Abstract
Background
Metabolic syndrome is an important risk factor for non-communicable diseases, particularly type 2 diabetes, coronary heart disease, and stroke. Long-term exposure to greenspace could be protective of metabolic syndrome, but evidence for such an association is lacking. Accordingly, we investigated the association between long-term exposure to greenspace and risk of metabolic syndrome.
Methods
The present longitudinal study was based on data from four clinical examinations between 1997 and 2013 in 6076 participants of the Whitehall II study, UK (aged 45–69 years at baseline). Long-term exposure to greenspace was assessed by satellite-based indices of greenspace including Normalized Difference Vegetation Index (NDVI) and Vegetation Continuous Field (VCF) averaged across buffers of 500 and 1000 meters surrounding the participants’ residential location at each follow-up. The ascertainment of metabolic syndrome was based on the World Health Organization (WHO) definition. Hazard ratios for the metabolic syndrome were estimated using Cox proportional hazards regression models, controlling for age, sex, ethnicity, lifestyle factors, and socioeconomic status.
Results
Higher residential surrounding greenspace was associated with lower risk of metabolic syndrome. An interquartile range increase in NDVI and VCF in the 500 m buffer was associated with 13% (95% confidence interval (CI): 1%, 23%) and 14% (95% CI: 5%, 22%) lower risk of metabolic syndrome, respectively. Greater exposure to greenspace was also associated with each individual component of metabolic syndrome, including a lower risk of high levels of fasting glucose, large waist circumference, high triglyceride levels, low HDL cholesterol, and hypertension. The association between residential surrounding greenspace and metabolic syndrome may have been mediated by physical activity and exposure to air pollution.
Conclusions
The findings of the present study suggest that middle-aged and older adults living in greener neighbourhoods are at lower risk of metabolic syndrome than those living in neighbourhoods with less greenspace.
Keywords: Metabolic syndrome, Longitudinal study, Cardiometabolic risk, Greenness, Built environment, Natural environment
Capsule
Our findings suggested that long-term exposure to greenspace may play a role in the prevention of metabolic syndrome in middle-aged and older adults, which could subsequently reduce the burden of non-communicable diseases.
Introduction
Non-communicable diseases (NCDs) such as cardiovascular conditions are the main cause of death worldwide (World Health Organization, 2014) and a major contributor to the global burden of disease in the older population (Prince et al., 2015). Metabolic syndrome, a cluster of conditions including obesity, hypertension, and impairment of lipids and glucose homeostasis (Galassi et al., 2006), is an important risk factor for NCDs, particularly type 2 diabetes, coronary heart disease, and stroke.
Currently, over 70% of the European population lives in cities (Kotzeva et al., 2016), where low levels of physical activity, sedentary behaviour, and exposure to air pollution, noise, and heat may increase the risk of metabolic syndrome (den Braver et al., 2018; Eze et al., 2015; Leal and Chaix, 2011; Matthiessen et al., 2018; Nieuwenhuijsen, 2018; Wallwork et al., 2017). In addition, urban residents often have limited access to greenspace, while recent studies have associated greenspace exposure with improved physical health, including improved cardiovascular health (Fong et al., 2018; Twohig-Bennett and Jones, 2018). Exposure to greenspace could also be beneficial for metabolic syndrome by providing opportunities for physical activity (Gong et al., 2014), fostering social cohesion and support (Hong et al., 2018), reducing feelings of stress (Gong et al., 2016), and mitigating exposure to air pollution (Dadvand et al., 2012) and noise (Markevych et al., 2017).
To our knowledge, no study to date has examined the longitudinal association between greenspace exposure and the risk of metabolic syndrome. Several studies investigated the association between greenspace exposure and individual components of metabolic syndrome. For instance, a recent systematic review found a significant association between greenspace and a decreased risk of diabetes in a meta-analysis of 6 longitudinal studies (Twohig-Bennett and Jones, 2018). In addition, several, mainly cross-sectional, studies investigated the association between greenspace and objectively-measured weight, although the findings were inconsistent (Michael et al., 2014; Sarkar, 2017; Villeneuve et al., 2018). However, longitudinal studies providing comparable evidence for the association with all individual components of the metabolic syndrome and studies on middle-aged and older adults are scarce.
The aim of the present study was to investigate the association between long-term exposure to greenspace and the risk of metabolic syndrome in middle-aged and older adults.
Material and Methods
Study population and setting
The Whitehall II study started in 1985 with 10 308 civil servants aged 35 to 55 years from 20 government departments in London, UK. The participants are invited for medical examinations and questionnaires every five years, irrespective of participation in previous follow-ups unless they had withdrawn from the study permanently. The present study period covered 15 years with data collection in 1997–1999, 2002–2004, 2007–2009, and 2012–2013. We included participants with data on metabolic syndrome and covariates for at least one follow-up and who lived in England, Scotland, or Wales (Figure S1); for a comparison between the included and excluded participants, see Table S1. In addition, we excluded participants with metabolic syndrome at their first measurement (n=302). Ethics approvals were received from the University College London Medical School Committee on the ethics of human research. Participants gave written informed consent for each follow-up.
Exposure assessment
We assessed outdoor greenspace surrounding the residential location of each participant at each follow-up (i.e. four repeated measures of greenspace for each participant). The residential location at each follow-up was geocoded based on the centroid of the participant’s postcode at that follow-up. The data on the postcodes’ centroids were obtained from the postcode directory of the corresponding year, provided by the Office for National Statistics (Office for National Statistics, 2017). A postcode held a median number of 14 (interquartile range (IQR): 20) households and 33 (IQR: 47) residents in 2011 (Office for National Statistics, 2013).
We applied two satellite-based indicators of outdoor greenspace. The Normalized Difference Vegetation Index (NDVI) is an indicator of greenspace based on land surface reflectance of visible (red) and near-infrared parts of spectrum. It ranges between −1 and 1 with higher values indicating more greenspace (i.e. photosynthetically active vegetation). The Vegetation Continuous Fields (VCF) is an estimate of the percentage of land (in each image pixel) covered by woody vegetation with a height of five meters or higher (Hansen et al., 2003). The NDVI and VCF maps were derived from satellite images obtained by the Moderate-resolution Imaging Spectroradiometer (MODIS) onboard the TERRA satellite and had a spatial resolution of 250 m by 250 m (Didan, 2015). All images were obtained from the Data Pool website of the NASA Land Processes Distributed Active Archive Center.
VCF images provided annual values. We downloaded the annual images of a relevant year to each follow-up (Table S2). In contrast, NDVI images were obtained over periods of 16 days. To take into account seasonal variability in greenspace, we downloaded images that were obtained between May and June (i.e. a period of maximum vegetation in our study region) and images obtained in December (i.e. a period of minimum vegetation) of the relevant years to each follow-up (Table S2). For NDVI, we used an average of the two estimates in the analyses.
Residential surrounding greenspace estimates were abstracted at each follow-up separately across linear circular buffers of 500 m and 1000 m around the corresponding postcode centroid, consistent with our previous studies (de Keijzer et al., 2019, 2018). Buffers smaller than 500 m were not possible due to the size of the postcode areas and the resolution of the NDVI and VCF maps. We selected the 500 m buffer to represent the immediate home surrounding environment, while the 1000 m buffer covered the general walking distance to places nearby the home (Stockton et al., 2016). We also abstracted NDVI and VCF estimates across the Lower layer Super Output Areas (LSOAs) corresponding to the residential postcode at each follow-up. LSOAs are administrative areas, created by grouping postcodes while considering proximity and social homogeneity, and contain around 1,500 residents and 650 households (Office for National Statistics, 2011; Stockton et al., 2016). To sum up, we abstracted estimates for two vegetation indices at four follow-ups for three surfaces (two buffers and LSOA) resulting in up to 24 exposure estimates per person.
Metabolic syndrome
We used the World Health Organization (WHO) definition of metabolic syndrome (Balkau and Charles, 1999; Eze et al., 2015), indicated by the presence of high fasting glucose (≥6.1 mmol/L) or treatment for diabetes and two or more of the following: (1) large waist circumference: ≥94 cm for men, ≥80 cm for women; (2) high serum triglyceride level: ≥1.7 mmol/L, or treatment for dyslipidaemia; (3) low HDL cholesterol: <0.9 mmol/L for men, <1.0 mmol/L for women, or treatment for dyslipidaemia; or (4) hypertension: systolic blood pressure (SBP) ≥140 or diastolic blood pressure (DBP) ≥90 mmHg, or use of antihypertensive medication.
For the measurement of triglycerides, HDL cholesterol, and fasting glucose, fasting blood samples were taken and analyzed within 72 hours in a serum stored at 4ºC using enzymatic calorimetric methods (Hamer et al., 2014). Blood pressure was measured in sitting position after five minutes of rest using the Hawksley random-zero sphygmomanometer in 1997–1999 and an OMRON HEM 907 digital sphygmomanometer in 2002–2004, 2007–2009, and 2012–2013 (Abell et al., 2018). At each follow-up, systolic and diastolic blood pressure were measured twice and the mean was used in the analysis. Waist circumference was measured in a standing position at the smallest circumference at or below the costal margin using a fibreglass tape measure at 600g tension (Singh-Manoux et al., 2014). Furthermore, participants reported their use of antihypertensive, lipid-lowering, and diabetes medication at each follow-up.
Covariates
Participants’ demographic characteristics (age, sex, and ethnicity) were recorded. Additionally, we collected two individual level (educational attainment and employment grade) and two neighbourhood level (employment and income domains of the Index of Multiple Deprivation (IMD)) indicators of socioeconomic status (SES). Data on lifestyle factors were collected at each follow-up and included the intake of fruit and vegetables, frequency of alcohol consumption, and smoking status. Lastly, rurality was assessed using the population density in the LSOA. Further information on the collection of these variables is given in the Supplement (S1).
Statistical analyses
Main analyses
We assessed the association between long-term exposure to greenspace and the risk of developing metabolic syndrome using Cox proportional hazards regression models with the follow-up time as the timescale. Entry time (time=0) was defined for each participant as the time at their first medical examination over the follow-up. Exit time was defined as the follow-up time at the first medical examination that identified metabolic syndrome or censoring (i.e. participant did not develop metabolic syndrome by the end of the follow-up, loss to follow-up, or death, whichever came first) (Dalton et al., 2016). The association with greenspace was reported per IQR increase in average NDVI or VCF based on all study participants. The analyses were adjusted for sex (male or female), ethnicity (white or non-white), age (continuous in years), rurality (rural or not rural), frequency of alcohol consumption (≥twice a day or less), smoking status (current, past, or never), intake of fruit and vegetables (≥twice a day or less), educational attainment (≤lower secondary school, higher secondary school, and ≥university), employment grade (administrative, professional and executive, and clerical), and country-specific tertiles of income and employment scores of the IMD. Except for sex, ethnicity, and education, all covariates were treated as time-varying variables. These confounders were selected a priori based on similar studies (Dalton et al., 2016; Eze et al., 2015; Virtanen et al., 2017; Wallwork et al., 2017). The model was not adjusted for factors that were suggested to be on the pathway between greenspace exposure and metabolic syndrome such as physical activity and air pollution (Dadvand et al., 2015; de Keijzer et al., 2018).
Further analyses
First, we investigated the association between greenspace and separate components of metabolic syndrome. Second, we explored the robustness of our findings to the way metabolic syndrome was defined by repeating the analyses defining metabolic syndrome according to the American Heart Association (AHA) and National Heart, Lung, and Blood Institute (NHLBI) criteria (Table S3) (Alberti et al., 2009; Bell et al., 2015; Virtanen et al., 2017). Third, we repeated the analyses using only the summer estimates of NDVI, representing the maximum greenness obtained from images from May-June. Fourth, to assess the impact of missing covariate data, we used multiple imputation for the missing covariate values. Multiple imputation was conducted by chained equations carrying out 25 imputations with 10 cycles for each imputation that generated 25 complete datasets (further information in Table S4).
Fifth, we restricted the analysis to participants who had not changed postcode over the study period (>62% of the study population) to evaluate the impact of moving. We hypothesized that the association may have been affected by moving if, for instance, participants with worse health moved to greener areas. Sixth, we repeated the main analyses (i) excluding rural areas (because greater exposure misclassification could occur in rural areas, which tend to have larger postcode areas), (ii) including only observations from England (to test the influence of country), and (iii) excluding non-white participants (to test the influence of ethnicity). We did not stratify the analyses based on rurality, country, or ethnicity, because only a small number of study participants lived in rural areas, lived in Wales or Scotland, or was non-white (Table 1). Furthermore, we further adjusted for marital status (married/cohabiting or not), which was assessed by questionnaire at each follow-up.
Table 1.
Descriptive characteristics of participants and new cases of metabolic syndrome per follow-up
| Variable | 1997–1999 | 2002–2004 | 2007–2009 | 2012–2013 |
|---|---|---|---|---|
| Participants; N | 5522 | 5206 | 4575 | 3789 |
| Age; M (Q1 – Q3) years | 54.7 (50.5–60.7) | 60.0 (56.0–66.0) | 64.6 (60.7–70.6) | 68.3 (64.6–74.0) |
| Sex; N(%) male | 4032 (73.0) | 3799 (73.0) | 3360 (73.4) | 2794 (73.7) |
| Ethnicity; N(%) white | 5153 (93.3) | 4852 (93.2) | 4299 (94.0) | 3601 (95.0) |
| Education; N(%) ≤Ordinary secondary school | 1946 (35.2) | 1805 (34.7) | 1538 (33.6) | 1251 (33.0) |
| Area income deprivation; M(Q1 – Q3) | 0.06 (0.03–0.11) | 0.06 (0.03–0.11) | 0.06 (0.03–0.10) | 0.06 (0.03–0.10) |
| Alcohol consumption; N(%) ≥2 day | 314 (5.7) | 298 (5.7) | 240 (5.3) | 202 (5.3) |
| Fruit and vegetable intake; N(%) ≥2 a day | 2183 (39.5) | 2169 (41.7) | 1898 (41.5) | 2284 (60.3) |
| Smoking status; N(%) current | 532 (9.6) | 378 (7.3) | 234 (5.1) | 111 (2.9) |
| Country; N(%) England | 5401 (97.8) | 5063 (97.3) | 4421 (96.6) | 3659 (96.6) |
| Rurality; N(%) rural | 424 (7.7) | 542 (10.4) | 521 (11.4) | 419 (11.1) |
| New cases of metabolic syndrome; N(%) | 0 (0) | 264 (5.1) | 219 (4.8) | 173 (4.6) |
Note: data are presented as median (M) and first quartile (Q1) - third quartile (Q3) or number of participants (N) and percentage (%).
Last, we explored indication of mediation of the association between greenspace and metabolic syndrome by two potential mediators for which we had data at each follow-up, i.e. physical activity and air pollution, following the criteria of Baron and Kenny (Baron and Kenny, 1986) (further information in the Supplement S2).
Stratified analyses
We explored variation in the association between greenspace and metabolic syndrome across strata of sex and SES by stratifying the main analyses by these variables. The associations were reported per IQR calculated separately for each exposure and each stratum.
Results
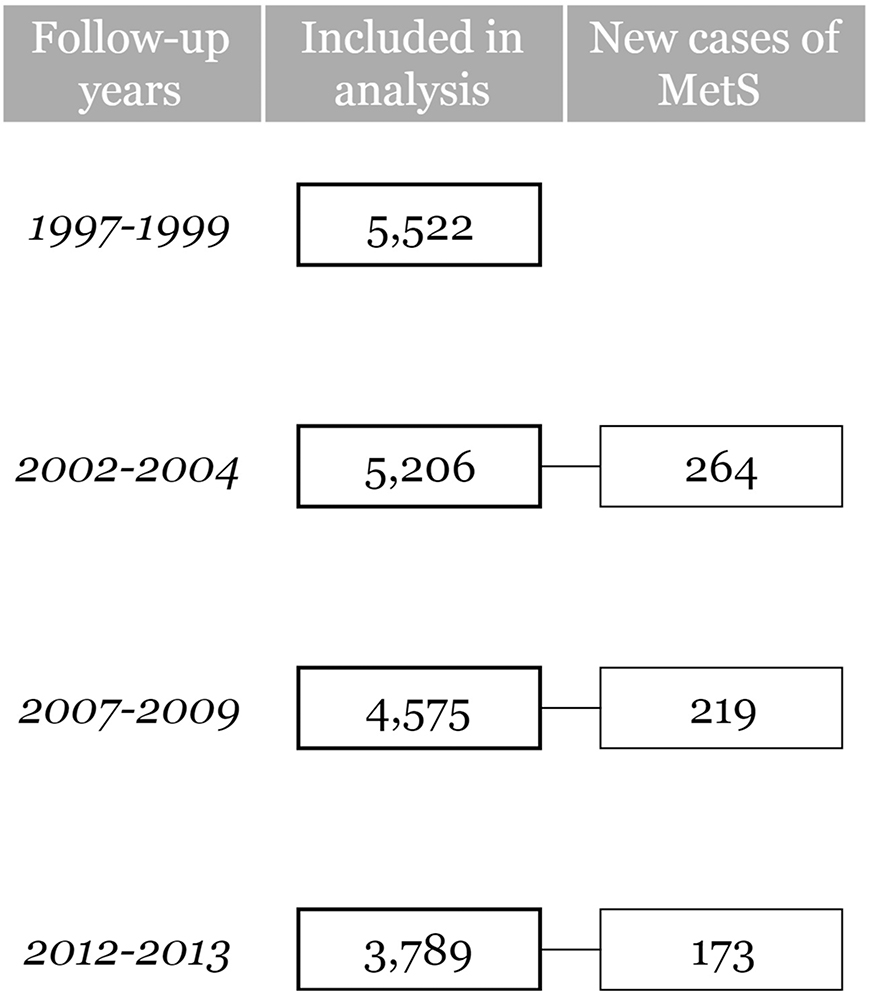
Our analyses included 6076 participants without metabolic syndrome at their first measurement and with complete observations for metabolic syndrome and covariates in at least one follow-up. Median follow-up time was 14.1 years (IQR: 6.3–14.6). The socio-demographic characteristics of the study participants are presented in Table 1. In total, 656 new cases of metabolic syndrome occurred over the study period (Figure 1). The median residential surrounding greenspace was slightly higher at the last follow-ups compared to the first follow-up (Table S5) and the estimates of NDVI and VCF were positively correlated (Table S6).
Figure 1.
Flow chart study population
Note: MetS = metabolic syndrome
Main analyses
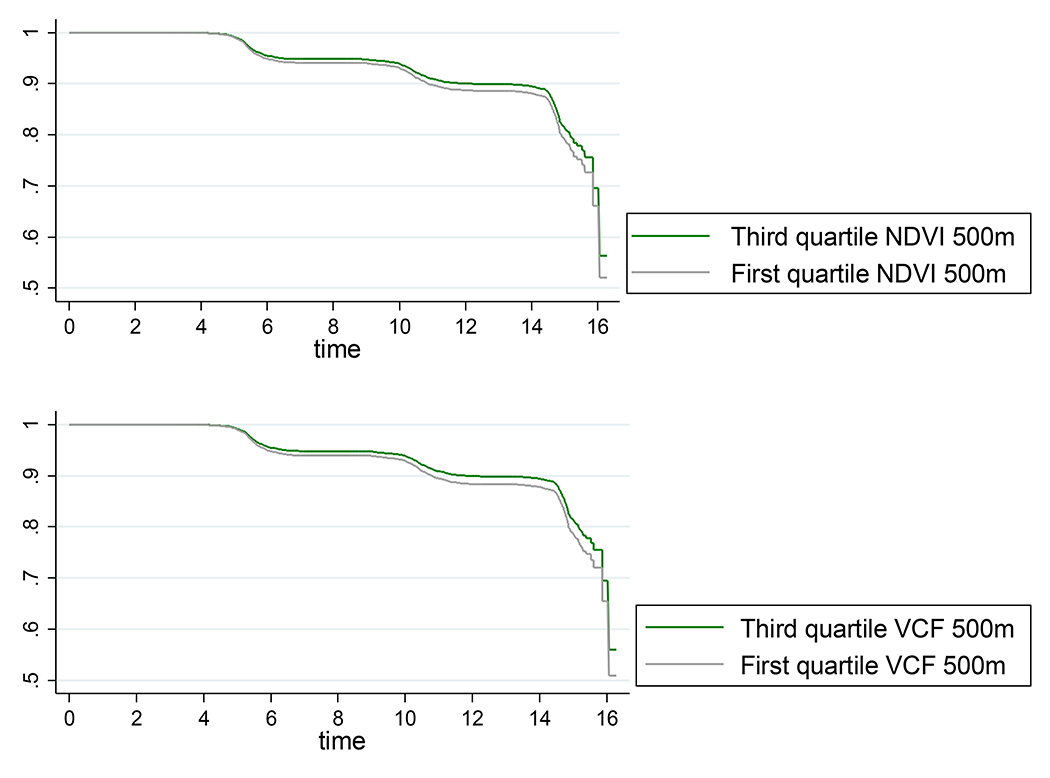
Higher residential surrounding greenspace was associated with lower risk of developing metabolic syndrome (Table 2). One-IQR increase in NDVI in the 500 m buffer was associated with a lower risk of metabolic syndrome of 13% (95% confidence interval (CI): 1%, 23%) (Table 2, Model 3; Figure 2). We also observed a lower risk of metabolic syndrome associated with NDVI in the 1000 m buffer and in the LSOA; however, these associations did not attain statistical significance (Table 2, Model 3). Higher VCF was also associated with lower risk of metabolic syndrome (Table 2). One-IQR increase in VCF in the 500 m buffer was associated with a 14% (95% CI: 5%, 22%) lower risk of metabolic syndrome (Table 2, Model 3; Figure 2). The minimally adjusted models (Model 1) and the models further adjusted for lifestyle factors (Model 2) showed similar associations as the fully adjusted models (Model 3) (Table 2).
Table 2.
Hazard ratios (95% confidence interval) of metabolic syndrome associated with an interquartile-range increase in residential surrounding greenspace (NDVI or VCF).
| 500 m buffer |
1000 m buffer |
LSOA |
|||||
|---|---|---|---|---|---|---|---|
| Vegetation index | Model | IQR | Hazard ratio | IQR | Hazard ratio | IQR | Hazard ratio |
| NDVI | 1 | 0.16 | 0.88 (0.79, 0.97)* | 0.15 | 0.90 (0.81, 0.99)* | 0.18 | 0.89 (0.80, 0.99)* |
| 2 | 0.88 (0.80, 0.98)* | 0.90 (0.81, 1.00) | 0.90 (0.81, 1.01) | ||||
| 3 | 0.87 (0.77, 0.99)* | 0.90 (0.79, 1.01) | 0.91 (0.79, 1.03) | ||||
| VCF | 1 | 9.4 | 0.84 (0.77, 0.93)* | 8.7 | 0.83 (0.76, 0.92)* | 10.1 | 0.81 (0.73, 0.90)* |
| 2 | 0.85 (0.77, 0.93)* | 0.84 (0.76, 0.93)* | 0.82 (0.74, 0.91)* | ||||
| 3 | 0.86 (0.78, 0.95)* | 0.85 (0.77, 0.94)* | 0.83 (0.75, 0.92)* | ||||
Note: All results from Cox Proportional Hazard models. Model (1): minimally adjusted model, adjusted for age, sex, and ethnicity; Model (2): Model (1) + alcohol consumption, fruit and vegetable consumption, and smoking; Model (3): fully adjusted model, Model (2) + individual socioeconomic status (education and employment grade), and neighbourhood socioeconomic status (income and employment deprivation). IQR, interquartile range; NDVI, Normalized Difference Vegetation Index; VCF, Vegetation Continuous Fields.
Figure 2.
Survival functions of metabolic syndrome by level of greenspace (the first quartile of NDVI or VCF in the 500 m buffer compared to the third quartile)
Further analyses
Higher residential surrounding greenspace was associated with lower risk of all components of metabolic syndrome (Table S7). Furthermore, the associations between greenspace and metabolic syndrome were similar using the AHA/NHLBI definition of metabolic syndrome (Table S8). However, no significant association between NDVI and the risk of metabolic syndrome was found when using only the summer estimates of NDVI (Table S9).
The associations did not change notably when multiple imputation was used for missing covariate data, when excluding participants who changed postcode over the study period, participants living in rural areas, or non-white participants, when including only observations from England, or when adjusting for marital status (Table S10).
Last, we found suggestions of mediation of the association between greenspace and metabolic syndrome by physical activity and air pollution (Table S11). Increases in NDVI were significantly associated with higher physical activity and lower air pollution and the association between NDVI and metabolic syndrome attenuated when adjusting for physical activity or air pollution (Table S11). For VCF, a significant association was only found with air pollution, and the association between VCF and metabolic syndrome attenuated when adjusting for air pollution (Table S11).
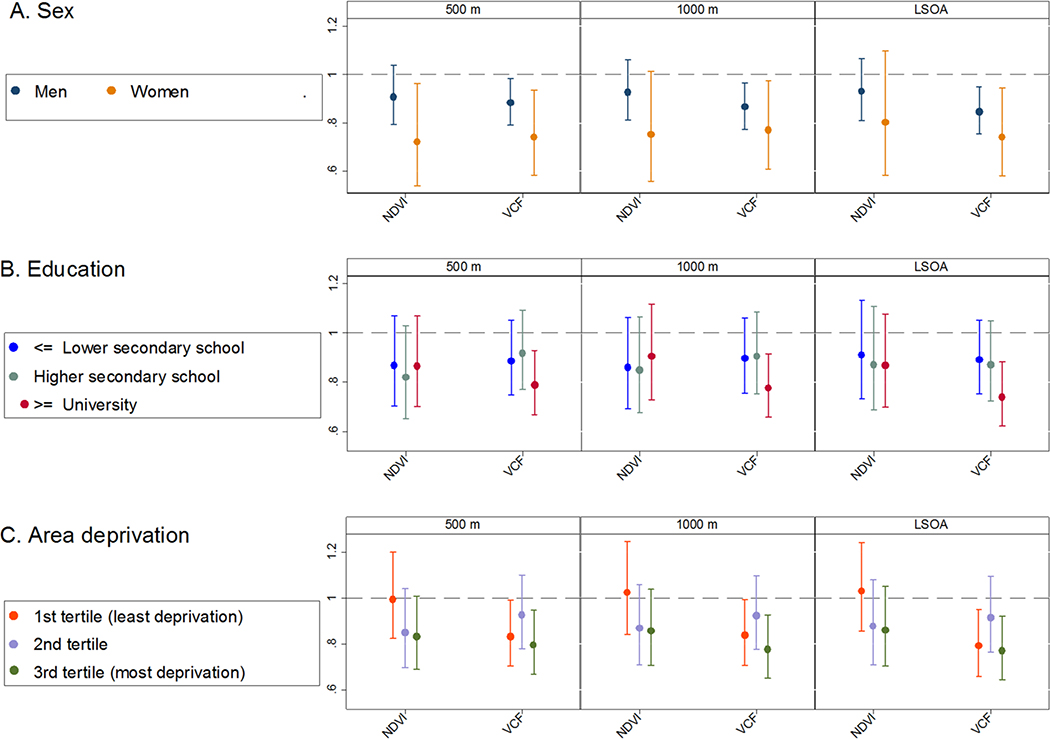
Stratified analyses
When stratified by sex, the associations between greenspace and metabolic syndrome were slightly stronger among women than among men, although the confidence intervals largely overlapped (Figure 3). No trend was observed when the analyses were stratified by education; higher NDVI or VCF was associated with lower odds of metabolic syndrome across all strata (Figure 3). However, for NDVI, there were indications for a slightly stronger association among those in the middle educational group compared to the lower and the highest educational group, while for VCF, there were suggestions for a stronger association for those participants with the highest educational levels compared to the lower and middle educational level (Figure 3). Furthermore, we did not observe a clear trend when the analyses were stratified by tertiles of the IMD income domain (Figure 3). However, the strongest association between greenspace and risk of metabolic syndrome was observed in participants living in areas with highest area deprivation (Figure 3).
Figure 3.
Hazard ratios (95% confidence interval) of metabolic syndrome associated with an interquartile-range increase in residential surrounding greenspace (NDVI or VCF in the 500 m buffer, 1000 m buffer, or LSOA) in stratified analyses (A. sex, B. education, and C. area income deprivation)
Note: All results from Cox Proportional Hazard models adjusted for age, sex, ethnicity, rurality, alcohol consumption, fruit and vegetable consumption, smoking, individual socioeconomic status (education and employment grade), and neighbourhood socioeconomic status (income and employment deprivation); NDVI, Normalized Difference Vegetation Index; VCF, Vegetation Continuous Fields.
Discussion
To our knowledge, this is the first longitudinal study to investigate the association of long-term residential surrounding greenspace with the risk of metabolic syndrome. Our study relied on four repeated measurements of metabolic syndrome over 15 years in a large, well-established cohort, together with the characterization of residential surrounding greenspace at each follow-up. We observed that higher residential surrounding greenspace was associated with a lower risk of metabolic syndrome. The observed associations were controlled for a wide range of potential confounders and were robust to various sensitivity analyses. Physical activity and air pollution may have mediated the associations. Furthermore, we observed suggestions for a stronger association between greenspace and metabolic syndrome in women as compared to men.
The association between greenspace and metabolic syndrome was stronger when using VCF estimates, indicating tree cover, than when using NDVI estimates; the association between NDVI and metabolic syndrome was significant when using averaged winter and summer estimates of NDVI in the 500 m buffer, but not when using NDVI estimates obtained in the 1000 m buffer or LSOA or when using only the summer estimates. These findings suggest that the distance to and type of greenspace may affect the association with cardio-metabolic health. In addition, the difference between VCF and NDVI estimates could also suggest a difference in built environment, which may also influence the association with health.
Comparison with other studies
Although we did not find previous studies on the association between long-term greenspace exposure and risk of metabolic syndrome, our results can be compared to two cross-sectional studies which examined alternative indicators of cardio-metabolic risk, namely the count of six cardiometabolic risk factors (hypertension, high waist circumference, low HDL cholesterol, raised triglycerides level, and raised fasting plasma glucose level) (Paquet et al., 2013) and a metabolic cluster score (calculated as the sum of the z-scores of the measurements of body fat percentage, fasting glucose, HDL cholesterol level, triglycerides level, and systolic blood pressure) (Dengel et al., 2009). Apart from different outcomes and study design, our study and the two cross-sectional studies also differed in the indicator of greenspace exposure and study population. Our study is on middle-aged and older adults from the UK aged 45 years and over, while the other studies included Australian adults aged 18 years and older (Paquet et al., 2013) or American adolescents aged 10 to 16 years old (Dengel et al., 2009). However, all three studies showed a protective association between long-term greenspace exposure and their indicator of cardio-metabolic risk. Similar to our study, the Australian study found an association between higher greenness of public open spaces (as assessed by NDVI) within 1000-m from participants’ residential locations and a lower number of cardio-metabolic risk factors in 3754 adults (Paquet et al., 2013). The American study observed that more land use dedicated to parks within the residential neighbourhood was associated with a lower metabolic cluster score in 188 adolescents, although the association did not reach statistical significance (p=0.07) (Dengel et al., 2009).
In addition, several studies investigated the association between greenspace and individual components of the metabolic syndrome, but studies on middle-to-older adults are scarce. The findings of our current study suggest that increases in NDVI and VCF were associated with a decreased risk of fasting glucose or diabetes, large waist circumference, high triglyceride level, low HDL cholesterol, and hypertension among adults aged 45 to 69 years old at baseline. These findings are in line with previous studies that observed that increases in NDVI were associated with a lower risk of developing diabetes in a longitudinal study among 380,738 Canadians aged 45 to 84 years old (Clark et al., 2017) and with lower odds of diabetes, hypertension, and hyperlipidemia in a cross-sectional study of 249,405 US Medicare beneficiaries (Brown et al., 2016). Such protective associations between long-term greenspace exposure and individual components of metabolic syndrome have also been observed in studies using alternative methods for exposure assessment. An increase in the proportion of land in the neighbourhood covered by greenspace was associated with a lower incidence of diabetes in a longitudinal study of 23,865 individuals aged 40 to 79 years from the UK (Dalton et al., 2016) and with reduced likelihood of overweight, obesity, and diabetes in two cross-sectional studies of over 245,000 Australian adults aged 45 years and older (Astell-Burt et al., 2014a, 2014b). Furthermore, an increase in self-reported park use was associated with lower odds of BMI-defined obesity and high fasting glucose level, but not with high total cholesterol levels or hypertension, in a longitudinal study of adults aged 45 to 72 years from Lithuania (Tamosiunas et al., 2014).
As there is no consensus on the definition of metabolic syndrome yet, we used the two most frequently used definitions to explore the robustness of our findings against the definition of metabolic syndrome. The results were generally consistent, although the strongest associations were found with the WHO definition of metabolic syndrome. This finding is in agreement with the findings of a cross-sectional study from Switzerland that investigated the association between air pollution and these two definitions of the metabolic syndrome, and also found the strongest association with the WHO-definition (Eze et al., 2015).
In our study, there was some indication of a stronger association between greenspace and metabolic syndrome among women compared to men. This finding is in agreement with a cross-sectional Australian study that found an association between residential surrounding greenspace and overweight and obesity among women, but not among men (Astell-Burt et al., 2014a). Other earlier studies also suggested that the association between greenspace exposure and health may be modified by sex and have provided various explanations. For instance, women may spend more time in the residential neighbourhood than men, and thus be more exposed to neighbourhood greenspace (de Keijzer et al., 2019). Another explanation may be that the use of greenspace may differ between men and women, as men may engage in more vigorous physical activity in parks than women (Cohen et al., 2007).
Furthermore, the association between greenspace and health has been suggested to vary by SES (Gascon et al., 2015; Maas et al., 2009), although not all studies observed this effect modification. A potential explanation of these inconsistent results is that the modifying effect of SES differs by study region, health outcome, and greenspace indicator, and in each situation, different underlying mechanisms may be at play, which may be affected differently by SES. In our study, stratified analysis did not show a clear trend across strata of SES. Our findings are in line with a previous longitudinal study from the UK of a cohort of 23,865 adults aged 40 to 79 years, which found SES not to modify the association between the amount of greenspace in the neighbourhood (assessed using a land cover map) and incident diabetes (Dalton et al., 2016).
Potential underlying mechanisms
Several mechanisms have been proposed for the association between greenspace exposures and health that could also apply to such an association with metabolic syndrome (Markevych et al., 2017). First, some studies found higher levels of physical activity in neighbourhoods with more greenspace (Gong et al., 2014), and physical activity is known to reduce the risk of metabolic syndrome (He et al., 2014). Our findings suggested mediation by physical activity of the association between NDVI and metabolic syndrome. However, the assessment of physical activity was based on self-reported levels of overall physical activity and data on where physical activity was undertaken were not available (i.e. physical activity in or near greenspace or not). Second, exposure to greenspace could reduce the risk of metabolic syndrome by reducing exposure to air pollution (Dadvand et al., 2012; Eze et al., 2015). Our findings support mediation by air pollution of the association of NDVI and VCF with metabolic syndrome, although our exposure assessment of air pollution was limited to modelled PM10 with a coarse spatial resolution. In addition to air pollution, other urban stressors such as noise may also be important mechanisms underlying the association between long-term greenspace exposure and health, but we did not have data on these stressors in our study. Furthermore, exposure to greenspace could reduce stress (Gong et al., 2016), which, in turn, could decrease the risk of metabolic syndrome (Bergmann et al., 2014). Moreover, exposure to greenspace has been reported to foster social support and cohesion (Hong et al., 2018), while better social support has been associated with a lower risk of metabolic syndrome (Yang et al., 2013). Further longitudinal research is needed to investigate mediation by these and other factors.
Limitations
Our study had some limitations. First, women and ethnic minorities are underrepresented in the Whitehall II study which might influence the generalisability of our findings. In addition, participants excluded from the analyses were different from those included in the analyses. Selection bias is, however, an unlikely explanation for the present findings as exclusions were mainly due to missing covariates and analyses using multiple imputation for these missing values showed similar results.
Second, our exposure assessment was limited to the assessment of greenspace using satellite-based vegetation indices. This enabled us to take into account small greenspace in a standardized way, but could not provide any information on the type, quality, or use of the greenspace. Moreover, our exposure assessment was limited to residential exposure, while participants might have spent time at other locations such as the workplace. However, many study participants retired during the study period and, in general, older adults tend to be more bound to their direct neighborhood environment (Yen et al., 2009).
Finally, the use of postcode centroids might have led to exposure misclassification, particularly in large postcode areas. However, large postcode areas are more common in rural areas, and our findings did not change notably when excluding these areas.
Conclusions
In a longitudinal study of an ageing population, we observed that greater long-term exposure to residential surrounding greenspace was associated with a lower risk of developing metabolic syndrome over the 15-year course of the study. Prevention of metabolic syndrome could subsequently reduce the burden of NCDs, which is one of the main public health priorities of the 21st century (Galassi et al., 2006; Prince et al., 2015; World Health Organization, 2014). If confirmed by future studies, our findings suggest that greenspace could play a role in the improvement of the neighbourhood environment and the reduction of burden of metabolic syndrome and hence NCDs. Future studies are needed to replicate our findings in other settings and climates and to investigate the underlying mechanisms of the association. In addition, our finding that the association with health was stronger with tree cover than overall vegetation cover (i.e. NDVI) provides ground for further research to identify characteristics of greenspace that could most strongly reduce the risk of the metabolic syndrome.
Supplementary Material
Highlights.
We investigated the longitudinal association between greenspace and risk of metabolic syndrome.
More residential surrounding greenspace was associated with lower risk of metabolic syndrome.
Our findings suggest that greenspace may protect cardio-metabolic health.
Acknowledgements
We thank the participants in the Whitehall II Study, as well as all Whitehall II research scientists, study and data managers and clinical and administrative staff who make the study possible. We are especially grateful to Aida Sanchez for managing and providing data.
The MODIS vegetation products were retrieved from the online Data Pool, courtesy of the NASA EOSDIS Land Processes Distributed Active Archive Center (LP DAAC), USGS/Earth Resources Observation and Science (EROS) Center, Sioux Falls, South Dakota, https://lpdaac.usgs.gov/.
Funding sources
The collection of data in the Whitehall II Study was supported by the UK Medical Research Council [MRC K013351, R024227/1], British Heart Foundation [RG/13/2/30098], and the US National Institute on Aging [NIA, R01AG056477, R01AG034454]. PD [RYC-2012-10995] and CT [RYC-2015-17402] are funded by Ramón y Cajal fellowships awarded by the Spanish Ministry of Economy and Competitiveness. MK is supported by the UK MRC, Helsinki Institute of Life Sciences and the Academy of Finland [311492]. The funders have not been involved in any part of the study design or reporting.
Footnotes
Declarations of interest: None.
References
- Abell JG, Kivimäki M, Dugravot A, Tabak AG, Fayosse A, Shipley M, Sabia S, Singh-Manoux A, 2018. Association between systolic blood pressure and dementia in the Whitehall II cohort study: role of age, duration, and threshold used to define hypertension. Eur. Heart J. ehy288–ehy288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alberti KGMM, Eckel RH, Grundy SM, Zimmet PZ, Cleeman JI, Donato KA, Fruchart J-C, James WPT, Loria CM, Smith SCJ, 2009. Harmonizing the metabolic syndrome: a joint interim statement of the International Diabetes Federation Task Force on Epidemiology and Prevention; National Heart, Lung, and Blood Institute; American Heart Association; World Heart Federation; International. Circulation 120, 1640–1645. doi: 10.1161/CIRCULATIONAHA.109.192644 [DOI] [PubMed] [Google Scholar]
- Astell-Burt T, Feng X, Kolt GS, 2014a. Greener neighborhoods, slimmer people? Evidence from 246,920 Australians. Int. J. Obes. 38, 156–159. doi: 10.1038/ijo.2013.64 [DOI] [PubMed] [Google Scholar]
- Astell-Burt T, Feng X, Kolt GS, 2014b. Is neighborhood green space associated with a lower risk of type 2 diabetes? Evidence from 267,072 Australians. Diabetes Care 37, 197–201. doi: 10.2337/dc13-1325 [DOI] [PubMed] [Google Scholar]
- Balkau B, Charles M, 1999. Comment on the provisional report from the WHO consultation. European Group for the Study of Insulin Resistance (EGIR). Diabet. Med. 16, 442–443. doi: 10.1046/j.1464-5491.1999.00059.x [DOI] [PubMed] [Google Scholar]
- Baron RM, Kenny DA, 1986. The moderator-mediator variable distinction in social psychological research: conceptual, strategic, and statistical considerations. J. Pers. Soc. Psychol. 51, 1173–1182. doi: 10.1037/0022-3514.51.6.1173 [DOI] [PubMed] [Google Scholar]
- Bell JA, Hamer M, Batty GD, Singh-Manoux A, Sabia S, Kivimäki M, 2015. Incidence of Metabolic Risk Factors Among Healthy Obese Adults: 20-Year Follow-Up. J. Am. Coll. Cardiol. 66, 871–873. doi: 10.1016/j.jacc.2015.06.014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bergmann N, Gyntelberg F, Faber J, 2014. The appraisal of chronic stress and the development of the metabolic syndrome: a systematic review of prospective cohort studies. Endocr. Connect. 3, R55–R80. doi: 10.1530/EC-14-0031 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown SC, Lombard J, Wang K, Byrne MM, Toro M, Plater-Zyberk E, Feaster DJ, Kardys J, Nardi MI, Perez-Gomez G, Pantin HM, Szapocznik J, 2016. Neighborhood Greenness and Chronic Health Conditions in Medicare Beneficiaries. Am. J. Prev. Med. 51, 78–89. doi: 10.1016/j.amepre.2016.02.008 [DOI] [PubMed] [Google Scholar]
- Clark C, Sbihi H, Tamburic L, Brauer M, Frank LD, Davies HW, 2017. Association of Long-Term Exposure to Transportation Noise and Traffic-Related Air Pollution with the Incidence of Diabetes: A Prospective Cohort Study. Environ. Health Perspect. 125, 87025. doi: 10.1289/EHP1279 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen DA, McKenzie TL, Sehgal A, Williamson S, Golinelli D, Lurie N, 2007. Contribution of public parks to physical activity. Am J Public Heal. 97. doi: 10.2105/AJPH.2005.072447 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dadvand P, de Nazelle A, Triguero-Mas M, Schembari A, Cirach M, Amoly E, Figueras F, Basagana X, Ostro B, Nieuwenhuijsen M, 2012. Surrounding greenness and exposure to air pollution during pregnancy: an analysis of personal monitoring data. Environ. Health Perspect. 120, 1286–1290. doi: 10.1289/ehp.1104609 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dadvand P, Nieuwenhuijsen MJ, Esnaola M, Forns J, Basagaña X, Alvarez-Pedrerol M, Rivas I, López-Vicente M, De Castro Pascual M, Su J, Jerrett M, Querol X, Sunyer J, 2015. Green spaces and cognitive development in primary schoolchildren. P Natl Acad Sci 112, 7937–7942. doi: 10.1073/pnas.1503402112 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dalton AM, Jones AP, Sharp SJ, Cooper AJM, Griffin S, Wareham NJ, 2016. Residential neighbourhood greenspace is associated with reduced risk of incident diabetes in older people: a prospective cohort study. BMC Public Health 16, 1171. doi: 10.1186/s12889-016-3833-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- de Keijzer C, Tonne C, Basagaña X, Valentín A, Singh-Manoux A, Alonso J, Antó JM, Nieuwenhuijsen MJ, Sunyer J, Dadvand P, 2018. Residential surrounding greenness and cognitive decline: A 10-year follow-up of the whitehall II cohort. Environ. Health Perspect. 126. doi: 10.1289/EHP2875 [DOI] [PMC free article] [PubMed] [Google Scholar]
- de Keijzer C, Tonne C, Sabia S, Basagaña X, Valentín A, Singh-Manoux A, Antó JM, Alonso J, Nieuwenhuijsen MJ, Sunyer J, Dadvand P, 2019. Green and blue spaces and physical functioning in older adults: Longitudinal analyses of the Whitehall II study. Environ. Int 122, 346–356. doi: 10.1016/j.envint.2018.11.046 [DOI] [PMC free article] [PubMed] [Google Scholar]
- den Braver NR, Lakerveld J, Rutters F, Schoonmade LJ, Brug J, Beulens JWJ, 2018. Built environmental characteristics and diabetes: a systematic review and meta-analysis. BMC Med. 16, 12. doi: 10.1186/s12916-017-0997-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dengel DR, Hearst MO, Harmon JH, Forsyth A, Lytle LA, 2009. Does the built environment relate to the metabolic syndrome in adolescents? Health Place 15, 946–951. doi: 10.1016/j.healthplace.2009.03.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Didan K, 2015. MOD13Q1 MODIS/Terra Vegetation Indices 16-Day L3 Global 250m SIN Grid V006 [Data set] [WWW Document]. doi: 10.5067/MODIS/MOD13Q1.006 [DOI] [Google Scholar]
- Eze IC, Schaffner E, Foraster M, Imboden M, von Eckardstein A, Gerbase MW, Rothe T, Rochat T, Kunzli N, Schindler C, Probst-Hensch N, 2015. Long-Term Exposure to Ambient Air Pollution and Metabolic Syndrome in Adults. PLoS One 10, e0130337. doi: 10.1371/journal.pone.0130337 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fong KC, Hart JE, James P, 2018. A Review of Epidemiologic Studies on Greenness and Health: Updated Literature Through 2017. Curr. Environ. Heal. Reports 5, 77–87. doi: 10.1007/s40572-018-0179-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- Galassi A, Reynolds K, He J, 2006. Metabolic syndrome and risk of cardiovascular disease: a meta-analysis. Am. J. Med. 119, 812–819. doi: 10.1016/j.amjmed.2006.02.031 [DOI] [PubMed] [Google Scholar]
- Gascon M, Triguero-Mas M, Martínez D, Dadvand P, Forns J, Plasència A, Nieuwenhuijsen MJ, 2015. Mental Health Benefits of Long-Term Exposure to Residential Green and Blue Spaces: A Systematic Review. Int. J. Environ. Res. Public Health 12, 4354–4379. doi: 10.3390/ijerph120404354 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gong Y, Gallacher J, Palmer S, Fone D, 2014. Neighbourhood green space, physical function and participation in physical activities among elderly men: the Caerphilly Prospective study. Int. J. Behav. Nutr. Phys. Act. 11, 1–11. doi: 10.1186/1479-5868-11-40 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gong Y, Palmer S, Gallacher J, Marsden T, Fone D, 2016. A systematic review of the relationship between objective measurements of the urban environment and psychological distress. Environ. Int. 96, 48–57. doi: 10.1016/j.envint.2016.08.019 [DOI] [PubMed] [Google Scholar]
- Hamer M, Stamatakis E, Steptoe A, 2014. Effects of substituting sedentary time with physical activity on metabolic risk. Med. Sci. Sports Exerc. 46, 1946–1950. doi: 10.1249/MSS.0000000000000317 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hansen MC, DeFries RS, Townshend JRG, Carroll M, Dimiceli C, Sohlberg RA, 2003. Global Percent Tree Cover at a Spatial Resolution of 500 Meters: First Results of the MODIS Vegetation Continuous Fields Algorithm. Earth Interact 7, 1–15. doi: [DOI] [Google Scholar]
- He D, Xi B, Xue J, Huai P, Zhang M, Li J, 2014. Association between leisure time physical activity and metabolic syndrome: a meta-analysis of prospective cohort studies. Endocrine 46, 231–240. doi: 10.1007/s12020-013-0110-0 [DOI] [PubMed] [Google Scholar]
- Hong A, Sallis JF, King AC, Conway TL, Saelens B, Cain KL, Fox EH, Frank LD, 2018. Linking green space to neighborhood social capital in older adults: The role of perceived safety. Soc. Sci. Med. 207, 38–45. doi: 10.1016/j.socscimed.2018.04.051 [DOI] [PubMed] [Google Scholar]
- Kotzeva M, Brandmüller T, Lupa I, Önnerfors A, Corselli-Nordblad L, Coyette C, Johansson A, Strandell H, Pascal W, 2016. Urban Europe - Statistics on cities, towns and suburbs [WWW Document]. doi: 10.2785/91120 [DOI] [Google Scholar]
- Leal C, Chaix B, 2011. The influence of geographic life environments on cardiometabolic risk factors: a systematic review, a methodological assessment and a research agenda. Obes. Rev. 12, 217–230. doi: 10.1111/j.1467-789X.2010.00726.x [DOI] [PubMed] [Google Scholar]
- Maas J, Verheij RA, de Vries S, Spreeuwenberg P, Schellevis FG, Groenewegen PP, 2009. Morbidity is related to a green living environment. J Epidemiol Commun H 63, 967–973. doi: 10.1136/jech.2008.079038 [DOI] [PubMed] [Google Scholar]
- Markevych I, Schoierer J, Hartig T, Chudnovsky A, Hystad P, Dzhambov AM, de Vries S, Triguero-Mas M, Brauer M, Nieuwenhuijsen MJ, Lupp G, Richardson EA, Astell-Burt T, Dimitrova D, Feng X, Sadeh M, Standl M, Heinrich J, Fuertes E, 2017. Exploring pathways linking greenspace to health: Theoretical and methodological guidance. Environ. Res. 158, 301–317. doi: 10.1016/j.envres.2017.06.028 [DOI] [PubMed] [Google Scholar]
- Matthiessen C, Lucht S, Hennig F, Ohlwein S, Jakobs H, Jockel K-H, Moebus S, Hoffmann B, 2018. Long-term exposure to airborne particulate matter and NO2 and prevalent and incident metabolic syndrome - Results from the Heinz Nixdorf Recall Study. Environ. Int. 116, 74–82. doi: 10.1016/j.envint.2018.02.035 [DOI] [PubMed] [Google Scholar]
- Michael YL, Nagel CL, Gold R, Hillier TA, 2014. Does change in the neighborhood environment prevent obesity in older women? Soc. Sci. Med. 102, 129–137. doi: 10.1016/j.socscimed.2013.11.047 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nieuwenhuijsen MJ, 2018. Influence of urban and transport planning and the city environment on cardiovascular disease. Nat. Rev. Cardiol. 15, 432–438. doi: 10.1038/s41569-018-0003-2 [DOI] [PubMed] [Google Scholar]
- Office for National Statistics, 2017. Geography [WWW Document]. URL https://www.ons.gov.uk/methodology/geography (accessed 12.16.16).
- Office for National Statistics, 2013. 2011 Census: Headcounts and household estimates for postcodes in England and Wales [WWW Document]. URL https://www.ons.gov.uk/peoplepopulationandcommunity/populationandmigration/populationestimates/datasets/2011censusheadcountsandhouseholdestimatesforpostcodesinenglandandwales (accessed 6.7.17).
- Office for National Statistics, 2011. 2011 Census: Population and Household Estimates for Small Areas in England and Wales, March 2011 [WWW Document]. URL https://www.ons.gov.uk/peoplepopulationandcommunity/populationandmigration/populationestimates/bulletins/2011censuspopulationandhouseholdestimatesforsmallareasinenglandandwales/2012-11-23
- Paquet C, Orschulok TP, Coffee NT, Howard NJ, Hugo G, Taylor AW, Adams RJ, Daniel M, 2013. Are accessibility and characteristics of public open spaces associated with a better cardiometabolic health? Landsc. Urban Plan. 118, 70–78. doi: 10.1016/j.landurbplan.2012.11.011 [DOI] [Google Scholar]
- Prince MJ, Wu F, Guo Y, Gutierrez Robledo LM, O’Donnell M, Sullivan R, Yusuf S, 2015. The burden of disease in older people and implications for health policy and practice. Lancet 385, 549–562. doi: 10.1016/S0140-6736(14)61347-7 [DOI] [PubMed] [Google Scholar]
- Sarkar C, 2017. Residential greenness and adiposity: Findings from the UK Biobank. Environ. Int. 106, 1–10. doi: 10.1016/j.envint.2017.05.016 [DOI] [PubMed] [Google Scholar]
- Singh-Manoux A, Sabia S, Bouillon K, Brunner EJ, Grodstein F, Elbaz A, Kivimaki M, 2014. Association of body mass index and waist circumference with successful ageing: 16 year follow-up of the Whitehall II study. Obesity (Silver Spring). 22, 1172–1178. doi: 10.1002/oby.20651 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stockton JC, Duke-Williams O, Stamatakis E, Mindell JS, Brunner EJ, Shelton NJ, 2016. Development of a novel walkability index for London, United Kingdom: cross-sectional application to the Whitehall II Study. BMC Public Health 16, 416. doi: 10.1186/s12889-016-3012-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tamosiunas A, Grazuleviciene R, Luksiene D, Dedele A, Reklaitiene R, Baceviciene M, Vencloviene J, Bernotiene G, Radisauskas R, Malinauskiene V, Milinaviciene E, Bobak M, Peasey A, Nieuwenhuijsen MJ, 2014. Accessibility and use of urban green spaces, and cardiovascular health: findings from a Kaunas cohort study. Environ. Heal. 13, 20. doi: 10.1186/1476-069X-13-20 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Twohig-Bennett C, Jones A, 2018. The health benefits of the great outdoors: A systematic review and meta-analysis of greenspace exposure and health outcomes. Environ. Res. doi: 10.1016/j.envres.2018.06.030 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Villeneuve PJ, Jerrett M, Su JG, Weichenthal S, Sandler DP, 2018. Association of residential greenness with obesity and physical activity in a US cohort of women. Environ. Res. 160, 372–384. doi: 10.1016/j.envres.2017.10.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Virtanen M, Ferrie JE, Akbaraly T, Tabak A, Jokela M, Ebmeier KP, Singh-Manoux A, Kivimaki M, 2017. Metabolic Syndrome and Symptom Resolution in Depression: A 5-Year Follow-Up of Older Adults. J. Clin. Psychiatry 78, e1–e7. doi: 10.4088/JCP.15m10399 [DOI] [PubMed] [Google Scholar]
- Wallwork RS, Colicino E, Zhong J, Kloog I, Coull BA, Vokonas P, Schwartz JD, Baccarelli AA, 2017. Ambient Fine Particulate Matter, Outdoor Temperature, and Risk of Metabolic Syndrome. Am. J. Epidemiol. 185, 30–39. doi: 10.1093/aje/kww157 [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization, 2014. Global status report on noncommunicable disease 2014 [WWW Document]. URL http://apps.who.int/iris/bitstream/handle/10665/148114/9789241564854_eng.pdf;jsessionid=F27A013F7BCFD327BB6DFCA1754B9718?sequence=1 (accessed 7.12.18). [Google Scholar]
- Yang C, Li T, Ji Y, 2013. Impact of social integration on metabolic functions: evidence from a nationally representative longitudinal study of US older adults. BMC Public Health 13, 1210. doi: 10.1186/1471-2458-13-1210 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yen IH, Michael YL, Perdue L, 2009. Neighborhood Environment in Studies of Health of Older Adults: A Systematic Review. Am. J. Prev. Med. 37, 455–463. doi: 10.1016/j.amepre.2009.06.022 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.