Abstract
Emotion Regulation Therapy (ERT) has demonstrated efficacy in both open and randomized trials for generalized anxiety disorder (GAD) with and without co-occurring depression. An important goal in ERT is to teach clients adaptive emotion regulation, including healthier metacognitive abilities such as decentering and cognitive reappraisal. A few studies thus far have demonstrated a mediating role for these metacognitive abilities in other cognitive behavioral therapies (CBTs) for GAD. However, a drawback to most of these has been the ability to demonstrate a causal role for improved metacognitive abilities in outcome. In the present study, we utilized multilevel time-lagged segment analyses to explore the temporal dynamics between session-by-session changes in metacognition and anxiety outcomes from ERT. Thirty-one young adults diagnosed with GAD with and without co-occurring depression received 16 sessions of ERT. Prior to each session, participants completed questionnaires pertaining to metacognition (i.e., decentering and cognitive reappraisal) and anxiety symptoms (i.e., worry, trait anxiousness, and generalized anxiety). Changes in decentering temporally preceded changes in worry and trait anxiousness of a medium to large magnitude, and changes in cognitive reappraisal temporally preceded changes in all three outcomes of a medium to large magnitude. The reverse direction, where mediators were predicted by outcomes, was non-significant. These findings support the notion that adaptive metacognitive emotion regulation is involved in reducing worry and anxiety in GAD. Having a clearer understanding of the temporal dynamics between metacognitive abilities and symptoms of anxiety can inform and improve not only ERT but other CBTs for GAD, as well.
Keywords: CBT, mediation, emotion regulation, GAD, distress disorders
Generalized anxiety disorder (GAD) is a costly and disabling mental disorder (e.g., Henning, Turk, Mennin, Fresco, & Heimberg, 2007). Epidemiological studies have documented GAD to be a highly prevalent disorder (Bandelow & Michaelis, 2015; Weisberg, 2009), which is unlikely to subside without treatment, and therefore is often considered a chronic disorder (Yonkers, Dyck, & Keller, 2001). GAD often co-occurs with major depressive disorder (MDD) and the two disorders are believed to share a heightened emotionality, as well as an overreliance on cognitive and behavioral avoidance (Mennin & Fresco, 2013). Given these high rates of comorbidity and overlapping symptoms, GAD and MDD have been termed “distress disorders” (e.g., Watson, 2005). When co-occurring, the subjective distress and functional impairment may be even larger, and the treatment response worse (Farabaugh et al., 2012; Newman, Przeworski, Fisher, & Borkovec, 2010; Olatunji, Cisler, & Deacon, 2010).
Self-reflection involves the ability to hold one’s self in awareness, offering the human species many advantages for survival and pursuit of reward (Mennin & Fresco, 2013). Humans naturally create internal representations in which we imagine ourselves in past situations or project ourselves into future situations, which assist us in deciding upon an optimal behavioral response. Self-referential mental activity such as mental time travel and self-awareness are crucial for managing a world in which there is ambiguity and uncertainty (e.g., Mennin & Fresco, 2013; Morin, 2011; Suddendorf & Corballis, 2007). Similarly, the ability to self-reflect is associated with better interpersonal functioning such as empathic relating to others (e.g., Amodio & Frith, 2006). A core feature of distress disorders is the engagement of maladaptive self-referential processes, including the metacognitive processes of worry and rumination (Nolen-Hoeksema, Wisco, & Lyubomirsky, 2008; Wells, 2005). Specifically concerning GAD, excessive worry is a defining diagnostic feature (American Psychiatric Association, 2013), and a number of models have been proposed with the aim of understanding the processes involved in and functions of worry (e.g., Berenbaum, 2010; Borkovec, Alcaine, & Behar, 2004; Hirsch & Mathews, 2012; Newman & Llera, 2011; Wells, 2005). Shared among these models is an understanding of worry as a response to perceived threats, indicating a discrepancy between a current emotional or motivational state and a representation of the future. Some models emphasize the processes involved in worry. For instance, in a two-phase model of worry, it has been suggested that it is important to distinguish between the degree to which an individual is prone to worry on one side, and is having difficulty terminating worry once the worrying process has begun on the other (Berenbaum, 2010). Other models underscore the function of worry as a regulatory strategy aimed at emotional avoidance and distress reduction (Borkovec et al., 2004; Newman & Llera, 2011).
Although variation exists between cognitive behavioral therapies (CBTs), a shared assumption among the underlying treatment models is that psychopathology is, in part, characterized by maladaptive cognitive processes which contribute to emotional dysfunction (Mennin, Ellard, Fresco, & Gross, 2013). Accordingly, clinical improvement is fostered via cognitive change, and many forms of CBTs for GAD have targeted worry through the building of healthier metacognitive skills (e.g., Clark & Beck, 2010; Mennin & Fresco, 2014; Roemer & Orsillo, 2009; Wells, 2009). In particular, decentering and reappraisal are two metacognitive skills, routinely practiced in CBT packages, considered to represent healthier metacognition.
Decentering refers to the ability to observe thoughts and feelings from a distanced perspective as transient internal events rather than permanent aspects of the self (Fresco et al., 2007; Safran & Segal, 1990). Although decentering is inversely correlated with negative self-referential processing, the ability to decenter has been found to explain unique variance in outcomes such as increased problem-solving behavior and improved interpersonal behavior during conflicts among couples (Ayduk & Kross, 2010), suggesting that decentering is not simply ‘the opposite’ of negative self-referentiality. Decentering has been associated with a range of positive mental health outcomes, including lower levels of anxiety and depression symptoms (for an overview see Bernstein et al., 2015). Cognitive reappraisal concerns the ability to change one’s evaluation of an event to alter its emotional significance (Gross, 2001)—in effect, it reflects a secondary appraisal of one’s initial interpretation of a situation. Across a number of studies, this ability has been associated with a range of positive outcomes, including affective (e.g., decreasing negative affect), cognitive (e.g., memory performance), and social outcomes (e.g., closer relationships with friends; for an overview see Gross, 2014). Individuals with GAD report using less reappraisal in daily life compared with healthy controls, and the extent to which reappraisal is employed has been inversely associated with anxiety severity and functional impairment across participants (Manber Ball, Ramsawh, Campbell-Sills, Paulus, & Stein, 2013).
CBTs have successfully treated GAD, demonstrating moderate to large effects during the acute phase of GAD treatment that are largely maintained throughout follow-up (Cuijpers et al., 2014; Hayes-Skelton, Roemer, & Orsillo, 2013; Mennin, Fresco, O’Toole, & Heimberg, 2018; Wells et al., 2010). Although metacognitive skills are considered crucial in producing change in these treatments for GAD (e.g., Clark & Beck, 2010; Roemer & Orsillo, 2009; Mennin & Fresco, 2014; Wells, 2009), much is yet to be understood in terms of why these treatments work. Indeed, factors responsible for change during these treatments are important to identify as they can point to pathways of improving therapeutic strategies so they more directly target change-potent components (Kazdin, 2014). Kazdin (2007) has defined a mechanism of psychological treatment as the steps or processes through which therapy actually unfolds and produces the change. Mechanisms explain how the intervention translates into events that lead to the outcome, whereas mediators account for a statistical association. A mechanism is thus an explanatory construct, where a mediator can be considered an intervening variable that explains the statistical association between an intervention and an outcome (Holmes et al., 2018). An important step in identifying treatment mechanisms is the investigation of research into statistical treatment mediators, taking the timeline of change into consideration, documenting that a change in the mediator precedes a change in outcome (Holmes et al., 2018; Kazdin, 2007; Pek & Hoyle, 2016; Tryon, 2018). However, only a sparse number of studies have conducted mediational investigations and even fewer have taken the timeline of change into account in the investigation of improved metacognitive abilities as facilitative of change in CBTs for GAD.
Hoge and colleagues (2015) investigated mindfulness and decentering as two possible treatment mediators during a mindfulness-based stress reduction (MBSR) program in a sample of individuals with GAD. Analyses revealed that changes in both mindfulness and decentering significantly mediated the effect of MBSR on anxiety symptoms but not worry. When both mediators were included in the model, only increases in decentering remained statistically significant. These analyses do not speak to the timeline of change, as mediators and outcomes were only evaluated pre- and posttreatment. Other studies have evaluated the proposed mediators multiple times during treatment. In a study by Arch and colleagues (2012), cognitive defusion was explored as a mediator of change in worry, among other outcomes. Cognitive defusion is related to the concept of decentering, but more specifically concerns decentering from the literal meaning of one’s cognition (Hayes, Strosahl, & Wilson, 2012). In a group of individuals with mixed anxiety disorders (19% had a diagnosis of GAD) following CBT and Acceptance and Commitment Therapy (ACT), session-by-session change in cognitive defusion was shown to mediate worry outcomes in both treatments. This finding was more prominent in patients receiving CBT as compared to ACT. Analyses were conducted according to the MacArthur guidelines as outlined by Kraemer and colleagues (2002), where a variable can be considered a mediator of treatment outcome if 1) it is measured during treatment, 2) the rate of change during treatment is correlated with the treatment of interest, 3) it either has a direct relation with the outcome variable or interacts with the treatment condition in its relation to the outcome. Although the mediator was evaluated multiple times during treatment, the outcome was only completed at pre- and posttreatment. It thus remains to be known, when during treatment the outcome changed, and if this indeed took place following a change in the mediator. In a study comparing Acceptance-Based Behavior Therapy (ABBT) and Applied Relaxation (AR) in the treatment of GAD (Hayes-Skelton et al., 2013), Hayes-Skelton and colleagues (2015), were able to establish a proper timeline of change because both the mediator (i.e., decentering) and outcome (i.e., anxiety symptoms) were evaluated during treatment. Decentering was found to be a common mediator across both treatment conditions. Decentering significantly increased across both treatment conditions, and this increase predicted better symptom outcomes. In terms of reappraisal, although widely studied within the context of other anxiety disorders (e.g., threat reappraisal; Smits, Julian, Rosenfield, Powers, & Smits, 2012), this research has been lacking in terms of GAD. Taken together, metacognitive skills including decentering and related constructs, appear to change as a function of a number of different CBTs and likely play a mediational role in the treatment of GAD. However, more research addressing the question of causality is clearly needed. One way of doing this is to measure both the proposed mediators and outcomes every session and perform so-called time-lagged segment analyses, where the mediator at sessionx, controlled for sessionX-1, predicts outcome at sessionX+1, controlled for sessionX, thus ensuring no overlap in time between the segments and allowing for causal interpretations.
In the present study, we utilized these time-lagged segment analyses in a secondary analysis of an open trial testing the efficacy of Emotion Regulation Therapy (ERT) for individuals with GAD with and without co-occurring depression (Renna et al., 2018). ERT has demonstrated considerable preliminary efficacy, not only in an open trial setting (Mennin, Fresco, Ritter, & Heimberg, 2015; Renna et al., 2018), but also in a randomized controlled trial (Mennin et al., 2018). ERT is hypothesized to work, in part, by improving emotion regulation skills, including the metacognitive skills of decentering and cognitive reappraisal. In a previous correlation-based mediation analysis, both cognitive reappraisal and decentering were shown to be associated with better anxiety outcomes, with the largest effects detected for the latter (Mennin et al., 2018). In further delineating these mechanisms, it is important to establish a proper timeline between changes in metacognitive skills and outcomes relevant to GAD.
Method
Participants and procedures
Participants (N = 31) were treatment-seeking young adults (age between 18 and 29 years old), enrolled in a large, urban, and diverse university in the northeastern United States. The main inclusion criterion was the presence of a GAD diagnosis (primary or secondary). Other comorbid mood and anxiety disorders were allowed. Current and lifetime diagnostic history was determined with the Structured Clinical Interview for DSM-IV Axis I Disorders (SCID; First, Spitzer, Gibbon, & Williams, 2002). Diagnostic reliability between the SCID interviewer and independent assessor for GAD was high with kappa ratings ranging from .71 to 1.00, demonstrating good to excellent reliability. Participants were required to speak and understand English, and to be stabilized on any psychotropic medications for at least 3 months prior to the start of treatment. Finally, participants could not be enrolled in any other form of psychological treatment during the acute phase of ERT (16 weeks) and had to be free of active suicidal intent or plan, psychosis, bipolar I disorder, anorexia or bulimia nervosa, somatoform disorders, or substance and alcohol dependence. The Institutional Review Board of the college approved all procedures.
Materials
Symptom outcome measures
To complement the assessment of treatment change reported in the parent trial (Renna et al., 2018), patients also completed a set of weekly measures. Prior to each session, participants completed questionnaires pertaining to metacognition (i.e., decentering and cognitive reappraisal) and anxiety symptoms (i.e., worry, trait anxiousness and symptom of generalized anxiety), all of which in their instructions inquired about the past week.
Worry was assessed with The Penn State Worry Questionnaire (PSWQ; Meyer, Miller, Metzger, & Borkovec, 1990; Stöber & Bittencourt, 1998). The PSWQ consists of 15 items (e.g., “My worries overwhelmed me” and ”Many situations made me worry”) and in the current study obtained a Cronbach’s alpha at session 1 of .80.
Trait anxiousness was assessed with The State Trait Anxiety Inventory–7 (STAI-7; Bieling, Antony, & Swinson, 1998; Spielberger, Gorsuch, Lushene, Vagg, & Jacobs, 1983), which is a seven-item measure of trait-level anxiety (e.g., “I felt nervous and restless” and “I feel that difficulties are piling up so I cannot overcome them”). Internal consistency of the STAI-7 was moderate at session 1 (Cronbach’s α = .64).
Symptoms of generalized anxiety disorder was evaluated with the GAD-7 (e.g, “Feeling nervous, anxious or on edge” and “Not being able to stop or control worrying”; Spitzer, Kroenke, Williams, & Löwe, 2006) and obtained an acceptable internal constancy at session 1 (α = .72).
Measures of metacognitive emotion regulation
Decentering was assessed with The Experiences Questionnaire (EQ; Fresco et al., 2007), using the decentering subscale consisting of 11 items, where higher scores indicate a greater ability to utilize this skill. In the current study, the original 11-item version was reduced to four specific items, evaluated to be appropriate for the weekly context (i.e., “I could separate myself from my thoughts and feelings”; “I could observe unpleasant feelings without being drawn into them”; ”I could actually see that I am not my thoughts”; “I viewed things from a wider perspective”). The internal consistency of the EQ at pretreatment was acceptable (α = .68).
Cognitive reappraisal as evaluated with The Emotion Regulation Questionnaire - Reappraisal Subscale (ERQ-R; Gross & John, 2003). The ERQ-R is a six-item measure where higher scores indicate a greater ability to utilize this skill (e.g., “In order to feel more positive emotion (such as joy and amusement), I changed what I was thinking about” and “I controlled my emotions by changing the way I thought about the situation”). The scale demonstrated strong internal consistency in the current study at session 1 (α = .86).
Treatment
ERT was delivered individually over 16 weekly sessions, each lasting 60 minutes, with the exception of sessions 10–13, which lasted 90 minutes each (Mennin & Fresco, 2014). The first half of ERT is focused on psychoeducation and the cultivation of emotion regulation skills, including attentional skills (i.e., shifting and sustaining attention on a difficult experience) and metacognition regulation skills such as decentering from (i.e., viewing oneself as separate from one’s emotional experience; introduced in session 5) and reappraisal of emotional experiences (i.e., the ability to change one’s evaluation of an event to alter its emotional significance; introduced in session 7). The second half of ERT aims to help clients utilize their learned skills towards confronting intrinsically rewarding activities when perceived risk is high. This objective is accomplished through hybrid exposure/activation exercises both within session, involving imaginal rehearsal and experiential dialogue, and outside of session, involving in vivo exposure. Twelve doctoral students in clinical psychology were trained to administer the ERT protocol and received weekly supervision by the protocol developers (DMF and DSM). Concerning adherence to the treatment protocol (i.e., therapist skillfulness and frequency of ERT components), all treatment sessions were audio recorded, and research assistants coded all 16 sessions from 40% of all cases, with 25% of these cases coded by two coders. Overall skillfulness of therapists and ERT intervention consistency was very high (>90%; for more details see Renna et al., 2018).
Analytic strategy
The causal predictive value of changes in metacognitive measures was investigated in multilevel time-lagged segment analyses, specifying the intercept, not the slope, as having a random component. In these analyses, metacognition at sessionx, controlled for sessionX-1, predicted anxiety symptoms at sessionX+1, controlled for sessionX. Thus, there was no overlap in time between the segments, potentially allowing for causal interpretations. With 16 sessions, this left 14 segments to be included in the analyses. When a proposed mediator significantly predicted an outcome across the 14 segments, the reverse causal direction was also explored. Multilevel models tolerate missing observations and all participants with missing observations were retained in the analyses with their available data without any imputation. Analyses were conducted in Stata version 14. Effect sizes were calculated by a z-to-r transformation, where correlations of .10, .30 and .50, were considered small, medium, and large, respectively (Cohen, 1988).
Results
Participants’ mean age was 22.3 years old (SD =2.5), the majority was female (n = 22, 71.0%), and demonstrated racial, ethnic, and sociodemographic diversity (for more details see Renna et al., 2018). Of the 31 participants in the study, 97% (n = 30) had a primary or co-primary diagnosis of GAD, and 3% (n = 1) had GAD as a secondary diagnosis. Co-primary MDD was present in 19% (n = 6) of participants, while 13 patients endorsed a secondary diagnosis of MDD. One participant was prescribed a stable, low-dose antidepressant medication (further details on participant characteristics can be found in Renna et al., 2018). Twenty-eight of 31 participants completed the full 16 weeks of ERT.
Means and standard deviations for the two mediators and three outcomes are presented in Table 1. All variables moved in the expected direction from pre- to posttreatment, corresponding to large effect sizes (Cohen’s d > .8, calculated as the mean difference between pre- and posttreatment, standardized by the SD difference score). Table 2 shows the correlations between session 1 scores and session 16 scores for all five variables. Changes in both proposed mediators were strongly correlated with all anxiety outcomes over the course of ERT (ps < .001, r range from .51 to .58), and the two mediators were also strongly correlated (p < .001, r = .67) over time.
Table 1.
Mediator and outcome descriptives
| Pretreatment M(SD) |
Posttreatment M(SD) |
t (p) | Cohen’s d | |
|---|---|---|---|---|
| EQ | 26.2 (6.3) | 38.8 (8.1) | −6.8 (<.001) | 1.3 |
| ERQ-R | 20.8 (7.8) | 29.2 (7.3) | −5.0 (<.001) | 0.9 |
| STAI-7 | 19.8 (3.3) | 13.6 (4.2) | 6.8 (<.001) | 1.3 |
| PSWQ | 69.1 (7.3) | 50.3 (11.8) | 7.8 (<.001) | 1.4 |
| GAD-7 | 13.4 (4.6) | 5.3 (4.0) | 6.5 (<.001) | 1.2 |
Note. EQ=Experience Questionnaire (decentering), ERQ-R=Emotion Regulation Questionnaire-Reappraisal subscale, GAD-7=Symptoms of Generalized Anxiety Disorder, PSWQ= The Penn State Worry Questionnaire, t = paired samples t-test, STAI-7= The State Trait Anxiety Inventory–7.
Table 2.
Pearson correlations between mediators and outcomes
| EQ | ERQ-R | STAI-7 | PSWQ | GAD-7 | |
|---|---|---|---|---|---|
| .62** | −.68*** | −.71*** | −.53** | ||
| ERQ-R | .49** | −.61** | −.63** | −.63** | |
| STAI-7 | −.13 | −.12 | .77*** | .85*** | |
| PSWQ | −.54** | −.35 | .45* | .69*** | |
| GAD-7 | −.26 | −.31 | .54** | .51** |
Note. Coefficients below the diagonal refers to correlations between session 1 scores. Coefficients above the diagonal refers to correlations between session 16 scores.
p < .05,
p < .01,
p < .001.
EQ=Experience Questionnaire (decentering), ERQ-R=Emotion Regulation Questionnaire-Reappraisal subscale, GAD-7=Symptoms of Generalized Anxiety Disorder, PSWQ= The Penn State Worry Questionnaire, t = paired samples t-test, STAI-7= The State Trait Anxiety Inventory–7.
Changes in decentering temporally preceded changes in worry (i.e., PSWQ, z = −2.56, p = .010, r = .46) and trait anxiousness (i.e., STAI-7, z = −2.01, p = .044, r = .36) but not generalized anxiety (i.e., GAD-7, z = −1.34, p = .180, r = .24). The reverse direction, where changes in worry (z = −1.48, p = .138, r = .27) and trait anxiousness (z = −1.76, p = .078, r = .32) temporally preceded changes in decentering were not significant, although the latter was trending. Changes in cognitive reappraisal temporally preceded changes in all three outcomes (PSWQ, z = −2.37, p = .018, r = .42; STAI-7, z = −2.43, p = .016, r = .43; GAD-7, z = −2.19, p = .029, r = .39). The reverse direction was non-significant for all outcomes predicting cognitive reappraisal (ps>.2).
All analyses were repeated with the presence of a diagnosis of MDD as a moderator. All turned out non-significant expect for the effect of changes in reappraisal on subsequent changes in trait anxiousness, which was only significant for patients with a diagnosis of MDD.
In terms of the temporal dynamics between the two proposed mediators, changes in decentering predicted subsequent changes in cognitive reappraisal at the trend level and of a moderate magnitude (p = .059, r = .34), and similar results were obtained for the reverse direction (p = .080, r = .31).
Discussion
Individuals with GAD demonstrate both excessive worry and lack of healthy metacognitive skills. Accordingly, CBTs for GAD include a variety of metacognitive components aimed at improving metacognitive abilities (Cuijpers et al., 2014; Hayes-Skelton, Roemer, & Orsillo, 2013; Mennin et al., 2018; Wells et al., 2010). However, although metacognitive skills are considered crucial in producing change in these treatments for GAD, much is yet to be understood in terms of how and why these treatments work. Knowledge of the mechanisms involved in treatment gains is crucial for the optimization of our available interventions for the many individuals affected by distress disorders. Mapping the causal timeline of change between skills development and outcome can guide us in selecting and emphasizing the most change-potent treatment components (Holmes et al., 2018). Accordingly, the present study utilized time-lagged segment analyses in a secondary analysis of an open trial, testing the efficacy of ERT for individuals with GAD with and without co-occurring depression (Renna et al., 2018). Specifically, we sought to investigate the temporal dynamics between change in metacognitive emotion regulation skills (i.e., decentering and cognitive reappraisal) and symptom improvement (i.e., worry, trait anxiousness, generalized anxiety) during ERT.
We demonstrated that changes in both decentering and cognitive reappraisal indeed preceded reductions in anxiety symptoms. Concerning decentering, it temporally preceded changes in worry and trait anxiousness of a moderate to large magnitude (rs > .3), which was not the case for generalized anxiety (r < .3). The direction of this effect appeared primarily unidirectional, since worry did not predict subsequent changes in decentering, nor did trait anxiousness although the latter association was trending and of a moderate magnitude (r = .3). The largest effect was obtained for worry, which may indicate that decentering primarily targets self-referential aspects of the GAD diagnosis. Changes in cognitive reappraisal temporally preceded changes in all three outcomes of a medium to large magnitude (rs > .3). Again, a unidirectional pattern was detected, in that the reverse direction was non-significant for any of the outcomes predicting cognitive reappraisal (rs < .3). These findings provide support for the assumption that the building of healthier metacognitive skills plays an important role in treatment gains during a course of ERT. Our design - with no competing mediators and no control group - prevents us from drawing firm causal conclusions (e.g., Kazdin, 2007). However, the findings should be viewed alongside a recent randomized controlled trial, in which we were able to establish indirect effects of both decentering and reappraisal, explaining the superior effect obtained for individuals receiving ERT compared with an attention control group (Mennin et al., 2018).
Decentering and reappraisal may be important mediators in CBTs, not only for GAD but also other anxiety and mood disorders (Mennin et al., 2013). Reappraisal has been evaluated as a mediator in a number of studies of CBT for anxiety disorders. Smits and colleagues (2012) conclude that reappraisal (i.e., threat reappraisal) is consistently related to anxiety symptom improvement in CBTs, but that a very limited number of studies meet most of the criteria necessary to conclusively demonstrate that it causes symptom improvement. In terms of decentering, session-by-session changes in decentering was recently found to predict pre- to posttreatment symptom improvement for individuals with social anxiety disorder during group CBT in an open trial. It was further found that change in decentering predicted outcome improvement over and above change in reappraisal (Hayes-Skelton & Lee, 2018). This finding adds to a large cross-sectional study utilizing structural equation modeling with the aim of establishing the shared or unique variance among decentering, cognitive reappraisal, and social anxiety (Hayes-Skelton & Graham, 2013). Results revealed that the relationship between cognitive reappraisal and social anxiety was fully accounted for by decentering. Given the small number of participants in the present study, a multiple mediation model was not feasible, and the explanation of unique variance could thus not be established.
In terms of skills building over the course of ERT, decentering and cognitive reappraisal bidrectionally predicted each other at the trend level and of a moderate magnitude (rs = .3) in the present study, indicative of skills improvement having a positive spillover effect on each other. That is, on a weekly basis, improvements in one skill over a particular week, points to the likely improvement in the other skill the following week. However, such dynamics at the weekly level should not be confused with the dynamics at the momentary level, at which the specific emotional experiences to be regulated actually occur. Indeed, emotion regulation is believed to occur dynamically throughout different points in the emotion generative process (e.g., Gross, 2015; Rottenberg & Gross, 2007). Accordingly, ERT targets a number of emotion regulation skills, believed to be optimally suited for regulation at these different time points. Specifically, decentering and cognitive reappraisal are considered elaborative metacognitive emotion regulation skills, meaning that they are verbally mediated, with reappraisal requiring the most cognitive elaboration (Mennin & Fresco, 2014). These metacognitive regulatory skills are ideally employed following successful engagement of less elaborative, attention regulation skills (e.g., shifting and sustained attention to difficult or painful parts of an emotional experience). In other words, if an emotional response is intensifying, its regulation may require increased cognitive elaboration or verbal mediation (Gross, 2015; Mennin & Fresco, 2014). Although limited, some evidence does support this cascade. For instance, in an experimental setting, Hirsch and colleagues (2011) found that when individuals engaged their attention with the emotional meaning of threat words, they worried more subsequently. Within the context of GAD specifically, Cooper and colleagues (2013) found that individuals with GAD who were shown an anxiety-inducing video and instructed to disengage from a subsequent slide presentation of disgusting images reported more worrying than both those with GAD who were not instructed to disengage and healthy controls. With weekly measures, as employed in the present study, we are not capturing the emotion dynamics at this momentary level. Future studies could therefore supplement with methods suited for capturing momentary changes in regulatory processes and their effect on outcomes. This objective could be accomplished by using diary and experience sampling (i.e., ESM) studies in the mapping of changes in emotion and emotion regulation dynamics at the momentary level over the course of therapy, representing an ecological valid evaluation of the emotion regulation strategies’ adaptiveness as they occur in moments of daily life (Aldao, Sheppes, & Gross, 2015; Bernstein, Hadash, & Fresco, in press; O’Toole, Zachariae, & Mennin, 2017; Verhagen, Hasmi, Drukker, van Os, & Delespaul, 2016). In terms of ERT, an important question to answer would be if patients become better able to calibrate their choice of regulation according the temporal dynamics proposed in the model, where different emotion regulation strategies should be engaged in a particular order adjusted to the intensity of the unfolding emotional response.
Detecting mediators of treatment and understanding its mechanisms can point to different ways of optimizing existing interventions. One implication of the present findings could be to adjust the dosing of the metacognitive components, granting them more weight in the overall treatment package. However, the dosage needed is likely not identical for all individuals, and we may therefore consider employing markers for proficiency of skills or skills consolidation. ERT, where theoretically derived treatment components are building upon each other, represents a treatment well suited for exploring such markers as signals of when to progress from one treatment component to the other within treatment. This suggestion aligns with recent movements toward individually tailored psychotherapy (e.g., Fisher & Boswell, 2016), and more work is needed to develop appropriate markers for skills proficiency, which could be indicated by self-efficacy, performance in an experimental setting, frequency of use in daily life to name a few. Another point to consider in moving forward is that although the present findings point to a main effect of the metacognitive treatment components, interaction effects were not explored. This means that other treatment components could be necessary for or enhancing this causal relationship between metacognitive abilities and anxiety outcome to exist. Indeed, the ERT model suggests that metacognitive regulation always involve attention regulation but that attention regulation can occur without metacognitive regulation (Mennin & Fresco, 2014). The Multiphase Optimization Strategy (MOST; Collins, 2018) represents a systematic approach to exploring the main and interactive effects of treatment components. Here, select treatment components are evaluated in a factorial design, a so-called 2k design, where k refers to the number of components under investigation. All possible combinations of the components are evaluated, after which the components showing a main effect, or an effect in combination with another component, are evaluated in a classical randomized design. A number of studies employing MOST within mental health setting are currently under way (e.g., Uwatoko et al., 2018; Watkins et al., 2016).
The present study must be considered in light of some important limitations. First, the small number of participants did not allow for testing a multiple mediation model, and the predictive value of each of the two mediators could thus not be evaluated in a combined model. Second, analyses were based on an open trial design, and we therefore cannot conclude anything pertaining to the specificity of the findings to ERT. However, correlation-based mediation analyses on a previous randomized controlled trial did show the particular metacognitive measures to statistically mediate outcomes in the ERT condition (Mennin et al., 2018). Third, two reliability analyses (i.e., EQ and STAI) revealed Cronbach’s alphas just below the often recommended 0.70 (Nunnally, 1978), which may in part be due to the low number of items, but still pose a threat to the internal reliability. Fourth, without addressing competing mediators, we cannot rule out the possibility of other unmeasured causes of change in the outcome variables. Fifth, changes in reappraisal predicted subsequent changes in trait anxiousness, only for those with a diagnosis of MDD. Although this finding suggests that the relationship for reappraisal and outcome may be driven by presence of MDD, the relatively small number of patients with MDD in the sample precludes any firm conclusions. An important next step would be to investigate the mediational role of metacognition in a larger sample of individuals with a diagnosis of depression to explore potential differences in the mediational role of metacognition in symptom improvement. Finally, the present findings rely on self-report data. This manner of assessment has obvious clinical utility and allows for an analysis like the one used in the current study, but can be subject to reporting bias and only reflects one modality of assessment. However, the neuroimaging studies accompanying the same parent trial as the present study (Renna et al., 2018) support these findings by showing neural correlates to the detected self-reported changes in metacognitive abilities (Fresco et al., 2017; Raab et al., under review; Scult et al., under review). In an initial fMRI study, Fresco and colleagues (2017) demonstrated that gains in decentering through the course of ERT was predicted by pretreatment intrinsic functional connectivity clusters in the anterior and posterior of the default network (Fresco et al., 2017), a network demonstrated to be central to self-referential processing. ERT has more recently been found to result in increased resting functional connectivity between the posterior cingulate cortex and the dorsolateral prefrontal cortex (PFC; reflecting greater connectivity between areas of self referentiality and executive control), and this connectivity was found to be associated with improvements in metacognitive ability (Scult et al., under review) —a finding that has recently been reported in the context of subjectively distressed adults and veterans with PTSD who were treated with mindfulness based interventions (King et al., 2016). Another neuroimaging study explored neural changes by obtaining an fMRI both before and after ERT during an explicit emotion regulation task for 21 participants. Following treatment, patients had lower negative affect ratings and greater recruitment of the lateral PFC to negative versus neutral images with strengthened dorsolateral PFC activity associated with improvements in both decentering and cognitive reappraisal as well as clinical outcomes (Raab et al., under review). Although these studies did not explicitly test mediation, they bolster the current study’s findings by suggesting potential neural markers that may accompany metacognitive mechanism improvements from ERT.
In conclusion, the present study adds to the literature on metacognitive components as drivers of change in CBTs for GAD. Specifically, we demonstrated that session-by-session improvements in decentering and cognitive reappraisal temporally preceded reductions in anxiety-related outcomes through a course of ERT, and that this was best conceptualized as a unidirectional relation. Having a clearer understanding of the temporal dynamics between metacognition and symptoms of anxiety can inform and improve not only ERT but also other treatments for GAD and the distress disorders, more generally.
Figure 1.
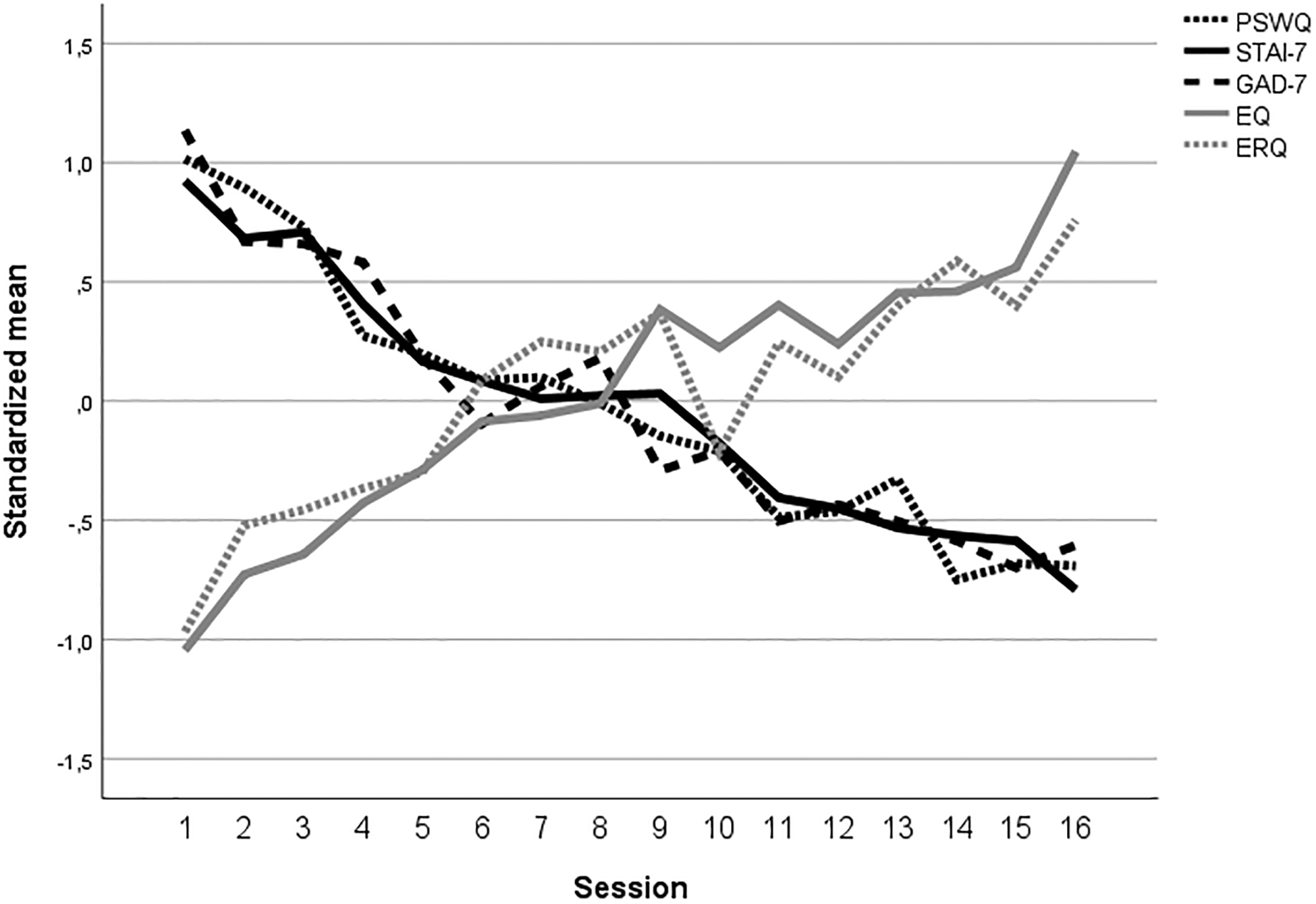
Changes over time in proposed metacognitive mediators (i.e., decentering [EQ] and reappraisal [ERQ]) and outcomes (i.e., worry [PSWQ], trait anxiousness [STAI-7], and generalized anxiety [GAD-7])
Highlights.
The study employed time-lagged segment analyses of session-by-session measures
Decentering and reappraisal were explored as mediators of ERT
Decentering and reappraisal temporally preceded symptom reduction
The reverse direction, where mediators were predicted by outcomes, was non-significant
Acknowledgments
Note: David M. Fresco was supported by National Heart, Lung, and Blood Institute Grant R01HL119977, National Institute of Nursing Research Grant P30NR015326, and National Center for Complimentary and Integrative Health Grant 1R61AT009867.
Contributor Information
Mia S. O’Toole, Aarhus University
Megan E. Renna, Teachers College, Columbia University
Douglas S. Mennin, Teachers College, Columbia University
David M. Fresco, Kent State University & Case Western Reserve University School of Medicine
References
- Aldao A, Sheppes G, & Gross JJ (2015). Emotion regulation flexibility. Cognitive Therapy and Research, 39, 263–278. doi: 10.1007/s10608-014-9662-4 [DOI] [Google Scholar]
- American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5th ed.). Arlington, VA: American Psychiatric Publishing. [Google Scholar]
- Amodio DM, & Frith CD (2006). Meeting of minds: the medial frontal cortex and social cognition. Nature Reviews.Neuroscience, 7, 268–277. doi: 10.1038/nrn1884 [DOI] [PubMed] [Google Scholar]
- Arch JJ, Wolitzky-Taylor KB, Eifert GH, & Craske MG (2012). Longitudinal treatment mediation of traditional cognitive behavioral therapy and acceptance and commitment therapy for anxiety disorders. Behaviour Research and Therapy, 50, 469–478. doi: 10.1016/j.brat.2012.04.007 [DOI] [PubMed] [Google Scholar]
- Ayduk Ö, & Kross E (2010). From a distance: Implications of spontaneous self-distancing for adaptive self-reflection. Journal of Personality and Social Psychology, 98, 809–829. doi: 10.1037/a0019205 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bandelow B, & Michaelis S (2015). Epidemiology of anxiety disorders in the 21st century. Dialogues in Clinical Neuroscience, 17, 327–335. doi: 10.1016/j.siny.2015.10.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berenbaum H (2010). An initiation-termination two-phase model of worrying. Clinical Psychology Review, 30, 962–975. doi: 10.1016/j.cpr.2010.06.011 [DOI] [PubMed] [Google Scholar]
- Bernstein A, Hadash Y, & Fresco DM (in press). Metacognitive processes model of decentering: Emerging methods and insights. Current Opinion in Psychology. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bernstein A, Hadash Y, Lichtash Y, Tanay G, Shepherd K, & Fresco DM (2015). Decentering and related constructs: A critical review and metacognitive processes model. Perspectives on Psychological Science, 10, 599–617. doi: 10.1177/1745691615594577 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bieling PJ, Antony MM, & Swinson RP (1998). The state-trait anxiety inventory, trait version: Structure and content re-examined. Behaviour Research and Therapy, 36, 777–788. doi: 10.1016/S0005-7967(98)00023-0 [DOI] [PubMed] [Google Scholar]
- Borkovec TD, Alcaine O, & Behar ES (2004). Avoidance theory of worry and generalized anxiety disorder In Heimberg R, Turk C, & Mennin DS (Eds.), Generalized anxiety disorder: Advances in research and practice (pp. 77–108). New York, NY: Guilford Press. [Google Scholar]
- Clark DA, & Beck AT (2010). Cognitive therapy of anxiety disorders: Science and practice. New York: Guilford Press. [Google Scholar]
- Cohen J (1988). Statistical power analysis for the behavioral sciences (2nd ed.). Hillsdale: Lawrence Erlbaum. [Google Scholar]
- Collins LM (2018). Optimization of multicomponent behavioral, biobehavioral, and biomedical interventions: The Multiphase Optimization Strategy (MOST). Cham: Springer International Publishing. doi: 10.1007/978-3-319-72206-1 [DOI] [Google Scholar]
- Cooper SE, Miranda R, & Mennin DS (2013). Behavioral indicators of emotional avoidance and subsequent worry in generalized anxiety disorder and depression. Journal of Experimental Psychopathology, 4, 566–583. doi: 10.5127/jep.033512 [DOI] [Google Scholar]
- Cuijpers P, Sijbrandij M, Koole S, Huibers M, Berking M, & Andersson G (2014). Psychological treatment of generalized anxiety disorder: A meta-analysis. Clinical Psychology Review, 34, 130–140. doi: 10.1016/j.cpr.2014.01.002 [DOI] [PubMed] [Google Scholar]
- Farabaugh A, Alpert J, Wisniewski SR, Otto MW, Fava M, Baer L, … Thase ME (2012). Cognitive therapy for anxious depression in STAR(*) D: what have we learned? Journal of Affective Disorders, 142, 213–218. doi: 10.1016/j.jad.2012.04.029 [DOI] [PMC free article] [PubMed] [Google Scholar]
- First MB, Spitzer RL, Gibbon M, & Williams JBW (2002). Structured Clinical Interview for DSM-IV-TR Axis I Disorders—Research version, non-patient edition with psychotic screen. New York, NY: Biometrics Research, New York State Psychiatric Institute. [Google Scholar]
- Fisher AJ, & Boswell JF (2016). Enhancing the personalization of psychotherapy with dynamic assessment and modeling. Assessment, 23, 496–506. doi: 10.1177/1073191116638735 [DOI] [PubMed] [Google Scholar]
- Fresco DM, Moore MT, van Dulmen MH, Segal ZV, Ma SH, Teasdale JD, & Williams JM (2007). Initial psychometric properties of the experiences questionnaire: validation of a self-report measure of decentering. Behavior Therapy, 38, 234–246. doi: 10.1016/j.beth.2006.08.003 [DOI] [PubMed] [Google Scholar]
- Fresco DM, Roy AK, Adelsberg S, Seeley S, García-Lesy E, Liston C, & Mennin DS (2017). Distinct functional connectivities predict clinical response with Emotion Regulation Therapy. Frontiers in Human Neuroscience, 11, 86. doi: 10.3389/fnhum.2017.00086 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gross JJ (2001). Emotion regulation in adulthood: Timing is everything. Current Directions in Psychological Science, 10, 214–219. [Google Scholar]
- Gross JJ (2014). Emotion regulation: Conceptual and empirical foundations In Gross JJ (Ed.), Handbook of emotion regulation (2nd ed., pp. 3–20). New York: The Guilford Press. [Google Scholar]
- Gross JJ (2015). Emotion regulation: Current status and future prospects. Psychological Inquiry, 26, 1–26. doi: 10.1080/1047840X.2014.940781 [DOI] [Google Scholar]
- Gross JJ, & John OP (2003). Individual differences in two emotion regulation processes: Implications for affect, relationships, and well-being. Journal of Personality and Social Psychology, 85, 348–362. doi: 10.1037/0022-3514.85.2.348 [DOI] [PubMed] [Google Scholar]
- Hayes-Skelton SA, Calloway A, Roemer L, & Orsillo SM (2015). Decentering as a potential common mechanism across two therapies for generalized anxiety disorder HHS Public Access. Journal of Consulting and Clinical Psychology, 83, 395–404. doi: 10.1037/a0038305 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hayes-Skelton SA, & Graham J (2013). Decentering as a common link among mindfulness, cognitive reappraisal, and social anxiety. Behavioural and Cognitive Psychotherapy, 41, 317–328. doi: 10.1017/S1352465812000902 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hayes-Skelton SA, & Lee CS (2018). Changes in decentering across cognitive behavioral group therapy for social anxiety disorder. Behavior Therapy, 49, 809–822. doi: 10.1016/j.beth.2018.01.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hayes-Skelton SA, Roemer L, & Orsillo SM (2013). A randomized clinical trial comparing an acceptance based behavior therapy to applied relaxation for generalized anxiety disorder. Journal of Consulting and Clinical Psychology, 81, 761–773. doi: 10.1016/j.biotechadv.2011.08.021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hayes SC, Strosahl KD, & Wilson KG (2012). Acceptance and commitment therapy: The process and practice of mindful change (2nd ed.). New York: The Guilford Press. [Google Scholar]
- Henning ER, Turk CL, Mennin DS, Fresco DM, & Heimberg RG (2007). Impairment and quality of life in individuals with generalized anxiety disorder. Depression and Anxiety, 24, 342–349. doi: 10.1002/da.20249 [DOI] [PubMed] [Google Scholar]
- Hirsch CR, MacLeod C, Mathews A, Sandher O, Siyani A, & Hayes S (2011). The contribution of attentional bias to worry: distinguishing the roles of selective engagement and disengagement. Journal of Anxiety Disorders, 25, 272–277. doi: 10.1016/j.janxdis.2010.09.013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hirsch CR, & Mathews A (2012). A cognitive model of pathological worry. Behaviour Research and Therapy, 50, 636–646. doi: 10.1016/j.brat.2012.06.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hoge EA, Bui E, Goetter E, Robinaugh DJ, Ojserkis RA, Fresco DM, … Ojserkis RA (2015). Change in decentering mediates improvement in anxiety in mindfulness-based stress reduction for generalized anxiety disorder. Cognitive Therapy and Research, 39, 228–235. doi: 10.1007/s10608-014-9646-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holmes EA, Ghaderi A, Harmer CJ, Ramchandani PG, Cuijpers P, Morrison AP, … Craske MG (2018). The Lancet Psychiatry Commission on psychological treatments research in tomorrow’s science. The Lancet Psychiatry, 5, 237–286. doi: 10.1016/S2215-0366(17)30513-8 [DOI] [PubMed] [Google Scholar]
- Kazdin AE (2007). Mediators and mechanisms of change in psychotherapy research. Annual Review of Clinical Psychology, 3, 1–27. doi: 10.1146/annurev.clinpsy.3.022806.091432 [DOI] [PubMed] [Google Scholar]
- Kazdin AE (2014). Moderators, mediators and mechanisms of change in psychotherapy In Lutz W & Knox S (Eds.), Explorations in mental health. Quantitative and qualitative methods in psychotherapy research (pp. 87–101). New York, NY: Routledge/Taylor & Francis Group. [Google Scholar]
- King AP, Block SR, Sripada RK, Rauch S, Giardino N, Favorite T, … Liberzon I (2016). Altered default mode network (DMN) resting state functional connectivity following a mindfulness-based exposure therapy for posttraumatic stress disorder (PTSD) in combat veterans of Afghanistan and Iraq. Depression and Anxiety, 33, 289–299. doi: 10.1002/da.22481 [DOI] [PubMed] [Google Scholar]
- Kraemer HC, Wilson GT, Fairburn CG, & Agras WS (2002). Mediators and moderators of treatment effects in randomized clinical trials. Archives of General Psychiatry, 59, 877–883. [DOI] [PubMed] [Google Scholar]
- Manber Ball T, Ramsawh HJ, Campbell-Sills L, Paulus MP, & Stein MB (2013). Prefrontal dysfunction during emotion regulation in generalized anxiety and panic disorder. Psychological Medicine, 43, 1475–1486. doi: 10.1017/S0033291712002383 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mennin DS, Ellard KK, Fresco DM, & Gross JJ (2013). United we stand: Emphasizing commonalities across cognitive-behavioral therapies. Behavior Therapy, 44, 234–248. doi: 10.1016/j.beth.2013.02.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mennin DS, & Fresco DM (2013). What, me worry and ruminate about dsm-5 and rdoc? The importance of targeting negative self-referential processing. Clinical Psychology: Science and Practice, 20, 258–267. doi: 10.1111/cpsp.12038 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mennin DS, & Fresco DM (2014). Emotion regulation therapy In Gross JJ (Ed.), Handbook of emotion regulation (2nd ed., pp. 469–490). New York: Guilford Press. [Google Scholar]
- Mennin DS, Fresco DM, O’Toole MS, & Heimberg RG (2018). A randomized controlled trial of emotion regulation therapy for generalized anxiety disorder with and without co-occurring depression. Journal of Consulting and Clinical Psychology, 86, 268–281. doi: 10.1037/ccp0000289 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mennin DS, Fresco DM, Ritter M, & Heimberg RG (2015). An open trial of Emotion Regulation Therapy for generalized anxiety disorder and coocurring depression. Depression and Anxiety, 32(8), 614–623. doi: 10.1002/da.22377 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meyer TJ, Miller ML, Metzger RL, & Borkovec TD (1990). Development and validation of the Penn State Worry Questionnaire. Behaviour Research and Therapy, 28, 487–495. doi: 10.1016/0005-7967(90)90135-6 [DOI] [PubMed] [Google Scholar]
- Morin A (2011). Self-Awareness Part 1: Definition, measures, effects, functions, and antecedents. Social and Personality Psychology Compass, 10, 807–823. [Google Scholar]
- Newman MG, & Llera SJ (2011). A novel theory of experiential avoidance in generalized anxiety disorder: A review and synthesis of research supporting a contrast avoidance model of worry ,☆,☆☆. Clinical Psychology Review, 31, 371–382. doi: 10.1016/j.cpr.2011.01.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Newman MG, Przeworski A, Fisher AJ, & Borkovec TD (2010). Diagnostic comorbidity in adults with generalized anxiety disorder: Impact of comorbidity on psychotherapy outcome and impact of psychotherapy on comorbid diagnoses. Behavior Therapy, 41, 59–72. doi: 10.1016/j.beth.2008.12.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nolen-Hoeksema S, Wisco BE, & Lyubomirsky S (2008). Rethinking rumination. Perspective on Psychological Science, 3, 400–424. [DOI] [PubMed] [Google Scholar]
- Nunnally JC (1978). Psychometric theory. New York: McGraw-Hill. [Google Scholar]
- O’Toole MS, Zachariae R, & Mennin DS (2017). Social anxiety and emotion regulation flexibility: considering emotion intensity and type as contextual factors. Anxiety, Stress and Coping, 30, 716–724. doi: 10.1080/10615806.2017.1346792 [DOI] [PubMed] [Google Scholar]
- Olatunji BO, Cisler JM, & Deacon BJ (2010). Efficacy of cognitive behavioral therapy for anxiety disorders: A review of meta-analytic findings. Psychiatric Clinics of North America, 33, 557–577. doi: 10.1016/j.psc.2010.04.002 [DOI] [PubMed] [Google Scholar]
- Pek J, & Hoyle RH (2016). On the (in)validity of tests of simple mediation: Threats and solutions. Social and Personality Psychology Compass, 10, 150–163. doi: 10.1111/spc3.12237 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Raab HA, Sandman CF, Seeley SH, Garcia-Lesy E, Liston C, Fresco DM, & Mennin DS (2018). Greater prefrontal recruitment associated with clinical improvement and regulatory skills in generalized anxiety patients following Emotion Regulation Therapy: A pilot investigation. Manuscript under Review. [Google Scholar]
- Renna ME, Quintero JM, Soffer A, Pino M, Ader L, Fresco DM, & Mennin DS (2018). A pilot study of Emotion Regulation Therapy for generalized anxiety and depression: Findings from a diverse sample of young adults. Behavior Therapy, 49, 403–418. doi: 10.1016/j.beth.2017.09.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roemer L, & Orsillo SM (2009). Mindfulness- & acceptance-based behavioral therapies in practice. New York: The Guilford Press. [Google Scholar]
- Rottenberg J, & Gross JJ (2007). Emotion and emotion regulation: A map for psychotherapy researchers. Clinical Psychology: Science and Practice, 14, 323–328. doi: 10.1111/j.1468-2850.2007.00093.x [DOI] [Google Scholar]
- Safran JD, & Segal ZV (1990). Interpersonal process in cognitive therapy. Lanham, MD, US: Jason Aronson; Retrieved from http://psycnet.apa.org/record/1990-97853-000 [Google Scholar]
- Scult MA, Fresco DM, Gunning FM, Liston C, Seeley SH, Garcia E, & Mennin DS (2018). Changes in functional connectivity following treatment with Emotion Regulation Therapy. Manuscript under Review. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smits JA, Julian K, Rosenfield D, Powers MB, & Smits J (2012). Threat reappraisal as a mediator of symptom change in cognitive-behavioral treatment of anxiety disorders: A systematic review. Journal of Consulting Clinical Psychology, 80, 624–635. doi: 10.1037/a0028957 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spielberger CD, Gorsuch RL, Lushene R, Vagg PR, & Jacobs GA (1983). Manual for the State-Trait Anxiety Inventory. Palo Alto, CA: Consulting Psychologists Press. [Google Scholar]
- Spitzer RL, Kroenke K, Williams JBW, & Löwe B (2006). A brief measure for assessing generalized anxiety disorder: The GAD-7. Archives of Internal Medicine, 166, 1092–1097. doi: 10.1001/archinte.166.10.1092 [DOI] [PubMed] [Google Scholar]
- Stöber J, & Bittencourt J (1998). Weekly assessment of worry: An adaptation of the Penn State Worry Questionnaire for monitoring changes during treatment. Behaviour Research and Therapy, 36, 645–656. doi: 10.1016/S0005-7967(98)00031-X [DOI] [PubMed] [Google Scholar]
- Suddendorf T, & Corballis MC (2007). The evolution of foresight: What is mental time travel, and is it unique to humans? Behavioral and Brain Sciences, 30, 299–313; discussion 313–51. doi: 10.1017/S0140525X07001975 [DOI] [PubMed] [Google Scholar]
- Tryon WW (2018). Mediators and Mechanisms. Clinical Psychological Science, 6, 619–628. doi: 10.1177/2167702618765791 [DOI] [Google Scholar]
- Uwatoko T, Luo Y, Sakata M, Kobayashi D, Sakagami Y, Takemoto K, … Furukawa TA (2018). Healthy Campus Trial: A multiphase optimization strategy (MOST) fully factorial trial to optimize the smartphone cognitive behavioral therapy (CBT) app for mental health promotion among university students: Study protocol for a randomized controlled trial. Trials, 19, 353. doi: 10.1186/s13063-018-2719-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- Verhagen SJW, Hasmi L, Drukker M, van Os J, & Delespaul PAEG (2016). Use of the experience sampling method in the context of clinical trials. Evidence-Based Mental Health, 19, 86–89. doi: 10.1136/ebmental-2016-102418 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Watkins E, Newbold A, Tester-Jones M, Javaid M, Cadman J, Collins LM, … Mostazir M (2016). Implementing multifactorial psychotherapy research in online virtual environments (IMPROVE-2): Study protocol for a phase III trial of the MOST randomized component selection method for internet cognitive-behavioural therapy for depression. BMC Psychiatry, 16. doi: 10.1186/s12888-016-1054-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Watson D (2005). Rethinking the mood and anxiety disorders: A quantitative hierarchical model for DSM-V. Journal of Abnormal Psychology, 114, 522–536. doi: 10.1037/0021-843X.114.4.522 [DOI] [PubMed] [Google Scholar]
- Weisberg RB (2009). Overview of generalized anxiety disorder: epidemiology, presentation, and course. The Journal of Clinical Psychiatry, 70, 4–9. [PubMed] [Google Scholar]
- Wells A (2005). The metacognitive model of GAD: Assessment of meta-worry and relationship with DSM-IV generalized anxiety disorder. Cognitive Therapy and Research, 29, 107–121. doi: 10.1007/s10608-005-1652-0 [DOI] [Google Scholar]
- Wells A (2009). Metacognitive therapy for anxiety and depression. New York, NY: Guilford Press. doi: 10.1080/10615800902833770 [DOI] [Google Scholar]
- Wells A, Welford M, King P, Papageorgiou C, Wisely J, & Mendel E (2010). A pilot randomized trial of metacognitive therapy vs applied relaxation in the treatment of adults with generalized anxiety disorder. Behaviour Research and Therapy, 48, 429–434. doi: 10.1016/j.brat.2009.11.013 [DOI] [PubMed] [Google Scholar]
- Yonkers KA, Dyck IR, & Keller MB (2001). An eight-year longitudinal comparison of clinical course and characteristics of social phobia among men and women. Psychiatric Services, 52, 637–643. [DOI] [PubMed] [Google Scholar]


