Abstract
Ultrasound (US) assessment of the wrist is frequently used for the evaluation of carpal tunnel due to high frequency of local compression of the median nerve (MN), but the ulnar–palmar wrist region (UPWR) has received limited attention in the medical literature. The possibilities of US in the assessment of UPWR are therefore likely underestimated by sonologists. This review article is focused on the US assessment of the normal anatomy and anatomic variations of the UPWR. The anatomy of this region of the wrist is complex and less studied than the radial side. In an effort to simplify it and to present it didactically, we have divided this region in three parts on the basis of osseous landmarks. Our review indicates sonography is effective in identifying the UPWR and related disorders, and is thus a valuable tool for ensuring appropriate management of a variety of disorders.
Keywords: Guyon’s canal, Ulnar nerve, Ulnar artery, Palmar carpal ligament, Transverse carpal ligament
Introduction
Ultrasound (US) assessment of the palmar aspect of the wrist is chiefly performed for evaluation of carpal tunnel due to the high frequency of local compression of the median nerve (MN).
US assessment of the ulnar–palmar wrist region (UPWR) has received less attention in the radiologic literature. Although the possibilities of US in the assessment of the UPWR are probably underestimated by sonologists, US enables a careful and accurate evaluation of local soft tissues because of their superficial location.
This review article is focused on the US assessment of the normal anatomy and anatomic variations of the UPWR.
Normal anatomy
The abbreviations of the main anatomic structures of the UPWR are listed in Abbreviation section in the order they appear in the article.
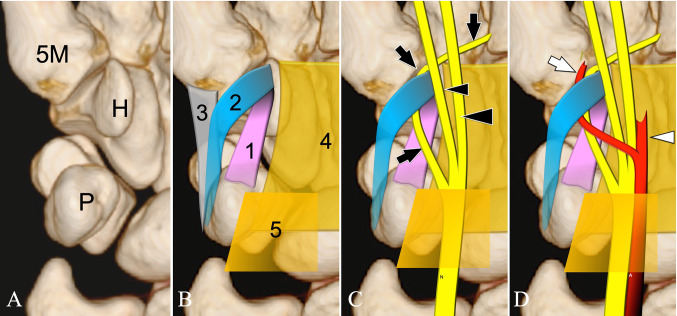
In an effort to simplify the UPWR anatomy and to present it didactically, we have divided this region in three parts on the basis of osseous landmarks (Fig. 1). The first part is located cranial to the proximal border of the pisiform bone (Pis). The second part corresponds to the Guyon canal (GC) [1]. The third part is located caudal to the distal border of the hook of the hamate bone (HH).
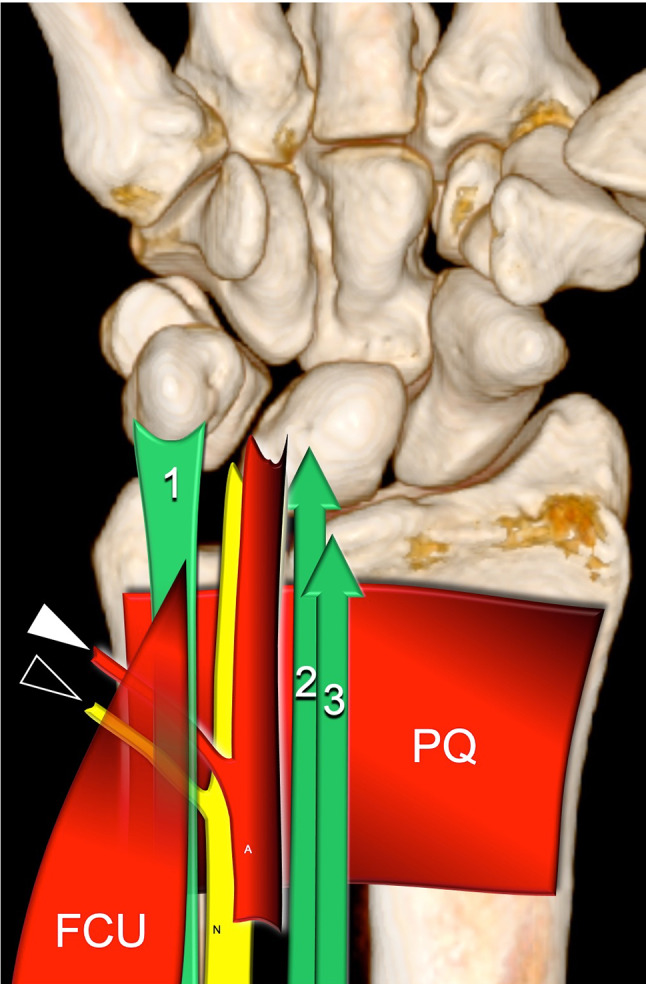
Fig. 1.
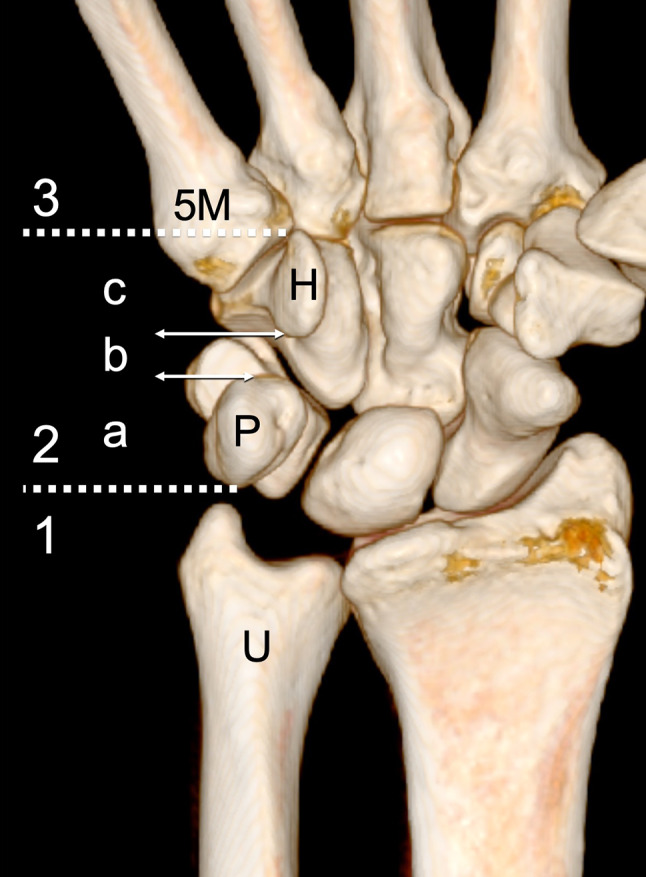
Palmar view of a reconstructed 3D CT of the wrist. Bone boundaries: fifth metacarpal (5 M), hook of the hamate (H), pisiform (P) and ulna (U). 1–3 correspond to the three regions as discussed in the text. For didactic purposes, the Guyon’s tunnel has been further divided in three parts (a–c)
First region
The main anatomic structures in this region are the flexor carpi ulnaris tendon (FCUt), the ulnar nerve (UN), and its dorsal cutaneous branch (DCBUN), the ulnar artery (UA), and the ulnar part of the pronator quadratus muscle (PQ) (Fig. 2). The region is delimited radially by the flexor tendons of the fifth finger.
Fig. 2.
The schematic drawing indicates the main anatomic structures of the first region (proximal to the pisiform). FCU = Flexor carpi ulnaris muscle and its tendon (1), PQ = pronator quadratus muscle. N = ulnar nerve and its dorsal cutaneous branch (black arrowhead), A = ulnar artery and its dorsal branch (white arrowhead), 2, 3 = flexor digitorum tendons of the fifth finger. Note that the dorsal branches of the ulnar nerve and artery run between the flexor carpi ulnaris and the pronator quadratus muscle
The FCUt is the most ulnar and palmar structure in the first region. It is a short, powerful tendon, not surrounded by a synovial sheath, that inserts into the proximal pole of the Pis. Its myotendinous junction is usually located 2–3 cm above the insertion, but sometimes the junction can be observed more distally, with some muscle fibers inserting directly into the sesamoid. The most palmar fibers of the ECUt overlie the Pis and continue distally into the pisohamate ligament (PHL). A small fiber contingent continues into the pisometacarpal ligament [2].
The UN and the UA descend together, lying radial to the FCUt. The artery runs radial to the nerve. The DCBUN is a small sensitive branch of the UN that detaches from its ulnar aspect to direct dorsally and then innervate the ulnar aspect of the dorsum of the hand [3]. A small branch of the UA runs close, usually in a more distal position, to the DCUN. Both travel between the flexor carpi ulnaris and the PQ muscle, a flat muscle located at the distal fourth of the volar forearm, deep into the flexor tendons of the fingers [4].
Second region: The GC
The GC is a conic canal with a larger cross-sectional area in its distal part [5]. It has a mean length of approximately 40 mm and extends from the proximal edge of the palmar carpal ligament (PCL) to the hook of the hamate bone (HH). We divided the GC in three regions to increase the clarity of the description (Fig. 1). The first region corresponds to the Pis level and the third to the HH level, while the second region lies between the two. The schematic appearance of the main anatomic structures lying in the GC are depicted in the coronal, sagittal, and axial drawings (Figs. 3, 4, 5).
Fig. 3.
Schematic drawings (a–d) indicate the main anatomic structures of the second region (Guyon’s tunnel). Coronal plane. a Bones: fifth metacarpal (5 M), hook of the hamate (H), pisiform (P). b Ligaments: pisohamate ligament (1), fibrous arcade of the hypothenar muscles (2), pisometacarpal ligament (3), transverse carpal ligament (4), palmar carpal ligament (5). c Nerves: Ulnar nerve (N) and its deep branch (black arrows). Proper digital nerve of the little finger (small black arrowhead) and the common digital nerve of the fourth webspace (large black arrowhead). d Arteries: Ulnar artery (A) and its deep (white arrow) and superficial (white arrowhead) branches
Fig. 4.
Schematic drawings (a–c) indicate the main anatomic structures of the second region (Guyon’s tunnel). Sagittal plane. a Ligaments and bones: pisohamate ligament (1), fibrous arcade of the hypothenar muscles (2), pisometacarpal ligament (3). Fifth metacarpal (5 M), hook of the hamate (H), pisiform (P). b Nerves: Ulnar nerve (N) and its deep branch (black arrows). Proper digital nerve of the little finger (small black arrowhead) and the common digital nerve of the fourth webspace (large black arrowhead). c Arteries: Ulnar artery (A) and its deep (white arrow) and superficial (white arrowhead) branches
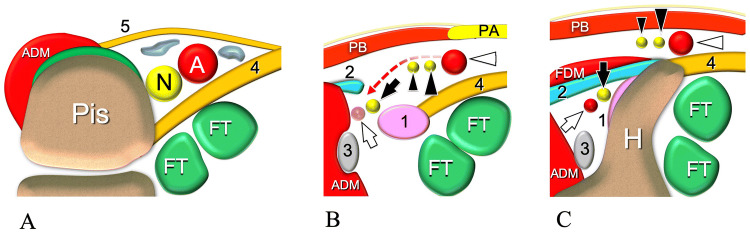
Fig. 5.
Schematic drawings indicate the main anatomic structures of the three parts of the Guyon’s tunnel. Axial plane. a, b drawings indicating the anatomy at the proximal (a), middle (b) and distal (c) parts. Bones: Pisiform (Pis), hook of the hamate (H). Muscles: abductor digiti minimi (ADM), palmaris brevis (PB) and flexor digiti minimi (FDM). Ligaments: pisohamate ligament (1), fibrous arcade of the hypothenar muscles (2), pisometacarpal ligament (3) transverse carpal ligament (4), palmar carpal ligament (5), palmar aponeurosis (PA). Nerves: Ulnar nerve (N). Deep branch of the ulnar nerve (black arrow). Proper digital nerve of the little finger (small black arrowhead) and the common digital nerve of the fourth webspace (large black arrowhead). Arteries: Ulnar artery (A). Deep (white arrow) and superficial (white arrowhead) branches of the ulnar artery. Tendons: flexor digitorum tendons of the fifth finger (FT)
Proximal part
At this level, the GC has a triangular appearance, with the base corresponding to the radial face of the Pis and the apex pointing radially (Fig. 5a). The roof is formed by the PCL, a local thickening of the antebrachial fascia that inserts into the FCU [6]. The floor is made by the transverse carpal ligament (TCL), which inserts into the deep-radial aspect of the Pis. The canal houses the UN, the UA, and two to three adjacent veins embedded in fat.
Middle part
This corresponds to the region located between the distal edge of the Pis and the proximal HH (Fig. 5b). Its floor is mainly formed by the ulnar part of the TCL, the PHL, while its roof is made by the hypothenar fascia [1, 6–8] and the palmaris brevis muscle (PBM). The ulnar aspect is bordered by the abductor digiti minimi muscle (ADM), while the radial aspect is bordered by the TCL. The UN, UA, and their branches lie superficial to the PHL, which originates from the Pis to direct distally and insert into the HH. Close to the distal edge of the Pis, the UN splits into its two terminal branches [6, 9]. The superficial branch (SBUN) is mostly sensitive, while the deep branch (DBUN) is purely motor [10]. The splitting of the UA into a superficial (SBUA) and deep (DBUA) branch occurs in a slightly more distal location.
The SBUN further divides into the proper digital nerve (PDN) of the little finger and the common digital nerve (CDN) for the fourth web space [11]. The division of the SBUN can sometimes be located more distally at the level of the distal part of the GC or distal to the tunnel [12]. According to Depukat, two other small branches within the canal originate from the SBUN: a cutaneous branch for the palmar skin and a motor branch for the palmaris brevis, the latter being the only motor branch of the SBUN [13]. The DBUN lies deep and ulnar to the SBUN. In general, the first branch of the DBUN is for the ADM, which may originate inside or outside the canal [6, 11, 14].
The SBUA and DBUA participate in the formation of the superficial and deep palmar arches, respectively. The larger SBUA runs close and radial to the SBUN, while the smaller DBUA joins the DBUN after crossing the SBUN from radial to ulnar and running superficial to it (Figs. 3, 4) [6].
Distal part
The distal part corresponds to the region of the HH. Two hiatuses, the superficial and the deep, are found at this level. They are separated by the fibrous arcade of the hypothenar muscles (FAHM), which inserts into the lateral face of the HH (Fig. 5c).
The SBUN and the SBUA run in the superficial hiatus, over the tip of the HH, protected by the PBM and the hypothenar fascia. The DBUN and the adjacent DBUA pass inside the deep hiatus, also called the pisohamate hiatus [15]. This is bordered by the distal PHL, the ulnar face of the HH and the FAHM, which forms the roof of the canal.
The GC then presents a proximal hiatus and two distal hiatuses. These are regions in which the vascular or nerve structures can be easily compressed by masses (proximal hiatus and pisohamate tunnel) or by external trauma (superficial distal tunnel) acting on the ulnar aspect of the palm (Fig. 6).
Fig. 6.
Axial schematic drawings indicate the inlet and outlets (heavenly area) of the Guyon’s tunnel. The levels of the proximal hiatus (a) and of the two distal hiatus (b) are indicated in the coronal drawing by the two dotted lines (A and B). In b, the black asterisk indicates the pisohamate hiatus, while the white asterisk indicates the superficial hiatus. Bones: Pisiform (P), hook of the hamate (H). Muscles: abductor digiti minimi (ADM), palmaris brevis (PB). Ligaments: pisohamate ligament (1), fibrous arcade of the hypothenar muscles (2), pisometacarpal ligament (3) transverse carpal ligament (4), palmar carpal ligament (5). Nerves: Ulnar nerve (N) and its deep branch (black arrow). Proper digital nerve of the little finger (small black arrowhead) and the common digital nerve of the fourth webspace (large black arrowhead). Arteries: Ulnar artery (A) and its deep (white arrow) and superficial (white arrowhead) branches. Tendons: flexor digitorum tendons of the fifth finger (FT)
Third region
At this level, the SBUN terminal branches, located superficial to the flexor tendons, direct to the ulnar side of the little finger (PDN) and to the fourth webspace (CDN). The DBUN points radially, accompanied by the DBUA, to innervate first the hypothenar muscles, and then the adductor pollicis and flexor pollicis brevis muscles [10] (Fig. 7).
Fig. 7.
Schematic drawings indicate the main anatomic structures of the hypothenar region. Coronal plane. a superficial plane. Hypothenar fascia (HF), palmar aponeurosis (PA) palmaris brevis muscle (PB) b deep plane. Abductor digiti minimi (A) flexor digiti minimi (B) opponens digiti minimi (C), fourth palmar interosseous muscle (PIM). Nerves: Ulnar nerve (N) and its deep branch (black arrows). Proper digital nerve of the little finger (small black arrowhead) and the common digital nerve of the fourth webspace (large black arrowhead). Note the deep branch of the ulnar nerve entering the pisohamate hiatus (curved arrow), delimited by the pisohamate ligament (1), and the fibrous arcade of the hypothenar muscles (2)
Located ulnar and distal to the GC, the three hypothenar muscles lie medially to the DBUN.
The medial ADM arises from the pisiform and the FAHM. The superficial flexor digiti minimi muscle (FDM) arises from the FAHM, while the opponens digiti minimi muscle (ODM) originates mainly from the hamulus. Its located first radial and then deep to the other two muscles (Fig. 7).
Us technique of examination and normal us anatomy of the guyon canal
US only allows for an accurate assessment of the UPWR if a rigorous examination technique is deployed. The patient has both hands lying supinated on the examination table. A brief history and a short clinical examination are obtained. Other imaging studies are reviewed if they are available. High-resolution broadband linear transducers are used. Small hockey-stick transducers allow a localized “US palpation,” which is helpful in evaluating a US Tinel test, for example [16]. We start the examination with transverse sonograms that enable simultaneous examination of several anatomic structures and thereby facilitate their identification. Longitudinal sonograms are then acquired for each structure.
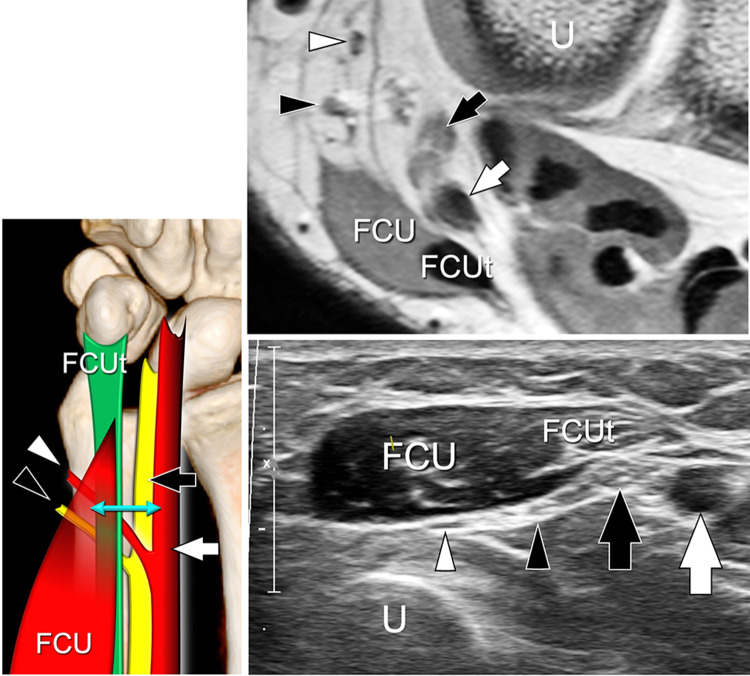
In the distal third of the forearm, the FCU originates from the radial part of its muscle. The UA is easily detected deep in it because of its pulsatility. The UN lies between the artery and the tendon, and presents a typical internal fascicular appearance. Accurate scanning shows the small DCBUN arising from its ulnar aspect (Fig. 8) and running palmar to the PQ. The small sensitive branch then crosses the medial border of the ulna, at an average distance from the styloid process of 17 mm, to innervate the dorso-ulnar part of the hand [3].
Fig. 8.
Normal US anatomy of the UPWR. First region. Schematic drawing in the coronal plane. Axial sonogram and corresponding T1-weighted MR image obtained at the level of the double arrow. Ulnar nerve (black arrows) and its dorsal cutaneous branch (black arrowheads), ulnar artery (white arrows), and its dorsal cutaneous branch (white arrowheads). 1, 2 = flexor digitorum tendons of the fifth finger. FCU = flexor carpi ulnaris muscle and its tendon (FCUt), U = ulna
At the proximal part of the GC, the Pis appears as a hyperechoic rounded structure with posterior acoustic shadow (Fig. 9) [16]. It is covered partially by the most superficial part of the FCU and medially by the origin of the ADM. Located medially to the Pis, the proximal hiatus of the GC has roughly a triangular shape. The UN is located between the Pis and the UA. The PCL and TCL appear as a fibrillar bands. While the thick TCL is always well imaged by US, the thin PCL can hardly be identified. Compression with a transducer allows for obliteration of the local veins inside the hiatus and simplifies the assessment of the UA and UN. Color Doppler is always performed to check the internal flow of the UA.
Fig. 9.
Normal US anatomy of the UPWR. Second region. Proximal part. Schematic drawing in the coronal plane. Axial sonogram and corresponding T1-weighted MR image obtained at the level of the double arrow. In the drawing, the quadrilaterum with dotted borders corresponds to the palmar carpal ligament. Ulnar nerve (black arrows), ulnar artery (white arrows). Pisiform (Pis). The black void arrowheads indicate the tendon of the flexor carpi ulnaris running over the pisiform. The white void arrowheads point to the most cranial fibers of the abductor digiti minimi muscle. The palmar carpal ligament is not visualized. The transverse carpal ligament is indicated by a curved arrow
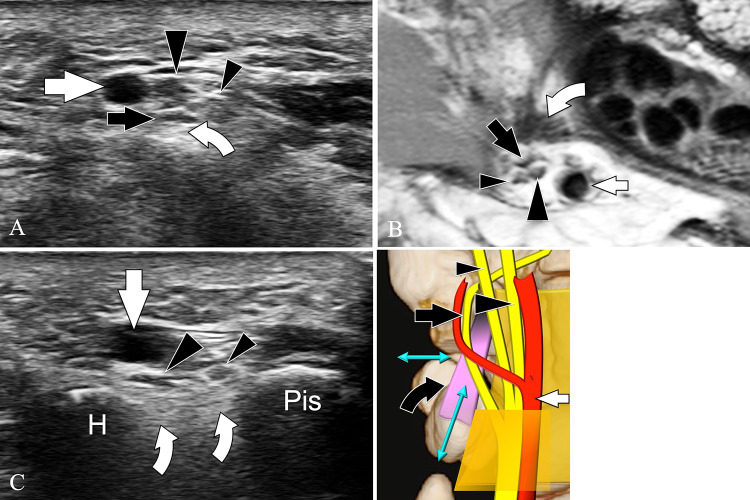
In the middle third of the GC, the tunnel is oval-shaped (Fig. 10). The PHL appears as a thin hyperechoic fibrillar structure extending from the pisiform to the HH. Longitudinal images are first acquired on the ligament, since they show it more easily. The transducer is then tilted during real-time scanning to image the ligament on the axial plane. The UN branches can be seen overlying it. Depending on the level of UN bifurcation, which is variable, two or three nerves, the DBUN, the SBUN and/or its divisional branches (PDN and CDN), can be found. In most subjects, US cannot detect SBUN branches for the PBM and the cutaneous branch for the hypothenar region because of their small size [13]. The DBUN becomes deeper and may appear hypoechoic at US due to its oblique path. It is rejoined, usually more distally, by the smaller DBUA, which can be difficult to detect because of its variability and small size. In some subjects, accurate US assessment can demonstrate a tiny nervous branch of the ADM detaching from the ulnar side of the DBUN (Fig. 11). After their identification on the axial plane, the UN, UA, and their branches are visualized by longitudinal sonograms. An accurate positioning of the transducers over each structure is necessary for optimal assessment (Fig. 12).
Fig. 10.
Normal US anatomy of the UPWR. Second region. Middle part. Schematic drawing in the coronal plane. Axial sonogram (a) and corresponding T1-weighted MR image (b) obtained at the level of the short double arrow. Longitudinal sonogram (c) obtained at the level of the long double arrow. The pisohamate ligament (curved arrows) appears on US as a hyperechoic fibrillar structure joining the pisiform (Pis) to the hook of the hamate bone (H). The ligament inserts into the tip of the hook. Note trifurcation of the ulnar nerve in the two sensitive (arrowheads) and the motor (arrows) terminal branches. Ulnar artery = white arrow
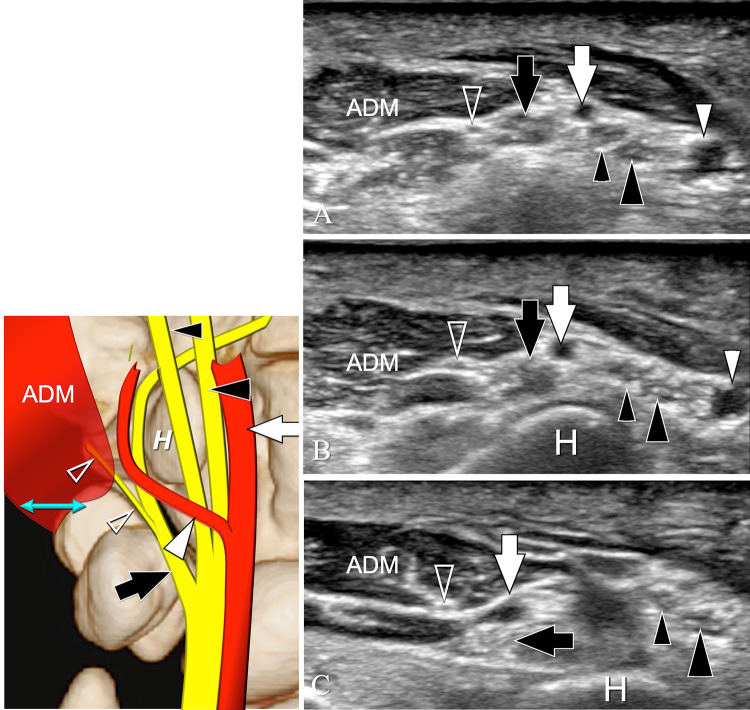
Fig. 11.
Normal US anatomy of the UPWR. Second region. Middle part. Schematic drawing in the coronal plane. Axial sonograms obtained from proximal (a) to distal (c). US shows the small nervous branch (void arrowhead) for the abductor digiti minimi muscle (ADM) detaching from the deep branch of the ulnar nerve (black arrows) (a) and pointing medially (b) to enter the muscle (c). Proper digital nerve of the little finger (small black arrowhead) and the common digital nerve of the fourth webspace (large black arrowhead). Deep (white arrow) and superficial (white arrowhead) branches of the ulnar artery. H = hamate hook
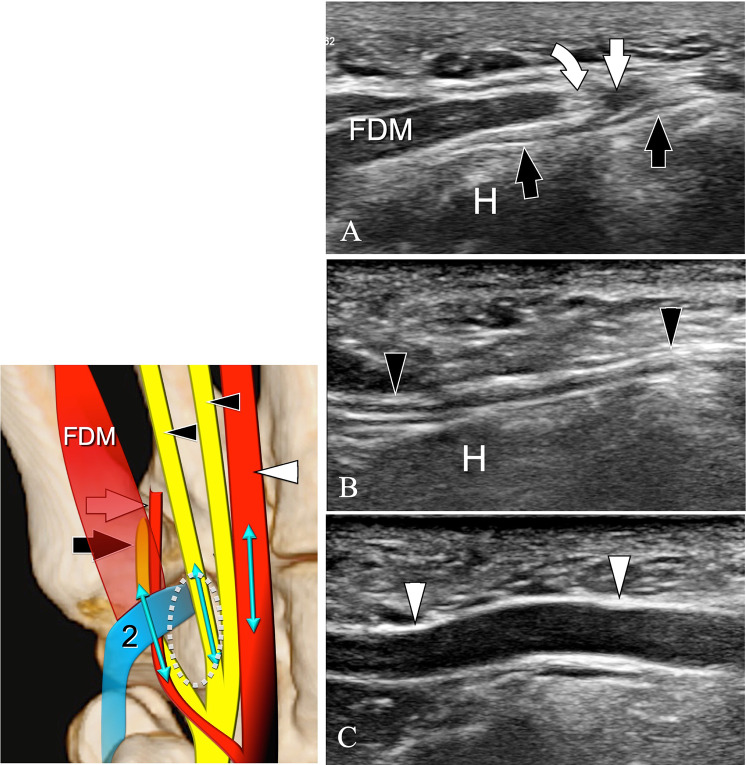
Fig. 12.
Normal US anatomy of the UPWR. Second region. Middle part. Schematic drawing in the coronal plane. Sagittal sonograms obtained from medial (a) to lateral (c) at the level indicated by the double arrows in the drawing. a US shows the flexor digiti minimi muscle (FDM) inserting into the fibrous arcade of the hypothenar muscles (curved arrow). The deep branch (black arrows) of the ulnar nerve runs first below the arcade and then under the FDM. The white arrow indicates the deep branch of the ulnar artery crossing over the deep branch. H = hook of the hamate. In a more lateral US image (b), a sensitive branch (black arrowheads) of the ulnar nerve travels superficial to the hamate hook. In a more lateral position (c), the superficial branch (white arrowheads) is depicted
In the distal third of the GC, at the level of the HH (Fig. 13), the two adjacent branches of the SBUN run medial to the larger SBUA. They are surrounded by fat and covered by the PBM, the subcutaneous tissues and the skin. The DBUN is more difficult to analyze with US because of its smaller size, location, and curvilinear path. For its optimal evaluation, sonograms must be obtained after tilting the transducer over the palmar–ulnar aspect of the wrist. The nerve runs close to the ulnar face of the HH, deep into the thin FAHM. The peculiar transducer orientation also facilitates the assessment of the ulnar face of the HH and the detection of HH fractures [17].
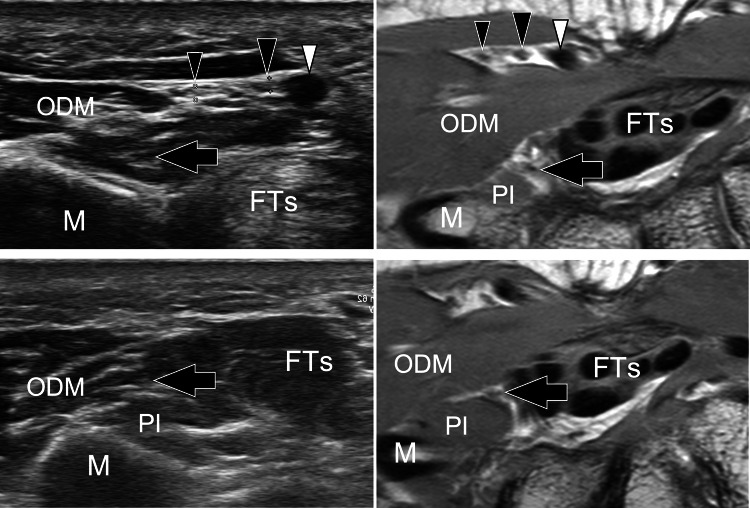
Fig. 13.
Normal US anatomy of the UPWR. Second region. Distal part. Schematic drawing in the coronal plane. Axial sonogram and corresponding T1-weighted MR image obtained at the level of the short double arrow in the drawing. H = hook of the hamate, FTs = flexor tendons inside the carpal tunnel, ADM = abductor digiti minimi muscle, PB = palmaris brevis muscle, asterisk = subcutaneous tissues. Deep branch (black arrow) of the ulnar nerve. Proper digital nerve of the little finger (small black arrowhead) and the common digital nerve of the fourth webspace (large black arrowhead). Deep (white arrow) and superficial (white arrowhead) branches of the ulnar artery. The two curved arrows point to the fibrous arcade of the hypothenar muscles. Note that the deep branches of the ulnar artery and nerve run below the arcade, while the superficial branches are located over it
More distally, the hypoechoic FDM is seen inserting into the thin hyperechoic FAHM. The muscle, together with the ADM and ODM, can then be followed distally by axial sonograms.
The US examination concludes with evaluation of the distal part of the UPWR (Fig. 14). The terminal, sensitive branches of the UN can be easily followed by transverse sonograms until the fingers. The DBUN is more difficult to follow because of its curvilinear path and position. It first runs deep to the ODM, between the palmar interossei and the flexor tendons, and then directs radially to reach the adductor pollicis and flexor pollicis brevis muscle [10].
Fig. 14.
Normal US anatomy of the UPWR. Third region. Axial sonograms and corresponding T1-weighted MR image obtained at the level of the proximal (upper images) and distal (lower images) portion of the third region. Proximally, the superficial branches of the ulnar nerve (black arrowheads) and artery (white arrowhead) are well demonstrated. The deep branch of the ulnar nerve (black arrows) runs among the flexor tendons of the fingers (FTs), the fourth palmar interosseous muscle (PI) and the opponens digiti minimi muscle (ODM). M = Fifth metacarpal
Anatomic variants
Anatomic variants of the UPWR are common and must be known by the sonologists to avoid misdiagnosis.
We describe here the main anatomic variants of the muscles, UA, UN, and bones.
Muscles
Variants of the distal myotendinous junction of the FCU have been classified into three types [2]. In type 1, the junction is located just proximal to the Pis; in type 2, the muscular belly ends proximally, with some fibers running parallel to the tendon and reaching the pisiform; in type 3, the myotendinous junction is proximal. Other variants of the FCU have previously been described [18, 19].
Variants of the ADM, including a single belly, two, or three bellies have been described. Distal insertions are usually at the proximal phalanx of the fifth finger and at the extensor aponeurosis; the latter distal attachment may be absent [20]. An accessory ADM muscle can be present, with frequency ranging from 25 to 35% of subjects [7, 9, 21]. The accessory muscle can originate proximally from the antebrachial fascia, the flexor carpi radialisor palmaris longus tendons to merge distally with the ADM [20]. In most cases, its position inside the proximal GC is palmar to the UA and UN (Fig. 15); less frequently, it is located between the two (Fig. 16) [22]. In our experience, the accessory muscle may also present two distinct bellies, radial, and ulnar to the UA, joining distally with the ADM (Fig. 17).
Fig. 15.
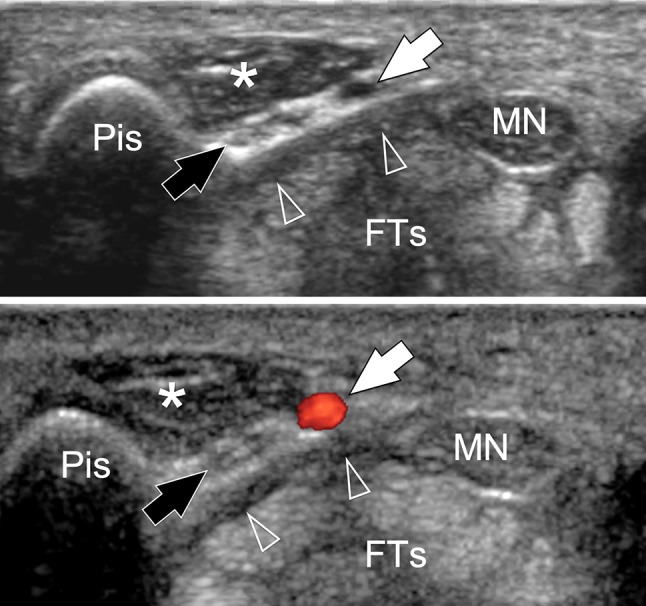
Anatomic variants of the UPWR. Accessory abductor digiti minimi muscle. Axial and axial color Doppler sonograms obtained at the level of the proximal part of the Guyon’s canal. Images show a well-defined mass (asterisks) presenting an internal structure typical of a muscle. The accessory muscle is located inside the Guyon’s tunnel and slightly compresses the ulnar nerve (black arrows) and artery (white arrows) against the transverse carpal ligament (void arrowheads). Pis = pisiform, MN = median nerve, FTs = flexor tendons of the fingers localized inside the carpal tunnel
Fig. 16.
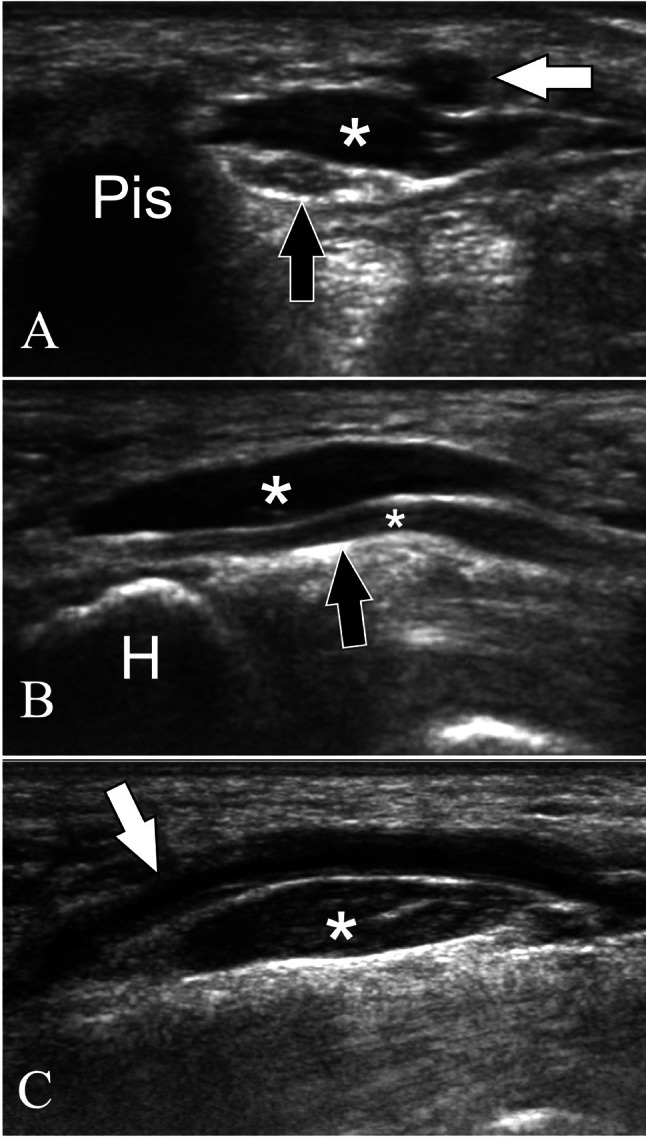
Anatomic variants of the UPWR. Accessory abductor digiti minimi muscle. Axial (a) and longitudinal (b, c) sonograms obtained at the Guyon’s canal. Images show a well-defined mass (asterisks) presenting an internal structure typical of a muscle. The accessory muscle is located inside the Guyon’s tunnel, between the ulnar nerve (black arrows) and artery (white arrows). Pis = pisiform, H = hamate hook
Fig. 17.
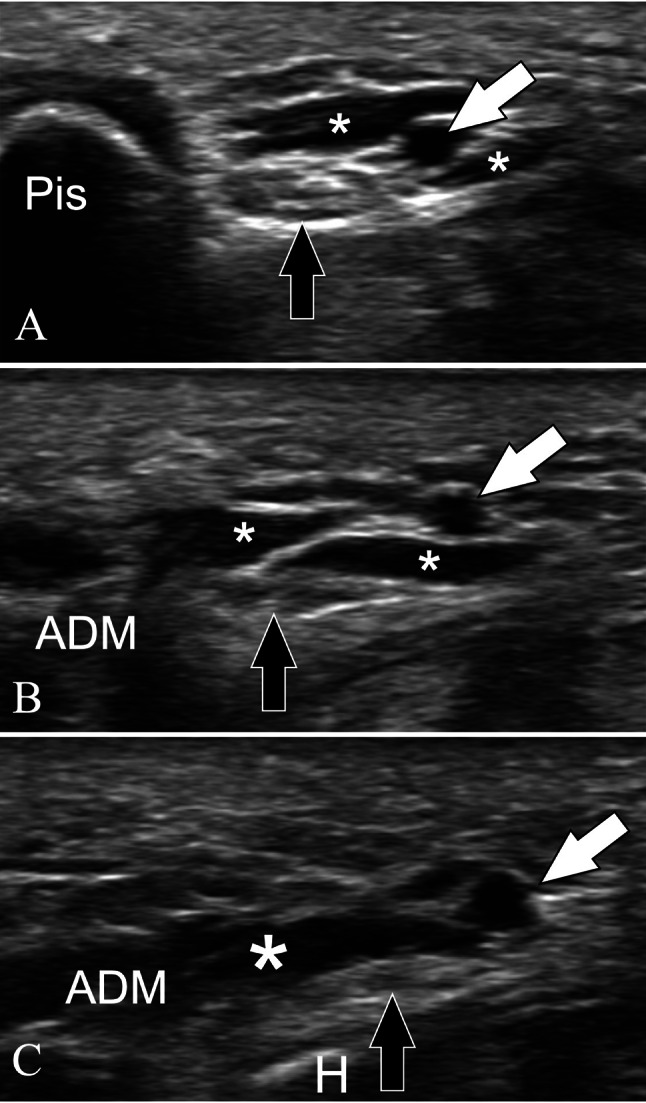
Anatomic variants of the UPWR. Accessory abductor digiti minimi muscle. Axial sonograms obtained from proximal (a) to distal (c) over the Guyon’s canal. Sonograms show an accessory abductor digiti minimi muscle that originates proximally via two distinct bellies (small asterisks). The bellies fuse distally to form a muscle (large asterisk) located between ulnar nerve (black arrows) and artery (white arrows). Pis = pisiform, ADM = Abductor digiti minimi, H = hamate hook
In some patients, the PBM can be hypertrophic [23]. Aplasia of the FDM was observed in 8/35 (Fig. 18) [11]. Sometimes, it is only composed of a tendon-like strip [20]. It usually fuses distally with the ADM, and may fuse proximally with the ODM muscle [11]. An anomalous FDM arising proximally from the antebrachial fascia has also been described, as has an accessory FDM, arising from the FCU and fusing distally with the FDM [24, 25]. The ODM may be absent as well, and may have an accessory head and/or accessory slips [20].
Fig. 18.
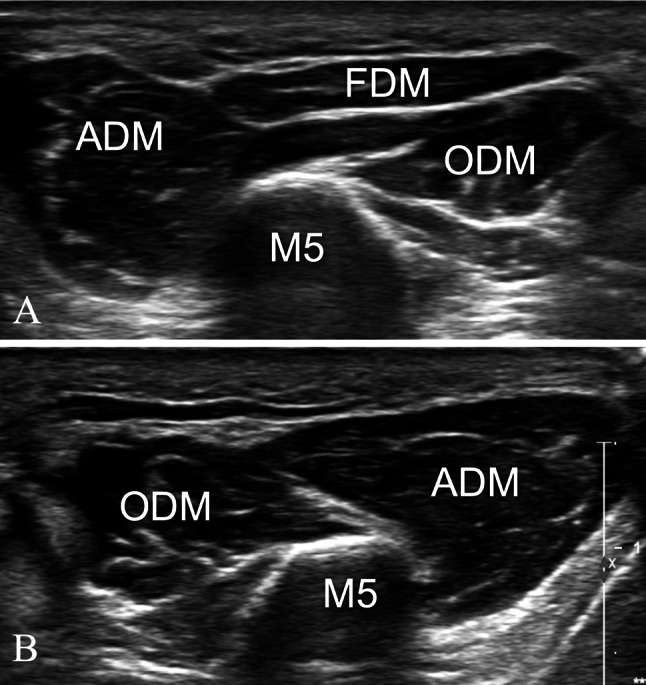
Anatomic variants of the UPWR. Aplasia of the flexor digiti minimi muscle. Axial sonograms obtained on the normal side (a) and the affected side (b). In a, the normal anatomy is depicted. Note the normal appearance of the abductor digiti minimi muscle (ADM), flexor digiti minimi muscle (FDM), and opponens digiti minimi muscle (ODM). The ADM is located medially and the FDM superficially and radially, while the ODM lies deep to the FDM. In b, the FDM is absent because of congenital aplasia. M5 = fifth metacarpal
UN variants
Variations of the UN at the forearm are common. Martin–Gruber anastomoses linking the UN and the median nerve have been reported in up to 39% of subjects [26, 27].
At the distal part of the forearm, the DCBUN, which is usually located between the FCU and PQ muscles [28], may run inside the FCU muscle (Fig. 19). The UN can divide before entering the GC [10, 12], but it usually bifurcates (70 to 86%) or trifurcates (13 to 30%) inside the tunnel [12]. Distal to the GC, anastomoses between the UN and the median nerve, such as the Riche–Cannieu and the Berrettini anastomose, have been reported [13, 26].
Fig. 19.

Anatomic variants of the UPWR. Ulnar nerve variants. Axial sonograms obtained: a on the proximal part of the dorsal cutaneous branch (black arrowheads) of the ulnar nerve (black arrows) and b in a more distal location. In a, the dorsal cutaneous branch runs below the flexor carpi ulnaris muscle (FCUm). In b, the small branch runs inside the muscle. Curved arrow = tendon of the flexor carpi ulnaris muscle. The arrowheads point to the space between the flexor carpi ulnaris muscle and the pronator quadratus muscle (PQ). White arrows = ulnar artery
UA variants
At the forearm, the UA can course inside the superficial fascia of flexor muscles (Fig. 20) in 0.7 to 9.4% of subjects [14, 29–32].
Fig. 20.

Anatomic variants of the UPWR. Ulnar artery variants. Axial sonogram obtained on the distal forearm. The ulnar artery (white arrow) courses inside the superficial fascia, together with two small veins (white arrowheads). Note that the artery is located at a distance from the ulnar nerve (black arrows), which lies in a normal position, close to the flexor carpi ulnaris muscle tendon (curved arrow)
At the level of the GC, the arborization of the UA is variable [33]. The DBUA can be absent [14, 33], hypoplastic, and show disparate origins and paths. At its proximal portion, it can run deep into the SBUN rather than superficial (Fig. 21), or it can enter the palm of the hand without entering the distal hiatus.
Fig. 21.
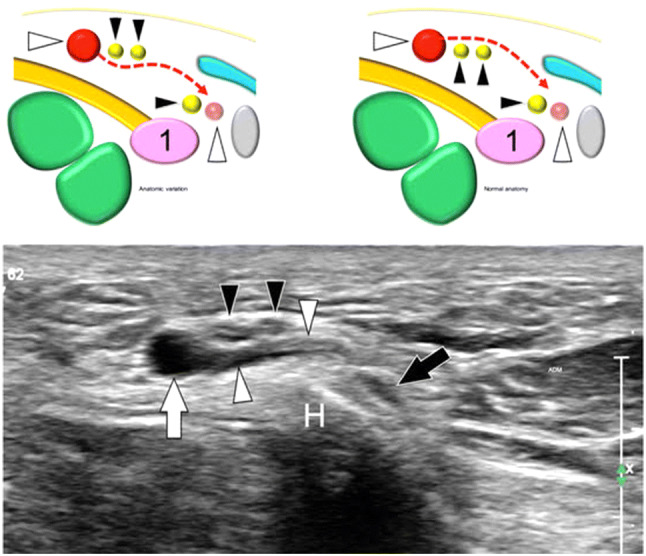
Anatomic variants of the UPWR. Ulnar artery variants. Axial sonogram obtained at the level of the hamate hook (H). Sonogram shows the superficial branch (white arrowheads) of the ulnar artery (white arrow) running under the two superficial branches (black arrowheads) of the ulnar nerve. This anatomic variation is demonstrated by the schematic drawing at left. The schematic drawing at right shows the normal anatomy for comparison. The black arrow points to the deep branch of the ulnar nerve running close to the hook of the hamate. ADM = abductor digiti minimi muscle
Bones
The Pis usually has one ossification center, which develops between the age of 9 and 12 years. Less frequently, the bone has two ossification centers that can unfuse with formation of an accessory ossicle, known as os pisiforme secondarium [34, 35]. Congenital absence of the Pis has been reported [35]. Pisiform–hamate coalition is a rare condition in which the two bones are joined by a band of cartilage/fibrous tissue (non-osseous coalition) or a continuous osseous bar (osseous coalition). Burnett reported five cases of this variation in the skeletal remains of 527 South Africans (0.76%) [36]. The condition is mostly asymptomatic, but can cause compression on the UN or median nerve and flexor tendons disorders [34].
The hamatum has two ossification centers, one for the body and one for the HH. A quite common variance is non-fusion of the centers with the formation of small rounded ossicle, the os hamuli proprium [37, 38]. Aplasia and hypoplasia of the HH was found in 1.6% of the 250 wrists studied by Pierre-Jerome with MRI. It may be the consequence of a mineral deficiency (Fig. 22) [5, 37].
Fig. 22.
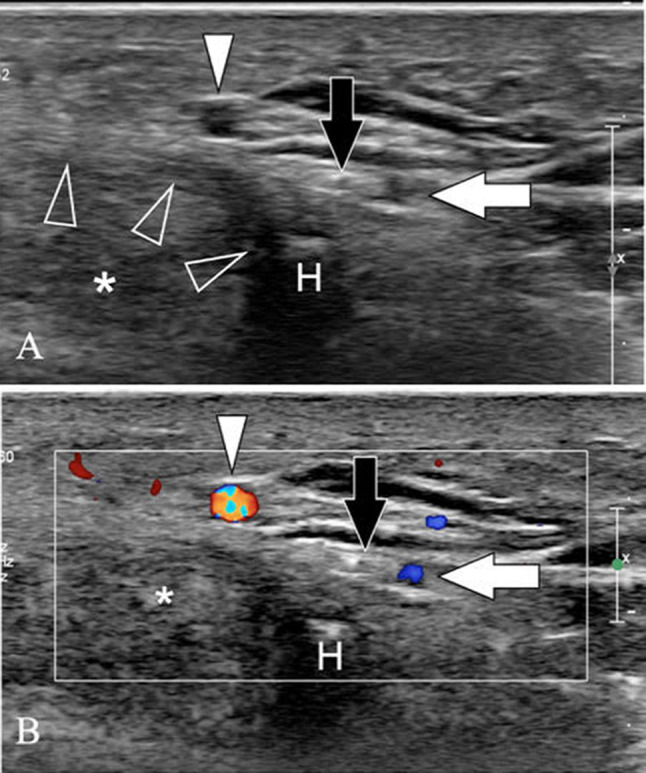
Anatomic variants of the UPWR. Hypoplasia of the hook of the hamate. Axial gray scale (a) and color Doppler (b) sonograms obtained at the level of the hamate hook (H). Sonogram shows the small size of the hook of the hamate. Note the distance between the hook and the superficial branch (white arrowheads) of the ulnar artery. The deep branches of the ulnar artery (white arrows) and ulnar nerve (black arrows) run palmar to the hook, and not medial, as usual. The transverse carpal ligament (void arrowheads) shows a convex appearance. Asterisks = flexor tendons of the fingers inside the carpal tunnel
Conclusion
The anatomy of the ulnar–palmar region of the wrist is complex and less studied than the radial side; sonography is effective in assessing the UPWR and related disorders; thus, representing a valuable tool for ensuring appropriate management of a variety of disorders.
Acknowledgements
We would like to acknowledge the invaluable help of Marco Becciolini MD.
Abbreviations
- FCU
Flexor carpi ulnaris
- PQ
Pronator quadratus
- GC
Guyon’s canal
- UA
Ulnar artery
- SBUA
Superficial branch of the ulnar artery
- DBUA
Deep branch of the ulnar artery
- UN
Ulnar nerve
- DCBUN
Dorsal cutaneous branch of the ulnar nerve
- DBUN
Deep branch of the ulnar nerve
- SBUN
Superficial branch of the ulnar nerve
- PDN
Proper digital nerve
- CDN
Common digital nerve
- PHL
Pisohamate ligament
- PCL
Palmar carpal ligament
- TCL
Transverse carpal ligament
- PBM
Palmaris brevis muscle
- ADM
Abductor digiti minimi
- FDM
Flexor digiti minimi muscle
- ODM
Opponens digiti minimi muscle
Compliance with ethical standards
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical standards
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Guyon F. Note sur une disposition anatomique propre à la face antérieure de la région du poignet et non encore décrite. Bulletin de la Societé anatomique, Paris. 1861;6:184–186. [Google Scholar]
- 2.Grechenig W, Clement H, Egner S, Tesch NP, Weiglein A, Peicha G. Musculo-tendinous junction of the flexor carpi ulnaris muscle. An anatomical study. Surg Radiol Anat. 2000;22(5–6):255–260. doi: 10.1007/s00276-000-0255-4. [DOI] [PubMed] [Google Scholar]
- 3.Le Corroller T, Bauones S, Acid S, Champsaur P. Anatomical study of the dorsal cutaneous branch of the ulnar nerve using ultrasound. Eur Radiol. 2013;23(8):2246–2251. doi: 10.1007/s00330-013-2832-z. [DOI] [PubMed] [Google Scholar]
- 4.Bianchi S, Martinoli C. Ultrasound of the musculoskeletal system. Berlin: Springer; 2007. Forearm; pp. 409–423. [Google Scholar]
- 5.Pierre-Jerome C, Moncayo V, Terk MR. The Guyon’s canal in perspective: 3-T MRI assessment of the normal anatomy, the anatomical variations and the Guyon’s canal syndrome. Surg Radiol Anat. 2011;33(10):897–903. doi: 10.1007/s00276-011-0842-6. [DOI] [PubMed] [Google Scholar]
- 6.Gross MS, Gelberman RH. The anatomy of the distal ulnar tunnel. Clin Orthop Relat Res. 1985;196:238–247. [PubMed] [Google Scholar]
- 7.Gil Y-C, Shin K-J, Lee J-Y, et al. Topographic anatomy of the ulnar tunnel. Surg Radiol Anat. 2015;37(7):757–764. doi: 10.1007/s00276-014-1415-2. [DOI] [PubMed] [Google Scholar]
- 8.Cobb TK, Carmichael SW, Cooney WP. Guyon’s canal revisited: an anatomic study of the carpal ulnar neurovascular space. J Hand Surg Am. 1996;21(5):861–869. doi: 10.1016/S0363-5023(96)80205-X. [DOI] [PubMed] [Google Scholar]
- 9.Zeiss J, Jakab E, Khimji T, Imbriglia J. The ulnar tunnel at the wrist (Guyon’s canal): normal MR anatomy and variants. Am J Roentgenol. 1992;158(5):1081–1085. doi: 10.2214/ajr.158.5.1566671. [DOI] [PubMed] [Google Scholar]
- 10.Riegler G, Lieba-Samal D, Brugger PC, et al. High-resolution ultrasound visualization of the deep branch of the ulnar nerve. Muscle Nerve. 2017;56(6):1101–1107. doi: 10.1002/mus.25614. [DOI] [PubMed] [Google Scholar]
- 11.Murata K, Tamai M, Gupta A. Anatomic study of variations of hypothenar muscles and arborization patterns of the ulnar nerve in the hand. J Hand Surg Am. 2004;29(3):500–509. doi: 10.1016/j.jhsa.2004.01.006. [DOI] [PubMed] [Google Scholar]
- 12.Niitsu M, Kokubo N, Nojima S. Variations of the ulnar nerve in Guyon’s canal: in vivo demonstration using ultrasound and 3 T MRI. Acta Radiol. 2010;51(8):939–946. doi: 10.3109/02841851.2010.503193. [DOI] [PubMed] [Google Scholar]
- 13.Depukat P, Henry BM, Popieluszko P, et al. Anatomical variability and histological structure of the ulnar nerve in the Guyon’s canal. Arch Orthop Trauma Surg. 2017;137(2):277–283. doi: 10.1007/s00402-016-2616-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Fadel ZT, Samargandi OA, Tang DT. Variations in the anatomical structures of the Guyon canal. Plast Surg. 2017;25(2):84–92. doi: 10.1177/2292550317694851. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Denman EE. The anatomy of the space of Guyon. Hand. 1978;10(1):69–76. doi: 10.1016/S0072-968X(78)80029-1. [DOI] [PubMed] [Google Scholar]
- 16.Bianchi S, Martinoli C. Ultrasound of the musculoskeletal System. Berlin: Springer; 2007. Wrist; pp. 425–494. [Google Scholar]
- 17.Celi J, De Gautard G, Della Santa JD, Bianchi S. Sonographic diagnosis of a radiographically undiagnosed hook of the hamate fracture. J Ultrasound Med. 2008;27(8):1235–1239. doi: 10.7863/jum.2008.27.8.1235. [DOI] [PubMed] [Google Scholar]
- 18.Ang GG, Rozen WM, Vally F, Eizenberg N, Grinsell D. Anomalies of the flexor carpi ulnaris: clinical case report and cadaveric study. Clin Anat. 2010;23(4):427–430. doi: 10.1002/ca.20952. [DOI] [PubMed] [Google Scholar]
- 19.Bhardwaj P, Bhandari L, Sabapathy SR. Supernumerary flexor carpi ulnaris—case report and review. Hand Surg. 2013;18(3):393–397. doi: 10.1142/S0218810413720222. [DOI] [PubMed] [Google Scholar]
- 20.Claassen H, Schmitt O, Schulze M, Wree A. Variation in the hypothenar muscles and its impact on ulnar tunnel syndrome. Surg Radiol Anat. 2013;35(10):893–899. doi: 10.1007/s00276-013-1113-5. [DOI] [PubMed] [Google Scholar]
- 21.Harvie P, Patel N, Ostlere SJ. Prevalence and epidemiological variation of anomalous muscles at Guyon’s canal. J Hand Surg Br. 2004;29(1):26–29. doi: 10.1016/j.jhsb.2003.08.004. [DOI] [PubMed] [Google Scholar]
- 22.Nam Y, Hwang S, Eo S. An aberrant abductor digiti minimi muscle crossing Guyon’s canal. J Wrist Surg. 2016;06(03):235–237. doi: 10.1055/s-0036-1597682. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kim DH, Bae JH, Kim HJ. Anatomical insights of the palmaris brevis muscle for clinical procedures of the hand. Clin Anat. 2017;30(3):397–403. doi: 10.1002/ca.22855. [DOI] [PubMed] [Google Scholar]
- 24.Madhavi C, Holla SJ. Anomalous flexor digiti minimi brevis in Guyon’s canal. Clin Anat. 2003;16(4):340–343. doi: 10.1002/ca.10087. [DOI] [PubMed] [Google Scholar]
- 25.Wahba MY, Singh GD, Lozanoff S. An anomalous accessory flexor digiti minimi profundus muscle: a case study. Clin Anat. 1998;11(1):55–59. doi: 10.1002/(SICI)1098-2353(1998)11:1<55::AID-CA9>3.0.CO;2-R. [DOI] [PubMed] [Google Scholar]
- 26.Al-Qattan MM, Alqahtani A, Al-Zahrani A. High trifurcation of the ulnar nerve with the volar sensory branch entering the hand superficial and radial to the Guyon’s canal: a case report. Int J Surg Case Rep. 2018;51:33–36. doi: 10.1016/j.ijscr.2018.08.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Lee KS, Oh CS, Chung IH, Sunwoo IN. An anatomic study of the Martin-Gruber anastomosis: electrodiagnostic implications. Muscle Nerve. 2005;31(1):95–97. doi: 10.1002/mus.20141. [DOI] [PubMed] [Google Scholar]
- 28.Rodrigues J, Santos-Faria D, Silva J, Azevedo S, Tavares-Costa J, Teixeira F. Sonoanatomy of anterior forearm muscles. J Ultrasound. 2019;22(3):401–405. doi: 10.1007/s40477-019-00388-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Kusztal M, Weyde W, Letachowicz K, Gołębiowski T, Letachowicz W. Anatomical vascular variations and practical implications for access creation on the upper limb. J Vasc Access. 2014;15(7_suppl):70–75. doi: 10.5301/jva.5000257. [DOI] [PubMed] [Google Scholar]
- 30.Senanayake KJ, Salgado S, Rathnayake MJ, Fernando R, Somarathne K. A rare variant of the superficial ulnar artery, and its clinical implications: a case report. J Med Case Rep. 2007;1:128. doi: 10.1186/1752-1947-1-128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Sato K, Murakami K, Mimata Y, Kikuchi Y, Oikawa R, Doita M. Superficial ulnar artery crossing over the palmaris longus tendon at the wrist in a cadaver: a case report. J Hand Surg. 2018;23(01):137–139. doi: 10.1142/S2424835518720074. [DOI] [PubMed] [Google Scholar]
- 32.Richards RS, Dowdy P, Roth JH. Ulnar artery palmar to palmaris brevis: cadaveric study and three case reports. J Hand Surg Am. 1993;18(5):888–892. doi: 10.1016/0363-5023(93)90061-7. [DOI] [PubMed] [Google Scholar]
- 33.Murata K, Tamai M, Gupta A. Anatomic study of arborization patterns of the ulnar artery in Guyon’s canal. J Hand Surg Am. 2006;31(2):258–263. doi: 10.1016/j.jhsa.2005.11.004. [DOI] [PubMed] [Google Scholar]
- 34.Moraux A, Lefebvre G, Pansini V, et al. Pisotriquetral joint disorders: an under-recognized cause of ulnar side wrist pain. Skeletal Radiol. 2014;43(6):761–773. doi: 10.1007/s00256-014-1848-z. [DOI] [PubMed] [Google Scholar]
- 35.Rayan GM. Pisiform ligament complex syndrome and pisotriquetral arthrosis. Hand Clin. 2005;21(4):507–517. doi: 10.1016/j.hcl.2005.08.010. [DOI] [PubMed] [Google Scholar]
- 36.Burnett SE. Hamate–pisiform coalition: morphology, clinical significance, and a simplified classification scheme for carpal coalition. Clin Anat. 2011;24(2):188–196. doi: 10.1002/ca.21086. [DOI] [PubMed] [Google Scholar]
- 37.Pierre-Jerome C, Roug IK. MRI of bilateral bipartite hamulus: a case report. Surg Radiol Anat. 1998;20(4):299–302. doi: 10.1007/BF01628496. [DOI] [PubMed] [Google Scholar]
- 38.Bianchi S, Abdelwahab IF, Federici E. Unilateral os hamuli proprium simulating a fracture of the hook of the hamate: a case report. Bull Hosp Jt Dis Orthop Inst. 1990;50:205–208. [PubMed] [Google Scholar]