splanchnic artery aneurysms. However, in patients with multiple aneurysms secondary to MALS, arterial reconstruction may be considered prior to performing an endovascular procedure to restore physiological blood flow in the visceral circulation.
MeSH Keywords: Aneurysm; Celiac Artery; Decompression, Surgical; Embolization, Therapeutic; Endovascular Procedures
Background
Median arcuate ligament syndrome (MALS), also called Dunbar Syndrome, is a rare and often misdiagnosed condition first reported by B. Lipshutz, and described in the 1960s by Harjola and Dunbar. It affects about 0.4% of the population, more frequently females, and is characterized by the following symptoms: postprandial abdominal pain, nausea or vomiting, and loss of weight, most frequently manifesting at ages 20–50 years [1]. The compensatory increased blood flow in the splanchnic arteries, secondary to the celiac axis stenosis or occlusion, facilitates the formation of true aneurysms of the visceral vessels. Treatment of celiac trunk stenosis coexisting with visceral artery aneurysms is a complex problem in which both endovascular and open surgical methods are feasible; however, there is no consensus on the treatment algorithms or preferred methods. In this report we discuss our clinical experience and approach to this complex issue, illustrated by the case of a successfully treated 45-year-old woman with multiple splanchnic artery aneurysms secondary to MALS.
Case Report
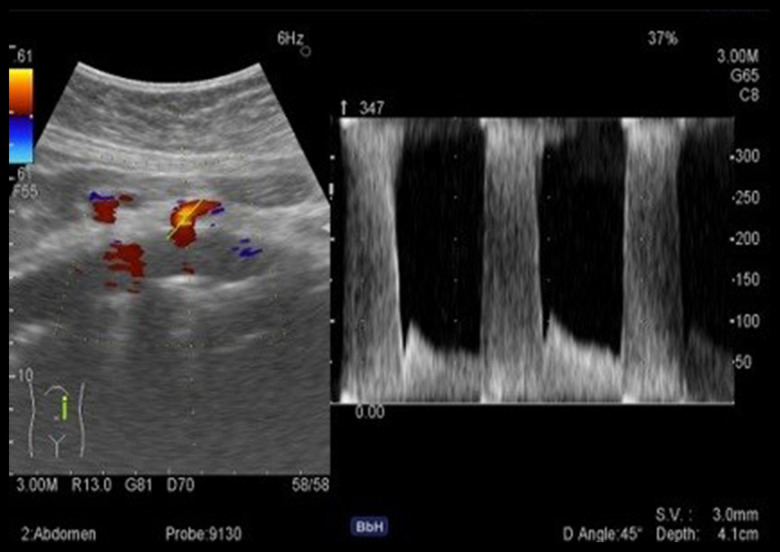
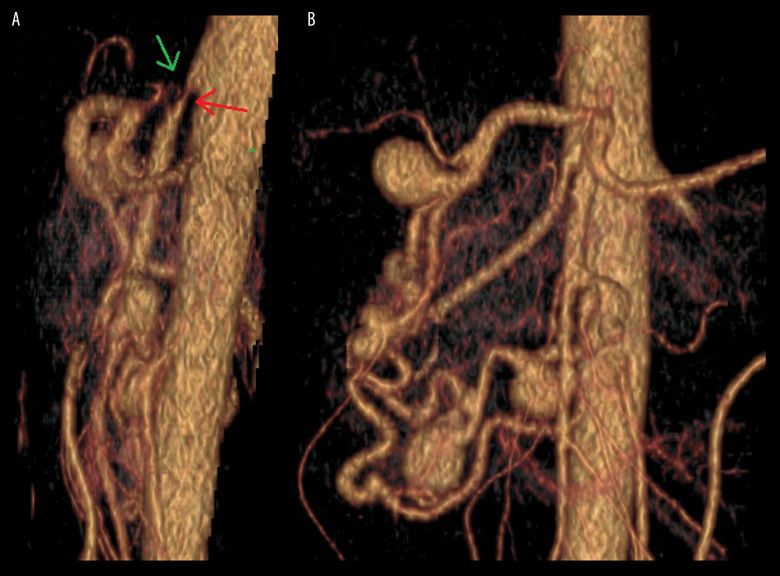
A 45-year-old woman with symptoms of chronic, recurrent, postprandial abdominal pain, nausea, and weight loss of approximately 15 kg in 1 year (from 65 to 50 kg and height of 180 cm) was admitted to our department. The patient described the pain as sharp and intense, exacerbated with meals, localized usually in the right upper quadrant (RUQ) and peri-umbilical area, and sometimes radiating to the suprapubic area. Her medical history was positive for hypertension and left inferior renal pole cysts. A computed tomography angiography (angio-CT) scan demonstrated complete occlusion of the celiac trunk, high origin of the superior mesenteric artery, and significant stenosis (assessed morphologically as 80–90%, with a significant >3.0 m/s increase of peak systolic velocity in Doppler ultrasound, Figure 1) caused by compression of the arteries in question by the median arcuate ligament and multiple aneurysms in the collateral circulation: 17-mm gastroduodenal artery aneurysm, 13-mm superior pancreatoduodenal artery aneurysm, and 11-mm aneurysm of the inferior pancreatoduodenal artery (Figure 2). No stenotic lesions were observed in the inferior mesenteric artery (IMA). Because only 1 of the 3 vessels supplying the visceral circulation was unchanged (IMA), the patient was qualified for surgical treatment. An endovascular approach was excluded at first because of the risk of potential failure, as the SMA stenosis was caused by the external compression, and therefore was inadequate for stent implantation (because of risk of fracture). Restoration of proper inflow to the visceral circulation can reduce the hyperkinetic collateral circulation, reducing the risk of aneurysm rupture. Therefore, the patient was qualified for open decompression of the splanchnic arteries accompanied by an aorto-hepatic vein graft as an initial step of treatment. From the transverse incision in the epigastric region, we exposed the aorta with the occluded celiac artery and hemodynamically significantly ste-nosed superior mesenteric artery branching from the anterior aortic wall. Initially, there was no palpable pulse on the distal part of the SMA. We performed surgical decompression of the medial arcuate ligament, which resulted in restoration of pulse in the superior mesenteric artery. Additionally, a 5-cm-long vein bypass graft harvested from the femoral part of the right great saphenous vein was implanted between the suprarenal aorta (superiorly to the coeliac artery, end-to-side anastomosis) and the common hepatic artery (end-to-side anastomosis), resulting in a palpable pulse in the common hepatic and splenic arteries. This bypass is shown in Figure 3. Following the surgery, the patient reported complete relief of the abdominal pain and nausea. The postoperative CT examination confirmed the patency and proper blood flow in the graft and superior mesenteric artery, but revealed aneurysmal remodelling – at least 5 small aneurysms (under 5 mm) and 2 aneurysms measuring 15 mm (enlargement of the 13-mm aneurysm of the superior pancreatoduodenal artery) and 13 mm (enlargement of the 11-mm aneurysm of the inferior pancreatoduodenal artery), respectively – in the arteries adjacent to the pancreatic head. Two endovascular aneurysm embolization procedures were performed within 4 months (at 1 month and 3.5 months after the surgery) as the second step of treatment. During the first procedure, the 2 aneurysms of the vessels branching from the gastroduodenal artery were embolized using 9 Concerto embolization coils (5×16 mm×40 cm, 2×16 mm×30 cm, 1×12 mm×30 cm, 1×14 mm×30 cm, and 1×8 mm×30 cm). Then, the 17-mm gastroduodenal artery aneurysm was embolized using 1 RUBY STANDARD 10×350 mm, and 4 CONCERTO embolization coils (8×300 mm, 6×200 mm, 2×5×200 mm), and the 13-mm pancreatoduodenal artery aneurysm was embolized with the use of RUBY STANDARD 12×600 mm, 8×400 mm and RUBY SOFT 8×600 mm, and 2×6×300 mm embolization coils. Both endovascular procedures were performed from the right femoral artery approach, and the femoral access site was closed with the Angioseal 6f and the Femoseal systems. The patient remained under direct supervision (48-month follow-up) undergoing angio-CT (Figure 4) and Doppler ultrasound at regular intervals, which confirmed patency of the graft, proper flow in the superior mesenteric artery, and visceral circulation following exclusion of the aneurysms. The patient denied having symptoms of Dunbar syndrome and she started to regain body weight, increasing it from 50 to 55 kg at 1 year after the surgery.
Figure 1.
Preoperative Doppler ultrasound showing significant stenosis of the superior mesenteric artery with >3 m/s increase in PSV and no flow in the celiac trunk.
Figure 2.
(A, B) 3D reconstruction of computed tomography angiography showing complete occlusion of the celiac artery (green arrow – A) and accompanying stenosis of the superior mesenteric artery (red arrow – A) caused by the median arcuate ligament, and multiple aneurysms in the collateral circulation: a 17-mm gastroduodenal artery aneurysm, a 13-mm superior pancreatoduodenal artery aneurysm, and an 11-mm aneurysm of the inferior pancreatoduodenal artery.
Figure 3.
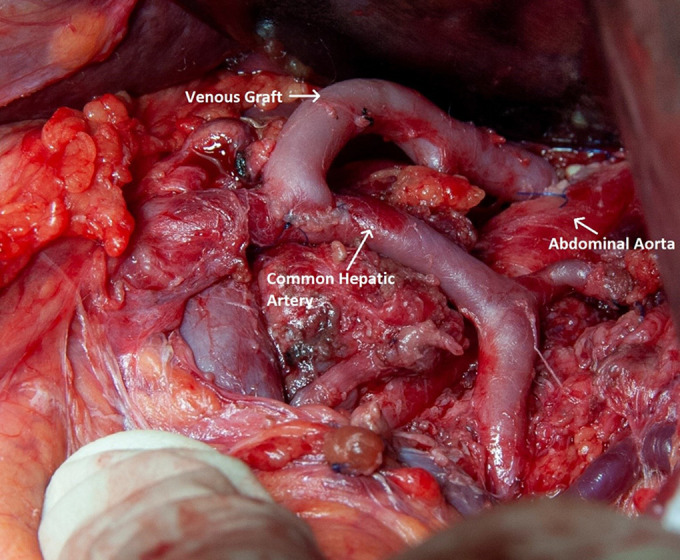
Intraoperative image of aorto-hepatic venous bypass between the aorta (superiorly to the coeliac artery, end-to-side anastomosis) and common hepatic artery (end-to-side anastomosis).
Figure 4.
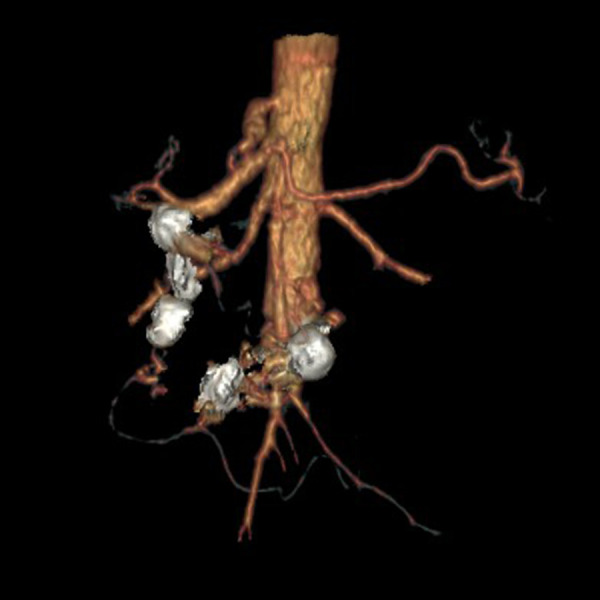
3D reconstruction of computed tomography angiography 48 months after treatment, showing patent aorto-hepatic graft, mesenteric arteries, and successfully embolized aneurysms.
Discussion
In 1965, Dunbar described surgical decompression of the celiac trunk in a group of 15 patients. Since this first publication, MALS has started to be recognised as a clinical condition [1,2].
Several authors, including Soman, Ilica, Gumus, Park, and Baskan, evaluated the incidence of celiac compression in asymptomatic individuals, finding radiological features of compression in 5.1%, 1.76%, 2.8%, 4%, and 4.6% of individuals, respectively. Furthermore, results in the literature suggest that up to 20% of the healthy population have features of external celiac compression [3–8].
Coeliac artery compression is 3–6 times more frequent in females in both symptomatic and asymptomatic patients. The morbidity peaks at 20–40 years old, but in some studies, the mean age of MALS symptoms occurrence is 50 years [7,8]. Our patient was 45 years old at the time of diagnosis, which is consistent with the epidemiological data described in the literature.
The typical triad of symptoms indicative of MALS is: postpran-dial abdominal pain, nausea or vomiting, and loss of weight. It is noteworthy that abdominal pain can be chronic, intermittent, or vague, and often radiates posteriorly or laterally. In differential diagnostics, other causes also should be taken into account – similar pain, but exacerbated by physical exercise, with relief of symptoms while leaning forward, is observed in athletes with renal arteries entrapment or compression [1,9].
The median arcuate ligament is a fibrous tissue joining the right and left crura of the diaphragm, usually at the level of the 12th thoracic vertebrae. It passes anteriorly to the aorta, forming the aortic hiatus, which contains the aorta, the azygos vein, and the thoracic duct. The celiac artery, which is the first major branch of the abdominal aorta, originates at the level of the 12th thoracic vertebrae. The relatively high origin of the celiac artery with low insertion of the diaphragm predisposes toward compression of the adjacent vascular structures, including the celiac artery and nervous structures, the celiac plexus containing celiac ganglia, and branches of the phrenic nerve [1,9,10].
The etiology of MALS remains unclear, but there are 2 main theories based on the compression of vascular and nervous structures. The sole vascular compression mechanism seems unlikely because the abundant collateral circulation via the mesenteric arteries provides adequate blood supply to organs of the digestive system. Moreover, in a vast percentage of asymptomatic individuals, features of celiac artery compression are observed [3–8,11]. However, a study conducted by Mensik et al., based on gastric tonometry, suggested that Dunbar syndrome symptoms can result from significant compression of the celiac trunk. Compression of the splanchnic plexus fibers, inner-vating sphincter muscles of the digestive tract, can alter the myoelectric activity of smooth muscles. Neurogenic-related pain can be caused either by splanchnic vasoconstriction or direct stimulation of pain neurons [12,13].
Aneurysms of visceral arteries are rarely encountered. Those of pancreaticoduodenal arteries were first described by Ferguson in 1895 [14]; most of them are pseudoaneurysms secondary to surgical procedures, pancreatitis, trauma, cholecystitis, or vasculitis [15–17]. True aneurysms of pancreaticoduodenal arteries account for only about 2% of all visceral aneurysms, and about 50% of these are associated with celiac axis occlusion or stenosis [18].
The visceral aneurysms coexisting with and caused by celiac axis lesions were first described in 1973 by Sutton and Lawton [19].
The compensatory increased blood flow in the collaterals connecting the celiac trunk and the superior mesenteric artery vascular beds, secondary to the celiac axis stenosis or occlusion, causes the blood vessels to enlarge and eventually causes the vessel wall to weaken, facilitating the formation of true aneurysms [15]. Arterial dilatation was also observed in patients with common hepatic artery occlusion [20]. Aneurysm formation in the visceral arteries due to increased blood flow was later reported by many authors, showing a 63–74% correlation between the prevalence of visceral aneurysms and celiac lesions [21]. Patten et al. reported that peripancreatic vascular network dilatation was observed in 80% of patients with celiac lesions [22]. Visceral aneurysms are mostly clinically “silent” and diagnosed incidentally. However, aneurysms of the pancreaticoduodenal arcade can present with symptoms of biliary ducts or bowel compression, such as vague abdominal pain, and, rarely, jaundice or gastrointestinal bleeding in case of rupture [15].
Because pancreaticoduodenal aneurysms carry a significant risk of rupture regardless of their size and are associated with relatively high mortality, early intervention is recommended [23].
The treatment options for visceral artery aneurysms include endovascular and open surgical methods. In patients with uncontrolled hypovolemic shock or failure using an endovascular approach, surgery is recommended [24]. Embolization of the inflow and outflow artery is an effective and less invasive method of treating splanchnic artery aneurysms. However, in case of pancreaticoduodenal artery aneurysms associated with celiac axis stenosis, ischemic damage to organs such as the liver or the pancreas can occur as a result of interruption of the collateral circulation after aneurysm embolization [23,24].
There is no consensus in the literature on the best treatment methods for use in patients with MALS and coexisting splanchnic artery aneurysms. Some authors prefer performing celiac revascularization first, stressing its role in preventing ischemia of abdominal cavity organs and reducing the risk of aneurysm recurrence. Others report satisfactory results using embolization only, without aneurysm recurrence or visceral ischemia [25].
In restoring physiological hemodynamics via arterial reconstruction, bypass, celiac angioplasty, or sectioning of the median arcuate ligament can reduce the risk of aneurysm formation [26]. Several authors reported regression of visceral aneurysms after celiac revascularization and restoration of physiologic blood flow conditions in the peripancreatic arcades [21,27,28]. It is also possible that restoration of proper inflow to the visceral circulation can cause transient elevation of blood pressure and blood volume in vascular beds, which perhaps was the cause of enlargement and de novo formation of small aneurysms in our patent. After considering possible options, open surgical repair was chosen as the first-line of treatment, and an aorto-hepatic bypass was successfully performed, resulting in the resolution of symptoms. The great saphenous vein has been reported to be safe and effective for use in aorto-hepatic bypass, and its use has been described in visceral ischemia [29,30]. Our department has experience with vein bypasses in this vascular area, which was why we chose this surgical technique. In the present patient, during 2 consecutive hospitalizations, endovascular coil embolization of visceral aneurysms was performed. In the 48-month follow-up period, there was no recurrence of symptoms and no de novo formation of aneurysms was observed.
Conclusions
Endovascular methods, which are less invasive and are associated with lower mortality and morbidity rates, should be the treatment of choice in patients with splanchnic artery aneurysms. However, in patients with multiple aneurysms secondary to MALS, arterial reconstruction should be considered prior to performing an endovascular procedure because of its potential role in prevention of malperfusion in case of embolization complications as well as its ability to help prevent de novo aneurysm formation.
Footnotes
Conflict of interests
None.
References:
- 1.Kim EN, Lamb K, Relles D, et al. Median arcuate ligament syndrome – review of this rare disease. JAMA Surg. 2016;151(5):471–77. doi: 10.1001/jamasurg.2016.0002. [DOI] [PubMed] [Google Scholar]
- 2.Dunbar JD, Molnar W, Beman FF, Marable SA. Compression of the celiac trunk and abdominal angina. Am J Roentgenol Radium Ther Nucl Med. 1965;95:731–44. doi: 10.2214/ajr.95.3.731. [DOI] [PubMed] [Google Scholar]
- 3.Soman S, Sudhakar SV, Keshava SN. Celiac axis compression by median arcuate ligament on computed tomography among asymptomatic persons. Indian J Gastroenterol. 2010;29(3):121–23. doi: 10.1007/s12664-010-0028-x. [DOI] [PubMed] [Google Scholar]
- 4.Ilica AT, Kocaoglu M, Bilici A, et al. Median arcuate ligament syndrome: Multidetector computed tomography findings. J Comput Assist Tomogr. 2007;31(5):728–31. doi: 10.1097/rct.0b013e318032e8c9. [DOI] [PubMed] [Google Scholar]
- 5.Gümüş H, Gümüş M, Tekbaş G, et al. Clinical and multidetector computed tomography findings of patients with median arcuate ligament syndrome. Clin Imaging. 2012;36(5):522–25. doi: 10.1016/j.clinimag.2011.11.031. [DOI] [PubMed] [Google Scholar]
- 6.Park CM, Chung JW, Kim HB, et al. Celiac axis stenosis: incidence and etiologies in asymptomatic individuals. Korean J Radiol. 2001;2(1):8–13. doi: 10.3348/kjr.2001.2.1.8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Baskan O, Kaya E, Gungoren FZ, Erol C. Compression of the celiac artery by the median arcuate ligament: multidetector computed tomography findings and characteristics. Can Assoc Radiol J. 2015;66(3):272–76. doi: 10.1016/j.carj.2015.01.001. [DOI] [PubMed] [Google Scholar]
- 8.Czihal M, Banafsche R, Hoffmann U, Koeppel T. Vascular compression syndromes. Vasa. 2015;44(6):419–34. doi: 10.1024/0301-1526/a000465. [DOI] [PubMed] [Google Scholar]
- 9.Gloviczki P, Duncan AA. Treatment of celiac artery compression syndrome: Does it really exist? Perspect Vasc Surg Endovasc Ther. 2007;19(3):259–63. doi: 10.1177/1531003507305263. [DOI] [PubMed] [Google Scholar]
- 10.Rongies-Kosmol M, Jakimowicz T. Celiac artery compression syndrome. Mini-review. Acta Angiol. 2015;21:1. : 21–24. [Google Scholar]
- 11.Levin DC, Baltaxe HA. High incidence of celiac axis narrowing in asymptomatic individuals. Am J Roentgenol Radium Ther Nucl Med. 1972;116:426–29. doi: 10.2214/ajr.116.2.426. [DOI] [PubMed] [Google Scholar]
- 12.Desmond CP, Roberts SK. Exercise-related abdominal pain as a manifestation of the median arcuate ligament syndrome. Scand J Gastroenterol. 2004;39:1310–13. doi: 10.1080/00365520410008150. [DOI] [PubMed] [Google Scholar]
- 13.Mensink PB, van Petersen AS, Kolkman JJ, et al. Gastric exercise tonometry: The key investigation in patients with suspected celiac artery compression syndrome. J Vasc Surg. 2006;44(2):277–81. doi: 10.1016/j.jvs.2006.03.038. [DOI] [PubMed] [Google Scholar]
- 14.Ferguson F. Aneurysm of superior pancreaticoduodenal artery. Proc NY Pathol Soc. 1895;24:45–49. [Google Scholar]
- 15.Kallamadi R, Demoya MA, Kalva SP. Inferior pancreaticoduodenal artery aneurysms in association with celiac stenosis/occlusion. Semin Intervent Radiol. 2009;26(3):215–23. doi: 10.1055/s-0029-1225671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Takeuchi H, Isobe Y, Hayashi M, et al. Ruptured pancreaticoduodenal artery aneurysm with acute gangrenous cholecystitis: A case report and review of the literature. Hepatogastroenterology. 2004;51(56):368–71. [PubMed] [Google Scholar]
- 17.Sato N, Yamaguchi K, Shimizu S, et al. Coil embolization of bleeding visceral pseudoaneurysms following pancreatectomy: The importance of early angiography. Arch Surg. 1998;133(10):1099–102. doi: 10.1001/archsurg.133.10.1099. [DOI] [PubMed] [Google Scholar]
- 18.Kalva SP, Athanasoulis CA, Greenfield AJ, et al. Inferior pancreaticoduodenal artery aneurysms in association with celiac axis stenosis or occlusion. Eur J Vasc Endovasc Surg. 2007;33(6):670–75. doi: 10.1016/j.ejvs.2006.12.021. [DOI] [PubMed] [Google Scholar]
- 19.Sutton D, Lawton G. Coeliac stenosis or occlusion with aneurysm of the collateral supply. Clin Radiol. 1973;24(1):49–53. doi: 10.1016/s0009-9260(73)80114-x. [DOI] [PubMed] [Google Scholar]
- 20.Porcellini M, Iaccarino V, Bernardo B, et al. Visceral artery aneurysms secondary to collateral circulation. Minerva Cardioangiol. 1996;44(9):443–45. [PubMed] [Google Scholar]
- 21.Ducasse E, Roy F, Chevalier J, et al. Aneurysm of the pancreaticoduodenal arteries with a celiac trunk lesion: Current management. J Vasc Surg. 2004;39:906–11. doi: 10.1016/j.jvs.2003.09.049. [DOI] [PubMed] [Google Scholar]
- 22.Patten RM, Coldwell DM, Ben-Menachem Y. Ligamentous compression of the celiac axis: CT findings in five patients. Am J Roentgenol. 1991;156:1101–3. doi: 10.2214/ajr.156.5.2017934. [DOI] [PubMed] [Google Scholar]
- 23.Corey MR, Ergul EA, Cambria RP, et al. The natural history of splanchnic artery aneurysms and outcomes after operative intervention. J Vasc Surg. 2016;63:949–57. doi: 10.1016/j.jvs.2015.10.066. [DOI] [PubMed] [Google Scholar]
- 24.Antoniak R, Grabowska-Derlatka L, Maciąg R, et al. Treatment algorithm of peripancreatic arteries aneurysm coexisting with coeliac artery lesion: Single institution experience. Biomed Res Int. 2018;2018:5745271. doi: 10.1155/2018/5745271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Boll JM, Sharp KW, Garrard CL, et al. Does management of true aneurysms of peripancreatic arteries require repair of associated celiac artery stenosis? J Am Coll Surg. 2017;224(2):199–203. doi: 10.1016/j.jamcollsurg.2016.10.030. [DOI] [PubMed] [Google Scholar]
- 26.Brocker JA, Maher JL, Smith RW. True pancreaticoduodenal aneurysms with celiac stenosis or occlusion. Am J Surg. 2012;204(5):762–68. doi: 10.1016/j.amjsurg.2012.03.001. [DOI] [PubMed] [Google Scholar]
- 27.Toriumi T, Shirasu T, Akai A, et al. Hemodynamic benefits of celiac artery release for ruptured right gastric artery aneurysm associated with median arcuate ligament syndrome: A case report. BMC Surg. 2017;17(1):116. doi: 10.1186/s12893-017-0320-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Proud G, Chamberlain J. Aneurysm formation on the small pancreatic arteries in association with celiac axis compression. Ann R Coll Surg Engl. 1978;60:294–97. [PMC free article] [PubMed] [Google Scholar]
- 29.Murakami Y, Toya N, Fukushima S, et al. Ascending aorta-common hepatic artery bypass for mesenteric revascularization. Int J Surg Case Rep. 2017;32:51–53. doi: 10.1016/j.ijscr.2017.02.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Chiche L, Kieffer E. Use of the ascending aorta as bypass inflow for treatment of chronic intestinal ischemia. J Vasc Surg. 2005;41(3):457–61. doi: 10.1016/j.jvs.2004.12.031. [DOI] [PubMed] [Google Scholar]