Abstract
OBJECTIVE
According to recent guidelines, individuals with type 1 diabetes should spend <4.0% of time per day with glucose levels <3.9 mmol/L (<70 mg/dL) and <1.0% per day with glucose levels <3.0 mmol/L (<54 mg/dL).
RESEARCH DESIGN AND METHODS
In the GOLD randomized crossover trial, 161 individuals with type 1 diabetes treated with multiple daily insulin injections (MDI) were randomized to continuous glucose monitoring (CGM) or conventional therapy with self-monitoring of blood glucose (SMBG) and evaluated over 16 months. We estimated the association between time spent in hypoglycemia and various mean glucose and HbA1c levels.
RESULTS
Time spent in hypoglycemia (<3.9 mmol/L and <3.0 mmol/L) increased significantly with lower mean HbA1c and mean glucose levels during both CGM and conventional therapy. During CGM, 24 (57.1%) individuals with HbA1c <7.5% (<58 mmol/mol) had <1.0% time spent in hypoglycemia <3.0 mmol/L and 23 (54.8%) had <4.0% time spent in hypoglycemia <3.9 mmol/L. During CGM, mean time spent in hypoglycemia for individuals with mean HbA1c 7.0% (52 mmol/mol) was estimated to be 5.4% for <3.9 mmol/L and 1.5% for <3.0 mmol/L. The corresponding values during SMBG were 9.2% and 3.5%, respectively. Individuals with mean glucose levels of 8 mmol/L spent 4.9% units more time with glucose levels <3.9 mmol/L and 2.8% units more time <3.0 mmol/L during SMBG compared with CGM.
CONCLUSIONS
Reaching current targets for time in hypoglycemia while at the same time reaching HbA1c targets is challenging for patients with type 1 diabetes treated with MDI both with CGM and SMBG monitoring. However, CGM is associated with considerably less time in hypoglycemia than SMBG at a broad range of HbA1c levels and is crucial for patients with MDI treatment if they are to have a chance to approach hypoglycemia targets.
Introduction
Intensive insulin therapy resulting in more frequently achieving glycemic targets delays the onset and slows the progression of diabetes-related complications in individuals with type 1 diabetes (1,2). One of the main obstacles related to insulin therapy is hypoglycemia, a complication associated with neurocognitive dysfunction and behavioral impairment over time (3).
For many years, conventional therapy with regular capillary self-monitoring of blood glucose (SMBG) has been crucial for diabetes management. However, SMBG only provides single point-in-time measurements and, therefore, often fails to detect nocturnal and asymptomatic hypoglycemia (4). In recent years, there has been increasing interest in the use of continuous glucose monitoring (CGM), including the flash glucose monitoring system. Since its introduction, CGM has provided unique opportunities to capture glucose profiles over several days, including time in range (TIR), time in hyperglycemia, and glycemic variability as well as nocturnal and daytime glucose level patterns (5). The use of CGM and flash glucose monitoring has increased and, nowadays, is widespread in several countries, whereas SMBG is still the most common glucose monitoring method in other countries.
According to recently published international consensus guidelines for glycemic targets, individuals with type 1 diabetes should spend <4.0% of time per day with glucose levels <3.9 mmol/L (<70 mg/dL) and <1.0% per day <3.0 mmol/L (<54 mg/dL) (6). This guideline is mostly based on studies with CGM and insulin pumps in adults and adolescents with type 1 diabetes. In adults with type 1 diabetes, multiple daily insulin injections (MDI) are the most common method of insulin delivery. However, corresponding suitable targets for MDI treatment are unclear due to lack of data.
To form a further basis for guidelines using CGM metrics, the aim of the current study was to evaluate the association between time spent in hypoglycemia and various HbA1c and mean glucose levels during CGM and SMBG therapy in people with type 1 diabetes treated with MDI.
Research Design and Methods
Cohort
The original GOLD trial was approved by the ethics committee at the University of Gothenburg (12 December 2013, diary number 857-13). The study was an investigator-initiated randomized, open-label, crossover trial carried out at 15 sites in Sweden (Supplementary Table 1) from 24 February 2014 to 1 June 2016. Before participation, all individuals provided verbal and written informed consent. The design of the GOLD trial has been described in detail (7).
Overall Procedures
Individuals ≥18 years old with type 1 diabetes and HbA1c ≥7.5% (58 mmol/mol) treated with MDI were included. Participants were required to have diabetes duration >1 year and fasting C-peptide levels <0.91 ng/mL (<0.3 nmol/L). Patients treated with insulin pumps and current CGM use (within the previous 4 months) were excluded. Study design, including other inclusion and exclusion criteria, has been described in detail (7–9). Each participant wore a masked CGM using the Dexcom G4 Platinum (Dexcom, Inc., San Diego, CA) for 2 weeks during a 6-week run-in phase. Afterward, participants were excluded if they either did not believe they would wear the CGM sensor >80% of the time or did not perform adequate calibrations on their CGM system during the run-in phase (on average ≥12 of 14 during a 7-day period). Participants were randomized 1:1 to either CGM using the Dexcom G4 Platinum stand-alone system or SMBG (conventional therapy) for the first treatment period of 26 weeks, with a 17-week washout period between treatment phases.
All participants were given basic instructions on insulin dosing, such as bolus correction, food choices, and the effect of physical activity on glucose control. In the conventional, SMBG, group, participants were encouraged to measure blood glucose levels according to guidelines (i.e., at least four times daily) and adjust insulin dosages according to those values. All patients had the possibility to contact the responsible staff member for the trial at each site for additional support between the visits if needed, e.g., for technical problems with SMBG meters or the Dexcom G4 system.
Clinical Assessments
Participants were assessed at the start of each treatment phase and at weeks 2, 4, 13, and 26. HbA1c was measured at visits in each treatment phase except week 2. During the conventional treatment phase (SMBG), masked CGM was performed during 2 of the last 4 weeks to evaluate the total time spent in hypoglycemia, TIR, hyperglycemia, and glycemic variability. Patients could then not see their CGM data, but the data were collected for comparisons with CGM treatment data. At all visits, CGM and SMBG data were downloaded and used for optimizing glycemic control. During the randomization visit, earlier advanced diabetes complications were self-reported.
End Points
We evaluated the association between HbA1c levels and amount of time (expressed as percentage) spent in hypoglycemia per day using two different cutoffs: <3.9 mmol/L (<70 mg/dL) and <3.0 mmol/L (<54 mg/dL). Corresponding analyses were performed between mean glucose level estimated by masked CGM and time spent in hypoglycemia. We also evaluated the association between percentage of time with glucose levels 3.9–10.0 mmol/L (70–180 mg/dL) (TIR) and time in hypoglycemia <3.9 mmol/L (<70 mg/dL) and <3.0 mmol/L (<54 mg/dL). We further evaluated the percentage of time spent in hypoglycemia at different mean glucose and HbA1c levels. Time spent in hypoglycemia was evaluated as a continuous variable in relation to HbA1c and mean blood glucose level. Additionally, we evaluated the percentage of patients who reached the target for time spent in hypoglycemia according to guidelines issued by ADA (6) for HbA1c <7.0% (<53 mmol/mol) and <7.5% (<58 mmol/mol). These analyses were performed at baseline and after 26 weeks of CGM and SMBG therapy, respectively.
Statistics
All continuous variables were described by mean, SD, median, range, and 95% CIs where applicable. Categorical variables were described as numbers and percentages, with exact 95% CI presented for percentages where applicable.
Time spent in hypoglycemia with glucose values <3.9 mmol/L (<70 mg/dL) and <3.0 mmol/L (<54 mg/dL) was expressed as a continuous proportion with the dependent variable analyzed with fractional response models (FRM) using a binomial distribution with log-link function, with either continuous HbA1c or glucose levels as explanatory variables. Robust sandwich estimators were applied in order to adjust for potential heteroscedasticity. Relative risk (RR) per 1.0% (10 mmol/mol) increase in HbA1c and 1 mmol/L (18 mg/dL) increase in glucose was presented with associated 95% CI. Additionally, estimated mean time spent in hypoglycemia with 95% CI was presented for various HbA1c and glucose levels.
Data for individuals from both treatment sequences, as per the original crossover randomization in the GOLD trial, were analyzed together in the analyses at the end of CGM and conventional treatment.
All tests were two-tailed and conducted at 0.05 significance level. All analyses were performed using SAS software (version 9.4, SAS Institute Inc., Cary, NC).
Results
Baseline Characteristics
Baseline characteristics of participants per treatment sequence are shown in Table 1. Between February and December 2014, 161 patients were included in the study, of whom 137 (85.1%) had either valid masked CGM data during the first 14 days of the run-in period or at the end of the SMBG treatment or valid CGM data during 14 days at the end of CGM treatment. In total, mean age was 44.6 years, and 43.1% were women. Mean HbA1c (SD) was 8.7% (0.85%) (71.5 [9.3] mmol/mol) at baseline, and mean diabetes duration was 22.3 years. The numbers of individuals in the analysis cohorts varied between 125 and 132. Baseline characteristics for the analysis cohorts are shown in Supplementary Table 2.
Table 1.
Baseline characteristics for patients included in analyses of time in hypoglycemia, mean glucose, and HbA1c
| Demographics and baseline characteristics | All patients (n = 137) |
|---|---|
| Age, years, mean ± SD | 44.6 ± 12.9 |
| Median (range) | 44 (19–77) |
| Sex | |
| Male | 78 (56.9) |
| Female | 59 (43.1) |
| Race | |
| Black | 1 (0.7) |
| White (Caucasian, including Middle East and North Africa) | 136 (99.3) |
| Ethnicity: not Hispanic or Latino | 137 (100.0) |
| Years from diabetes onset to inclusion, mean ± SD | 22.3 ± 11.8 |
| Median (range) | 21.7 (1.4–56.6) |
| Smoking | |
| Current | 17 (12.4) |
| Previous | 31 (22.6) |
| Never | 89 (65.0) |
| Medical history | |
| Previous laser photocoagulation of the retina | 27 (19.7) |
| Previous myocardial infarction | 3 (2.2) |
| Previous stroke | 2 (1.5) |
| Previous bypass graft | 1 (0.7) |
| Previous PCI | 2 (1.5) |
| Previous amputation | 1 (0.7) |
| Previous diabetic foot (or leg) ulcer | 6 (4.4) |
| Current diabetic foot (or leg) ulcer | 3 (2.2) |
| Number of hypoglycemias per week in last 2 months,* mean ± SD | 2.18 ± 1.91 |
| Median (range) | 2 (0–12) |
| Number of patients | 130 |
| Number of severe hypoglycemias past year, mean ± SD | 0.074 ± 0.358 |
| Median (range) | 0 (0–3) |
| Number of patients | 136 |
| Number of severe hypoglycemias past 5 years, mean ± SD | 0.618 ± 2.235 |
| Median (range) | 0 (0–20) |
| Number of patients | 136 |
| HbA1c at visit 2 and randomization | |
| HbA1c at visit 2 (IFCC, mmol/mol), mean ± SD | 71.5 ± 9.3 |
| Median (range) | 70 (58–104) |
| HbA1c at visit 2 (NGSP, %), mean ± SD | 8.70 ± 0.85 |
| Median (range) | 8.56 (7.46–11.67) |
| HbA1c at visit 4 randomization (IFCC, mmol/mol), mean ± SD | 68.9 ± 9.5 |
| Median (range) | 67 (50–103) |
| Number of patients | 136 |
| HbA1c at visit 4 randomization (NGSP, %), mean ± SD | 8.46 ± 0.87 |
| Median (range) | 8.28 (6.73–11.58) |
| Number of patients | 136 |
| Diabetes medication at randomization visit | |
| Base insulin type | |
| Insulatard (NPH insulin) | 3 (2.2) |
| Glargine | 110 (80.3) |
| Detemir | 17 (12.4) |
| Degludec | 7 (5.1) |
| Meal insulin type | |
| Lispro | 52 (38.0) |
| Aspart | 76 (55.5) |
| Glulisine | 7 (5.1) |
| Insulin regular human | 2 (1.5) |
| Total daily meal insulin dose (units), mean ± SD | 27.6 ± 13.5 |
| Median (range) | 25 (0–80) |
| Total daily base insulin dose (units), mean ± SD | 30.5 ± 13.9 |
| Median (range) | 26 (8–90) |
| Total daily insulin dose (units), mean ± SD | 58.1 ± 23.5 |
| Median (range) | 55 (21–138) |
| Number of insulin injections, mean ± SD | 4.82 ± 0.97 |
| Median (range) | 5 (1–8) |
| Metformin used at randomization visit | 2 (1.5) |
Data are n (%) unless otherwise indicated. IFCC, the International Federation of Clinical Chemistry and Laboratory Medicine; NGSP, the National Glycohemoglobin Standardization Program; PCI, percutaneous coronary intervention.
Hypoglycemias experienced per week in last 2 months based on subjective estimation, not blood glucose values.
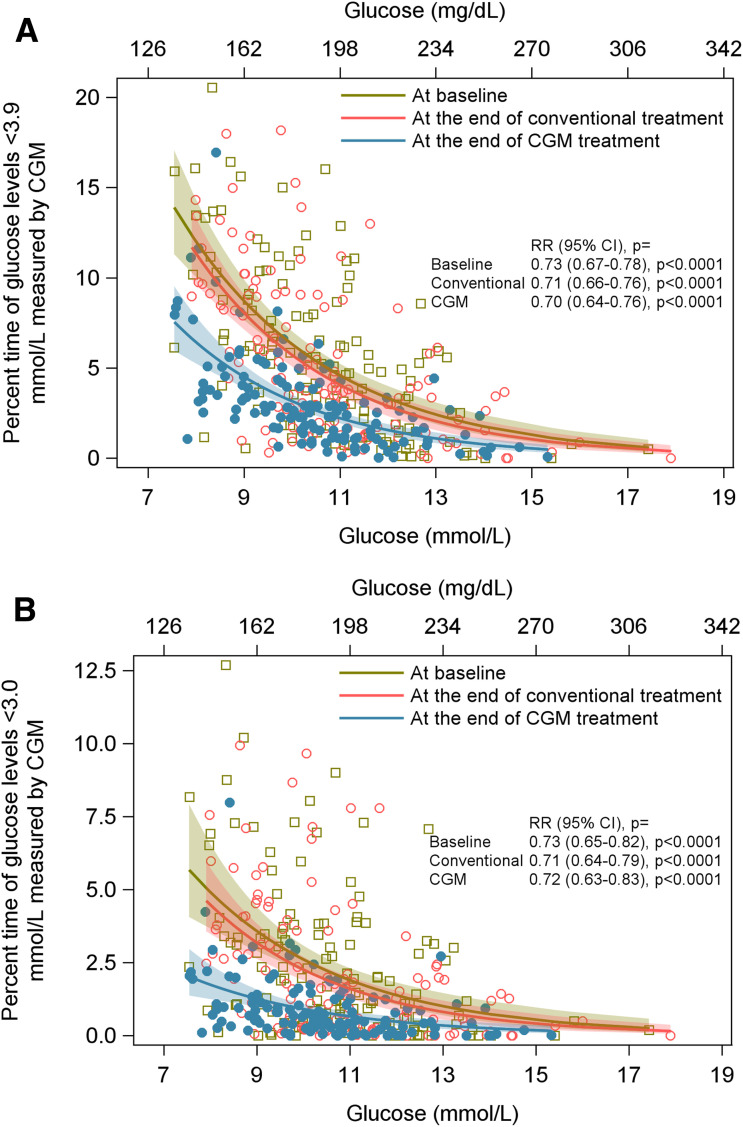
Association Between Mean Glucose Levels and Time Spent in Hypoglycemia
Time spent in hypoglycemia <3.9 mmol/L (70 mg/dL) and <3.0 mmol/L (54 mg/dL) increased significantly with lower mean glucose levels during both CGM (P < 0.0001 and P < 0.0001) and SMBG (P < 0.0001 and P < 0.0001) (Supplementary Table 3). The associations between mean glucose values (mmol/L) and time spent in hypoglycemia <3.9 mmol/L (<70 mg/dL) and <3.0 mmol/L (<54 mg/dL), respectively, at baseline and at the end of CGM and SMBG therapy are shown in Fig. 1A and B.
Figure 1.
A: The association between mean glucose levels (mmol/L) and time with glucose level <3.9 mmol/L (<70 mg/dL) at baseline, at the end of conventional (SMBG) treatment, and at the end of CGM treatment. B: The association between mean glucose levels (mmol/L) and time with glucose level <3.0 mmol/L (<54 mg/dL) at baseline, at the end of conventional (SMBG) treatment, and at the end of CGM treatment.
According to masked CGM readings from the run-in period, when all subjects used SMBG readings for monitoring and treatment adjustments, individuals with mean glucose levels of 8 mmol/L (144 mg/dL) spent, on average, 12.0% of their time with glucose levels <3.9 mmol/L (<70 mg/dL) and 4.9% of their time with levels <3.0 mmol/L (<54 mg/dL). The amount of time spent in hypoglycemia decreased with higher mean glucose levels. At a mean glucose level of 14 mmol/L (252 mg/dL), 1.7% and 0.7% of time was spent in hypoglycemia <3.9 mmol/L (<70 mg/dL) and <3.0 mmol/L (<54 mg/dL), respectively.
Overall, there was less time spent in hypoglycemia with CGM treatment compared with SMBG. In individuals with mean glucose levels of 8 mmol/L (144 mg/dL), the mean percentage of time spent with glucose levels <3.9 mmol/L (<70 mg/dL) was 11.3% in the SMBG group, whereas the corresponding value for individuals using CGM was 6.4%. Corresponding values at glucose levels <3.0 mmol/L (<54 mg/dL) were 4.5% with SMBG versus 1.7% with CGM use. With increasing mean glucose levels, time spent in hypoglycemia was further reduced at the end of SMBG and CGM therapy. Relative risks were similar for all six analyses performed on the impact of a 1 mmol/L (18 mg/dL) increase in glucose on time spent in hypoglycemia and ranged between 0.70 and 0.73—i.e., a 1 mmol/L (18 mg/dL) increase in glucose resulted in an approximate 30% reduction in time spent in hypoglycemia (Supplementary Table 3).
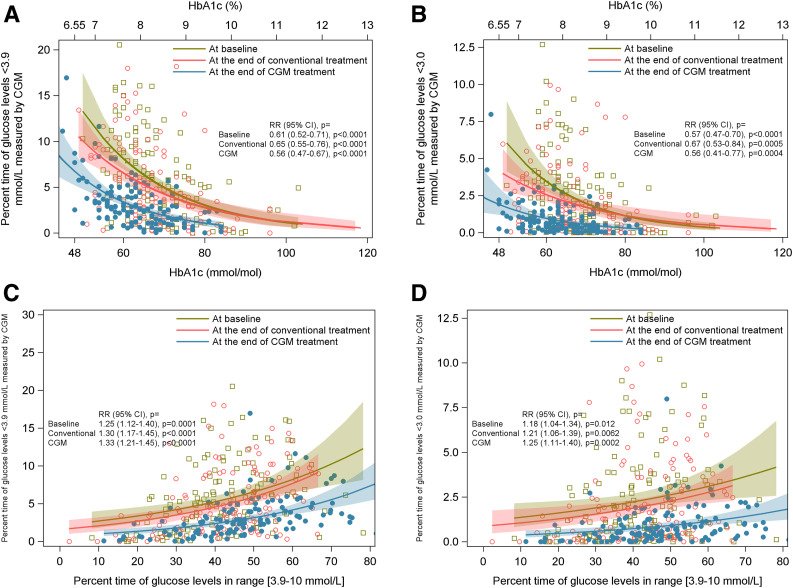
Association Between HbA1c Levels and Time Spent in Hypoglycemia
Figure 2A and B show the association between different HbA1c levels (mmol/mol) and time spent in hypoglycemia at baseline and at the end of CGM and SMBG therapy. Time spent in hypoglycemia <3.9 mmol/L (70 mg/dL) and <3.0 mmol/L (54 mg/dL) increased significantly with lower HbA1c levels during CGM (P < 0.0001 and P = 0.0004) and SMBG (P < 0.0001 and P = 0.0005).
Figure 2.
A: The association between HbA1c levels (mmol/mol) and time in glucose level <3.9 mmol/L (<70 mg/dL) at baseline, at the end of conventional (SMBG) treatment, and at the end of CGM treatment. B: The association between HbA1c levels (mmol/mol) and time in glucose level <3.0 mmol/L (<54 mg/dL) at baseline, at the end of conventional (SMBG) treatment, and at the end of CGM treatment. C: The association between percent TIR 3.9–10 mmol/L (70–180 mg/dL) and time with glucose level <3.9 mmol/L (<70 mg/dL) at baseline, at the end of conventional (SMBG) treatment, and at the end of CGM treatment. D: The association between percent TIR 3.9–10 mmol/L (70–180 mg/dL) and time with glucose level <3.0 mmol/L (<54 mg/dL) at baseline, at the end of conventional (SMBG) treatment, and at the end of CGM treatment.
At baseline, when all patients had SMBG, individuals with HbA1c 7.0% (52 mmol/mol) spent on average 12.0% of their time with glucose levels <3.9 mmol/L (<70 mg/dL) and 5.4% with glucose levels <3.0 mmol/L (<54 mg/dL). Individuals with HbA1c levels 9.7% (83 mmol/mol) spent less time in hypoglycemia, with baseline values of 2.6% at <3.9 mmol/L (<70 mg/dL) versus 0.9% at <3.0 mmol/L (<54 mg/dL) (Supplementary Table 4).
At the end of CGM use, individuals with HbA1c 7.0% (52 mmol/mol) reduced their time spent in hypoglycemia compared with SMBG therapy. Time spent in hypoglycemia <3.9 mmol/L (<70 mg/dL) was 5.4% at the end of CGM use compared with 9.2% with SMBG therapy. The corresponding values for CGM and SMBG at glucose values <3.0 mmol/L (<54 mg/dL) were 1.5% and 3.5%, respectively. Individuals with CGM use and higher HbA1c levels further decreased their time in hypoglycemia for both the higher and lower hypoglycemia cutoffs. As seen in Supplementary Table 4, the effect was more pronounced at the end of CGM use, with time spent in hypoglycemia reduced by 44.0% per 1.0% (10 mmol/mol) increase in HbA1c. In the SMBG group, the corresponding values were ∼34.0% per 1.0% (10 mmol/mol) increase in HbA1c.
Association Between TIR and Time Spent in Hypoglycemia
The associations between percent TIR (3.9–10.0 mmol/L [70–180 mg/dL]) and time spent in hypoglycemia at <3.9 mmol/L (70 mg/dL) and <3.0 mmol/L (54 mg/dL), respectively, at baseline and at the end of CGM and SMBG therapy are shown in Fig. 2C and D.
Time in hypoglycemia (both <3.9 mmol/L [<70 mg/dL] and <3.0 mmol/L [<54 mg/dL]) showed an increase with more TIR. Moreover, patients using CGM had less time in hypoglycemia at all degrees of TIR compared with SMBG. With a TIR of 60%, i.e., slightly below target of 70%, the mean time in hypoglycemia was still above targets, 4.2% <3.9 mmol/L (<70 mg/dL) and 1.1% <3.0 mmol/L (<54 mg/dL) during CGM and 7.7% and 2.8%, respectively, during SMBG.
Percentage of Patients Reaching Target HbA1c Levels and Time in Hypoglycemia
Number, percentage, and 95% CI for percentages of patients with HbA1c <7.5% (<58 mmol/mol) and <7.0% (<52 mmol/mol) and the defined target values for time in hypoglycemia (<3.0 mmol/L and <3.9 mmol/L) are shown in Table 2. During CGM use, 24 (57.1%, 95% CI 41.0–72.3) individuals with type 1 diabetes and HbA1c <7.5% (<58 mmol/mol) spent <1.0% of their time in hypoglycemia <3.0 mmol/L compared with 5 (21.7%, 95% CI 7.5–43.7) individuals with SMBG and 2 (15.4%, 95% CI 1.9–45.5) at baseline. The corresponding numbers for <4.0% time spent in hypoglycemia <3.9 mmol/L were 23 (54.8%, 95% CI 38.7–70.2) with CGM, 5 (21.7%, 95% CI 7.5–43.7) with SMBG, and 3 (23.1%, 95% CI 5.0–53.8) at baseline. For individuals with type 1 diabetes and HbA1c levels <7.0% (<52 mmol/mol), 3 (27.3%, 95% CI 6.0–61.0) had spent <1.0% time in hypoglycemia <3.0 mmol/L and 3 (27.3%, 95% CI 6.0–61.0) had spent <4.0% time in hypoglycemia <3.9 mmol/L at the end of CGM therapy. The corresponding numbers for the end of SMBG treatment were 1 (25.0%, 95% CI 0.6–80.6) and 1 (25.0%, 95% CI 0.6–80.6%), respectively (Table 2).
Table 2.
Number and percentage of patients reaching target HbA1c levels and time in hypoglycemia
| Time point and variable | n (%) | 95% CI for % |
|---|---|---|
| Baseline | ||
| HbA1c <7.5% and <1.0% time in hypoglycemia (<3.0 mmol/L) | 2 (15.4) | 1.9–45.5 |
| HbA1c <7.5% and <4.0% time in hypoglycemia (<3.9 mmol/L) | 3 (23.1) | 5.0–53.8 |
| HbA1c <7.0% and <1.0% time in hypoglycemia (<3.0 mmol/L) | 0 (0.0) | |
| HbA1c <7.0% and <4.0% time in hypoglycemia (<3.9 mmol/L) | 0 (0.0) | |
| End of conventional treatment | ||
| HbA1c <7.5% and <1.0% time in hypoglycemia (<3.0 mmol/L) | 5 (21.7) | 7.5–43.7 |
| HbA1c <7.5% and <4.0% time in hypoglycemia (<3.9 mmol/L) | 5 (21.7) | 7.5–43.7 |
| HbA1c <7.0% and <1.0% time in hypoglycemia (<3.0 mmol/L) | 1 (25.0) | 0.6–80.6 |
| HbA1c <7.0% and <4.0% time in hypoglycemia (<3.9 mmol/L) | 1 (25.0) | 0.6–80.6 |
| End of CGM treatment | ||
| HbA1c <7.5% and <1.0% time in hypoglycemia (<3.0 mmol/L) | 24 (57.1) | 41.0–72.3 |
| HbA1c <7.5% and <4.0% time in hypoglycemia (<3.9 mmol/L) | 23 (54.8) | 38.7–70.2 |
| HbA1c <7.0% and <1.0% time in hypoglycemia (<3.0 mmol/L) | 3 (27.3) | 6.0–61.0 |
| HbA1c <7.0% and <4.0% time in hypoglycemia (<3.9 mmol/L) | 3 (27.3) | 6.0–61.0 |
Conclusions
Principal Findings
This study, based on data from the GOLD randomized clinical trial, showed that people with type 1 diabetes treated with MDI have difficulties reaching targets for time in hypoglycemia and simultaneously reaching HbA1c targets. This was evident both with CGM and SMBG monitoring, but the time in hypoglycemia was considerably less during CGM than during SMBG monitoring. When HbA1c levels <7.5% (<58 mmol/mol)—i.e., somewhat above target—were evaluated, >40% of patients during CGM and >70% during SMBG spent more time in hypoglycemia than recommended by recent guidelines. At HbA1c 7.0% (52 mmol/mol), time spent in hypoglycemia <3.9 mmol/L (70 mg/dL) was ∼5.5% and 9.0% during CGM and SMBG treatment, respectively, and 1.5% and 3.5% for the hypoglycemia cutoff <3.0 mmol/L (54 mg/dL). A consistent association was found both during CGM and SMBG monitoring over a broad range of HbA1c levels showing that the lower the HbA1c level obtained, the more time in hypoglycemia.
Guidelines and Earlier Studies
Our results from the current study show that it will remain challenging for many individuals with type 1 diabetes treated with MDI to achieve the targets set for time spent in hypoglycemia in recent international guidelines even with modern CGM devices. For patients using SMBG for glucose monitoring, which is still the most common method in many developed countries for people with type 1 diabetes, few are likely to achieve hypoglycemia targets. The recent guidelines for recommended time spent in hypoglycemia are mainly based on a clinical trial of the semi-closed-loop system where patients obtained a mean HbA1c level of 6.9% (52 mmol/mol) and 3.3% time in hypoglycemia <3.9 mmol/L and 0.6% time <2.8 mmol/L. Of note, patients included in that trial had HbA1c close to recommended glycemic target of HbA1c 7.4% (57 mmol/mol) at baseline and possibly achieved better results with a semi-closed-loop system than other patients further from glycemic targets (10). Moreover, patients generally receive more support in clinical trials than clinical practice. In a recent randomized trial of a semi-closed-loop system, patients with HbA1c 7.4% (57 mmol/mol) at baseline spent 1.58% of their time in hypoglycemia <3.9 mmol/L and 0.29% of time <3.0 mmol/L (11). It is essential to note that time spent in hypoglycemia may differ by various semi-closed-loop systems depending on sensor and algorithms used (10,11).
Explanations
Although direct comparisons between different studies should be performed with caution, the proportion of time spent in hypoglycemia seems to be greater in MDI-treated patients than in patients with semi-closed-loop systems. A recent study that compared adding CGM to MDI and pump treatment showed relatively similar effects with respect to HbA1c and time spent in hypoglycemia when patients fully performed insulin dosing (12). Halting the insulin infusion by sensor-augmented pump therapy has been shown to further reduce time spent in hypoglycemia (13). Interestingly, insulin delivery by semi-closed-loop systems reduced not only HbA1c but also time spent in hypoglycemia compared with a pump system only halting insulin delivery at low glucose levels (10). Thus, it likely will be difficult for many patients using MDI to reach effects on time spent in hypoglycemia similar to those seen with semi-closed-loop systems because, for example, continuous modification of insulin delivery cannot be performed during MDI treatment and because of the difficulty many patients experience making appropriate adjustments on a regular basis as compared with an automatic algorithm. Furthermore, in this study, 80.3% had basal insulin glargine. It is possible that with novel development of insulins, basal and mealtime insulin may further reduce the time spent in hypoglycemia.
Implications
Our results imply that targets for time spent in hypoglycemia may be further discussed for MDI- and semi-closed-loop–treated patients. Additionally, if people with MDI are to have a chance to reach targets for time spent in hypoglycemia, they will need CGM support, since patients in the current study had considerably less time in hypoglycemia at all evaluated HbA1c levels compared with SMBG. Patients using SMBG were in general far from reaching hypoglycemia targets. Moreover, to obtain targets many individuals will likely benefit from replacing MDI treatment with semi-closed-loop systems. Additionally, lately, the TIR metric has been more in focus in clinical practice. It is noteworthy that during CGM use, less time in hypoglycemia existed at all evaluated degrees of TIR compared with when patients used SMBG. However, the majority still had difficulties simultaneously reaching the target of 70% TIR and the targets for time in hypoglycemia. Semi-closed-loop systems likely provide a safer strategy to achieve near-normal glycemic control in the absence of hypoglycemia risk compared with CGM alone (11). However, it should be noted that these systems are relatively new, and safety data from further long-term trials and real-life studies will be needed, although current clinical trial data look promising including one where no severe hypoglycemia occurred in 168 patients over 6 months (11). Finally, studies aimed at supporting patients using MDI treatment with algorithms and education for optimal insulin dosing decisions are warranted to obtain better results in lowering of HbA1c and simultaneously reducing time spent in hypoglycemia.
HbA1c Level and Time Spent in Hypoglycemia
When the main results of the Diabetes Complications and Control Trial were released in 1993, it was clear that the risk of hypoglycemia increased substantially with lower mean HbA1c levels (1). It was recently debated to what extent this association exists, with modern glucose monitoring having the capability to alarm for low glucose levels. The current study, however, shows that during MDI treatment and CGM use, this association still exists. When discussing goals for hypoglycemia targets with an individual patient, it is essential to take the current HbA1c level into consideration. The reason is that there is an exponential relationship between HbA1c and risk of long-term complications (1,14). This means that reductions in HbA1c at high levels will lead to much greater reductions in risk of complications than at levels closer to HbA1c targets. Since many patients with type 1 diabetes and MDI will not reach HbA1c and hypoglycemia targets simultaneously, these must be weighed against each other for certain patients. For many patients, it may be reasonable to accept a certain increase in risk of hypoglycemia in exchange for lowering HbA1c from high levels, whereas such a risk may not be reasonable when HbA1c levels are already close to general targets.
Strengths and Limitations
Strengths of the current study include that patients were examined in a clinical trial where detailed procedures were used for downloading and storing CGM data. The same CGM system was used among patients, and HbA1c was analyzed at a central laboratory. Moreover, CGM data were obtained both during CGM treatment and conventional SMBG treatment (when masked CGM was performed) for one and the same patient. Information obtained during SMBG treatment presented here is important since the majority of individuals with type 1 diabetes worldwide still use this type of glucose monitoring. Limitations include that relatively few patients could be evaluated at the general HbA1c target of 7.0% (52 mmol/mol), especially during conventional therapy. On the other hand, we saw that even at higher HbA1c levels (7.5%, 58 mmol/mol), many patients did not reach hypoglycemia targets. Another limitation is that since this study was performed, CGM technology has improved (e.g., no calibrations are needed with the Dexcom G6). Although direct comparisons do not exist of Dexcom G4 and G6 of accuracy, studies of individual systems indicate an increasing accuracy for Dexcom G6 (15). Data on frequency of calibrations, calibration errors, and transmitter issues were not reported during this study. Although the number of SMBG measurements has earlier been shown to be fewer during CGM treatment (2.75 vs. 3.66), it is noteworthy that during Dexcom G4 use, in contrast to current generations of CGM, capillary testing was performed for calibrations during CGM (8). It should also be noted that the current study was performed in adults and may not be generalizable to children with type 1 diabetes treated with MDI. Additionally, the study cohort represents individuals who feel they would wear CGM >80% of the time, possibly leading to a somewhat selected study population. Therefore, further studies in a more general population of people with type 1 diabetes are of interest.
Conclusion
Time spent in hypoglycemia for people with type 1 diabetes treated with MDI increases both during CGM and SMBG therapy with lower mean glucose and lower mean HbA1c levels. It is difficult for many patients with type 1 diabetes and MDI treatment to reach targets for time spent in hypoglycemia even with somewhat higher HbA1c levels than the general target of 7.0% both with CGM and SMBG. CGM is, however, associated with considerably less time with hypoglycemia than SMBG both at HbA1c levels close to target and at high HbA1c levels. Overall, patients with type 1 diabetes treated with MDI need CGM treatment for glucose monitoring to have a chance to approach hypoglycemia targets and simultaneously reach HbA1c targets.
Article Information
Acknowledgments. The authors thank all participating sites and thank Joseph Murphy, an independent medical writer, for language editing of the manuscript.
Funding. The study was financed by grants from Swedish State (ALF agreement). CGM sensors and CGM systems were received from Dexcom for carrying out the GOLD trial.
Duality of Interest. I.B.H. has done research for Medtronic Diabetes and consulting for Abbott Diabetes Care, Roche, and Bigfoot. J.H. has been a speaker and/or on the advisory board for Novo Nordisk, Bayer, Merck Sharp & Dohme, Eli Lilly, Sanofi, Boehringer Ingelheim, and Abbot. M.E. is an employee of Novo Nordisk and holds shares in Novo Nordisk A/S. T.H. received research funds from Adocia, Boehringer Ingelheim, Dance Pharmaceuticals, Eli Lilly, Gan & Lee Pharmaceuticals, Johnson & Johnson, Mars, Medimmune, Mylan, Nordic Bioscience, Novo Nordisk, Pfizer, Poxel, Saniona, Sanofi, Wockhardt, and Zealand Pharma; received speaker honoraria and travel grants from Eli Lilly and Novo Nordisk; and is a member of advisory panels for Mylan and Novo Nordisk. W.P. served as a consultant for Dexcom and Abbott Diabetes Care. M.W. has served on advisory boards and/or lectured for Merck Sharp & Dohme, Eli Lilly, Novo Nordisk, and Sanofi and has organized a professional regional meeting sponsored by Eli Lilly, Rubin Medical, Sanofi, Novartis, and Novo Nordisk. E.S. has lectured for Novo Nordisk, Sanofi, Boehringer, Abbot, Rubin Medical, and Eli Lilly. M.L. has received grants from Dexcom and Novo Nordisk; has consulted or received honoraria from AstraZeneca, Dexcom, Eli Lilly, Medtronic, Novo Nordisk, and Rubin Medical; and has participated in advisory boards for AstraZeneca, Boehringer Ingelheim, Merck Sharp & Dohme, and Novo Nordisk. No other potential conflicts of interest relevant to this article were reported.
Financial support was received from Dexcom for carrying out the GOLD trial. No financial support was received from Dexcom for the current analyses of the GOLD data or publication. Dexcom was not involved in any parts of this study (designing the current study, analyses or intepretation of data, writing of the report, or decision to submit the publication).
Author Contributions. S.S.A. wrote the first draft of the manuscript. S.S.A., A.P., and M.L. designed the study. A.P. performed the statistical calculations. I.B.H., J.H., T.H., W.P., S.D., and M.L. were on the steering committee for this study. All authors participated in interpreting the data and revising the manuscript, and all approved the final version. S.S.A. and M.L. are the guarantors of this work and, as such, had full access to all the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis.
Prior Presentation. Parts of this study were presented in oral form at the 13th International Conference on Advanced Technologies & Treatments for Diabetes, Madrid, Spain, 19–22 February 2020.
Footnotes
Clinical trial reg. no. NCT02092051, clinicaltrials.gov
This article contains supplementary material online at https://doi.org/10.2337/figshare.12357506.
References
- 1.Nathan DM, Genuth S, Lachin J, et al.; Diabetes Control and Complications Trial Research Group . The effect of intensive treatment of diabetes on the development and progression of long-term complications in insulin-dependent diabetes mellitus. N Engl J Med 1993;329:977–986 [DOI] [PubMed] [Google Scholar]
- 2.Nathan DM, Cleary PA, Backlund JY, et al.; Diabetes Control and Complications Trial/Epidemiology of Diabetes Interventions and Complications (DCCT/EDIC) Study Research Group . Intensive diabetes treatment and cardiovascular disease in patients with type 1 diabetes. N Engl J Med 2005;353:2643–2653 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kalra S, Mukherjee JJ, Venkataraman S, et al. Hypoglycemia: the neglected complication. Indian J Endocrinol Metab 2013;17:819–834 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Danne T, Nimri R, Battelino T, et al. International consensus on use of continuous glucose monitoring. Diabetes Care 2017;40:1631–1640 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.American Diabetes Association 7. Diabetes technology: Standards of Medical Care in Diabetes—2019. Diabetes Care 2019;42(Suppl. 1):S71–S80 [DOI] [PubMed] [Google Scholar]
- 6.Battelino T, Danne T, Bergenstal RM, et al. Clinical targets for continuous glucose monitoring data interpretation: recommendations from the international consensus on time in range. Diabetes Care 2019;42:1593–1603 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lind M, Polonsky W, Hirsch IB, et al. Design and methods of a randomized trial of continuous glucose monitoring in persons with type 1 diabetes with impaired glycemic control treated with multiple daily insulin injections (GOLD study). J Diabetes Sci Technol 2016;10:754–761 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lind M, Polonsky W, Hirsch IB, et al. Continuous glucose monitoring vs conventional therapy for glycemic control in adults with type 1 diabetes treated with multiple daily insulin injections: the GOLD randomized clinical trial. JAMA 2017;317:379–387 [DOI] [PubMed] [Google Scholar]
- 9.Ólafsdóttir AF, Polonsky W, Bolinder J, et al. A randomized clinical trial of the effect of continuous glucose monitoring on nocturnal hypoglycemia, daytime hypoglycemia, glycemic variability, and hypoglycemia confidence in persons with type 1 diabetes treated with multiple daily insulin injections (GOLD-3). Diabetes Technol Ther 2018;20:274–284 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bergenstal RM, Garg S, Weinzimer SA, et al. Safety of a hybrid closed-loop insulin delivery system in patients with type 1 diabetes. JAMA 2016;316:1407–1408 [DOI] [PubMed] [Google Scholar]
- 11.Brown SA, Kovatchev BP, Raghinaru D, et al.; iDCL Trial Research Group . Six-month randomized, multicenter trial of closed-loop control in type 1 diabetes. N Engl J Med 2019;381:1707–1717 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Šoupal J, Petruželková L, Grunberger G, et al. Glycemic outcomes in adults with T1D are impacted more by continuous glucose monitoring than by insulin delivery method: 3 years of follow-up from the COMISAIR study. Diabetes Care 2020;43:37–43 [DOI] [PubMed] [Google Scholar]
- 13.Bergenstal RM, Klonoff DC, Garg SK, et al.; ASPIRE In-Home Study Group . Threshold-based insulin-pump interruption for reduction of hypoglycemia. N Engl J Med 2013;369:224–232 [DOI] [PubMed] [Google Scholar]
- 14.Tönnies T, Stahl-Pehe A, Baechle C, et al. Risk of microvascular complications and macrovascular risk factors in early-onset type 1 diabetes after at least 10 years duration: an analysis of three population-based cross-sectional surveys in Germany between 2009 and 2016. Int J Endocrinol 2018;2018:7806980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Welsh JB, Gao P, Derdzinski M, et al. Accuracy, utilization, and effectiveness comparisons of different continuous glucose monitoring systems. Diabetes Technol Ther 2019;21:128–132 [DOI] [PMC free article] [PubMed] [Google Scholar]