Abstract
Objectives:
To examine: (1) How perceptions of harm for seven non-cigarette tobacco products predict subsequent use; (2) How change in use is associated with changes in perceptions of product harm; (3) Whether sociodemographic variables moderate the association between perceptions and use.
Methods:
Data are from the adult sample (18+) of the Population Assessment of Tobacco and Health (PATH) Study, a nationally representative longitudinal cohort survey conducted September 2013-December 2014 (Wave 1 (W1) n=32,320) and October 2014-October 2015 (Wave 2 (W2) n=28,362).
Results:
Wave 1 users and non-users of e-cigarettes, filtered cigars, cigarillos, and pipes, who perceived these products as less harmful had greater odds of using the product at W2. For the other products, there was an interaction between W1 perceived harm and W1 use status in predicting W2 product use. At W2, a smaller percentage of U.S. adults rated e-cigarettes as less harmful than cigarettes compared to W1 (41.2% W1, 29.0% W2). Believing non-cigarette products to be less harmful than cigarettes was more strongly associated with subsequent product use in the oldest age group (55+ years) while weaker effects were observed in the youngest age group (18–24 years). This moderating effect of age was significant for e-cigarettes, hookah, traditional cigars, and cigarillos.
Conclusions:
Strategies to prevent initiation and promote cessation of these products may benefit from understanding and addressing perceptions of these products.
Keywords: Harm perceptions, tobacco products, e-cigarettes
INTRODUCTION
Different tobacco products can present qualitatively and quantitatively different risks to the user, even within a product class (classes include, but are not limited to: cigarettes, e-cigarettes, cigars, cigarillos, hookah, pipes or smokeless tobacco). However, scientific and public health organizations are frequently making broad distinctions between product classes in terms of their overall health risks [1–3]. For example, the 2018 Report of the U.S. National Academies of Sciences, Engineering, and Medicine (NASEM) concludes that “there is conclusive evidence that completely substituting e-cigarettes for combusted cigarettes reduces one’s exposure to toxicants and carcinogens and substantial evidence that complete switching reduces short-term adverse health outcomes” [4]. Given that the burning of combusted products generates a wider range and higher levels of toxicants compared to non-combusted products, combustible products are recognized as generally more harmful than non-combustible ones to long-term users of each product type [5], although this may not apply to all specific products and disease endpoints.
Tobacco product consumers’ beliefs about product risk often do not align with scientific bodies’ conclusion that combustible products generally tend to be more harmful than non-combustible ones to long-term users of each product type [5–7]. In one recent nationally representative sample of United States (U.S.) adults, fewer than half (40.7%) believed that e-cigarettes were less harmful than cigarettes, and hookah was the next most likely product to be perceived as less harmful than cigarettes (17.8% of respondents). In contrast, smokeless tobacco was most likely to be perceived as more harmful than cigarettes (27.6%) [7].
Perceptions of product harm have been associated with product use, as users of tobacco products report lower perceptions of product harm than non-users [7]. The same study also demonstrated an association between lowered perceptions of harm of eight tobacco products (e-cigarettes, hookah, traditional cigars, filtered cigars, snus, smokeless tobacco, pipes, and cigarillos), and increased likelihood of using the product [7]. A limitation of much of the existing nationally representative research conducted in the U.S. is that it relies on cross-sectional data. Of the few longitudinal studies that have been conducted to date, a U.S. longitudinal cohort survey of young adults (aged 18–24) also demonstrated that perceptions of the relative harm of hookah were associated with hookah initiation 6 months later [8]. Two U.S. nationally representative longitudinal cohort studies of adolescents have found that perceptions of lower harm of tobacco products relative to cigarettes at baseline are associated with greater likelihood of product use at follow-up [9,10]. Additionally, a study of U.S. adult dual users of cigarettes and e-cigarettes found that perceiving e-cigarettes as less harmful than cigarettes predicted completely switching to e-cigarettes one year later [11]. No studies to date have examined how perceptions of the relative harm of a variety of tobacco products relate to subsequent product use in a nationally representative U.S. longitudinal cohort sample of adults. Previous research has also demonstrated significant variability in perceptions of the harm of non-cigarette tobacco products by socio-demographic groups [7], raising the possibility that harm perceptions among sub-populations may in part explain differences in patterns of use.
Because perceptions of product harm are shown to be associated with subsequent product use, it is important to monitor harm perceptions of product consumers as these often help to explain changing patterns of tobacco use. Recent changes in the prevalence of e-cigarette and hookah use [12–15] may be driven in part by changing beliefs about product harm [16,17]. Tracking product harm perceptions is therefore important to the Food and Drug Administration’s (FDA) efforts to regulate tobacco products and their marketing.
Using nationally representative, longitudinal data from the Population Assessment of Tobacco and Health (PATH) Study, this paper addresses gaps in the existing literature to achieve the following specific aims across all US adults: (1) to examine how Wave 1 perceptions of harm for 7 non-cigarette tobacco products (e-cigarettes, traditional cigars, cigarillos, filtered cigars, hookah, pipes, and smokeless tobacco), relative to cigarettes, predict product use at Wave 2 (in terms of initiation, cessation, continued use/non-use); (2) to examine how tobacco product use (initiation, cessation, continued use/non-use) between Waves 1 and 2 is associated with changes in perceptions of tobacco product harm; and (3) to examine whether sociodemographic variables (e.g., gender, age, sexual orientation, socioeconomic status, race/ethnicity) moderate the association between harm perceptions and subsequent product use.
METHODS
The PATH Study is an ongoing, nationally representative, longitudinal cohort study of adults and youth in the U.S. The PATH Study uses audio computer-assisted self-interviews (ACASI), available in English and Spanish, to collect self-reported information on tobacco-use patterns and associated health behaviors. Wave 1 data collection was conducted from September 12, 2013 to December 14, 2014; Wave 2 was conducted from October 23, 2014 to October 30, 2015. Wave 2 interviews were conducted as close as possible to the 1-year anniversary of each respondent’s wave 1 interview. The PATH Study recruitment employed a stratified address-based, area-probability sampling design at Wave 1 that oversampled adult tobacco users, young adults (18 to 24 years), and African-American adults. An in-person screener was used at Wave 1 to select youths and adults from households for participation.
Population and replicate weights were created that adjusted for the complex study design characteristics (e.g., oversampling at Wave 1), and for nonresponse at Waves 1 and 2. Combined with the use of a probability sample, the weights allow analyses of the PATH Study data to compute estimates that are representative of the non-institutionalized, civilian U.S. population ages 12 years and older. The analyses were conducted using the Restricted Use Data File (RUF). Further details regarding the PATH Study design and methods are published elsewhere [18]. Details on survey interview procedures, questionnaires, sampling, weighting, and information on accessing the data are available at http://doi.org/10.3886/Series606. The study was conducted by Westat and approved by the Westat institutional review board. All participants (18 and older) provided informed consent.
At Wave 1, the weighted response rate for the household screener was 54.0%. Among households that were screened, the overall weighted response rate at Wave 1 was 74.0% for the Adult Interview. At Wave 2, the overall weighted response rate was 83.2% for the Adult Interview.
At Wave 1, interviews were completed with 32,320 adults (ages 18 years and older). Data for this analysis were based on 26,446 adults (age 18 or older at Wave 1) who responded to the Adult Interview at Wave 1 and Wave 2. The differences in number of completed interviews between Wave 1 and Wave 2 reflect attrition due to non-response, mortality, and other factors. Adolescents at Wave 1 who were adults at Wave 2 (n=1,915) were not included in the analyses because questions about the perceived harm of each tobacco product differed in the Youth Interview.
Measures
Awareness of Tobacco Products
At Wave 1, respondents were presented a brief description and shown pictures of tobacco products (except cigarettes) and asked whether they had seen or heard of each of the following: e-cigarettes, traditional cigars, cigarillos and filtered cigars, hookah, pipes, and smokeless tobacco (such as snus pouches, loose snus, moist snuff, dip, spit or chewing tobacco). Only respondents who had heard of each non-cigarette product were asked subsequent questions about perceptions of harm and use of that product. At Wave 2, it was assumed that all respondents had heard of all products given that they had been asked questions about them at Wave 1.
Perceptions of Harm
For each product, respondents were asked if smoking/using the product is “less harmful, about the same, or more harmful than smoking cigarettes?” Follow-up responses of “don’t know” were only available when respondents skipped the initial question. Questions for e-cigarettes and smokeless tobacco (including snus pouches) replaced “smoking” with “using.” Consistent with previous research [7], for each of the two perceived harm variables, we created binary variables for less harmful (1=less harmful and 0=more/the same/don’t know) and more harmful (1=more harmful and 0=less/the same/don’t know). To examine changes in perceptions of tobacco product harm over time, we compared Wave 1 and Wave 2 perceptions of the harm of each product. Perceptions were coded as “decreased perception of harm” if respondents indicated that the product was “more harmful” at Wave 1 and “about the same or “less harmful” at Wave 2 or if respondents indicated that the product was “about the same” at Wave 1 and “less harmful” at Wave 2. Perceptions were coded as “increased perception of harm” if respondents indicated that the product was “less harmful” at Wave 1 and “about the same” or “more harmful” at Wave 2 or if the respondents indicated that the product was “about the same” at Wave 1 and “more harmful” at Wave 2. Perceptions were coded as “no change” if respondents indicated the same response at both Wave 1 and Wave 2.
Non-Cigarette Tobacco Product Use
Consistent with previous research, current users of non-cigarette tobacco products were identified as those who currently used the specific tobacco product “every day” or “some days” [4]. Respondents who were not current product users (including never and formers users) were classified as non-users. Changes in product use categories were constructed according to the following four groups: non-users at Wave 1 who remained non-users at Wave 2, non-users at Wave 1 who became current users at Wave 2, current users at Wave 1 who became non-users at Wave 2, and current users at Wave 1 who remained current users at Wave 2.
Covariates
Demographic measures were from Wave 1 assessment and included gender, age (derived using the imputed variable in the Restricted Use File (RUF)1), race/ethnicity (derived using the imputed variable in the RUF), sexual orientation, educational attainment, and household income. Cigarette smoking status at Wave 1 was also a covariate. Respondents who smoked ≥ 100 cigarettes in their lifetime and currently smoke every day or some days were coded as “current established cigarette smokers”; respondents who were never smokers, who had smoked <100 cigarettes, or who currently did not smoke at all were coded as non-current cigarette smokers.
Statistical Analysis
Analyses were conducted using SUDAAN 11.0.1. Statistical methods appropriate for complex survey data were used to estimate for each non-cigarette tobacco product the percentage of U.S. adults believing that product to be less harmful than cigarettes. Variances were estimated using Balanced Repeated Replication (BRR) with a Fay adjustment factor of 0.3 [19,20]. Estimates were weighted to be representative of the U.S. adult population. Logit confidence limits (95% confidence intervals) were estimated for descriptive statistics. An omnibus test for each covariate was used to determine the significance of each factor in logistic regression models and relationships described using odds ratios.
To examine how baseline perceptions of harm were associated with subsequent Wave 2 use among Wave 1 users and non-users, we estimated separate logistic regression models (one for each product) using Wave 1 perceptions of harm as the primary explanatory variable, along with Wave 1 use of that product. The interaction between Wave 1 perceptions and product use was also tested, using Wald F tests, to determine whether product use modified the relationship between Wave 1 perceptions of harm and product use at Wave 2. All models controlled for demographic covariates and cigarette smoking status (current established cigarette smoker vs. non-current cigarette smoker), measured at Wave 1.
Overall frequencies of the perception that each product was less harmful than cigarettes were calculated and included the response “don’t know” and at Wave 1 “hadn’t heard of the product”. However, respondents who indicated “don’t know” at either wave or “hadn’t heard of the product” at Wave 1 were excluded from the statistical models looking at changes in perceptions of harm given that we were unable to quantify the direction of change (the percentages of “don’t know” by product are provided in Figure 1). Multinomial logistic regression was used to estimate how perceptions of harm changed over time (decreased, increased or stayed the same). These models estimated whether changes in product use, entered as the interaction between Wave 1 and Wave 2 use, were associated with a change in harm perceptions. One model was estimated for each product and marginal estimates of the proportion of the population changing their perceptions were estimated controlling for demographic covariates and cigarette smoking status. Thus, these models were used to estimate, for example, how perceptions changed among non-users of a given product who remained non-users of that product, vs. how perceptions changed among non-users who started using that product. Similarly, changes in perceptions were estimated for users who remained users and users who stopped using a particular product. Changes in perceptions (marginal differences in prevalence rates) were tested using a t-test for respondents who had change in use (or no use) of a product, compared with respondents who had no change in use (or no use) of that product from Wave 1 to Wave 2; p-values were adjusted for multiple comparisons using a Bonferroni correction.
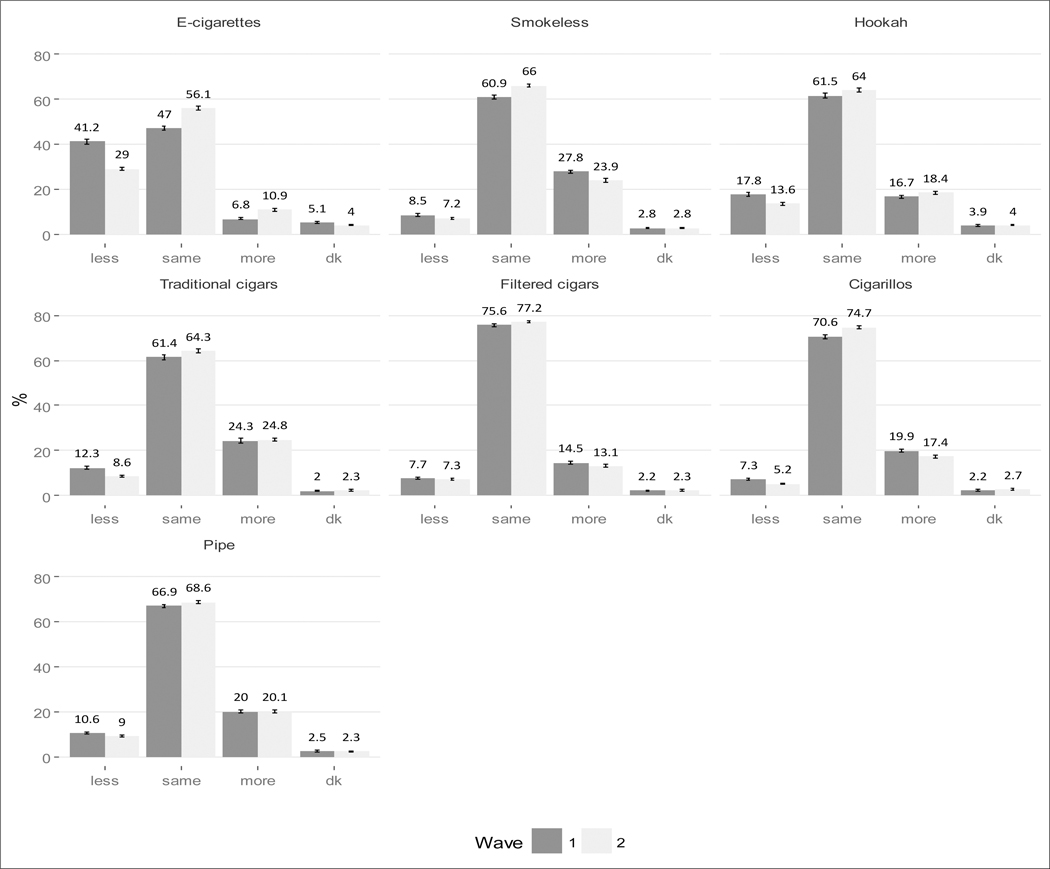
Figure 1.
Perceptions of the harm of using non-cigarette tobacco products among adults at Waves 1 and 2 of the PATH Study (Weighted).
Finally, we conducted logistic regression analysis to test whether sociodemographic factors (i.e., gender, age, race/ethnicity, sexual orientation, education, and income) modified the relationship between harm perceptions of each product at Wave 1 and subsequent use of that product in Wave 2. Separate models were estimated to test the interaction of each demographic covariate with baseline perceptions of harm for each product, and each of these models controlled for all other demographic covariates, baseline cigarette smoking status and baseline use of each product. F-tests were used to test the significance of the overall interaction. Denominator degrees of freedom for all tests was 100. For filtered cigars, the “Asian” category was collapsed with the “other” category. For cigarillos, “something else” was collapsed with the “lesbian/gay/bisexual” category due to low sample sizes to allow the model to be reliably estimated.
RESULTS
Overall frequencies of the perceptions of the relative harm of non-cigarette tobacco products at Wave 1 and Wave 2 are presented in Figure 1. The greatest overall change in perceptions was for e-cigarettes: the perception that e-cigarettes are less harmful than cigarettes declined from 41.2% to 29.0%. There were few other changes in perceptions, at the aggregate level: there was a decline in the perception that hookah is less harmful than cigarettes (17.8% to 13.6%) and a decline that traditional cigars are less harmful than cigarettes (12.3% to 8.6%). There was also an increase at each wave in the perception that the harm of each product is “the same” as cigarettes (Figure 1).
Perceptions of relative harm of products and subsequent product use
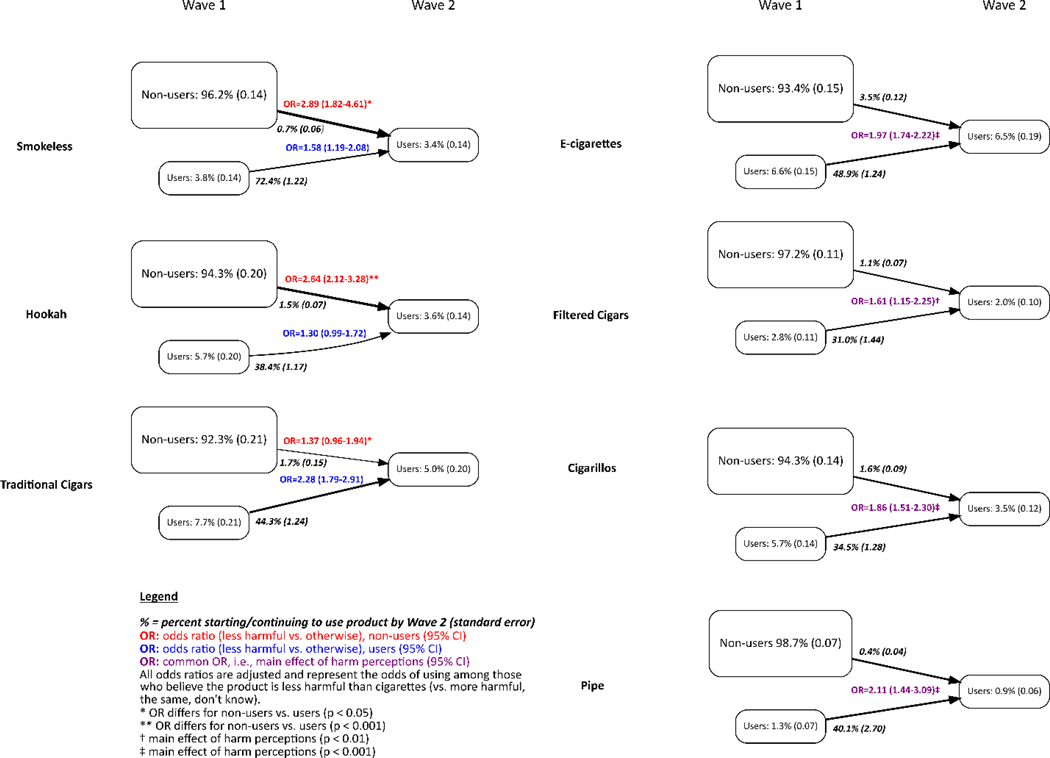
Figure 2 summarizes results showing the relationship between Wave 1 perceptions of product harm compared to cigarettes and subsequent use of that product assessed at Wave 2.
Figure 2.
Wave 1 perceptions of product harm (compared to cigarettes) predicting Wave 2 use of non-cigarette tobacco products in the PATH Study.
For example, 6.6% of respondents were e-cigarette users at Wave 1 and 93.4% were non-users. At Wave 2, 6.5% were e-cigarette users. Among non-users at Wave 1, 3.5% became users by Wave 2 whereas 48.9% of e-cigarette users at Wave 1 remained users at Wave 2. Perceptions that a product was less harmful at Wave 1 was associated with an increased likelihood of using the product at Wave 2, although differences were not always statistically significant. Among both Wave 1 users and non-users of e-cigarettes (OR=1.97, 95% CI 1.74–2.22), filtered cigars (OR=1.61, 95% CI 1.15–2.25), cigarillos (OR=1.86, 95% CI 1.51–2.30), or pipes (OR=2.11, 95% CI 1.44–3.09), respondents who perceived these products as less harmful at Wave 1 had greater odds of using the product at Wave 2. There was no significant interaction between Wave 1 use and perceptions of harm predicting Wave 2 use for these four tobacco products.
There was a significant interaction between product use at Wave 1 and the perceptions of harm predicting subsequent use at Wave 2 for three tobacco products (smokeless, hookah, and traditional cigars). For example, among hookah non-users at Wave 1, respondents who perceived that hookah was less harmful than cigarettes were significantly more likely to use hookah (OR=2.64, 95% CI 2.12–3.28) at Wave 2, compared with those perceiving the product as more harmful, about the same, or didn’t know. This association between Wave 1 harm perception predicting Wave 2 use was non-significant (OR=1.30, 95% CI 0.99–1.72) among Wave 1 hookah users (Figure 2). The association between harm perceptions and Wave 2 product use was stronger among non-users at Wave 1 for both smokeless tobacco (F-test=4.67, p=0.03) and hookah (F-test=15.57, p<0.001). In contrast, the association between harm perceptions and Wave 2 product use was stronger among Wave 1 traditional cigar users (F-test=5.89, p=0.02).
Changes in Perceptions of Product Harm by Use Wave 1-Wave 2
Table 1 summarizes results examining changes in perceptions of product harm between Wave 1 and Wave 2 by respondent product use. Across all products and all user categories, the majority of respondents did not change their perceptions of the harm of each of the tobacco products over time. There was a significant interaction between Wave 1 and Wave 2 product use category associated with changes in perceptions of the relative harm of e-cigarettes and hookah, but no other interaction effects were significant.
Table 1.
Changes in perceptions of the harmfulness of non-cigarette tobacco products by wave 1-wave 2 product use
| Change in Perceptions | ||||
|---|---|---|---|---|
| Decreased | Increased | No Change | ||
| NCTP Product | NCTP | %*(SE) | %*(SE) | %*(SE) |
| E-cigarettes (n = 20,628) | Non-user→Non- | 11.3 (0.31) (a) | 24.8 (0.48) (b) | 64.0 (0.46) |
| Non-user→User | 21.9 (1.42) (a) | 13.5 (1.14) (b) | 64.6 (1.84) | |
| User→Non-user | 7.0 (0.73) | 33.3 (1.48) (c) | 59.7 (1.59) (d) | |
| User→User | 6.5 (0.70) | 15.2 (1.09) (c) | 78.3 (1.25) (d) | |
| Smokeless (n = 19,484) | Non-user→Non- | 18.4 (0.41) | 15.1 (0.39) | 66.6 (0.52) |
| Non-user→User | 23.2 (3.86) | 12.8 (3.40) | 64.0 (4.51) | |
| User→Non-user | 12.5 (1.83) | 24.1 (2.47) | 63.3 (2.97) | |
| User→User | 12.1 (1.17) | 17.2 (1.32) | 70.6 (1.34) | |
| Hookah (n = 18,393) | Non-user→Non- | 16.6 (0.41) | 15.2 (0.36) | 68.2 (0.53) (e) |
| Non-user→User | 22.3 (2.21) | 17.8 (2.05) | 59.9 (2.73) (e) | |
| User→Non-user | 9.8 (0.98) (f) | 22.2 (1.45) | 68.0 (1.68) | |
| User→User | 14.2 (1.27) (f) | 19.0 (1.59) | 66.8 (1.77) | |
| Cigars (n = 13,565) | Non-user→Non- | 14.8 (0.46) | 15.4 (0.49) | 69.8 (0.64) |
| Non-user→User | 20.2 (3.74) | 13.7 (2.82) | 66.1 (4.28) | |
| User→Non-user | 13.8 (1.26) | 16.0 (1.32) | 70.2 (1.65) | |
| User→User | 13.7 (1.19) | 14.6 (1.44) | 71.7 (1.77) | |
| Filtered cigars (n = 18,566) | Non-user→Non- | 13.3 (0.37) | 11.8 (0.36) | 74.9 (0.47) |
| Non-user→User | 14.9 (2.35) | 10.6 (1.57) | 74.5(2.34) | |
| User→Non-user | 10.5 (1.46) | 17.5 (1.86) | 71.9 (1.84) | |
| User→User | 12.5 (1.80) | 12.2 (1.97) | 75.3 (2.58) | |
| Cigarillos (n = 18,194) | Non-user→Non- | 14.0 (0.37) | 12.3 (0.36) | 73.7 (0.42) |
| Non-user→User | 18.2 (2.31) | 9.8 (1.25) | 72.0 (2.31) | |
| User→Non-user | 12.1 (1.00) | 18.3 (1.26) | 69.6 (1.44) | |
| User→User | 11.5 (1.36) | 16.9 (1.66) | 71.6 (2.11) | |
| Pipe (n = 20,941) | Non-user→Non- | 14.7 (0.36) | 14.7 (0.35) | 70.6 (0.44) |
| Non-user→User | 16.5 (3.50) | 12.1 (3.85) | 71.4 (4.60) | |
| User→Non-user | 10.2 (1.75) | 21.3 (2.69) | 68.6 (2.99) | |
| User→User | 18.0 (2.90) | 16.9 (2.95) | 65.1 (3.30) | |
Adjusted for: Gender, age group, race/ethnicity, sexual orientation, education, income and smoking status.
Significant differences between groups are noted by:
higher percentage of decreased risk perceptions among e-cigarette non-users at Wave 1 who become users vs. stay non-users at Wave 2 (p<0.001)
higher percentage of increased risk perceptions among e-cigarette non-users at Wave 1 who stayed non-users vs. became users at Wave 2 (p<0.001)
higher percentage of increased risk perceptions among e-cigarette users at Wave 1 who become non-users vs. stay users at Wave 2 (p<0.001)
higher percentage of no change in risk perceptions among e-cigarette users at Wave 1 who stayed users at Wave 2 vs. became non-users at Wave 2 (p<0.001)
higher percentage of no change in risk perceptions among hookah non-users at Wave 1 who stayed non-users at Wave 2 vs. became users at Wave 2 (p=0.03)
higher precentage of increases in risk perceptions among hookah users at Wave 1 who stayed users at Wave 2 vs. became non-users at Wave 2 (p=0.03).
A significantly higher percentage of respondents who started using e-cigarettes between Wave 1 and Wave 2 had decreased perceptions of harm compared to those who remained non-users of e-cigarettes between surveys (21.9% vs. 11.3%, respectively). In contrast, a significantly greater percentage of non-users of e-cigarettes at Wave 1 who remained non-users at Wave 2 had increased perceptions of harm, compared to non-users at Wave 1 who started using e-cigarettes at Wave 2 (24.8% vs. 13.5%, respectively). In addition, 33.3% of users at Wave 1 who were not currently using e-cigarettes at Wave 2 had increased perceptions of harm compared to only 15.2% of users who were currently using e-cigarettes at both waves. A significantly higher percentage of users who remained users at Wave 2 (78.3%) had no change in perceptions of the harm of e-cigarettes compared to users at Wave 1 who became non-users at Wave 2 (59.7%).
Perceptions of the harm of hookah decreased among a significantly higher percentage of hookah users who remained hookah users (14.2%) compared to hookah users who stopped using hookah (9.8%). A significantly higher proportion of non-users who remained non-users (68.2%) had no change in perceptions of the harm of hookah relative to non-users who became users (59.9%).
Interaction between Sociodemographic Groups and Perceptions of Harm on Subsequent Use
Supplemental Table 2 presents results from logistic regression models examining whether sociodemographic factors modified the relationship between perceptions of harm and subsequent use of each of the non-cigarette tobacco products. In general, sociodemographic factors did not consistently modify the relationship between harm perceptions and subsequent product use. The exception was age; generally, believing non-cigarette products to be less harmful than cigarettes was more strongly associated with subsequent product use in the oldest age group (55+ years) while weaker effects were observed in the youngest age group (18–24 years). This moderating effect of age was significant for e-cigarettes, hookah, traditional cigars, and cigarillos.
DISCUSSION
This was the first nationally representative longitudinal cohort study to date to examine the association between perceptions of the relative harm of seven tobacco products compared to cigarettes and subsequent use among U.S. adults. The study demonstrates that harm perceptions not only predict future product uptake in non-product users, but also predict continued product use among existing users. This study also confirms that tobacco product users often have beliefs about the relative health risks of different tobacco products [5,6] that are inconsistent with the conclusions of authoritative sources that combustible tobacco products are generally more harmful than non-combustible ones to long-term users of each product type [1–3, 21]. For example, a greater percentage of respondents believed that smokeless tobacco products were more harmful than cigarettes (Wave 1: 27.8%; Wave 2: 23.9%) than believed that cigarettes were more harmful (Wave 1: 8.5%; Wave 2: 7.2%). As another example, at Wave 2, 10.9% of Americans believed that e-cigarettes were more harmful than cigarettes. Many users of non-cigarette tobacco products such as a smokeless tobacco also smoke cigarettes, and this may be attributable to their perception that cigarettes are no worse than other products [22].
Consistent with recent evidence [17], we found a substantial decrease in the proportion of the population perceiving that e-cigarettes are less harmful than cigarettes between Waves 1 and 2 (from 41.2% to 29.0%). These findings underscore the importance of better understanding the factors that help to shape tobacco product consumer perceptions of relative product harm such as product marketing, government-mandated warnings about product risks (i.e., content of product warnings), media coverage of product risks, and public health campaigns [23–25]. We also found that in each year the percentage of respondents indicating that they believed that each product was just as harmful as cigarettes increased, suggesting that there are increasing perceptions that all products are harmful.
Across all products (except for pipes), the prevalence of having decreased product harm perceptions was highest in those moving from non-use to use, and the prevalence of increased harm perceptions was highest among those who stopped using a product. This finding is consistent with a cognitive dissonance process in which users of tobacco products may reduce cognitive dissonance by changing their beliefs to rationalize their behavior [26]. In this case, non-cigarette tobacco users were more likely to reduce cognitive dissonance by lowering their perceptions of the harm of the tobacco product, whereas those who stop using a product would change their perceptions of harm to be more in line with the perceptions held by non-users, because they no longer need to rationalize their behaviour. Given that harm perceptions are important predictors of product use, if users tend to lower their harm perceptions this would increase their likelihood of continuing to use.
Limitations
The study uses self-reporting of perceptions of tobacco product harm and use. Therefore, the study is subject to limitations inherent to any study using self-report data such as reporting bias, although studies examining bias in self-reporting of tobacco use have not found evidence of bias [27,28]. As previously noted [4], the PATH Study uses a direct comparative measure of product harm relative to cigarettes which would likely provide a more conservative measure of the harm perception (fewer respondents reporting these products are less harmful), relative to cigarettes, than if indirect measures had been used [29–31]. Additionally, a study comparing direct and indirect measures found that direct measures may be more valid [32].
Conclusions
This study demonstrates the importance of perceptions of the harm of non-cigarette tobacco products in predicting tobacco product use. Strategies to promote tobacco product abstinence, cessation, or product switching may benefit from understanding and addressing perceptions of these products.
Supplementary Material
Highlights.
This study demonstrates the importance of perceptions of the harm of non-cigarette tobacco products in predicting tobacco product use.
Harm perceptions not only predict future product uptake in non-product users, but also predict continued product use among existing users
Strategies to promote tobacco product abstinence, cessation, or product switching may benefit from understanding and addressing perceptions of these products.
Acknowledgements
Dr. Elton-Marshall acknowledges funding from Canadian Institutes of Health Research (CIHR) for the Ontario CRISM Node Team (grant #SMN-139150). Dr. Fong has a Senior Investigator Award from the Ontario Institute for Cancer Research. Dr. Wackowski has received grant funding from the National Cancer Institute on the topic of tobacco product relative harm perceptions and communication. These funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Statement 3: Conflict of Interest
K. Michael Cummings has received grant funding from the Pfizer, Inc., to study the impact of a hospital based tobacco cessation intervention. K. Michael Cummings also receives funding as an expert witness in litigation filed against the tobacco industry. Geoffrey T. Fong has served as an expert for governments whose tobacco control policies have been challenged in litigation. All other co-authors indicate that they have no conflict of interest to declare.
Role of Funding Sources
This manuscript is supported with Federal funds from the National Institute on Drug Abuse, National Institutes of Health, and the Center for Tobacco Products, Food and Drug Administration, Department of Health and Human Services, under a contract to Westat (Contract No. HHSN271201100027C). The views and opinions expressed in this manuscript are those of the authors only and do not necessarily represent the views, official policy or position of the U.S. Department of Health and Human Services or any of its affiliated institutions or agencies.
Footnotes
Disclaimer: The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the U.S. Department of Health and Human Services or any of its affiliated institutions or agencies
Missing data on age, gender, race, Hispanic ethnicity, and adult education were imputed as described in the PATH Study Restricted Use File User’s Guide (United States Department of Health and Human Services 2015. http://www.icpsr.umich.edu/icpsrweb/NAHDAP/series/00606)
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
REFERENCES
- [1].Drope J, Cahn Z, Kennedy R, et al. Key issues surrounding the health impacts of electronic nicotine delivery systems (ENDS) and other sources of nicotine. CA Cancer J Clin. 2017;67:449–471. [DOI] [PubMed] [Google Scholar]
- [2].U.S. Department of Health and Human Services. E-Cigarette Use Among Youth and Young Adults: A Report of the Surgeon General—Executive Summary. Atlanta, GA: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health; 2016. [Google Scholar]
- [3].Royal College of Physicians. Nicotine without smoke: Tobacco harm reduction. London: RCP; 2016. [Google Scholar]
- [4].National Academies of Sciences, Engineering, and Medicine. Public Health Consequences of E-Cigarettes. Washington, DC: The National Academies Press; 2018. [PubMed] [Google Scholar]
- [5].Kiviniemi MT, Kozlowski LT. Deficiencies in public understanding about tobacco harm reduction: results from a United States national survey. Harm Reduc J. 2015;12(1):21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].O’Connor RJ, McNeill A, Borland R, et al. Smokers’ beliefs about the relative safety of other tobacco products: findings from the ITC collaboration. Nic Tob Res. 2007;9(10):1033–42. [DOI] [PubMed] [Google Scholar]
- [7].Fong GT, Elton-Marshall T, Driezen P, et al. Public perceptions about tobacco product harm: descriptive findings from the PATH study adult questionnaire. Addict Behav. 2019;91:180–87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Villanti AC, Cobb CO, Cohn AM, Williams VF, Rath JM. Correlates of hookah use and predictors of trial in U.S. young adults. Am J Prev Med. 2015;48(6):742–46. [DOI] [PubMed] [Google Scholar]
- [9].Parker MA, Villanti AC, Quisenberry AJ, Stanton CA, Doogan NJ, Redner R, Gaalema DE, Kurti AN, Nighbor T, Roberts ME, Cepeda-Benito A, Higgins ST. Tobacco product harm perceptions and new use. Pediatrics. 2018; 142(6): e20181505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Strong DR, Leas E, Elton-Marshall T, Wackowski OA, Travers M, Bansal-Travers M, Hyland A, White M, Noble M, Cummings KM, Taylor K, Kaufman AR, Choi K, Pierce JP. Harm perceptions and tobacco use initiation among youth in Wave 1 and 2 of the Population Assessment of Tobacco and Health (PATH) Study. Prev Med. 2019; 123:185–191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Persoskie A, O’Brien EK, Poonai K. Perceived relative harm of using e-cigarettes predicts future product switching among US adult cigarette and e-cigarette dual users. Addiction. doi: 10.1111/add.14730. [DOI] [PubMed] [Google Scholar]
- [12].Arrazola RA, Singh T, Corey CG, et al. Tobacco use among middle and high school students-United States, 2011–2014. MMWR. 2015;64(14):381–5. [PMC free article] [PubMed] [Google Scholar]
- [13].Dockrell M, Morrison R, Bauld L, McNeill A. E-cigarettes: Prevalence and attitudes in Great Britain. Nicotine Tob Res. 2013;15(10):1737–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].King BA, Alam S, Promoff G, Arrazola R, Dube SR. Awareness and ever-use of electronic cigarettes among US adults, 2010–2011. Nicotine Tob Res. 2013;15(9):1623–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Centers for Disease Control and Prevention. Notes from the field: electronic cigarette use among middle and high school students-United States, 2011–2012. MMWR. 2013;62(35):729. [PMC free article] [PubMed] [Google Scholar]
- [16].Majeed BA, Weaver SR, Gregory KR, et al. Changing perceptions of harm of e-cigarettes among US adults, 2012–2015. Am J Prev Med. 2017;52(3):331–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17].Tan AS, Bigman CA. E-cigarette awareness and perceived harm: prevalence and associations with smoking-cessation outcomes. Am J Prev Med. 2014;47(2):141–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18].Hyland A, Ambrose BK, Conway KP, et al. Design and methods of the Population Assessment of Tobacco and Health (PATH) Study. Tob Control. 2017;26(4):373–378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [19].McCarthy PJ. Pseudoreplication: further evaluation and applications of the balanced half-sample technique. Vital Health Stat 2. 1969;2:1–24. [PubMed] [Google Scholar]
- [20].Judkins DR. Fay’s method for variance estimation. J Offic Stat. 1990;6:223–39. [Google Scholar]
- [21].FDA. FDA’s Deeming Regulations for E-Cigarettes, Cigars, and Other Tobacco Products. https://www.fda.gov/TobaccoProducts/GuidanceComplianceRegulatoryInformation/ucm394909.htm. Accessed April 26, 2018.
- [22].Kozlowski LT, Sweanor DT. Young or adult users of multiple tobacco/nicotine products urgently need to be informed of meaningful differences in product risks. Addictive Behaviors. 2018; 76:376–381. [DOI] [PubMed] [Google Scholar]
- [23].Wackowski OA, Lewis MJ, Delnevo CD. Interviews with smokers about smokeless tobacco products, risk messages and news articles. Tob Control. 2016;25(6):671–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [24].Wackowski OA, Lewis MJ, Delnevo CD, Ling PM. Smokeless tobacco risk comparison and other debate messages in the news. Health Behav Policy Rev. 2014;1(3):183–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [25].Wackowski OA, Lewis MJ, Delnevo CD, Ling PM. A content analysis of smokeless tobacco coverage in U.S. newspapers and news wires. Nicotine Tob Res. 2013;15(7):1289–96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [26].Fotuhi O, Fong GT, Zanna MP, Borland R, Yong HH, Cummings KM. Patterns of cognitive dissonance-reducing beliefs among smokers: a longitudinal analysis from the International Tobacco Control (ITC) Four Country Survey. Tob Control. 2013;22(1):52–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [27].Persoskie A, Nelson WL. Just blowing smoke? Social desirability and reporting of intentions to quit smoking. Nicotine Tob Res. 2013;15(12):2088–93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [28].Yeager DS, Krosnick JA. The validity of self-reported nicotine product use in the 2001–2008 National Health and Nutrition Examination Survey. Med Care. 2010;48(12):1128–32. [DOI] [PubMed] [Google Scholar]
- [29].Popova L, Ling PM. Perceptions of relative risk of snus and cigarettes among US smokers. Am J Public Health. 2013;103(11):e21–e23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [30].Kaufman AR, Suls JM, Klein WM. Communicating tobacco product harm: compared to what? Addict Behav. 2016;52:123–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [31].Wackowski OA, Bover Manderski MT, Delnevo CD. Comparison of direct and indirect measures of e-cigarette risk perceptions. Tob Regul Sci. 2016; 2(1):38–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [32].Persoskie A, Nguyen AB, Kaufman AR, Tworek C. Criterion validity of measures of perceived relative harm of e-cigarettes and smokeless tobacco compared to cigarettes. Addict Behav. 2017;67:100–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.