Abstract
Introduction
In a time of global uncertainty, understanding the psychological health of the American public is imperative. There are no current data on anxiety trends among adults in the United States (US) over time. This study aimed to investigate prevalence of anxiety among US adults from 2008 to 2018.
Methods
Data from the National Survey on Drug Use and Health (NSDUH), which is an annual, cross-sectional survey on substance use and mental health in the US, were analyzed in 2020. Prevalence of past-month anxiety was estimated among those ages ≥18, by survey year from 2008 to 2018. Time trends were tested using logistic regression.
Results
Anxiety increased from 5.12% in 2008 to 6.68% in 2018 (p < 0.0001) among adult Americans. Stratification by age revealed the most notable increase from 7.97% to 14.66% among respondents 18–25 years old (p < 0.001), which was a more rapid increase than among 26–34 and 35–49 year olds (differential time trend p < 0.001). Anxiety did not significantly increase among those ages 50 and older. Anxiety increased more rapidly among those never married and with some college education, relative to their respective counterparts. Apart from age, marital status and education, anxiety increased consistently among sociodemographic groups.
Conclusions
Anxiety is increasing among adults under age 50 in the US, with more rapid increase among young adults. To prepare for a healthier adulthood and given direct and indirect (via 24/7 media) exposure to anxiety-provoking world events, prophylactic measures that can bolster healthy coping responses and/or treatment seeking seem warranted on a broad scale.
Keywords: Anxiety, Nervousness, Mental health, Epidemiology, NSDUH
Highlights
-
•
Anxiety increased from 2008 to 2018 among American adults.
-
•
Nearly 7% of adults and 15% of young adults reported anxiety in 2018.
-
•
Anxiety increased most rapidly among young adults ages 18–25 years old.
-
•
Anxiety did not significantly increase among individuals 50 years old and older.
1. Introduction
Anxiety is associated with greater mortality and may be a stronger predictor of negative health consequences than self-reported illness (Ringbäck Weitoft and Rosén, 2005). Exposure to environmental risk factors for anxiety (e.g., financial strain) are on the rise (American Psychological Association, 2019). The prevalence of depression, suicide and substance use disorders have increased in the United States (US) in recent years (Case and Deaton, 2015; Weinberger et al., 2018). While earlier studies have suggested that certain types of anxiety (e.g., panic attacks) have increased over time (Goodwin, 2003), whether and to what degree anxiety has increased among adults over the past decade is unknown. Obtaining an estimate of whether and among whom anxiety is increasing in the US can provide critical information toward understanding the mental health of the country and may help with planning community-based prevention measures and directing public health and clinical treatment resources to populations in greater need.
The current study aimed to fill this gap in knowledge by investigating trends in the prevalence of past-30-day anxiety among US adults ages ≥18 from 2008 to 2018. The study examined trends in anxiety overall and also by key sociodemographic characteristics in order to examine whether certain sociodemographic subgroups are more vulnerable to increased anxiety over time.
2. Methods
2.1. Study population
Data were drawn from the National Survey on Drug Use and Health (NSDUH) public-use data files. The NSDUH is an annual, cross-sectional survey on substance use and mental health in the US. Data from 2008 through 2018 were concatenated, and a new weight variable was created by dividing the original weight by the number of survey years combined (11 years). More detailed descriptions of the sampling methods and survey techniques can be found elsewhere (Center for Behavioral Health Statistics and Quality, 2018). Sample sizes per year ranged from 37,349–42,697 and response rates ranged from 73.3% to 88.6%. For this study, analyses were conducted in 2020 and restricted to adults (ages ≥18) who responded to the nervousness measure described below (total sample from 2008 to 2018 n = 439,691).
2.2. Measures
Anxiety was quantified using a self-report measure of past-month anxiety. This variable was assessed with the item “how often did you feel nervous during the past 30 days” with five response options: all of the time, most of the time, some of the time, a little of the time, and none of the time. For these analyses, the five response options were recoded into two categories: no anxiety (i.e., none of the time, a little of the time, some of the time) and high anxiety (i.e., most of the time, all of the time). Only participants ages ≥18 were asked this question. To assess mental health treatment, respondents were asked to report whether they received any mental health treatment in the past year (yes/no).
Sociodemographic variables were categorized as follows: age (18–25, 26–34, 35–49, ≥50 years old), race/ethnicity (non-Hispanic White, non-Hispanic Black, Hispanic, other/mixed race), gender (male, female), total annual family household income (<$20,000, $20,000–$49,999, ≥$50,000), marital status (married, widowed/divorced/separated, never married), and educational attainment (less than high school, high school graduate or equivalent, some college, college graduate or above).
2.3. Statistical analysis
First, the prevalence of past-month anxiety and associated standard errors were estimated among the whole adult population, by survey year from 2008 to 2018. Time trends in the prevalence of anxiety were tested using logistic regression with a continuous indicator for survey year used as the linear time trend. These analyses were conducted both unadjusted and adjusted for age, race/ethnicity, gender, family income, marital status, and education. Second, similar time trends were estimated using logistic regressions that further stratified by either age, race/ethnicity, gender, family income, marital status, or education. Similar to above, both unadjusted and adjusted models were estimated. Differential time trends in past-month anxiety between subgroups of each sociodemographic factor of interest were tested via two-way interactions of year x sociodemographic factor. All analyses were preformed incorporating NSDUH sampling weights and controlling for the complex clustered sample using SAS-callable SUDAAN version 11.0.1 (RTI International, Research Triangle Park, NC).
3. Results
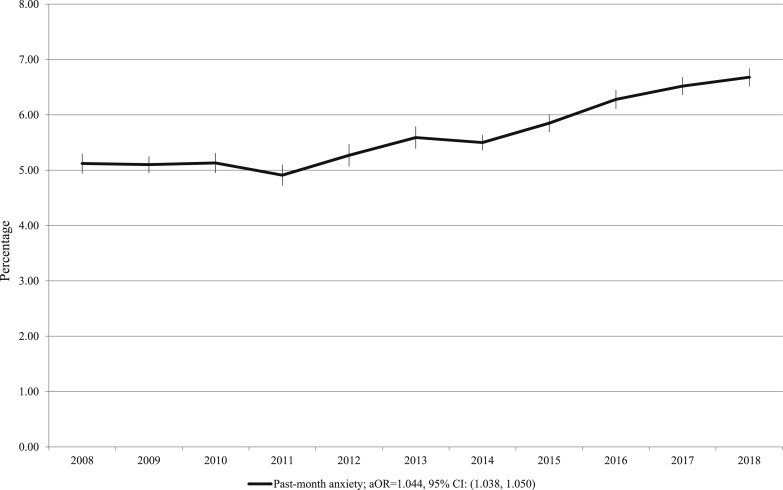
Overall, anxiety increased from 5.12% in 2008 to 6.68% in 2018 among respondents ages 18 and older, a statistically significant linear trend after adjusting for sociodemographics (adjusted odds ratio (aOR) = 1.044, 95% confidence interval (CI)=(1.016, 1.023), p < 0.0001; see Fig. 1 ). In 2018, 43.36% of those with anxiety reported seeking mental health treatment in the past year.
Fig. 1.
Prevalence of past-month anxiety from 2008 to 2018 (NSDUH, US adults ages 18 years and older)a.
Abbreviations: aOR, adjusted odds ratio; CI, confidence interval; NSDUH, National Survey on Drug Use and Health.
aAnxiety was operationalized as self-reported nervousness in the past month most of the time or all of the time.
Note: Odds ratio for calendar yearly linear trend was adjusted for age, gender, race/ethnicity, income, marital status, and educational attainment.
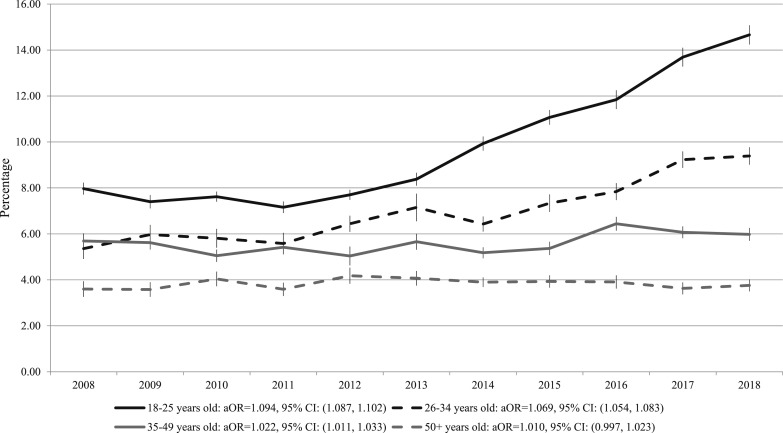
3.1. Age
Notable differences in trends in anxiety were found by age (see Fig. 2 and Supplementary Table 1). Among 18 to 25-year-old respondents, 7.97% in 2008 versus 14.66% in 2018 reported anxiety (p < 0.001). Significant increases were also noted among 26 to 34 and 35 to 49-year-old respondents (ps < 0.001). The increase was significantly more rapid among those ages 18–25 years than any other age group (differential time trend p < 0.001). In contrast to the younger age groups, anxiety remained stable among those ages 50 and older (3.60% in 2008 to 3.76% in 2018, p = 0.128).
Fig. 2.
Prevalence of past-month anxiety by age from 2008 to 2018 (NSDUH, US adults ages 18 years and older)a.
Abbreviations: aOR, adjusted odds ratio; CI, confidence interval; NSDUH, National Survey on Drug Use and Health.
aAnxiety was operationalized as self-reported nervousness in the past month most of the time or all of the time.
Note: Odds ratio for calendar yearly linear trend was adjusted for gender, race/ethnicity, income, marital status, and educational attainment.
3.2. Race/ethnicity
Anxiety increased among non-Hispanic White adults (from 4.98% in 2008 to 7.06% in 2018, p < 0.001), non-Hispanic Black adults (from 5.24% in 2008 to 5.88% in 2018, p < 0.001), Hispanic adults (from 5.56% in 2008 to 6.29% in 2018, p = 0.001), and other/mixed race adults (from 5.48% in 2008 to 5.67% in 2018, p = 0.002). There were no differences in the rate of increase in the prevalence of anxiety by race/ethnicity (see Supplementary Table 2).
3.3. Gender
Anxiety increased among both women (from 5.95% in 2008 to 7.91% in 2018, p < 0.001) and men (from 4.22% in 2008 to 5.35% in 2018, p < 0.001) with no difference in the rate of increase between women and men, though the prevalence was consistently higher among women (see Supplementary Table 3).
3.4. Income
Anxiety increased among all income groups with the highest prevalence among the lowest income group (i.e., total annual income of <$20,000) and no differences in the rate of increase by income group (differential time trend p = 0.775; see Supplementary Table 4).
3.5. Marital status
Anxiety increased among adults who had never been married (from 7.25% in 2008 to 11.48% in 2018, p < 0.001), adults who were married (from 3.76% in 2008 to 4.01% in 2018, p = 0.001), and among adults who were widowed, divorced, or separated (from 6.13% in 2008 to 6.61% in 2018, p = 0.001). The increases in anxiety over time among those never married was significantly more rapid than the increase among those who were married (differential time trend p < 0.001; see Supplementary Table 5), and never married adults reported prevalences of anxiety that were approximately more than two times higher than married adults in every year of the study.
3.6. Education
Anxiety increased among all education groups and the most rapid increase in anxiety was seen among those with some college (from 5.16% in 2008 to 7.47% in 2018, aOR = 1.062 (1.050, 1.073); see Supplementary Table 6). Compared to those without a high school diploma, all other education groups demonstrated significantly more rapid increases in anxiety (differential time trend p < 0.001). Notably, the prevalence of anxiety was higher among those without a high school diploma than other groups across the time period (e.g., 8.74% versus 7.48% for high school graduates, 7.47% for those with some college, and 4.48% for college graduates in 2018).
4. Discussion
Overall, our results are consistent with and extend prior findings that mental health has worsened in the US by showing that anxiety, too, has broadly increased among adults in the US over the past decade. Anxiety appears most common among young adults and has increased more rapidly among 18 to 25-year-olds than among any other age group. Anxiety also increased more rapidly among those never married versus married and among those with a high school diploma or some college versus those who did not complete high school. Anxiety increased consistently across racial/ethnic, gender and income subgroups. Adults over age 50 was the only demographic subgroup among whom anxiety did not change from 2008 to 2018.
The overall increase in anxiety in the US population was broad and consistent across sociodemographic groups, suggesting that large-scale public health approaches to mitigate anxiety may be needed, in addition to outreach and increasing accessibility of mental health services. In terms of education, the increase in anxiety was slower among those who did not complete high school versus those with higher formal education. Of all subgroups, unmarried adults and young adults showed the most rapid increases in anxiety. Being married has been consistently associated with health benefits (Curtin and Tejada-Vera, 2019; Kaplan and Kronick, 2006; Rendall et al., 2011). These findings may relate to many factors including differences in social isolation, social support and financial stability (Cacioppo et al., 2014; Holt-Lunstad et al., 2015; Petitte et al., 2015). Some data suggest a link between loneliness and anxiety (Igbokwe et al., 2020), though there is little research on the relationship between social isolation and anxiety. Especially considering extended social isolation across the world due to the COVID-19 pandemic, this is an issue that may gain even more salience in protecting the mental health of the country (Elran-Barak and Mozeikov, 2020).
Anxiety is most common and has increased most rapidly among young adults. Anxious temperament and subclinical anxiety earlier in life is associated with increased risk of subsequent onset of anxiety disorders, depression, substance use disorders and physical health problems (e.g., Bittner et al., 2004; Goodwin, 2002; Goodwin et al., 2004a, b; Olafiranye et al., 2011; Ringbäck Weitoft and Rosén, 2005; Roy-Byrne et al., 2008; Taha et al., 2014; Wittchen et al., 2003). Young adulthood is the key period of vulnerability for the onset of these conditions. Therefore, increasing anxiety in this vulnerable group would be expected to have a greater impact on longer-term mental health and functional outcomes than increases in anxiety in older age groups. In addition, anxiety or stress has been shown to influence brain development, which is not completed until approximately age 25 (e.g., McEwen, 2011; Piccolo and Noble, 2018; Saleh et al., 2017). Increased persistent anxiety among young adults therefore could have long-term impact on academic, psychological and social development. Further, the explosion of social media, which is associated with increased anxiety and depression among young people, may be a contributing factor to the increase in anxiety over time, especially after 2011 (Barthorpe et al., 2020; Hollis et al., 2020; Riehm et al., 2019).
On a population level, our findings are consistent with recent data from Sweden reporting that adults, and young adults in particular, experienced an increase in poor sleep, stress and poorer general health from 2000 to 2016 (Blom et al., 2020). Data from US adults also suggest increased levels of stress, with work and money articulated as the most common reasons for anxiety (American Psychological Association, 2014, 2016). The time frame of the current study included the 2016 presidential election, which was reported by more than half of US adults, including more than half of Millennials (ages 20 to 35), as a significant source of stress (American Psychological Association, 2017; Hoyt et al., 2018; Zeiders et al., 2019). No direct relationship between specific events and changes in anxiety can be drawn from this study. Therefore, similar to findings regarding increases in mental health problems and the 2008 financial crisis (e.g., Case and Deaton, 2015), any connection between changes in anxiety and the effect of national events on a population level would be speculative but may be important to consider in individual-level clinical efforts to address and reduce anxiety. Such relationships may be worthy of consideration in both public health and clinical planning to address the increasing anxiety that appears widespread in the US, especially among young adults. Young people are confronting more potentially anxiety-provoking world events than prior generations, and exposure to such events is now pervasive with access to 24/7 media.
While symptoms of anxiety are associated with increased likelihood of subsequent anxiety disorders and depression, treatment for subclinical anxiety has also been shown to reduce the risk of these outcomes (Goodwin and Gorman, 2002; Goodwin and Olfson, 2001). The assessment of anxiety in the current study (self-reported nervousness) is not diagnostic of either subclinical or clinical anxiety, but the finding that over 40% of those classified as having anxiety in these analyses (i.e., those reporting nervousness most or all of the time) reported past-year treatment suggests that their anxiety was related to distress or impairment, given that a minority of individuals with anxiety are seen for treatment in the US. Treatment for anxiety is delayed in the vast majority of cases (Iza et al., 2013; Kessler et al., 1998), and most anxiety symptoms or disorders go untreated due to various issues including, but not limited to, lack of awareness of symptoms and effectiveness of treatment, stigma and lack of parity in mental health coverage (Christiana et al., 2000; Wang et al., 2004).
4.1. Limitations
Limitations of this study must be considered when interpreting these results. First, although technically synonymous with “anxiety,” “nervousness” is one expression of anxiety and neither encompasses all types of anxiety nor is reflective of a clinically diagnosed anxiety disorder. Yet, in light of the fact that a substantial percentage of respondents with anxiety reported seeking mental health treatment—on par with those with mental health problems who receive specialized treatment—supports the likelihood that this variable is capturing clinically significant anxiety (Olfson et al., 2019). There is a relative paucity of anxiety measures in national surveys assessed consistently over time. To our knowledge, this is the only measure that could be considered an indicator of anxiety that has been assessed consistently over the past decade in a nationally representative sample. Second, it is possible that the observed increase in anxiety is due to differences in reporting related to decreasing stigma associated with mental disorders. However, it seems less likely that differences in age groups and other sociodemographics would be observed were that the case, and the fact that “nervousness” is not a disorder seems to reduce the likelihood that this is the sole reason for this finding, though it is possible. Third, NSDUH data are repeated cross-sectional samples and longitudinal data would be important for examining changes in anxiety, changes in variables potentially associated with anxiety, and the timing of changes in anxiety and associated variables among individuals. Finally, while this study was designed to examine sociodemographic differences in anxiety over time, there may be other variables associated with anxiety that may be useful to identify vulnerable subgroups.
5. Conclusions
The results from this study suggest poorer mental health in the US in terms of increasing anxiety overall and among most sociodemographic subgroups over the past 11 years. These findings should be considered in conjunction with other data that show increasing mental health problems of other types (e.g., depression), as well as the role of anxiety as a precursor to or indicator of the severity of co-occurring mental health problems. Focusing resources on reducing anxiety, especially among young adults, is a cost-effective clinical and public health approach to stemming the tide of this problem; this would set the foundation for a healthier society in the future, as young adults age and adolescents reach adulthood.
Declaration of competing interest
None declared.
Acknowledgement
The research presented in this paper is that of the authors and does not reflect the official policy of the National Institutes of Health (NIH) or National Institute on Drug Abuse (NIDA).
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.jpsychires.2020.08.014.
Funding
Funding was provided by grant DA20892 to Dr. Goodwin from the NIH/NIDA. The funding organization had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication.
Contributors
Dr. Goodwin conceived the study aims, Drs. Goodwin, Weinberger and Kim designed the analytic plan and Dr. Kim conducted the data analysis. All authors contributed to interpretation of the data, as well as drafting the manuscript and/or critically revising it for important intellectual content. All authors read and approved the final version of the submitted manuscript. All authors agree that they are accountable for all aspects of the work.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- American Psychological Association . Stress in America™ Survey. American Psychological Association; Washington, DC: 2014. Stress in America: are teens adopting adults' stress habits? [Google Scholar]
- American Psychological Association . Stress in AmericaTM Survey. American Psychological Association; Washington, DC: 2016. Stress in America: the impact of discrimination. [Google Scholar]
- American Psychological Association . Stress in America™ Survey. American Psychological Association; Washington, DC: 2017. Stress in America: coping with change. [Google Scholar]
- American Psychological Association . Stress in America™ Survey. American Psychological Association; Washington, DC: 2019. Stress in America: stress and current events. [Google Scholar]
- Barthorpe A., Winstone L., Mars B., Moran P. Is social media screen time really associated with poor adolescent mental health? A time use diary study. J. Affect. Disord. Advance online publication. 2020 doi: 10.1016/j.jad.2020.05.106. [DOI] [PubMed] [Google Scholar]
- Bittner A., Goodwin R.D., Wittchen H.U., Beesdo K., Hofler M., Lieb R. What characteristics of primary anxiety disorders predict subsequent major depressive disorder? J. Clin. Psychiatr. 2004;65(5):618–626. doi: 10.4088/jcp.v65n0505. quiz 730. [DOI] [PubMed] [Google Scholar]
- Blom V., Kallings L.V., Ekblom B., Wallin P., Andersson G., Hemmingsson E., Ekblom O., Soderling J., Ekblom Bak E. Self-reported general health, overall and work-related stress, loneliness, and sleeping problems in 335,625 Swedish adults from 2000 to 2016. Int. J. Environ. Res. Publ. Health. 2020;17(2) doi: 10.3390/ijerph17020511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cacioppo S., Capitanio J.P., Cacioppo J.T. Toward a neurology of loneliness. Psychol. Bull. 2014;140(6):1464–1504. doi: 10.1037/a0037618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Case A., Deaton A. Rising morbidity and mortality in midlife among white non-Hispanic Americans in the 21st century. Proc. Natl. Acad. Sci. U.S.A. 2015;112(49):15078–15083. doi: 10.1073/pnas.1518393112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Center for Behavioral Health Statistics and Quality . Substance Abuse and Mental Health Services Administration; Rockville, MD: 2018. 2017 National Survey on Drug Use and Health: Methodological Summary and Definitions. [Google Scholar]
- Christiana J.M., Gilman S.E., Guardino M., Mickelson K., Morselli P.L., Olfson M., Kessler R.C. Duration between onset and time of obtaining initial treatment among people with anxiety and mood disorders: an international survey of members of mental health patient advocate groups. Psychol. Med. 2000;30(3):693–703. doi: 10.1017/s0033291799002093. [DOI] [PubMed] [Google Scholar]
- Curtin S.C., Tejada-Vera B. Mortality among adults aged 25 and over by marital status: United States, 2010–2017. NCHS Health E-Stat. 2019 [Google Scholar]
- Elran-Barak R., Mozeikov M. One month into the reinforcement of social distancing due to the COVID-19 outbreak: subjective health, health behaviors, and loneliness among people with chronic medical conditions. Int. J. Environ. Res. Publ. Health. 2020;17(15):5403. doi: 10.3390/ijerph17155403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goodwin R.D. Anxiety disorders and the onset of depression among adults in the community. Psychol. Med. 2002;32(6):1121–1124. doi: 10.1017/s0033291702005482. [DOI] [PubMed] [Google Scholar]
- Goodwin R.D. The prevalence of panic attacks in the United States: 1980 to 1995. J. Clin. Epidemiol. 2003;56(9):914–916. doi: 10.1016/s0895-4356(03)00126-4. [DOI] [PubMed] [Google Scholar]
- Goodwin R.D., Fergusson D.M., Horwood L.J. Association between anxiety disorders and substance use disorders among young persons: results of a 21-year longitudinal study. J. Psychiatr. Res. 2004;38(3):295–304. doi: 10.1016/j.jpsychires.2003.09.002. [DOI] [PubMed] [Google Scholar]
- Goodwin R.D., Fergusson D.M., Horwood L.J. Early anxious/withdrawn behaviours predict later internalising disorders. JCPP (J. Child Psychol. Psychiatry) 2004;45(4):874–883. doi: 10.1111/j.1469-7610.2004.00279.x. [DOI] [PubMed] [Google Scholar]
- Goodwin R.D., Gorman J.M. Psychopharmacologic treatment of generalized anxiety disorder and the risk of major depression. Am. J. Psychiatr. 2002;159(11):1935–1937. doi: 10.1176/appi.ajp.159.11.1935. [DOI] [PubMed] [Google Scholar]
- Goodwin R.D., Olfson M. Treatment of panic attack and risk of major depressive disorder in the community. Am. J. Psychiatr. 2001;158(7):1146–1148. doi: 10.1176/appi.ajp.158.7.1146. [DOI] [PubMed] [Google Scholar]
- Hollis C., Livingstone S., Sonuga-Barke E. The role of digital technology in children and young people's mental health–a triple-edged sword? JCPP (J. Child Psychol. Psychiatry) 2020;61(8):837–841. doi: 10.1111/jcpp.13302. [DOI] [PubMed] [Google Scholar]
- Holt-Lunstad J., Smith T.B., Baker M., Harris T., Stephenson D. Loneliness and social isolation as risk factors for mortality: a meta-analytic review. Perspect. Psychol. Sci. 2015;10(2):227–237. doi: 10.1177/1745691614568352. [DOI] [PubMed] [Google Scholar]
- Hoyt L.T., Zeiders K.H., Chaku N., Toomey R.B., Nair R.L. Young adults' psychological and physiological reactions to the 2016 U.S. presidential election. Psychoneuroendocrinology. 2018;92:162–169. doi: 10.1016/j.psyneuen.2018.03.011. [DOI] [PubMed] [Google Scholar]
- Igbokwe C.C., Ejeh V.J., Agbaje O.S., Umoke P.I.C., Iweama C.N., Ozoemena E.L. Prevalence of loneliness and association with depressive and anxiety symptoms among retirees in North central Nigeria: a cross-sectional study. BMC Geriatr. 2020;20(1):153. doi: 10.1186/s12877-020-01561-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Iza M., Olfson M., Vermes D., Hoffer M., Wang S., Blanco C. Probability and predictors of first treatment contact for anxiety disorders in the United States: analysis of data from the National Epidemiologic Survey on Alcohol and Related Conditions (NESARC) J. Clin. Psychiatr. 2013;74(11):1093–1100. doi: 10.4088/JCP.13m08361. [DOI] [PubMed] [Google Scholar]
- Kaplan R.M., Kronick R.G. Marital status and longevity in the United States population. J. Epidemiol. Community Health. 2006;60(9):760–765. doi: 10.1136/jech.2005.037606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler R.C., Olfson M., Berglund P.A. Patterns and predictors of treatment contact after first onset of psychiatric disorders. Am. J. Psychiatr. 1998;155(1):62–69. doi: 10.1176/ajp.155.1.62. [DOI] [PubMed] [Google Scholar]
- McEwen B.S. Effects of stress on the developing brain. Cerebrum. 2011;2011 14-14. [PMC free article] [PubMed] [Google Scholar]
- Olafiranye O., Jean-Louis G., Zizi F., Nunes J., Vincent M. Anxiety and cardiovascular risk: review of epidemiological and clinical evidence. Mind Brain. 2011;2(1):32–37. [PMC free article] [PubMed] [Google Scholar]
- Olfson M., Wang S., Wall M., Marcus S.C., Blanco C. Trends in serious psychological distress and outpatient mental health care of US adults. JAMA Psychiatry. 2019;76(2):152–161. doi: 10.1001/jamapsychiatry.2018.3550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Petitte T., Mallow J., Barnes E., Petrone A., Barr T., Theeke L. A systematic review of loneliness and common chronic physical conditions in adults. Open Psychol. J. 2015;8(Suppl. 2):113–132. doi: 10.2174/1874350101508010113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Piccolo L.R., Noble K.G. Perceived stress is associated with smaller hippocampal volume in adolescence. Psychophysiology. 2018;55(5) doi: 10.1111/psyp.13025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rendall M.S., Weden M.M., Favreault M.M., Waldron H. The protective effect of marriage for survival: a review and update. Demography. 2011;48(2):481–506. doi: 10.1007/s13524-011-0032-5. [DOI] [PubMed] [Google Scholar]
- Riehm K.E., Feder K.A., Tormohlen K.N., Crum R.M., Young A.S., Green K.M., Pacek L.R., La Flair L.N., Mojtabai R. Associations between time spent using social media and internalizing and externalizing problems among US youth. JAMA Psychiatry. 2019;76(12):1266–1273. doi: 10.1001/jamapsychiatry.2019.2325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ringbäck Weitoft G., Rosén M. Is perceived nervousness and anxiety a predictor of premature mortality and severe morbidity? A longitudinal follow up of the Swedish survey of living conditions. J. Epidemiol. Community Health. 2005;59(9):794–798. doi: 10.1136/jech.2005.033076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roy-Byrne P.P., Davidson K.W., Kessler R.C., Asmundson G.J., Goodwin R.D., Kubzansky L., Lydiard R.B., Massie M.J., Katon W., Laden S.K., Stein M.B. Anxiety disorders and comorbid medical illness. Gen. Hosp. Psychiatr. 2008;30(3):208–225. doi: 10.1016/j.genhosppsych.2007.12.006. [DOI] [PubMed] [Google Scholar]
- Saleh A., Potter G.G., McQuoid D.R., Boyd B., Turner R., MacFall J.R., Taylor W.D. Effects of early life stress on depression, cognitive performance and brain morphology. Psychol. Med. 2017;47(1):171–181. doi: 10.1017/S0033291716002403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taha F., Lipsitz J.D., Galea S., Demmer R.T., Talley N.J., Goodwin R.D. Anxiety disorders and risk of self-reported ulcer: a 10-year longitudinal study among US adults. Gen. Hosp. Psychiatr. 2014;36(6):674–679. doi: 10.1016/j.genhosppsych.2014.07.005. [DOI] [PubMed] [Google Scholar]
- Wang P.S., Berglund P.A., Olfson M., Kessler R.C. Delays in initial treatment contact after first onset of a mental disorder. Health Serv. Res. 2004;39(2):393–415. doi: 10.1111/j.1475-6773.2004.00234.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weinberger A.H., Gbedemah M., Martinez A.M., Nash D., Galea S., Goodwin R.D. Trends in depression prevalence in the USA from 2005 to 2015: widening disparities in vulnerable groups. Psychol. Med. 2018;48(8):1308–1315. doi: 10.1017/S0033291717002781. [DOI] [PubMed] [Google Scholar]
- Wittchen H.U., Beesdo K., Bittner A., Goodwin R.D. Depressive episodes--evidence for a causal role of primary anxiety disorders? Eur. Psychiatr. 2003;18(8):384–393. doi: 10.1016/j.eurpsy.2003.10.001. [DOI] [PubMed] [Google Scholar]
- Zeiders K.H., Nair R.L., Hoyt L.T., Pace T.W., Cruze A. Latino early adolescents' psychological and physiological responses during the 2016 US presidential election. Cult. Divers Ethnic Minor. Psychol. 2019;26(2):169–175. doi: 10.1037/cdp0000301. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.