Abstract
Patient: Male, 76-year-old
Final Diagnosis: Digoxin toxicity • xanthopsia
Symptoms: Dyspnea • leg edema • xanthopsia
Medication:—
Clinical Procedure: Intravenous hydration
Specialty: Cardiology
Objective:
Unusual clinical course
Background:
Manifestations of digoxin toxicity vary, such as cardiac disturbances and gastrointestinal symptoms, and most are not specific to digoxin toxicity. We report a case of xanthopsia (yellow vision), a rare and relatively specific manifestation of digoxin toxicity, causing traffic accidents.
Case Report:
A 76-year-old man was admitted to our hospital for treatment of heart failure. He reported that his digoxin dose had been increased from 0.125 mg daily to 0.25 mg daily 3 weeks before admission. His serum digoxin level was 7.3 ng/mL (therapeutic range 0.8 to 2.0). Additional history-taking revealed that he had xanthopsia several days before admission and stopped riding a motorbike because of two traffic accidents. On ophthalmological examination, he had decreased responses on flash, cone, and 30-Hz flicker electroretinograms in both eyes without visual field impairment. Intravenous hydration was initiated and digoxin was withdrawn. Xanthopsia gradually improved along with the decline of serum digoxin levels and disappeared within a week. One month after admission, electroretinography findings were normal.
Conclusions:
Our case highlights the importance of acknowledging color vision deficiencies due to digoxin toxicity even in the modern era. This condition may increase risk of adverse events because affected patients are less likely to recognize color vision deficiencies.
MeSH Keywords: Accidents, Traffic; Diagnostic Techniques, Ophthalmological; Digoxin; Drug-Related Side Effects and Adverse Reactions
Background
Digoxin has long been widely prescribed for treatment of heart failure, but close attention should be paid to the drug’s toxicity due to its narrow therapeutic dose range [1,2]. Symptoms of digoxin toxicity vary, such as cardiac disturbances, gastrointestinal symptoms, and central nervous system issues [3], most of which are not specific to heart failure [2]. We report a case of xanthopsia (yellow vision), a rare and relatively specific manifestation of digoxin toxicity [4], which caused the patient to experience traffic accidents.
Case Report
A 76-year-old man was admitted to our hospital because of dyspnea and bilateral leg edema. The patient had been in his normal state of health until approximately 2 months before admission, when bilateral leg edema developed. A diagnosis of heart failure was made at another hospital and diuretics were prescribed. The man’s symptoms improved but recurred, and 3 weeks before admission, digoxin at a dose of 0.125 mg daily was added. The digoxin dosage was increased to 0.25 mg daily, but the patient’s symptoms persisted. He was transferred to our hospital for dyspnea. Review of systems was negative for nausea, vomiting, chest pains, back pains, dizziness, and loss of conscience.
The patient had hypertension, benign prostatic hyperplasia, and dementia. His medications included digoxin at a dose of 0.25 mg daily, furosemide at a dose of 20 mg daily, and spironolactone at a dose of 25 mg daily. He quit smoking 20 years earlier after a 37.5 pack-year history. The patient had been a binge drinker (approximately 4L of brandy, 40% ethanol, per month) and stopped drinking 1 year before admission. He never used illicit drugs and had no known allergies. There was no family history of cardiovascular diseases.
On examination, he was alert but disoriented. His height was 157 cm, weight 46.2 kg, and body mass index 18.7. His blood pressure was 130/46 mmHg, pulse 42 beats per minute, body temperature 36.7°C, respiratory rate 28 breaths per minute, and oxygen saturation 96% while breathing ambient air. The patient’s jugular venous pulse was high at 12 cm of water. Chest auscultation revealed a systolic ejection murmur (grade 3/6) and bibasilar lung crackles. His abdomen was soft and nondistended, and there was moderate edema of both lower legs.
Electrocardiography demonstrated atrial fibrillation with a heart rate of 40 to 50 beats per minute, and ST-segment depressions in leads I, II, aVF, and V3 to V6. Anteroposterior chest radiography revealed a cardiothoracic ratio of 59% with pulmonary congestion and a small amount of bilateral pleural effusion. As shown in the Table 1, the level of creatinine and estimated glomerular filtration rate were 1.6 mg/dL and 33.5 mL/min/1.73 m2 of body-surface area, respectively. The brain natriuretic peptide level was 681.1 pg/mL (reference value, ≤18.4) and the serum digoxin level was 7.3 ng/mL (therapeutic range 0.8 to 2.0). Neither ventricular dysfunction nor moderate or greater valvular heart disease was detected on echocardiography. A diagnosis of digoxin toxicity was made. Additional history-taking revealed that the patient had xanthopsia several days before admission. He stated that he had stopped riding a motorbike because he had experienced two traffic accidents (e.g., hitting a curb) within 1 week before admission while riding on a familiar road.
Table 1.
Laboratory data.
| Variable | Reference range | On admission | 3 days after admission | 1 week after admission |
|---|---|---|---|---|
| Urea nitrogen (mg/dL) | 8–20 | 32 | 17 | |
| Creatinine (mg/dL) | 0.45–0.81 | 1.60 | 1.04 | |
| eGFR (mL/min/1.73 m2) | ≥60 | 33.5 | 53.6 | |
| Brain natriuretic peptide (pg/mL) | ≤18.4 | 681.1 | 410.6 | |
| Serum digoxin (ng/mL) | 0.8–2.0 | 7.30 | 2.69 | 1.50 |
eGFR – estimated glomerular filtration rate.
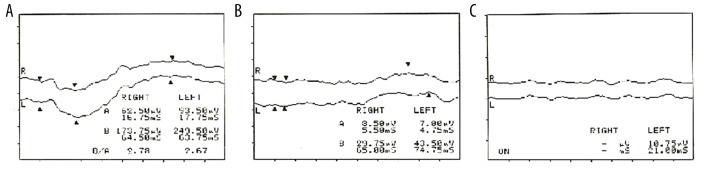
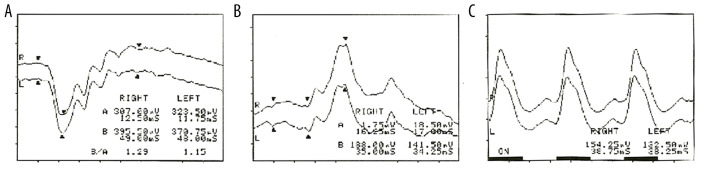
The man’s corrected visual acuity was 6/20 on the right side and 6/60 on the left side, in addition to abnormal electroretinography (Figure 1) without visual field impairment. No abnormalities were observed on optical coherence tomography; no fundus angiography was performed. Intravenous hydration was initiated and digoxin was withdrawn. Catecholamine was required for bradycardia, but no temporary pacing was placed. Xanthopsia and heart failure symptoms gradually improved, corresponding with the decline of serum digoxin levels (Table 1), and disappeared within a week, but the patient’s clinical course was complicated by aspiration pneumonia and delirium. One month after admission, electroretinography findings were normal (Figure 2), although the patient’s corrected visual acuity was still low (i.e., 6/12 on the right side and 6/20 on the left side). He was later transferred to a rehabilitation facility.
Figure 1.
Electroretinography on admission. Responses are decreased on flash (A), cone (B), and 30-Hz flicker (C) electroretinograms in the right and left eyes.
Figure 2.
Follow-up electroretinography. Responses on flash (A), cone (B), and 30-Hz flicker (C) are almost normal 1 month later.
Discussion
Digoxin was initiated in combination with diuretics and the dose was increased for the treatment of heart failure in this case. The patient had two traffic accidents while riding a motorbike on a familiar road and was later diagnosed with digoxin toxicity. Based on his clinical course, we considered digoxin toxicity to have caused xanthopsia, leading to the traffic accidents.
Incidence of hospitalization for digoxin toxicity has decreased over the years (e.g., more than 23% in 1970 [5] to 2% in the 1990s [6]), but the narrow therapeutic window of digoxin limits its clinical utility even in the modern era. Furthermore, digoxin toxicity can occur even in the normal range when accompanied by other conditions such as hypopotassemia, acidosis, hypothyroidism, and myocardial ischemia [2]. Clinical factors considered to increase risk of digoxin toxicity include older age, impaired renal function, low body weight, diuretic usage, and female gender [7,8], most of which were observed in our case. Accidental overdose as a result of dementia may also have affected the development of digoxin toxicity, such taking more than the prescribed dose, although this was not confirmed.
Of note, color vision deficiencies reportedly develop in approximately 80% of intoxicated patients who receive digoxin for at least 4 weeks as maintenance therapy, although only a few patients report the color disturbances [9]. Similarly, in our case, presence of ocular toxicity was highly suspected based on electroretinography, but the patient had not recognized the color vision deficiencies until asked. Ocular symptoms related to digoxin toxicity are xanthopsia, as observed in our case, chloropsia (green vision), photopsias, photophobia, and visual hallucinations, with or without decreased visual acuity [10–12]. All visual disturbances are likely to disappear days to weeks after digoxin discontinuation [13].
Digoxin-related xanthopsia has been acknowledged since its introduction by Withering more than 200 years ago [14] and has affected many people, such as Vincent van Gogh, the Dutch postimpressionist painter known for “high yellow palette” [4,15]. The retina is considered the main site of digoxin toxicity, as observed on electroretinography in our case. Digoxin inhibits membrane-bound alpha subunits of sodium-potassium ATPase, thereby promoting sodium-calcium exchange, leading to an intracellular calcium concentration that is available to contractile proteins [3]. Digoxin can also inhibit sodium-potassium ATPase in retinal Müller cells, photoreceptors, and pigment epithelium, and result in alteration of retinal electrical properties [16]. Although the precise mechanism is not fully understood, xanthopsia due to digoxin toxicity is likely associated with a selective effect on receptors of the retina [3].
Conclusions
Our case highlights the importance of acknowledging color vision deficiencies due to digoxin toxicity even in the modern era. This condition may increase risk of adverse events because affected patients are less likely to recognize color vision deficiencies.
References:
- 1.Yang EH, Shah S, Criley JM. Digitalis toxicity: A fading but crucial complication to recognize. Am J Med. 2012;125:337–43. doi: 10.1016/j.amjmed.2011.09.019. [DOI] [PubMed] [Google Scholar]
- 2.Kirilmaz B, Saygi S, Gungor H, et al. Digoxin intoxication: An old enemy in modern era. J Geriatr Cardiol. 2012;9:237–42. doi: 10.3724/SP.J.1263.2012.01101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Eichhorn EJ, Gheorghiade M. Digoxin. Prog Cardiovasc Dis. 2002;44:251–66. doi: 10.1053/pcad.2002.31591. [DOI] [PubMed] [Google Scholar]
- 4.Arnold WN, Loftus LS. Xanthopsia and van Gogh’s yellow palette. Eye (Lond) 1991;5:503–10. doi: 10.1038/eye.1991.93. [DOI] [PubMed] [Google Scholar]
- 5.Beller GA, Smith TW, Abelmann WH, et al. Digitalis intoxication. A prospective clinical study with serum level correlations. N Engl J Med. 1971;284:989–97. doi: 10.1056/NEJM197105062841801. [DOI] [PubMed] [Google Scholar]
- 6.Digitalis Investigation Group The effect of digoxin on mortality and morbidity in patients with heart failure. N Engl J Med. 1997;336:525–33. doi: 10.1056/NEJM199702203360801. [DOI] [PubMed] [Google Scholar]
- 7.Marik PE, Fromm L. A case series of hospitalized patients with elevated digoxin levels. Am J Med. 1998;105:110–15. doi: 10.1016/s0002-9343(98)00195-8. [DOI] [PubMed] [Google Scholar]
- 8.Aarnoudse AL, Dieleman JP, Stricker BH. Age- and gender-specific incidence of hospitalisation for digoxin intoxication. Drug Saf. 2007;30:431–36. doi: 10.2165/00002018-200730050-00006. [DOI] [PubMed] [Google Scholar]
- 9.Rietbrock N, Alken RG. Color vision deficiencies: A common sign of intoxication in chronically digoxin–treated patients. J Cardiovasc Pharmacol. 1980;2:93–99. [PubMed] [Google Scholar]
- 10.Lely AH, van Enter CH. Large-scale digitoxin intoxication. Br Med J. 1970;3:737–40. doi: 10.1136/bmj.3.5725.737. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Butler VP, Jr, Odel JG, Rath E, et al. Digitalis-induced visual disturbances with therapeutic serum digitalis concentrations. Ann Intern Med. 1995;123:676–80. doi: 10.7326/0003-4819-123-9-199511010-00006. [DOI] [PubMed] [Google Scholar]
- 12.Shi L, Sun LD, Odel JG. Colored floaters as a manifestation of digoxin toxicity. Am J Ophthalmol Case Rep. 2018;10:233–35. doi: 10.1016/j.ajoc.2018.02.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kim E, Fine HF, Ober MD. Retinal and uveal drug toxicity. Retinal Physician [serial online] 2008. Available from: https://www.retinalphysician.com/issues/2008/jan-feb/retinal-and-uveal-drug-toxicity.
- 14.Withering W. An account of the foxglove and some of its medical uses: With practical remarks on dropsy and other diseases. London, England: M Swinney for GGJ and J Robinson; 1785. p. 207. [Google Scholar]
- 15.Lee TC. Van Gogh’s vision. Digitalis intoxication? JAMA. 1981;245:727–29. [PubMed] [Google Scholar]
- 16.Burke JM, McKay BS. In vitro aging of bovine and human retinal pigment epithelium: Number and activity of the Na/K ATPase pump. Exp Eye Res. 1993;57:51–57. doi: 10.1006/exer.1993.1098. [DOI] [PubMed] [Google Scholar]