Abstract
Introduction
Smokers and nicotine users have a higher risk of femoral neck fracture non-union and prolonged time to fracture union. The impact of smoking resulting in revision surgery after fixation of femoral neck fractures, however, rarely has been studied. The aim of this retrospective study was to review if cigarette smoking had an influence on re-operation and revision after femoral neck fracture treatment.
Methods
Three groups of patients (Group 1: active smokers; Group 2: former smokers; and Group 3: non-smokers) who sustained a femoral neck fracture from January 2012 through August 2018 were included. Outcomes investigated included femoral neck fracture type, operative fixation type, fixation failure, and time interval between initial fixation and revision.
Results
A total of 1,452 subjects were identified (Group 1: 165 subjects; Group 2: 507 subjects; and Group 3: 780 subjects). In the male population, Groups 1 and 2 had higher rates of femoral neck fracture than Group 3. Twelve cases required revisions (Group 1: three cases (6%); Group 2: two cases (2%); Group 3: seven cases (4%)), with all but one revision within the first year following initial fixation. Group 1 patients tended to be younger than the other two groups.
Conclusion
Smoking has a positive association with the risk of femoral neck fracture amongst active and former male smokers. This study concluded that active smokers have a higher risk of non-union compared with non-smokers or former smokers. Smoking history, especially heavy or long-term, should play a role in deciding which fixation construct type to use for femoral neck fractures.
Keywords: smoking, femoral neck fracture, open fracture reduction, internal fracture fixation, cigarette
INTRODUCTION
Hip fracture is a worldwide health issue and is associated with substantial morbidity and mortality.1–3 Approximately 312,000 hip fractures occur in the United States yearly, and these numbers are predicted to increase in the coming decades.4–9 There are three hip fracture types, of which femoral neck fractures account for approximately half.10,11 Treatment of choice for hip fractures typically involves either closed or open reduction with internal fixation with either cannulated hip screws, a dynamic hip screw (DHS), cephalomedullary nail (CMN), or arthroplasty fixation with hemiarthroplasty (HA) or total hip arthroplasty (THA) depending on the morphology of the fracture.4,12–14 Patient factors, including, but not limited to, age, activity, comorbidities, functional demands, and the perceived risk of secondary surgery, also affect the treatment of choice for femoral neck fractures.4,15 Regardless of fixation method, studies have reported complication rates of up to 45%, including hardware complications, screw penetration, nonunion, and osteonecrosis of the femoral head.16–18 Several factors have been implicated, including age, gender, unhealthy lifestyle, alcohol use, previous fracture, and cigarette smoking.19–24
Cigarette smoking has been associated with many problems involving the musculoskeletal system. Previous studies have shown that smokers and nicotine users are more likely to have prolonged wound healing, higher risk of wound infection, higher incidence of fracture, higher incidence of nonunion of fracture, higher risk of malunion, prolonged time to fracture union, and increased risk of osteomyelitis following fracture.25–33 Kahlenberg and colleagues34 examined many risk factors associated with conversion from closed reduction with percutaneous pinning (CRPP) to arthroplasty. Their results found that smoking was not associated with revision of CRPP to HA or THA. The study, however, only investigated patients older than 65 years of age, neglecting a population likely more active, and more likely to be a smoker. Gardner and colleagues35 investigated failure of open reduction using sliding hip screws versus cannulated screws in patients younger than 60. This study, however, only looked at failure in the first six months following initial surgery and had only nine smokers in the study. The impact of smoking that results in re-operation and revision surgery after repair of femoral neck fractures, however, remains unclear, and there are limited studies that have evaluated or discussed this issue rigorously. The specific aim of this study was to review if there is an influence of cigarette smoking on re-operation and revision after femoral neck fracture treatment.
METHODS
Subjects
Institutional Review Board approval was obtained for the study. This study retrospectively reviewed clinical charts and radiographic studies of patients who sustained a femoral neck fracture. The inclusion criteria were confined to subjects who were older than 18 years and received treatment of femoral neck fracture from January 2012 to August 2018 from numerous hospitals within a selected single institute in the Midwest region. Subjects with a history of previous hip surgery, with pathological fractures (other than from osteoporosis), or with fractures involving either trochanter or extending beyond the intertrochanteric line were excluded from the study.
Study Groups
Pre- and post-operative hip radiographs (anteroposterior and lateral views) were reviewed and categorized by femoral neck fractures type, initial surgical treatment, and complication identification evaluation. The femoral neck fracture type was categorized with the Garden classification (Type I: non-displaced incomplete or valgus-impacted fracture; Type II: complete fracture without displacement of the fracture fragments; Type III: complete fracture with partial displacement of fracture fragments; Type IV: complete fracture with total displacement of the fracture fragments with femoral head able to rotate back to anatomic position). Three groups of subjects were compared: active smokers (Group 1), former smokers (Group 2), and non-smokers (Group 3). Group 1 included those that reported smoking use at the time of fracture and surgery, Group 2 included those that reported smoking use but had quit at least six months prior to fracture and surgery, and Group 3 included those that had no smoking history.
Variables
Clinical chart review was performed including documentation of age, gender, body mass index (BMI), surgical date, side of procedure, and smoking status. Radiographic study variables included the femoral neck fracture type, initial fixation method (CMN, DHS, cannulated hip screws, HA, or THA), and for cases of initial treatment failure undergoing revision, type of failure, type of revision, and time between initial treatment and revision were also recorded.
Statistical Analysis
A two-sample t-test was used to determine if there were any observed differences between groups regarding subject demographics (age and BMI). The Chi-square statistic was used to compare a distribution of gender for each group of surgical treatment of neck fracture. The Fisher’s exact test method was utilized to compare significant effects among different treating methods between the three groups. All statistical testing methods used were performed using IBM SPSS Statistics software (Version 24.0.0.0; SPSS Inc., Chicago, IL), and the statistically significant relationships were defined as those with a p value less than 0.05.
RESULTS
A total of 1,484 femoral neck fracture cases were identified, of which 32 cases were excluded due to not being able to identify the patient’s smoking status. Overall, there were 165 active smokers (91 females, 74 males), 506 former smokers (254 females, 252 males), and 780 non-smokers (586 females, 194 males; Table 1). The mean age and BMI were 79 ± 13 years (range: 19 – 104 years) and 25.2 ± 4.9 kg/m2 (range: 10.6 – 52.3 kg/m2), respectively. There was no statistical difference found between each group in BMI (p > 0.05), however, patients who were active smokers tended to be younger than patients who were former smokers or never smokers (p < 0.05; Table 1). In subjects less than 65 years old, the active smoker group had an elevated risk of femoral neck fracture than the former smoker group or the non-smoker group (43% vs. 9% vs. 10%, p < 0.0005; Table 2).
Table 1.
Patient demographics for each group.
| Variable | Group 1 (Active smoker) (N = 165) | Group 2 (Former smoker) (N = 506) | Group 3 (Non-smoker) (N = 780) | Overall (N = 1,452) | |
|---|---|---|---|---|---|
| Gender | Female | 91 (55%) | 254 (50%) | 586 (75%) | 931 (64%) |
| Male | 74 (45%) | 252 (50%) | 194 (25%) | 521 (36%) | |
| Age (year, mean ± SD) (range) | 66 ± 13 (29 – 94) | 79 ± 10 (38 – 102) | 81 ± 13 (19 – 104) | 79 ± 13 (19 – 104) | |
| Age < 65 years | 71 (43%) | 48 (9%) | 80 (10%) | 200 (14%) | |
| Age < 50 years | 16 (10%) | 6 (1%) | 25 (3%) | 47 (3%) | |
| BMI (kg/m2, mean ± SD) (range) | 24.3 ± 5.3 (14.7 – 40.8) | 25.6 ± 5.0 (14.8 – 48.4) | 25.1 ± 4.8 (10.6 – 52.3) | 25.2 ± 4.9 (10.6 – 52.3) | |
Table 2.
Initial fracture type and fixation construct type for each group.*
| Overall | Fracture type (Garden classification) | Fixation construct type** | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| ORIF | Arthroplasty | ||||||||||
| I | II | III | IV | Screws | DHS | CMN | HA | THA | |||
| Group 1 | Total | 165 | 23 (14%) | 46 (28%) | 57 (35%) | 39 (24%) | 43 (26%) | 4 (2%) | 6 (4%) | 55 (33%) | 57 (35%) |
| Age < 65 years | 71 (43%) | 11 (7%) | 19 (12%) | 22 (13%) | 19 (12%) | 26 (16%) | 1 (1%) | 2 (1%) | 9 (5%) | 33 (20%) | |
| Age < 50 years | 16 (10%) | 2 (1%) | 6 (4%) | 4 (2%) | 4 (2%) | 10 (6%) | 0 (0%) | 2 (1%) | 1 (1%) | 3 (2%) | |
| Group 2 | Total | 506 | 45 (9%) | 146 (29%) | 240 (47%) | 75 (15%) | 106 (21%) | 4 (1%) | 3 (0%) | 308 (61%) | 85 (17%) |
| Age < 65 years | 48 (9%) | 8 (2%) | 12 (2%) | 18 (4%) | 10 (2%) | 16 (3%) | 0 (0%) | 1 (0%) | 5 (1%) | 26 (5%) | |
| Age < 50 years | 6 (1%) | 2 (0%) | 1 (0%) | 3 (1%) | 0 (0%) | 4 (1%) | 0 (0%) | 1 (0%) | 0 (0%) | 1 (0%) | |
| Group 3 | Total | 780 | 51 (7%) | 246 (32%) | 272 (35%) | 211 (27%) | 146 (19%) | 13 (2%) | 10 (1%) | 506 (65%) | 105 (13%) |
| Age < 65 years | 80 (10%) | 6 (1%) | 34 (4%) | 19 (2%) | 21 (3%) | 35 (4%) | 7 (1%) | 1 (0%) | 9 (1%) | 28 (4%) | |
| Age < 50 years | 25 (3%) | 1 (0%) | 13 (2%) | 7 (1%) | 4 (1%) | 13 (2%) | 6 (1%) | 0 (0%) | 1 (0%) | 5 (1%) | |
The values are given as the number of cases (percent).
Screws: cannulated hip screws;
DHS: dynamic hip screw; CMN: cephalomedullary nail; HA: hemiarthroplasty; THA: total hip arthroplasty; ORIF: Open Reduction Internal Fixation
A higher rate of femoral neck fracture was found in females (64%) than males (36%), especially in the active smoker group (55%) and the non-smoker group (75%; Table 1). Within the male population, both active smokers (74 of 165 subjects; 45%) and former smokers (252 of 506 subjects; 50%) tended to have higher rates of femoral neck fracture compared to the non-smokers (194 of 780 subjects; 25%; p < 0.0005; Table 1).
A higher percentage (20%) of younger active smokers (less than 65 years of age) were treated with THA compared to the other groups (Group 2: 5%, Group 3: 4%; p < 0.0005; Table 2). Overall, a total of 335 cases were treated with open reduction internal fixation (ORIF) (Group 1: 53 cases, Group 2: 113 cases, Group 3: 169 cases), and only 12 cases (4%, 12 of 335 subjects) had re-operation and required revisions. Ten cases (3%) were revised due to nonunion, and two cases (1%) were revised due to hardware failure. Three of 53 cases (6%) in the active smokers group (Group 1) required revision. Two of these three cases were Type II fractures initially fixed with cannulated hip screws, and one was a Type IV fracture initially fixed with CMN (Table 3). Two of 113 cases (2%) in the former smoker group (Group 2) had initial failure fixation that required revision. Seven of 169 cases (4%) in the non-smoker group had initial failure fixation that required revision and one of these cases had the prominent hardware (Table 3). Statistically, no significant difference was found between each group in re-operation and revision in the ORIF groups (p > 0.05). Female patients for each group were observed to encounter in most revisions (67%; Table 3).
Table 3.
Cases of initial open reduction internal fixation failure for each group.
| Initial fracture type (Garden classification) | |||||||
|---|---|---|---|---|---|---|---|
| I | II | III | IV | Total | |||
| Group 1 (Active smoker) | Screws | Cases | 18 | 21 | 3 | 1 | 43 |
| Revision | 0 | 2 | 0 | 0 | 2 | ||
| Revision days (sex) | 63 (F) 292 (M) |
||||||
| DHS | Cases | 1 | 1 | 2 | 0 | 4 | |
| Revision | 0 | 0 | 0 | 0 | 0 | ||
| Revision days (sex) | |||||||
| CMN | Cases | 1 | 1 | 2 | 2 | 6 | |
| Revision | 0 | 0 | 0 | 1 | 1 | ||
| Revision days (sex) | 93 (F) | ||||||
| Group 2 (Former smoker) | Screws | Cases | 29 | 69 | 8 | 0 | 106 |
| Revision | 0 | 1 | 0 | 0 | 1 | ||
| Revision days (sex) | 30 (F) | ||||||
| DHS | Cases | 1 | 2 | 1 | 0 | 4 | |
| Revision | 0 | 0 | 1 | 0 | 1 | ||
| Revision days (sex) | 364 (F) | ||||||
| CMN | Cases | 1 | 1 | 1 | 0 | 3 | |
| Revision | 0 | 0 | 0 | 0 | 0 | ||
| Revision days (sex) | |||||||
| Group 3 (Non-smoker) | Screws | Cases | 40 | 101 | 4 | 1 | 146 |
| Revision | 1 | 4 | 0 | 1 | 6 | ||
| Revision days (sex) | 23 (M) | 20 (F) 101 (F) 67 (M) 42 (M) |
70 (F) | ||||
| DHS | Cases | 3 | 6 | 2 | 2 | 13 | |
| Revision | 0 | 0 | 0 | 0 | 0 | ||
| Revision days (sex) | |||||||
| CMN | Cases | 1 | 4 | 5 | 0 | 10 | |
| Revision | 0 | 0 | 1 (20%) | 0 | 1 (10%) | ||
| Revision days (sex) | 390 (F) | ||||||
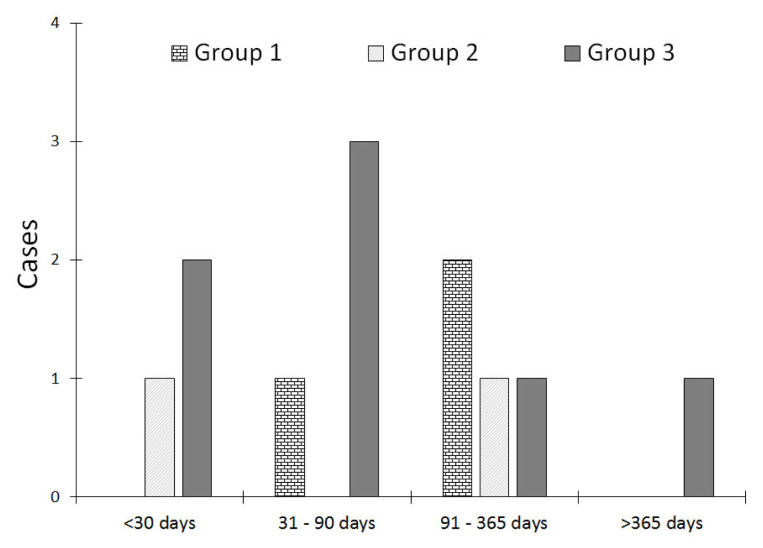
All fractures of each group had different time intervals between the fracture and revision. Most revisions (92%) occurred within one year of initial fixation (Figure 1). Only one case in Group 3 (63-year-old female) that sustained a Type III fracture initially fixed with a CMN was revised 390 days post-operatively to a THA due to non-union (Table 3).
Figure 1.
Time intervals (days) between initial femoral neck fracture fixation and revision.
DISCUSSION
Cigarette smoking is a significant public health problem in the United States, and has been shown to increase the risk for hip osteoporotic fractures,19,23,36,37 and have a negative impact on surgical outcome and complication rates.27,28,38–42 The results of this study indicated that cigarette smoking has a positive influence on re-operation and revision after femoral neck fracture treatment. This is especially apparent amongst the active and former male smokers who had 20% to 25% higher risk of sustaining a femoral neck fracture compared with those who had never smoked. This is consistent with previous studies and recently published meta-analyses.19,23,36,37,43 One possible reason for this is that smoking may reduce bone mass by changing the proliferation of bone cells, specifically osteoblasts and osteoclasts.44–46 Calcium is a major factor for maintaining bone health, and smoking may influence and impair the absorption of calcium and resultant metabolism of bone.44,46
This study found that femoral neck fractures occurred more commonly in younger patients (< 65 or < 50 years of age) who were active smokers compared to those who were former smokers or nonsmokers; likely a reflection of the bone mass reduction associated with smoking. Several meta-analyses have demonstrated cigarette smoking leading to bone mass loss,47,48 and previous studies have demonstrated unfavorable effects of smoking on bone density and geometry in young men.49–51 Other studies have shown that the negative effects of smoking on bone mass, including lower bone density and thinner bone cortex, amongst young adults would only be expected for individuals with greater tobacco intake.52–55
This study evaluated the impact of smoking resulting in revision surgery after fixation of femoral neck fractures, and the results of this study have demonstrated an increased risk of non-union in active smokers. A higher percentage of younger active smoker patients (age < 65 years) were fixed with arthroplasty (either HA or THA). Treatment for displaced femoral neck fractures involving an arthroplasty procedure typically is viewed as less favorable for younger patients as they face greater physical demands over a longer period following a surgical procedure compared with older, less active patients. Additionally, revision THA in this population is fraught with complications, and each additional procedure carries increased risk and worsening outcomes. Currently, no literature supports basing femoral neck fracture treatment decision-making on smoking status; however, many of the young active smokers in this study struggled with osteonecrosis, poorer bone quality, existing degenerative or inflammatory arthritis; all of which are suspected to be due to smoking. Thus, combination of age and smoking history should play an indirect role in deciding which fixation construct type to use for femoral neck fractures.
It is postulated that only those patients without smoking-associated severe bone mass reduction were fixed with cannulated hip screws, a dynamic hip screw, and cephalomedullary nail. Only 4% (Group 1: 1%, Group 2: 1%, and Group 3: 2%) of all these fixation types for femoral neck fracture were revised to HA or THA, with non-union being the predominant reason for revision. This is a much lower revision rate than previously reported.8,34,56 Kahlenberg et al.34 and Kain et al.56 found that approximately 10% of patients with closed reduction with percutaneous pinning for the femoral neck fracture required conversion to hip arthroplasty.
The preferred operative treatment choice for femoral neck fractures is to allow early patient mobilization to decrease the risk for complications and improve patient outcomes. Three cannulated hip screw fixation is a widely accepted surgical treatment for valgus-impacted and non-displaced femoral neck fractures (Garden Type I and II fractures),12 however, the results of this study indicated that there was a trend toward higher re-operation rates in active smokers with Garden Type II fractures, but no statistically significant differences were found. As such, using a cannulated hip screw construct for femoral neck fixation in patients, especially active smokers with complete, nondisplaced fractures, should be used with caution. The other concerning fixation method in active smokers is the use of a cephalomedullary nail. Although only a few cephalomedullary nails were used in this study, half of those implanted for completely displaced femoral neck fractures required revision. While there is insufficient evidence to discourage the use of cephalomedullary nails in instances such as these, this construct should be used cautiously until more evidence is available to support the use of this implant for Type IV femoral neck fractures in smokers.
Previous studies34,56 have investigated the time between initial fracture fixation surgery and revision surgery and demonstrated an approximate average of 9 to 10 months. The findings in the present study corroborated these findings. The majority of revision surgeries in our study were less than one year post-operatively, except one case in which the revision occurred 390 days post-operatively. There is no pattern of when revision surgery was pursued in any of our study groups.
This study had certain limitations. The most significant limitation was the retrospective review nature with limited data (six years in a single health system). Due to lack of randomization or blinding, there is potential for selection and/or observation bias that may underestimate the impact smoking status may have on treatment choice for femoral neck fracture. Another limitation was that the patients who received open reduction internal fixation for femoral neck fracture may have undergone revision surgery outside our institution later than 12 months postoperatively, which would not have been registered in this study, and subsequently contributing to lack of long term follow-up data and fewer numbers of recorded revisions. This prevented application of tests of significance and reduced the ability to evaluate the correlation quantitatively. Last, this study did not evaluate the adequacy of anatomic reduction following surgical intervention, nor the time between fracture and surgical intervention, each of which may have played a role in the need for eventual revision. Despite these limitations, the implications of this study served an important role in supporting previous studies and adding to the literature regarding fixation constructs for femoral neck fractures, especially for smokers to best avoid the risk of necessary revision. Further research utilizing a larger study population is needed, and surgeons should encourage active smoker patients to quit, not only to reduce the risk of revision but also to increase bone healing.
CONCLUSION
In summary, the overall findings of this study tended to show that cigarette smoking had a positive influence on re-operation and revision surgery after femoral neck fracture treatment especially amongst active and former male smokers. Active smokers tended to have a higher risk of re-operation that required revision compared with non-smokers or former smokers. Smoking history, especially heavy or long-term, should be considered when deciding which type of fixation construct to use for femoral neck fractures.
ACKNOWLEDGEMENTS
The authors acknowledge the Enterprise Data and Analytics team from Sanford Health for their support on retrieving data from our institute. The authors wish to thank Dr. Todd Sekundiak for his assistance, revision, and critical comments on the paper.
REFERENCES
- 1.Lee YK, Lee YJ, Ha YC, Koo KH. Five-year relative survival of patients with osteoporotic hip fracture. J Clin Endocrinol Metab. 2014;99(1):97–100. doi: 10.1210/jc.2013-2352. [DOI] [PubMed] [Google Scholar]
- 2.Orces CH. In-hospital hip fracture mortality trends in older adults: The National Hospital Discharge Survey, 1988–2007. J Am Geriatr Soc. 2013;61(12):2248–2249. doi: 10.1111/jgs.12567. [DOI] [PubMed] [Google Scholar]
- 3.Kim SM, Moon YW, Lim SJ, et al. Prediction of survival, second fracture, and functional recovery following the first hip fracture surgery in elderly patients. Bone. 2012;50(6):1343–1350. doi: 10.1016/j.bone.2012.02.633. [DOI] [PubMed] [Google Scholar]
- 4.Gjertsen JE, Fevang JM, Matre K, Vinje T, Engesaeter LB. Clinical outcome after undisplaced femoral neck fractures. Acta Orthop. 2011;82(3):268–274. doi: 10.3109/17453674.2011.588857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Burge R, Dawson-Hughes B, Solomon DH, Wong JB, King A, Tosteson A. Incidence and economic burden of osteoporosis-related fractures in the United States, 2005–2025. J Bone Miner Res. 2007;22(3):465–475. doi: 10.1359/jbmr.061113. [DOI] [PubMed] [Google Scholar]
- 6.Johnell O, Kanis JA. An estimate of the worldwide prevalence and disability associated with osteoporotic fractures. Osteoporos Int. 2006;17(12):1726–1733. doi: 10.1007/s00198-006-0172-4. [DOI] [PubMed] [Google Scholar]
- 7.Healy WL, Iorio R. Total hip arthroplasty: Optimal treatment for displaced femoral neck fractures in elderly patients. Clin Orthop Relat Res. 2004;(429):43–48. [PubMed] [Google Scholar]
- 8.Eisler J, Cornwall R, Strauss E, Koval K, Siu A, Gilbert M. Outcomes of elderly patients with nondisplaced femoral neck fractures. Clin Orthop Relat Res. 2002;(399):52–58. doi: 10.1097/00003086-200206000-00008. [DOI] [PubMed] [Google Scholar]
- 9.Gullberg B, Johnell O, Kanis JA. World-wide projections for hip fracture. Osteoporos Int. 1997;7(5):407–413. doi: 10.1007/pl00004148. [DOI] [PubMed] [Google Scholar]
- 10.Murphy DK, Randell T, Brennan KL, Probe RA, Brennan ML. Treatment and displacement affect the reoperation rate for femoral neck fracture. Clin Orthop Relat Res. 2013;471(8):2691–2702. doi: 10.1007/s11999-013-3020-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Keating J. Femoral neck fractures. In: Bucholz RW, Heckman JD, Court-Brown CM, Tornetta P, editors. Rockwood and Green’s Fractures in Adults. Philadelphia: Lippincott Williams & Wilkins; 2010. pp. 1561–1596. [Google Scholar]
- 12.Florschutz AV, Langford JR, Haidukewych GJ, Koval KJ. Femoral neck fractures: Current management. J Orthop Trauma. 2015;29(3):121–129. doi: 10.1097/BOT.0000000000000291. [DOI] [PubMed] [Google Scholar]
- 13.Gao H, Liu Z, Xing D, Gong M. Which is the best alternative for displaced femoral neck fractures in the elderly? A meta-analysis. Clin Orthop Relat Res. 2012;470(6):1782–1791. doi: 10.1007/s11999-012-2250-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Souder CD, Brennan ML, Brennan KL, Song J, Williams J, Chaput C. The rate of contralateral proximal femoral fracture following closed reduction and percutaneous pinning compared with arthroplasty for the treatment of femoral neck fractures. J Bone Joint Surg Am. 2012;94(5):418–425. doi: 10.2106/JBJS.J.01134. [DOI] [PubMed] [Google Scholar]
- 15.Gjertsen JE, Vinje T, Engesaeter LB, et al. Internal screw fixation compared with bipolar hemiarthroplasty for treatment of displaced femoral neck fractures in elderly patients. J Bone Joint Surg Am. 2010;92(3):619–628. doi: 10.2106/JBJS.H.01750. [DOI] [PubMed] [Google Scholar]
- 16.Davidovitch RI, Jordan CJ, Egol KA, Vrahas MS. Challenges in the treatment of femoral neck fractures in the nonelderly adult. J Trauma. 2010;68(1):236–242. doi: 10.1097/TA.0b013e3181c428ce. [DOI] [PubMed] [Google Scholar]
- 17.Bhandari M, Tornetta P, 3rd, Hanson B, Swiontkowski MF. Optimal internal fixation for femoral neck fractures: Multiple screws or sliding hip screws? J Orthop Trauma. 2009;23(6):403–407. doi: 10.1097/BOT.0b013e318176191f. [DOI] [PubMed] [Google Scholar]
- 18.Lu-Yao GL, Keller RB, Littenberg B, Wennberg JE. Outcomes after displaced fractures of the femoral neck. A meta-analysis of one hundred and six published reports. J Bone Joint Surg Am. 1994;76(1):15–25. doi: 10.2106/00004623-199401000-00003. [DOI] [PubMed] [Google Scholar]
- 19.Shen GS, Li Y, Zhao G, et al. Cigarette smoking and risk of hip fracture in women: A meta-analysis of prospective cohort studies. Injury. 2015;46(7):1333–1340. doi: 10.1016/j.injury.2015.04.008. [DOI] [PubMed] [Google Scholar]
- 20.LeBlanc KE, Muncie HL, Jr, LeBlanc LL. Hip fracture: Diagnosis, treatment, and secondary prevention. Am Fam Physician. 2014;89(12):945–951. [PubMed] [Google Scholar]
- 21.Poh KS, Lingaraj K. Complications and their risk factors following hip fracture surgery. J Orthop Surg (Hong Kong) 2013;21(2):154–157. doi: 10.1177/230949901302100207. [DOI] [PubMed] [Google Scholar]
- 22.Thorin MH, Wihlborg A, Åkesson K, Gerdhem P. Smoking, smoking cessation, and fracture risk in elderly women followed for 10 years. Osteoporos Int. 2016;27(1):249–255. doi: 10.1007/s00198-015-3290-z. [DOI] [PubMed] [Google Scholar]
- 23.Wu ZJ, Zhao P, Liu B, Yuan ZC. Effect of cigarette smoking on risk of hip fracture in men: A meta-analysis of 14 prospective cohort studies. PLoS One. 2016;11(12):e0168990. doi: 10.1371/journal.pone.0168990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Cornuz J, Feskanich D, Willett WC, Colditz GA. Smoking, smoking cessation, and risk of hip fracture in women. Am J Med. 1999;106(3):311–314. doi: 10.1016/s0002-9343(99)00022-4. [DOI] [PubMed] [Google Scholar]
- 25.Kim JH, Patel S. Is it worth discriminating against patients who smoke? A systematic literature review on the effects of tobacco use in foot and ankle surgery. J Foot Ankle Surg. 2017;56(3):594–599. doi: 10.1053/j.jfas.2017.02.006. [DOI] [PubMed] [Google Scholar]
- 26.Pearson RG, Clement RG, Edwards KL, Scammell BE. Do smokers have greater risk of delayed and non-union after fracture, osteotomy and arthrodesis? A systematic review with meta-analysis. BMJ Open. 2016;6(11):e010303. doi: 10.1136/bmjopen-2015-010303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Nåsell H, Ottosson C, Törnqvist H, Lindé J, Ponzer S. The impact of smoking on complications after operatively treated ankle fractures--a follow-up study of 906 patients. J Orthop Trauma. 2011;25(12):748–755. doi: 10.1097/BOT.0b013e318213f217. [DOI] [PubMed] [Google Scholar]
- 28.Sloan A, Hussain I, Maqsood M, Eremin O, El-Sheemy M. The effects of smoking on fracture healing. Surgeon. 2010;8(2):111–116. doi: 10.1016/j.surge.2009.10.014. [DOI] [PubMed] [Google Scholar]
- 29.Gaston MS, Simpson AH. Inhibition of fracture healing. J Bone Joint Surg Br. 2007;89(12):1553–1560. doi: 10.1302/0301-620X.89B12.19671. [DOI] [PubMed] [Google Scholar]
- 30.Krannitz KW, Fong HW, Fallat LM, Kish J. The effect of cigarette smoking on radiographic bone healing after elective foot surgery. J Foot Ankle Surg. 2009;48(5):525–527. doi: 10.1053/j.jfas.2009.04.008. [DOI] [PubMed] [Google Scholar]
- 31.Harvey EJ, Agel J, Selznick HS, Chapman JR, Henley MB. Deleterious effect of smoking on healing of open tibia-shaft fractures. Am J Orthop (Belle Mead NJ) 2002;31(9):518–521. [PubMed] [Google Scholar]
- 32.Adams CI, Keating JF, Court-Brown CM. Cigarette smoking and open tibial fractures. Injury. 2001;32(1):61–65. doi: 10.1016/s0020-1383(00)00121-2. [DOI] [PubMed] [Google Scholar]
- 33.Porter SE, Hanley EN. The musculoskeletal effects of smoking. J Am Acad Orthop Surg. 2001;9(1):9–17. doi: 10.5435/00124635-200101000-00002. [DOI] [PubMed] [Google Scholar]
- 34.Kahlenberg CA, Richardson SS, Schairer WW, Cross MB. Rates and risk factors of conversion hip arthroplasty after closed reduction percutaneous hip pinning for femoral neck fractures-a population analysis. J Arthroplasty. 2018;33(3):771–776. doi: 10.1016/j.arth.2017.10.004. [DOI] [PubMed] [Google Scholar]
- 35.Gardner S, Weaver MJ, Jerabek S, Rodriguez E, Vrahas M, Harris M. Predictors of early failure in young patients with displaced femoral neck fractures. J Orthop. 2014;12(2):75–80. doi: 10.1016/j.jor.2014.01.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Kanis JA, Johnell O, Oden A, et al. Smoking and fracture risk: A meta-analysis. Osteoporos Int. 2005;16(2):155–162. doi: 10.1007/s00198-004-1640-3. [DOI] [PubMed] [Google Scholar]
- 37.Høidrup S, Prescott E, Sørensen TI, et al. Tobacco smoking and risk of hip fracture in men and women. Int J Epidemiol. 2000;29(2):253–259. doi: 10.1093/ije/29.2.253. [DOI] [PubMed] [Google Scholar]
- 38.Guo S, Dipietro LA. Factors affecting wound healing. J Dent Res. 2010;89(3):219–229. doi: 10.1177/0022034509359125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Castillo RC, Bosse MJ, MacKenzie EJ, Patterson BM LEAP Study Group. Impact of smoking on fracture healing and risk of complications in limb-threatening open tibia fractures. J Orthop Trauma. 2005;19(3):151–157. doi: 10.1097/00005131-200503000-00001. [DOI] [PubMed] [Google Scholar]
- 40.Manassa EH, Hertl CH, Olbrisch RR. Wound healing problems in smokers and nonsmokers after 132 abdominoplasties. Plast Reconstr Surg. 2003;111(6):2082–2087. doi: 10.1097/01.PRS.0000057144.62727.C8. discussion 2088–2089. [DOI] [PubMed] [Google Scholar]
- 41.Møller AM, Pedersen T, Villebro N, Munksgaard A. Effect of smoking on early complications after elective orthopaedic surgery. J Bone Joint Surg Br. 2003;85(2):178–181. doi: 10.1302/0301-620x.85b2.13717. [DOI] [PubMed] [Google Scholar]
- 42.Møller AM, Villebro N, Pedersen T, Tønnesen H. Effect of preoperative smoking intervention on postoperative complications: A randomised clinical trial. Lancet. 2002;359(9301):114–117. doi: 10.1016/S0140-6736(02)07369-5. [DOI] [PubMed] [Google Scholar]
- 43.Olofsson H, Byberg L, Mohsen R, Melhus H, Lithell H, Michaëlsson K. Smoking and the risk of fracture in older men. J Bone Miner Res. 2005;20(7):1208–1215. doi: 10.1359/JBMR.050208. [DOI] [PubMed] [Google Scholar]
- 44.Wang D, Chen XH, Fu G, et al. Calcium intake and hip fracture risk: A meta-analysis of prospective cohort studies. Int J Clin Exp Med. 2015;8(8):14424–14431. [PMC free article] [PubMed] [Google Scholar]
- 45.Lutfy K, Aimiuwu O, Mangubat M, et al. Nicotine stimulates secretion of corticosterone via both CRH and AVP receptors. J Neurochem. 2012;120(6):1108–1116. doi: 10.1111/j.1471-4159.2011.07633.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Jones G, Scott FS. A cross-sectional study of smoking and bone mineral density in premenopausal parous women: Effect of body mass index, breastfeeding, and sports participation. J Bone Miner Res. 1999;14(9):1628–1633. doi: 10.1359/jbmr.1999.14.9.1628. [DOI] [PubMed] [Google Scholar]
- 47.Ward KD, Klesges RC. A meta-analysis of the effects of cigarette smoking on bone mineral density. Calcif Tissue Int. 2001 May;68(5):259–70. doi: 10.1007/bf02390832. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Law MR, Hackshaw AK. A meta-analysis of cigarette smoking, bone mineral density and risk of hip fracture: Recognition of a major effect. BMJ. 1997;315(7112):841–846. doi: 10.1136/bmj.315.7112.841. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Taes Y, Lapauw B, Vanbillemont G, et al. Early smoking is associated with peak bone mass and prevalent fractures in young, healthy men. J Bone Miner Res. 2010;25(2):379–387. doi: 10.1359/jbmr.090809. [DOI] [PubMed] [Google Scholar]
- 50.Szulc P, Garnero P, Claustrat B, Marchand F, Duboeuf F, Delmas PD. Increased bone resorption in moderate smokers with low body weight: The Minos study. J Clin Endocrinol Metab. 2002;87(2):666–674. doi: 10.1210/jcem.87.2.8232. [DOI] [PubMed] [Google Scholar]
- 51.Pompe E, Bartstra J, Verhaar HJ, et al. Bone density loss on computed tomography at 3-year follow-up in current compared to former male smokers. Eur J Radiol. 2017;89:177–181. doi: 10.1016/j.ejrad.2017.02.011. [DOI] [PubMed] [Google Scholar]
- 52.Välimäki MJ, Kärkkäinen M, Lamberg-Allardt C, et al. Exercise, smoking, and calcium intake during adolescence and early adulthood as determinants of peak bone mass. Cardiovascular Risk in Young Finns Study Group. BMJ. 1994;309(6949):230–235. doi: 10.1136/bmj.309.6949.230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Ortego-Centeno N, Muñoz-Torres M, Jódar E, Hernández-Quero J, Jurado-Duce A, de la Higuera Torres-Puchol J. Effect of tobacco consumption on bone mineral density in healthy young males. Calcif Tissue Int. 1997;60(6):496–500. doi: 10.1007/s002239900270. [DOI] [PubMed] [Google Scholar]
- 54.Kuo CW, Chang TH, Chi WL, Chu TC. Effect of cigarette smoking on bone mineral density in healthy Taiwanese middle-aged men. J Clin Densitom. 2008;11(4):518–524. doi: 10.1016/j.jocd.2008.07.005. [DOI] [PubMed] [Google Scholar]
- 55.Szulc P, Garnero P, Claustrat B, Marchand F, Duboeuf F, Delmas PD. Increased bone resorption in moderate smokers with low body weight: the Minos study. J Clin Endocrinol Metab. 2002;87(2):666–674. doi: 10.1210/jcem.87.2.8232. [DOI] [PubMed] [Google Scholar]
- 56.Kain MS, Marcantonio AJ, Iorio R. Revision surgery occurs frequently after percutaneous fixation of stable femoral neck fractures in elderly patients. Clin Orthop Relat Res. 2014;472(12):4010–4014. doi: 10.1007/s11999-014-3957-3. [DOI] [PMC free article] [PubMed] [Google Scholar]