ABSTRACT
Coronavirus disease 2019 (COVID-19) characterized by immuno-pathological host responses including pneumonia, lymphopenia, and cytokine storm that leads to severe lung inflammation, developed in acute respiratory distress syndrome (ARDS). In the absence of an effective vaccine or any definitive cure, the use of host-directed therapies is an effective alternative and demanding treatment option in the current pandemic outbreak of COVID-19.
KEYWORDS: Infectious disease, Covid-19, SARS-CoV-2, host-directed
1. Coronavirus disease 2019
The SARS-CoV-2 virus is spreading on a rapid scale around the globe, causing COVID-19 and thus the breakdown of human activity and the global economy due to lockdowns. Citing the alarming levels of COVID-19 spread and its severity, WHO has declared a global emergency on 30 January 2020. The incubation period for COVID-19 ranges from 2–14 days, with an average of 5 days. The majority of patients (~80%) exhibit mild or moderate symptoms while about 14% are severe infections (requiring oxygen therapy) and about 5% are critical infections, ultimately develops acute respiratory distress syndrome (ARDS), sepsis, and multi-organ failure [1,2]. Symptomatic management of disease and oxygen therapy has remained the mainstay of clinical treatment, in absence of any specifically approved treatment for COVID-19. Until, vaccine development is ongoing to establish the herd immunity, but testing and development of vaccines may likely take a year. Additionally, several known antiviral drugs are being actively repurposed for the treatment of COVID-19 but none of them are specifically approved yet. Apart from this, many approaches that directly block the viral entry and even immunopathology based treatment strategies are of major interest. However, rapid mutations resulting in the new pathogenic strains of SARS-CoV-2 that develop an urgent need for suitable therapeutic strategies [3]. The infection can be transmitted mainly via inhalation of aerosol droplets from coughing, sneezing, or talking of symptomatic and asymptomatic individuals. Inhaled SARS-CoV-2 first binds to the nasal epithelium and starts replication where SARS-CoV-2 entry factors (entry receptor angiotensin-converting enzyme 2 (ACE2) and entry-associated protease (TMPRSS2)) are highly expressed together with innate immune genes [4,5]. Then SARS-CoV-2 reaches the alveolar space of the lung and infects alveolar type II cells, rich in the ACE2 receptor [6]. Similar to SARS-CoV and MERS infection, patients with COVID-19 show clinical manifestations including fever, nonproductive cough, difficulty in breathing, and severe lung pathology leading to death [7]. Currently, there is no drug or vaccine available for COVID-19 and further, because of mutation in new strains of SARS-CoV-2 along with patient-derived mutations [8], it becomes more difficult to treat SARS-CoV-2 infection. In this situation, several available host-directed therapies might play as a potential approach to combat ongoing pandemic COVID-19 [9].
2. Expert opinion
Lymphopenia is a common feature in patients with severe COVID-19, with drastically reduced numbers of CD4+, CD8+ T cells, B cells and natural killer (NK) cells, and reduced percentage of monocytes, eosinophils, and basophils [2,6]. It has been found that COVID-19 patients have very low levels of NK cells in their blood [10]. Taking lower levels of NK cells into consideration, researchers at Seattle Research Institute in collaboration with Celularity (cell therapeutics company), USA are trying out a potential new therapy, infusing patients with NK cells (CYNK-001), which would be very helpful for combating the virus (NCT04365101). Therefore providing patients with effective supplements of NK cells may help thwart the disease more efficiently. Additionally, isolation and short term expansion of SARS-CoV-2 specific T cells and their use as the cellular drug could be an efficient treatment option for COVID-19.
In most severe patients, the SARS-CoV-2 infection is associated with a lethal immuno-pathological event termed as ‘cytokine storm’, which can be characterized as increased plasma concentration of cytokines like IL-6, IL-1, IL-2, IL-8, IL-17, G-CSF, GM-CSF, IP10, MCP1, MIP1α and TNFα [1,11–13]. From a recent meta-analysis, IL-6 levels reported three-fold higher in COVID-19 patients that requiring ICU care and suggested clinical indicators disease severity [14]. A multicenter, randomized clinical study has been conducted, to evaluate the efficacy and safety of tocilizumab (IL-6 receptor-targeted monoclonal antibody), and reported a quick recovery in clinical symptoms in 21 severe COVID-19 patients (ChiCTR2000029765). Similarly, anti-TNFα antibodies like infliximab or adalimumab, have a well-established safety profile and maybe a potentially effective therapy to treat COVID-19. The blockage of IL-17 might also prove beneficial in COVID-19 patients as it has been shown promising involvement in chronic inflammation [15] and could be further investigated.
Interestingly, SARS-CoV-2 showed a high replication rate and a lower induction of host interferon in human lungs when compared to SARS-CoV [16]. Further, it has been reported that deficiency or low activity of type-I interferon (IFN) is associated with high blood viral load of SARS-CoV-2 in COVID-19 patients and inversely related to the NFĸB-driven inflammatory response that results in increased levels of IL-6 and TNF-α [17]. Based on the evidence, direct administration of IFN and anti-inflammatory host-directed therapies targeting IL-6 and TNF-α might potentially reduce the severe disease symptoms in COVID-19 patients, thus have been suggested for urgent trials [18,19].
Host-directed therapies using mesenchymal stem cells (MSCs) have been shown to prevent the cytokine storm and repair pulmonary cell damage by promoting alveolar fluid clearance in COVID-19 patients [20]. A recent study, based on MSC transplantation in COVID-19 patients, has shown significant improvement in clinical symptoms of all the patients [21].
In severe condition, COVID-19 develops ARDS which leads to the thrombosis, anti-inflammatory function of endothelial cells, coagulopathy, complement in platelet activation, and ultimately disseminated intravascular coagulation (DIC) syndrome [22]. In this effect, anticoagulant therapy, primarily by low molecular weight heparin (LMWH) has been reported with a decreased mortality in COVID-19 patients [23]. Similarly, eculizumab, a human monoclonal antibody that designed to bind and inhibit terminal complement protein C5, is being investigated in a cohort multiple randomized controlled trials (cmRCT) (NCT04346797 and NCT04355494).
Additionally, vascular leakage and pulmonary edema are also common in severe COVID-19 patients. A clinical trial (NCT04342897) revealing the circulating levels of angiopoietin 2 and its correlation with pulmonary edema and mortality in ARDS associated COVID-19 patients that might be a potential host-directed therapy. Further, bevacizumab, a monoclonal anti-VEGF antibody that binds to VEGF and neutralizes its vessel-permeabilizing effect in COVID-19 patients is also under clinical trials (NCT04344782, NCT04275414, and NCT04305106). Host-directed therapies using LMWH, fondaparinux, betrixaban, and rivaroxaban have been suggested at prophylaxis doses in DIC associated COVID-19 patients [24,25].
Anti-inflammatory drugs are another potential option that has been reported as efficient candidates for host-directed therapies in infectious diseases [26,27]. A timely anti-inflammatory treatment initiated at the right time might helpful in COVID-19 management and can also be designed for the individual patient [28]. Dexamethasone, an anti-inflammatory corticosteroid, recently, reported having protective outcomes in COVID-19 patients with ARDS in a multicentre, randomized, controlled clinical trial [29,30]. Further, FDA approved drugs including baricitinib, fedratinib, and ruxolitinib, are janus kinase inhibitors and suggested as potential drugs for the treatment of COVID-19 [31,32]. Being strong anti-inflammatory and suppose to reduce the consequences of enhanced levels of cytokines, these drugs might be used as potential host-directed therapy for COVID-19.
In conclusion, host-directed therapies (Figure 1) may serve a strategic better option to treat COVID-19 when there is no specific drug or vaccine available at present.
Figure 1.
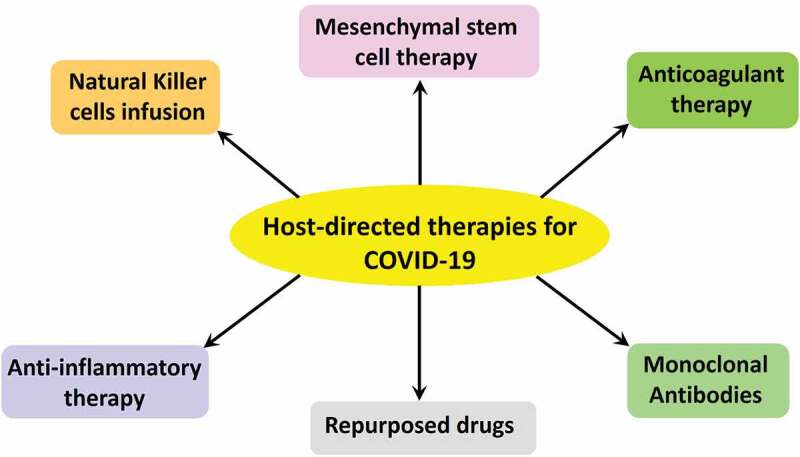
Different host-directed therapies for the treatment of COVID-19.
Acknowledgments
The authors apologize to all the researchers whose work they cannot cite here owing to space constraints.
Declaration of interest
The authors have no relevant affiliations or financial involvement with any organization or entity with a financial interest in or financial conflict with the subject matter or materials discussed in the manuscript. This includes employment, consultancies, honoraria, stock ownership or options, expert testimony, grants or patents received or pending, or royalties.
Reviewer disclosures
Peer reviewers on this manuscript have no relevant financial relationships or otherwise to disclose.
References
Papers of special note have been highlighted as either of interest (•) or of considerable interest (••) to readers.
- 1.Huang C, Wang Y, Li X, et al. Clinical features of patients infected with 2019 Novel Coronavirus in Wuhan, China. Lancet. 2020;395(10223):497–506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Xu Z, Shi L, Wang Y, et al. Pathological findings of COVID-19 associated with acute respiratory distress syndrome. Lancet Respir Med. 2020;8:420–422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Dhama K, Khan S, Tiwari R, et al. Coronavirus Disease 2019–COVID-19. Clin Microbiol Rev. 2020;33(4):e00028–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Sungnak W, Huang N, Bécavin C, et al. SARS-CoV-2 entry factors are highly expressed in nasal epithelial cells together with innate immune genes. Nat Med. 2020;26:681–687. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Mason RJ. Pathogenesis of COVID-19 from a Cell Biology Perspective. Eur Respir J. 2020;55(4):2000607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Dhama K, Patel SK, Pathak M, et al. An update on SARS-CoV-2/COVID-19 with particular reference to its clinical pathology, pathogenesis, immunopathology and mitigation strategies. Travel Med Infect Dis. 2020:101755 DOI: 10.1016/j.tmaid.2020.101755. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wang D, Hu B, Hu C, et al. Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus-infected pneumonia in Wuhan, China. JAMA. 2020;323:1061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Yao H, Lu X, Chen Q, et al. Patient-derived mutations impact pathogenicity of SARS-CoV-2. medRxiv. 2020. April 14;20060160 DOI: 10.1101/2020.04.14.20060160. [DOI] [Google Scholar]
- 9.Zumla A, Chan JFW, Azhar EI, et al. Coronaviruses-drug discovery and therapeutic options. Nat Rev Drug Discov. 2016;15:327–347. [DOI] [PMC free article] [PubMed] [Google Scholar]; • Detailed article providing the epidemiology, clinical features, management strategies and challenges in current treatment option for COVID-19 along with the shedding a light on development of anti-CoV therapeutics.
- 10.Zheng M, Gao Y, Wang G, et al. Functional exhaustion of antiviral lymphocytes in COVID-19 patients. Cell Mol Immunol. 2020. DOI: 10.1038/s41423-020-0402-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hui DSC, Zumla A.. Severe acute respiratory syndrome: historical, epidemiologic, and clinical features. Infect Dis Clin North Am. 2019;33:869–889. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Li G, Fan Y, Lai Y, et al. Coronavirus infections and immune responses. J Med Virol. 2020. DOI: 10.1002/jmv.25685. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Zumla A, Hui DS, Azhar EI, et al. Reducing mortality from 2019-NCoV: host-directed therapies should be an option. Lancet. 2020;395(10224):e35-e36. [DOI] [PMC free article] [PubMed] [Google Scholar]; • First article providing hints regarding importance of host-directed therapies for the treatment of COVID-19.
- 14.Xu L, Yaqian M, Chen G. Risk factors for severe corona virus disease 2019 (COVID-19) patients: a systematic review and meta analysis. medRxiv. 2020. DOI: 10.1101/2020.03.30.20047415 [DOI] [Google Scholar]
- 15.Isailovic N, Daigo K, Mantovani A, et al. Interleukin-17 and innate immunity in infections and chronic inflammation. J Autoimmun. 2015;60:1–11. [DOI] [PubMed] [Google Scholar]
- 16.Chu H, Chan JFW, Wang Y, et al. Comparative replication and immune activation profiles of SARS-CoV-2 and SARS-CoV in human lungs: an ex vivo study with implications for the pathogenesis of COVID-19. Clin Infect Dis. 2020. DOI: 10.1093/cid/ciaa410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hadjadj J, Yatim N, Barnabei L, et al. Impaired type I interferon activity and exacerbated inflammatory responses in severe Covid-19 patients. medRxiv. 2020. DOI: 10.1101/2020.04.19.20068015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Feldmann M, Maini RN, Woody JN, et al. Trials of anti-tumour necrosis factor therapy for COVID-19 are urgently needed. Lancet. 2020;395:1407–1409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Xu X, Han M, Li T, et al. Effective treatment of severe COVID-19 patients with tocilizumab. Proc Natl Acad Sci U S A. 2020;117:10970–10975. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Shetty AK. Mesenchymal stem cell infusion shows promise for combating coronavirus (COVID-19)- induced pneumonia. Aging Dis. 2020;11(2):462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Leng Z, Zhu R, Hou W, et al. Transplantation of ACE2- mesenchymal stem cells improves the outcome of patients with COVID-19 pneumonia. Aging Dis. 2020;11(2):216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Han H, Yang L, Liu R, et al. Prominent changes in blood coagulation of patients with SARS-CoV-2 infection. Clin Chem Lab Med. 2020;58:1116–1120. [DOI] [PubMed] [Google Scholar]
- 23.Tang N, Bai H, Chen X, et al. Anticoagulant Treatment Is Associated with Decreased Mortality in Severe Coronavirus Disease 2019 Patients with Coagulopathy. J Thromb Haemost. 2020. DOI: 10.1111/jth.14817 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Marietta M, Ageno W, Artoni A, et al. COVID-19 and haemostasis: a position paper from Italian society on thrombosis and haemostasis (SISET). Blood Transfus. 2020. DOI: 10.2450/2020.0083-20 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Becker RC. COVID-19 update: covid-19-associated coagulopathy. J Thromb Thrombolysis. 2020;50(1):54–67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Baindara P. Host-directed therapies to combat tuberculosis and associated non-communicable diseases. Microb Pathog. 2019;130:156–168. [DOI] [PubMed] [Google Scholar]; • Detailed review explaining the importance of host-directed therapies for the treatment of tuberculosis and associated noncommunicable diseases.
- 27.Kaufmann SHE, Dorhoi A, Hotchkiss RS, et al. Host-directed therapies for bacterial and viral infections. Nat Rev Drug Discov. 2018;17:35–56. [DOI] [PMC free article] [PubMed] [Google Scholar]; • Detailed review suggesting the potential of host-directed therapies for bacterial and viral infectious diseases.
- 28.Zhang W, Zhao Y, Zhang F, et al. The use of anti-inflammatory drugs in the treatment of people with severe coronavirus disease 2019 (COVID-19): the experience of clinical immunologists from China. Clin Immunol. 2020;214:108393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Villar J, Ferrando C, Martínez D, et al. Dexamethasone treatment for the acute respiratory distress syndrome: a multicentre, randomised controlled trial. Lancet Respir Med. 2020;8(3):267–276. [DOI] [PubMed] [Google Scholar]
- 30.Horby P, Lim WS, Emberson J, et al. Dexamethasone for COVID-19-preliminary report effect of dexamethasone in hospitalized patients with COVID-19 - preliminary report. medRxiv. 2020. DOI: 10.1101/2020.06.22.20137273. [DOI] [Google Scholar]
- 31.Stebbing J, Phelan A, Griffin I, et al. COVID-19: combining antiviral and anti-inflammatory treatments. Lancet Infect Dis. 2020;20(4):400–402. [DOI] [PMC free article] [PubMed] [Google Scholar]; • Interesting article suggesting combination of antiviral and anti-inflammatory therapies to mitigate the COVID-19.
- 32.Richardson P, Griffin I, Tucker C, et al. Baricitinib as potential treatment for 2019-NCoV acute respiratory disease. Lancet. 2020;395:e30-e31. [DOI] [PMC free article] [PubMed] [Google Scholar]


