Abstract
Ethnic South Asian Americans (SAAs) have the highest relative risk of type 2 diabetes mellitus (T2DM) in the United States (US). Culturally tailored lifestyle interventions have the potential to promote South Asian diabetes prevention; however, the extent of their use and evaluation in US settings remains limited. This systematic review characterizes and evaluates outcomes of community-based lifestyle interventions targeted towards T2DM indicators among South Asians living in the US. A PRISMA-informed search of Pubmed, Embase, Cochrane, Web of Science, and clinical trial registry databases using key words pertaining to South Asians migrants and diabetes indicators (glucose and insulin outcomes) was conducted of community-based lifestyle interventions published up until October, 31 2019. Of the eight studies included in the final synthesis, four interventions focused on cultural and linguistic adaptations of past chronic disease prevention curricula using group-based modalities to deliver the intervention. Hemoglobin A1c (A1c) was the most common outcome indicator measured across the interventions. Three of the five studies observed improvements in indicators post-intervention. Based on these findings, this review recommends 1) greater exploration of community-based lifestyle interventions with high quality diabetes indicators (such as fasting blood glucose) in ethnic SAA communities, 2) expanding beyond traditional modalities of group-based lifestyle interventions and exploring the use of technology and interventions integrated with passive, active, and individualized components, and 3) development of research on diabetes prevention among second generation SAAs.
Keywords: Diabetes, Insulin, Glucose, Lifestyle, South Asian, Migrants, Community health
1. Background
1.1. Diabetes among South Asians in the US
In 2017 approximately 30.3 million people in the US were living with diabetes, creating an epidemic cost of 327 billion (American Diabetes Association, 2018, Centers for Disease Control and Prevention, 2017). Ethnic SAAs have a disproportionately high burden of T2DM; ethnic Asian Indians for instance have a higher odds of prevalent T2DM compared to both whites and other Asian American subgroups (Lee et al., 2011). In clinical and research settings, the primary outcome indicators used to measure and screen for T2DM include measures of blood glucose, such as A1c, fasting plasma glucose (FPG), the oral glucose tolerance test (OGTT), and measures of insulin resistance, such as the Homeostasis Model Assessment (HOMA) and the Quantitative Insulin Sensitivity Check Index (QUICKI) (Gutch et al., 2015, American Diabetes Association, 2004). Lifestyle factors (such as poor diet and exercise) have been recognized as key contributors to the sharp rise in T2DM (Hu, 2011). Among ethnic South Asians, factors such as migration and cultural values pertaining to diet and exercise have been observed to further compound the rising prevalence of T2DM (Bhopal, 2013).
Much of the existing literature and reviews on interventions targeting T2DM among South Asian migrants have targeted diabetes management and focused on populations living in the United Kingdom and Europe (Navodia et al., 2019, Ballotari et al., 2017, Khunti et al., 2008). Yet, compared to the United Kingdom and Europe, the United States attracts a significantly greater population of highly educated, first-generation South Asian migrants (Platonova and Urso, 2013, Gov, 2018, Lopez et al., 2017). The significant differences in socio-demographics, relevant to intervention design between South Asian migrants living in the US versus those in the UK and Europe, suggests the need for region-based intervention analysis. Likewise, given the rise of pre-diabetes in the United States, preventing diabetes incidence is also of paramount importance (Centers for Disease Control and Prevention, 2017).
1.2. Diabetes prevention interventions
Although diabetes management remains a concern among many ethnic South Asians in the United States, there has been a growing impetus to focus attention on diabetes prevention among individuals with pre-diabetes and patients who have not yet developed diabetes but may be at-risk (Alberti et al., 2007). Diabetes prevention programs focus on promoting health-protective lifestyle changes; however, these programs must be tailored in a culturally sensitive way to optimize programmatic effectiveness (Alberti et al., 2007).
In the United States, the large, multi-ethnic, multi-center Diabetes Prevention Program (DPP) has provided robust evidence for diabetes prevention (Kramer et al., 2009). However, the program lacks a separate analysis of ethnic South Asian community outcomes. Its generalizability for the Asian American migrant community has also been criticized, in part, due to limited cultural relevance in the diet, exercise, and behavior change components of the program (Nguyen et al., 2015). Indeed, with the observed need for cultural precision in diabetes prevention campaigns, there is a gap in understanding the impact that existing diabetes prevention interventions (with varying levels of cultural sensitivity in design) have had on at-risk subpopulations such as ethnic SAAs.
Community-based lifestyle interventions are particularly promising for diabetes prevention among ethnic SAAs. The strength of this approach lies in a number of key aspects (Institute of Medicine, 2012). First, targeting an intervention at the population level among individuals with varying levels of risk allows for maximum reach and access to intervention materials, especially relevant for communities such as ethnic SAAs who may not be able to afford or seek clinical services (South Asian Americans Leading Together (SAALT), 2009). Second, since diabetes progression involves complex dynamics between behavioral and environmental factors, community-based approaches can be designed to affect social or environmental conditions in ways that clinical services cannot. Finally, community-based prevention can be culturally tailored to a certain populations’ unique barriers to disease prevention.
The aims of this systematic review are twofold: 1) describe characteristics of community-based lifestyle interventions which have assessed changes in T2DM glucose and insulin indicators among ethnic SAAs, and 2) evaluate the effectiveness of these interventions in improving T2DM glucose and insulin indicators. In doing so, this review will identify components associated with successful community-based lifestyle interventions among ethnic SAAs as well as opportunities for further research.
2. Methods
2.1. Search strategy
A systematic search of literature published up through October 31, 2019 was performed adhering to Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines (Moher et al., 2009). Database search included PubMed, Web of Sciences, Embase, Cochrane, and SCOPUS. A manual search was conducted for further peer-reviewed studies, grey literature, and registered clinical trials from WHO International Clinical Trials Registry Platform, Clinicaltrial.gov, and Google Scholar. Authors of protocols, registered trials, and studies with only baseline data were individually contacted to assess if post-intervention data was available for inclusion (three contact attempts were made of each author).
The detailed search strategy employed in the formal database search is displayed in Table 1. Key words used included community-based lifestyle intervention related terms informed from past systematic reviews along with terms focused on South Asian immigrant populations (those ethnically identifying as Indian, Pakistani, Bangladeshi, Sri Lankan, Nepalese, Bhutanese, or Maldivian), and terms relating to diabetes, including glucose or insulin indicators (A1C, plasma blood glucose, 2 h post load glucose, insulin sensitivity, among others) (Satterfield et al., 2003).
Table 1.
Search Strategy.
| Component | Key Words |
|---|---|
| Population | (South Asia* OR India* OR Sri Lanka* OR Nepal* OR Bangladesh* OR Bhutan* OR Maldiv* OR Pakistan*) AND (Migra* OR Immigra* OR Emigra* OR Minorit*) |
| Intervention | (implementation OR intervention OR health promotion OR clinical trial OR lay worker OR lay health advisor OR lay health educator OR lay health worker OR peer counseling OR peer support OR peer-based OR peer-support OR peers OR peer education OR group education OR group support OR group-based OR peer counseling OR peer support OR peer led intervention OR peer-led intervention OR peer based intervention OR community-led OR community-based OR school based OR work based OR mosque based OR temple based OR gurdwara based OR family based) |
| Outcome | (diabetes OR T2DM OR tidm OR iddm OR niddm OR diabetes mellitus OR glucose intolerance OR HbA1C OR A1C OR hemoglobin a1c OR blood glucose OR plasma glucose OR fasting glucose OR fasting blood glucose OR postload glucose OR post load glucose OR postprandial glucose OR post prandial glucose OR oral glucose OR insulin OR insulin resistance OR insulin sensitivity OR homeostasis model assessment OR HOMA OR quantitative insulin sensitivity check index OR QUICKI OR Matsuda index OR normoglycemia OR IGT OR impaired glucose tolerance OR IFT OR impaired fasting glucose) |
2.2. Eligibility of studies
A screening reliability test was conducted by two independent reviewers (SA and BM) of 60 abstracts within the full screening sample, followed by complete abstract and title screening. Studies conducted on ethnic SAA populations above the age of 18 were within the scope of the study. A study was included if it satisfied the following criteria. First, the study had to focus, at least partly, on a specific South Asian population (including the seven identified South Asian nationalities) that were residing in the US at the time of study. Second, the study must discuss a community-based intervention defined as an “approach directed to a population rather than individuals, implemented in community settings rather than hospital or health care settings, and approaches coordinated through friends, family, neighbors, community members, worksites, schools or primary health care centers” (Satterfield et al., 2003). Third, the study had to include at least baseline data. Fourth, the study had to include biomarkers commonly used to assess diabetes risk: blood glucose or insulin related indicators. A study was excluded if it was a review, lacked an ethnic SAA sample, focused exclusively on diabetes management among individuals with T2DM, or lacked a community-based component (e.g., exclusively structural or clinic/hospital-based).
2.3. Data extraction
A data extraction form was developed by the study authors and pilot tested before being implemented for the final study sample. Data extracted included study participant characteristics, intervention characteristics, and outcome variable data. Full-text assessment and data extraction were conducted by two independent reviewers (SA and SM), and the senior author (RD) served as a tiebreaker when a consensus could not be reached. If demographic information for control and intervention group was presented separately, a weighted average was calculated for the variables of interest.
2.4. Quality assessment of included studies
The National Heart, Lung, and Blood Institute (NHLBI) study quality assessment tool was applied to all included studies by two independent reviewers (SA and SM). One of two NHLBI checklists were used, depending on study design: controlled intervention studies or before-after (pre-post) studies with no control group (National Heart Lung and Blood Institute (NHLBI), n.d.). Given the heterogeneity in the study designs, the checklists were supplemented by a brief narrative quality assessment focused on aspects of feasibility, acceptability, retention, and the meaningful role of cultural and community-based design and adaptation measures.
3. Results
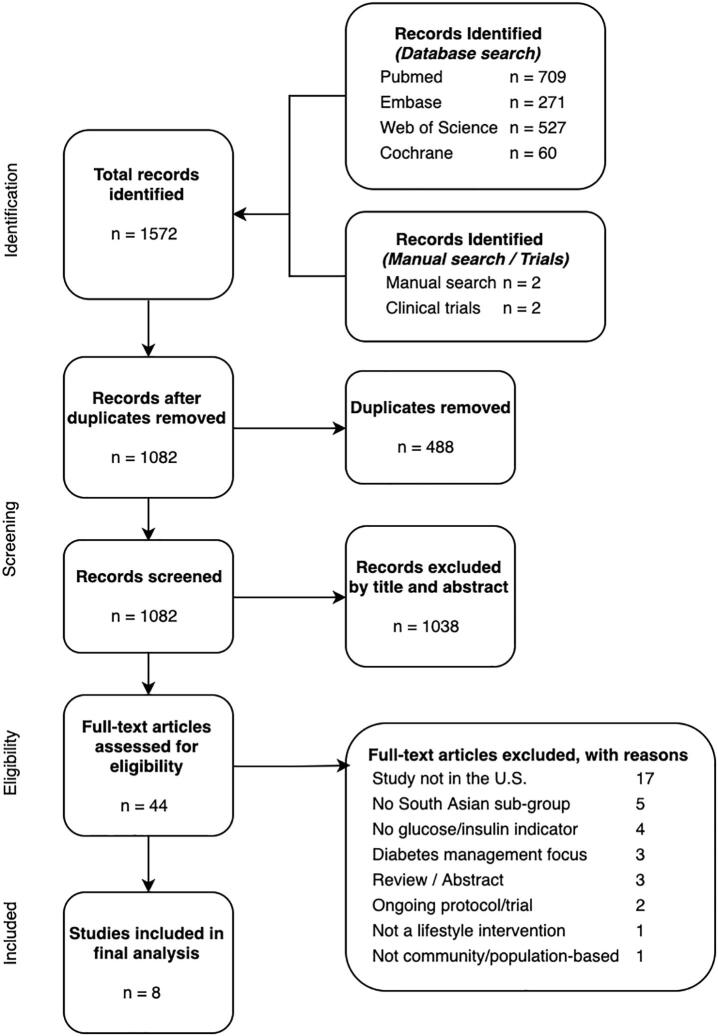
The search strategy retrieved 1571 individual articles, of which 44 passed through title and abstract screening. Another 36 studies were excluded through the full text assessment process specified in Fig. 1. Of the one protocol and two registered trials that passed through screening, study authors of only one registered trial (Narayan, 2010) were able to provide an unpublished manuscript with both baseline and post-intervention data, which has since been published (Weber et al., 2020).
Fig. 1.
PRISMA flowchart of search strategy and included studies.
3.1. Included studies
Eight studies were included in the final qualitative synthesis, including two randomized controlled trials (Kandula et al., 2015, Patel et al., 2017), two two-group pre-post studies (Islam et al., 2014, Lim et al., 2019), three one-group pre-post studies (Gany et al., 2014, Kandula et al., 2016), and one experimental study with only baseline data (Sathe et al., 2013) (Table 2). While the number of participants analyzed in intervention or control groups across most studies was between 20 and 54, one single-group pilot study had only 9 participants with follow-up data (Weber et al., 2020), while another large intervention trial had 2726 participants (Sathe et al., 2013).
Table 2.
List of included studies.
| Author (year) | Location of study | Study Design | Description of study population | Study participants analyzed | Glucose/insulin indicators | Effectiveness of intervention | NHLBI Quality Assessment 1,2 |
|---|---|---|---|---|---|---|---|
| Kandula et al. (2015) | Chicago, IL |
RCT | Asian Indians or Pakistanis with at least one atherosclerotic cardiovascular disease risk factor | Intervention: 31 Control: 32 |
A1C,Fasting blood glucose (mg/DL) |
6-month 0.43% decrease in A1C, no significant change in fasting glucose | Good1 |
| Patel et al. (2017) | Houston,TX | RCT | Gujarati Asian Indians at-risk for T2DM | Intervention: 26 Control: 20 |
A1C | 6-month 1.96 mmol/mol and 12-month 2.42 mmol/mol decrease in A1C | Good1 |
| Islam et al. (2014) | New York City, NY | 2GPP | Sikh Asian Indians at-risk for T2DM | Intervention: 54 Control: 48 |
2 h fasting blood glucose (mg/DL) | 6-month 25.6 mg/dL decrease in blood glucose | Fair1 |
| Lim et al. (2019) | New York City, NY | 2GPP | Sikh Asian Indians at-risk for T2DM | Intervention: 71 Control: 89 |
2 h fasting blood glucose (mg/DL | 6-month 19.6 mg/dl decrease in blood glucose | Good1 |
| Gany et al. (2014) | New York City, NY | 1GPP | Asian Indian, Pakistani, and Bangladeshi taxi drivers | Intervention: 47 Control: N/A |
Random glucose test (mg/DL) | No significant change in blood glucose | Good2 |
| Kandula et al. (2016) | Chicago, IL |
1GPP | South Asian women with children (age 6–12) who were at-risk for T2DM | Intervention: 30 Control: N/A |
A1C | 4-month 0.1% increase in A1C | Good2 |
| Weber et al. (2020) | Atlanta, GA |
1GPP | Overweight, pre-diabetic South Asians | Intervention: 9 Control: N/A |
A1C, Normoglycemia, Isolated IGT, Isolated IFT | ^Decrease in A1C, iIGT, iIFT, increase in normoglycemia | Fair2 |
| Sathe et al. (2013) | Alameda, CA |
Baseline | South Asians at-risk for cardiovascular disease | Intervention: 2726 Control: N/A |
Random glucose test (mg/DL) | N/A (Baseline only) | N/A |
1GPP: One-group pre-test/post-test study; 2GPP: Two-group pre-test/post-test study; RCT: Randomized controlled trial;
NHLBI Controlled Intervention Studies tool.
NHLBI Before-After (Pre-Post) Studies With No Control Group tool.
statistical testing not conducted due to small sample size.
The sample characteristics of the studies varied (Table 3). All studies were conducted in large, urban centers across different regions of the US. While many studies targeted ethnic South Asians Americans broadly, others were more specifically focused on categories of ethnicity (Patel et al., 2017), religion (Islam et al., 2014), occupation (Gany et al., 2014), or motherhood status (Kandula et al., 2016). Most studies were primarily based on populations at risk for a chronic illness. Three studies focused on populations at risk for T2DM through the American Diabetes Association risk assessment tool (Islam et al., 2014, Lim et al., 2019) or the Madras Diabetes Research Foundation’s Indian Diabetes Risk Score (Patel et al., 2017). One study focused on overweight (using the ≥22 kg/m2 cut-off identified for Asian populations (WHO Expert Consultation, 2004) participants with pre-diabetes (FPG 100–125 mg/dl and/or 2-hour post-load glucose of 140–199 mg/dl) (Weber et al., 2020). Other at-risk factors used for participant eligibility included BMI of ≥25 kg/m2 (Kandula et al., 2016), family history of diabetes (Kandula et al., 2016), or at least one cardiovascular disease risk factor (BMI ≥ 25 kg/m2, total cholesterol ≥ 200, LDL cholesterol ≥ 130, prediabetes using FPG > 100 or A1c 5.7–6.4, diabetes using FPG > 126 or A1c > 6.4, systolic blood pressure ≥ 140, or diastolic blood pressure ≥ 90) (Kandula et al., 2015).
Table 3.
Characteristics of populations studied (baseline + interventional studies).
| Author (year) | Included sub-groups | Males | Females | Born abroad | Born in US | Average age (range) | Education range | Income range |
|---|---|---|---|---|---|---|---|---|
| Kandula et al. (2015) | Indian, Pakistani |
37% | 63% | 100% | 0% | 50.0 (30–59) | Below high school: 27% | N/A |
| Patel et al. (2017) | Indian | 46% | 54% | 98% | 2% | 53.1 | High school: 13% Bachelor’s degree: 46% Graduate degree: 41% |
N/A |
| Islam et al. (2014) | Indian | 19% | 81% | 100% | 0% | 46.3 (18–75) | Below high school: 13% High school/some college: 67% College: 17% |
N/A |
| Lim et al. (2019) | Indian, Bangladeshi | 31% | 69% | 100% | 0% | 46.5 (18–75) | Below high school: 13% High school/some college: 70% College: 14% |
N/A |
| Gany et al. (2014) | Indian, Pakistani, Bangladeshi | 100% | 0% | 100% | 0% | 47.9 (30–79) | Post college/graduate school: 28% College/some college: 34% High school and below: 38% |
N/A |
| Kandula et al. (2016) | Indian, Pakistani, Other | 0% | 100% | 100% | 0% | N/A | High school and below: 57% | N/A |
| Weber et al. (2020) | Self-identified South Asian | 77% | 23% | N/A | N/A | 46.9 | Some college and above: 100% | N/A |
| Sathe et al. (2013) | Indian, Pakistani, Bangladeshi, Sri Lankan, Nepali | 69% | 31% | 92% | 4% | 43 | Bachelor’s degree or higher: 96% | N/A |
While two studies exclusively studied men (Gany et al., 2014) or women (Kandula et al., 2016), four predominantly included men (Sathe et al., 2013) or women (Kandula et al., 2015, Islam et al., 2014, Lim et al., 2019), and only one study showed a relatively balanced gender profile (Patel et al., 2017). Five studies focused only on first-generation South Asian immigrants (born outside of the US), and among the two studies with US-born participants, these individuals represented only 2% and 4% of the total study sample, respectively (Patel et al., 2017, Sathe et al., 2013). The average age of participants ranged from 43 to 53.1 years; however, education status varied markedly. While 87% and 96% of two studies, respectively, had participants with bachelor’s degree or higher (Patel et al., 2017, Sathe et al., 2013), other studies had significant (or majority) of participants with high school (or below) levels of educational attainment (Gany et al., 2014, Kandula et al., 2016).
The quality of the studies was generally good for their study design, with all but two studies scoring in the (“Good”) category on the three-option (“Good, Fair, Poor”) NHLBI assessment tool. Most studies were pilot studies and did not include a control group. Among controlled studies, a few used randomizations but others, such as Islam et al., did not due to negative community perceptions toward randomization (Islam et al., 2014). Most studies compared the characteristics of those who dropped out of the study with those who stayed in the study (with issues of time-commitment being a salient reason for attrition across the interventions); however, only one study included a full qualitative process evaluation through participant interviews to understand barriers and facilitators of the intervention (Kandula et al., 2016). Community-based participatory research (CBPR) approaches were also widely employed to enhance study quality; Kandula et al. (2015) credited their 100% participant retention to integrating CBPR tenets throughout the study (Kandula et al., 2015). Although only baseline data was provided in Sathe et al.’s health coaching intervention, of the 2726 individuals analyzed during baseline, only 50% (1359) completed full participation, with authors citing lack of time and not understanding the program or its benefits among the reasons for attrition (Sathe et al., 2013).
3.2. Characteristics of interventions
The structure of the community-based lifestyle interventions varied considerably (Table 4). Group-class formats of positive lifestyle behavior promotion were most popular (Islam et al., 2014, Kandula et al., 2015, Lim et al., 2019, Patel et al., 2017, Weber et al., 2020). Most interventions were between 12 and 16 weeks in duration, while some lasted 6 months (Islam et al., 2014, Lim et al., 2019) or 1 year (Sathe et al., 2013). Community settings, such as religious institutions, non-profit organization venues, local fitness facilities, and other convenient community spaces were common for intervention settings. Other studies had non-specific venues; Ganey et al. provided participants with pedometers to use throughout daily activities (Gany et al., 2014), while Sathe et al.’s health coaching intervention was largely phone or email based (Sathe et al., 2013).
Table 4.
Characteristics of interventions.
| Author (year) | Length of lifestyle Intervention | Intervention Setting | Physical Activity component | Diet/nutrition component | Other components | Cultural adaptation | Language adaptation | Technology involved |
|---|---|---|---|---|---|---|---|---|
| Kandula et al. (2015) | 16 weeks | Community-based non-profit organization | 1–1.5 h weekly group classes: exercise promotion. Group ‘Melas’: Yoga, aerobic exercise built on folk dances | 1–1.5 h group classes: reducing fat/salt, increasing healthy fruits/vegetables/ grains. Group ‘Melas’: healthy cooking with South Asian chef, cooking competition | 1–1.5 h weekly group classes: heart disease risk factors, weight control, stress and tension control | Sociocultural context and beliefs integrated into curriculum. Festive activities (‘Melas’) with culturally salient activities to reinforce healthy behaviors | Participants assigned to group classes based on language preference. Translation of study documents through community partners | Pedometer, Telephone-support |
| Patel et al. (2017) | 12 weeks | Hindu temple (‘mandir’) | 75-min weekly group session: increasing physical activity Some sessions also included: 20-min group physical activity |
75-min group session: increasing fruit/vegetable intake, barriers. Some sessions included: cooking demonstrations, food samples, grocery store tour, recipe makeover, pot-luck party | N/A | Existing curriculum (P2P) adapted and culturally tailored. Inspirational cultural messaging, visuals | Gujarati American facilitator orally translated materials, personalized with colloquialisms, customs, traditions | Pedometer, text messaging app, email |
| Islam et al. (2014) | 6 months | Community settings convenient to Sikh Asian Indian community | 2 h weekly group classes: Physical activity promotion, home-based exercises/activities | 2 h group classes: Identifying high salt/sugar foods, incorporating healthfulness in traditional Indian cooking, reading food labels | 2 h group weekly classes: General diabetes awareness, stress and mental health, access to healthcare | Existing curriculum (NHLBI, P2P, DPP, RH) culturally adapted through formative research. Sikh nutritionist created healthy recipes | All curriculum materials translated into Punjabi | Telephone-based follow-ups after sessions |
| Lim et al. (2019) | 6 months | Community settings (neighborhood gurdwara or education center) convenient to Sikh Asian Indian community | 2 h weekly group classes: Physical activity promotion | 2 h weekly group classes: improving nutrition, healthy Indian cooking | 2 h weekly group classes: General diabetes awareness, stress and mental health, access to healthcare | Culture adaptions further described in pilot paper (Islam et al., 2014): Existing curriculum (NHLBI, P2P, DPP, RH, other) culturally adapted. | All surveys administered in Punjabi by community health workers. Interventions lead by bilingual community health workers. | Telephone-based follow-ups after sessions |
| Gany et al. (2014) | 12 weeks | Remote | Daily pedometer usage | N/A | N/A | N/A | Multi-lingual research participants consented participants. Questionnaire administered in drivers’ preferred language | Pedometer |
| Kandula et al. (2016) | 16 weeks | Community-based non-profit organization, local fitness facility | 45 min (2+/wk) of moderate intensity exercise (Zumba, aerobics) | Optional group classes: culturally tailored healthy eating, reducing fat and salt intake | N/A | Community partners involved in development of culturally tailored strategies as part of intervention | Study staff participated in exercises for Hindi translation | Pedometer (Fitbit Zip wireless activity tracker) |
| Weber et al. (2020) | 16 weeks | Community locations near city | Group classes: physical activity awareness, traditional Indian dance exercises, group walks, work-out videos | Group classes: diet awareness | N/A | Existing curriculum (DPP) culturally adapted through focus group research. | N/A | Video-based exercise routines |
| Sathe et al. (2013) | 1 year | Remote | Health coach recommendations | Health coach recommendations | Health coach recommendations | Health coaches trained to integrated culturally tailored strategies | N/A | Phone, email-based coaching |
Most (seven) studies incorporated some form of cultural and linguistic tailoring to the intervention design. Formative, qualitative research with South Asian communities was explored by some studies to directly inform curriculum design and adaptation (Islam et al., 2014, Weber et al., 2020). Others involved community partners (Kandula et al., 2016); Islam et al. for instance recruited a Sikh nutrition expert to help create healthy recipes (Islam et al., 2014). Lim et al. expanded on the successes of Islam et al.’s pilot study and included many of the same cultural adaptions (Islam et al., 2014, Lim et al., 2019). The adaptation of existing chronic disease prevention curriculum was common, including the materials from the United States DPP (Islam et al., 2014, Lim et al., 2019), the National Diabetes Education Program’s Power to Prevent curriculum (P2P) (Patel et al., 2017, Islam et al., 2014, Lim et al., 2019), and the NHLBI Healthy Heart, Healthy Family curriculum (Islam et al., 2014, Lim et al., 2019). Linguistic tailoring was included in four of the five group-class based interventions through some form of oral or written translation of study materials (Kandula et al., 2015, Patel et al., 2017, Islam et al., 2014, Lim et al., 2019). Likewise, Gany et al.’s pedometer-based intervention had questionnaires administered in participants’ preferred language (Gany et al., 2014), and Kandula et al.’s exercise-based intervention had Hindi-speaking study staff participating in fitness classes for translation (Kandula et al., 2016).
While technology was not a significant component included in the interventions, pedometers were used in multiple interventions. Three studies incorporated pedometers as an explicit component of the intervention (Kandula et al., 2015, Kandula et al., 2016, Gany et al., 2014) while one primarily used the technology to track daily step counts (Patel et al., 2017). Patel et al. employed a smartphone app messaging software to allow participants to receive weekly reminders about mailing weekly logs and coming to weekly group sessions (Patel et al., 2017). Moreover, Sathe et al.’s health coaching intervention was largely phone and email based (Sathe et al., 2013), Islam et al. and Lim et al. incorporated telephone-based follow ups with participants after sessions (Islam et al., 2014, Lim et al., 2019, Kandula et al., 2015) included a telephone-based motivational interviewing component in their intervention (Kandula et al., 2015).
Physical activity was widely explored across the interventions. General promotion of physical activity strategies through group class formats (ranging from 60 min to 120 min on a weekly or biweekly basis) (Kandula et al., 2015, Patel et al., 2017, Islam et al., 2014, Lim et al., 2019) or targeted health coaching (Sathe et al., 2013) was common. However, more active exercise-based interventions were also explored. For example, Kandula et al. (2016) conducted a biweekly, 45-minute moderate-intensity Zumba and aerobics-based exercise intervention (Kandula et al. (2016)). Others incorporated exercise into aspects of the intervention; Kandula et al. (2015) conducted four group melas (a term used in South Asia for a gathering or festival) over the course of the year-long intervention involving yoga and folk-dance-based aerobic exercises (Kandula et al., 2015), Patel et al. incorporated group physical activities and demonstrations in some group classes (Patel et al., 2017), and Weber et al. incorporated traditional Indian dancing, work-out videos, and group walks (Weber et al., 2020).
Diet and nutrition were similarly explored in different culturally sensitive ways. The promotion of healthy eating practices (mainly focused on reducing unhealthy fats, sugars, and sodium while increasing fruit and vegetable intake) was common across the group-class based interventions (Islam et al., 2014, Kandula et al., 2015, Lim et al., 2019, Patel et al., 2017). Culturally-tailored cooking activities were also explored; Kandula et al. (2015) collaborated with a South Asian chef to teach healthy cooking and have cooking competitions (Kandula et al. (2015)), Islam et al. promoted techniques of incorporating healthfulness in traditional Indian cooking (Islam et al., 2014), and Patel et al. conducted cooking demonstrations, food sampling, grocery store tours, recipe makeovers, and pot-luck parties in some group sessions (Patel et al., 2017).
3.3. Effectiveness of interventions
The most common blood glucose outcome indicators assessed was A1C (measured as % and mmol/mol) (Kandula et al., 2015, Kandula et al., 2016, Patel et al., 2017). Two interventions used random plasma glucose (measured as mg/dL and mmol/L) (Gany et al., 2014, Sathe et al., 2013), two used 2 h fasting blood glucose (mg/dl) (Islam et al., 2014, Lim et al., 2019), while one used a general fasting plasma glucose test of an unspecified time length (mg/dl) (Kandula et al., 2015). While most studies assessed blood glucose measures on a continuous scale, Gany et al. conducted a categorical analysis based on subjects with a random plasma blood glucose of <200 mg/dL, 200–399 mg/dL, and ≥400 mg/dL (Gany et al., 2014). Unlike other studies, Weber et al. also assessed the number of individuals with normoglycemia, isolated impaired fasting glucose (iIFG), and isolated impaired glucose tolerance (iIGT) (Weber et al., 2020). Measures specifically targeting insulin sensitivity and resistance, such as QUICKI or HOMA, were not used.
Overall, most interventional studies demonstrated effectiveness in improving glucose and insulin indicators among participants. However, only four studies were conducted with the primary objective of diabetes prevention (Islam et al., 2014, Kandula et al., 2016, Patel et al., 2017), and only two studies conducting data collection included a follow-up period longer than immediately post-intervention, measuring at 2 months (Weber et al., 2020) or 6 months (Patel et al., 2017) after its completion. Four of the six studies statistically assessing post-intervention efficacy showed statistically significant reductions in blood glucose and A1C (Kandula et al., 2015, Patel et al., 2017, Islam et al., 2014, Lim et al., 2019). Kandula et al. (2015) observed a greater sex-adjusted A1c (%) decrease of 0.43 (p < 0.01) in the intervention group compared to the control group at the sixth month of the study period, although fasting glucose showed no statistically significant change (Kandula et al., 2015). Patel et al.’s 12-week study among participants with prediabetes similarly found the intervention participants reduce A1c from baseline (38.96 mmol/mol) to the 12-week postintervention assessment (37.00 mmol/mol) and to 24-week follow-up (or 12-weeks after the conclusion of the intervention, 36.54 mmol/mol), both of which were significant (p < 0.0005) compared to control (Patel et al., 2017). However, the small-scale, pilot nature of much of these studies limit the clinical meaningfulness of their observed effectiveness. Among the remaining two studies, Gany et al. observed improvement in individuals with <200 mg/dL glucose readings but it was not statistically significant (p = 0.32) (Gany et al., 2014), while Kandula et al. observed a slight but not clinically meaningful increase in A1c post-intervention (Kandula et al., 2016).
4. Discussion
Diabetes prevention among ethnic SAAs is a major public health concern. This review sought to systematically assess characteristics and effectiveness of community-based lifestyle interventions involving T2DM blood glucose and insulin indicators. We found that community-based lifestyle interventions targeting diabetes prevention remains relatively unexplored in ethnic SAA populations (reflected by the small sample of eight articles included in the review, all published within the last five years). While cultural and linguistic adaption was widely explored across the interventions, most studies employed traditional group-class intervention delivery formats targeting lifestyle behaviors based on standard curricula of chronic disease prevention. Assessing effectiveness of the interventions was largely confined to A1c, 2 h fasting blood glucose, and random plasma blood glucose indicators, and while some observed negative or no impact of the interventions in improving blood glucose indicators, the success observed in most studies suggest that community-based lifestyle interventions, indeed, may be a promising strategy to reduce the rising public health burden of T2DM among ethnic SAAs.
While most studies were derived from evidence-driven approaches and formative research or incorporated standard diabetes prevention curriculums, many tended to focus exclusively on either passive, group-class based formats of lifestyle behavior change promotion or more active, physical-activity based lifestyle behavior change activities. Multiple studies had significant active and passive components to the interventions (Kandula et al., 2015, Patel et al., 2017), while some intervention components were infrequently implemented or did not occur on a weekly or biweekly basis (Kandula et al., 2015, Patel et al., 2017), or some components were simply optional (Kandula et al., 2016). Different delivery methods of lifestyle interventions play a unique role in tackling the myriad complex barriers to healthy lifestyle behavior change, and the development of past comprehensive lifestyle interventions rely on active, passive, and individualized components to enhance efficacy (Schuette et al., 2017). Indeed, there are many lessons to be learned from multi-level health promotion intervention research in Europe; Andersen et al. conducted a randomized controlled trial among Pakistani immigrant men living in Norway that observed significant reductions in post-intervention insulin levels directly targeting constructs of Social Cognitive Theory (Andersen et al., 2013, Bandura, 2001). Notably, this single intervention included components observed across separate interventions in this review, including bi-weekly group exercises similar to Kandula et al. (2016), group lectures similar to that employed in multiple studies, individualized counseling similar to Sathe et al. (2013), and motivational phone-based contacts similar to Kandula et al. (2015). There is an opportunity for further research in the US to design similar multi-component interventions that incorporate passive (lecture-based), active (activity-based), and individualized (such as targeted counseling) health promotion and behavior change aspects.
Likewise, past utilization of theoretical lenses to understand the nuances of chronic diseases prevention among ethnic South Asians provides a starting point on behavior change constructs which may be particularly salient for diabetes prevention; Haider et al. for example employed the Social Cognitive Theory to predict exercise behavior among a cohort of largely first-generation South Asian college students in US and observed the construct of self-efficacy to be the only salient predictor of exercise behavior (Haider et al., 2012). Such findings suggest that efficacy-building may be particularly suited for this population, although further theory-based analysis on lifestyle behavior change among other ethnic SAA subgroups (e.g. second-generation immigrants, or older adults) is needed to provide more substantial insights to support intervention design.
The observed lack of studies involving second-generation South Asian migrants in the US reflects a broader gap in research on this subpopulation (Ali et al., in press) and represents a significant opportunity for future work. Indeed, while first-generation migrants still constitute a significant proportion of ethnic SAAs, there are approximately 800,000 second generation ethnic Indian Americans in the US, a number that is expected to significantly rise in the similar way as second and third generation South Asian communities have grown in the UK after waves of migration (Lopez et al., 2017, Migration Policy Institute, 2014). Second-generation South Asian migrants around the world have been observed to have significantly higher levels of educational attainment and linguistic integration, greater socio-economic advantage, more favorable attitudes towards physical activity, exercise more, and have less pressure to conform to traditional norms of diet and exercise (Bhatnagar et al., 2015, Grace et al., 2008, Tran et al., 2019). Indeed, the fact that almost all studies in the current sample did not specifically exclude second-generation or US-born ethnic SAAs suggests a need for greater sampling of second-generation South Asians (or potentially interventions specifically targeting the community) to provide a better understanding of the general applicability of community-based lifestyle interventions and provide implications for future work. Specifically, mixed-methods formative research among second-generation ethnic SAAs my identify certain foods or exercise behaviors more salient or culturally acceptable in this sub-population compared to first-generation migrants, which can then directly be integrated into diabetes prevention interventions targeting the community.
Studies showed mixed but generally positive improvements in blood glucose indicators post-intervention. The quality assessment conducted found that such findings were limited by small sample sizes, lack of comparison groups, and limited post-intervention follow up assessment. Likewise, these mixed results corroborate other community-based diabetes prevention-oriented lifestyle interventions in ethnic South Asian communities living in New Zealand (Rush et al., 2007) and Norway (Andersen et al., 2013) that similarly showed mixed results in improvements of diabetes indicators. The common utilization of A1c and random plasma glucose measures across the included studies can, at least in part, be explained by the ease and convenience of both tests for participants and researchers. Lack of clinical meaningfulness was also identified as an issue of concern with respect to some results (Kandula et al., 2016), further supporting the need for large-scale, rigorous intervention trials to assess efficacy. Indeed, as multiple studies in this review have shown, feasibility constraints of measurements such as fasting blood glucose, which require greater effort on the part of the participant, can be successfully overcome to ensure greater quality of the glucose and insulin outcomes. Thus, these mixed, yet generally positive, findings are compelling to support further high-quality intervention research in the field of T2DM prevention.
This study identified areas for further exploration of high-quality glucose and insulin outcome indicators in community-based lifestyle interventions. Most studies only employed a single blood glucose indicator, and evidence from included studies involving multiple indicators suggest that significant trends may not be reflected across all diabetes prevention outcomes (Kandula et al., 2015). Indeed, there is evidence highlighting the extent to which different blood glucose or insulin resistance outcomes may have uniquely salient roles in explaining diabetes prevalence across racial groups, including among ethnic South Asians (Sacks, 2011, Kanaya et al., 2014). Kananya et al.’s study on ethnic SAA diabetes prevalence observed that low β-cell function and insulin resistance was particularly high among South Asians and called for further research to identify the biological pathways and mechanisms behind diabetes progression among ethnic South Asians (Kanaya et al., 2014). Similarly, the measurement of A1c in distinguishing between individuals with pre-diabetes and those without diabetes (the main focus of diabetes prevention interventions) has been shown to be lower than its ability in distinguishing individuals with diabetes and individuals with pre-diabetes, compelling scholars to advocate the use of FPG or OGTT verification for individuals diagnosed as without diabetes or with pre-diabetes (Karakaya et al., 2014). Insulin resistance indicators (such as HOMA) were not assessed, and FPG and the Oral Glucose Tolerance Test (OGTT) – the traditional gold standards for diabetes diagnosis – were not employed (Sacks, 2011). Thus, there is a need for the incorporation of multiple, high-quality blood glucose and insulin indicators in further community-based diabetes prevention research in the US. To meet future aims, intervention studies in other settings provide insights on opportunities worthy of exploration in US settings; Rush et al.’s community-based lifestyle intervention among Asian Indians in New Zealand, for instance, assessed glucose (mmol/L), insulin (pmol/L), HOMA-B (%), and HOMA-S (%) (Rush et al., 2007).
4.1. Limitations
This review has some key limitations. First, this study relied on the precedent set by selected past literature to define ‘lifestyle interventions’ and operationalize the community-based lens in the search strategy (Satterfield et al., 2003). Second, this study excluded research focusing on the broader sub-group, ‘Asian Americans,’ a group which may have included significant numbers of South Asians, given the heterogeneity observed in Asian American subgroups and issues in generalizability between culturally targeted interventions among different Asian American communities. Finally, the review’s broad scope on general diabetes prevention meant that some studies did not explicitly exclude individuals with pre-existing diabetes which limits the interpretability of the findings (although among such studies, the percentage of individuals with diabetes was consistently small) – further research may focus more specifically on populations who exclusively do not meet criteria for diabetes or pre-diabetes.
5. Conclusion
Preventing T2DM among ethnic SAA communities remains a pressing public health concern in the US, and community-based lifestyle interventions present a promising opportunity to address this challenge. This review provides information on the potential efficacy and gaps pertaining to community-based lifestyle intervention design to inform further research and health promotion activities in this field. Based on the findings of this study, we have the following recommendations. First, there is a need for greater exploration of community-based lifestyle interventions with high quality diabetes indicators (such as fasting plasma glucose) in ethnic SAA communities. Second, further interventions should expand beyond traditional formats of group-class based lifestyle interventions and explore the use of innovative technologies and interventions integrated with passive, active, and individualized components. For example, the examination of telehealth and mhealth components (e.g. phone based or smartphone application based interventions) was limited, and the potential importance of such platforms has been further highlighted after the COVID-19 pandemic; further formative and interventional research using these technologies should be explored, and may provide insights on whether certain subsets of the population (e.g. second generation or young ethnic SAAs) may particularly benefit from interventions with these technologies. Likewise, expanding standard curricula for diabetes prevention by integrating group-based education, interactive activities (e.g. exercise sessions), and individualized one-on-one consultations with other culturally adaptive components (such as group melas or festivals) may enhance the applicability and effectiveness of interventions. Finally, there is a strong need to explore diabetes prevention among second generation SAAs through crucial phases of formative research and greater inclusion in diabetes prevention interventions. Indeed, fundamentally addressing diabetes prevention among ethnic SAAs requires both effective and sustainable interventions; to this extent, community-based lifestyle interventions culturally adapted to the preferences and norms of the ethnic SAA community have the strong potential to meet these needs.
CRediT authorship contribution statement
Shahmir H. Ali: Conceptualization, Methodology, Investigation, Writing - original draft. Supriya Misra: Methodology, Investigation, Writing - review & editing. Niyati Parekh: Writing - review & editing. Bridget Murphy: Investigation, Writing - review & editing. Ralph J. DiClemente: Conceptualization, Methodology, Investigation, Writing - review & editing, Supervision.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgement
We acknowledge the support of Ms. Dorice L. Vieira in providing assistance in search strategy design and implementation. No specific funding was recieved for this work.
References
- Alberti K.G.M.M., Zimmet P., Shaw J. International Diabetes Federation: a consensus on Type 2 diabetes prevention. Diabetic Med. 2007;24(5):451–463. doi: 10.1111/j.1464-5491.2007.02157.x. [DOI] [PubMed] [Google Scholar]
- Ali, S.H., DiClemente, R.J., Parkeh, N., in press. Changing the landscape of South Asian migrant health in the United States by advancing second-generation immigrant health research. Transl. Behav. Med. [DOI] [PubMed]
- American Diabetes Association Screening for type 2 diabetes. Diabetes Care. 2004;27(suppl. 1):s11–s14. doi: 10.2337/diacare.27.2007.s11. [DOI] [PubMed] [Google Scholar]
- American Diabetes Association Economic costs of diabetes in the U.S. in 2017. Diabetes Care. 2018;41(5):917–928. doi: 10.2337/dci18-0007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Andersen E. Intervention effects on physical activity and insulin levels in men of Pakistani origin living in Oslo: a randomised controlled trial. J. Immigr. Minor. Health. 2013;15(1):101–110. doi: 10.1007/s10903-012-9686-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ballotari P. Lifestyle-tailored interventions for South Asians with type 2 diabetes living in high-income countries: a systematic review. Acta Diabetol. 2017;54(8):785–794. doi: 10.1007/s00592-017-1008-8. [DOI] [PubMed] [Google Scholar]
- Bandura A. Social cognitive theory: an agentic perspective. Annu. Rev. Psychol. 2001;52:1–26. doi: 10.1146/annurev.psych.52.1.1. [DOI] [PubMed] [Google Scholar]
- Bhatnagar P., Shaw A., Foster C. Generational differences in the physical activity of UK South Asians: a systematic review. Int. J. Behav. Nutr. Phys. Act. 2015;12:96. doi: 10.1186/s12966-015-0255-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bhopal R.S. A four-stage model explaining the higher risk of Type 2 diabetes mellitus in South Asians compared with European populations. Diabetic Med. 2013;30(1):35–42. doi: 10.1111/dme.12016. [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. National Diabetes Statistics Report. Centers for Disease Control and Prevention 2017 [cited 2019 November 7]; Available from: <https://www.cdc.gov/diabetes/pdfs/data/statistics/national-diabetes-statistics-report.pdf>.
- Gany F. Supporting South Asian Taxi Drivers to Exercise through Pedometers (SSTEP) to decrease cardiovascular disease risk. J. Urban Health. 2014;91(3):463–476. doi: 10.1007/s11524-013-9858-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gov UK. People born outside the UK. UK Office for National Statistics, 2018 [cited 2019 November 6]; Available from: <https://www.ethnicity-facts-figures.service.gov.uk/uk-population-by-ethnicity/demographics/people-born-outside-the-uk/latest>.
- Grace C. Prevention of type 2 diabetes in British Bangladeshis: qualitative study of community, religious, and professional perspectives. BMJ. 2008;337 doi: 10.1136/bmj.a1931. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gutch M. Assessment of insulin sensitivity/resistance. Indian J. Endocrinol. Metab. 2015;19(1):160–164. doi: 10.4103/2230-8210.146874. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haider T., Sharma M., Bernard A. Using social cognitive theory to predict exercise behavior among South Asian college students. J. Commun. Med. Health Educ. 2012;2(6):2–6. [Google Scholar]
- Hu F.B. Globalization of diabetes. Diabetes Care. 2011;34(6):1249–1257. doi: 10.2337/dc11-0442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Institute of Medicine . National Academies Press; Washington DC: 2012. Community-Based Prevention, in an Integrated Framework for Assessing the Value of Community-Based Prevention; pp. 23–52. [PubMed] [Google Scholar]
- Islam N.S. Diabetes prevention in the New York City Sikh Asian Indian community: a pilot study. Int. J. Environ. Res. Public Health. 2014;11(5):5462–5486. doi: 10.3390/ijerph110505462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kanaya A.M. Understanding the high prevalence of diabetes in U.S. South Asians compared with four racial/ethnic groups: the MASALA and MESA studies. Diabetes Care. 2014;37(6):1621. doi: 10.2337/dc13-2656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kandula N.R. Translating a heart disease lifestyle intervention into the community: the South Asian Heart Lifestyle Intervention (SAHELI) study; a randomized control trial. BMC Public Health. 2015;15:1064. doi: 10.1186/s12889-015-2401-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kandula N.R. An exercise intervention for South Asian mothers with risk factors for diabetes. Transl. J. Am Coll. Sports Med. 2016;1(6):52–59. [PMC free article] [PubMed] [Google Scholar]
- Karakaya J. The performance of hemoglobin A1c against fasting plasma glucose and oral glucose tolerance test in detecting prediabetes and diabetes. J. Res. Med. Sci. 2014;19(11):1051–1057. [PMC free article] [PubMed] [Google Scholar]
- Khunti K. Educational interventions for migrant South Asians with Type 2 diabetes: a systematic review. Diabetic Med. 2008;25(8):985–992. doi: 10.1111/j.1464-5491.2008.02512.x. [DOI] [PubMed] [Google Scholar]
- Kramer M.K. Translating the Diabetes Prevention Program: a comprehensive model for prevention training and program delivery. Am. J. Prev. Med. 2009;37(6):505–511. doi: 10.1016/j.amepre.2009.07.020. [DOI] [PubMed] [Google Scholar]
- Lee J.W.R., Brancati F.L., Yeh H.-C. Trends in the prevalence of type 2 diabetes in Asians versus whites: results from the United States National Health Interview Survey, 1997–2008. Diabetes Care. 2011;34(2):353–357. doi: 10.2337/dc10-0746. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lim S. A culturally adapted diabetes prevention intervention in the New York City Sikh Asian Indian community leads to improvements in health behaviors and outcomes. Health Behav. Res. 2019;2(1):p. Art. 4. doi: 10.4148/2572-1836.1027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lopez, G.R., Neil G., Patten, Eileen. 2017. Key facts about Asian Americans, a diverse and growing population. Pew Research Center [cited 2019 November 6]; Available from: <https://www.pewresearch.org/fact-tank/2017/09/08/key-facts-about-asian-americans/>.
- Migration Policy Institute. The Indian Diaspora in the United States. Migration Policy Institute, 2014 [cited 2019 November 20]; Available from: <https://www.migrationpolicy.org/sites/default/files/publications/RAD-IndiaII-FINAL.pdf>.
- Moher D. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;6(7) doi: 10.1371/journal.pmed.1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Narayan, V. A Culturally Tailored Lifestyle Intervention to Prevent Diabetes in South Asians (SHAPE). ClinicalTrials.gov 2010 [cited 2019 November 21]; Available from: <https://clinicaltrials.gov/ct2/show/NCT01084928>.
- National Heart Lung and Blood Institute (NHLBI). Study Quality Assessment Tools. National Heart, Lung, and Blood Institute (NHLBI) n.d. [cited 2019 December 16]; Available from: <https://www.nhlbi.nih.gov/health-topics/study-quality-assessment-tools>.
- Navodia N. Culturally tailored self-management Interventions for South Asians with type 2 diabetes: a systematic review. Can. J. Diabetes. 2019;43(6):445–452. doi: 10.1016/j.jcjd.2019.04.010. [DOI] [PubMed] [Google Scholar]
- Nguyen T.H. Type 2 diabetes among Asian Americans: prevalence and prevention. World J Diabetes. 2015;6(4):543–547. doi: 10.4239/wjd.v6.i4.543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patel R.M. Effectiveness of a group-based culturally tailored lifestyle intervention program on changes in risk factors for type 2 diabetes among Asian Indians in the United States. J Diabetes Res. 2017;2017:2751980. doi: 10.1155/2017/2751980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Platonova A., Urso G. Asian Immigration to the European Union, United States and Canada: an initial comparison. J. Global Policy Gov. 2013;1(2):143–156. [Google Scholar]
- Rush E.C., Chandu V., Plank L.D. Reduction of abdominal fat and chronic disease factors by lifestyle change in migrant Asian Indians older than 50 years. Asia Pac. J. Clin. Nutr. 2007;16(4):671–676. [PubMed] [Google Scholar]
- Sacks D.B. A1C versus glucose testing: a comparison. Diabetes Care. 2011;34(2):518–523. doi: 10.2337/dc10-1546. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sathe A. A culturally specific health coaching program targeting cardiovascular disease risk in South Asians: rationale, design, and baseline data. Ethnic Dis. 2013;23(3):304–309. [PubMed] [Google Scholar]
- Satterfield D.W. Community-based lifestyle interventions to prevent type 2 diabetes. Diabetes Care. 2003;26(9):2643. doi: 10.2337/diacare.26.9.2643. [DOI] [PubMed] [Google Scholar]
- South Asian Americans Leading Together (SAALT). Health Care Issues Affecting South Asians in the United States South Asian Americans Leading Together (SAALT), 2009 [cited 2019 December 16]; Available from: <http://saalt.org/wp-content/uploads/2012/09/Health-Care-Issues-Affecting-South-Asians-in-the-United-States.pdf>.
- Schuette S.A.P. A scoping review of positive lifestyle and wellness interventions to inform the development of a comprehensive health promotion program: “HealthPro”. Am. J. Lifestyle Med. 2017;13(4):336–346. doi: 10.1177/1559827617704825. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tran V.C., Lee J., Huang T.J. Revisiting the Asian second-generation advantage. Ethnic Racial Stud. 2019;42(13):2248–2269. [Google Scholar]
- Weber M.B., Hennink M.M., Narayan K.M.V. Tailoring lifestyle programmes for diabetes prevention for US South Asians. Fam. Med. Community Health. 2020;8(2) doi: 10.1136/fmch-2019-000295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- WHO Expert Consultation Appropriate body-mass index for Asian populations and its implications for policy and intervention strategies. Lancet. 2004;363(9412):P157–P163. doi: 10.1016/S0140-6736(03)15268-3. [DOI] [PubMed] [Google Scholar]