Abstract
Coronavirus disease 2019 (COVID-19) has posed an unparalleled challenge to the medical communities and patients worldwide. This is the third coronavirus pandemic of the decade and worst so far in terms of the number of patients affected and related deaths. Although COVID-19 is a systemic illness, the respiratory system is obvious to be involved first, and takes most of the brunt of SARS-CoV-2 infection. Common upper and lower respiratory presentations could be sore throat, consolidation, ground glass opacities, and acute respiratory distress syndrome in severe cases. Pneumothorax, pneumomediastinum are uncommon clinical findings in association with COVID-19. We hereby report a rare case of spontaneous pneumomediastinum with a synchronous pneumopericardium.
Case description
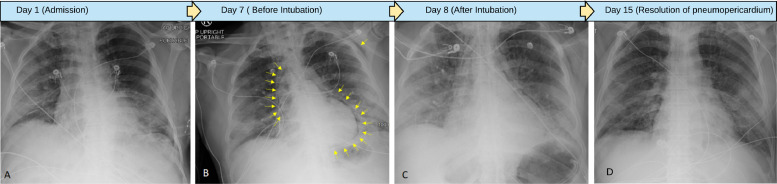
This 61-year-old male, nonsmoker with past medical history significant for hypertension presented to the hospital with fever, and short of breath for one week. At presentation to emergency room, his vitals were: Temperature 100.8 F, pulse 90/min, blood pressure 147/80 mmHg, respiratory rate 19/min, SpO2 96% on 2 liters O2 through nasal canula. Chest X ray showed bilateral peripheral patchy airspace opacities (Fig. 1 A). Suspecting COVID-19 pneumonia, he was put in airborne and contact precautions. His laboratory tests showed a C-reactive protein concentration of 136 mg/L (normal range 0·00–4.9 mg/L), D-dimer value-2.90 mg/L (<0.5 mg/L), serum ferritin-2539 ng/ml (30-400). Complete blood count showed elevated leukocytes (11,400 cells per μL [normal range 3900–1100 per μL]), lymphocyte count 900 [700–4500 cells per μL]). His nasopharyngeal swab for RT PCR for COVID-19 was sent which came back positive. Patient gradually started deteriorating with worsening hypoxia, increased work of breathing and requiring high level of oxygen. He was given remdesevir intravenously for 5 days and one unit of plasma therapy. The patient was also tested for other respiratory viruses like influenza A and B viruses, respiratory syncytial virus which were negative.
Fig. 1.
A. Chest X ray showing bilateral peripheral patchy airspace opacities
Fig. 1B. Chest X ray showing new air tracking along the pericardium and subcutaneous tissue
Fig. 1C. Chest X ray (post intubation) showing mild resolution of the pneumopericardium.
Fig. 1D. Chest X ray at follow up showing resolution of pneumomediastinum and pneumopericardium.
On day 7 of hospital stay, patient started worsening acutely with increase work of breathing. He was switched from high flow to BiPAP to support for his worsening breathing efforts and hypoxia. A repeat chest X ray showed pneumomediastinum and pneumopericardium (Fig. 1B). Patient continued to have worsening breathlessness, and some chest discomfort. Clinical Examination also suggested evidence of subcutaneous emphysema. A decision was made to intubate the patient and a repeat chest X ray showed mild resolution of pneumomediastinum (Fig. 1C). Patient subsequently had followed up imaging studies which showed resolution of the pneumomediastinum and pneumopericardium (Fig. 1D). He received tocilizumab therapy (8 mg/kg body weight), however soon succumbed to illness.
Discussion
Most of the patients presenting with COVID-19 have a mild disease.1 Only small percentage of patients present with severe form with hypoxia, dyspnea, and >50% lung involvement. A further smaller percentage progress to advanced illness, with cytokine storm syndrome, acute respiratory distress syndrome and death.2
Wali et al recently reported 5 cases of pneumomediastinum following intubation in COVID-19.3 The development of pneumomediastinum from the time of tracheal intubation ranged from 4 hours to 14 days. Four patients also had subcutaneous emphysema. Our patient also had developed subcutaneous emphysema along with pneumopericardium and pneumomediastinum. Wali et al suggested the increased risk of alveolar damage, tracheobronchial injury, and higher ventilation pressures as the possible mechanisms of development of pneumomediastinum. Three out of the five patients reported by Wali et al survived. Unlike Wali et al's case, our patient developed spontaneous pneumomediastinum and pneumopericardium without any direct trauma like intubation. The possible explanation of spontaneous pneumomediastinum can be explained by Macklin's phenomenon.4 This phenomenon is defined as the tracking of alveolar air from ruptured alveoli along peri-bronchial vascular sheaths towards the mediastinum and pericardium. Wang et al reported a single patient who developed combination of pulmonary pathologies with spontaneous pneumothorax, pneumomediastinum and subcutaneous emphysema at the same time.5
Spontaneous pneumopericardium is rarer than pneumomediastinum and so far, has not been reported in COVID-19. In past, individuals report of pneumopericardium after Whipple Procedure, thymic surgery, and lung transplantation.6, 7, 8 Drug abusers are exposed to variety of complications related to cardiovascular and pulmonary system.9 , 10 An interesting case of spontaneous pneumopericardium secondary to cannabinoid hyperemesis syndrome was reported by Hansen et al.11
Conclusion
Our case endorses for the fact that any acute worsening in the clinical picture of the patient with rapid oxygen desaturation in a COVID-19 patient should be thoroughly evaluated and possibility of spontaneous pneumothorax, pneumomediastinum, and pneumopericardium should be considered n addition to other common differentials like worsening pneumonia, flash pulmonary edema, and cardiac tamponade.12, 13, 14
Ethical statement
The article doesn't contain the participation of any human being and animal.
Verification
All authors have seen the manuscript and agree to the content and data. All the authors played a significant role in the paper
Declaration of Competing Interest
Authors have no conflicts of interest to declare.
References
- 1.Sahu K., Kumar R. Current perspective on pandemic of COVID-19 in the United States. J Fam Med Prim Care. 2020 May 20;9(4):1784. doi: 10.4103/jfmpc.jfmpc_424_20. http://www.jfmpc.com/text.asp?2020/9/4/1784/283431 [Internet]. 2020 [citedAvailable from. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Lal A., Mishra A.K., Sahu K.K. CT chest findings in coronavirus disease-19 (COVID-19) J Formos Med Assoc. 2020 doi: 10.1016/j.jfma.2020.03.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Wali A., Rizzo V., Bille A., Routledge T., Chambers A. Pneumomediastinum following intubation in COVID-19 patients: a case series [published online ahead of print, 2020 May 6] Anaesthesia. 2020 doi: 10.1111/anae.15113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Wintermark M., Schnyder P. The Macklin effect: a frequent etiology for pneumomediastinum in severe blunt chest trauma. Chest. 2001;120(2):543‐547. doi: 10.1378/chest.120.2.543. [DOI] [PubMed] [Google Scholar]
- 5.Wang W., Gao R., Zheng Y., Jiang L. COVID-19 with spontaneous pneumothorax,pneumomediastinum and subcutaneous emphysema [published online ahead of print, 2020 Apr 25] J Travel Med. 2020;27(5) doi: 10.1093/jtm/taaa062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Stassen J., Frederiks P. Late onset pneumopericardium after lung transplantation [published online ahead of print, 2020 Apr 21] Acta Cardiol. 2020:1‐2. doi: 10.1080/00015385.2020.1756054. [DOI] [PubMed] [Google Scholar]
- 7.Vrakopoulou G.Z., Michalopoulou V., Kormentza C.E. Pneumomediastinum and pneumopericardium 11 days after Whipple procedure. A case report and review if the literature [published online ahead of print, 2020 May 8] Int J Surg Case Rep. 2020;71:27‐29. doi: 10.1016/j.ijscr.2020.04.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Yamamoto K, Sawada T, Kuwahara M, Yamamoto S. Kyobu Geka. 2020;73(2):124‐126. [PubMed]
- 9.Sahu K.K., Mishra A.K., Naraghi L. Erythema ab igne as a complication of cannabinoid hyperemesis syndrome. BMJ Case Rep. 2019;12(1) doi: 10.1136/bcr-2018-227836. Published 2019 Jan 29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Sahu K.K., Tsitsilianos N., Mishra A.K., Suramaethakul N., Abraham G. Neck abscess secondary to pocket shot intravenous drug abuse. BMJ Case Rep. 2020;13(3) doi: 10.1136/bcr-2019-234033. Published 2020 Mar 18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hansen G.M. Asymptomatic pneumopericardium in a young male cannabis smoker Ugeskr Laeger. 2020;182(12):V12190719. [PubMed]
- 12.Lal A., Mishra A.K., Sahu K.K., Noreldin M. Spontaneous pneumomediastinum: rare complication of tracheomalacia. Arch Bronconeumol. 2020;56(3):185‐186. doi: 10.1016/j.arbres.2019.09.017. [DOI] [PubMed] [Google Scholar]
- 13.Sahu K.K., Sherif A.A., Mishra A.K., Vyas S., George S.V. Perineal ulcer: a rare cause of extensive subcutaneous emphysema. BMJ Case Rep. 2019;12(4) doi: 10.1136/bcr-2019-229918. Published 2019 Apr 20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Dalia T., Masoomi R., Sahu K.K., Gupta K. Cardiac tamponade causing severe reversible hyponatraemia. BMJ Case Rep. 2018;2018 doi: 10.1136/bcr-2017-222949. Published 2018 Jan 3. [DOI] [PMC free article] [PubMed] [Google Scholar]