Abstract
Acromioclavicular joint osteoarthritis is often a cause of shoulder pain. On the other hand, imaging frequently leads to such a diagnosis, especially in elderly patients, and some authors believe it to have a poor correlation with the clinical picture. It is, however, widely accepted that such a condition can be the cause of rotator cuff impingement. In the case of shoulder pain, it is important to distinguish between symptomatic acromioclavicular osteoarthritis and other causes, especially rotator cuff pathology, which is more common. Sometimes, the clinical picture does not allow for differential diagnosis; in these cases, the injection of a local anesthetic into the acromioclavicular joint or into the subacromial bursa can be of great help. Ultrasonography can easily detect acromioclavicular osteoarthritis and rotator cuff pathology, and it is highly effective in guiding the articular or bursal injection of a local anesthetic to assess the origin of the pain. In addition, in conservative therapy, ultrasonography can guide the articular or bursal injection of corticosteroids and hyaluronic acid.
Keywords: Acromioclavicular joint, Osteoarthritis, Shoulder, Ultrasonography
Introduction
The acromioclavicular (AC) joint is a diarthrodial joint with a limited range of motion, and it is the only articular connection between the axial skeleton and the scapula; osteoarthritis is by far its most common pathology [1]. Some authors [2] point out that there is a poor correlation between imaging evidence of AC osteoarthritis and clinical evidence. The diagnosis of osteoarthritis by imaging (not only with ultrasonography but also with magnetic resonance imaging (MRI), which is the most powerful diagnostic tool for AC osteoarthritis [3]) is much more common than the clinical picture of shoulder pain, especially in elderly patients. Other authors [4], however, report that AC osteoarthritis is a frequently overlooked cause of shoulder pain.
AC joint abnormalities, whether congenital (i.e., os acromiale or hook-shaped acromion) or acquired (i.e., osteoarthritis or post-traumatic changes), have also been widely and unanimously recognized as an important cause of rotator cuff (RC) superior impingement syndrome.
Ultrasonography is considered a fully reliable imaging approach for studying RC pathology, and it can also easily and quickly detect some abnormalities related to AC degenerative pathology [even though X-ray, computed tomography (CT), and magnetic resonance imaging provide a more precise and complete assessment of AC joint pathology]. In fact, evaluation of the AC joint is universally considered to be a part of the standard ultrasonographic examination of the shoulder [5].
We cannot disregard, however, the central role that clinical examination plays in assessing shoulder pain, considering the poor correlation between imaging-detected AC osteoarthritis and clinical symptoms.
Obtaining a correct differential diagnosis for a painful shoulder can be difficult in the case of AC osteoarthritis. Nevertheless, it is crucial, as such a differential diagnosis leads to different therapy choices and prognoses. In this regard, ultrasonography (US) can play a vital role as practical and effective imaging guidance for the selective articular injection of local anesthetics to reach a correct diagnosis, in combination with the use of corticosteroids and hyaluronic acid in conservative therapy. On the other hand, the US can also provide reliable imaging guidance for intrabursal injection of steroids and anesthetics in case of correspondence between pain and subacromial impingement syndrome.
Anatomy and biomechanics
The AC joint is a diarthrodial joint: the distal clavicle has a convex surface that articulates with the slightly convex surface of the acromion facet, which is oriented anteromedially toward the distal clavicle [4]. The facets are covered with hyaline cartilage; between them, there is a fibrocartilage disk that is somewhat similar to the meniscus of the knee. Degenerative changes are a natural process, and in early adulthood, the fibrocartilage disk is degenerated [1], with only fibrous remnants left.
The joint is surrounded by a fibrous capsule lined with synovial tissue, and it is reinforced by different ligaments: the AC ligaments, the coracoacromial (CA) ligament, and the coracoclavicular (CC) ligaments. The joint is also stabilized by dynamic stabilizers, such as the deltoid muscle anteriorly and the trapezius muscle posteriorly [6].
The superior and inferior AC ligaments, the former being thicker than the latter (Fig. 1), offer resistance to anterior–posterior forces. The inferior surface of the capsuloligamentous complex is in direct contact with the subacromial bursa, and this fact is strictly related to the important role that AC osteoarthritic joint changes play in RC tendinopathy [7].
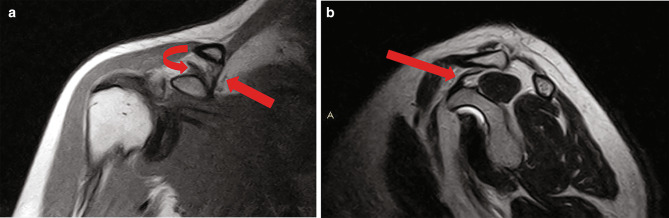
Fig. 1.

Coronal T1 MRI scan. The joint capsule is reinforced by the two acromioclavicular ligaments, the superior and the inferior one, the former being thicker. A fibrocartilage disk separates the two bone extremities
The CC ligaments are the conoid ligament, oriented in an anterior–posterior direction and located more medially, and the trapezoid ligament, oriented in a medial–lateral direction (Fig. 2a, b). The trapezoid ligament represents the main restraint to compression of the joint [1].
Fig. 2.
Coronal T1 MRI scan. a The conoid ligament (arrow) is the more medial component of the coracoid-clavicular ligament. The trapezoid ligament (curved arrow) has a medial to lateral direction and is the main restraint to the compression of the joint. b Sagittal T2 MRI scan. The conoid ligament has a posterior to anterior direction (arrow)
The CA ligament blends inferiorly with the inferior AC ligament and reinforces it. It forms an arch structure, and pathology at this location can cause narrowing of the supraspinatus outlet, potentially leading to impingement syndrome (Fig. 3) [8].
Fig. 3.
Oblique anterior US scan. The coracoacromial ligament (arrows) runs between the two bones forming an arch just superficially to the supraspinatus, being a possible cause of impingement at the supraspinatus outlet
Although the AC joint connects the scapula with the axial skeleton through the clavicle and the clavicle can rotate 45° around its axis, the actual motion of the joint is restricted between 5° and 8° [9]. The possible motions of the joint are anterior to posterior gliding of the scapula on the clavicle, abduction–adduction of the scapula on the clavicle, and rotation along the long axis of the clavicle [4, 10]. The wider range of motions takes place at the sternoclavicular joint.
It is widely accepted that the morphologic classification of the acromion according to Bigliani (type 1: flat; type 2: concave; type 3: hooked; type 4: convex downwards) can play a significant role in the pathogenesis of RC impingement syndrome.
Os acromiale, an ossicle which results from an unfused accessory center of ossification of the anterior portion of the acromion and that shows a prevalence in the general population of about 8% [11], is reported to be a potential cause of superior impingement, with the ossicle being pulled downwards by the deltoid muscle or because of bone spurs on its lower margin [6].
Acromioclavicular osteoarthritis: clinical and imaging evaluation
although AC osteoarthritis is much less common than degenerative pathology at other locations, such as the knee or the hip, it is much more frequent than glenohumeral osteoarthritis. According to a study [12], 54–57% of elderly patients had X-ray evidence of degenerative changes of the AC joint. On the other hand, clinically relevant AC osteoarthritis is less common [1], although it is more frequently related to other more common pathologies, such as RC superior impingement syndrome. The topic is somewhat controversial though: one study [2] states that there appears to be no real correlation between MRI signs of osteoarthritis and clinical findings; another study [13], however, concludes that the MRI finding of capsule hypertrophy strongly correlates with a good clinical outcome of pain relief after intra-articular injection.
Primary osteoarthritis strongly correlates with age, and the degenerative process begins in early adulthood. Oblique orientation or incongruencies of the facets along with disk degeneration can worsen the usual stresses, accelerating degenerative changes [14].
The most common pattern of degenerative change is the elongation of the acromial side in the sagittal plane; it has been reported that anteroposterior elongation is accompanied by reduced proliferation of osteophytes in the superoinferior plane. The distal clavicle commonly shows broadening and rounding [15].
Secondary osteoarthritis, mainly following traumas such as joint sprains (Fig. 4a, b) or distal clavicular fractures (Fig. 5), appears to be even more common than primary osteoarthritis [1].
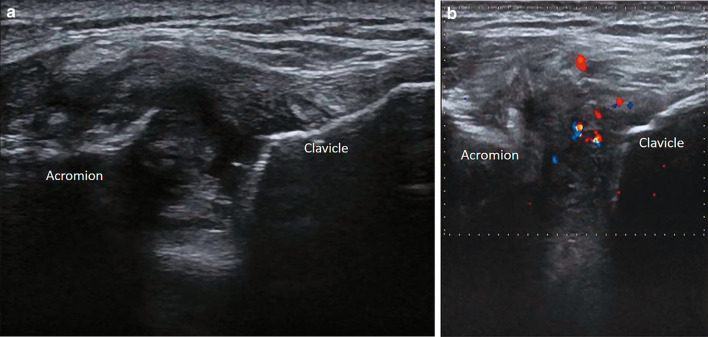
Fig. 4.
US coronal scan. a Synovial hypertrophy and osteophytes in osteoarthritis secondary to acromioclavicular dislocation. b Color Doppler shows hypervascularity of the synovium
Fig. 5.

X-ray study, AP standard view. In secondary acromioclavicular osteoarthritis after distal clavicle fracture, the usual signs of degenerative disease (joint space narrowing, sclerosis, and osteophytes) are easily depicted by X-ray imaging
The clinical picture is represented by aching at the anterior/superior aspect of the shoulder, sometimes radiating to the base of the neck/trapezius muscle. Pain is elicited by everyday movements or sports activities involving overhead or cross-body motions. Local tenderness can be caused by palpation of the AC joint. Such a range of symptoms is not specific though and is also reported in cervical spine pathologies and RC impingement syndromes, which are much more common causes of shoulder pain. A differential diagnosis may be made with the help of direct intra-articular injection of anesthetics.
Imaging evaluation of the AC joint starts with an X-ray. The joint can be studied with normal AP views of the shoulder, even though the best option according to the literature is the Zanca view (a cephalad tilt of 10–15° with 50% exposure reduction compared to the standard AP view of the shoulder). Imaging findings are those typical of degenerative diseases: sclerosis, osteophytes, subchondral cysts, and joint space narrowing. CT depicts more precisely the same bone degenerative changes as seen with X-ray, while MRI is more valuable for the evaluation of alterations in capsuloligamentous structures, bone edema, and abnormalities in surrounding soft tissues (Fig. 6) (i.e., bursal effusion or tendon pathology) [3].
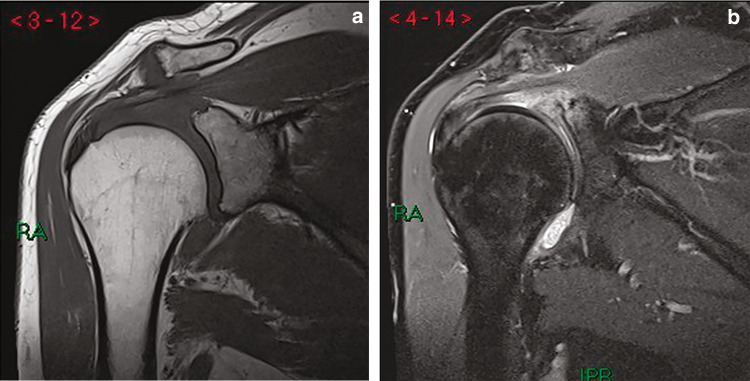
Fig. 6.
Coronal T1 MRI scan. Joint space narrowing, superior and inferior osteophytes, and capsular hypertrophy are MR landmarks of acromioclavicular osteoarthritis. The coronal PD FS MRI scan shows bone edema of the articular extremities; underlying supraspinatus tendinopathy and subtle bursal effusion are also present. The axillary pouch of the glenohumeral capsule is also distended by effusion
Ultrasonographic findings
The AC joint can be evaluated only partially by the US, but it ought to be a part of the routine shoulder US examination (Bianchi and Martinoli, p. 232), as AC joint osteoarthritis can sometimes mimic rotator cuff tendinopathy, and it can be a cause of anterosuperior impingement of the shoulder. AC osteophytes are found in 50% of patients with rotator cuff tears and in 14% of patients without rotator cuff tears [16, 17].
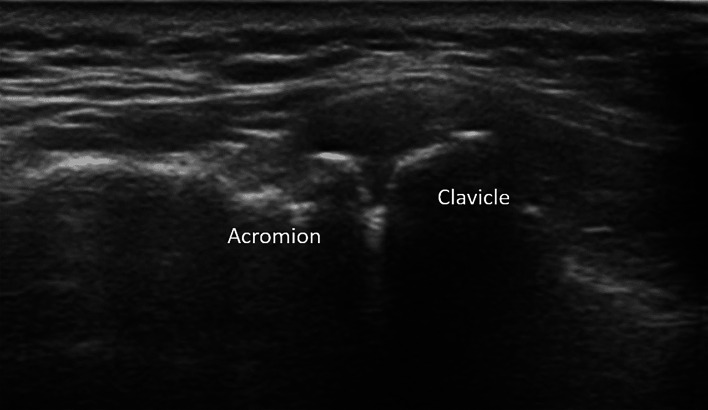
By positioning the linear high-frequency probe on a coronal plane at the level of the joint, it is possible to assess the two articular extremities of the acromion and the clavicle. The superior AC ligament is clearly seen as a band arch-like echoic structure overlying the bones (Fig. 7); underneath it, the joint space can vary in size and echogenicity with movements. Only in younger patients can the fibrocartilaginous disk sometimes be seen as a thin hyperechoic structure between the articular extremities.
Fig. 7.
US coronal scan. The superior acromioclavicular ligament can be seen as an arch-like thickening of the capsule that connects the two articular bone extremities
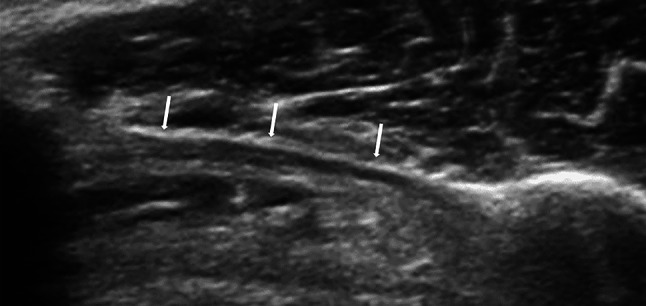
Os acromiale (Fig. 8) is an anatomical variant that can be detected by the US as a discontinuity of the distal acromial bone surface. Recognizing this discontinuity is important as it can be a cause of anterosuperior RC impingement [11].
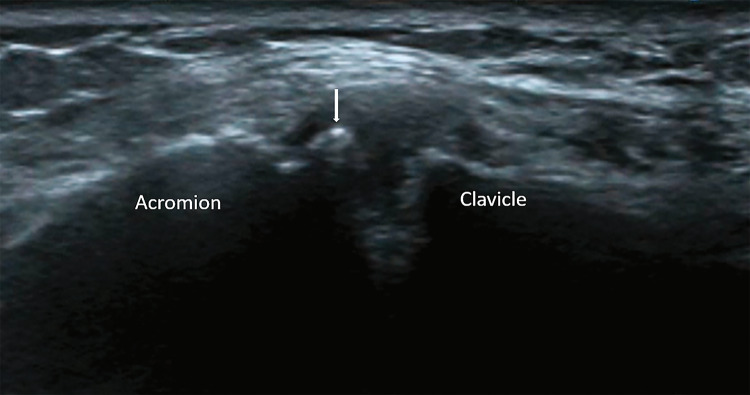
Fig. 8.
US coronal scan. Os acromiale (arrow) is a developmental alteration that results from an unfused accessory center of ossification of the anterior portion of the acromion and is reported to be a potential cause of superior impingement. The US shows a discontinuity in the superior aspect of the articular end of the acromion
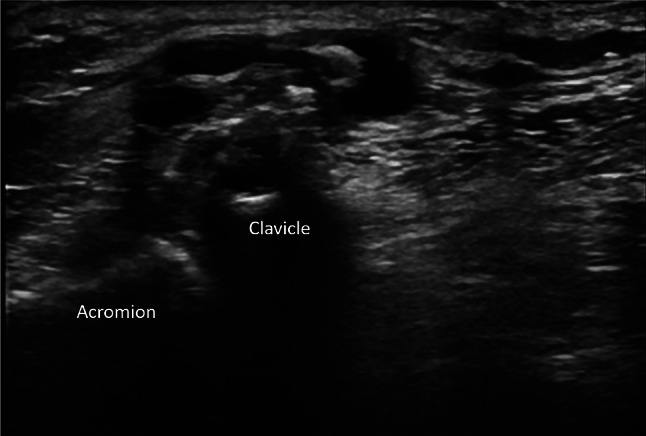
In the case of AC joint osteoarthritis, the US can assess superficial bone irregularities and osteophytes, capsular hypertrophy, joint space narrowing (Fig. 9), and joint effusion or synovial hypertrophy.
Fig. 9.
US coronal scan. Joint space narrowing, superficial osteophytes, and capsular hypertrophy are typical US signs of acromioclavicular osteoarthritis
Bilateral evaluation of the AC joint is always advisable to assess capsular hypertrophy and joint space narrowing with higher sensitivity [16].
The US findings at the AC joint always need to be correlated with rotator cuff and bursal findings and with the clinical picture. Shoulder pain related to AC joint osteoarthritis can be diagnosed only in the absence of RC abnormalities and with a clinical picture consistent with such a condition. On the other hand, as we have previously stated, the US signs of acromioclavicular osteoarthritis and rotator cuff or bursal pathology are frequently associated (Figs. 9, 10); in this case, the joint injection test can be a highly valuable diagnostic tool [1, 4]. The US can also show other rare causes of anterior shoulder pain, such as pathologies involving the pectoralis major tendon [18, 19].
Fig. 10.

Bursal effusion in the same patient as in (Fig. 9), possibly secondary to acromioclavicular osteoarthritis
Another not uncommon US finding is an AC joint cyst. The pathogenesis of these cysts is still debated [20, 21]. It is, however, more commonly related to RC full-thickness tears. The tendon tear allows the humeral head to migrate cranially and damage the inferior AC joint capsule, creating a connection between the glenohumeral joint and the AC joint. This, however, does not explain the presence of mucoid content and fibrous walls that are sometimes found [19], and some authors, therefore, suggest instability of the joint as a pathogenetic factor.
These cysts can have septa or echogenic-solid textures, which can be explained by the presence of synovial tissue or pyrophosphate calcium deposits (Fig. 11); it is important to know this to avoid performing a needle biopsy of such a benign lesion [16].
Fig. 11.
US coronal scan. An acromioclavicular ganglion in a patient with acromioclavicular osteoarthritis
Articular injection diagnosis
Injection of a local anesthetic into the AC joint can greatly assist in confirming the cause of shoulder pain if imaging is consistent with AC joint degenerative changes.
The commonly used anesthetics are lidocaine (1 or 2%) and mepivacaine or bupivacaine (0.5–1%) hydrochloride. Normally 1–2 ml of the anesthetic is injected into the joint using a short thin needle (23G); if after a few minutes the patient reports significant pain relief, the AC origin of the shoulder pain is confirmed.
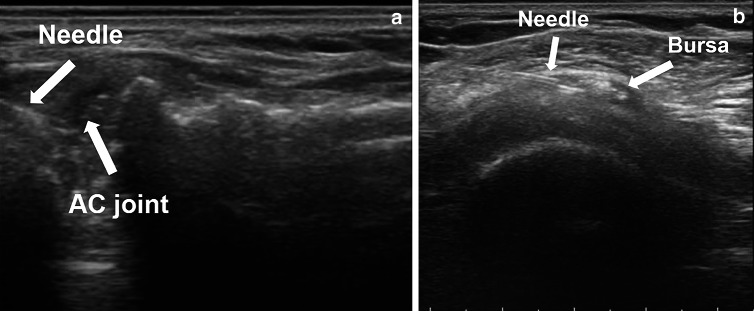
The articular injection can be easily performed under US guidance. Even though the AC joint is superficial, given its oblique orientation and tight capsule, the injection of an anesthetic is somewhat difficult. US guidance allows good visualization of the superior aspect of the joint. While holding the probe on a coronal plane, keeping the joint line on the lateral third of the view, the needle access is just lateral to the probe. Keeping the needle oblique, with a 25–30° angle to the probe, which can be evaluated and adjusted by the direct visualization of the needle itself thanks to US guidance, the injection of the anesthetic into the correct intra-articular site can be performed and confirmed by real-time imaging (Fig. 12).
Fig. 12.
US scan of AC joint injection. a The needle is visible as a thin hyperechoic line extending into the AC joint space. b US scan of subacromial bursa injection. The needle (arrow) is visible as three parallel hyperechoic lines with the tip inside the subacromial bursa. Hyperechoic calcifications are visible within the bursa
If no pain relief is reported, intrabursal injection of an anesthetic can be useful, with rotator cuff disease being the most common differential diagnosis for shoulder pain; once again, the US can be very helpful in guiding the needle in the correct intrabursal site. In this case, the probe lies on an axial plane, the patient is in a supine position, and the same kind of needle used for AC joint injection is used to inject the bursa, always keeping an oblique direction entering just lateral to the probe. By injecting small amounts of the anesthetic, the correct intrabursal positioning of the needle can be easily demonstrated by the gradual distention of the bursa itself.
Conservative therapy and US articular injection guidance
Conservative therapy is the first option for shoulder pain caused by AC joint osteoarthritis, while surgical therapy, whether open or arthroscopic, is nowadays reserved only for patients who do not improve with conservative therapy [4].
Conservative therapy is based on the intra-articular injection of corticosteroids and hyaluronic acid, physical therapy, and avoidance of all everyday movements that stress the joint. Physical therapy, however, has little effect because of the limited range of motion of the AC joint [4].
Although osteoarthritis is not considered an inflammatory disease, it has been proven by synovial biopsies that synovial hyperplasia and mononuclear cell infiltrates are present at a certain point during the course of the disease [20]. Corticosteroids inhibit the recruiting of macrophages and neutrophils in the joint and reduce vasodilation and capillary permeability and therefore exudation. They also inhibit the release of cytokines, which are thought to play a role in cartilage damage by releasing collagenases [21–23]. Triamcinolone and methylprednisolone are the most used corticosteroids for articular injection.
Synovial hyaluronic acid levels are found to be decreased in patients with advanced degenerative joint disease, and this is the rationale on which viscosupplementation is based. In addition, hyaluronic acid has been found to prevent the escaping of proteoglycans from the cartilage to the articular space and is useful as a barrier against inflammatory cells. Hyaluronic acid thus plays the double role of viscosupplementation and a long-lasting anti-inflammatory substance [24, 25]. Articular hyaluronic acid injection is approved by the FDA only for knee osteoarthritis, but its off-label use for other joints is widespread, as is shown by the large number of studies published in the scientific literature.
US is a reliable and simple guidance method for the injection of such a tight and obliquely oriented joint as the AC joint. Therapy generally consists of a cycle of three injections spaced three to 4 weeks apart. With each injection, corticosteroids (20–40 mg methylprednisolone) and hyaluronic acid (medium or high molecular weight, generally 1 ml only, because of the scarce distensibility and tightness of the capsule) are injected into the joint, preceded by an injection of 1 ml of a local anesthetic. Extreme care must be taken to perform each injection in conditions of sterility to avoid complications such as infective arthritis. The patient lies supine, and a short needle (21–23 G) is inserted into the joint capsule, entering just laterally to the US probe with an oblique (25–30°) approach.
If the US also shows signs of bursitis or tendon abnormalities, a second injection of corticosteroids and hyaluronic acid can be performed in the subacromial bursa [26], especially in the absence of a certain diagnosis of the cause of the pain. The patient lies in the same position as for the injection of the AC joint, the probe is moved on an axial-oblique plane just below the acromion, and the needle enters just laterally to the probe with an oblique approach until it reaches the bursa. The bursal localization is proven by the bursal distention obtained with the injection of a small amount of a local anesthetic prior to the injection of corticosteroids (20–40 mg methylprednisolone) and hyaluronic acid (1–2 ml of medium molecular weight hyaluronic acid) [27, 28].
The effects of this therapy are variable, but it is found to be generally effective for a period that can stretch from weeks to months. Normally, a cycle of three injections can be repeated every 6 months. In the absence of a certain degree of shoulder pain relief and an increase in the range of movements, the surgical option must be taken into consideration.
Discussion
AC osteoarthritis is a common imaging finding, especially in elderly patients, and can sometimes be an overlooked cause of shoulder pain. On the other hand, it can also cause subacromial impingement and therefore can be associated with rotator cuff tendon lesions and subacromial bursal inflammation.
X-ray and MRI give the most complete imaging picture of AC anatomy and pathology, but given the large number of US examinations performed to investigate shoulder pain, the AC joint must be included in the routine evaluation of the shoulder. US can, in fact, easily detect signs of AC osteoarthritis. All imaging findings need to be matched with clinical assessment, and in the case of uncertain differential diagnosis between AC osteoarthritis and rotator cuff pathology, articular injection of a local anesthetic can help guide the clinician toward the more likely cause of the shoulder pain. US guidance is nowadays an extremely helpful tool for performing such a diagnostic test easily and effectively.
US guidance is also of great help in the articular injection of corticosteroids and hyaluronic acid as the basis of the conservative treatment of symptomatic AC osteoarthritis. In the case of the coexistence of rotator cuff abnormalities and AC osteoarthritis signs, articular AC and subacromial bursal injection of corticosteroids and hyaluronic acid can be performed in the same session, avoiding the accidental injection of corticosteroids in the underlying tendons.
Compliance with ethical standards
Conflicts of interest
The authors declare that they have no conflict of interest.
Ethics approval
All procedures performed in the studies were in accordance to the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. This article does not contain any studies with human participants or animals performed by any of the authors.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Shaffer BS. Painful conditions of the acromioclavicular joint. J Am Acad Orthop Surg. 1999;7(3):176–188. doi: 10.5435/00124635-199905000-00004. [DOI] [PubMed] [Google Scholar]
- 2.Jordan LK, Kenter K, Griffiths HL. Relationship between MRI and clinical findings in the acromioclavicular joint. Skeletal Radiol. 2002;31(9):516–521. doi: 10.1007/s00256-002-0530-z. [DOI] [PubMed] [Google Scholar]
- 3.de Abreu MR, Chung CB, Wesselly M, Jin-Kim H, Resnick D. Acromioclavicular joint osteoarthritis: comparison of findings derived from MR imaging and conventional radiography. Clin Imaging. 2005;29(4):273–277. doi: 10.1016/j.clinimag.2004.11.021. [DOI] [PubMed] [Google Scholar]
- 4.Buttaci CJ, Stitik TP, Yonclas PP, Foye PM. Osteoarthritis of the acromio-clavicular joint: a review of anatomy, biomechanics, diagnosis and treatment. Am J Phys Med Rehabil. 2004;83(10):791–797. doi: 10.1097/01.PHM.0000140804.46346.93. [DOI] [PubMed] [Google Scholar]
- 5.Beggs I, Bianchi S, et al. Musculoskeletal ultrasound technical guidelines – shoulder. Eur SocMusculoskelet Radiol. 2010;20:91–156. [Google Scholar]
- 6.Ha AS, Petscavage-Thomas JM, Tagoylo GH. Acromioclavicular joint: the other joint in the shoulder. AJR Am J Roentgenol. 2014;202(2):375–385. doi: 10.2214/AJR.13.11460. [DOI] [PubMed] [Google Scholar]
- 7.Chen AL, Rokito AS, Zuckerman JD. The role of the acromioclavicular joint in impingement syndrome. Clin Sports Med. 2003;22:343–358. doi: 10.1016/S0278-5919(03)00015-2. [DOI] [PubMed] [Google Scholar]
- 8.Mcdonald S, Hopper MA. Acromioclavicular joint disease. Semin Musculoskelet Radiol. 2015;19(3):300–306. doi: 10.1055/s-0035-1549323. [DOI] [PubMed] [Google Scholar]
- 9.Rockwood CA, Jr, Williams GR, Young DC. Injuries to the acromioclavicular joint. In: Rockwood CA Jr, Bucholz RW, Green DP, Heckman JD, editors. Fractures in Adults. 4. Philadelphia: Lippincott-Raven; 1996. pp. 1341–1413. [Google Scholar]
- 10.Worcester JN, Jr, Green DP. Osteoarthritis of the acromioclavicular joint. Clin Orthop. 1968;58:69–73. doi: 10.1097/00003086-196805000-00010. [DOI] [PubMed] [Google Scholar]
- 11.Sammarco VJ. Os acromiale: frequency, anatomy and clinical implications. J Bone Joint Surg Am. 2000;82:394–400. doi: 10.2106/00004623-200003000-00010. [DOI] [PubMed] [Google Scholar]
- 12.Horvat F, Kery L. Degenerative deformations of the acromioclavicular joint in the elderly. Arch Gerontol Geriatr. 1984;3:259–265. doi: 10.1016/0167-4943(84)90027-X. [DOI] [PubMed] [Google Scholar]
- 13.Strobel K, Pfirrmann CW, Zanetti M, Nagy L, Hodler J. MRI features of the acromioclavicular joint that predict pain relief from intraarticular injection. AJR Am J Roentgenol. 2003;181(3):755–760. doi: 10.2214/ajr.181.3.1810755. [DOI] [PubMed] [Google Scholar]
- 14.Mall NA, Foley E, Chalmers PN, Cole BJ, Romeo AA, Bach BR., Jr Degenerative joint disease of the acromioclavicular joint: a review. Am J Sports Med. 2014;41(11):2684–2692. doi: 10.1177/0363546513485359. [DOI] [PubMed] [Google Scholar]
- 15.Edelson JG. Patterns of degenerative change in the acromioclavicular joint. J Bone Joint Surg. 1996;78:242–243. doi: 10.1302/0301-620X.78B2.0780242. [DOI] [PubMed] [Google Scholar]
- 16.Bianchi S, Martinoli C. Shoulder. In: Bianchi S, Martinoli C, editors. Ultrasound of musculoskeletal system. Heidelberg: Springer; 2007. p. 232. [Google Scholar]
- 17.Petersson CJ, Gentz CF. Ruptures of the supraspinatus tendon. The significance of distally pointing acromioclavicular osteophytes. Clin Orthop Relat Res. 1983;174:143–148. [PubMed] [Google Scholar]
- 18.Ruiz Santiago F, Ruiz Tristán A, Butani P. Anomalous insertion of the pectoralis minor tendon at the greater tuberosity. J Ultrasound. 2019;11:1–3. doi: 10.1007/s40477-019-00414-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Draghi F, Cocco G, Lomoro P, Bortolotto C, Schiavone C. Non-rotator cuff calcific tendinopathy: ultrasonographic diagnosis and treatment. J Ultrasound. 2019;13:12. doi: 10.1007/s40477-019-00393-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Craig EV. The acromioclavicular joint cyst. An unusual presentation of a rotator cuff tear. Clin Orthop Relat Res. 1986;202:189–192. [PubMed] [Google Scholar]
- 21.Montet X, Zamorani-Bianchi MP, Mehdizade A, Martinoli C, Bianchi S. Intramuscular ganglion arising from the acromioclavicular joint. Clin Imaging. 2004;28(2):109–112. doi: 10.1016/S0899-7071(03)00104-9. [DOI] [PubMed] [Google Scholar]
- 22.Haraoui B, Pelletier JP, Cloutier JM, et al. Synovial membrane histology and immunopathology in rheumatoid arthritis and osteoarthritis. Arthritis Rheum. 1991;34:153–163. doi: 10.1002/art.1780340205. [DOI] [PubMed] [Google Scholar]
- 23.Weitoft T, Forsberg C. Importance of immobilization after intraarticular glucocorticoid treatment for elbow synovitis: a randomized controlled study. Arthritis Care Res (Hoboken) 2010;62(5):735–737. doi: 10.1002/acr.20039. [DOI] [PubMed] [Google Scholar]
- 24.Eyigor C, Eyigor S, Kivilcim Korkmaz O. Are intra-articular corticosteroid injections better than conventional TENS in treatment of rotator cuff tendinitis in the short run? A randomized study. Eur J Phys Rehabil Med. 2010;46(3):315–324. [PubMed] [Google Scholar]
- 25.Habib GS, Saliba W, Nashashibi M. Local effects of intra-articular corticosteroids. Clin Rheumatol. 2010;29(4):47–56. doi: 10.1007/s10067-009-1357-y. [DOI] [PubMed] [Google Scholar]
- 26.Balazs E. The physical properties of synovial fluid and the specific role of hyaluronic acid. In: Helfet AJ, editor. Disorders of the knee. Philadelphia: JB Lippincott; 1982. pp. 61–74. [Google Scholar]
- 27.Smith MM, Ghosh P. The synthesis of hyaluronic acid by human synovial fibroblasts is influenced by the nature of the hyaluronate in the extracellular environment. Rheumatol Int. 1987;7(3):113–122. doi: 10.1007/BF00270463. [DOI] [PubMed] [Google Scholar]
- 28.Byun SD, Park DH, Choi WD, Lee ZI. Subacromial bursa injection of hyaluronate with steroid in patients with peri-articular shoulder disorders. Ann Rehabil Med. 2011;35(5):664–672. doi: 10.5535/arm.2011.35.5.664. [DOI] [PMC free article] [PubMed] [Google Scholar]