Abstract
Introduction
This study is the first nationally representative survey of U.S. adults (18+) to examine perceptions of the relative harms of eight non-cigarette tobacco products.
Methods
Data are from Wave 1 of the Population Assessment of Tobacco and Health (PATH) Study Adult Questionnaire, a nationally representative study of 32,320 adults in the United States conducted from September 2013 to December 2014.
Results
40.7% of adults believed that electronic cigarettes were less harmful than cigarettes, and 17.8% of adults believed that hookah was less harmful than cigarettes. Those less knowledgeable about the health risks of smoking were more likely to believe that the non-cigarette products were less harmful than cigarettes. Current non-cigarette tobacco product users were more likely to perceive that product to be less harmful than cigarettes (except filtered cigars). There was a significant positive correlation between beliefs that cigarettes were harmful and the likelihood of using hookah; perceptions of the harmfulness of cigarettes was not associated with the likelihood of using any other product.
Conclusions
Perceptions of harmfulness varied widely across non-cigarette tobacco products. E-cigarettes and hookah in particular are seen as less harmful compared to cigarettes.
Keywords: electronic cigarette, hookah, perception of harm, tobacco products
BACKGROUND
The Family Smoking Prevention and Tobacco Control Act (TCA) enacted in 2009 granted the Food and Drug Administration (FDA) regulatory authority over “the manufacture, marketing, and distribution of tobacco products.”1 In addition, FDA finalized a rule, effective August 2016 that extended its authority to all products that meet the definition of a tobacco product including e-cigarettes, cigars, pipes, and water pipes/hookahs.2 Included in the provisions are a national minimum age for sales, required health warnings, tobacco product ingredient reporting, and reporting of harmful and potentially harmful constituents.
Understanding public perceptions about tobacco products can help to inform the FDA as it develops policies and regulations for tobacco products and the marketing of those products. The Population Assessment of Tobacco and Health (PATH) Study is a nationally representative, longitudinal cohort study of adults and youth in the U.S., designed to inform and monitor the impact of FDA’s regulatory actions to reduce tobacco-related death and disease.3 Its sampling design, cohort design, and very large sample size endows the PATH Study with the potential for more rigorous investigations of perceptions that the US public holds of cigarettes and of non-cigarette tobacco products. In recent years, the range of non-cigarette tobacco products, especially in the class of e-cigarettes, has expanded greatly, and in this new and more complex market of tobacco products it is even more important to understand consumer perceptions about these tobacco products.
Perceptions of harmfulness are important determinants of tobacco product selection,4 quit intentions,5 and quitting behavior.6 Perceptions of the relative harmfulness of different types of tobacco products are influenced, in part, by advertising (e.g. historical messages with explicit and implicit health claims),7 packaging and labelling (e.g., package colors, historical brand descriptors such as “light” and “low tar”),4,8 and consumer reactions to trying a product (i.e., chemosensory responses—taste, harshness).9 Product harm perceptions are important to understand since they are predictors of whether people will be interested in trying a product or not.4,10,11 For example, perceptions that filtered and low tar/nicotine brand cigarettes were less harmful was an important factor in the market growth of filtered and low tar/nicotine cigarettes.7,12 Similarly, among young adults the uptake of electronic cigarettes has been linked to the perception that these products provide lower overall health risks compared to cigarettes.13
Studies comparing perceptions of the relative harmfulness of different tobacco products to cigarettes have found that e-cigarettes14,15 and hookah16–18 are perceived to be less harmful than cigarettes. Cigars, cigarillos, and little cigars are perceived as just as harmful as cigarettes.19–21 Non-combusted tobacco products including snus, smokeless tobacco, and dissolvables are perceived as just as harmful as or more harmful than cigarettes.22–26
Cigarette smokers (relative to non-smokers)27 and users of e-cigarettes,25,28 hookah,29 and smokeless tobacco (including snus and snuff)24–26 dissolvables,25 cigars,20 little cigars and cigarillos,19 relative to non-users were more likely to believe that these products were less harmful than cigarettes. These findings are in line with previous observations that many tobacco users are subject to an optimism bias and therefore tobacco users may be more likely to underestimate their health risks compared to non-users.30
Comparing across multiple combusted tobacco products, a nationally representative survey (conducted from 2002–2004) found that among the U.S. adult sample of 13,322 smokers, 22.2% reported that some combusted tobacco products were less harmful than others.24 Another study (conducted in 2013) used a sample of 10,000 students in two U.S. universities and found that across multiple combusted and non-combusted tobacco products, e-cigarettes were rated the least harmful to health followed by hookah, cigarettes, and cigar products, whereas smokeless tobacco was rated as the most harmful.31 These findings indicate that perceptions of the harmfulness of tobacco products may not correspond with the current scientific evidence on the levels of toxicants in tobacco products23,26 which has demonstrated that in general combustible tobacco products are more harmful to long-term users than non-combustible tobacco products.32
A limitation of the existing research is that the majority of studies are not nationally representative, or rely on convenience samples.13,16–21,25,28,29 Further, whereas previous research has examined risk perceptions of non-cigarette tobacco products typically one at a time (e.g. perceptions of e-cigarettes15 or a few products at a time (e.g. risk perceptions of e-cigarettes and smokeless tobacco,23 this study examines risk perceptions across multiple products in a single study therefore allowing comparisons of the relative percpetions of the harmfulness of different products (by controlling for differences in samples and sampling design).23–26 Additionally, a study by Bernat et al (2017) examined absolute perceptions of the harmfulness of seven tobacco products in a single study.33 Research has demonstrated that there are differences in perceptions of harm according to whether an absolute or a relative risk is examined. Therefore, the current study will complement research by Bernet et al (2017) by examining perceptions of the relative harmfulness of tobacco products compared to cigarettes across eight different products (Aim 1).33 Additionally, Weaver et al., 2016 examined awareness and use of tobacco products but did not examine factors associated with risk perceptions of these different products and this study may be limited by its sampling design (an internet panel).34 The study will therefore address this gap by using a large, robust, nationally representative face-to-face study examining how perceptions of the relative harmfulness of tobacco products relate to use (Aim 3). Finally, the existing research studies are mostly descriptive 16,17,20,23 and few examine the factors associated with harm perceptions of multiple products (Aim 2) 24–26 and there is a lack of research examining how perceptions of the harmfulness of cigarettes are related to product use among adults (Aim 4).
The current study is the first to utilize a nationally representative sample of U.S. adults (ages 18 years and older) to examine perceptions of the relative harms of eight non-cigarette tobacco products: e-cigarettes, hookah, traditional cigars, filtered cigars, cigarillos, pipe, smokeless tobacco, and dissolvables. This study has four aims: (1) to measure perceptions of the harmfulness of eight non-cigarette tobacco products relative to cigarettes and to determine how these perceptions vary across these products; (2) to identify the characteristics of U.S. adults that are associated with perceptions of harmfulness of non-cigarette tobacco products, especially the characteristics related to perceiving that a particular non-cigarette tobacco product is less harmful (vs. no different or more harmful) than cigarettes; (3) to determine the relation between perceived harmfulness of each non-cigarette tobacco product and the likelihood of using that product; and (4) to measure the perceptions of harmfulness of cigarettes and determine how these perceptions vary as a function of products used.
METHODS
Data are from Wave 1 of the PATH Study conducted from September 12, 2013 to December 15, 2014 and analyzed in 2016. The PATH Study is a nationally representative, longitudinal cohort study of 45,971 adults and youth in the U.S., ages 12 years and older. The National Institutes of Health, through the National Institute on Drug Abuse, is partnering with the FDA’s Center for Tobacco Products to conduct the PATH Study under a contract with Westat. This cross sectional analysis is based on 32,320 Wave 1 adult (18 years and older) interviews and subsets of those adults who were aware of different types of non-cigarette tobacco products.
Recruitment employed address-based, area-probability sampling, using an in-person household screener to select youths and adults. Adult tobacco users, young adults aged 18 to 24, and African Americans were oversampled relative to population proportions. The PATH Study used Audio-Computer Assisted Self-Interviews (ACASI) available in English and Spanish to collect information on tobacco-use patterns and associated health behaviors.
The weighting procedures adjusted for oversampling and nonresponse; combined with the use of a probability sample, the weighted data allow the estimates produced by Wave 1 of the PATH Study to be representative of the non-institutionalized, civilian U.S. population. The weighted response rate for the household screener was 54.0%. Among households that were screened, the overall weighted response rate was 74.0% for the Adult Interview. Further details regarding the PATH Study design and methods are available in Hyland et al. (2016)3 and on the PATH Study’s website (www.pathstudyinfo.nih.gov)35. Westat’s Institutional Review Board approved the study design and protocol and the Office of Management and Budget approved the data collection.
Measures
Awareness of Tobacco Products
Respondents were given a brief description and shown pictures of tobacco products (except cigarettes) and asked whether they had seen or heard of each of the following: an electronic cigarette (or e-cigarette), traditional cigars, cigarillos and filtered cigars, hookah, pipes, dissolvable tobacco, and smokeless tobacco such as snus pouches, loose snus, moist snuff, dip, spit or chewing tobacco. Only respondents who had heard of the non-cigarette product that was being measured were asked subsequent questions about perceptions of harm and use of that product.
Perceptions of Harmfulness
For each product, respondents were asked: “is smoking (insert one of the following: traditional cigars, filtered cigars, cigarillos, pipes, hookah) less harmful, about the same, or more harmful than smoking cigarettes?” Response options were “less harmful”, “about the same”, and “more harmful”. If respondents skipped this question they were given the option of saying “don’t know”. The frequency of responding “don’t know” for each product is provided in Table 1. Questions for e-cigarettes, smokeless tobacco, and dissolvables replaced “smoking” with “using”. Note that questions about use of snus pouches and smokeless tobacco were asked separately whereas perceptions of relative harm were only asked about “smokeless tobacco” generally. Based on each of the perceived harm variables, we created binary versions for less harmful (1=less harmful and 0=more/the same/don’t know) and more harmful (1=more harmful and 0=less/the same/don’t know).
Table 1.
Awareness and perceptions of the harmfulness (relative to cigarettes) of the eight non-cigarette tobacco products (n=32,320). SOURCE: PATH Study Wave 1
| Product | Aware of Product % (95% CI) | Perception of Harmfulness | Unweighted Frequency | Weighted Estimates % (95% CI) |
|---|---|---|---|---|
| E-cigarettes | 85.7 (84.9–86.3) | Less harmful | 13,728 | 40.7 (39.8–41.5) |
| About the same | 12,715 | 47.3 (46.6–48.0) | ||
| More harmful | 1,831 | 6.9 (6.4–7.3) | ||
| Don’t know | 1,051 | 5.1 (4.7–5.6) | ||
| Smokeless tobacco | 81.6 (80.9–82.3) | Less harmful | 2,573 | 8.6 (8.1–9.1) |
| About the same | 16,405 | 60.9 (60.0–61.7) | ||
| More harmful | 7,635 | 27.6 (26.8–28.4) | ||
| Don’t know | 643 | 3.0 (2.7–3.4) | ||
| Traditional cigars | 66.0 (65.2–66.9) | Less harmful | 2,438 | 12.1 (11.5–12.8) |
| About the same | 10,616 | 61.7 (60.6–62.8) | ||
| More harmful | 5,075 | 23.9 (22.8–24.9) | ||
| Don’t know | 319 | 2.3 (2.0–2.6) | ||
| Filtered cigars* | 81.6 (80.6–82.5) | Less harmful | 1,933 | 7.6 (7.2–8.0) |
| About the same | 18,536 | 75.5 (74.8–76.3) | ||
| More harmful | 4,410 | 14.5 (13.9–15.2) | ||
| Don’t know | 437 | 2.3 (2.0–2.7) | ||
| Cigarillos* | Less harmful | 1,990 | 7.1 (6.7–7.6) | |
| About the same | 16,967 | 70.7 (70.0–71.5) | ||
| More harmful | 5,908 | 19.8 (19.1–20.5) | ||
| Don’t know | 445 | 2.4 (2.1–2.7) | ||
| Pipe | 89.6 (89.0–90.2) | Less harmful | 3,250 | 10.3 (9.8–10.9) |
| About the same | 18,520 | 66.8 (66.0–67.6) | ||
| More harmful | 6,730 | 20.1 (19.5–20.8) | ||
| Don’t know | 622 | 2.8 (2.5–3.1) | ||
| Hookah | 70.3 (69.4–71.1) | Less harmful | 6,118 | 17.8 (17.1–18.6) |
| About the same | 14,423 | 61.5 (60.6–62.4) | ||
| More harmful | 4,222 | 16.7 (16.0–17.4) | ||
| Don’t know | 706 | 4.0 (3.6–4.5) | ||
| Dissolvables | 10.9 (10.5–11.4) | Less harmful | 648 | 13.5 (12.2–14.9) |
| About the same | 2,670 | 62.0 (60.0–64.0) | ||
| More harmful | 932 | 22.1 (20.2–24.1) | ||
| Don’t know | 94 | 2.4 (1.7–3.3) |
Awareness was assessed for filtered cigars and cigarillos combined.
Perceived harmfulness of cigarettes was measured by asking “how harmful do you think cigarettes are to health?”; response options (“not at all harmful,” “slightly harmful,” “somewhat harmful,” “very harmful,” and “extremely harmful”) were coded 1 = very or extremely harmful and 0 = not at all/slightly/somewhat harmful.
Current Use of Products
Former tobacco users were former established or former experimental users of cigarettes or any non-cigarette tobacco product (derived variables in the PATH Study’s Restricted Use File [RUF]).36,37 Current users of non-cigarette tobacco products were identified as those who currently used any tobacco product irrespective of how frequently they used it. Respondents who were not current or former users were classified as non-users. Nonusers had to indicate that they did not use all 10 products to be considered non-users because otherwise they may still use the product but skipped the question. Respondents who said that they used ANY of the products were classified as a user because there was sufficient information to make that classification. Of 32,320, 2.1% (689) could not be classified as a result of the classification system we used. “Never” and “low level” users were used to define the “non-user” category.
Covariates
Demographic measures included: sex, age (derived using the imputed variable in the RUF), race/ethnicity (derived using the imputed variable in the RUF), sexual orientation, educational attainment, and household income. Missing data on age, gender, race, Hispanic ethnicity were logically assigned from household screener data, as described in the PATH Study Restricted Use File User’s Guide (United States Department of Health and Human Services 2015. http://doi.org/10.3886/ICPSR36231.v2). Current tobacco use status was also a covariate (non-user “does not use any tobacco product,” “former tobacco user,” and “current tobacco user”). Respondents who had never smoked (not even once) and those who had used less than 100 cigarettes in their lifetime were classified as non-smokers. Respondents who used cigarettes everyday were classified as daily smokers and respondents who used cigarettes on some days were classified as non-daily smokers. All categories and reference groups for each variable are provided in Table 2.
Table 2.
Factors associated with the belief that each of the eight non-cigarette tobacco products is less harmful than cigarettes. ± SOURCE: PATH Study Wave 1.
| Covariate | E-cigarettes (n = 25,832) OR (95% CI) |
Smokeless Tobacco (n = 24,082) OR (95% CI) |
Traditional Cigars (n = 16,451) OR (95% CI) |
Filtered Cigars (n = 22,784) OR (95% CI) |
Cigarillos (n = 22,780) OR (95% CI) |
Pipe (n = 25,575) OR (95% CI) |
Hookah (n = 22,695) OR (95% CI) |
Dissolvables (n = 3,944) OR (95% CI) |
|---|---|---|---|---|---|---|---|---|
| Gender (vs. Female) | ||||||||
| Male | 1.32 (1.23–1.42) | 2.05 (1.77–2.37) | 2.17 (1.88–2.51) | 1.45 (1.26–1.67) | 1.80 (1.54–2.11) | 1.54 (1.36–1.74) | 1.03 (0.94–1.14) | 1.58 (1.17–2.15) |
| Age (vs. 65+) | ||||||||
| 18–24 | 2.29 (1.94–2.69) | 1.08 (0.88–1.34) | 1.14 (0.90–1.43) | 1.06 (0.84–1.33) | 1.19 (0.92–1.54) | 0.82 (0.66–1.02) | 6.69 (5.24–8.55) | * |
| 25–34 | 1.96 (1.68–2.29) | 0.82 (0.65–1.03) | 0.79 (0.62–1.01) | 0.49 (0.37–0.64) | 0.66 (0.49–0.90) | 0.55 (0.44–0.69) | 3.51 (2.77–4.45) | * |
| 34–44 | 1.73 (1.46–2.05) | 0.90 (0.72–1.13) | 0.81 (0.63–1.05) | 0.52 (0.37–0.72) | 0.71 (0.51–0.99) | 0.53 (0.42–0.68) | 1.96 (1.50–2.56) | * |
| 45–54 | 1.82 (1.55–2.13) | 1.05 (0.84–1.32) | 0.84 (0.65–1.09) | 0.76 (0.58–1.00) | 0.93 (0.69–1.24) | 0.64 (0.51–0.81) | 1.49 (1.16–1.91) | * |
| 55–64 | 1.51 (1.24–1.84) | 0.87 (0.68–1.11) | 0.86 (0.68–1.10) | 0.78 (0.61–0.99) | 0.94 (0.70–1.25) | 0.75 (0.60–0.93) | 1.16 (0.87–1.55) | * |
| Sexual orientation (vs. Straight) | ||||||||
| Bisexual | 1.20 (0.98–1.47) | 0.62 (0.40–0.95) | 1.18 (0.78–1.79) | 1.42 (0.97–2.09) | 1.58 (1.07–2.34) | 1.52 (1.11–2.08) | 1.24 (0.99–1.56) | * |
| Gay or lesbian | 1.20 (0.91–1.56) | 1.05 (0.64–1.72) | 0.93 (0.55–1.55) | 0.99 (0.62–1.57) | 1.13 (0.71–1.79) | 1.15 (0.79–1.68) | 1.25 (0.93–1.68) | * |
| Something else | 1.24 (0.87–1.76) | 1.19 (0.67–2.10) | 1.55 (0.89–2.69) | 0.98 (0.61–1.59) | 1.14 (0.65–1.99) | 1.74 (1.17–2.59) | 1.23 (0.84–1.79) | * |
| Race (vs. Non-Hispanic White) | ||||||||
| Non-Hispanic Black/African American | 0.72 (0.67–0.79) | 0.87 (0.74–1.01) | 0.82 (0.63–1.07) | 1.11 (0.90–1.38) | 1.47 (1.19–1.81) | 0.77 (0.64–0.93) | 1.07 (0.93–1.24) | 0.46 (0.33–0.64) |
| Non-Hispanic American Indian or Alaska Native | 0.54 (0.36–0.82) | * | * | * | * | * | * | * |
| Non-Hispanic Asian/Native Hawaiian/Other Pacific Islander | 0.64 (0.53–0.78) | 0.67 (0.44–1.01) | 0.87 (0.51–1.47) | 1.48 (0.95–2.32) | 1.15 (0.65–2.04) | 0.62 (0.40–0.95) | 1.17 (0.91–1.51) | * |
| Non-Hispanic of two or more races | 1.10 (0.90–1.34) | 0.84 (0.61–1.16) | 1.36 (1.00–1.86) | 1.32 (0.91–1.93) | 1.32 (0.95–1.83) | 1.26 (0.94–1.68) | 1.13 (0.94–1.34) | 0.71 (0.43–1.16) |
| Hispanic | 0.64 (0.58–0.71) | 0.65 (0.51–0.83) | 1.09 (0.88–1.34) | 0.82 (0.65–1.04) | 0.78 (0.62–0.98) | 0.69 (0.55–0.86) | 1.00 (0.88–1.15) | 0.63 (0.42–0.95) |
| Education (vs. < high school) | ||||||||
| Some high school, no diploma | 0.89 (0.71–1.12) | 0.64 (0.42–0.97) | 0.80 (0.49–1.31) | 0.85 (0.49–1.48) | 1.26 (0.81–1.97) | 0.83 (0.49–1.40) | 0.80 (0.55–1.15) | * |
| GED | 1.02 (0.81–1.29) | 0.58 (0.39–0.87) | 0.80 (0.49–1.30) | 0.66 (0.39–1.14) | 0.94 (0.59–1.50) | 0.63 (0.41–0.96) | 1.00 (0.69–1.46) | * |
| High school graduate - diploma | 1.04 (0.82–1.32) | 0.64 (0.44–0.92) | 0.98 (0.67–1.43) | 1.02 (0.66–1.57) | 1.28 (0.90–1.82) | 1.06 (0.69–1.62) | 1.14 (0.80–1.62) | * |
| Some college but no degree | 1.24 (1.00–1.55) | 0.68 (0.48–0.97) | 1.30 (0.89–1.91) | 1.16 (0.72–1.87) | 1.63 (1.11–2.39) | 1.29 (0.86–1.92) | 1.68 (1.17–2.40) | * |
| Associate degree - occupational/ vocational | 1.10 (0.83–1.46) | 0.55 (0.35–0.86) | 1.56 (1.00–2.43) | 1.09 (0.64–1.86) | 1.47 (0.93–2.34) | 1.38 (0.89–2.15) | 1.57 (1.08–2.28) | * |
| Associate degree - academic program | 1.19 (0.90–1.57) | 0.81 (0.54–1.22) | 1.60 (1.05–2.44) | 1.64 (0.97–2.76) | 1.78 (1.14–2.78) | 1.36 (0.84–2.20) | 1.79 (1.23–2.61) | * |
| Bachelor’s degree | 1.49 (1.18–1.89) | 0.73 (0.49–1.09) | 1.95 (1.37–2.78) | 1.93 (1.21–3.07) | 2.34 (1.65–3.31) | 1.89 (1.25–2.85) | 2.42 (1.69–3.48) | * |
| Master’s degree+ | 1.40 (1.10–1.78) | 0.90 (0.58–1.39) | 1.66 (1.12–2.47) | 1.61 (0.98–2.65) | 1.91 (1.29–2.82) | 1.82 (1.23–2.69) | 2.63 (1.79–3.86) | * |
| Household income (vs. < $10,000) | ||||||||
| $10,000–$14,999 | 1.00 (0.87–1.15) | 1.08 (0.82–1.43) | 1.16 (0.86–1.58) | 1.14 (0.88–1.46) | 0.95 (0.72–1.25) | 0.96 (0.76–1.21) | 1.03 (0.85–1.25) | 0.91 (0.60–1.38) |
| $15,000–$24,999 | 0.95 (0.84–1.07) | 0.83 (0.65–1.07) | 1.21 0.93–1.57) | 1.13 (0.85–1.48) | 0.96 (0.73–1.25) | 1.07 (0.86–1.34) | 0.99 (0.86–1.15) | 0.79 (0.52–1.20) |
| $25,000–$34,999 | 1.06 (0.92–1.21) | 0.98 (0.75–1.28) | 1.02 (0.75–1.38) | 0.98 (0.78–1.22) | 0.85 (0.64–1.15) | 0.85 (0.68–1.07) | 1.02 (0.85–1.23) | 0.79 (0.48–1.29) |
| $35,000–$49,999 | 0.96 (0.83–1.13) | 1.11 (0.86–1.42) | 1.17 (0.87–1.58) | 1.07 (0.83–1.38) | 1.06 (0.80–1.41) | 1.03 (0.81–1.32) | 1.11 (0.92–1.33) | 0.74 (0.47–1.17) |
| $50,000–$74,999 | 1.13 (0.97–1.30) | 0.98 (0.78–1.22) | 1.31 (1.00–1.72) | 1.18 (0.91–1.53) | 1.25 (0.93–1.67) | 0.97 (0.79–1.19) | 0.96 (0.80–1.15) | 1.14 (0.72–1.82) |
| $75,000–$99,000 | 1.05 (0.91–1.21) | 1.28 (0.99–1.66) | 1.48 (1.13–1.95) | 1.39 (1.03–1.87) | 1.36 (1.05–1.76) | 0.98 (0.79–1.21) | 1.05 (0.87–1.28) | * |
| $100,000+ | 1.23 (1.07–1.42) | 1.30 (1.04–1.64) | 1.66 (1.28–2.16) | 1.45 (1.12–1.88) | 1.47 (1.13–1.91) | 1.09 (0.87–1.36) | 1.27 (1.04–1.55) | 1.39 (0.87–2.23) |
| Current tobacco use (vs. Non-user) | ||||||||
| Former user | 1.39 (1.24–1.56) | 0.95 (0.77–1.17) | 1.88 (1.47–2.42) | 1.12 (0.90–1.38) | 1.87 (1.43–2.45) | 1.69 (1.36–2.09) | 1.67 (1.45–1.91) | 1.09 (0.66–1.78) |
| Current user | 2.43 (2.19–2.71) | 1.42 (1.19–1.68) | 2.36 (1.87–2.99) | 1.24 (1.01–1.53) | 2.64 (2.06–3.37) | 1.98 (1.63–2.40) | 2.25 (1.95–2.59) | 1.87 (1.22–2.88) |
| Knowledge of health harms (composite index) 1 point decrease | 1.09 (1.07–1.11) | 1.12 (1.10–1.15) | 1.13 (1.09–1.17) | 1.12 (1.09–1.16) | 1.10 (1.07–1.14) | 1.14 (1.10–1.17) | 1.10 (1.07–1.13) | 1.11 (1.05–1.17) |
Estimates are statistically unreliable and have been suppressed. The relative standard error was used to determine whether an estimate was statistically unreliable. The relative standard error is computed as RSE = 100x (SE of estimate/estimate) and is analogous to the coefficient of variation. Odds ratios having an RSE > 0.3 were flagged as statistically unreliable and were therefore suppressed.
Based on multivariable logistic regression analysis
Among those who were aware of the product
Consistent with existing research,38 we constructed a knowledge index examining whether the respondent believed that cigarette smoking causes: (1) stroke, (2) lung cancer, (3) heart disease, (4) blindness, (5) poor circulation, (6) bladder cancer, (7) mouth cancer, (8) lung disease, (9) lung disease in non-smokers, (10) heart attack in non-smokers, and (11) fetal harm. All respondents to the survey were asked these questions. Affirmative responses were coded as being knowledgeable of the harm (=1); the index was then created as the sum of all items and ranged from 0 to 11.
Statistical Analysis
Analyses were conducted using SAS version 9.3. Statistical methods appropriate for complex survey data were used to estimate for each non-cigarette tobacco product the percentage of U.S. adults believing that product to be less harmful than cigarettes. Variances were estimated using Balanced Repeated Replication (BRR) with a Fay adjustment factor of 0.3. Estimates were weighted to be representative of the U.S. adult population. Logit confidence limits (95% confidence intervals) were estimated for descriptive statistics only through the use of PROC SURVEYFREQ. An omnibus test for each covariate was used to determine the significance of each factor in logistic regression models using odds ratios.
Aim 1
Differences in perceptions between products were tested using multivariable logistic regression. The outcome for this analysis was the “product harmfulness” variable and all pairwise differences in the odds of each product being less (or more) harmful than cigarettes were estimated. A “step down” approach was used to test specific contrasts (shown in Figure 1) specifically by comparing the largest proportion of respondents believing that the product was less harmful to the second largest to the third, etc., which yielded seven comparisons: e-cigarette vs. hookah, hookah vs. dissolvables, dissolvables vs. traditional cigars, traditional cigars vs. pipe, pipe vs. smokeless, smokeless vs. filtered cigars, and filtered cigars vs. cigarillos. A second analysis using this model examined the belief that each product was more harmful. Models controlled for all demographic variables and overall knowledge of the harms of cigarette smoking. Tests were adjusted for multiple comparisons using a Bonferroni correction. The model here is based on a type of repeated measures analysis, where each respondent aware of one or more products was included in the analysis.
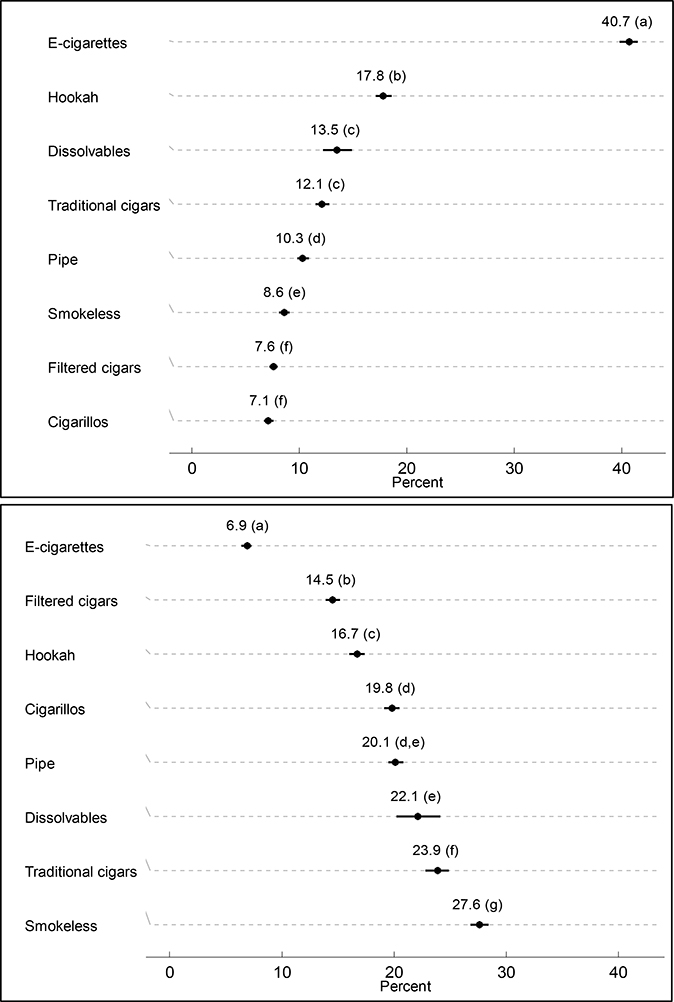
Figure 1.
A: % of Population thinking each product is less harmful than cigarettes
B: % of Population thinking each product is more harmful than cigarettes
SOURCE: PATH Wave 1
N=31,414 for statistical modelling
*Among those who had heard of the product
± Products having different letters are significantly different than the product that was ranked immediately below it in terms of perceived harmfulness. For example, 40.7% of people aware of e-cigarettes said e-cigarettes are less harmful than cigarettes while 17.8% of people aware of hookah said hookah is less harmful than cigarettes. These two percentages are significantly different (p<0.05) after controlling for multiple comparisons using a Bonferroni correction.
Aim 2
Multivariable logistic regression models were used to examine the factors associated with believing each of the non-cigarette tobacco products were “less harmful than cigarettes”; these models adjusted for demographic variables and knowledge of the health harms caused by cigarette smoking. Only those who were aware of the product were included in the model. Sample sizes for each model are shown in Table 2.
Aim 3
Multivariable logistic regression models were used to examine whether perceptions of harmfulness of a product were associated with use of that product; these models adjusted for demographic variables (excluding current tobacco use) and cigarette smoking status. Given our interest in examining whether respondents had an opinion of harm related to use, for analyses examining product use as an outcome, respondents who said “don’t know” for the harmfulness of the product were excluded. The total sample size differed according to product but ranged from 16,413 for traditional cigars to 25,536 for pipes.
Aim 4
Descriptive statistics appropriate for complex survey data were used to estimate the proportion of respondents who used each non-cigarette tobacco or cigarette product if they believed that cigarettes were not at all/slightly or somewhat harmful and if they believed that cigarettes were very/extremely harmful. Only current users of any of the non-cigarette tobacco products or cigarettes were included in this analysis (n=17,690).
RESULTS
Among current tobacco users, cigarettes were perceived as being “very” or “extremely harmful” (77.0%). Descriptive statistics of the sample are presented in Supplemental Table S1.
Table 1 presents both awareness and perception of harmfulness of each non-cigarette tobacco product among the U.S. population. Awareness was highest for pipes (89.6%) and e-cigarettes (85.7%).
Figure 1 presents the percentage of the population who believed that each product is less harmful than cigarettes (among those who had heard of that product) (Figure 1a); and more harmful than cigarettes (Figure 1b). E-cigarettes were most likely to be perceived as less harmful than cigarettes (40.7%), followed by hookah (17.8%), dissolvables (13.5%), traditional cigars (12.1%), pipes (10.3%), smokeless tobacco (8.6%), filtered cigars (7.6%), and cigarillos (7.1%) (Figure 1a). Turning to perceptions that a product was more harmful than cigarettes, smokeless tobacco was most likely to be perceived as more harmful than cigarettes, followed by traditional cigars, dissolvables, pipes, cigarillos, hookah, filtered cigars, and e-cigarettes (Figure 1b). Within Figure 1, different letters shown in parentheses indicate significant differences in harmfulness beliefs between products, as tested in the logistic regression analyses.
Table 2 presents the factors associated with the belief that each non-cigarette tobacco product is less harmful than cigarettes. The only factor associated with perceptions of harmfulness across all of the products was knowledge about the health risks of smoking. Those less knowledgeable about the health risks were significantly more likely to believe that each non-cigarette tobacco product was less harmful than cigarettes. Additionally, with the exception of hookah, male respondents were significantly more likely than female respondents to believe that each non-cigarette product was less harmful. Of note, young adults (18–24) were significantly more likely than older adults to believe that e-cigarettes and hookah were less harmful than cigarettes. Other factors associated with perceptions of the relative harmfulness of non-cigarette tobacco products varied by product type. For example, those who were younger, higher educated, have higher income levels, and current or former tobacco users were more likely to say e-cigarettes were less harmful compared to cigarettes. Black, American Indian/Alaska Native, Asian, and Hispanic ethnicities were less likely than whites to believe that e-cigarettes were less harmful than cigarettes. A different pattern of predictors was seen for other tobacco products, as illustrated in Table 2. Factors associated with perceptions that each product is more harmful than cigarettes are presented in Supplemental Table 2. Black and Hispanic respondents were significantly more likely than White respondents to believe that each of the products is more harmful than cigarettes. No other factors consistently predicted perceptions of greater harm across all non-cigarette tobacco products.
Perceptions of the harmfulness of a non-cigarette tobacco product were related to whether or not the product was used (data not shown in tables). Respondents who perceived a tobacco product as less harmful than cigarettes were more likely to use that product: e-cigarettes (OR=3.20., 95% CI 2.91–3.51), hookah (OR=3.19, 95% CI 2.82–3.60), traditional cigars (OR=3.25, 95% CI 2.84–3.73), filtered cigars (OR=2.46, 95% CI 1.88–3.21), snus pouches (OR=2.49, 95% CI 1.91–3.26), smokeless tobacco (OR=3.72, 95% CI 3.24–4.27), pipes (OR=3.66, 95% CI 2.94–4.55), and cigarillos (OR=3.37, 95% CI 2.87–3.95). Complementary to these findings, for most non-cigarette tobacco products, those who perceived it to be more harmful than cigarettes were significantly less likely to use that product: e-cigarettes (OR=0.52, 95% CI, 0.39–0.69), snus pouches (OR=0.40, 95% CI 0.28–0.56), smokeless tobacco (0.41, 95% CI 0.34–0.49), traditional cigars (OR=0.74, 95% CI 0.640.86), pipes (OR=0.62, 95% CI 0.48–0.80) and cigarillos (OR=0.72, 95% CI 0.65–0.81). There was no association for filtered cigars (OR=0.84, 95% CI 0.69–1.03) and hookah (OR=0.88, 95% CI 0.75–1.04).
Table 3 presents the prevalence of current non-cigarette use by perceptions of cigarette harmfulness. A significantly larger proportion of respondents who said that cigarettes were “very” or “extremely” harmful used hookah compared to those who said that cigarettes were “not at all,” “slightly,” or “somewhat” harmful. In contrast, smaller proportions of respondents who said that cigarettes were “very” or “extremely” harmful used: filtered cigars, cigarillos, pipes, and dissolvables. There was no significant difference in use of: e-cigarettes, snus pouches, smokeless tobacco, or traditional cigars by perceptions of the harmfulness of cigarettes.
Table 3.
Prevalence of non-cigarette use and cigarette smoking by perceptions of cigarette harmfulness± (n=17,690). SOURCE: PATH Study Wave 1
| Perceptions of Cigarette harmfulness | ||||||
|---|---|---|---|---|---|---|
| Not at all/slightly/somewhat harmful | Very/extremely harmful | Rao-Scott ChiSq Test | ||||
| Current Tobacco Product Use* | % | (95% CI) | % | (95% CI) | ChiSq | p-value |
| E-cigarettes | 19.1 | (17.8, 20.4) | 19.9 | (19.0, 20.8) | 1.08 | 0.298 |
| Snus pouches | 2.8 | (2.2, 3.4) | 2.7 | (2.3, 3.0) | 0.11 | 0.743 |
| Smokeless | 10.7 | (9.6, 12.0) | 11.1 | (10.3, 12.0) | 0.27 | 0.602 |
| Traditional cigars | 14.9 | (13.8, 16.1) | 16.2 | (15.4, 17.0) | 2.82 | 0.093 |
| Filtered cigars | 9.6 | (8.6, 10.7) | 6.4 | (5.9, 6.9) | 47.92 | <.001 |
| Cigarillos | 18.6 | (17.2, 20.0) | 14.5 | (13.8, 15.3) | 26.65 | <.001 |
| Pipe | 5.3 | (4.5, 6.2) | 3.5 | (3.2, 3.9) | 20.20 | <.001 |
| Hookah | 11.5 | (10.4, 12.7) | 15.8 | (14.9, 16.7) | 45.50 | <.001 |
| Dissolvables | 0.6 | (0.4, 0.9) | 0.2 | (0.2, 0.3) | 9.72 | 0.002 |
| Cigarettes | 88.0 | (86.8, 89.1) | 71.9 | (70.8, 72.9) | 291.05 | <.001 |
among current tobacco users who currently use one or more tobacco products.
Current users of non-cigarette tobacco products were defined on the basis of two questions: ever use and current someday use/current daily use. Respondents who had ever used the product and currently used it every day or some days were classified as current users. Current cigarette smokers were defined differently, relying on an additional restriction of established use (i.e., more than 100 cigarettes in lifetime). Current cigarette smokers were those respondents who had smoked at least 100 cigarettes in their lifetimes and who currently smoke every day or some days.
DISCUSSION
The PATH Study is the first nationally representative study examining perceptions of relative harmfulness across eight non-cigarette tobacco products. The nationally representative sample and the very large sample size of the PATH Study allowed for the possibility of sufficiently powered analyses to examine the perceptions of harmfulness of a broader range of non-cigarette tobacco products than past studies using data from adult populations.
Perceptions of the harmfulness of non-cigarette tobacco products relative to cigarettes varied widely across the eight products. About 41% of respondents who were aware of e-cigarettes believed that e-cigarettes were less harmful than cigarettes, and almost 18% of those who were aware of hookah believed that hookah smoking was less harmful than cigarette smoking. In contrast, fewer U.S. adults perceive cigars of any type, pipe tobacco, and smokeless tobacco to be less harmful than cigarettes. Consistent with other studies, only a small percentage of people believed that smokeless tobacco was less harmful than cigarettes (8.6%),24 compared to 27.6% who believed that smokeless tobacco was more harmful than cigarettes. Similarly, with the exception of filtered cigar users, being a current user of a non-cigarette tobacco product was associated with a greater likelihood of endorsing the view that the product was less harmful than cigarettes.18–21
Few factors were consistently associated with harmfulness perceptions of the various products. Previous studies have found that male respondents were significantly more likely than female respondents to believe that smokeless tobacco24,26 and e-cigarettes14 are less harmful than regular cigarettes. The current study found that males and those less knowledgeable about the health risks of smoking were more likely to believe that each of the tobacco products (except hookah for males) were less harmful than cigarettes. Therefore those who are more aware of the health risks of smoking may also be more likely to believe that other tobacco products are also harmful. Consistent with other research,15–18,29 current tobacco use was also associated with a greater likelihood of believing that each of the tobacco products was less harmful than cigarettes for most products.
The factors associated with perceptions of harmfulness were, in many instances, product-specific. For example, younger respondents were more likely to believe that e-cigarettes and hookah are less harmful than cigarettes. Consistent with previous research,15 we found that respondents with higher education levels were more likely to believe that each product (except smokeless tobacco) was less harmful than cigarettes. Consistent with research examining absolute perceptions of product harm, Black respondents were more likely to believe that cigarillos are less harmful. However, whereas Black respondents have been found to have greater absolute perceptions of the harmfulness of smokeless, cigars, roll your own, pipes and hookah but not e-cigarettes, the current study found that Black respondents are less likely to believe that e-cigarettes, pipes and dissolvables are less harmful than cigarettes. These findings point to the importance of examining both absolute and relative perceptions of harmfulness and can inform educational campaigns about the harmfulness of non-cigarette tobacco products to certain sub-populations.
For every non-cigarette tobacco product examined, a lower perception of product harmfulness, in comparison to cigarettes, was associated with a greater likelihood of using that product. However, higher perceptions of the harmfulness of cigarettes was only associated with a greater likelihood of using hookah. The PATH Study longitudinal data may allow us to examine whether product harmfulness perceptions predict future use of products and the extent to which marketing and other factors influence perceptions of harmfulness.
Limitations
In the PATH Study Adult Questionnaire, “don’t know” responses were not given as an initial response option; rather, respondents who did not respond had the option of then saying “don’t know” in a follow-up question. It is therefore unclear how strongly respondents may hold a given belief. In previous research, a high proportion of respondents indicated that they “don’t know” whether these products are less harmful.23,25,28 However, in our analyses, only those respondents who were aware of each of the products were included. The responses therefore represent the respondents’ impression of the harmfulness of the product as it compares to the harm of cigarettes. The PATH Study Wave 1 Adult questionnaire did not include measures of absolute harm but rather compared the harmfulness of non-cigarette tobacco products relative to cigarettes. Previous research suggests that the direct comparative measure used in the PATH Study would provide a more conservative measure of the harm perception associated with these products, relative to cigarettes, than if indirect measures had been used.39 Further, the comparative nature of the items included in the PATH Study used cigarettes as the referent, so it is unknown how perceptions of harmfulness may differ if the reference is different (e.g. no tobacco).40
This paper reports cross-sectional data, which precludes judgments about causal relationships. Future waves of the PATH Study may allow analyses with greater potential to discern causal direction in observed associations, to address, for example, the extent to which perceiving a product to be less harmful than cigarettes leads to a greater likelihood of trial and regular use of that product, and/or the extent to which product use leads to a greater likelihood of perceiving that product to be less harmful than cigarettes.
IMPLICATIONS
Perceptions of harmfulness varied widely across eight types of non-cigarette tobacco products. We observed an association between perceptions of product harmfulness and product use, but further longitudinal research may be useful to determine whether such perceptions are useful predictors of future product adoption. These results point to the potential value of enhancing knowledge, within the U.S. population, of the harm of tobacco products to prevent tobacco use and to encourage tobacco users to quit, through providing new information about the harms that may not be widely known and/or through countering misperceptions that may exist.
Supplementary Material
Highlights.
E-cigarettes (40.7%) were most likely to be seen as less harmful than cigarettes
Hookah (17.8%) was next most likely to be seen as less harmful than cigarettes
Belief that cigarettes are harmful associated with using hookah
Product users more likely to believe their product less harmful than cigarettes
ACKNOWLEDGEMENTS
This manuscript is supported with Federal funds from the National Institute on Drug Abuse, National Institutes of Health, and the U. S. Food and Drug Administration, Department of Health and Human Services, under a contract to Westat (Contract No. HHSN271201100027C).
The views and opinions expressed in this manuscript are those of the authors only and do not necessarily represent the views, official policy, or position of the US Department of Health and Human Services or any of its affiliated institutions or agencies. Westat’s Institutional Review Board approved the study design and protocol. The authors would like to thank Michelle Bauer and Dana Komer for their assistance with paper formatting and referencing, and Annika Green for assistance with literature reviews.
AUTHOR DISCLOSURE
K. Michael Cummings has received grant funding from Pfizer, Inc., to study the impact of hospital based tobacco cessation interventions. He also receives funding as an expert witness in litigation filed against the tobacco industry. Geoffrey Fong also receives support from a Senior Investigator Award from the Ontario Institute for Cancer Research. All other authors report no disclosures.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Geoffrey T. Fong, Department of Psychology, University of Waterloo, Waterloo, Ontario, Canada School of Public Health and Health Systems, University of Waterloo, Waterloo, Ontario, Canada; Ontario Institute for Cancer Research, Toronto, Ontario, Canada.
Tara Elton-Marshall, Institute for Mental Health Policy Research, Centre for Addiction and Mental Health, London, Ontario, Canada Dalla Lana School of Public Health, University of Toronto, Toronto, Ontario, Canada; Department of Epidemiology and Biostatistics, Schulich School of Medicine and Dentistry.
Pete Driezen, Department of Psychology, University of Waterloo, Waterloo, Ontario, Canada
Annette R. Kaufman, US Department of Health and Human Services, National Cancer Institute, National Institutes of Health, Bethesda, Maryland, USA.
K. Michael Cummings, Department of Psychiatry and Behavioral Sciences, Medical University of South Carolina, Charleston, SC, USA
Kelvin Choi, Division of Intramural Research, National Institute on Minority Health and Health Disparities, Bethesda, MD, USA.
Jonathan Kwan, Center for Tobacco Products, United States Food and Drug Administration, Silver Spring, MD, USA
Amber Koblitz, Center for Tobacco Products, United States Food and Drug Administration, Silver Spring, MD, USA.
Andrew Hyland, Department of Health Behavior, Division of Cancer Prevention and Population Sciences, Roswell Park Cancer Institute, Buffalo, NY, USA
Maansi Bansal-Travers, Department of Health Behavior, Division of Cancer Prevention and Population Sciences, Roswell Park Cancer Institute, Buffalo, NY, USA
Charles Carusi, Westat, Rockville, MD, USA
Mary E. Thompson, Department of Statistics and Actuarial Science, University of Waterloo, Waterloo, Ontario, Canada .
REFERENCES
- 1.Family Smoking Prevention and Tobacco Control Act. (Pub.L. 111–31, H.R. 1256). June 22, 2009.
- 2.FDA’s Deeming Regulations for E-Cigarettes, Cigars, and Other Tobacco Products. https://www.fda.gov/TobaccoProducts/GuidanceComplianceRegulatoryInformation/ucm394909.htm Accessed April 26, 2018.
- 3.Hyland A, Ambrose BK, Conway KP, et al. Design and methods of the Population Assessment of Tobacco and Health (PATH) Study. Tob Control. 2017. July; 26(4):371–378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bansal-Travers M, Hammond D, Smith P, et al. The impact of cigarette pack design, descriptors, and warning labels on risk perception in the U.S. Am J Prev Med. 2011;40(6):674–682. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kaufman AR, Waters EA, Parascandola M, et al. Food and Drug Administration evaluation and cigarette smoking risk perceptions. Am J Health Beh. 2011;35(6):766–76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Costello MJ, Logel C, Fong GT, et al. Perceived risk and quitting behaviors: results from the ITC 4-country survey. Am J Health Beh. 2012;36(5):681–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Pollay RW, Dewhirst T. The dark side of marketing seemingly “light” cigarettes: Successful images and failed fact. Tob Control. 2002;11(Suppl 1):i18–i31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hammond D, Parkinson C. The impact of cigarette package design on perceptions of risk. J Pub Health. 2009;31:345–353. [DOI] [PubMed] [Google Scholar]
- 9.Elton-Marshall T, Fong GT, Zanna MP, et al. Beliefs about the relative harm of “light” and “low tar” cigarettes: Findings from the International Tobacco Control (ITC) China Survey. Tob Control. 2010;19(Suppl 2):i54–i62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bansal-Travers M, O’Connor R, Fix BV, et al. What do cigarette pack colors communicate to smokers in the U.S.? Am J Prev Med. 2011;40(6):683–689. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hastrup JL, Cummings KM, Swedrock T, et al. Consumers’ knowledge and beliefs about the safety of cigarette filters. Tob Control. 2001;10(1):84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.U.S. Department of Health and Human Services, Public Health Service, National Institutes of Health, National Cancer Institute. Monograph 13: Risks associated with smoking cigarettes with low tar machine-measured yields of tar and nicotine. In: Smoking and Tobacco Control Monographs; 2001. [Google Scholar]
- 13.Choi K, Forster JL. Beliefs and experimentation with electronic cigarettes: A prospective analysis among young adults. Am J Prev Med. 2014;46(2):175–178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kaufman AR, Finney Rutten LJ, Parascandola M, et al. Food and Drug Administration tobacco regulation and product judgments. Am J Prev Med. 2015;48(4):445–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Pearson JL, Richardson A, Niaura R, et al. E-cigarette awareness, use, and harm perceptions in US adults. Am J Pub Health. 2012;102(9):1758–1766. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Aljarrah K, Ababneh ZQ, Al-Delaimy WK. Perceptions of hookah smoking harmfulness: Predictors and characteristics among current hookah users. Tob Induc Dis. 2009;5(1):16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Smith-Simone S, Maziak W, Ward KD, et al. Waterpipe tobacco smoking: Knowledge, attitudes, beliefs, and behavior in two U.S. samples. Nic Tob Res. 2008;10(2):393–398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Sutfin EL, McCoy TP, Reboussin BA, et al. Prevalence and correlates of waterpipe tobacco smoking by college students in North Carolina. Drug Alc Dep. 2011;115:131–136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Cohn A, Cobb C, Niaura R, et al. The other combustible products: Prevalence and correlates of little cigar/cigarillo use among cigarette smokers. Nic Tob Res. 2015. December;17(12):1473–81. [DOI] [PubMed] [Google Scholar]
- 20.Nyman AL, Taylor TM, Biener L. Trends in cigar smoking and perceptions of health risks among Massachusetts adults. Tob Control. 2002;11(Suppl 2):ii25–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Sterling K, Berg CJ, Thomas AN, et al. Factors associated with small cigar use among college students. Am J Health Beh. 2013;37(3):325–333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kaufman AR, Mays D, Koblitz AR, et al. Judgments, awareness, and the use of snus among adults in the United States. Nic Tob Res. 2014;16(10):1404–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kiviniemi MT, Kozlowski LT. Deficiencies in public understanding about tobacco harm reduction: results from a United States national survey. Harm Reduc J. 2015;12(1):21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.O’Connor RJ, McNeill A, Borland R, et al. Smokers’ beliefs about the relative safety of other tobacco products: findings from the ITC collaboration. Nic Tob Res. 2007;9(10):1033–42. [DOI] [PubMed] [Google Scholar]
- 25.Richardson A, Pearson J, Xiao H, et al. Prevalence, harm perceptions, and reasons for using noncombustible tobacco products among current and former smokers. Am J Pub Health. 2014;104(8):1437–1444. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Borland R, Cooper J, McNeill A, et al. Trends in beliefs about the harmfulness and use of stop-smoking medications and smokeless tobacco products among cigarettes smokers: Findings from the ITC four-country survey. Harm Reduc J. 2011;8:21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Minaker LM, Shuh A, Burkhalter RJ, et al. Hookah use prevalence, predictors, and perceptions among Canadian youth: Findings from the 2012/2013 Youth Smoking Survey. Cancer Causes Control. 2015;26:831–838. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Sutfin EL, McCoy TP, Morrell HER, et al. Electronic cigarette use by college students. Drug Alc Dep. 2013;131:214–221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Eissenberg T, Ward KD, Smith-Simone S, et al. Waterpipe tobacco smoking on a U.S. college campus: Prevalence and correlates. J Adol Health. 2009;42(5):526–529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Weinstein ND, Marcus SE, Moser RP. Smokers’ unrealistic optimism about their risk. Tob Control. 2005;14(1):55–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Berg CJ, Stratton E, Schauer GL, et al. Perceived ham, addictiveness, and social acceptability of tobacco products and marijuana among young adults: Marijuana, hookah, and electronic cigarettes win. Subst Use Misuse. 2015;50(1):79–89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Zeller M, Hatsukami D, Strategic Dialogue on Tobacco Harm Reduction Group. The Strategic Dialogue on Tobacco Harm Reduction: a vision and blueprint for action in the US. Tob Control. 2009; 18(4), 324–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Bernat JK, Ferrer RA, Margolis KA, & Blake KD US adult tobacco users’ absolute harm perceptions of traditional and alternative tobacco products, information-seeking behaviors, and (mis) beliefs about chemicals in tobacco products. Addictive Behaviors. 2017; 71, 38–45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Weaver SR, Majeed BA, Pechacek TF, Nyman AL, Gregory KR, & Eriksen MP Use of electronic nicotine delivery systems and other tobacco products among USA adults, 2014: results from a national survey. International Journal of Public Health. 2016; 61(2), 177–188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.United States Department of Health and Human Services. National Institutes of Health. National Institute on Drug Abuse, and United States Department of Health and Human Services. Food and Drug Administration. Center for Tobacco Products Population Assessment of Tobacco and Health (PATH) Study [United States] Restricted-Use Files. ICPSR36231. Ann Arbor, MI: Inter-university Consortium for Political and Social Research; [distributor], 2016-05-24 10.3886/ICPSR36231. [DOI] [Google Scholar]
- 36.Kasza K, Conway KP, Borek N, et al. Youth tobacco use in the Population Assessment of Tobacco and Health (PATH) Study: Wave 1 2013/2014 (under review).
- 37.Kasza K, Ambrose BK, Conway KP, et al. Adult tobacco use in the Population Assessment of Tobacco and Health (PATH) Study: Wave 1, 2013/2014 (under review).
- 38.Yang J, Hammond D, Driezen P, et al. Health knowledge and perception of risks among Chinese smokers and non-smokers: findings from the Wave 1 ITC China Survey. Tob Control. 2010;19:18–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Popova L, Ling PM. Perceptions of relative risk of snus and cigarettes among US smokers. Am J Pub Health. 2013;103(11):e21–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Kaufman A, Klein W, Suls J. Communicating tobacco product harm: Compared to what? Addict Behav. 2016. June;52:123–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.