Abstract
Groin pain can be caused by a myriad of pathologies. Abnormalities of the rectus femoris are a very rare cause of groin pain; calcific tendinopathy of the direct head is particularly so, with only two case reports in the literature. We report the first case of calcific tendinopathy of the direct head of the rectus femoris that was treated effectively with ultrasound-guided percutaneous irrigation of calcific tendinopathy (USPICT). The anatomy of the rectus femoris and the technique for US-PICT of the rectus femoris are also described.
Keywords: Calcific, Tendinopathy, Rectus, Femoris, Percutaneous, Irrigation
Introduction
Groin pain can be caused by a myriad of pathologies. Calcific tendinopathy of the rectus femoris tendon is a relatively rare cause of groin pain. We report a case of calcific tendinopathy of the direct head of rectus femoris in a previously fit and well 40-year-old patient, which was treated effectively with US-PICT.
Case report
A normally fit and well 40-year-old female presented with a one-year history of right groin pain aggravated by hip flexion. There was no significant medical or medication history. The onset of pain was gradual and there was no history of preceding trauma.
Imaging
Imaging was performed to evaluate the cause of the patient’s pain. Initial radiographs of the pelvis were unremarkable. A MRI of pelvis and an MR arthrogram of the right hip were performed, but did not reveal any abnormality apart from subtle oedema in relation to the direct head of rectus femoris (Fig. 1). There was no labral tear, and the iliopsoas, gluteal and hamstring tendons were normal, with no tendinopathy or tear identified. No iliopsoas, subgluteal or trochanteric bursitis was demonstrated. There was no evidence of an inguinal or femoral hernia. Ultrasound of right hip identified a 2 cm focus of amorphous calcification within the direct head of the rectus femoris, close to its origin from the anterior inferior iliac spine (AIIS) (Fig. 2). The tendon was intact, with no tear identified. There was no increased signal on Doppler. The indirect head of the rectus femoris iliopsoas and adductor tendons were normal. A CT of the pelvis was performed, and demonstrated normal morphology of the AIIS, with no evidence of prior avulsion injury. An irregular focus of calcification was noted in the direct head of rectus femoris, in keeping with calcific tendinopathy (Fig. 3).
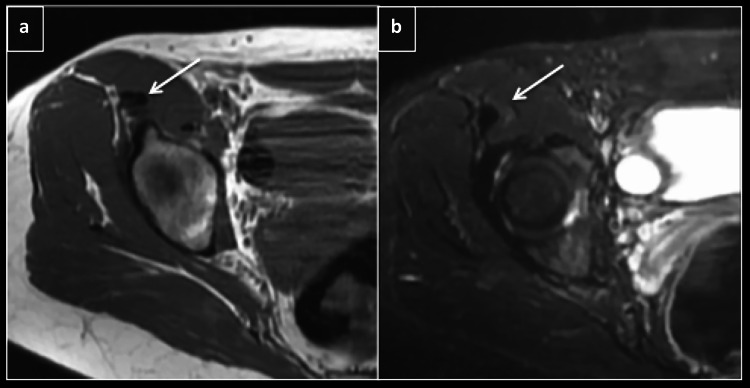
Fig. 1.
Axial T1 (a) and STIR (b) showing direct head of rectus femoris (arrow) with subtle edema
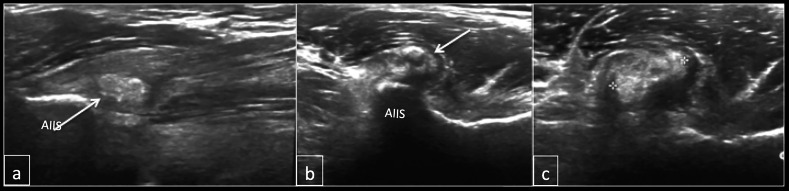
Fig. 2.
Longitudinal (a) and axial (b and c) of the hip demonstrating amorphous calcification within the direct head of rectus femoris (arrow). AIIS- anterior inferior iliac spine
Fig. 3.
CT Axial (a) and sag (b) showing calcification in the direct head of rectus femoris
Treatment
The patient was initially managed symptomatically with analgesia, without any benefit. US-PICT was performed by identifying the direct head of the rectus femoris in the longitudinal plane (Fig. 4). Following aseptic technique and local anaesthetic (1% Lidocaine), using a 19G needle with 3 ml of 1% lidocaine, multiple (15–20) passes were made through the calcification with intermittent pulse lavage. Subsequently, the local anaesthetic with approximately 1 ml of calcium was aspirated while further passes were performed (Fig. 5). Injection of corticosteroid (40 mg Depomedrone) was then performed around the direct head. The patient was advised to avoid strenuous exercise for one week. Her pain significantly decreased post US-PICT from a VAS scale of 10–2 over a six-week period.
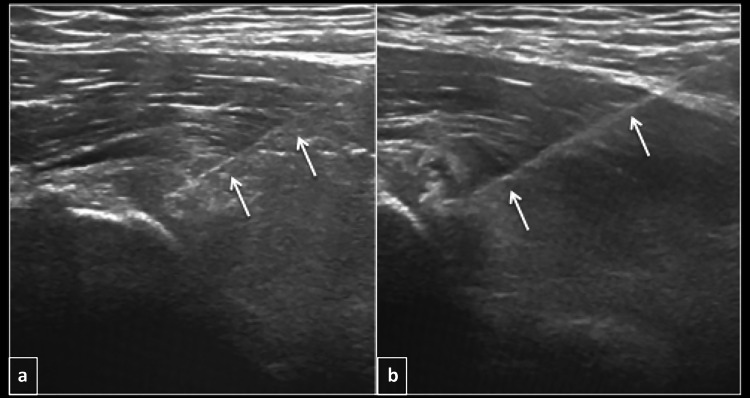
Fig. 4.
Longitudinal ultrasound (a and b) showing needle (arrows) within the calcification during barbotage
Fig. 5.
Syringe with white coloured fluid containing calcific deposits post barbotage
Discussion
Groin pain is a commonly encountered symptom in the musculoskeletal setting. The differential diagnosis is wide, and includes pathologies involving the adductor, iliopsoas or rectus femoris tendons/muscles, the adductor-rectus abdominus aponeurosis, the hip joint and related structures and inguinal/femoral hernias.
Pathologies arising in the rectus femoris include muscle/tendon tears and avulsion injuries, tendinopathy, myositis ossificans and bone/soft tissue tumours, and are a relatively rare cause of groin pain in adults.
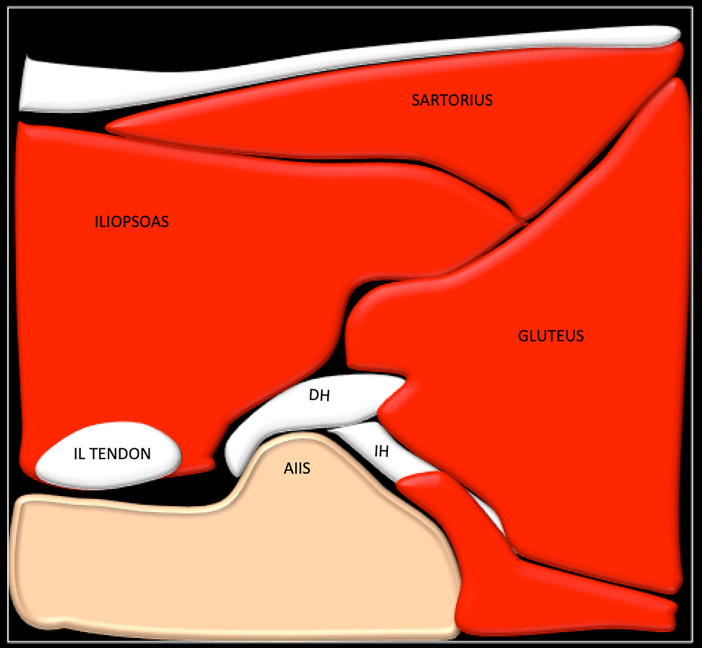
The rectus femoris is the most superficial of the quadriceps muscles in the anterior compartment of the thigh, and is involved in hip flexion and knee extension. It is comprised of two heads, which can be clearly delineated on magnetic resonance imaging (MRI). The direct head arises from the anteroinferior iliac spine (AIIS) and the indirect head arises from the superior acetabular ridge [1] (Fig. 6 and 7). A lesser-known third head has also been identified in cadaveric studies, and arises from the lateral aspect of the direct head, inserting onto the iliofemoral ligament [2]. The distal insertion of the rectus femoris is onto the superior pole of the patella. The posterior division of the femoral nerve innervates the rectus femoris [3].
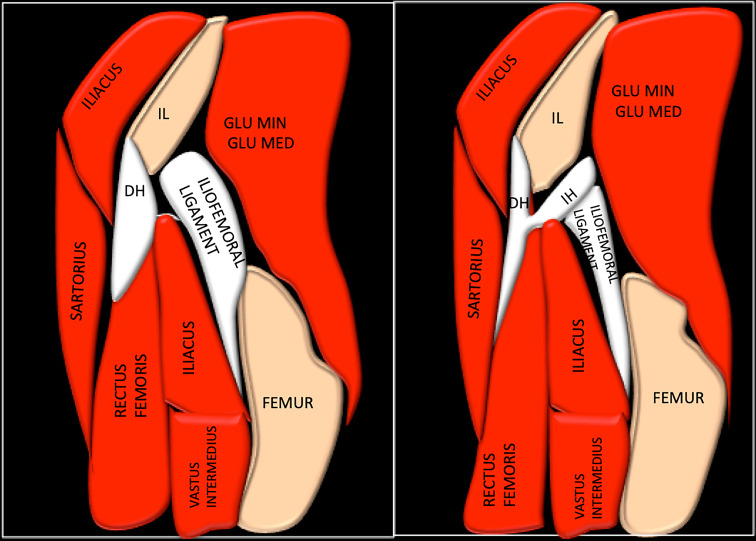
Fig. 6.
Diagrammatic representation of the sagittal of hip joint showing the direct head (DH) and indirect head of rectus femoris. IL- ilium, Glu Med- gluteus medius, Glu Min- gluteus minimus
Fig. 7.
Diagrammatic representation of the axial of hip showing the direct head (DH) and indirect head of rectus femoris. AIIS- anterior inferior iliac spine, IL- iliopsoas
Calcific tendinopathy is the abnormal periarticular deposition of calcium hydroxyapatite crystals within tendons, leading to local inflammation and necrosis [1]. The most common location for calcific tendinopathy is the shoulder, but it has also been reported in the hip, hand, spine and elbow [4]. Calcific tendinopathy of rectus femoris is a rare but recognised pathology, with a number of cases described in the literature, the majority of which involve the indirect head [4–17]. In contrast, our case involves the direct head of the rectus femoris and is a much rarer, with only two case reports in the literature [6, 18]. Identification of calcification on radiographs can be difficult due to its amorphous nature and location. Ultrasound or CT helps to better delineate the extent and location of calcification within the rectus femoris tendon. Patients typically present with groin pain aggravated by hip flexion. In patients with calcific tendinopathy of the indirect head, groin pain is of acute onset because of its close proximity to the hip joint, whereas in patients with calcific tendinopathy of the direct head, the onset of pain is gradual, as in our case. Although the pathogenesis of calcific tendinopathy is not fully understood, repetitive trauma, genetic and local metabolic abnormalities have been suggested as causative factors [7, 19–22].
The differential diagnosis of calcific tendinopathy of the rectus femoris is a previous avulsion injury of the AIIS. These entities can be relatively easily differentiated by assessing the focus of calcification: in calcific tendinopathy, the calcification appears amorphous and immature. In contrast, the calcification in an avulsion fracture is mature and a donor site may be visible from the AIIS. Normally, intervening tendon is seen between the origin of the direct head from the AIIS and the calcific deposit, which is not the case with avulsion fractures.
Patients with calcific tendinopathy of the rectus femoris are usually managed symptomatically with oral non-steroidal anti-inflammatory drugs (NSAIDS), although a number of other treatment options have been described, including image-guided steroid injection [8], arthroscopic removal of calcification [15], radiotherapy [13], extracorporal shock wave therapy [23] and open surgical removal [9]. To the best of our knowledge, US-PICT of the direct head of rectus femoris has not previously been described. Previous studies evaluating US-PICT of the rotator cuff in the shoulder have shown positive results, with > 70% improvement in pain using this technique, which has been shown to be more effective than ultrasound-guided steroid injection alone [24, 25]. De Zordo and colleagues reported a case of calcific tendinopathy treated with US-PICT using the two-needle technique. However, it is unclear whether that case involved the direct head or indirect head. In our case, US-PICT was performed using the single-needle technique [26], which resulted in a significant decrease in symptoms and should be considered in patients with calcific tendinopathy of the direct head of the rectus femoris.
Conclusion
Rectus femoris calcific tendinopathy should be considered in the differential diagnosis for atypical groin pain, and routine assessment of the rectus femoris should be undertaken in these cases. US-PICT should be considered in the treatment of this condition if symptomatic treatment with NSAIDS fails.
Funding
No funding received
Compliance with ethical standards
Conflict of interest
The authors declare that they have no conflict of interest.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Pesquer L, Poussange N, Sonnery-Cottet B, Graveleau N, Meyer P, Dallaudiere B, et al. Imaging of rectus femoris proximal tendinopathies. Skelet Radiol. 2016;45:889–897. doi: 10.1007/s00256-016-2345-3. [DOI] [PubMed] [Google Scholar]
- 2.Hasselman CT, Best TM, Hughes C, Martinez S, Garrett WE. An explanation for various rectus femoris strain injuries using previously undescribed muscle architecture. Am J Sports Med. 1995;23(4):493–499. doi: 10.1177/036354659502300421. [DOI] [PubMed] [Google Scholar]
- 3.Ryan JM, Harris JD, Graham WC, Virk SS, Ellis TJ. Origin of the direct and reflected head of the rectus femoris: an anatomic study. Arthrosc J Arthrosc Relat Surg. 2014;30(7):796–802. doi: 10.1016/j.arthro.2014.03.003. [DOI] [PubMed] [Google Scholar]
- 4.Braun-Moscovici Y, Schapira D, Nahir AM. Calcific tendinitis of the rectus femoris. J Clin Rheumatol Pract Rep Rheum Musculoskelet Dis. 2006;12(6):298–300. doi: 10.1097/01.rhu.0000249896.43792.62. [DOI] [PubMed] [Google Scholar]
- 5.Archer BD, Friedman L, Stilgenbauer S, Bressler H. Symptomatic calcific tendinitis at unusual sites. Can Assoc Radiol J. 1992;43:203–207. [PubMed] [Google Scholar]
- 6.Pope TL, Keats TE. Case report 733. Calcific tendinitis of the origin of the medial and lateral heads of the rectus femoris muscle and the anterior iliac spin (AIIS) Skelet Radiol. 1992;21(4):271–272. doi: 10.1007/BF00243072. [DOI] [PubMed] [Google Scholar]
- 7.Holt PD, Keats TE. Calcific tendinitis: a review of the usual and unusual. Skelet Radiol. 1993;22:1–9. doi: 10.1007/BF00191518. [DOI] [PubMed] [Google Scholar]
- 8.Sarkar JS, Haddad FS, Crean SV, et al. Acute calcific tendinitis of the rectus femoris. J Bone Jt Surg Br. 1996;78:814–816. doi: 10.1302/0301-620X.78B5.0780814. [DOI] [PubMed] [Google Scholar]
- 9.Yun HH, Park JH, Park JW, Lee JW. Calcific tendinitis of the rectus femoris. Orthopedics. 2009;32(7):490. doi: 10.3928/01477447-20090527-13. [DOI] [PubMed] [Google Scholar]
- 10.Chow HY, Recht MP, Schils J, et al. Acute calcific tendinitis of the hip. Arthritis Rheum. 1997;40:974–977. doi: 10.1002/art.1780400528. [DOI] [PubMed] [Google Scholar]
- 11.Hodge JC, Schneider R, Freiberger RH, et al. Calcific tendinitis in the proximal thigh. Arthritis Rheum. 1993;36:1476–1482. doi: 10.1002/art.1780361021. [DOI] [PubMed] [Google Scholar]
- 12.Resnick D. Calcium hydroxyapatite crystal deposition disease. In: Resnick D, editor. Diagnosis of bone and joint disorders. 3. Phila-delphia: WB Saunders; 1995. [Google Scholar]
- 13.King JW, Vanderpool DW. Calcific tendinitis of the rectus femoris. Am J Orthop. 1967;9:110–111. [PubMed] [Google Scholar]
- 14.Kobayashi H, Kaneko H, Homma Y, et al. Acute calcific tendinitis of the rectus femoris: a case series. J Orthop Case Rep. 2015;5(3):32–34. doi: 10.13107/jocr.2250-0685.301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Peng X, Feng Y, Chen G, Yang L. Arthroscopic treatment of chronically painful calcific tendinitis of the rectus femoris. Eur J Med Res. 2013;18:49. doi: 10.1186/2047-783X-18-49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Mohan R, Gopakumar TS, Rajendran VR, Rehiman S. Acute rectus femoris calcific tendinitis. JCR. 2015;5:458–462. doi: 10.17659/01.2015.0118. [DOI] [Google Scholar]
- 17.Zini R, Panascì M, Papalia R, Franceschi F. Rectus femoris tendon calcification. Arthroscopic excision in 6 top amateur athletes. Orthop J Sports Med. 2014 doi: 10.1177/2325967114561585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Pierannunzii L, Tramontana F, Gallazzi M. Case report: calcific tendinitis of the rectus femoris: a rare cause of snapping hip. Clin Orthop Relat Res. 2010;468(10):2814–2818. doi: 10.1007/s11999-009-1208-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Cannon RB, Schmid FR. Calcific periarthritis involving multiple sites in identical twins. Arthritis Rheum. 1973;16:393–396. doi: 10.1002/art.1780160316. [DOI] [PubMed] [Google Scholar]
- 20.Uhthoff HK, Sarkar K, Maynard JA. Calcifying tendinitis: a new concept of its pathogenesis. Clin Orthop Relat Res. 1976;118:164–168. [PubMed] [Google Scholar]
- 21.Becciolini M, Bonacchi G, Galletti S. Intramuscular migration of calcific tendinopathy in the rotator cuff: ultrasound appearance and a review of the literature. J Ultrasound. 2016;19:175. doi: 10.1007/s40477-016-0202-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Cocco G, Ricci V, Boccatonda A, et al. Migration of calcium deposit over the biceps brachii muscle, a rare complication of calcific tendinopathy: ultrasound image and treatment. J Ultrasound. 2018;21:351. doi: 10.1007/s40477-018-0336-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Oh KJ, Yoon JR, Shin DS, Yang JH. Extracorporeal shock wave therapy for calcific tendinitis at unusual sites around the hip. Orthopedics. 2010;33(10):769. doi: 10.3928/01477447-20100826-30. [DOI] [PubMed] [Google Scholar]
- 24.de Witte PB, Selten JW, Navas A, Nagels J, Visser CP, Nelissen RG, Reijnierse M. Calcific tendinitis of the rotator cuff: a randomized controlled trial of ultrasound-guided needling and lavage versus subacromial corticosteroids. Am J Sports Med. 2013;41(7):1665–1673. doi: 10.1177/0363546513487066. [DOI] [PubMed] [Google Scholar]
- 25.Lanza E, Banfi G, Serafini G, Lacelli F, Orlandi D, Bandirali M, Sardanelli F, Sconfienza LM. Ultrasound-guided percutaneous irrigation in rotator cuff calcific tendinopathy: what is the evidence? a systematic review with proposals for future reporting. Eur Radiol. 2015;25(7):2176–2183. doi: 10.1007/s00330-014-3567-1. [DOI] [PubMed] [Google Scholar]
- 26.De Zordo T, Ahmad N, Ødegaard F, Girtler MT, Jaschke W, Klauser AS, Chhem RK, Romagnoli C. US-guided therapy of calcific tendinopathy: clinical and radiological outcome assessment in shoulder and non-shoulder tendons. Ultraschall Med. 2011;32(Suppl 1):S117–S123. doi: 10.1055/s-0029-1245333. [DOI] [PubMed] [Google Scholar]