To the Editor:
Patients critically ill with coronavirus disease 2019 (COVID-19) spend significant time on mechanical ventilation and have prolonged hospitalization duration.1 Whether these patients have immediate pulmonary and neurocognitive recovery following discharge is unknown.
Methods
Patients were admitted to the University of Virginia (UVA) Medical Center ICU with COVID-19 and underwent follow-up at the UVA Post-COVID-19 ICU clinic approximately 6 weeks following discharge. Lung function and exercise capacity were assessed by using spirometry, lung volumes, diffusion capacity, and the 6-min walk test. Depression, cognitive function, and insomnia were assessed by using the Patient-Reported Outcomes Measurement Information System Depression 8a-Short Score, the Quality of Life in Neurological Disorders adult cognitive function version 2.0 score, the Montreal Cognitive Assessment (MOCA) score, and the insomnia severity index. The study was approved by the UVA Institutional Review Board.
Results
As of July 30, 2020, a total of 102 patients with COVID-19 were admitted to the UVA ICU. Fifty-nine patients (57.84%) were discharged alive, 22 (21.57%) died, and 21 (20.59%) remained hospitalized. Every discharged patient is contacted to follow up in the UVA Post-ICU COVID-19 clinic. The first patient was seen on June 2, 2020. Twenty-eight of the 29 scheduled patients attended the clinic as of July 30, 2020 (Table 1 ), resulting in a 96% show-rate. The remaining discharged patients are scheduled but have not yet been seen. Seven (25%) and 10 (57.14%) patients self-identified as African American and non-white Hispanic, respectively. The median age was 56 years (interquartile range [IQR], 47.5-65.75 years); 24 patients (85.71%) required mechanical ventilation, and the median number of days on mechanical ventilation was 11 (IQR, 3.25-15 days). The mean Sequential Organ Failure Score, the Acute Physiology and Chronic Health Evaluation II score, and the Simplified Acute Physiology Score II were 6 ± 2.5, 14 ± 6.2, and 32 ± 12.4, respectively. Seventy-five percent were diagnosed with delirium in the ICU. Median ICU and hospital length of stay were 14 (IQR, 6-21.5) days and 22 (IQR, 11.5-31) days, respectively. Two patients were discharged on antipsychotic agents or opiates.
Table 1.
Epidemiologic and Clinical Characteristics of Patients
| Patient No. | Age, y | Sex | Self-Reported Ethnicity | Lowest Po2/ Fio2 | Days on MV | Received Paralysis and Proning | Evidence of Deliriuma | ICU LOS | Hospital LOS | Days From Discharge to Visit | Spirometry | Diffusion Capacity (% Predicted) | 6MWD (m)/ % Predicted | PROMIS Depression 8a T Scoreb | Neuro-QoL Adult Cognitive Function T Scorec | MOCA Scored | Insomnia Severity Indexe | SOFAf/APACHE IIg/SAPS IIh |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 59 | F | African American | 118 | 14 | Yes | Yes | 17 | 32 | 36 | Mixed obstruction and restriction | Reduced (59%) | 362/76% | 38.2 | 40.9 | 26 | NA | 10/15/11 |
| 2 | 54 | M | Hispanic | 128 | 7 | No | Yes | 9 | 13 | 36 | Normal | Normal (97%) | 168/38% | 44.7 | 64.2 | 22 | 15 | 3/8/34 |
| 3 | 67 | M | African American | 212 | 5 | No | No | 6 | 14 | 40 | Normal | Normal (83%) | 390/67% | 44.7 | 50.9 | 27 | NA | 7/22/46 |
| 4 | 74 | F | White | 66 | 15 | No | Yes | 22 | 34 | 41 | Normal | Normal (70%) | 350/78% | 38.2 | 48.3 | 20 | 16 | 3/11/21 |
| 5 | 71 | M | Hispanic | 138 | 3 | No | No | 5 | 15 | 30 | Normal | Normal (99%) | 378/85% | 38.2 | 42.9 | 18 | 7 | 4/13/42 |
| 6 | 75 | M | White | 111 | 27 | Yes | Yes | 38 | 39 | 36 | Unable to perform | Unable to perform | NA | 47.5 | 48.3 | 22 | 22 | 5/25/56 |
| 7 | 69 | M | African American | 150 | 18 | Yes | Yes | 22 | 31 | 40 | Restriction | Reduced (58%) | 327/57% | 38.2 | 50.9 | 18 | 7 | 9/21/52 |
| 8 | 65 | F | Asian Indian | 47 | 15 | Yes | Yes | 17 | 26 | 41 | Obstruction | Unable to perform | 201/46% | 55.1 | 43.9 | 27 | 2 | 8/19/44 |
| 9 | 66 | F | African American | RA | 0 | None | No | 2 | 2 | 43 | Normal | Normal (80%) | 311/87% | 59.4 | 48.3 | 28 | NA | NA |
| 10 | 59 | M | African American | 170 | 7 | No | Yes | 9 | 13 | 40 | Obstruction | Normal (83%) | 352/72% | 38.2 | 48.3 | 29 | 11 | 8/13/33 |
| 11 | 43 | M | Hispanic | 143 | 6 | No | No | 13 | 20 | 35 | Obstruction | Reduced (62%) | 50/1% | 64.9 | 46 | 19 | 19 | 4/4/27 |
| 12 | 30 | F | Hispanic | 42 | 16 | Yes | Yes | 23 | 31 | 38 | Obstruction | Normal (107%) | 345/83% | 56.8 | 56.3 | 18 | 12 | 7/10/15 |
| 13 | 60 | F | Hispanic | NA | 0 | No | No | 3 | 6 | 31 | Restriction | Reduced (67%) | NA | 38.2 | n.a | 23 | 25 (known OSA) | 4/21/35 |
| 14 | 41 | M | Hispanic | 88 | 14 | Yes | Yes | 16 | 23 | 41 | Normal | Normal (115%) | 325/52% | 38.2 | 48.3 | 24 | NA | 8/12/36 |
| 15 | 70 | M | Hispanic | 146 | 15 | No | Yes | 25 | 38 | 40 | Normal | Normal (90%) | 250/59% | 63.9 | 35 | 11 | NA | 8/20/48 |
| 16 | 58 | F | White | 180 | 22 | No | Yes | 23 | 46 | 39 | Normal | Reduced (69%) | 287/54% | 58.5 | 38.9 | 29 | 13 | 7/16/34 |
| 17 | 51 | M | Hispanic | 80 | 12 | Yes | Yes | 18 | 28 | 39 | Restriction | Normal (106%) | 268/50% | 38.2 | 64.2 | 27 | NA | 8/9/23 |
| 18 | 64 | F | African American | 115 | 26 | Yes | yes | 27 | 33 | 40 | Normal | Normal (79%) | 203/52% | 38.2 | 50.9 | 24 | 14 | 7/15/45 |
| 19 | 51 | M | Hispanic | 70 | 10 | Yes | yes | 11 | 19 | 35 | Normal | Normal (85%) | 386/63% | 38.2 | 59 | 21 | 3 | 9/12/27 |
| 20 | 50 | M | White | 92 | 16 | Yes | Yes | 20 | 28 | 42 | Restriction | Reduced (69%) | 325/50% | 55.3 | 44.9 | 26 | 16 | 9/20/38 |
| 21 | 59 | M | Hispanic | 100 | 9 | No | No | 12 | 25 | 44 | Restriction | Reduced (62%) | 326/69% | 37.1 | 64.2 | 23 | 0 | 8/28/38 |
| 22 | 52 | M | Hispanic | 100 | 14 | Yes | Yes | 15 | 21 | 43 | Normal | Normal (114%) | 400/87% | 43.3 | 64.2 | 23 | 1 | 4/12/34 |
| 23 | 51 | F | Hispanic | 200 | 3 | No | Yes | 4 | 6 | 40 | Normal | Normal (103%) | 340/64% | 37.1 | 39.9 | 17 | 10 | 3/12/21 |
| 24 | 39 | M | Hispanic | NA | 0 | No | No | 6 | 11 | 35 | Normal | Normal (86%) | 350/59% | 37.1 | 52.4 | 23 | 0 | 2/6/11 |
| 25 | 47 | F | African American | 138 | 3 | No | No | 4 | 11 | 32 | Normal | Normal (90%) | 304/95% | 49.8 | 47.1 | 29 | 2 | 3/6/33 |
| 26 | 49 | M | Hispanic | 104 | 15 | Yes | Yes | 20 | 27 | 42 | Unable to perform | Normal (110%) | 444/75% | 53.4 | 56.3 | 22 | 2 | 9/13/24 |
| 27 | 36 | F | Hispanic | NA | 0 | No | No | 6 | 9 | 38 | Normal | Normal (114%) | 339/69% | 37.1 | 64.2 | 24 | 3 | 3/11/11 |
| 28 | 44 | M | Hispanic | 95 | 4 | No | No | 7 | 9 | 38 | Normal | Normal (101%) | 418/72% | 43.4 | 52.4 | 19 | 1 | 5/12/29 |
| Mean ± SD | 55.5 ± 11.9 | 118 ± 45 | 10.6 ± 7.7 | 14.3 ± 8.6 | 21.8 ± 11.5 | 38.4 ± 3.6 | 315 ± 85)/63% | 45.4 ± 9.24 | 50.8 ± 8.4 | 23 ± 4 | 9 ± 8 | 6 ± 2.5/14 ± 6.2 /32 ± 12.4 |
6MWD = 6-min walk distance; APACHE = Acute Physiology and Chronic Health Evaluation; F = female; LOS = length of stay; M = male; MOCA = Montreal Cognitive Assessment; MV = mechanical ventilation; NA = not available; Neuro-QoL = Quality of Life in Neurological Disorders; PROMIS = Patient-Reported Outcomes Measurement Information System; RA = room air; SAPS = Simplified Acute Physiology Score; SOFA = Sequential Organ Failure Assessment.
Delirium is assessed by the nursing staff every shift using the Confusion Assessment Method for the ICU.
T score > 45 represents no depression, 40 to 45 represents mild depression, 30 to 40 represents moderate depression, and < 30 represents severe depression.
Neuro-QoL adult cognitive function version 2.0: T score > 45 represents normal cognition, 40 to 45 represents mild cognitive impairment, 30 to 40 represents moderate cognitive impairment, and < 30 represents severe cognitive impairment.
MOCA scores > 25 represent normal cognition; 18 to 25 represent mild cognitive impairment; 10 to 17 represent moderate cognitive impairment; and scores < 10 represent severe cognitive impairment.
Insomnia: scores 0 to 7 represent no clinically significant insomnia; 8 to 14 represent subthreshold insomnia; 15 to 21 represent moderate severity clinical insomnia; and 22 to 28 represent severe clinical insomnia.
Scores on the SAPS II range from 0 to 163; higher scores indicate more severe disease and higher risk of death.
Scores on the APACHE II range from 0 to 71; higher scores indicate more severe disease and higher risk of death.
Scores on the SOFA range from 0 to 24; higher scores indicate more severe disease and higher risk of death.
The median number of days to follow-up in the clinic posthospital discharge was 39.5 (IQR, 36-41 days). Results of prior lung function tests were not available for comparison. At follow-up, 16 patients (61.54%) had normal lung function, four (15.38%) had obstruction, five (19.23%) had restriction, one (3.85%) had mixed obstruction and restriction, and seven (26.92%) had reduced diffusion capacity. The mean 6-min walk distance was 315 ± 85.4 m, and mean percent predicted was 65.5 (IQR, 51.5-76.5). None of the patients required supplemental oxygen.
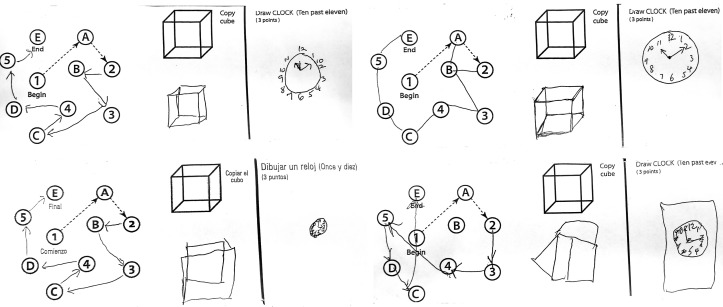
None of the patients had clinically diagnosed depression, cognitive impairment, or insomnia prior to admission. At follow-up, seven patients had mild to moderate depression. Assessment of mild cognitive impairment was more frequent according to MOCA (n = 16 [57.14%]) but not according to the Quality of Life in Neurological Disorders (n = 6 [22%]) score. All but one patient (96%) performed activities of daily life without difficulty. Five of 23 patients who completed the insomnia severity index had moderate to severe insomnia. Detailed patient information is given in Table 1, and Figure 1 shows representative examples of the visuospatial/executive MOCA test.
Figure 1.
Four representative examples of the visuospatial/executive part of the Montreal Cognitive Assessment test. In this component of the test, the patient needs to connect alternating numbers and letters from low to high, copy a three-dimensional cube, and free-draw a clock showing a time of 11:10.
Discussion
To the best of our knowledge, this analysis is the first case series of outpatient follow-up visits for patients who were hospitalized in the ICU with COVID-19. We found a low prevalence of obstruction and restriction, similar to previously published data in ARDS.1 , 2 The prevalence of diffusion impairment in this cohort was lower compared with post-ARDS follow-up.3 The mean 6-min walk distance in the current cohort was higher compared with what has been reported in prior ARDS studies.3 Despite significant dosages for sedation and a high prevalence of delirium in the ICU, the majority of the current patients had no or only mild cognitive impairment at 6 weeks following hospital discharge. This observation, and the fact that only one patient still had difficulties with activities of daily life, differs from previous reports of survivors of critical illness.4 The prevalence of depression and insomnia were comparable with previous post-ICU outcome studies.5 , 6 The majority of the post-ICU clinic patients were African American or Hispanic, which is supportive of recent studies that suggest non-white racial/ethnic groups are severely affected by COVID-19.7
This was a single-center case series, and we do not have sufficient long-term data to assess how these outcomes change over time. The long-term impact of this disease remains unclear but our study suggests the feasibility of an in-person outpatient clinic for post-ICU COVID-19 patients and a low burden of pulmonary and neurocognitive morbidity at immediate follow-up.
Acknowledgments
Other contributions: The authors acknowledge the efforts of Norma Nelson, RN, and Amanda Campbell, RRT, for the help with scheduling follow-up visits and pulmonary function tests.
Footnotes
FINANCIAL/NONFINANCIAL DISCLOSURES: None declared.
References
- 1.Chiumello D., Coppola S., Froio S., Gotti M. What's next after ARDS: long-term outcomes. Respir Care. 2016;61(5):689–699. doi: 10.4187/respcare.04644. [DOI] [PubMed] [Google Scholar]
- 2.Cummings M.J., Baldwin M.R., Abrams D. Epidemiology, clinical course, and outcomes of critically ill adults with COVID-19 in New York City: a prospective cohort study. Lancet. 2020;395(10239):1763–1770. doi: 10.1016/S0140-6736(20)31189-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Herridge M.S., Moss M., Hough C.L. Recovery and outcomes after the acute respiratory distress syndrome (ARDS) in patients and their family caregivers. Intensive Care Med. 2016;42(5):725–738. doi: 10.1007/s00134-016-4321-8. [DOI] [PubMed] [Google Scholar]
- 4.Sevin C.M., Bloom S.L., Jackson J.C., Wang L., Ely E.W., Stollings J.L. Comprehensive care of ICU survivors: development and implementation of an ICU recovery center. J Crit Care. 2018;46:141–148. doi: 10.1016/j.jcrc.2018.02.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Altman M.T., Knauert M.P., Pisani M.A. Sleep disturbance after hospitalization and critical illness: a systematic review. Ann Am Thorac Soc. 2017;14(9):1457–1468. doi: 10.1513/AnnalsATS.201702-148SR. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Jackson J.C., Pandharipande P.P., Girard T.D. Depression, post-traumatic stress disorder, and functional disability in survivors of critical illness in the BRAIN-ICU study: a longitudinal cohort study. Lancet Respir Med. 2014;2(5):369–379. doi: 10.1016/S2213-2600(14)70051-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Martinez D.A., Hinson J.S., Klein E.Y. SARS-CoV-2 positivity rate for Latinos in the Baltimore-Washington, DC region. JAMA. 2020;324(4):392–395. doi: 10.1001/jama.2020.11374. [DOI] [PMC free article] [PubMed] [Google Scholar]