Abstract
目的
系统总结新型冠状病毒肺炎(COVID-19)儿童病例的临床特征。
方法
计算机检索PubMed、Embase、Web of Science、The Cochrane Library、中国知网、重庆维普和万方数据库,搜集关于儿童COVID-19的临床研究,检索时限均为建库至2020年5月21日。由2名研究者独立筛选文献、提取资料并评价纳入研究的偏倚风险后,对纳入研究进行描述性分析。并与严重呼吸窘迫综合征(SARS)、中东呼吸综合征(MERS)儿童病例相关指标进行比较。
结果
共纳入75个研究,包括COVID-19儿童病例806例。研究结果显示:患儿年龄在生后36 h到18岁不等,男女比例为1.21:1。与SARS、MERS病例类似,COVID-19病例最常见感染方式为家庭聚集感染,占74.6%(601/806)。COVID-19、SARS及MERS病例临床症状相似,以发热、咳嗽为主。部分患儿出现消化道症状。上述三者无症状感染儿童比例分别为17.9%(144/806)、2.5%(2/81)及57.1%(12/21)。COVID-19、MERS病例胸部影像学病变以双侧为主,病变阳性率分别为63.4%(421/664)及26.3%(5/19),均低于其病毒核酸检测阳性率(分别为99.8%及100%)。而SARS病例胸部影像学以单侧病变为主,其影像学阳性率为88.9%(72/81),高于病毒核酸检测阳性率(29.2%)。COVID-19及SARS患儿粪便中均检测到病毒核酸,检测阳性率分别为60.2%(56/93)、71.4%(5/7)。COVID-19患儿重症率及病死率分别为4.5%(31/686)、0.1%(1/806);SARS儿童重症率及病死率分别为1.5%(1/68)、0%;MERS儿童重症率及病死率分别为14.3%(3/21)、9.5%(2/21)。
结论
儿童COVID-19临床症状与儿童SARS、MERS相似,以发热、咳嗽为主,均存在无症状感染者,但COVID-19和SARS儿童的病情较MERS轻。家庭聚集感染为COVID-19儿童重要的感染方式。流行病学接触史、影像学检查及病毒核酸检测结果是诊断COVID-19的重要依据。
Keywords: 新型冠状病毒肺炎, 严重呼吸窘迫综合征, 中东呼吸综合征, 系统评价, 临床特点, 儿童
Abstract
Objective
To systematically summarize the clinical features of coronavirus disease 2019 (COVID-19) in children.
Methods
PubMed, Embase, Web of Science, The Cochrane Library, CNKI, Weipu Database, and Wanfang Database were searched for clinical studies on COVID-19 in children published up to May 21, 2020. Two reviewers independently screened the articles, extracted data, and assessed the risk of bias of the studies included. A descriptive analysis was then performed for the studies. Related indices between children with COVID-19 and severe acute respiratory syndromes (SARS) or Middle East respiratory syndrome (MERS) were compared.
Results
A total of 75 studies were included, with a total of 806 children with COVID-19. The research results showed that the age of the children ranged from 36 hours after birth to 18 years, with a male-female ratio of 1.21:1. Similar to SARS and MERS, COVID-19 often occurred with familial aggregation, and such cases accounted for 74.6% (601/806). The children with COVID-19, SARS, and MERS had similar clinical symptoms, mainly fever and cough. Some children had gastrointestinal symptoms. The children with asymptomatic infection accounted for 17.9% (144/806) of COVID-19 cases, 2.5% (2/81) of SARS cases, and 57.1% (12/21) of MERS cases. The children with COVID-19 and MERS mainly had bilateral lesions on chest imaging examination, with a positive rate of lesions of 63.4% (421/664) and 26.3% (5/19) respectively, which were lower than the corresponding positive rates of viral nucleic acid detection, which were 99.8% and 100% respectively. The chest radiological examination of the children with SARS mainly showed unilateral lesion, with a positive rate of imaging of 88.9% (72/81), which was higher than the corresponding positive rate of viral nucleic acid detection (29.2%). Viral nucleic acid was detected in the feces of children with COVID-19 or SARS, with positive rates of 60.2% (56/93) and 71.4% (5/7) respectively. The children with COVID-19 had a rate of severe disease of 4.6% (31/686) and a mortality rate of 0.1% (1/806), the children with SARS had a rate of severe disease of 1.5% (1/68) and a mortality rate of 0%, and those with MERS had a rate of severe disease of 14.3% (3/21) and a mortality rate of 9.5% (2/21).
Conclusions
Children with COVID-19 have similar symptoms to those with SARS or MERS, mainly fever and cough. Asymptomatic infection is observed in all three diseases. Children with COVID-19 or SARS have milder disease conditions than those with MERS. COVID-19 in children often occurs with familial aggregation. Epidemiological contact history, imaging examination findings, and viral nucleic acid testing results are important bases for the diagnosis of COVID-19.
Keywords: Coronavirus disease 2019, Severe acute respiratory syndrome, Middle East respiratory syndrome, Systematic review, Clinical feature, Child
2019年12月,一种新型冠状病毒(severe acute respiratory syndrome coronavirus 2, SARS-CoV-2)开始流行,该病毒所引起的疾病命名为新型冠状病毒肺炎(coronavirus disease-19, COVID-19)[1]。截至2020年5月21日,全球共有4 992 845例感染病例,死亡325 196例,病死率为6.5%[2]。2020年1月31日世界卫生组织将其定性为公共卫生紧急事件,威胁着全人类健康[3]。
SARS-CoV-2人群普遍易感。儿童病例也陆续有报道,但儿童COVID-19患者的疾病特征尚不完全清楚。本文系统回顾儿童感染SARS-CoV-2的临床特点。同时,由于SARS-CoV-2与重症急性呼吸综合征(severe acute respiratory syndrome, SARS)冠状病毒、中东呼吸综合征(Middle East respiratory syndrome, MERS)冠状病毒有一定同源性,故本研究还与已报道的SARS、MERS儿童病例对比,旨在了解COVID-19儿童病例的临床特点,为儿童COVID-19的防控与诊疗提供依据。
1. 资料与方法
1.1. 文献纳入标准
本团队前期已针对儿童SARS及MERS感染病例进行了系统评价[4-5],本研究将儿童COVID-19病例与这两个系统评价纳入的SARS、MERS儿童病例进行对比分析。因此,本研究仅对儿童COVID-19相关文献的纳入通过系统检索。
纳入标准:(1)文献类型:病例报道、病例系列、病例对照、快报、简报等一次文献;(2)研究对象:目前全球发表的儿童感染SARS-CoV-2确诊病例(包括临床确诊及病毒核酸检测确诊);(3)文献语言:中文、英文;(4)结局指标数据完整。排除重复发表的文献。
1.2. 观察指标
观察指标包括:一般人口学特征(性别、年龄等)、流行病学特征(感染途径等)、临床特征(临床表现、实验室检查及治疗等)及转归等。
1.3. 文献检索策略
计算机检索PubMed、Embase、Web of Science、The Cochrane Library、中国知网、中文期刊全文数据库(维普)和万方数据库,搜集关于儿童COVID-19的研究,检索时限均为建库至2020年5月21日。采用主题词与自由词相结合的方式检索。中文检索词包括:新型冠状病毒肺炎、新型冠状病毒、新生儿、婴儿、幼儿、儿童、学龄前儿童、青少年等;英文检索词包括:COVID-19、coronavirus disease-19、severe acute respiratory syndrome coronavirus 2、newborn、infant、child、preschool、adolescent等。
1.4. 资料提取及文献质量评价
由2名研究者独立筛选文献及提取数据。若筛选及提取数据过程中发生分歧,则两人讨论或第3人加入直至达成共识。筛选文献需先排除重复文献,再浏览标题与摘要后排除,剩余文献需阅读全文再确定是否纳入。文献资料提取内容主要包括:纳入文献的基本信息,包括文献题目、作者、发表年份;SARS-CoV-2感染儿童的人口学特征、相关临床特征及结局指标。病例报道文献使用JBI标准评价[6],总体评价为纳入、排除及寻求进一步信息,总评分为8分。病例系列文献采用2012年加拿大卫生经济研究所(Institute of Health Economics, IHE)制定的质量评价工具[7],满足14条及以上为高质量文献。病例对照文献采用NOS进行评价[8],5分及以上为高质量文献。快报/简报/通讯目前尚无统一的质量评价工具,故暂未进行质量评价。
1.5. 统计学分析
因SARS及MERS病例数较少,因此,本系统评价采用频数、百分率(%)等进行描述性分析。
2. 结果
2.1. 文献筛选流程及结果
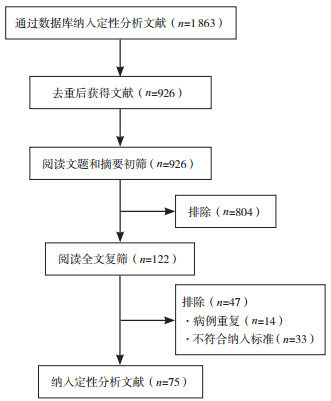
从上述7个数据库共检索到英文文献1 672篇,中文文献191篇。其中PubMed 724篇,Embase 338篇,Web of Science 586篇,The Cochrane Library 24篇,中国知网107篇,维普数据库26篇,万方数据库58篇。经逐层筛选,最终纳入75篇文献[9-83],其中病例报道43篇[9-51],病例系列18篇[52-69],病例对照2篇[70-71],快报/简报/通讯12篇[72-83]。Dong等[84]报道了2 143例儿童感染病例,为迄今为止最大的儿童病例数,但其数据来源为中国疾控中心,与纳入的其他病例存在重复可能,同时由于文章对于患儿的临床特点、治疗及转归未进行详细描述,故未纳入统计分析。文献筛选流程及结果见图 1。
1.
文献筛选流程及结果
2.2. 纳入文献偏倚风险评价结果
所纳入43篇病例报道文献评分在5~8分间。纳入18篇病例系列文献中,17篇满足IHE评价工具中9~13条内容,仅有1篇满足15条,为高质量研究。纳入2篇病例对照文献的质量评分为4分或5分,其中1篇为高质量研究。见表 1。
1.
纳入COVID-19文献的基本情况
| 纳入文献 | 国家 | 文献类型 | 例数 | 年龄 | 性别(男/女, 例) | 质量评价(分数或符合条数) |
| 赵瑞红2020[9] | 中国 | 病例报道 | 1 | 13岁 | 1/0 | 7 |
| 陈锋2020[10] | 中国 | 病例报道 | 1 | 1.08岁 | 1/0 | 8 |
| Chan 2020[11] | 中国 | 病例报道 | 1 | 10岁 | 1/0 | 5 |
| Kam 2020[12] | 新加坡 | 病例报道 | 1 | 0.5岁 | 1/0 | 5 |
| 张国勋2020[13] | 中国 | 病例报道 | 2 | 1.2岁 | 0/2 | 8 |
| 熊静娴2020[14] | 中国 | 病例报道 | 6 | 8~13岁 | 4/2 | 7 |
| Zhang 2020[15] | 中国 | 病例报道 | 3 | 6~9岁 | 3/0 | 7 |
| Fan 2020[16] | 中国 | 病例报道 | 1 | 0.25岁 | 0/1 | 5 |
| Cui 2020[17] | 中国 | 病例报道 | 1 | 55 d | 0/1 | 7 |
| Ji 2020[18] | 中国 | 病例报道 | 2 | 9~15岁 | 2/0 | 7 |
| Le 2020[19] | 越南 | 病例报道 | 1 | 0.3岁 | 0/1 | 7 |
| Lin 2020[20] | 中国 | 病例报道 | 1 | 7岁 | 0/1 | 8 |
| Park 2020[21] | 韩国 | 病例报道 | 1 | 10岁 | 0/1 | 5 |
| Shen 2020[22] | 中国 | 病例报道 | 9 | 1~12岁 | 3/6 | 6 |
| Su 2020[23] | 中国 | 病例报道 | 9 | 0.9~9岁 | 3/6 | 6 |
| Xing 2020[24] | 中国 | 病例报道 | 3 | 1.5~6岁 | 2/1 | 7 |
| 王劲2020[25] | 中国 | 病例报道 | 1 | 19 d | 1/0 | 7 |
| Wang 2020[26] | 中国 | 病例报道 | 1 | 1.5 d | 1/0 | 7 |
| 曾凌空2020[27] | 中国 | 病例报道 | 1 | 17 d | 1/0 | 7 |
| Kamali Aghdam 2020[28] | 伊朗 | 病例报道 | 1 | 15 d | 1/0 | 5 |
| 程行峰2020[29] | 中国 | 病例报道 | 2 | 0.9~1.2岁 | 1/1 | 7 |
| 邓慧玲2020[30] | 中国 | 病例报道 | 2 | 3.8~13岁 | 1/1 | 6 |
| 戢太阳2020[31] | 中国 | 病例报道 | 4 | 0.8~10岁 | 3/1 | 6 |
| 刘苗2020[32] | 中国 | 病例报道 | 1 | 9岁 | 1/0 | 6 |
| 沙广娟2020[33] | 中国 | 病例报道 | 1 | 5.5岁 | 1/0 | 7 |
| 王建云2020[34] | 中国 | 病例报道 | 1 | 1.7岁 | 0/1 | 7 |
| 杨丽丽2020[35] | 中国 | 病例报道 | 1 | 10岁 | 0/1 | 6 |
| 余增渊2020[36] | 中国 | 病例报道 | 1 | 22 d | 1/0 | 8 |
| 张华勇2020[37] | 中国 | 病例报道 | 2 | 13.3~13.7岁 | 2/0 | 7 |
| Li 2020[38] | 中国 | 病例报道 | 5 | 0.8~6岁 | 4/1 | 6 |
| Sun 2020[39] | 中国 | 病例报道 | 8 | 0.1~15岁 | 6/2 | 6 |
| Dugue 2020[40] | 美国 | 病例报道 | 1 | 0.1岁 | 1/0 | 5 |
| Genovese 2020[41] | 意大利 | 病例报道 | 1 | 8岁 | 0/1 | 6 |
| Han 2020[42] | 韩国 | 病例报道 | 1 | 27 d | 0/1 | 7 |
| Kan 2020[43] | 美国 | 病例报道 | 1 | 0.1岁 | 0/1 | 7 |
| Mansour 2020[44] | 黎巴嫩 | 病例报道 | 1 | 1.3岁 | 0/1 | 7 |
| Mao 2020[45] | 中国 | 病例报道 | 1 | 1.2岁 | 1/0 | 7 |
| Paret 2020[46] | 美国 | 病例报道 | 2 | 25~56 d | 2/0 | 6 |
| Shi 2020[47] | 中国 | 病例报道 | 1 | 0.3岁 | 1/0 | 7 |
| Yin 2020[48] | 中国 | 病例报道 | 1 | 9岁 | 0/1 | 6 |
| 周昀2020[49] | 中国 | 病例报道 | 9 | 0.6~3岁 | 4/5 | 7 |
| Eghbalian 2020[50] | 伊朗 | 病例报道 | 1 | 6 d | 0/1 | 6 |
| Piersigilli 2020[51] | 美国 | 病例报道 | 1 | 7 d | 0/1 | 7 |
| Cai 2020[52] | 中国 | 病例系列 | 10 | 0.3~11岁 | 4/6 | 9 |
| Xia 2020[53] | 中国 | 病例系列 | 20 | 1 d~14.5岁 | 13/7 | 10 |
| 王端2020[54] | 中国 | 病例系列 | 31 | 0.5~17岁 | 15/16 | 15 |
| Chen 2020[55] | 中国 | 病例系列 | 12 | 0.6~17岁 | 6/6 | 11 |
| Tang 2020[56] | 中国 | 病例系列 | 26 | 1~13岁 | 9/17 | 11 |
| Xu 2020[57] | 中国 | 病例系列 | 10 | 0.17~15岁 | 6/4 | 11 |
| 谭鑫2020[58] | 中国 | 病例系列 | 13 | 1~17岁 | 4/9 | 12 |
| Zhu 2020[59] | 中国 | 病例系列 | 10 | 1.6~17岁 | 5/5 | 12 |
| Zheng 2020[60] | 中国 | 病例系列 | 25 | 2~9岁 | 14/11 | 13 |
| Qiu 2020[61] | 中国 | 病例系列 | 36 | 1~16岁 | 23/13 | 13 |
| Denina 2020[62] | 意大利 | 病例系列 | 8 | 0.2~10岁 | 5/3 | 9 |
| 陈军2020[63] | 中国 | 病例系列 | 20 | 0.7~14岁 | 7/13 | 12 |
| 马慧静2020[64] | 中国 | 病例系列 | 22 | 0.2~14岁 | 12/10 | 11 |
| 李茜2020[65] | 中国 | 病例系列 | 30 | 0~14岁 | 18/12 | 9 |
| 钟正2020[66] | 中国 | 病例系列 | 9 | 0.3~12岁 | 5/4 | 9 |
| Song 2020[67] | 中国 | 病例系列 | 16 | 0.3~12岁 | 10/6 | 12 |
| Tan 2020[68] | 中国 | 病例系列 | 10 | 1~11.7岁 | 3/7 | 11 |
| Wu 2020[69] | 中国 | 病例系列 | 74 | 0.1~15.1岁 | 44/30 | 14 |
| Du 2020[70] | 中国 | 病例对照 | 14 | 未报道 | 6/8 | 4 |
| Han 2020[71] | 中国 | 病例对照 | 7 | 0.1~13岁 | 4/3 | 5 |
| Jiang 2020[72] | 中国 | 快报 | 2 | 3.6~6.7岁 | 0/2 | - |
| Lou 2020[73] | 中国 | 通讯 | 3 | 0.5~8岁 | 1/2 | - |
| Ng 2020[74] | 英国 | 简报 | 8 | 5 d~1岁 | 2/6 | - |
| Wei 2020[75] | 中国 | 快报 | 9 | 0.1~0.9岁 | 2/7 | - |
| Liu 2020[76] | 中国 | 快报 | 6 | 1~7岁 | 2/4 | - |
| Lu 2020[77] | 中国 | 快报 | 171 | 1 d~15岁 | 104/67 | - |
| Xu 2020[78] | 中国 | 快报 | 2 | 10~18岁 | 1/1 | - |
| Tang 2020[79] | 中国 | 快报 | 1 | 10岁 | 1/0 | |
| Zeng 2020[80] | 中国 | 快报 | 3 | 2~3岁 | 3/0 | - |
| Parri 2020[81] | 意大利 | 快报 | 100 | 0~17.5岁 | 57/43 | - |
| Wu 2020[82] | 中国 | 快报 | 1 | 2.8岁 | 1/0 | - |
| Chacón-Aguilar 2020[83] | 西班牙 | 快报 | 1 | 26 d | 1/0 | - |
2.3. 儿童SARS、MERS及COVID-19病例临床资料的比较
所纳入的75篇COVID-19文献中,包括COVID-19儿童病例806例(男442例,女364例),病例主要来源于中国(676例)及意大利(109例),美国、伊朗、韩国及越南有散在病例报道(共21例)。纳入SARS及MERS儿童病例分别为81例、21例[4-5]。纳入75篇儿童COVID-19文献的基本情况见表 1。
在纳入的806例COVID-19患儿中,年龄在生后36 h到18岁不等,男女比例为1.21 : 1,而SARS及MERS患儿女性感染病例占比更大,男女比例分别为1 : 1.1、1 : 1.6。SARS、MERS、COVID-19患儿大多有明确的流行病学史,最常见感染途径为家庭聚集感染,分别占所有病例的46.9%(38/81)、57.1%(12/21)、74.6%(601/806)。儿童COVID-19、SARS及MERS的临床症状相似,均以发热、咳嗽为主;出现明显气促或呼吸困难的比例分别为5.8%(47/806)、13.6%(11/81)及14.3%(3/21)。三者均有部分患儿出现腹泻、呕吐等消化道症状。MERS儿童病例的无症状患者高达57.1%(12/21),而SARS及COVID-19患儿比例分别为2.5%(2/81)与17.9%(144/806)。
在COVID-19儿童病例中,儿童血液学变化以炎症指标改变较为常见,包括C-反应蛋白(C-reactive protein, CRP)及降钙素原(procalcitonin, PCT)升高,比例分别为20.6%(82/398)及17.7%(58/328)。不同的是,报道的SARS患儿最常见的血液学变化为淋巴细胞减少,其比例高达64.2%(43/67),而报道的MERS病例血液学检查阳性率均不高。COVID-19、SARS及MERS的RT-PCR病毒核酸检测阳性率分别为99.8%(804/806)、29.2%(14/48)及100%(21/21)。部分COVID-19和SARS患儿粪便病毒核酸检测阳性,阳性率分别为60.2%、71.4%。报道的COVID-19、SARS以及MERS感染患儿出现影像学变化的发生率分别为63.4%(421/664)、88.9%(72/81)及26.3%(5/19),COVID-19及MERS患儿病变以双侧病变为主,而SARS以单侧改变为主。
在治疗上,COVID-19、SARS及MERS均以对因治疗及支持治疗为主。COVID-19、SARS及MERS抗病毒治疗的比例分别为67.7%(195/288)、71.4%(25/35)及0%(0/11)。其次为大剂量激素治疗。对于SARS儿童病例,激素使用率高达37.1%(13/35)。而COVID-19及MERS儿童病例激素使用率较低,分别为5.1%(19/373)及9.1%(1/11)。氧疗是重要的支持治疗方式之一。所报道的COVID-19患儿中,1.6%(10/609)需进行呼吸机辅助通气,8.9%(33/371)需无创氧疗。SARS患儿中需要使用呼吸机辅助呼吸者占1.5%(1/68),需无创氧疗者占8.8%(6/68)。而MERS患儿需呼吸机辅助呼吸及无创氧疗者均为15%(3/15)。另外,COVID-19患儿中,17.1%(37/217)患儿使用中医药治疗。
SARS的重症比例为1.5%(1/68),无死亡SARS病例报道,其住院时间为7~40 d。COVID-19患儿重症比例为4.5%(31/686),除73例仍在住院外,住院时间为3~29 d,死亡1例,死亡占比为0.1%。而MERS的重症率及病死率均较SARS及COVID-19高,住院时间较长。儿童SARS、MERS及COVID-19感染病例临床资料的比较见表 2。
2.
SARS、MERS与COVID-19儿童病例的临床资料比较
| 项目 | SARS | MERS | COVID-19 |
| 注:[SARS]严重呼吸窘迫综合征;[MERS]中东呼吸综合征;[COVID-19]新型冠状病毒肺炎;[CRP] C-反应蛋白;[AST]天门冬氨酸氨基转移酶酶;[ALT]丙氨酸氨基转移酶;[PCT]降钙素原。# 9例未报告性别。 | |||
| 报道文献数(篇) | 7 | 5 | 75 |
| 总例数 | 81 | 21 | 806 |
| 基本情况 | |||
| 年龄(范围) | 56 d~17.5岁 | 9个月~ 16岁 | 36 h~18岁 |
| 性别(男/女, 例) | 34/38# | 8/13 | 442/364 |
| 流行病学史[n/N (%)] | 48/81(59.3) | 17/21(81.0) | 747/806(92.7) |
| 家庭聚集感染[n/N (%)] | 38/81(46.9) | 12/21(57.1) | 601/806(74.6) |
| 其他感染方式[n/N (%)] | 10/81(12.3) | 5/21(23.8) | 146/806(18.1) |
| 症状[n/N(%)] | |||
| 发热 | 76/81(93.8) | 7/21(33.3) | 391/806(48.5) |
| 咳嗽 | 40/81(49.4) | 3/21(14.3) | 337/806(41.8) |
| 咽痛 | 11/81(13.6) | 0/21(0) | 34/806(4.2) |
| 流涕 | 17/81(21.0) | 0/21(0) | 69/806(8.6) |
| 气促/呼吸困难 | 11/81(13.6) | 3/21(14.3) | 47/806(5.8) |
| 鼻塞 | 6/81(7.4) | 0/21(0) | 20/806(2.5) |
| 呕吐 | 2/81(2.5) | 2/21(9.5) | 52/806(6.5) |
| 乏力 | 0/81(0) | 0/21(0) | 39/806(4.8) |
| 头痛 | 13/81(16.0) | 0/21(0) | 21/806(2.6) |
| 腹泻 | 9/81(11.1) | 2/21(9.5) | 78/806(9, 7) |
| 无症状 | 2/81(2.5) | 12/21(57.1) | 144/806(17.9) |
| 辅助检查[n/N(%)] | |||
| 淋巴细胞减少(< 1.0×109/L) | 43/67(64.2) | 0/1(0) | 61/501(12.2) |
| 白细胞减少(< 5.0×109/L) | 38/72(52.8) | 2/19(10.5) | 80/677(11.8) |
| 血小板减少(< 140×109/L) | 15/66(22.7) | 3/19(15.8) | 6/261(2.3) |
| AST或ALT升高 | 12/63(19.0) | 0/7(0) | 43/329(13.1) |
| 乳酸脱氢酶升高 | 22/34 (64.7) | 未描述 | 62/225(27.6) |
| CRP升高 | 10/33(30.0) | 1/1(100) | 82/398(20.6) |
| PCT升高 | 未描述 | 未描述 | 58/328(17.7) |
| 胸部影像学异常 | 72/81(88.9) | 5/19(26.3) | 421/664(63.4) |
| 胸部影像学双侧病变 | 21/81(25.9) | 5/19(26.3) | 203/664(30.6) |
| 胸部影像学单侧病变 | 51/81(63.0) | 0/19(0) | 180/664(27.1) |
| 呼吸道标本病毒核酸阳性 | 14/48(29.2) | 21/21(100) | 771/806(95.7) |
| 粪便标本病毒核酸阳性 | 5/7(71.4) | 未描述 | 56/93(60.2) |
| 治疗[n/N(%)] | |||
| 抗病毒 | 25/35(71.4) | 0/11(0) | 195/288(67.7) |
| 激素 | 13/35(37.1) | 1/11(9.1) | 19/373(5.1) |
| 免疫球蛋白 | 未描述 | 未描述 | 26/360(7.2) |
| 中医药治疗 | 未描述 | 未描述 | 37/217(17.1) |
| 呼吸机辅助呼吸 | 1/68(1.5) | 3/20(15.0) | 10/609(1.6) |
| 无创吸氧 | 6/68(8.8) | 3/20(15.0) | 33/371(8.9) |
| 重症监护治疗 | 1/68(1.5) | 3/21(14.3) | 31/686(4.5) |
| 结局及预后 | |||
| 病死率[n/N(%)] | 0/81(0) | 2/21(9.5) | 1/806(0.1) |
| 住院时间(范围, d) | 7~40 | 0~60 | 3~29 |
| 治愈出院[n/N(%)] | 81/81(100) | 19/21(90.5) | 732/806(90.8) |
| 报道时仍住院治疗[n/N(%)] | 0/81(0) | 0/21(0) | 73/806(9.1) |
3. 讨论
COVID-19疫情早期儿童COVID-19病例较少,但随着疫情全面暴发,儿童病例逐渐增多。目前来自中国及美国疾控中心数据显示,约98%的COVID-19病例为成人,18岁以下的儿童感染占总感染人数的2.0%~2.4%,年龄跨度从生后36 h到18岁不等[85-86]。但儿童发病率低并不代表儿童不易感,研究显示10岁以下的儿童与其他年龄组的感染风险相同;儿童感染的风险为7.4%,与普通人群相似[87]。
与SARS相似,SARS-CoV-2的主要传播途径为经呼吸道飞沫及接触传播[88]。此外,陆续有报道患儿粪便及肠道中检测到病毒核酸[24-25, 35]。本系统评价所纳入文献中,共检测了93名COVID-19患儿粪便,其中56例为阳性,阳性率为60.2%;7名SARS患儿粪便中5例病毒核酸为阳性,占71.4%。且肛拭子核酸检测阳性往往滞后于咽拭子检测,并在咽拭子转阴后可持续阳性数周[89]。粪便污染环境后可导致气溶胶经呼吸道或接触传播,因此建议增加感染患者隔离时间。74.6%的COVID-19儿童病例以及近半数的SARS及MERS儿童患者均为家庭聚集感染,提示家庭聚集感染为冠状病毒感染儿童最主要的感染形式。另外,目前报道的COVID-19新生儿病例中,均考虑为家庭聚集感染,尚无SARS-CoV-2母婴传播的证据。在实际疫情防控中,儿童病例大多是追踪成人病例进而筛查出来的。因此,针对有流行病学史的家庭,应做好手卫生,佩戴口罩,同时加强监测和评估儿童感染情况。
冠状病毒感染最常见的临床症状为发热、咳嗽。相比于MERS儿童病例,COVID-19与SARS儿童病例总体症状较轻,以上呼吸道感染症状及消化道症状为主,呼吸困难发生率低。值得注意的是,无症状儿童并不少见。据大数据研究显示,94.1%的儿童病例是无症状感染或轻中症[84],考虑可能与儿童免疫系统T细胞功能不成熟、儿童经常受到其他呼吸道病毒感染的刺激导致病毒间的竞争性抑制有关。但近期英美国家陆续有儿童不明原因的川崎病样病症报道,且重症比例高,部分患儿COVID-19血清抗体检测阳性,但核酸检测阴性[90],故目前尚不清楚其是否与COVID-19相关联[91],因此,我们将持续关注后续报道。
感染早期影像学改变是重要特征之一,虽本系统评价中MERS及COVID-19病例影像学证据较病毒核酸检测阳性率低,但既往对SARS儿童病例的研究显示,病毒核酸检测的假阴性率高,同时COVID-19儿童轻症及无症状者较多,考虑可能存在漏诊者,因此,应重视影像学检查与核酸检测相结合进行早期发现及诊断。
纵观本世纪流行的SARS冠状病毒、MERS冠状病毒及SARS-CoV-2 3种冠状病毒感染,其治疗主要以对症支持治疗为主。目前尚未报道该3种冠状病毒感染的特效抗病毒药物。本系统评价显示,儿童SARS-CoV-2抗病毒药物的使用率为67.7%,主要为洛匹那韦利托那韦、盐酸阿比洛尔及干扰素,但由于儿童病例大多为轻症,且“上海方案”主张对于非重症儿童可不使用抗病毒药物[52],因此需进一步探讨抗病毒药物的疗效以规范儿童抗病毒的治疗指征。值得注意的是,此次COVID-19提出中医辨证论治,且在普通成人病例中证明有效,儿童中也有使用,可为轻症患儿的治疗提供参考。
本系统评价所纳入的806例COVID-19病例中,死亡1例,除73例报道时仍住院者,其余均治愈出院,总体预后较好,病死率低;SARS儿童重症1例,无死亡病例。COVID-19和SARS儿童重症率及病死率低于MERS患儿。
本研究的局限性:纳入分析的文献以病例系列和病例报道为主;且分析病例数量少,研究时间段短,由于原始文献中儿童年龄分层较模糊,无法针对年龄进行分层分析,证据级别较低。有一些感染人群尚未进行系统报道,仅纳入已报道病例,可能无法全面反映疾病流行情况。
综上所述,相比于MERS儿童病例,COVID-19和SARS儿童病例具有更高的相似性。COVID-19儿童病例轻症居多,病死率低,存在无症状感染者。家庭聚集感染为COVID-19儿童重要的感染方式。加强儿童监管,注意家庭卫生,根据流行病学接触史、影像学检查及病毒核酸检测结果进行早期识别对儿童COVID-19的防控具有重要意义。
Biographies
何洋, 女, 博士研究生
Tang J, Email: tj1234753@sina.com
Funding Statement
国家临床重点专科(儿科新生儿专业)建设项目(1311200003303)
References
- 1.World Health Organization. WHO Director-General's remarks at the media briefing on 2019-nCoV on 11 February 2020[EB/OL]. (2020-02-11)[2020-05-21]. https://www.who.int/dg/speeches/detail/who-director-general-s-remarks-at-the-media-briefing-on-2019-ncov-on-11-february-2020.
- 2.World Health Organization. Coronavirus disease (COVID-2019) situation reports[EB/OL].[2020-05-21]. https://www.who.int/emergencies/diseases/novel-coronavirus-2019/situation-reports.
- 3.World Health Organization. Coronavirus disease (COVID-19) Pandemic-Emergency Use Listing Procedure (EUL) open for in vitro diagnostics[EB/OL]. (2020-02-28)[2020-05-21]. https://www.who.int/diagnostics_laboratory/EUL/en/.
- 4.李 文星, 唐 军, 曾 燕, et al. SARS感染孕产妇、新生儿及儿童、青少年的系统评价. http://www.wanfangdata.com.cn/details/detail.do?_type=perio&id=zgxzyx202004009 中国循证医学杂志. 2020;20(4):426–436. [Google Scholar]
- 5.何 洋, 唐 军, 张 萌, et al. 孕产妇及儿童MERS患者临床特征的系统评价. http://www.wanfangdata.com.cn/details/detail.do?_type=perio&id=zgxzyx202005013 中国循证医学杂志. 2020;20(5):576–584. [Google Scholar]
- 6.Institute TJB. Joanna Briggs Institute Reviewers' Manual: 2016 edition[EB/OL].[2020-05-21]. https: //joannabriggs.org/.
- 7.Moga C, Guo B, Schopflocher D, et al. Development of a quality appraisal tool for case series studies using a modified Delphi technique[EB/OL]. (2012-03-07)[2020-05-21]. https://www.ihe.ca/advanced-search/development-of-a-quality-appraisal-tool-for-case-series-studies-using-a-modified-delphi-technique.
- 8.Wells GA, Shea B, Connell DO, et al. The Newcastle-Ottawa scale (NOS) for assessing the quality of nonrandomized studies in meta-analyses. http://www.wanfangdata.com.cn/details/detail.do?_type=perio&id=WK_LWW201705250348848 Appl Eng Agric. 2002;18(6):727–734. [Google Scholar]
- 9.赵 瑞红, 沈 晓敏, 徐 凯进, et al. 儿童感染新型冠状病毒肺炎1例. http://www.wanfangdata.com.cn/details/detail.do?_type=perio&id=zjyx202004003 浙江医学. 2020;42(4):305–306. [Google Scholar]
- 10.陈 锋, 刘 智胜, 张 芙蓉, et al. 中国首例儿童危重型新型冠状病毒肺炎. http://www.wanfangdata.com.cn/details/detail.do?_type=perio&id=zhek202003004 中华儿科杂志. 2020;58(3):179–182. [Google Scholar]
- 11.Chan JF, Yuan S, Kok KH, et al. A familial cluster of pneumonia associated with the 2019 novel coronavirus indicating person-to-person transmission:a study of a family cluster. Lancet. 2020;395(10223):514–523. doi: 10.1016/S0140-6736(20)30154-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kam KQ, Yung CF, Cui L, et al. A well infant with coronavirus disease 2019(COVID-19) with high viral load. Clin Infect Dis. 2020;71(15):847–849. doi: 10.1093/cid/ciaa201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.张 国勋, 张 爱民, 黄 丽, et al. 一对双胎女童同时感染新型冠状病毒. http://www.zgddek.com/CN/abstract/abstract24958.shtml. 中国当代儿科杂志. 2020;22(3):221–225. doi: 10.7499/j.issn.1008-8830.2020.03.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.熊静娴, 周驰宇, 曾文兵.儿童新型冠状病毒肺炎患者的CT表现[J/OL].重庆医学. (2020-04-03)[2020-05-21]. https://kns.cnki.net/kcms/detail/50.1097.R.20200403.1227.011.html.
- 15.Zhang T, Cui X, Zhao X, et al. Detectable SARS-CoV-2 viral RNA in feces of three children during recovery period of COVID-19 pneumonia. J Med Virol. 2020;92(7):909–914. doi: 10.1002/jmv.25795. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Fan Q, Pan Y, Wu Q, et al. Anal swab findings in an infant with COVID-19. http://www.wanfangdata.com.cn/details/detail.do?_type=perio&id=ekx-e202001014. Pediatr Investig. 2020;4(1):48–50. doi: 10.1002/ped4.12186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Cui Y, Tian M, Huang D, et al. A 55-day-old female infant infected with 2019 novel coronavirus disease:presenting with pneumonia, liver injury, and heart damage. J Infect Dis. 2020;221(11):1775–1781. doi: 10.1093/infdis/jiaa113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ji LN, Chao S, Wang YJ, et al. Clinical features of pediatric patients with COVID-19:a report of two family cluster cases. World J Pediatr. 2020;16(3):267–270. doi: 10.1007/s12519-020-00356-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Le HT, Nguyen LV, Tran DM, et al. The first infant case of COVID-19 acquired from a secondary transmission in Vietnam. Lancet Child Adolesc Health. 2020;4(5):405–406. doi: 10.1016/S2352-4642(20)30091-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Lin J, Duan J, Tan T, et al. The isolation period should be longer:lesson from a child infected with SARS-CoV-2 in Chongqing, China. Pediatr Pulmonol. 2020;55(6):E6–E9. doi: 10.1002/ppul.24763. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Park JY, Han MS, Park KU, et al. First pediatric case of coronavirus disease 2019 in Korea. J Korean Med Sci. 2020;35(11):e124. doi: 10.3346/jkms.2020.35.e124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Shen Q, Guo W, Guo T, et al. Novel coronavirus infection in children outside of Wuhan, China. http://www.wanfangdata.com.cn/details/detail.do?_type=perio&id=10.1097/ALN.0000000000003301. Pediatr Pulmonol. 2020;55(6):1424–1429. doi: 10.1002/ppul.24762. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Su L, Ma X, Yu H, et al. The different clinical characteristics of corona virus disease cases between children and their families in China-the character of children with COVID-19. Emerg Microbes Infect. 2020;9(1):707–713. doi: 10.1080/22221751.2020.1744483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Xing YH, Ni W, Wu Q, et al. Prolonged viral shedding in feces of pediatric patients with coronavirus disease 2019. J Microbiol Immunol Infect. 2020;53(3):473–480. doi: 10.1016/j.jmii.2020.03.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.王 劲, 王 丹, 陈 国策, et al. 以消化道症状为首发表现的新生儿SARS-CoV-2感染1例. http://www.zgddek.com/CN/abstract/abstract24956.shtml. 中国当代儿科杂志. 2020;22(3):211–214. doi: 10.7499/j.issn.1008-8830.2020.03.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Wang S, Guo L, Chen L, et al. A case report of neonatal COVID-19 infection in China. Clin Infect Dis. 2020;71(15):853–857. doi: 10.1093/cid/ciaa225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.曾 凌空, 陶 旭炜, 袁 文浩, et al. 中国首例新生儿新型冠状病毒肺炎. http://www.wanfangdata.com.cn/details/detail.do?_type=perio&id=zhek202004011 中华儿科杂志. 2020;58(4):279–280. [Google Scholar]
- 28.Kamali Aghdam M, Jafari N, Eftekhari K. Novel coronavirus in a 15-day-old neonate with clinical signs of sepsis, a case report. http://www.wanfangdata.com.cn/details/detail.do?_type=perio&id=10.1080/23744235.2020.1747634. Infect Dis (Lond) 2020;52(6):427–429. doi: 10.1080/23744235.2020.1747634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.程 行锋, 张 芙蓉, 熊 瑞华, et al. 2例婴幼儿新型冠状病毒肺炎并发弥散性血管内凝血病例报道. http://www.wanfangdata.com.cn/details/detail.do?_type=perio&id=zgzxyjhjjzz202001013 中国中西医结合急救杂志. 2020;27(1):46–49. [Google Scholar]
- 30.邓 慧玲, 张 玉凤, 王 义, et al. 儿童新型冠状病毒感染二例报道. http://www.wanfangdata.com.cn/details/detail.do?_type=perio&id=xejjyx202002005 中国小儿急救医学. 2020;27(2):81–83. [Google Scholar]
- 31.戢 太阳, 陈 全景, 陈 富超, et al. 4例儿童新型冠状病毒肺炎的临床特点和药物治疗分析. http://www.wanfangdata.com.cn/details/detail.do?_type=perio&id=ekyx202004008 儿科药学杂志. 2020;26(4):24–27. [Google Scholar]
- 32.刘 苗, 万 曦, 涂 晓燕, et al. 一起家庭聚集性儿童感染新型冠状病毒分析. http://www.wanfangdata.com.cn/details/detail.do?_type=perio&id=hubeiykdxxb202003005 武汉大学学报(医学版) 2020;41(3):362–365. [Google Scholar]
- 33.沙 广娟. 1例儿童感染新型冠状病毒合并流感病毒的报告. http://www.wanfangdata.com.cn/details/detail.do?_type=perio&id=hnyfyxzz202005002 河南预防医学杂志. 2020;31(5):323–324. [Google Scholar]
- 34.王 建云, 王 永军, 周 莹荃, et al. 儿童新型冠状病毒肺炎1例病例报告. http://www.wanfangdata.com.cn/details/detail.do?_type=perio&id=zgxzekzz202001010 中国循证儿科杂志. 2020;15(1):42–44. [Google Scholar]
- 35.杨 丽丽, 叶 佩佩, 葛 怀志, et al. 多次血尿、反复肛拭子或粪便核酸检测阳性的轻型COVID-19患儿1例. http://www.wanfangdata.com.cn/details/detail.do?_type=perio&id=wzyxyxb202005015 温州医科大学学报. 2020;50(5):423–424. [Google Scholar]
- 36.余 增渊, 薛 伟, 冯 迎军, et al. 新生儿重型新型冠状病毒肺炎转运治疗1例病例报告. http://www.wanfangdata.com.cn/details/detail.do?_type=perio&id=zgxzekzz202001009 中国循证儿科杂志. 2020;15(1):37–41. [Google Scholar]
- 37.张 华勇, 张 勇. 儿童COVID-19合并高血压2例. http://www.zgddek.com/CN/abstract/abstract24998.shtml. 中国当代儿科杂志. 2020;22(5):425–428. doi: 10.7499/j.issn.1008-8830.2004017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Li W, Cui H, Li K, et al. Chest computed tomography in children with COVID-19 respiratory infection. Pediatr Radiol. 2020;50(6):796–799. doi: 10.1007/s00247-020-04656-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Sun D, Li H, Lu XX, et al. Clinical features of severe pediatric patients with coronavirus disease 2019 in Wuhan:a single center's observational study. World J Pediatr. 2020;16(3):251–259. doi: 10.1007/s12519-020-00354-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Dugue R, Cay-Martínez KC, Thakur KT, et al. Neurologic manifestations in an infant with COVID-19. Neurology. 2020;94(24):1100–1102. doi: 10.1212/WNL.0000000000009653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Genovese G, Colonna C, Marzano AV. Varicella-like exanthem associated with COVID-19 in an 8-year-old girl:a diagnostic clue? Pediatr Dermatol. 2020;37(3):435–436. doi: 10.1111/pde.14201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Han MS, Seong MW, Heo EY, et al. Sequential analysis of viral load in a neonate and her mother infected with SARS-CoV-2. Clin Infect Dis. 2020 doi: 10.1093/cid/ciaa447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Kan MJ, Grant LMC, Muña MA, et al. Fever without a source in a young infant due to SARS-CoV-2. J Pediatric Infect Dis Soc. 2020 doi: 10.1093/jpids/piaa044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Mansour A, Atoui R, Kanso K, et al. First case of an infant with COVID-19 in the Middle East. Cureus. 2020;12(4):e7520. doi: 10.7759/cureus.7520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Mao LJ, Xu J, Xu ZH, et al. A child with household transmitted COVID-19. BMC Infect Dis. 2020;20(1):329. doi: 10.1186/s12879-020-05056-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Paret M, Lighter J, Pellett Madan R, et al. SARS-CoV-2 infection (COVID-19) in febrile infants without respiratory distress. Clin Infect Dis. 2020 doi: 10.1093/cid/ciaa452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Shi B, Xia Z, Xiao S, et al. Severe pneumonia due to SARS-CoV-2 and respiratory syncytial virus infection:a case report. Clin Pediatr (Phila) 2020;59(8):823–826. doi: 10.1177/0009922820920016. [DOI] [PubMed] [Google Scholar]
- 48.Yin X, Dong L, Zhang Y, et al. A mild type of childhood Covid-19-a case report. Radiol Infect Dis. 2020 doi: 10.1016/j.jrid.2020.03.004. doi: 10.1016/j.jrid.2020.03.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.周 昀, 杨 根东, 冯 凯, et al. 婴幼儿2019冠状病毒病的临床特点及胸部CT表现. http://www.zgddek.com/CN/abstract/abstract24957.shtml. 中国当代儿科杂志. 2020;22(3):215–220. doi: 10.7499/j.issn.1008-8830.2020.03.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Eghbalian F, Esfahani AM, Jenabi E. COVID-19 virus in a 6-day-old girl neonate:a case report. Clin Pediatr (Phila) 2020 doi: 10.1177/0009922820946010. doi: 10.1177/0009922820946010. [DOI] [PubMed] [Google Scholar]
- 51.Piersigilli F, Carkeek K, Hocq C, et al. COVID-19 in a 26-week preterm neonate. Lancet Child Adolesc Health. 2020;4(6):476–478. doi: 10.1016/S2352-4642(20)30140-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Cai J, Xu J, Lin D, et al. A case series of children with 2019 novel coronavirus infection:clinical and epidemiological features. Clin Infect Dis. 2020 doi: 10.1093/cid/ciaa198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Xia W, Shao J, Guo Y, et al. Clinical and CT features in pediatric patients with COVID-19 infection:different points from adults. Pediatr Pulmonol. 2020;55(5):1169–1174. doi: 10.1002/ppul.24718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.王 端, 鞠 秀丽, 谢 峰, et al. 中国北方六省(自治区)儿童2019新型冠状病毒感染31例临床分析. http://www.wanfangdata.com.cn/details/detail.do?_type=perio&id=zhek202004004 中华儿科杂志. 2020;58(4):269–274. [Google Scholar]
- 55.Chen J, Zhang ZZ, Chen YK, et al. The clinical and immunological features of pediatric COVID-19 patients in China. Genes Dis. 2020 doi: 10.1016/j.gendis.2020.03.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Tang AJ, Xu WH, Shen M, et al. A retrospective study of the clinical characteristics of COVID-19 infection in 26 children[J/OL]. medRxiv. (2020-03-10)[2020-05-21]. DOI: 10.1101/2020.03.08.20029710. Epub ahead of print.
- 57.Xu Y, Li X, Zhu B, et al. Characteristics of pediatric SARS-CoV-2 infection and potential evidence for persistent fecal viral shedding. Nat Med. 2020;26(4):502–505. doi: 10.1038/s41591-020-0817-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.谭 鑫, 黄 娟, 赵 芬, et al. 长沙市儿童新型冠状病毒感染13例临床特征分析. http://www.zgddek.com/CN/abstract/abstract24966.shtml. 中国当代儿科杂志. 2020;22(4):294–298. doi: 10.7499/j.issn.1008-8830.2003199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Zhu L, Wang J, Huang R, et al. Clinical characteristics of a case series of children with coronavirus disease 2019. http://www.wanfangdata.com.cn/details/detail.do?_type=perio&id=10.1097/INF.0000000000002700. Pediatr Pulmonol. 2020;55(6):1430–1432. doi: 10.1002/ppul.24767. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Zheng F, Liao C, Fan QH, et al. Clinical characteristics of children with coronavirus disease 2019 in Hubei, China. Curr Med Sci. 2020;40(2):275–280. doi: 10.1007/s11596-020-2172-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Qiu H, Wu J, Hong L, et al. Clinical and epidemiological features of 36 children with coronavirus disease 2019(COVID-19) in Zhejiang, China:an observational cohort study. Lancet Infect Dis. 2020;20(6):689–696. doi: 10.1016/S1473-3099(20)30198-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Denina M, Scolfaro C, Silvestro E, et al. Lung ultrasound in children with COVID-19. Pediatrics. 2020;146(1):e20201157. doi: 10.1542/peds.2020-1157. [DOI] [PubMed] [Google Scholar]
- 63.陈 军, 王 险峰, 张 培发. 新型冠状病毒感染无症状患儿20例临床分析. http://www.zgddek.com/CN/abstract/abstract24994.shtml. 中国当代儿科杂志. 2020;22(5):414–418. doi: 10.7499/j.issn.1008-8830.2003084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.马 慧静, 邵 剑波, 王 永姣, et al. 新型冠状病毒肺炎儿童高分辨率CT表现. http://www.wanfangdata.com.cn/details/detail.do?_type=perio&id=zhfsx202004011 中华放射学杂志. 2020;54(4):310–313. [Google Scholar]
- 65.李 茜, 彭 雪华, 孙 子燕, et al. 儿童新型冠状病毒肺炎(COVID-19)的临床及影像学表现. http://www.wanfangdata.com.cn/details/detail.do?_type=perio&id=fsxsj202003008 放射学实践. 2020;35(3):277–280. [Google Scholar]
- 66.钟 正, 谢 幸芷, 黄 巍, et al. 儿童2019冠状病毒病患者的胸部CT表现和临床特征. http://www.wanfangdata.com.cn/details/detail.do?_type=perio&id=hnykdx202003004. 中南大学学报(医学版) 2020;45(3):236–242. doi: 10.11817/j.issn.1672-7347.2020.200206. [DOI] [PubMed] [Google Scholar]
- 67.Song W, Li J, Zou N, et al. Clinical features of pediatric patients with coronavirus disease (COVID-19) J Clin Virol. 2020;127:104377. doi: 10.1016/j.jcv.2020.104377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Tan YP, Tan BY, Pan J, et al. Epidemiologic and clinical characteristics of 10 children with coronavirus disease 2019 in Changsha, China. J Clin Virol. 2020;127:104353. doi: 10.1016/j.jcv.2020.104353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Wu Q, Xing Y, Shi L, et al. Coinfection and other clinical characteristics of COVID-19 in children. Pediatrics. 2020;146(1):e20200961. doi: 10.1542/peds.2020-0961. [DOI] [PubMed] [Google Scholar]
- 70.Du W, Yu J, Wang H, et al. Clinical characteristics of COVID-19 in children compared with adults in Shandong Province, China. Infection. 2020;48(3):445–452. doi: 10.1007/s15010-020-01427-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Han YN, Feng ZW, Sun LN, et al. A comparative-descriptive analysis of clinical characteristics in 2019-coronavirus-infected children and adults. J Med Virol. 2020 doi: 10.1002/jmv.25835. [DOI] [PubMed] [Google Scholar]
- 72.Jiang S, Liu P, Xiong G, et al. Coinfection of SARS-CoV-2 and multiple respiratory pathogens in children. http://www.wanfangdata.com.cn/details/detail.do?_type=perio&id=DGYTcclm-2020-0434. Clin Chem Lab Med. 2020;58(7):1160–1161. doi: 10.1515/cclm-2020-0434. [DOI] [PubMed] [Google Scholar]
- 73.Lou XX, Shi CX, Zhou CC, et al. Three children who recovered from novel coronavirus 2019 pneumonia. J Paediatr Child Health. 2020;56(4):650–651. doi: 10.1111/jpc.14871. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Ng KF, Bandi S, Bird PW, et al. COVID-19 in neonates and infants:progression and recovery. Pediatr Infect Dis J. 2020;39(7):e140–e142. doi: 10.1097/INF.0000000000002738. [DOI] [PubMed] [Google Scholar]
- 75.Wei M, Yuan J, Liu Y, et al. Novel coronavirus infection in hospitalized infants under 1 year of age in China. JAMA. 2020;323(13):1313–1314. doi: 10.1001/jama.2020.2131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Liu W, Zhang Q, Chen J, et al. Detection of Covid-19 in children in early January 2020 in Wuhan, China. N Engl J Med. 2020;382(14):1370–1371. doi: 10.1056/NEJMc2003717. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Lu X, Zhang L, Du H, et al. SARS-CoV-2 infection in children. N Engl J Med. 2020;382(17):1663–1665. doi: 10.1056/NEJMc2005073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Xu R, Du M, Li L, et al. CT imaging of one extended family cluster of corona virus disease 2019(COVID-19) including adolescent patients and "silent infection". http://cn.bing.com/academic/profile?id=e7b3b76cb9a74a542a6d11bf34ded8a5&encoded=0&v=paper_preview&mkt=zh-cn. Quant Imaging Med Surg. 2020;10(3):800–804. doi: 10.21037/qims.2020.02.13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Tang A, Tong ZD, Wang HL, et al. Detection of novel coronavirus by RT-PCR in stool specimen from asymptomatic child, China. Emerg Infect Dis. 2020;26(6):1337–1339. doi: 10.3201/eid2606.200301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Zeng LK, Xia SW, Yuan WH, et al. Neonatal early-onset infection with SARS-CoV-2 in 33 neonates born to mothers with COVID-19 in Wuhan, China. JAMA Pediatr. 2020;174(7):722–725. doi: 10.1001/jamapediatrics.2020.0878. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Parri N, Lenge M, Buonsenso D, et al. Children with Covid-19 in pediatric emergency departments in Italy. N Engl J Med. 2020;383(2):187–190. doi: 10.1056/NEJMc2007617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Wu P, Liang L, Chen C, et al. A child confirmed COVID-19 with only symptoms of conjunctivitis and eyelid dermatitis. Graefes Arch Clin Exp Ophthalmol. 2020;258(7):1565–1566. doi: 10.1007/s00417-020-04708-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Chacón-Aguilar R, Osorio-Cámara JM, Sanjurjo-Jimenez I, et al. COVID-19:fever syndrome and neurological symptoms in a neonate. An Pediatr (Engl Ed) 2020;92(6):373–374. doi: 10.1016/j.anpede.2020.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Dong Y, Mo X, Hu Y, et al. Epidemiology of COVID-19 among children in China. Pediatrics. 2020;145(6):e20200702. doi: 10.1542/peds.2020-0702. [DOI] [PubMed] [Google Scholar]
- 85.中华人民共和国国家卫生健康委员会疾病预防控制局.中国-世界卫生组织新型冠状病毒肺炎(COVID-19)联合考察报告[EB/OL]. (2020-02-29)[2020-05-21]. http://www.nhc.gov.cn/jkj/s3578/202002/87fd92510d094e4b9bad597608f5cc2c.shtml.
- 86.CDC COVID-19 Response Team Coronavirus disease 2019 in children-United States, February 12-April 2, 2020. http://www.wanfangdata.com.cn/details/detail.do?_type=perio&id=10.1097/RTI.0000000000000527. MMWR Morb Mortal Wkly Rep. 2020;69(14):422–426. doi: 10.15585/mmwr.mm6914e4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Bi QF, Wu YS, Mei SJ, et al. Epidemiology and transmission of COVID-19 in Shenzhen China: analysis of 391 cases and 1, 286 of their close contacts[J/OL]. medRxiv. (2020-03-03)[2020-05-21]. DOI: 10.1101/2020.03.03.20028423.
- 88.中华人民共和国国家卫生健康委员会医政医管局.新型冠状病毒肺炎诊疗方案(试行第七版)[EB/OL]. (2020-03-03)[2020-05-21]. http://www.nhc.gov.cn/yzygj/s7653p/202003/46c9294a7dfe4cef80dc7f5912eb1989/files/ce3e6945832a438eaae415350a8ce964.pdf.
- 89.Wang L, Shi Y, Xiao T, et al. Chinese expert consensus on the perinatal and neonatal management for the prevention and control of the 2019 novel coronavirus infection (First edition) Ann Transl Med. 2020;8(3):47. doi: 10.21037/atm.2020.02.20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Riphagen S, Gomez X, Gonzalez-Martinez C, et al. Hyperinflammatory shock in children during COVID-19 pandemic. Lancet. 2020;395(10237):1607–1608. doi: 10.1016/S0140-6736(20)31094-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.焦 富勇. 川崎病——儿童COVID-19的一种新的表现形式. http://www.zgddek.com/CN/abstract/abstract25030.shtml. 中国当代儿科杂志. 2020;22(7):677–678. doi: 10.7499/j.issn.1008-8830.2005117. [DOI] [PMC free article] [PubMed] [Google Scholar]


