Abstract
Early detection of local complications (venipuncture complications, nerve lesions, infections, arthritis, and tenosynovitis, tendon adhesions and re-tears, complications related to orthopaedic hardware) after hand surgery is required for prompt treatment. Ultrasound has proven to be a valuable imaging modality for detecting and assessing a variety of disorders of the wrist and hand. The purpose of this pictorial essay is to present a wide range of complications after wrist and hand surgery assessed by ultrasound.
Keywords: Ultrasound, Hand surgery, Local complications, Hand surgery local complications
Introduction
Early detection of local complications after hand surgery is required for prompt treatment. Imaging is frequently obtained and helps clinicians in their accurate assessment. Ultrasound (US) has proven to be a noninvasive, dynamic, and cheap imaging modality for detecting and assessing a variety of disorders of the wrist and hand [1–3]. The purpose of this pictorial essay is to present a wide range of complications after wrist and hand surgery assessed by US.
Complications
Before surgery
Venipuncture complications
Nerve lesions
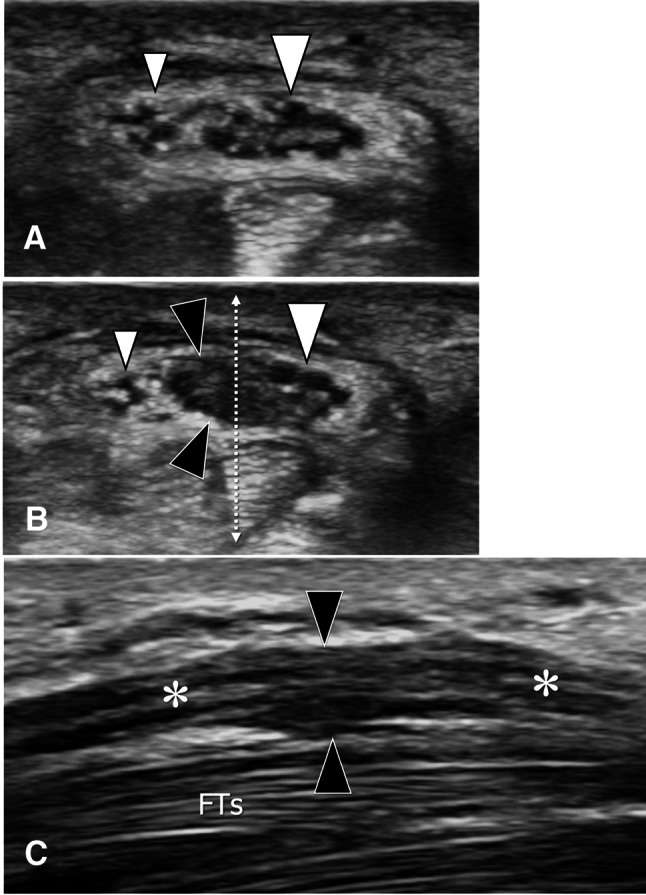
Phlebotomy of the dorsal veins of the wrist and hand is commonly performed in patients as a presurgical preparation and can be associated with injuries of adjacent small subcutaneous nerves [3, 4]. The most frequently injured nerve is the superficial branch of the radial nerve (SBRN), which runs close to the cephalic vein at the radial aspect of the distal forearm [5, 6]. At this level, the SBRN splits into two or three distal branches that cross the cephalic vein running below it. During vein cannulation, the immobilisation of the vein facilitates venipuncture but also immobilises the SBRN branches and facilitates their injury. As a result, painful neuroma can be observed. This presents at US as a focal fusiform hypoechoic swelling of the nerve (Fig. 1). Short-axis sonograms are best suited to demonstrate the neuroma since longitudinal images are difficult to obtain because of the small size of the SBRN branches. US-guided local compression of the neuroma is painful and helps in establishing the diagnosis (US Tinel sign).
Fig. 1.
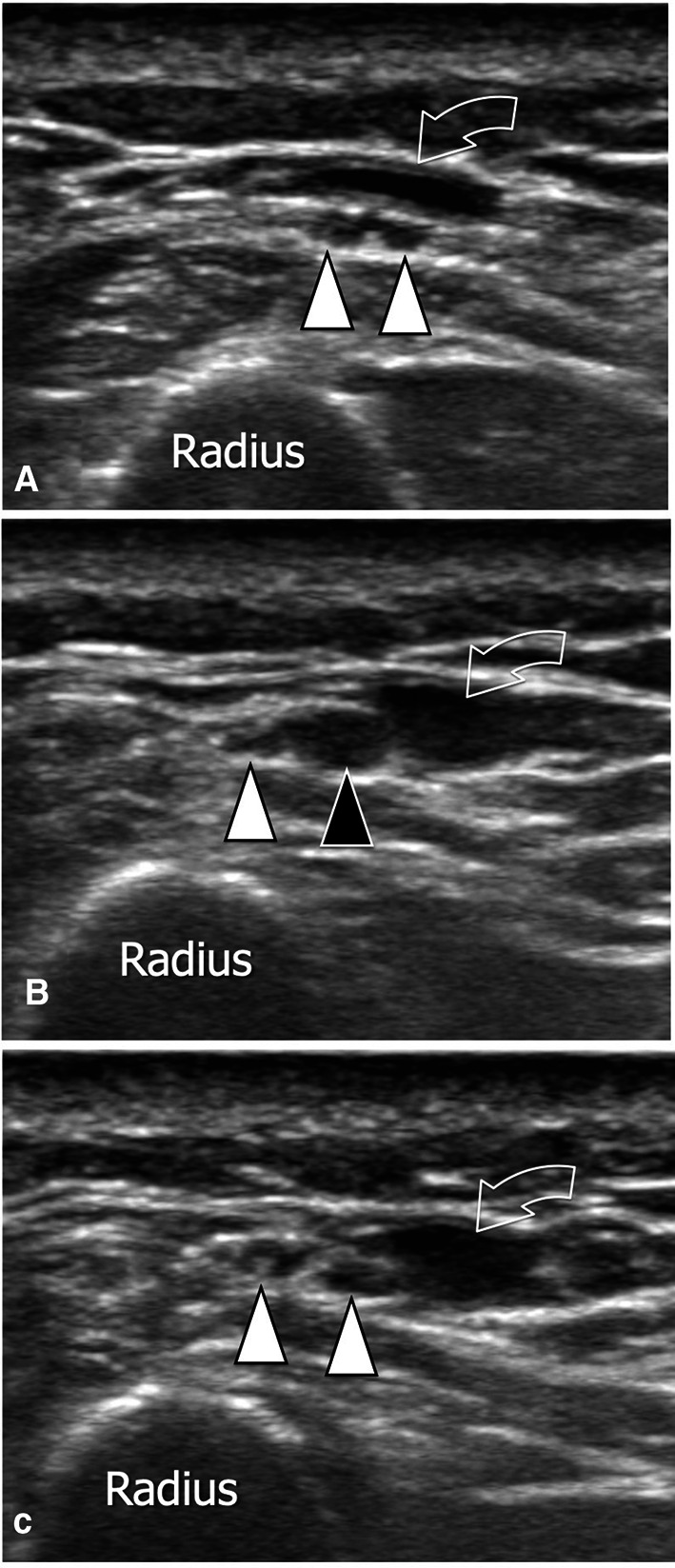
Postvenipuncture in-continuity neuroma. a–c Transverse sonograms obtained from proximal (a) to distal (c) at the lateral aspect of the distal forearm in a patient with Wartenberg syndrome following catheterisation of the cephalic vein (curved arrows). At this level, the superficial branch of the radial nerve is composed of two small branches (white arrowheads), which show a normal appearance in (a). In b, at the level of the venipuncture, the medial branch (black arrowhead) is swollen and hypoechoic and very painful at local pressure. The findings are typical of an in-continuity posttraumatic neuroma. Note the normal appearance of both branches distal to the site of traumatism (c)
Tendon lesions
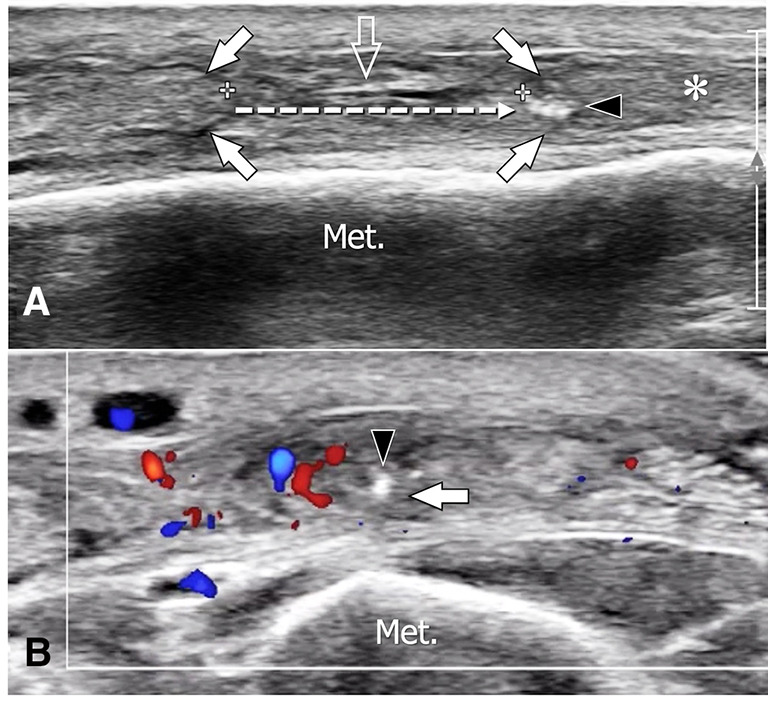
Injuries of other structures are rare during venipuncture. The cannulation of one vein at the dorsum of the hand can injure the extensor tendons and be followed by a partial tear and intratendinous cyst formation [7] (Fig. 2).
Fig. 2.
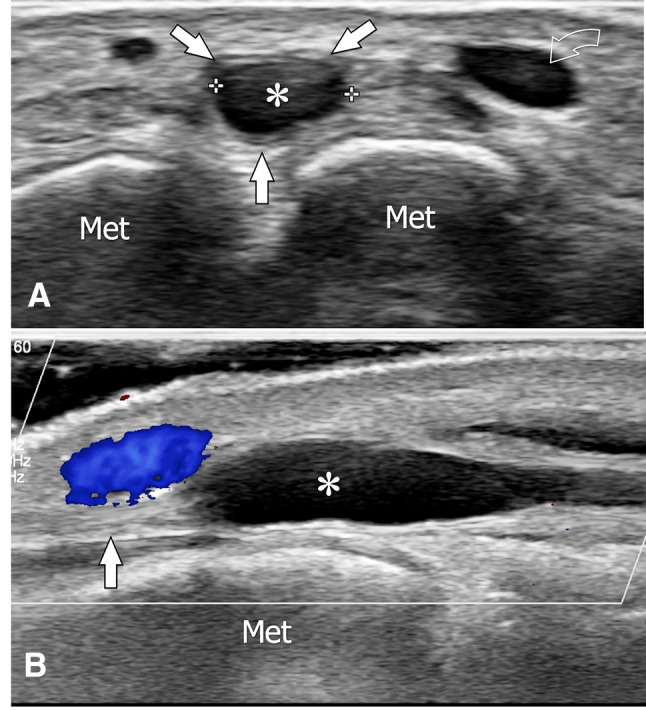
Postvenipuncture intratendineous ganglion. Axial (a) and longitudinal colour Doppler (b) sonograms obtained at the dorsum of the hand in a patient with a localised swelling that appeared after local venipuncture. The swelling is due to an intratendinous anechoic ganglion (asterisks). In a, the ganglion appears surrounded by tendon fibres (white arrowheads). The curved arrow points to the vein. In b, note the close relationship of the ganglion with the subcutaneous vein that was catheterised
During surgery
Nerve lesions
Due to their small size, hand nerves can be accidentally injured during hand surgery. Basically, three types of lesions are observed: end neuromas, neuromas in continuity, and scar-tethered nerves [8]. End neuromas, observed when a nerve is completely sectioned, are bulbous swellings of the distal end of the nerve that are due to local ineffective nerve regeneration. When only some nerve fascicles are injured, a similar reactive lesion affecting only a part of the nerve is observed (neuromas in continuity). Scar-tethered nerves are related to the injury of a normal nerve by tethering and compression by the scar of the perineural tissues.
Due to the superficial location of hand nerves, high-frequency US can detect pathologic nerve changes and distinguish between the different types of nerve injury [1–3]. In end neuroma, complete interruption of the affected nerve is seen. At its end, the nerve shows a bulbous hypoechoic swelling with an irregular structure replacing the internal fascicular pattern (Fig. 3). The more proximal portion of the nerve presents a normal size and structure. In neuromas in continuity, the nerve is continuous but presents a localised fusiform enlargement that can vary in length. The internal structure is irregularly hypoechoic with a blurring of the internal fascicular pattern. Depending on the mechanism and magnitude of the trauma, the neuroma can affect the entire nerve (Fig. 4) or only a part of it (Fig. 5). Scar-tethered nerves are surrounded by an irregular area of hypoechogenicity of the surrounding tissues. The detection of the nerve running inside the fibrous area can be very difficult due to the similar echogenicity of the nerve and scar (Fig. 6). An accurate scanning technique is necessary to follow the nerve proximally, inside the adherence area and distally to it.
Fig. 3.
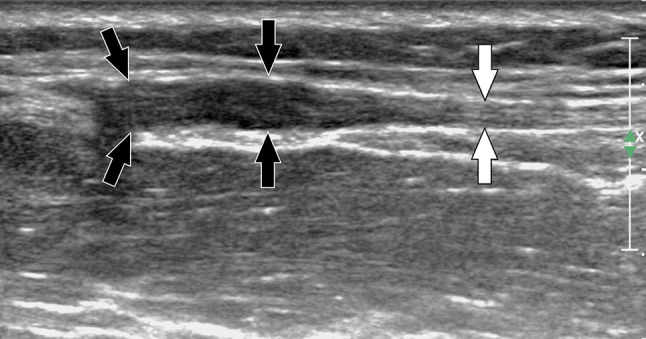
Post-traumatic complete section of nerves. Sagittal sonogram obtained over the superficial branch of the radial nerve in a patient with previous local surgery and paraesthesia of the dorsum of the hand. US shows a complete section of the nerve (white arrows) associated with a stump neuroma (black arrowheads)
Fig. 4.
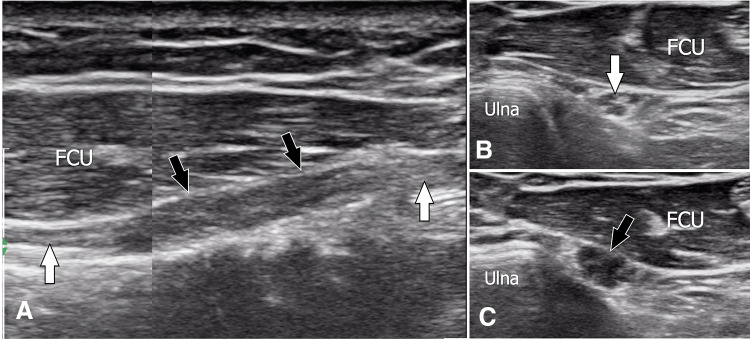
Posttraumatic in-continuity neuroma. Sagittal a and transverse b, c sonograms obtained over the dorsal sensitive branch of the ulnar nerve in a patient with previous local surgery and paraesthesia of the dorsum of the hand. In a, US shows a segmental enlargement of the nerve (black arrowheads), which appears hypoechoic. Note the loss of the normal internal fascicular structure. The appearance is typical of posttraumatic in-continuity neuroma. The white arrows point to the normal proximal and distal nerves. Axial US obtained proximal to the neuroma (b) depicts a normal nerve. Pathologic nerve changes are confirmed at the axial sonograms obtained over the neuroma (c). FCU flexor carpi ulnaris
Fig. 5.
Posttraumatic in-continuity neuroma complicating osteosynthesis of the distal radius. Axial sonogram (a) obtained from the proximal shows the normal appearance of the median nerve (arrow). More distally, the nerve shows an in-continuity neuroma as an area of loss of fascicular structure (black arrowheads) located at its radial portion. Note the disappearance of the normal fascicular pattern inside the neuroma, while the fascicles located in the ulnar portion of the nerve (arrowheads) are normal. The appearance is evocative of a nerve trauma due to surgical distractors. The asterisks point to a normal irregularity of local soft tissues related to surgery
Fig. 6.
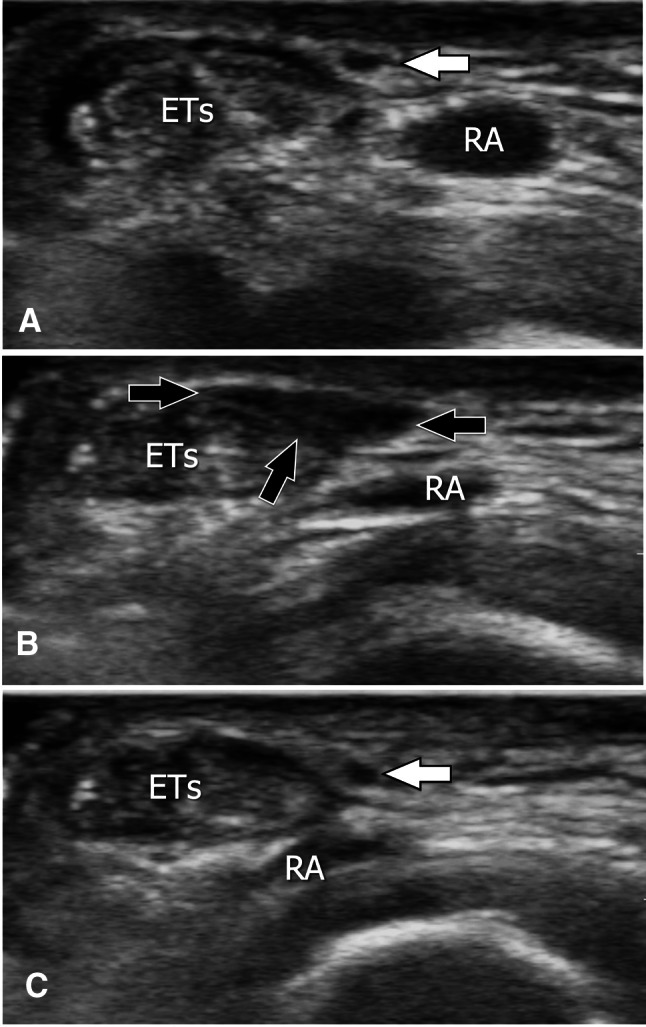
Axial sonograms (a–c) obtained from proximal (a) to distal (c) over the superficial branch of the radial nerve in a patient with previous surgical treatment for De Quervain tenosynovitis. In a, the nerve appears normal (white arrow). More distally (b), the nerve is not detectable because it runs inside a hypoechoic area (black arrows) related to postsurgical fibrosis. Further distally (c), note the normal appearance of the nerve (white arrow) surrounded by normal soft tissues. ETs extensor tendons of the first compartment, RA radial artery
The treatment of surgical nerve complications changes according to the underlying pathology [8]. End neuromas are mostly relocated to a proximal deeper site. Neuromas in continuity and scar-tethered nerves are usually treated by neurolysis followed by nerve wrapping using autogenous tissues or nerve conduits (cylindrical tubes made by synthetic material) [9] (Fig. 7).
Fig. 7.
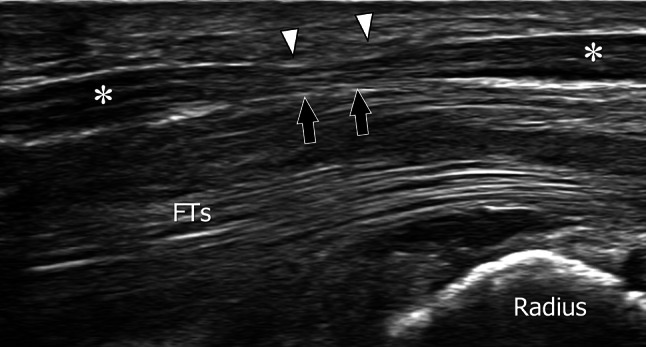
US appearance of nerve conduits. Longitudinal (a) and axial (b, c) sonograms obtained over a nerve conduit located at the palmar-radial aspect of the distal forearm. The nerve conduit presents at US as a tubuliform structure with hyperechoic walls. The nerve located inside the conduit appears normal (white arrowheads) proximally. Note the thickening and hypoechogenicity of the nerve (black arrowheads) in the middle of the conduit
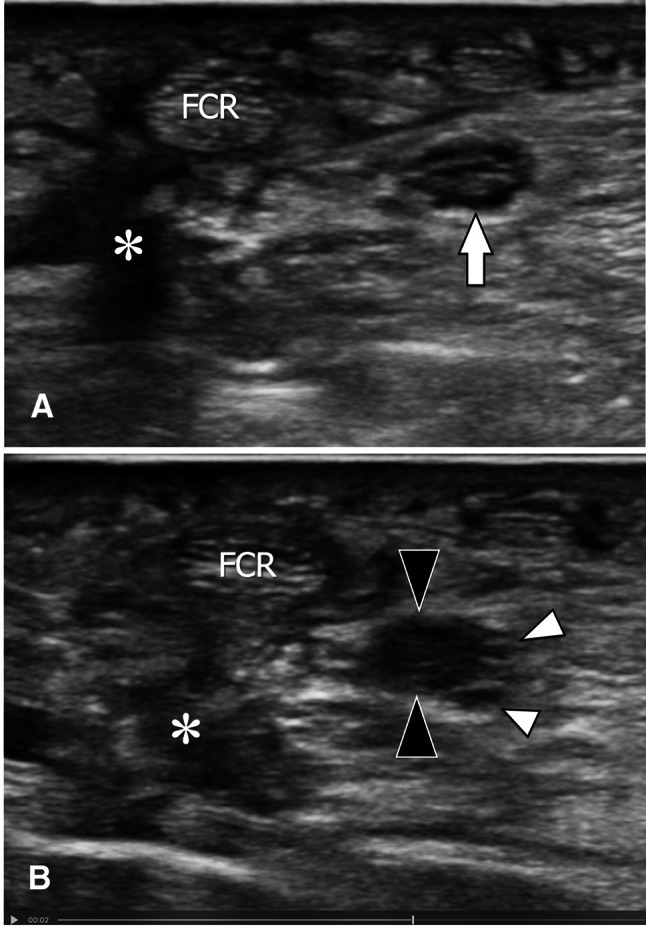
Due to the high frequency of surgery for carpal tunnel syndrome (CTS), postoperative complications are not rare in the daily US office practice. Persistent compression is seen when a part of the transverse carpal ligament (TCL) was not sectioned and is responsible for residual compression on the palmar aspect of the median nerve (MN) (Fig. 8). In these patients, symptoms are present immediately after surgery. In postsurgical perineural fibrosis, symptoms are noted only after a variable time from surgery. The MN shows indistinct borders that can be found mostly at the contact with the sectioned TCL (Fig. 9). The palmar cutaneous branch of the MN can be injured during CTS surgery because of its anatomical position [10]. This small branch detaches from the radial aspect of the MN at the distal forearm to run close to the flexor carpi radialis tendon. At the wrist, it runs over or inside the TCL to finally give sensitive innervation of the skin of thenar eminence. When the branch is damaged, US shows a small neuroma in continuity as a hypoechoic mass (Fig. 10). Direct injuries of the MN are rare. They can be detected as neuroma in continuity (Fig. 11) and/or a complete section of the distal branch of the nerve, usually observed in arthroscopic treatment of CTS (Fig. 12).
Fig. 8.
Complications after carpal tunnel surgery. Sagittal sonogram shows a residual compression of the median nerve. Note the persistent proximal portion of the transverse carpal ligament (arrowheads) associated with focal thinning of the nerve (black arrows). The nerve proximal and distal to the compression appears swollen (asterisks)
Fig. 9.
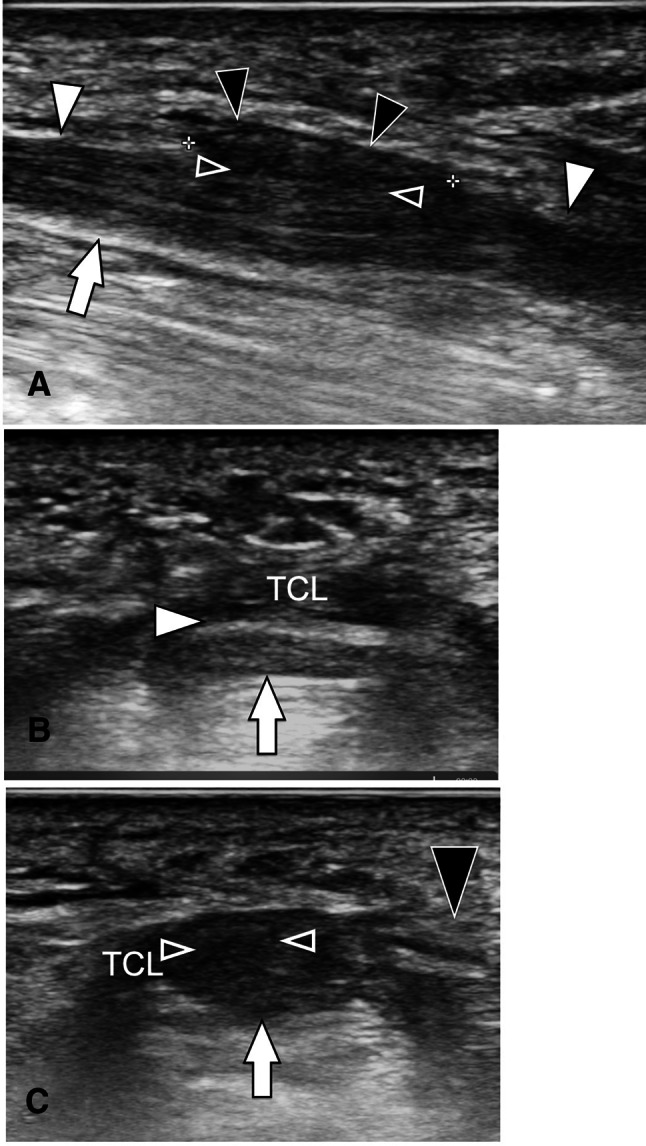
Complications after carpal tunnel surgery. Longitudinal (a) and axial sonograms obtained from proximal (b) to distal (c). In a, note the blurred demarcation (void arrowheads) between the median nerve (arrows) and the sectioned transverse carpal ligament (black arrowheads). Note the distinct demarcation of the nerve and adjacent tissues proximal and distal to the area of fibrosis (white arrowheads). Axial sonogram (c) obtained at the level of the fibrosis confirms fibrotic changes between the nerve and the transverse carpal ligament (TCL)
Fig. 10.
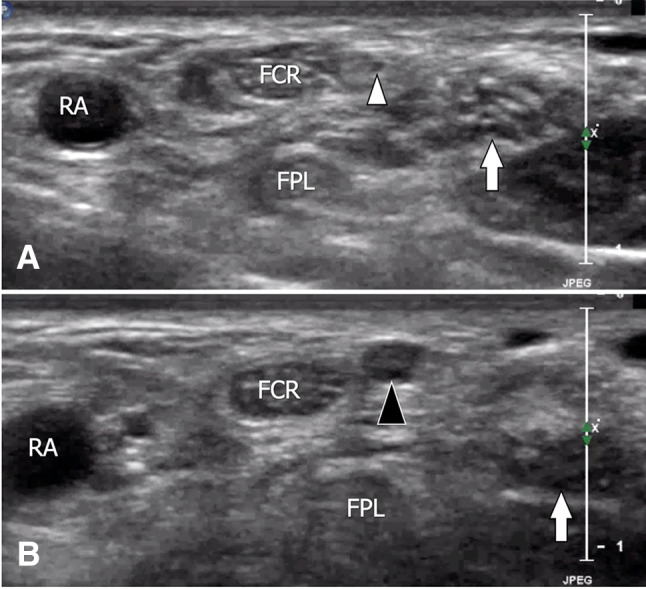
Complications after carpal tunnel surgery. Axial sonograms obtained from proximal (a) to distal (b) in a patient with hypoesthesia of the thenar em.inence. a shows the normal appearance of the median nerve (arrow) and its palmar sensitive branch (arrowhead). More distally (b), the palmar branch is swollen and hypoechoic (black arrowhead) because of the formation of a posttraumatic neuroma. RA radial artery, FCR flexor carpi radialis, FPL flexor pollicis longus
Fig. 11.
Complications after carpal tunnel surgery. Transverse (a, b) and sagittal (c) sonograms obtained over the median nerve in a patient with previous local surgery and persistent paraesthesia. Axial sonogram (a) obtained at a proximal level shows a bifid median nerve consisting of a large radial component (large arrowhead) and a small ulnar component (small arrowhead). More distally, the radial component of the nerve shows a focal hypoechoic enlargement of its medial portion (black arrowheads) associated with a blurred fascicular pattern. A sagittal sonogram obtained over the pathologic nerve (dotted line in b) shows a focal in-continuity neuroma (black arrowheads). Note the normal proximal and distal nerves (asterisks)
Fig. 12.
Complications after carpal tunnel surgery. Sagittal sonogram obtained at the palm, over a distal branch of the median nerve, in a patient with arthroscopic carpal tunnel release and persistent symptoms. A complete section of the nerve branch appears as a complete interruption (callipers). The proximal and distal stumps (white arrowheads) show a stump neuroma at their extremities (black arrowheads)
After surgery
Infections
Although not frequent, infections can complicate hand surgery. Depending on the location, US can assess the involvement of a joint space (Fig. 13) or a tendon sheath (Fig. 14). When a bone involvement is suspected, magnetic resonance imaging (MRI) is mandatory for optimal assessment. Soft-tissue abscesses are also well evaluated at US (Fig. 15).
Fig. 13.
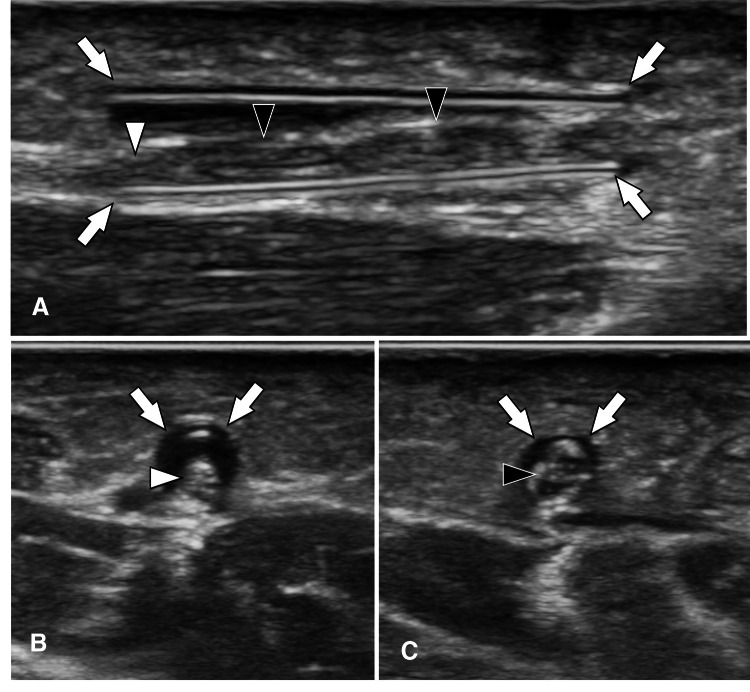
Postsurgical septic arthritis. Sagittal (a) and axial (b) colour Doppler sonograms, as well as sagittal T1-weighted (c) and transverse T1-weighted post-Gd-injection (d) MRI images, obtained at the proximal interphalangeal joint of the third finger in a patient presenting postsurgical septic arthritis. US shows hypertrophy of the synovium (asterisk) associated with erosion (arrow) of the dorsal aspect of the proximal phalanx (PP) head. In b, the important hypervascularisation of the synovium also extends into the periarticular soft tissues (curved arrow). MRI confirms the US appearance. In d, note the contrast enhancement of the synovium (asterisks), bone (arrow), and dorsal periarticular soft tissues (curved arrow)
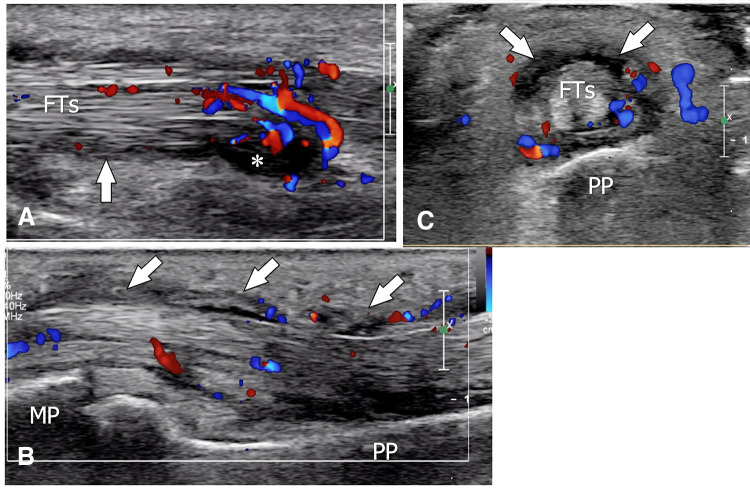
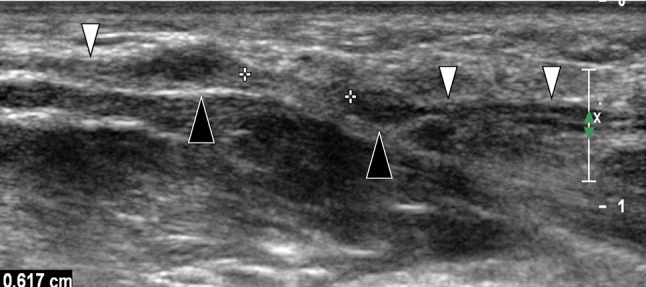
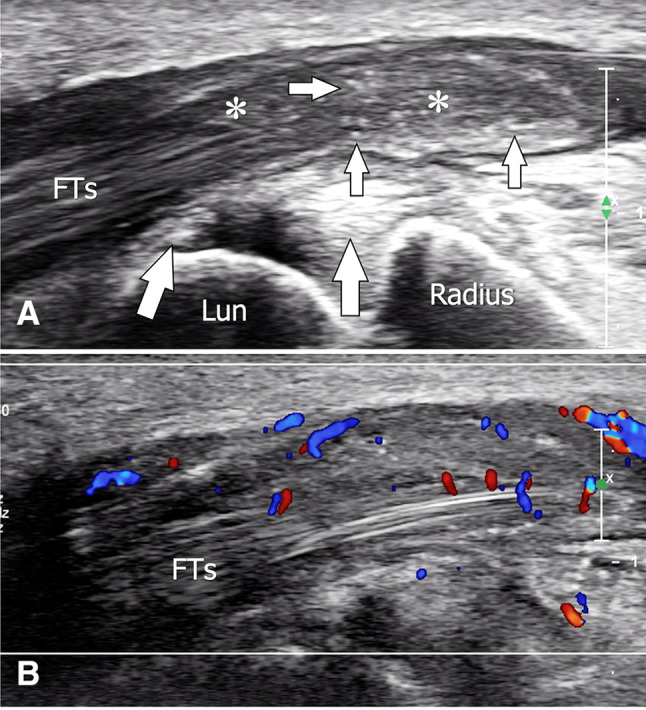
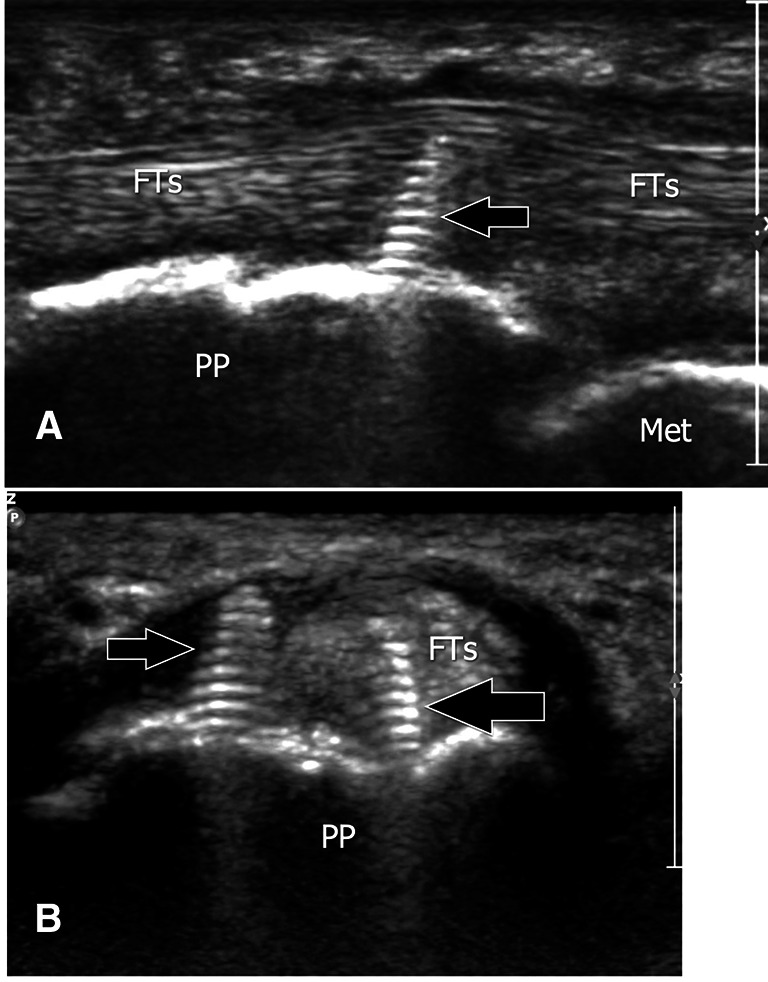
Fig. 14.
Postsurgical septic tenosynovitis. Sagittal (a, b) and axial (c) colour Doppler sonograms obtained over the flexor tendons (FTs) of the third finger in a patient presenting postsurgical septic tenosynovitis. US shows hypertrophy (arrows) and hypervascularisation of the common tendon sheath associated with a small amount of fluid (asterisk). MP middle phalanx, PP proximal phalanx
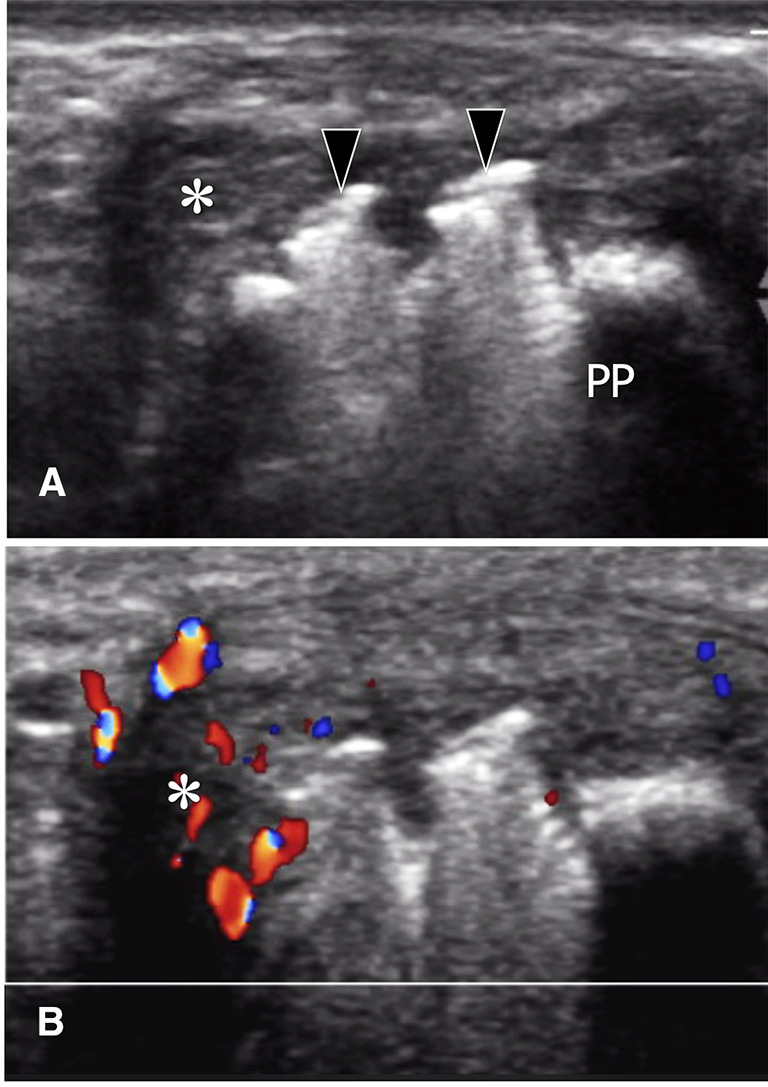
Fig. 15.
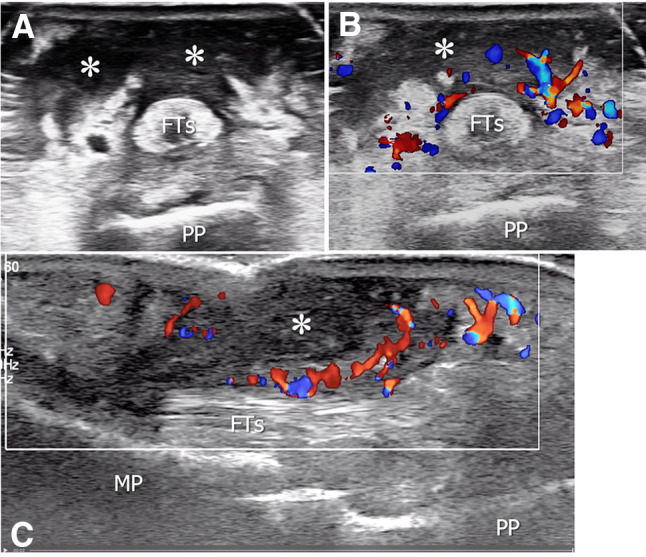
Postsurgical abscess. Axial greyscale (a) and axial and sagittal (b, c) colour Doppler sonograms obtained over the flexor tendons (FTs) of the fourth finger in a patient presenting a postsurgical palmar abscess. US shows a fluid collection (asterisks) with irregular borders and surrounded by hyperaemia at colour Doppler. FTs flexor tendons, MP middle phalanx, PP proximal phalanx
Arthritis and tenosynovitis
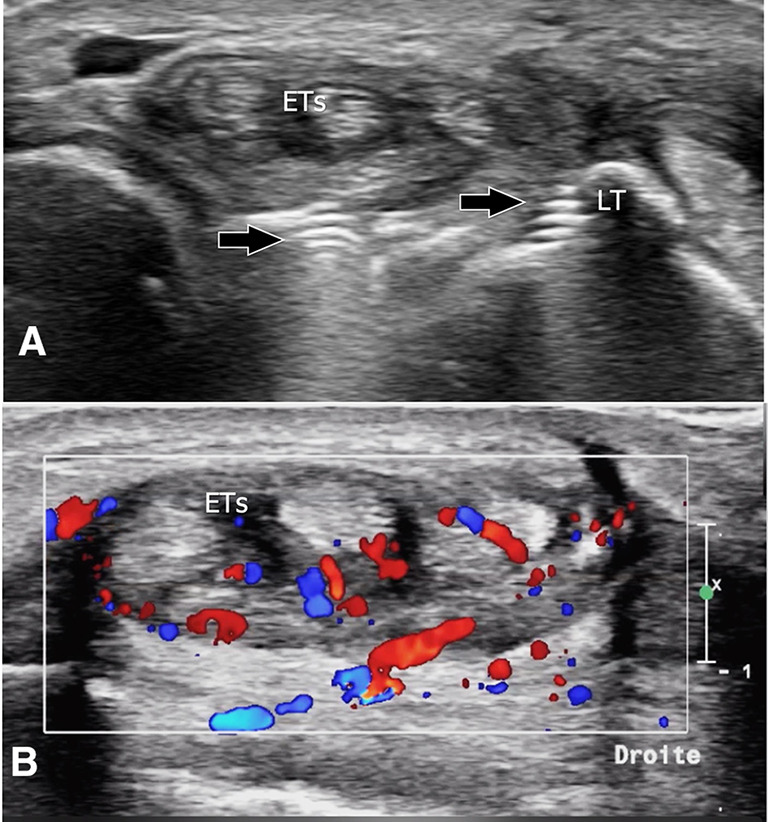
Acute arthritis or tenosynovitis affecting the hand and wrist in the postoperative period is usually related to gout (Fig. 16) or crystal pyrophosphate deposition disease (pseudogout, chondrocalcinosis) (Fig. 17). US easily detects local inflammatory changes with hypertrophy of the synovium showing hypervascular changes at colour Doppler [11]. A hyperechoic line on the cartilage surface indicates gout, while calcifications inside the cartilage and capsule point to calcium pyrophosphate deposition (CPPD). If an effusion is present, US can help in guiding a needle aspiration and subsequently allowing examination with polarised light for a definite diagnosis.
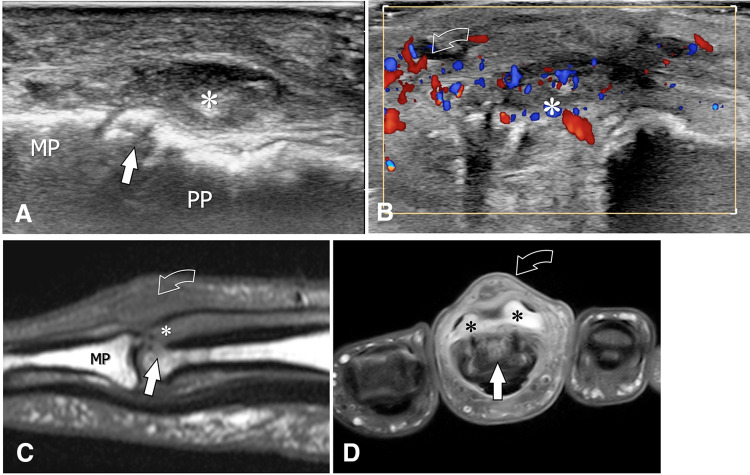
Fig. 16.
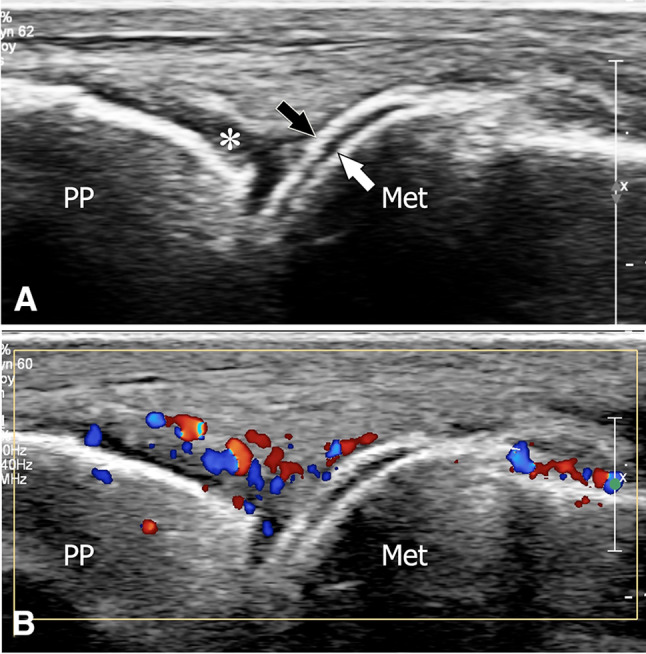
Acute postsurgical gout. Sagittal (a) and sagittal colour Doppler (b) sonograms obtained at the dorsum of the metacarpophalangeal joint of the index in a patient with gout presenting postsurgical monoarthritis. In a, note the hyperechoic linear band (black arrow) located at the surface of the cartilage (white arrow) of the metacarpal head. The hyperechoic line corresponds to the deposition of urate crystal on the cartilage surface. The asterisk points to synovial hypertrophy. In b, note the hypervascular changes inside the synovium. PP proximal phalanx, Met metacarpal
Fig. 17.
Acute postsurgical pseudogout. Sagittal (a) and sagittal colour Doppler (b) sonograms obtained over the carpal tunnel in a patient with crystal pyrophosphate deposition disease presenting postsurgical tenosynovitis of the flexor digitorum tendons (FTs). In a, note the hypertrophy of the synovial tendon sheath (asterisks) associated with multiple (small white arrows) internal hyperechoic spots due to crystal deposition. The larger arrows point to calcium deposition in the capsular palmar aspect of the radiocarpal joint. Lun lunate. In b, colour Doppler shows hypervascularity inside the inflamed tendon sheath
Tendon adhesions and re-tears
Tenorrhaphy of the tendons of the wrist and hand can be complicated by adhesions limiting gliding of the tendons and re-tear. The differential diagnosis between the two conditions can be difficult clinically. In adhesions, US shows ill-defined borders of the affected tendon in continuity with a hypoechoic area in the adjacent soft tissues (Fig. 18). Dynamic examination obtained during tendon movements (when feasible) confirms the diagnosis. In re-tear, tendon stumps can be detected as well as their degree of retraction (Figs. 19, 20, 21).
Fig. 18.
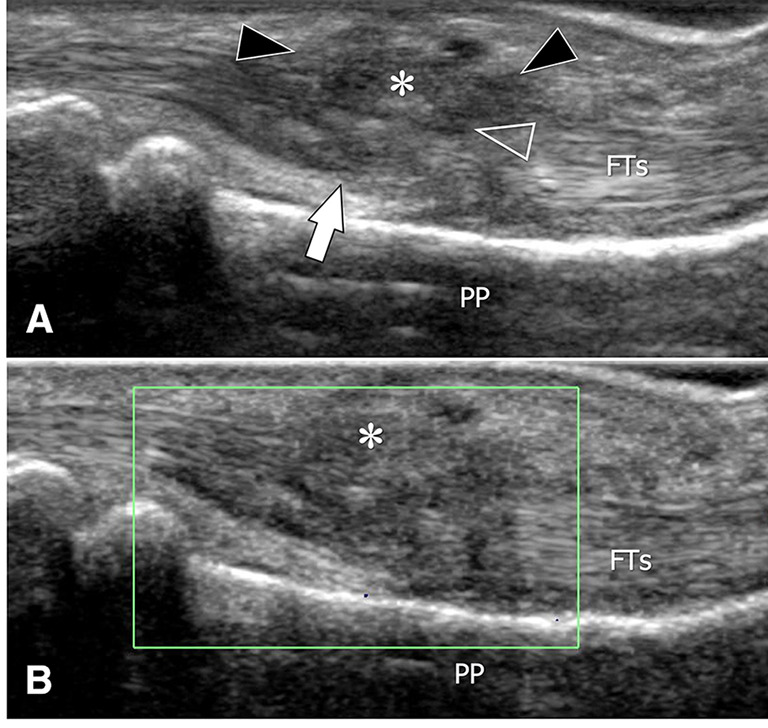
Adherences after tenorrhaphy of the flexor tendons of the third finger. Note the irregular appearance (white arrow) of the flexor tendons (FTs) secondary to surgery. A hypoechoic area (asterisk, black arrowheads) located inside the palmar soft tissue corresponds to adherences. Note that the limit between the adherences and the tendons (void arrowhead) is not appreciable. In b, the adherences do not show internal hyperemia
Fig. 19.
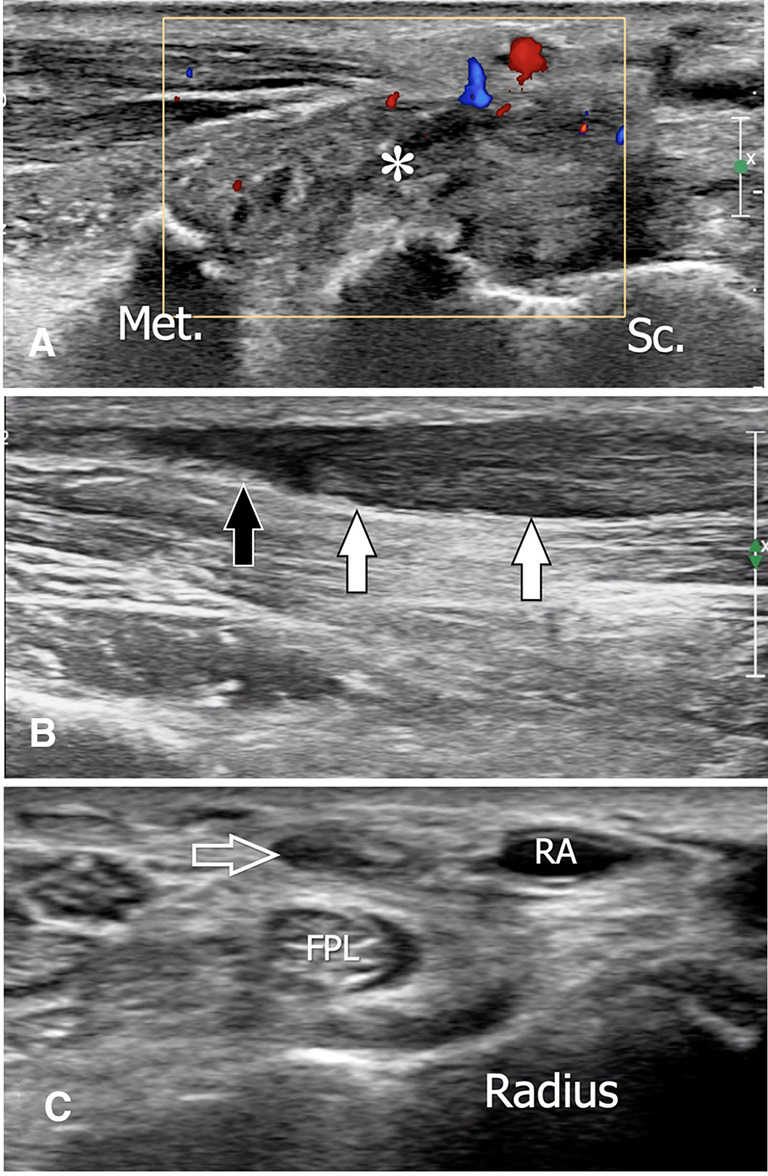
Tendon rupture after trapeziectomy. Sagittal (a, b) sonograms obtained over the wrist (a) and the distal metaphysis of the radius (b). Transverse (c) sonogram obtained over the distal epiphysis of the radius. The images were obtained for local pain in a patient with the previous trapeziectomy. In a, US shows local tear of the flexor carpi radialis tendon, which is replaced by a hypoechoic area (asterisk). b The tendon is retracted proximally and appears swollen and hypoechoic (white arrows). A small effusion is located inside the tendon sheath, distally to the tendon (black arrow). In c, the tendon sheath is empty (void arrow). Met first metacarpal, Sc scaphoid, FPL flexor pollicis longus, RA radial artery
Fig. 20.
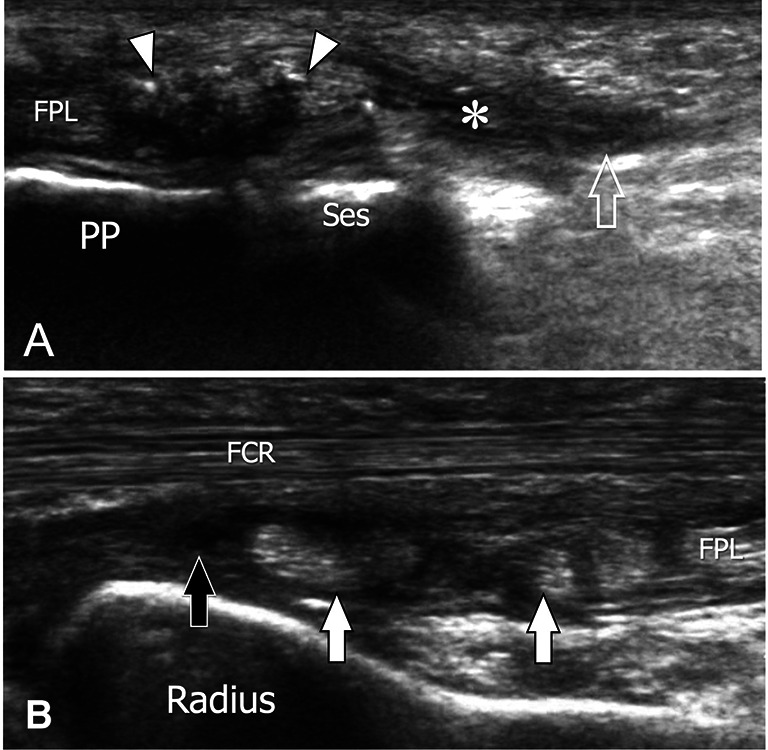
Tendon rerupture after suture. Sagittal sonograms obtained over the palmar aspect of the metacarpophalangeal joint of the thumb (a) and at the distal epiphysis of the radius (b) in a patient with retear of the flexor pollicis longus tendon. In a, US shows the irregular distal stump of the tendon (arrowheads). The tendon sheath (void arrow) proximally to the stump presents a hypoechoic content (asterisk). In b, the retracted tendon shows a wrinkled appearance. The tendon sheath distal to it contains a small amount of fluid (black arrow). FPL flexor pollicis tendon, PP proximal phalanx, Ses ulnar sesamoid, FCR flexor carpi radialis
Fig. 21.
Tendon rerupture after suture. Dorsal sagittal (a) and transverse (b) sonograms obtained over the third metacarpal in a patient with re-rupture of the D3 extensor tendon. In (a), US shows the two stumps of the tendon (white arrows). The proximal stump (asterisk) is retracted (dashed line) and contains some surgical stitches (arrowhead). The proximal tendon is surrounded by an area of inflammation associated with hyperaemia at colour Doppler (b)
Complications related to orthopaedic hardware
Impingement
The most frequent complications of orthopaedic hardware (OH) suitable to US assessment are tendon disorders due to protrusion of screws [1, 12] and impingement on the distal border of a palmar plate. Whereas MRI is limited by the presence of OH, US allows an accurate assessment of hardware impingement on local soft tissues. Fractures of the proximal phalanges treated by screw osteosynthesis can be complicated by tendon lesions due to the extrusion of screws causing a conflict with the flexor tendons (Fig. 22) or the dorsal soft tissues (Fig. 23). Open reduction and fixation by the volar plate is frequently performed for fractures of the distal radius when a significant dorsal tilt is present or in unstable fractures. Protrusion of the screw tip out of the dorsal cortex of the radius can lead to impingement of the dorsal tendons with subsequent tenosynovitis (Fig. 24) and partial (Fig. 25) or complete (Fig. 26) tendon tear.
Fig. 22.
Complication related to orthopaedic hardware. Sagittal (a) and transverse (b) sonograms obtained over the palmar aspect of the proximal phalanx of the fourth finger in a patient with previous surgical fixation of a P1 displaced fracture. The images show two screws (arrows) extruding from the palmar cortex of the phalanx. One screw (larger arrow) is located inside the flexor tendons (FTs) and was responsible for virtually absent gliding of the tendons at US dynamic examination. Met metacarpal
Fig. 23.
Complication related to orthopaedic hardware. Transverse greyscale (a) and colour Doppler (b) sonograms obtained over the dorsal aspect of the proximal phalanx of the third finger in a patient with previous surgical fixation of a displaced fracture of P1. The images show the heads (arrowheads) of two screws extruding from the cortex of the phalanx (PP). Impingement of the screws on the adjacent soft tissues is associated with a hypoechoic area of inflammation (asterisks). In b, note local hyperaemia
Fig. 24.
Complication related to orthopaedic hardware. Transverse greyscale (a) and colour Doppler (b) sonograms obtained over the dorsal aspect of the distal radius (a) and wrist (b) in a patient with extensor tendon tenosynovitis due to impingement on screws’ tips. In a, two screw tips are well demonstrated (black arrows) to be extruding from the bone’s dorsal cortex of the radius. Note the thickening or the tendon sheath surrounding the ETs. In b, colour Doppler shows intense local hyperaemia. LT lister tubercle
Fig. 25.
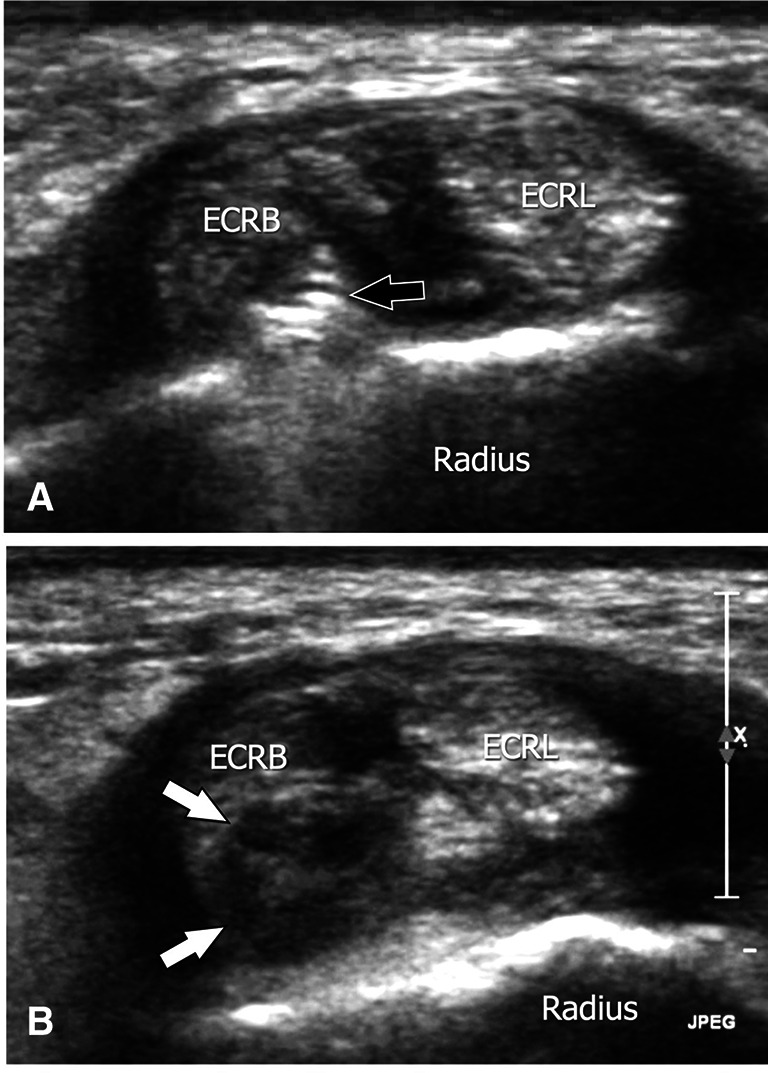
Complication related to orthopaedic hardware. Transverse (a, b) sonograms obtained from proximal (a) to distal (b) over the dorso-radial aspect of the distal radius in a patient with extensor carpi radialis brevis (ECRB) partial tear due to impingement on screws’ tips. In a, a screw tip is well demonstrated (black arrows) to be extruding from the cortex of the radius and penetrating the ERCB. In b, US shows a partial tear (white arrows) affecting the deep part of the tendon secondary to impingement on the screw’s tip. ECRL extensor carpi radialis longus
Fig. 26.
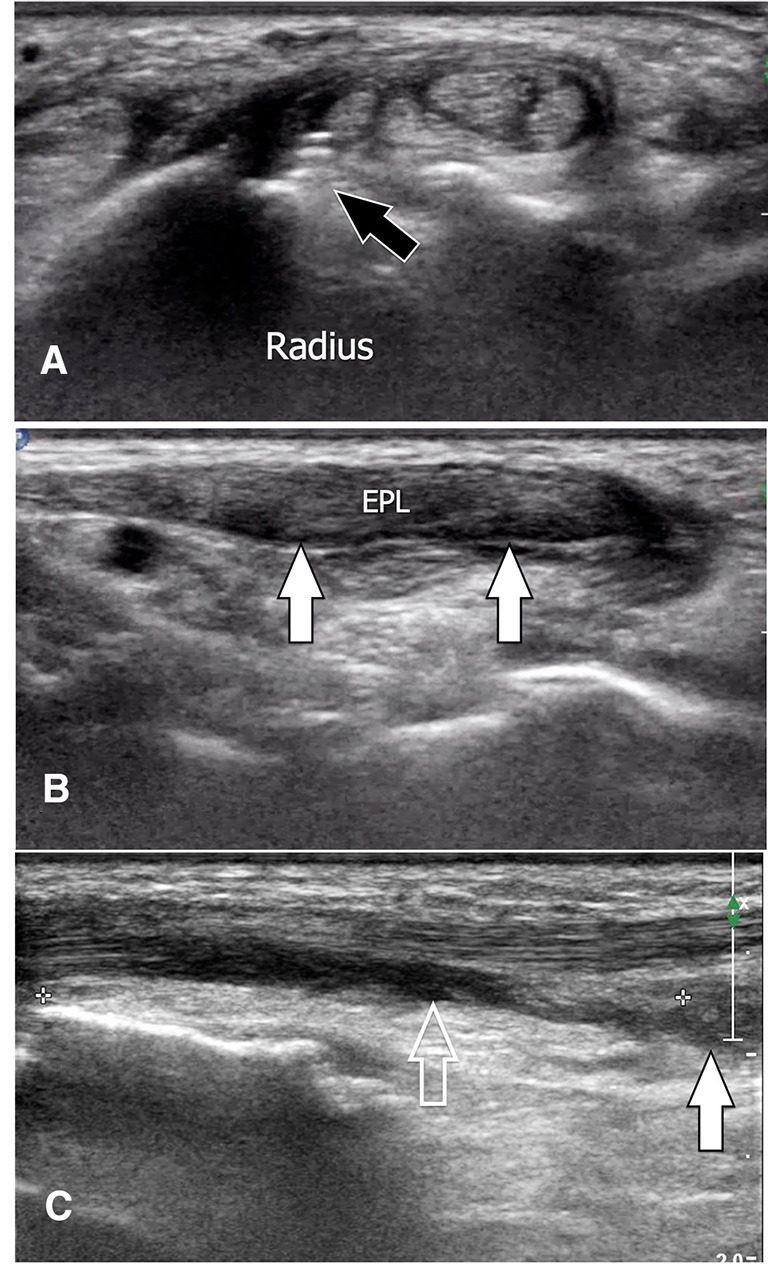
Complication related to orthopaedic hardware. Transverse (a) and longitudinal (b, c) sonograms obtained over the dorsum of the hand (b) and on the dorsal aspect of the distal radius (c) in a patient with a complete tear of the extensor pollicis longus (EPL) due to impingement on a screw’s tip. In a, a screw tip is well demonstrated (black arrows) to be extruding from the bone’s dorsal cortex of the radius. In b, US shows the distal hypoechoic swollen stump (arrows). In c, note the retracted proximal stump (white arrow). The void arrow points to the empty tendon’s sheath
Migration of screws
Migration of a screw can be easily demonstrated because of the tomographic capabilities of US. Dynamic examination allows a precise location of the screw (Fig. 27).
Fig. 27.
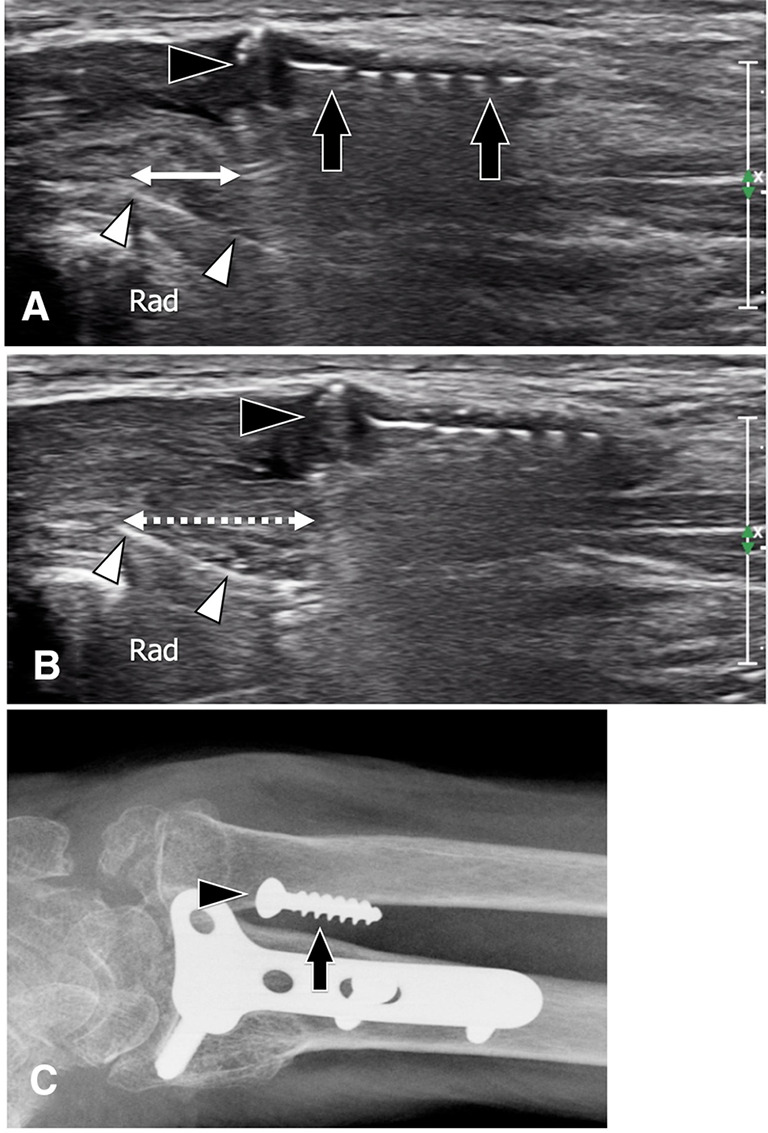
Complication related to orthopaedic hardware. Sagittal sonograms obtained at the palmar aspect of the distal forearm in a patient with the previous osteosynthesis for a radius fracture. The images were obtained with finger extension (a) and flexion (b). A surgical screw (arrows) is seen inside the palmar soft tissues. Arrowheads point to the screw head. The proximal displacement (larger double arrow) of the screw in (b) demonstrates its intramuscular location. Arrowheads indicate the surgical palmar plate. A conventional radiograph confirms migration of the screw inside the soft tissues
Gossypiboma
Gossypibomas are soft-tissue masses caused by a foreign body reaction to gauze left behind following surgery. They are rare in the hand. They present as heterogeneous masses with a central core showing a posterior shadowing (13) (Fig. 28).
Fig. 28.
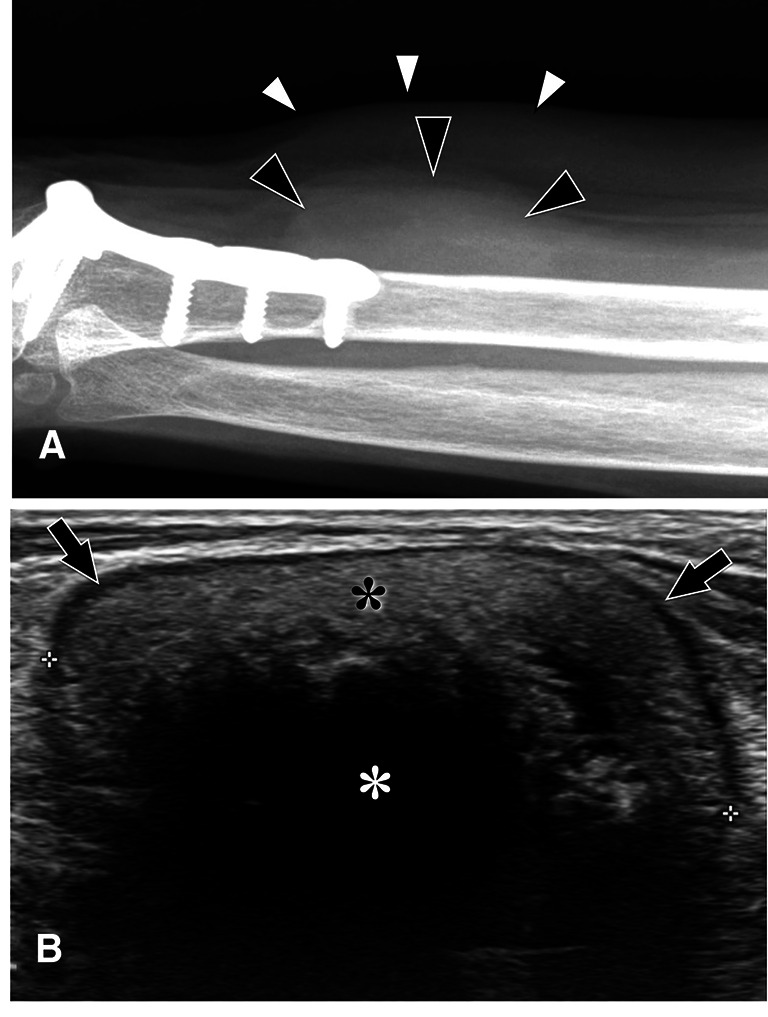
Complication related to orthopaedic hardware. L-L conventional radiograph (a) and sagittal sonogram (b) obtained over a painless soft tissue mass at the palmar aspect of the distal forearm in a patient with a previous radius fracture treated with a palmar plate. In a, a mass (black arrowheads) without internal calcification causes a bulging of the skin (white arrowheads). US (b) shows a hyperechoic mass (black asterisk) with a central anechoic core (white asterisk) and a peripheral hypoechoic pseudo capsule. Histology revealed a gossypiboma
Failed surgery
Sometimes surgery fails to treat very small glomus tumours (Fig. 29) or tiny foreign bodies (Fig. 30) because of their minuscule size. Persistence of symptoms after surgery indicates such a possibility. US can assess the persistence of these lesions. In these patients, the optimal sharing of US information between the sonologist and the hand surgeon is mandatory.
Fig. 29.
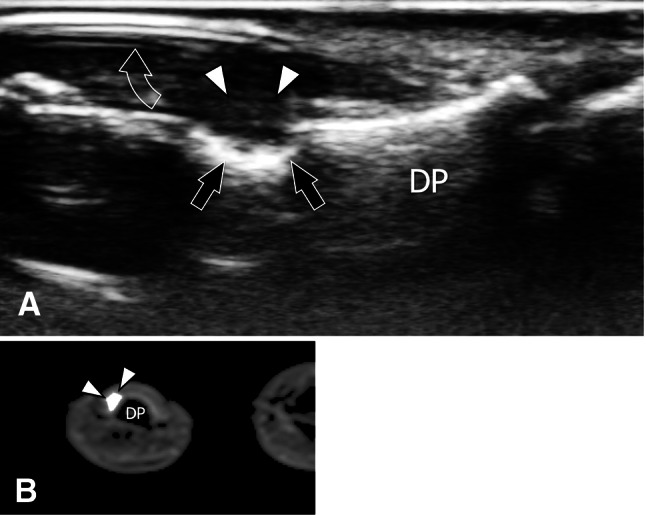
Persistent glomus tumour after negative surgical exploration. Sagittal sonogram (a) and transverse T1-weighted post-Gd-injection MRI image (b) obtained over the dorsal aspect of the distal phalanx (DP) in a patient presenting unchanged persistent excruciating pain after surgery for a glomus tumour. US shows the persistence of a glomus tumour (white arrowheads) located between the nail (void arrow) and the phalanx cortex. Note the surface erosion on the bone (black arrows) due to chronic local compression by the tumour. A second look at the MRI images revealed a small solid tumour showing contrast enhancement that was undetected at the first lecture
Fig. 30.
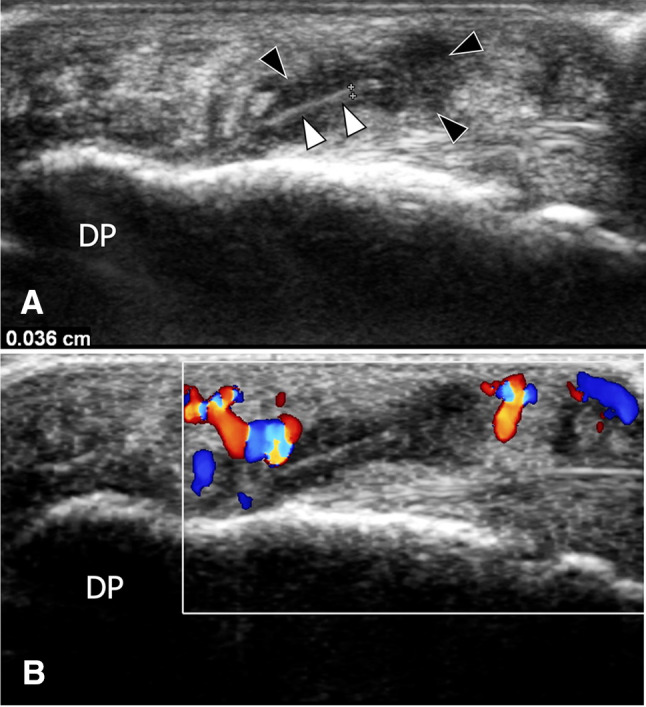
Persistent foreign body after negative surgical exploration. Sagittal greyscale (a) and colour Doppler (b) sonograms obtained on the fingertip of the fifth finger in a patient presenting persistent pain after negative surgical exploration for a suspected foreign body. In a, US shows a wood splinter (white arrowheads) located in the palmar soft tissue. The thickness (callipers) of the splinter is 0.36 mm. A hypoechoic area (black arrowheads) related to oedema surrounds the splinter. Colour Doppler shows local hypervascularisation related to inflammatory changes (b)
Conclusion
A variety of complications is commonly encountered in hand surgery in daily clinical practice. Knowledge of the medical history, as well as the symptoms and signs, is necessary for a correct diagnostic approach. However, imaging is often required to narrow down the list of different diagnoses. Apart from differential diagnosis, sonography is effective in assessing the complications of hand surgery, thus representing a valuable tool for ensuring appropriate management and limiting functional impairment.
Compliance with ethical standards
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical standards
This study was in accordance with the ethical standards of the institutional research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Gitto S, Draghi AG, Draghi F. Sonography of non-neoplastic disorders of the hand and wrist tendons. J Ultrasound Med. 2018;37:51–68. doi: 10.1002/jum.14313. [DOI] [PubMed] [Google Scholar]
- 2.Hoffman DF, Grothe HL, Bianchi S. Sonographic evaluation of hindfoot disorders. J Ultrasound. 2014;17:141–150. doi: 10.1007/s40477-014-0089-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bianchi S, Becciolini M, Urigo C. Ultrasound of disorders of small nerves of the extremities. Less recognized localizations. J Ultrasound Med. 2019;38:2821–2842. doi: 10.1002/jum.15014. [DOI] [PubMed] [Google Scholar]
- 4.Robotti G, Canepa MG, Bortolotto C, Draghi F. Interventional musculoskeletal US: an update on materials and methods. J Ultrasound. 2013;16:45–55. doi: 10.1007/s40477-013-0018-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Boeson MB, Hranchook A, Stoller J. Peripheral nerve injury from intravenous cannulation: a case report. AANA J. 2000;68:53–57. [PubMed] [Google Scholar]
- 6.Sheu JJ, Yuan RY. Superficial radial neuropathy following venipuncture. Int J Clin Pract. 2001;55:422–423. [PubMed] [Google Scholar]
- 7.Botchu R, Bharath A, Uhiara O, Davies M, James S. Iatrogenic Intratendinous ganglion cyst of the extensor digitorum tendon following intravenous cannulation. J Ultrasound. 2018;21(4):329–331. doi: 10.1007/s40477-017-0275-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Elliot D. Surgical management of painful peripheral nerves. Clin Plast Surg. 2014;41:589–613. doi: 10.1016/j.cps.2014.03.004. [DOI] [PubMed] [Google Scholar]
- 9.Arslantunali D, Dursun T, Yucel D, Hasirci N, Hasirci V. Peripheral nerve conduits: technology update. Med Devices (Auckl) 2014;7:405–424. doi: 10.2147/MDER.S59124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Tagliafico A, Pugliese F, Bianchi S, et al. High-resolution sonography of the palmar cutaneous branch of the median nerve. AJR Am J Roentgenol. 2008;191:107–114. doi: 10.2214/AJR.07.3383. [DOI] [PubMed] [Google Scholar]
- 11.Taljanovic MS, Melville DM, Gimber LH, et al. High-resolution US of rheumatologic diseases. Radiographics. 2015;35:2026–2048. doi: 10.1148/rg.2015140250. [DOI] [PubMed] [Google Scholar]
- 12.Bianchi S, Van Aaken J, Glauser T, et al. Screw impingement on the extensor tendons in distal radius fractures treated by volar plating: sonographic appearance. AJR Am J Roentgenol. 2008;191:W199–203. doi: 10.2214/AJR.08.1057. [DOI] [PubMed] [Google Scholar]
- 13.Urigo C, Moraux A, Bianchi S. Sonographic appearance of a soft-tissue gossypiboma in the forearm with pathologic correlation. J Clin Ultrasound. 2020;48:174–177. doi: 10.1002/jcu.22792. [DOI] [PubMed] [Google Scholar]