Abstract
Purpose
This is a rare case of a post-traumatic rectus abdominis muscle tear in an adolescent female diagnosed by ultrasonography (US). Conservative management is also described.
Methods
A 14-year-old female presented to a chiropractic clinic with extreme pain and tenderness in the right lower quadrant (RLQ) after post-plyometric power kneel box jumps. Movement aggravated her pain and she demonstrated active abdominal guarding with RLQ palpation. Ultrasonography revealed a subacute Grade 2 right rectus abdominis muscle tear, without evidence of hyperemia or a hematoma. Following the diagnosis of a right rectus abdominis muscle tear, she was treated with spinal manipulation and a course of musculoskeletal rehabilitation directed at truncal stabilization.
Results
After treatment, the patient was able to return to play 5 week post-injury without any pain or discomfort. A follow-up US at 3 months provided evidence of muscle healing without complications.
Conclusion
This case demonstrates the diagnosis of a rare rectus abdominis muscle tear managed conservatively. To our knowledge, less than a dozen cases are reported using US in the evaluation and diagnosis of a rectus abdominis tear.
Keywords: Rectus abdominis tear, Ultrasonography, Spinal manipulation, Muscle tear, Rehabilitation
Introduction
Acute muscle injuries frequently occur in both amateur and professional athletes, with approximately 30% of sports injuries resulting in muscle injury [1–5]. The normal appearance of muscle fibers on ultrasonography (US) is arranged in a parallel hypoechoic manner surrounded by echogenic fibro-fatty septa in pennate (long axis) and starry night (short axis) patterns. Disruption of the pennate and starry night pattern with enlargement, heterogeneity, and hypoechogenicity indicates a muscular tear [2, 3, 6–9]. Power Doppler may be used to detect local hyperemia or hematoma formation after muscular injury [10].
Muscle injury may occur as a result of external trauma leading to a contusion/compression rupture or from an indirect excessive tensile force leading to a distraction rupture. Distraction ruptures are classified into grades depending on the extent of the tear [9, 11–13]. The most commonly injured muscles are the hamstrings, rectus femoris, and the medial head of the gastrocnemius. In acute injuries, the muscle is damaged from an eccentric action and typically occurs at the myotendinous junction, the weakest link within the muscle tendon unit. In passive muscle injuries, it is secondary to tensile overstretch in the absence of muscle contraction [11, 14].
Diagnostic imaging is essential for classifying the extent of muscle injury, predicting feasible complications, guiding management, establishing recovery times, and determining the appropriate point of return to play [1, 3, 14]. The most commonly and widely used imaging techniques for muscle are US and magnetic resonance imaging (MRI) [3, 6]. Ultrasonography has a multi-planar approach and a dynamic component that demonstrates excellent spatial resolution and definition of normal muscle and pathology [2, 3, 10]. Ultrasonography has an overall sensitivity of 87.6% in correctly identifying muscle injuries. MRI allows for determination of small and large muscle injuries, as well as detection of minimal muscle alterations that are not macroscopically visible on US [1].
Ultrasonography provides for the evaluation of interval change in the muscular appearance and hyperemia through the reparative process. Skeletal muscle healing typically occurs over 3–7 weeks. During the healing phase, US may demonstrate complications that may arise from muscle tears. These complications include post-traumatic myositis ossificans, muscle hernias, and muscle cysts [2].
This case demonstrates a rare rectus abdominis muscle tear diagnosed by US and its conservative management. To our knowledge, less than dozen cases have used diagnostic US in the evaluation and diagnosis of a rectus abdominis tear.
Case report
A 14-year-old female presented to the chiropractic clinic with a chief complaint of right lower quadrant (RLQ) abdominal pain for 1 day. Her acute abdominal pain began after performing plyometric power kneel box jumps for softball conditioning. She described her pain as sharp and stabbing with occasional throbbing. The pain was aggravated by movement and resulted in shortness of breath. Patient denied radiation of symptoms and described her pain localized to the RLQ. This was her initial consultation and examination for this injury. Ibuprofen and ice did not relieve symptoms.
During the physical examination, she expressed extreme pain and tenderness during palpation of the RLQ. She rated her pain at a 7/10 on the verbal numeric rating scale (VNRS), with zero being no pain and ten being the most severe pain. There was extremely limited active and resisted right hip flexion due to pain. All other ROM were unremarkable. She was unable to cough or perform the Valsalva maneuver without eliciting pain. Palpation during Valsalva showed active abdominal guarding with extreme localized pain in the RLQ. Transitional movement from supine to sitting and sitting to standing created discomfort. Due to acuteness of injury and examination findings, no treatment was administered on the first visit. Ultrasonography was performed to evaluate the right lower abdominal wall with a pending diagnosis of athletic pubalgia.
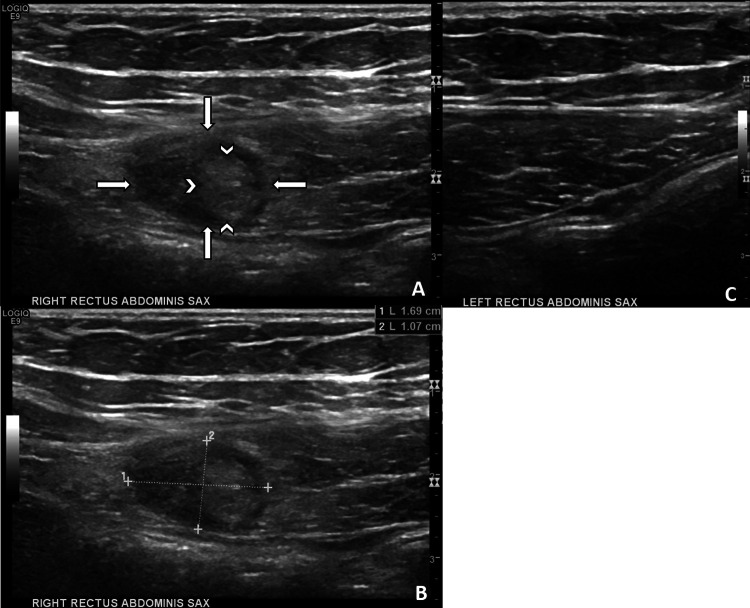
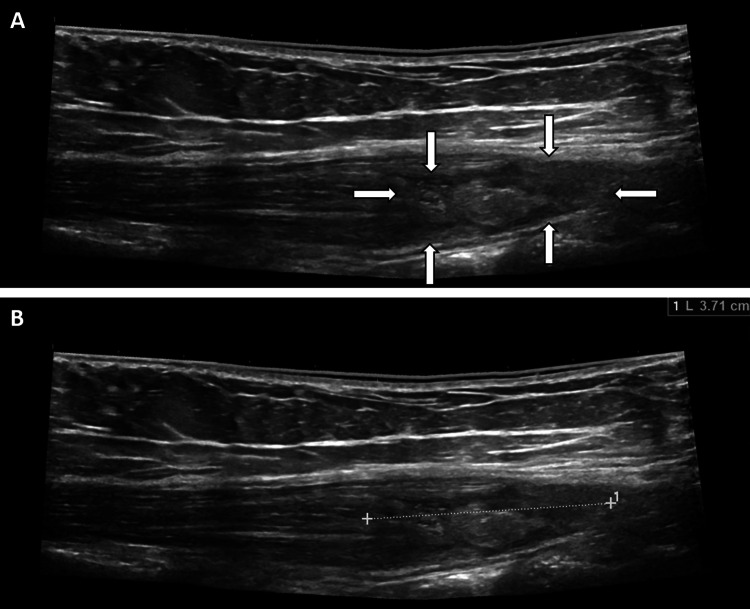
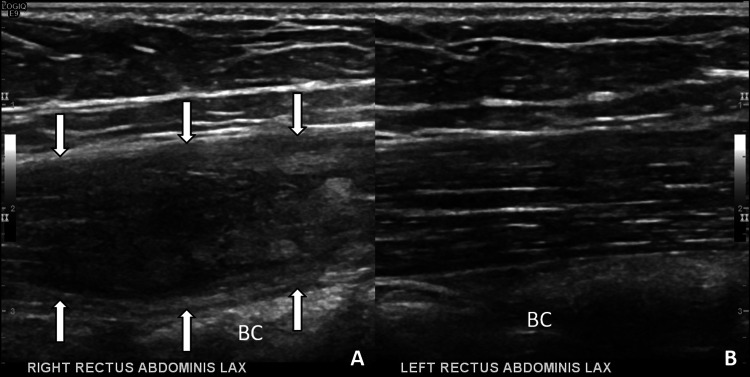
Ultrasonography revealed a 1.7 cm wide × 1.1 cm deep × 3.7 cm long heterogeneous, hypoechoic disruption of the normal starry night and pennate muscle pattern of the right lower rectus abdominis muscle (Figs. 1a, 2a, 3a). The left lower rectus abdominis displayed a normal starry night (Fig. 1c) and pennate (Fig. 3b) muscle pattern. In short axis, torn muscle fragments were visualized floating within the tear, which indicated the bell clapper sign (Fig. 1a). The tear was approximately 3 cm proximal to the pubis symphysis. The patient reported focal tenderness and pain with palpation over the abnormal muscle. There was no hyperemia or herniation of bowel content with Valsalva maneuver. There was no hematoma within the rectus sheath and no rectus fascial disruption. The remaining abdominal musculature and fascia were unremarkable. The final diagnosis was a subacute Grade 2 right rectus abdominis muscle tear.
Fig. 1.
Short-axis right rectus abdominis muscle. a There is an intramuscular heterogeneous hypoechoic tear of the rectus abdominis muscle (arrows) and visualization of the bell clapper sign within the tear (arrowheads). b Right rectus tear measured 1.69 cm wide × 1.07 cm deep. There is no adjacent hematoma or tear of the rectus sheath. c Normal left rectus abdominis muscle with visualization of the starry night pattern
Fig. 2.
Long-axis-extended field-of-view right rectus abdominis. a There is an intramuscular heterogeneous hypoechoic disruption of the normal pennate pattern in the distal one-third of the rectus abdominis muscle belly (arrows). b Tear measured 3.71 cm long. There is no evidence of a rectus sheath tear or hematoma
Fig. 3.
Long-axis comparison of the right and left rectus abdominis muscles. a There is expansion of the muscle contour and disruption of the pennate pattern (arrows), which is indicative of a tear of the right rectus abdominis muscle. b Normal left rectus abdominis muscle with visualization of the pennate pattern. BC bowel content
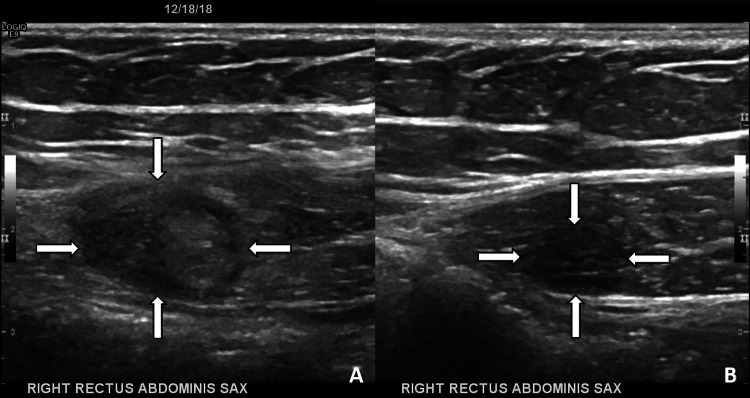
Subsequent to the US diagnosis of right rectus abdominis tear, the patient was treated 2×/week for 4 weeks. Treatment included spinal manipulation of the thoracic and lumbar spine after motion palpation revealed spinal restriction from T4 to T8 and T10 to L1. Additional treatment and rehabilitation was employed. Treatment included myofascial therapy, Class IV laser, and acupuncture/dry needling to decrease acute inflammation and severity of pain. Rehabilitation included dynamic neuromuscular stabilization (DNS) to improve use of the diaphragm in respiration and provide postural truncal stabilization. The patient was instructed to cease all physical sport-related activities for 2 weeks. She was then directed to gradually return to minimal activity (50% of energy expenditure) in the third week of care and moderate activity in the fourth week. After the fifth week post-injury, the patient was released and returned to play without any restrictions, pain, or discomfort. Three months after return to play, a follow-up US examination of the rectus abdominis was performed. Interval healing of the rectus abdominis tear in short and long axes was identified (Figs. 4, 5). The patient made a full recovery with no subsequent complications at 3 month follow-up.
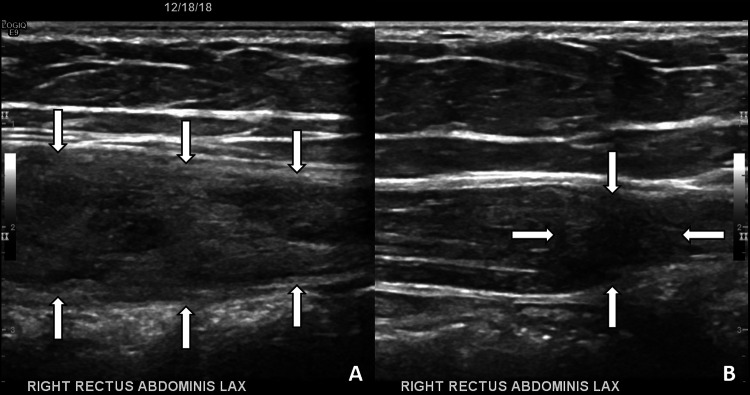
Fig. 4.
Short-axis interval healing of the right rectus abdominis muscle. a Acute tear of the right rectus abdominis (arrows) with visualization of the bell clapper sign. b At 3 month follow-up, volume reduction and resolution of the bell clapper sign is demonstrated
Fig. 5.
Long-axis interval healing of the right rectus abdominis muscle. a Acute tear of the right rectus abdominis (arrows). b At 3 month follow-up, volume reduction and restoration of the echogenic muscle perimysium was visualized
Discussion
The abdominal musculature plays a significant role in the stability of the trunk and core, as well as providing a mechanical link between the lower and upper extremities. The lower abdominal muscles function as both stabilizers and prime movers, which consequently exposes them to elevated risk of injury [7]. The rectus abdominis muscles are paired, strap-like, and separated by the midline linea alba aponeurosis. The muscles originate on the anterior surface of the pubis symphysis (medial head) and pubic crest (lateral head) and insert onto the fifth-to-seventh costal cartilages. A rectus abdominis tear can be difficult to differentiate from an intra-abdominal pathological process like appendicitis. To aid in clinical distinction, a key diagnostic clue is localized pain and tenderness that accentuates with muscle contraction and decreases with muscle relaxation [15]. To differentiate if the pain originates from the abdominal viscera or the abdominal wall, Carnett’s sign may be utilized during the clinical examination. Deep palpation is performed at the point of maximal abdominal pain. The patient is then asked to tense the abdominal muscles, while the point is released and is followed again with deep palpation. If the source of pain is from the abdominal wall, both stages of the test are painful. If the source of pain is from the abdominal viscera, only the first stage is painful [16].
The multi-planar approach of US demonstrates excellent spatial resolution and definition of muscle structure, tendons, and cartilage. The additional dynamic component allows for assessment of muscle contraction and capacity to characterize sonographic textures of muscular tissue. It is rapid and easily accessible, inexpensive, non-invasive, and ease of evaluation allows it to be the first line of examination [2, 3, 6, 8, 10, 14, 17–21]. In addition, US can reveal the muscle structure and other relevant anatomy surrounding an injury that can often be obscured by edema on MRI. After assessing at rest, US allows the same areas to be evaluated dynamically with active and/or passive muscular contraction. Dynamic evaluation allows for interpretation of altered muscle function, movement of disrupted fibers, and the consistency of the abnormal lesion [3, 10]. Connell et al. [7] concluded that MRI offered no advantage over US in making the diagnosis of rectus abdominis injuries. In addition, US is preferred to MRI in the pediatric setting, since it does not require sedation and allows for dynamic interpretation. The limitations with US in addition to being highly operator dependent include its limited field of view and inability to evaluate bone-marrow or intra-articular ligaments, since sound waves are not able to penetrate through the cortical bone [8, 13].
The main goal of US in muscle injury is to determine if a tear is present. If a muscle tear is present, the lesion will be qualified as severe and require a longer resting time. Hematoma formation is a key sign of a muscle tear. It will appear as a hypo- or anechoic circumscribed lesion in most cases [2]. Ultrasonography grading of muscular lesions are listed in Table 1 [2, 3]. Grade 0 is an absence of US lesion. Grade 1 represents minimal elongations with less than 5% of muscle fiber disruption and may have a normal appearance. Grade 2 refers to a partial rupture with greater than 5% of the muscle involved and may present with pain and loss of function. In this case, there was a Grade 2 tear of the right rectus abdominis revealing a hypoechoic gap of the muscle fibers. The bell clapper sign was observed in short axis. Grade 3 involves complete rupture of a muscle with fiber retraction [2–4, 11, 17, 22]. Maintaining the probe perpendicular to the underlying muscle avoids the anisotropy artifact, which can be mistaken for a muscle injury [8]. Ultrasonography Power Doppler detects signals from low flow vasculature and indirectly measures the number of red blood cells creating the Doppler frequency. Therefore, Power Doppler is able to depict neovascularity, which may be seen in the acute (hyperemic) and healing phases of muscle injury [7, 10].
Table 1.
| Ultrasonography muscle injury grading system | |
| Grade 0 | Lack of any ultrasonic lesion |
| Grade 1 | No abnormalities or focal/diffuse bleeding, hypoechoic area with no or < 5% fiber disruption |
| Grade 2 | Partial rupture with 5–50% muscle involved, partial muscle rupture with hypo- or anechoic gap, with or without fascial injury, with “bell clapper” sign |
| Grade 3 | Complete full-thickness tear of muscle or fascia with retraction |
The necessary healing time for a muscle tear is approximately 3–6 weeks for complete recovery, but is dependent on the extent of the lesion. Skeletal muscle heals by a reparative process, resulting in scar formation [5]. The larger the lesion, the greater volume of scar formation and increased duration of the healing process [2, 7]. Observable findings on US during normal muscular healing depend on the original nature of the injury. A Grade 1 injury will demonstrate increased echogenicity during healing and a reduction in size and/or resolution of echogenicity. Grade 2 injuries may appear more hypoechoic due to fluid adjacent to muscle fibrils or epimysium. Resolution of fluid is expected during a normal healing process. Over time, small tears may fill with echogenic material, likely representative of scar tissue formation [3]. Complications of muscle tears include post-traumatic myositis ossificans (more common), muscle hernias, and muscle cysts. Post-traumatic myositis ossificans (PTMO) occurs within skeletal muscle at the site of previous injury and/or hematoma [2, 13]. An additional complication of calcific tendinopathy may occur with migration to the myotendinous junction. This setting may impair function and generate pain [23].
There are a range of treatment methods from conservative care to surgical depending on the location and severity of the muscular tear. Conservative methods include rest, immobilization, Class IV laser therapy, nonsteroidal anti-inflammatory medications, functional rehabilitation, and physical therapy [14, 24–26]. As an example of functional rehabilitation, we employed DNS in this case to provide postural truncal stabilization and optimize recovery from muscle injury [25]. The duration of immobilization should be limited to allow time for sufficient scar production, then gradual return to activity within limits of pain tolerance. Early return to activity is advisable to optimize regeneration of healing muscle and to recover the injured muscle to pre-injury strength and flexibility. Surgical intervention is reserved for Grade 3 tears, which are complete tears of the muscle belly or of the myotendinous junction. Another surgical indication is a partial tear that is associated with persistent pain and loss of strength after a conservative trial of care. However, surgical repair of a muscle tear is difficult and the likelihood of clinical failure is high [13, 14]. Return to sport occurs when there is pain-free use and the ability to stretch the injured muscle with basic movements [13].
Limitations
Case reports have inherent limitations. As this is a single case report, parameters regarding diagnosis or treatment outcomes may not necessarily be applicable in other patients or the general public.
Conclusion
Ultrasonography is regarded as the first-line examination in the evaluation of muscle trauma. Ultrasonography is safe and readily available. It allows for muscular dynamic assessment, accurate depiction of the extent of injury, guides patient management, detects complications, and supports serial evaluation of the healing process. Conservative management is often the treatment of choice for muscle injury. We report a rare case of a rectus abdominis muscle tear and to the best of our knowledge, less than a dozen cases are reported.
Funding
No funding was received.
Compliance with ethical standards
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. This article does not contain any studies with animals performed by any of the authors.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Megliola A, Eutropi F, Scorzelli A, et al. Ultrasound and magnetic resonance imaging in sports-related muscle injuries. Radiol Med. 2006;111(6):836–845. doi: 10.1007/s11547-006-0077-5. [DOI] [PubMed] [Google Scholar]
- 2.Peetrons P. Ultrasound of muscles. Eur Radiol. 2002;12(1):35–43. doi: 10.1007/s00330-001-1164-6. [DOI] [PubMed] [Google Scholar]
- 3.Guermazi A, Roemer FW, Robinson P, Tol JL, Regatte RR, Crema MD. Imaging of muscle injuries in sports medicine: sports imaging series. Radiology. 2017;285(3):1063. doi: 10.1148/radiol.2017174038. [DOI] [PubMed] [Google Scholar]
- 4.Grassi A, Quaglia A, Canata GL, Zaffagnini S. An update on the grading of muscle injuries: a narrative review from clinical to comprehensive systems. Joints. 2016;4(1):39–46. doi: 10.11138/jts/2016.4.1.039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Jarvinen TA, Jarvinen TL, Kaariainen M, Kalimo H, Jarvinen M. Muscle injuries: biology and treatment. Am J Sports Med. 2005;33(5):745–764. doi: 10.1177/0363546505274714. [DOI] [PubMed] [Google Scholar]
- 6.Minardi J, Shaver E, Monseau A, Pratt A, Layman SM. Right lower quadrant pain in a young female: ultrasound diagnosis of rectus abdominis tear. J Emerg Med. 2015;49(5):623–626. doi: 10.1016/j.jemermed.2015.05.013. [DOI] [PubMed] [Google Scholar]
- 7.Connell D, Ali K, Javid M, Bell P, Batt M, Kemp S. Sonography and MRI of rectus abdominis muscle strain in elite tennis players. AJR Am J Roentgenol. 2006;187(6):1457–1461. doi: 10.2214/AJR.04.1929. [DOI] [PubMed] [Google Scholar]
- 8.Forney MC, Delzell PB. Musculoskeletal ultrasonography basics. Cleve Clin J Med. 2018;85(4):283–300. doi: 10.3949/ccjm.85a.17014. [DOI] [PubMed] [Google Scholar]
- 9.Hashimoto BE, Kramer DJ, Wiitala L. Applications of musculoskeletal sonography. J Clin Ultrasound. 1999;27(6):293–318. doi: 10.1002/(SICI)1097-0096(199907/08)27:6<293::AID-JCU1>3.0.CO;2-C. [DOI] [PubMed] [Google Scholar]
- 10.Pillen S, Boon A, Van Alfen N. Muscle ultrasound. Handb Clin Neurol. 2016;136:843–853. doi: 10.1016/B978-0-444-53486-6.00042-9. [DOI] [PubMed] [Google Scholar]
- 11.Chan O, Del Buono A, Best TM, Maffulli N. Acute muscle strain injuries: a proposed new classification system. Knee Surg Sports Traumatol Arthrosc. 2012;20(11):2356–2362. doi: 10.1007/s00167-012-2118-z. [DOI] [PubMed] [Google Scholar]
- 12.Draghi F, Zacchino M, Canepari M, Nucci P, Alessandrino F. Muscle injuries: ultrasound evaluation in the acute phase. J Ultrasound. 2013;16(4):209–214. doi: 10.1007/s40477-013-0019-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Jarvinen TA, Jarvinen TL, Kaariainen M, et al. Muscle injuries: optimising recovery. Best Pract Res Clin Rheumatol. 2007;21(2):317–331. doi: 10.1016/j.berh.2006.12.004. [DOI] [PubMed] [Google Scholar]
- 14.Maffulli N, Del Buono A, Oliva F, et al. muscle injuries: a brief guide to classification and management. Transl Med UniSa. 2015;12:14–18. [PMC free article] [PubMed] [Google Scholar]
- 15.Lacroix VJ. A complete approach to groin pain. Phys Sportsmed. 2000;28(1):66–86. doi: 10.3810/psm.2000.01.626. [DOI] [PubMed] [Google Scholar]
- 16.Tanizaki R, Takemura Y. Anterior cutaneous nerve entrapment syndrome with pain present only during Carnett’s sign testing: a case report. BMC Res Notes. 2017;10(1):503. doi: 10.1186/s13104-017-2816-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Lee JC, Healy J. Sonography of lower limb muscle injury. AJR Am J Roentgenol. 2004;182(2):341–351. doi: 10.2214/ajr.182.2.1820341. [DOI] [PubMed] [Google Scholar]
- 18.Jacobson JA, Khoury V, Brandon CJ. Ultrasound of the groin: techniques, pathology, and pitfalls. AJR Am J Roentgenol. 2015;205(3):513–523. doi: 10.2214/AJR.15.14523. [DOI] [PubMed] [Google Scholar]
- 19.Arend CF. Static and dynamic sonography for diagnosis of abdominal wall hernias. J Ultrasound Med. 2013;32(7):1251–1259. doi: 10.7863/ultra.32.7.1251. [DOI] [PubMed] [Google Scholar]
- 20.Kumbhare D, Shaw S, Ahmed S, Noseworthy MD. Quantitative ultrasound of trapezius muscle involvement in myofascial pain: comparison of clinical and healthy population using texture analysis. J Ultrasound. 2018 doi: 10.1007/s40477-018-0330-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Barbuto L, Di Serafino M, Della Vecchia N, et al. Pediatric musculoskeletal ultrasound: a pictorial essay. J Ultrasound. 2018;22(4):491–502. doi: 10.1007/s40477-018-0337-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Takebayashi S, Takasawa H, Banzai Y, et al. Sonographic findings in muscle strain injury: clinical and MR imaging correlation. J Ultrasound Med. 1995;14(12):899–905. doi: 10.7863/jum.1995.14.12.899. [DOI] [PubMed] [Google Scholar]
- 23.Cocco G, Ricci V, Boccatonda A, Iannetti G, Schiavone C. Migration of calcium deposit over the biceps brachii muscle, a rare complication of calcific tendinopathy: ultrasound image and treatment. J Ultrasound. 2018;21(4):351–354. doi: 10.1007/s40477-018-0336-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Souza J, Gottfried C. Muscle injury: review of experimental models. J Electromyogr Kinesiol. 2013;23(6):1253–1260. doi: 10.1016/j.jelekin.2013.07.009. [DOI] [PubMed] [Google Scholar]
- 25.Frank C, Kobesova A, Kolar P. Dynamic neuromuscular stabilization and sports rehabilitation. Int J Sports Phys Ther. 2013;8(1):62–73. [PMC free article] [PubMed] [Google Scholar]
- 26.Baoge L, Van Den Steen E, Rimbaut S, et al. Treatment of skeletal muscle injury: a review. ISRN Orthop. 2012;2012:689012. doi: 10.5402/2012/689012. [DOI] [PMC free article] [PubMed] [Google Scholar]