Abstract
Calcific tendinitis is a common disorder in adults. Although rare, humerus involvement associated with pectoralis major tendon calcification migration has previously been reported in studies that focus on its CT and MRI appearance. We present four cases of intraosseous migration of pectoralis major tendon calcification and their ultrasound features. Calcification migration into osseous structures is associated with cortical erosions, intraosseous calcifications, and bone marrow edema. These findings may be misleading on MRI, where the significant bone marrow and surrounding tissue inflammation may raise concerns regarding neoplasia and lead to unnecessary invasive biopsy. In these cases, echography can be less alarming, enabling the identification of the calcification, its location in the pectoralis major tendon enthesis, and the continuity between the calcification and the typical cortical erosion. Ultrasound features may be diagnostic and might help avoid additional costly imaging studies or invasive biopsy.
Keywords: Pectoralis major tendon, Calcific tendinitis, Intraosseous calcification migration, Ultrasound
Introduction
Calcific tendinitis is a common disorder secondary to the periarticular deposition of hydroxyapatite crystals, and is found in about 3% of adults [1]. It occurs most frequently at the rotator cuff, with the distal supraspinatus tendon being the most common site of involvement. Other locations include the hip, elbow, wrist, knee, and neck [2]. According to Uhthoff, the natural evolution of calcific tendinopathy occurs in four stages: precalcific, formative, resorptive, and postcalcific [3, 4]. Migration of intra-tendinous calcifications into nearby structures (bone, bursa, or muscles) can occur during stage three, the resorptive stage, and may be responsible for acute pain [2, 5]. When calcifications migrate into osseous structures, cortical erosions, intraosseous calcifications, and bone marrow edema can be observed using computed tomography (CT) and magnetic resonance imaging (MRI), as previously reported [1, 2]. These findings, associating cortical destruction and bone marrow edema, may sometimes be misleading, particularly on MRI, where the significant bone marrow and surrounding tissue inflammation may raise concerns regarding neoplasia and lead to unnecessary invasive biopsy [6]. Only a few studies focus on the ultrasound (US) features of this condition [7, 8].
Although rare, several cases of humerus involvement associated with pectoralis major (PM) tendon calcification migration have previously been reported, in studies that focus on their CT and MRI aspects [2, 6, 9–12]. We hereby present the ultrasound features of four painful cases of intraosseous migration of PM tendon calcifications with follow-up.
Case 1 (Fig. 1)
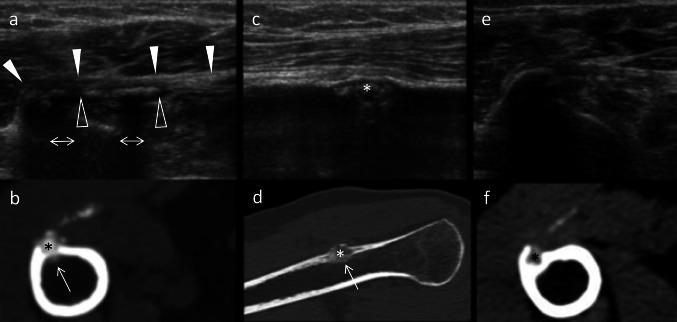
Fig. 1.
Typical aspect of pectoralis major tendon calcification on US and CT. a US, axial view. Linear, bow-shaped hyperechoic calcification (empty arrowheads) with partial posterior acoustic shadowing (double arrows), located along the deep fibers of the pectoralis major tendon (full arrowheads), and with a long axis parallel to the long axis of the tendon. b Non-contrast CT, axial view. Superimposable findings with cortical erosion (asterisk). CT reveals an endo-medullary migration of calcification fragments (arrow) not seen on US. c US, sagittal view. Humeral oval-shaped cortical erosion located at the site of insertion of the pectoralis major tendon, containing hyperechoic calcified fragments (asterisk). d Non-contrast CT, sagittal view. Corresponding findings with cortical erosion (asterisk) and endo-medullary calcified fragment (arrow). e US, axial view. Two-month follow-up shows regression of calcification. f Non-contrast CT, axial view. Two-month follow-up CT shows partial resorption of cortical erosion (asterisk)
A 68-year-old female was referred to our center with an acute anterior pain in the proximal portion of her right arm. An US was initially performed and found a linear, bow-shaped, hyperechoic calcification of 19 mm, with partial posterior acoustic shadowing, located along the deep fibers of the PM tendon, and with a long axis parallel to the tendon long axis. This calcification was in continuity with a 15-mm oval-shaped cortical erosion of the humerus containing hyperechoic calcified fragments and located at the site of insertion of the PM tendon. Peripheral reactional hyperostosis was associated. Non-contrast CT presented superimposable findings and revealed endo-medullary migration of calcification fragments. These findings were compatible with intraosseous migration of PM tendon calcification.
At 2-month follow-up, control US and CT revealed partial resorption of the cortical erosion, fragmentation of calcifications with loss of posterior acoustic shadowing, and complete regression of endo-medullary calcification. No pain relapse was reported.
Case 2 (Fig. 2)
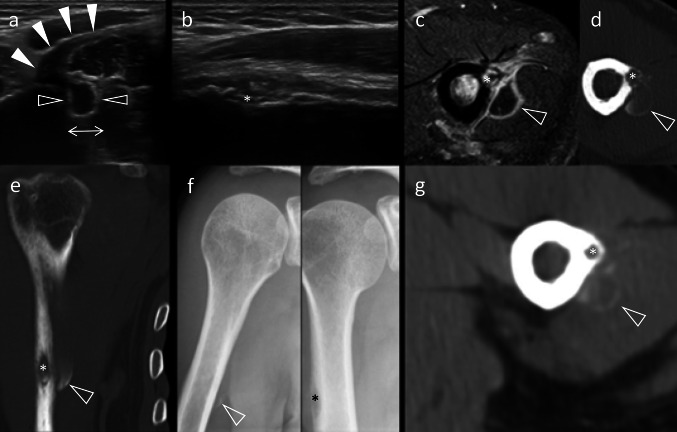
Fig. 2.
Liquid-like calcification of the pectoralis major: US, CT, and MRI correlations. a US, axial view. Anechoic liquid-like calcification (empty arrowheads) with posterior acoustic enhancement (double arrow) originating from the deep fibers of the pectoralis major tendon (full arrowheads). b US, sagittal view. Cortical erosion (asterisk) of the humerus at the site of pectoralis major tendon insertion. c MRI, STIR sequence, axial view. Superimposable semiology is seen, with hypointense calcification (empty arrowhead), cortical erosion (asterisk), and local inflammation with surrounding soft-tissue hyperintensity. d, e Non-contrast CT, axial and coronal views. Cortical erosion (asterisk) and calcium–fluid level within calcification (empty arrowhead). f X-ray, internal rotation, and neutral position views. Superimposable findings with calcification (empty arrowhead), visible only on the internal rotation film, and cortical erosion (asterisk) as viewed on neutral position film. g Non-contrast CT, axial view. Ten-day follow-up shows partial resorption of calcification (empty arrowhead) and re-ossification of cortical erosion (asterisk)
A 56-year-old female was referred to our center for biopsy of a suspicious mass on the right humerus. The patient was suffering from an intense pain in her right upper arm. A non-contrast CT and an MRI had initially been performed, which were read as remarkable for a possible necrotic neoplasia of soft tissues, warranting biopsy. We decided to perform further evaluation with an US. US revealed a 22-mm oval-shaped, liquid-like calcification located in the deep fibers of the PM tendon, presenting a hyperechoic rim and an anechoic center, and without posterior acoustic shadowing. The long axis of the calcification was not parallel to the long axis of the tendon. The nearby humerus presented a 16-mm oval-shaped cortical erosion, associated with reactional hyperostosis, at the site of the PM tendon insertion. Intraosseous calcification migration was confidently diagnosed with US, and biopsy was not performed. Non-contrast CT and MRI were concordant with the US findings, with a liquified calcification showing a calcium–fluid level within the tendon.
At 10-day follow-up, reduction in the calcification and re-ossification of the cortical erosion was observed on imaging. The patient’s pain had disappeared.
Case 3 (Fig. 3)
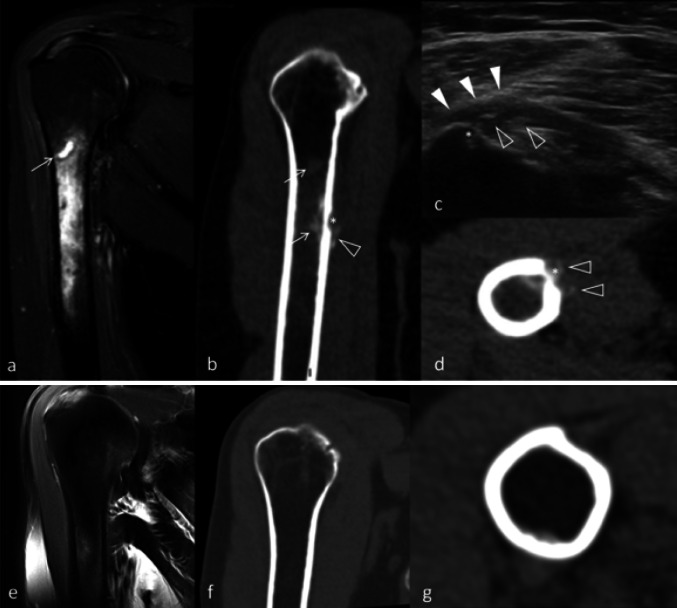
Fig. 3.
Deceptive aspect of calcification migration on MRI and diagnosis rectification by US. a MRI, STIR sequence, coronal view. Intra-medullary diffuse edema associated with small, liquid-like hyperintense foci of the bone marrow was secondarily identified as a calcification (arrow). b Non-contrast CT, coronal view. Cortical erosion (asterisk) with peripheral soft-tissues calcification (empty arrowhead) and intra-medullary calcifications (arrows). Notice the correspondence of the intra-medullary calcification with the MRI. c US, axial view. Typical aspect of calcification migration, with calcifications (empty arrowheads) sitting in the interstitial and deep fibers of the pectoralis major tendon (full arrowheads), in continuity with the cortical erosion (asterisk). No posterior acoustic shadowing is observed. d Non-contrast CT, axial view. Corresponding image, with humeral cortical erosion (asterisk) and calcifications on both sides (empty arrowheads). e, f, g Respectively, MRI, T2 Fat Sat sequence, coronal view; non-contrast CT, coronal view; non-contrast CT, axial view. Notice the restitutio “ad integrum” at 1-year follow-up. The intra-medullary edema, the cortical erosion, and the tendinous calcifications have entirely disappeared
A 62-year-old female was referred to our center for biopsy of a suspicious lesion on the right proximal humerus. The patient suffered from chronic non-traumatic pain in the upper right arm, with recent worsening. An MRI of the right upper extremity had initially been performed at another center. Images revealed extensive T2 hyperintensity of the medulla, corresponding to bone marrow edema. The possibility of an intra-medullary calcification migration was mentioned by our radiologist after reexamination of the MRI images, and further evaluation with US and non-contrast CT was performed. US images were significant for a 10-mm linear, bow-shaped calcification with irregular contours and without posterior acoustic shadowing, sitting in the interstitial and deep fibers of the PM tendon. The long axis of the calcification was parallel to the long axis of the PM. This calcification was in continuity with calcified fragments located at the center of an 8-mm oval-shaped regular cortical erosion, whose long axis was parallel to the diaphyseal axis of the humerus. US confirmed the diagnosis of intraosseous calcification migration and avoided biopsy. Reinterpretation of the initial MRI identified a possible intra-medullary calcification, highlighting the challenge of identifying calcification on MRI.
One-year follow-up imaging showed complete resolution of medullary edema, cortical erosion, and tendinous calcifications. The patient was symptom-free at that time.
Case 4 (Fig. 4)
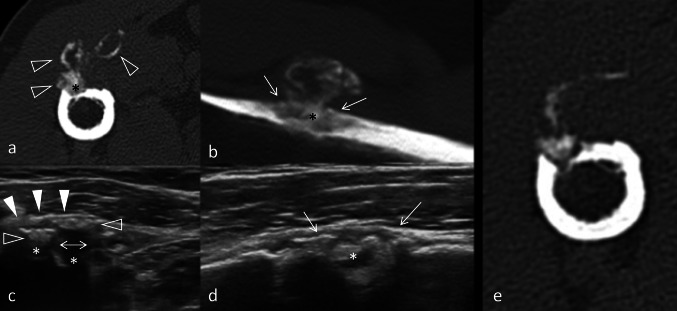
Fig. 4.
Deceptive aspect of calcification migration on CT and diagnosis rectification by US. a Non-contrast CT, axial view. Globular heterogeneous calcification extending into soft tissues (empty arrowheads) associated with cortical erosion (asterisk). These findings were initially interpreted as suspicious for malignancy. b Non-contrast CT, sagittal view. Cortical erosion (asterisk) parallel to the humeral cortical bone, with calcified fragments in its center and peripheral reactive hyperostosis (arrows). c US, axial view. Typical aspect of calcification migration with heterogeneous calcifications (empty arrowheads) affecting the entire thickness of the tendon (full arrowheads) and contiguous cortical erosion (asterisk). Notice the incomplete posterior acoustic shadowing (double arrows). d US, sagittal view. Cortical erosion (asterisk) with elevated borders by reactive hyperostosis. e Non-contrast CT, axial view. Partial resorption of calcification at 2-week follow-up
A 62-year-old female was referred to our center for biopsy of a right humerus lesion. The patient presented with a rapidly worsening non-traumatic pain in the right shoulder. A non-contrast CT had previously been performed at another center; the CT was significant for proximal humerus cortical erosion with hyperostosis and extensive calcifications of the surrounding soft tissues. The possibility of an intra-medullary calcification migration was mentioned by our radiologist after the images were re-read, and an US was performed. Ultrasound findings included a 28-mm globular, bow-shaped calcification parallel to the tendon long axis, sitting in the interstitial and deep PM tendon fibers. This calcification was irregular, ill-defined, and powdery, and it presented an incomplete posterior acoustic shadowing. The calcification was in continuity with calcific fragments situated within a cortical erosion of the humerus at the PM tendon insertion. The erosion was oval shaped, measured 15 mm, and was parallel to the long axis of the humerus diaphysis. Reactional hyperostosis was significant, with elevated borders of the cortical erosion. Again, in this case, US confirmed the diagnosis of intraosseous calcification migration, and biopsy was not necessary.
Two-week imaging follow-up showed partial resorption of the calcification, and the patient’s pain was alleviated.
Discussion
In our experience, US accurately diagnosed intraosseous migration of PM tendon calcification and rectified an initial diagnosis of suspicious lesion in three out of four cases. On US examination, calcifications of various sizes presented linear, bow-like shape reflecting the anatomic position of the tendon; sat preferentially in the interstitial and deep tendinous fibers; and were parallel to the tendon major axis. Bone erosions were small (< 2 cm), oval shaped, located in the sub-cortical region, contained calcific fragments, and were associated with reactional peripheral hyperostosis. They were located at the PM tendon insertion on the humerus, and US always depicted the continuity between tendon calcification and the cortical erosions. Bone marrow changes and intra-medullary calcification were not visualized with US. These features were consistent with previously described aspects in other locations, and could therefore apply to osseous erosions secondary to PM tendon calcification migration [2, 13].
Plain radiographs and US are often the first-line imaging techniques in the initial workup of an acute, non-traumatic body extremity pain. Because of their location, identification of PM tendon calcifications can be challenging on plain X-rays, where they are often only visible on the internal rotation view. Although the elementary description of calcifications on echography is well known in the radiology community, specific features may apply when they migrate in nearby osseous structures: Calcifications are often fragmented with scalloped contours, and present very little or no posterior acoustic shadowing. A pseudo-liquid aspect is even possible [14]. US features of osseous modifications facing the tendinous calcification also deserve to be detailed: (1) Cortical bone erosions are oval shaped, with a long axis parallel to the bone axis; (2) erosions are centered by the tip of the calcification and contain migrated calcified fragments; and (3) peripheral hypertrophic osseous reaction is present (Fig. 5).
Fig. 5.
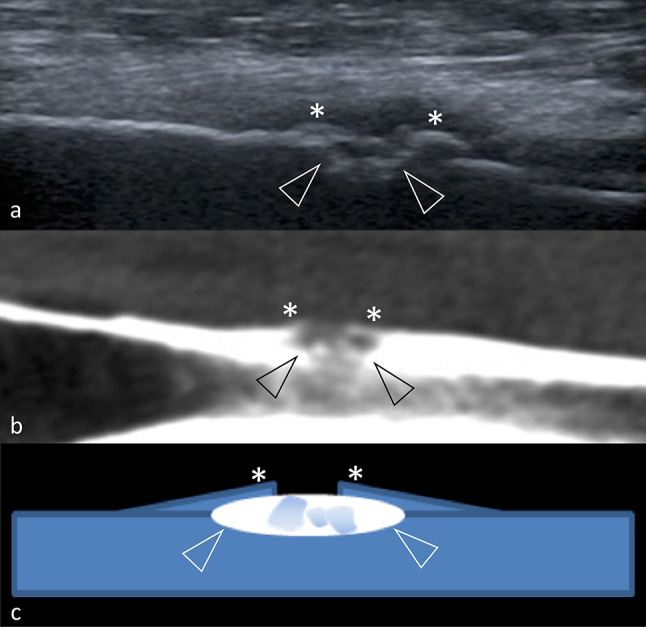
Typical features of cortical erosion associated with calcification migration. a US, sagittal view. Cortical erosion (empty arrowheads) with a long axis parallel to the diaphyseal axis. Reactional hyperostosis is present, with elevated borders of the erosion (asterisk). Notice the crater-like shape of the erosion and the calcified fragments located at the heart of the erosion. b Non-contrast CT, sagittal view. Corresponding image of cortical erosion. c Schematization of cortical erosion and hyperostosis
MRI features of calcification migration can be misleading, and may lead to unnecessary invasive biopsy [2, 6]. Calcifications can be difficult to identify with this technique, and are often not visible [15]. Additionally, with MRI, intraosseous calcification migration is often accompanied by a significant edema extending to the bone marrow and to surrounding soft tissues, which is secondary to calcium fragments migration [2]. This aspect can cause concern for the radiologist, especially when the calcification is not readily visible. Indeed, in the presence of cortical destruction and extensive edema, two differentials must be ruled out: aggressive tumoral lesions and infectious osteitis [6]. Similarly, CT may mislead by indicating the association of cortical erosion and adjacent calcifications. Although calcifications are well analyzed with CT, their intra-tendinous locations are more difficult to assess, as tendons insertions are difficult to individualize on CT.
US can confidently identify a calcification, its location within the PM tendon enthesis, and its connection with the cortical erosion which presents typical features. US also rules out a soft-tissue mass. The location, the layout, and the US aspect of tendinous calcifications are distinct from bony sequestrum or periosteal appositions. Hence, US rules out a calcified abscess or an infection-related calcification.
Conclusion
US is a simple technique which can accurately identify PM tendon calcifications with intraosseous migration in patients presenting with pain in the proximal humerus. Radiologists should be familiar with the typical ultrasound features of this pathology in order to prevent unnecessary invasive biopsies.
Compliance with ethical standards
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Flemming DJ, Murphey MD, Shekitka KM, Temple HT, Jelinek JJ, Kransdorf MJ. Osseous involvement in calcific tendinitis: a retrospective review of 50 cases. AJR Am J Roentgenol. 2003;181(4):965–972. doi: 10.2214/ajr.181.4.1810965. [DOI] [PubMed] [Google Scholar]
- 2.Malghem J, Omoumi P, Lecouvet F, Vande Berg B. Intraosseous migration of tendinous calcifications: cortical erosions, subcortical migration and extensive intramedullary diffusion, a SIMS series. Skelet Radiol. 2015;44(10):1403–1412. doi: 10.1007/s00256-015-2165-x. [DOI] [PubMed] [Google Scholar]
- 3.Cocco G, Ricci V, Boccatonda A, Iannetti G, Schiavone C. Migration of calcium deposit over the biceps brachii muscle, a rare complication of calcific tendinopathy: ultrasound image and treatment. J Ultrasound. 2018;21(4):351–354. doi: 10.1007/s40477-018-0336-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Cocco G, Draghi F, Schiavone C. Ultrasonographic diagnosis and percutaneous treatment of insertional calcific tendinopathy of iliotibial band: case report. Euro Rad. 2018 doi: 10.1594/eurorad/case.15881. [DOI] [Google Scholar]
- 5.Pereira BPG, Chang EY, Resnick DL, Pathria MN. Intramuscular migration of calcium hydroxyapatite crystal deposits involving the rotator cuff tendons of the shoulder: report of 11 patients. Skeletal Radiol. 2016;45(1):97–103. doi: 10.1007/s00256-015-2255-9. [DOI] [PubMed] [Google Scholar]
- 6.Hayes CW, Rosenthal DI, Plata MJ, Hudson TM. Calcific tendinitis in unusual sites associated with cortical bone erosion. Am J Roentgenol. 1987;149(5):967–970. doi: 10.2214/ajr.149.5.967. [DOI] [PubMed] [Google Scholar]
- 7.Nogueira-Barbosa MH, Gregio-Junior E, Lorenzato MM. Retrospective study of sonographic findings in bone involvement associated with rotator cuff calcific tendinopathy: preliminary results of a case series. Radiol Bras. 2015;48(6):353–357. doi: 10.1590/0100-3984.2014.0077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Della Valle V, Bassi EM, Calliada F. Migration of calcium deposits into subacromial–subdeltoid bursa and into humeral head as a rare complication of calcifying tendinitis: sonography and imaging. J Ultrasound. 2015;18(3):259–263. doi: 10.1007/s40477-015-0163-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Dürr HR, Lienemann A, Silbernagl H, Nerlich A, Refior HJ. Acute calcific tendinitis of the pectoralis major insertion associated with cortical bone erosion. Eur Radiol. 1997;7:1215–1217. doi: 10.1007/s003300050277. [DOI] [PubMed] [Google Scholar]
- 10.Cahir J, Saifuddin A. Calcific tendonitis of pectoralis major: CT and MRI findings. Skelet Radiol. 2005;34(4):234–238. doi: 10.1007/s00256-004-0842-2. [DOI] [PubMed] [Google Scholar]
- 11.Morán Blanco LM, González Leyte M. Calcifying tendinosis of the pectoralis major muscle with intraosseous migration. Radiologia. 2011;53(4):364–367. doi: 10.1016/j.rx.2010.10.007. [DOI] [PubMed] [Google Scholar]
- 12.El-Essawy MT, Vanhoenacker FM. Calcific tendinopathy of the pectoralis major insertion with intracortical protrusion of calcification. JBR-BTR. 2012;95(6):374. doi: 10.5334/jbr-btr.733. [DOI] [PubMed] [Google Scholar]
- 13.Marinetti A, Sessa M, Falzone A, Della Sala SW. Intraosseous migration of tendinous calcifications: two case reports. Skelet Radiol. 2018;47(1):131–136. doi: 10.1007/s00256-017-2769-4. [DOI] [PubMed] [Google Scholar]
- 14.Farin PU. Consistency of rotator-cuff calcifications. Observations on plain radiography, sonography, computed tomography, and at needle treatment. Investig Radiol. 1996;31(5):300–304. doi: 10.1097/00004424-199605000-00010. [DOI] [PubMed] [Google Scholar]
- 15.Kraemer EJ, El-Khoury GY. Atypical calcific tendinitis with cortical erosions. Skelet Radiol. 2000;29(12):690–696. doi: 10.1007/s002560000278. [DOI] [PubMed] [Google Scholar]