Abstract
PURPOSE:
The purpose is to compare the clinical results of using silk versus nylon sutures for conjunctival autograft suturing in pterygium surgery.
METHODS:
In this prospective, randomized, controlled, clinical trial 50 eyes from 50 patients with primary nasal pterygium were randomized to undergo pterygium surgery with the use of either nylon sutures or silk sutures for conjunctival autograft suturing. Patients were followed up for 6 months. Main outcome measures included recurrence, postoperative discomfort according to a visual analog scale (VAS), graft hyperemia, and graft edema.
RESULTS:
According to the results, there was no significant difference between groups regarding recurrence rate of pterygium (P = 0.72). A significant decrease in the mean VAS discomfort score from day 1 to day 14 was observed in both groups (P = 0.001); postoperative discomfort during the first 2 weeks, was not significantly different between the two groups. At 2 weeks' postoperatively, significantly greater number of nylon sutures remained on the autograft (P = 0.021), some of which were buried and could not be removed.
CONCLUSION:
Both silk and nylon are effective suture materials for autograft suturing in pterygium surgery with similar postoperative discomfort and recurrence rate. Significantly greater number of nylon sutures remains buried on the autograft and could not be removed easily.
Keywords: Conjunctival autograft, nylon, pterygium surgery, silk
Introduction
Pterygium is a wingshaped fibrovascular lesion of the ocular surface, which is associated with chronic sunlight exposure.[1] Cameron's map shows a direct relationship between pterygium prevalence and proximity to the equator (warm and dry climate).[2] Its incidence is more in males with a male to female ratio of 2:1, it is more common in farmers than in city dwellers, and more prevalent in those who do not wear eyeglasses. Elderly patients have the highest prevalence rate, although the highest incidence rate was among much younger age group (20-to 40-year old).[3] Although various surgical procedures have been described for the treatment of pterygium, recurrence remains the main complication of the surgery.[1] Pterygium excision followed by conjunctival autograft has been shown to be a safe and effective procedure for pterygium surgery, with recurrence rates ranging from 2% to 39%[4,5,6,7,8] The suture materials commonly used for conjunctival autograft suturing include polyglactin, silk, and nylon.[9] Silk sutures are nonabsorbable, sterile, nonmutagenic surgical sutures composed of natural proteinaceous silk fibers called fibroin. Silk sutures elicit a minimal acute inflammatory reaction in tissues, which is followed by gradual encapsulation of the suture by fibrous connective tissue. In vivo while silk sutures are not absorbed, progressive degradation of the proteinaceous silk fiber may result in gradual loss of tensile strength over time.[10] Nylon, on the other hand, is a nonabsorbable monofilament suture composed of polyamides, with minimal induction of cellular response and prolonged tensile strength retention.[9,10]
Various suture materials and techniques are employed to secure the autograft including absorbable and nonabsorbable sutures of different diameters. Sutures are placed in interrupted or continuous fashion, with the knots left exposed or buried. Although many reports have surveyed technical modifications and recurrence rates of conjunctival autograft for pterygium surgery, few have compared the use of different suture materials in terms of postoperative patient discomfort. Suture-related complications include postoperative discomfort, infection, prolonged operating time, suture abscesses, buttonholes, pyogenic granuloma, and chronic inflammation.[11]
Many studies have evaluated risk factors for recurrence. Younger age, thicker (6-0 to 8-0) sutures, and untreated postoperative inflammation are known to be risk factors for recurrence. The morphology of pterygium may also affect the recurrence.[12]
The purpose of our randomized, controlled trial was to assess the clinical outcomes of using two different suture materials, silk, and nylon in suturing of conjunctival autograft in pterygium surgery. Our main outcome measures included postoperative discomfort, conjunctival reactions, graft complications as well as the rate of recurrence.
Materials and Methods
In this single-blinded randomized controlled trial 50 eyes from 50 patients with primary pterygium were prospectively recruited. We conducted the study at Khalili Hospital affiliated to Shiraz University of Medical Sciences. Inclusion criteria included patients with primary nasal pterygium aged 18 years or older who were capable to withstand the surgery under local anesthesia. Exclusion criteria were recurrent pterygium, temporal or double-head pterygium, scarred superior conjunctiva, previous surgery involving the superior bulbar conjunctiva, patients with the history of glaucoma, and/or cicatricial ocular surface disease. Patients with systemic diseases such as diabetes, hypertension, and collagen vascular disease were also omitted. The study protocol was approved by our institution ethics committee. We obtained informed consent from all patients.
Randomization with a block randomization list was used to allocate patients to either silk or nylon suture groups. Patients were unaware of the suture material being used, but the surgeon and postoperative assessor were not masked to the assignment. Preoperatively, complete eye examination including Snellen visual acuity measurement, slit-lamp examination, intraocular pressure (IOP) (by Goldman applanation tonometry), fundus examination, slit-lamp photography, and corneal topography was performed for all patients.
During the first examination, pterygium was graded according to the grading system developed by Tan et al.[8] as atrophic (Type 1), with minimal inflammation (Type 2), and with moderate/severe inflammation or showing active growth (Type 3). Unlike Type 1 pterygium, which are nonelevated lesions in which the underlying episcleral vessels could clearly be observed, Type 3 pterygium lesions were elevated and showed straight horizontal vascularization, obscuring the episcleral vessels underneath. All other pterygium lesions were classified as Type 2 if episcleral vessels were partially obscured. The size of pterygium was also measured preoperatively.
All operations performed by a single surgeon (HJ) under topical anesthesia with tetracaine 0.5% eye drops (produced by Sina Darou, Tehran-Iran) that was applied twice at 5-min intervals 10 min before the surgery, supplemented with a subconjunctival anesthetic, 0.5 ml of 2% HCL lidocaine with 1/80,000 epinephrine (Darupakhsh, Tehran-Iran) that was injected subconjunctival beneath the pterygium body at the beginning of the surgery. Then, the pterygium head grasped with forceps and lifted off the cornea, subconjunctival fibrovascular pterygium tissue was dissected with scissors, the bare scleral defect covered with conjunctival autograft harvested from the superior bulbar conjunctiva with careful attention to avoid inclusion of any Tenon's tissue or formation of a conjunctival buttonhole. Autograft was sized accordingly to overlap the edges of the defect by 1 mm horizontally and vertically on each side. The autograft transposed to the scleral defect with limbal part of the graft facing directly to the limbal region of the bare area of the sclera.
Interrupted 8-0 silk sutures or 10-0 nylon sutures placed with four cardinal sutures and three noncardinal sutures. All knots remained unburied.
Postoperatively, all patients received an identical regimen of a topical antibiotic for 1 week and tapering topical steroids tapering within 3 months. The latter included 0.1% betamethasone (Sina Darou, Tehran-Iran) four times daily for 1 month followed by 0.1% fluorometholone (Sina Darou, Tehran, Iran) four times daily for 2 weeks, 3 times daily for 2 weeks, twice daily for 2 weeks, followed by once daily dosage for 2 weeks. Postoperatively, the patients were revisited at the intervals of the end of 1st day, 1st week, 2nd week, 1st month, 2nd month, 3rd month, and 6th month. Sutures removed after 14 days in both groups.
At each postoperative visit, patients were asked to rate their discomfort using a 10-cm visual analog scale (VAS) with one end labeled as “no discomfort” and the other end was labeled as “worst possible discomfort.” Mild pain was given a value of 1–4; moderate pain 5–6; and severe pain 7–10.
Slit-lamp examination was performed to assess the amount of graft hyperemia, edema and flap retraction and premature suture loosening. All of which documented by slit-lamp photography performed at each postoperative examination. Topography was repeated at 1st, 3rd and 6th month postoperatively. The primary outcome revealed the difference in VAS score between the two groups. Secondary outcomes included graft hyperemia, edema and flap retraction and premature suture loosening. Complications such as stitch granuloma, graft dehiscence, and pterygium recurrence were also noted.
Pterygium recurrence defined according to the grading system reported by Prabhasawat et al. was as follows:[7] no recurrence as Grade 1, fine episcleral vessels without fibrous tissue in the surgical area as Grade 2, fibrovascular tissue in the surgical area without invasion onto the corneal surface (conjunctival recurrence) as Grade 3. Finally, Grade 4 was defined as true recurrence in which the fibrovascular tissue invaded onto the cornea (corneal recurrence).
According to similar articles and α = 0.05 and power 90%, the calculated minimal required sample size was 25 eyes in each group. All data entered into SPSS software, Version 22. (Armonk, NY: IBM Corp). The differences in VAS score, graft hyperemia, edema and flap retraction, and premature suture loosening between the two groups were analyzed using the nonparametric Mann–Whitney U-test. Fisher's exact test was performed to compare recurrence rate between the two groups. Comparison of Serial VAS scores was performed using the Wilcoxon signed rank test. A P ≤ 0.05 was considered as statistically significant.
Results
A total of 50 eyes from 50 patients were recruited, 25 of which were randomized to each of the nylon group and the silk group. Three patients in the nylon group and five patients in silk group discontinued follow-up during the study. The baseline demographics and size of pterygium lesion were comparable between the two groups [Table 1]. There was no intraoperative complications.
Table 1.
Summary of patient demographics and size of pterygium lesion
| Nylon group | Silk group | |
|---|---|---|
| Mean age (years) | 44.136 | 49.067 |
| Maximum age (years) | 72 | 80 |
| Minimum age (years) | 28 | 30 |
| Male | 13 | 10 |
| Female | 12 | 15 |
| Length of pterygium (mm) | ||
| Mean | 3.478 | 3.650 |
| Maximum | 6 | 6 |
| Minimum | 3 | 2.5 |
| Breadth of pterygium (mm) | ||
| Mean | 4.391 | 4.800 |
| Maximum | 6 | 7 |
| Minimum | 3 | 4 |
Based on the study of Tan et al.,[8] clinical appearance of the lesions was graded [Table 2].
Table 2.
Number of different lesion grades in each group
| Nylon group | Silk group | |
|---|---|---|
| Number of lesion Grade 1 | 3 | 1 |
| Percentage of lesion Grade 1 (%) | 12 | 4 |
| Number of lesion Grade 2 | 19 | 22 |
| Percentage of lesion Grade 2 (%) | 76 | 88 |
| Number of lesion Grade 3 | 3 | 2 |
| Percentage of lesion Grade 3 (%) | 12 | 8 |
Interestingly, among all patients participating in the study, six patients were driver, in whom pterygium in these six patients were in their left eye that was more exposed to sunlight while the opposite side had no clinically significant lesion.
Among all patients in this study, 24% of patients had no lesion in the opposite eye, and 24% had pinguecula and 52% had pterygium in the opposite eye [Table 3].
Table 3.
Status of fellow eye
| Condition | n (%) |
|---|---|
| No lesion | 12 (24) |
| Pinguecula | 12 (24) |
| Pterygium | 26 (52) |
| Total | 50 (100) |
About 40% of the patients were living in the village and another 20% were used to live in village previously. 28% and 20% of the patients were wearing sunglasses on occasion in the nylon group and the silk group, respectively. Meanwhile, many of these patients, especially older patients, had not used sunglasses regularly. Approximately 8% of patients in the nylon group, and 16% in silk group, sometimes used hat during working hours. Thirty patients (60%) were working outdoors, 32 of the patients (64%) had positive family history of pterygium in their first degree relatives and 8 of the patients (16%) had a positive history of pterygium surgery in their fellow eyes that was recurred in 2 cases [Table 4].
Table 4.
The number and percentage of some factors that may affect the pterygium incidence
| Condition | n (%) |
|---|---|
| Working outdoors | 30 (60) |
| Life in the village | 20 (40) |
| Sunglasses | 12 (24) |
| Family history | 32 (64) |
| History of pterygium surgery in fellow eye | 8 (16) |
There was no significant relationship between working outdoors and the horizontal extension of pterygium on the corneal surface (P = 0.746); similarly, there was no significant relationship between horizontal extension of the pterygium and life in the village (P = 0.83).
The average IOP of the patients before the operation was 14.6 mmHg and the maximum IOP was measured to be 18 mmHg, while the mean postoperative IOP was 14.2 and the maximum postoperative IOP was measured to be 16. The average of the BCVA (logarithm minimum angle of resolution [logMAR] BCVA) was 0.11 (interval: 0–0.69) before the operation and was 0.071 (interval: 0–0.52) after the operation. The average astigmatism level of patients before operation was 2.39 (in 0–6.41 interval) and after operation was 1.18 (in 0.75–2.83 interval), before and after the operation, respectively [Table 5].
Table 5.
A comparison between some of the most important indices studied in the patients of both groups before and after the operation
| Nylon group (n=25) | Silk group (n=25) | Total (n=50) | |
|---|---|---|---|
| Preoperative mean logMAR BCVA | 0.17 | 0.05 | 0.11 |
| Preoperative IOP (mmHg) | 15 | 14.2 | 14.6 |
| Mean preoperative astigmatism | −2.03 | −2.75 | −2.39 |
| Postoperative mean logMAR BCVA | 0.11 | 0.03 | 0.07 |
| Mean postoperative IOP (mmHg) | 14.5 | 13.9 | 14.2 |
| Mean postoperative astigmatism | −1.5 | −1.8 | −1.18 |
IOP: Intraocular pressure, BCVA: Best-corrected visual acuity, LogMAR: Logarithm minimum angle of resolution
Postoperatively, there was a significant decrease in the mean VAS discomfort score from week 1 to week 2 in both groups (P = 0.001), but there was no significant difference between the two groups in patient discomfort scores [Figure 1].
Figure 1.

Visual analog scale score of postoperative patient discomfort in the nylon and silk groups
Prabhasawat et al.[7] defined a grading system for recurrence of the lesions, in which Grade 1 indicates a normal appearance of the operative site, Grade 2 indicates the presence of some fine episcleral vessels, but without any fibrous tissue in the excised area extending up to but not beyond the limbus, Grade 3 indicates the presence of additional fibrous tissues in the excised area without invading the cornea, Grade 4 represents a true recurrence with a fibrovascular tissue invading the cornea.
According to this grading system, three patients in the nylon group and 4 in the silk group (12% in nylon group and 16% in silk group) were noted to exhibit pterygium recurrence at month 6, among which two patients had Grade 3 (conjunctival) and five patients had Grade 4 (corneal) recurrence. With another definition of recurrence as any vascular or fibrovascular tissue >1.5 mm on the cornea five patients were noted to have pterygium recurrence at month 6 [Figures 2 and 3].
Figure 2.

Recurrence of lesions after pterygium surgery in a patient of nylon group (a) before, (b) 1st day after operation, (c) 2 weeks after operation, and (d) 6 months' postoperation
Figure 3.
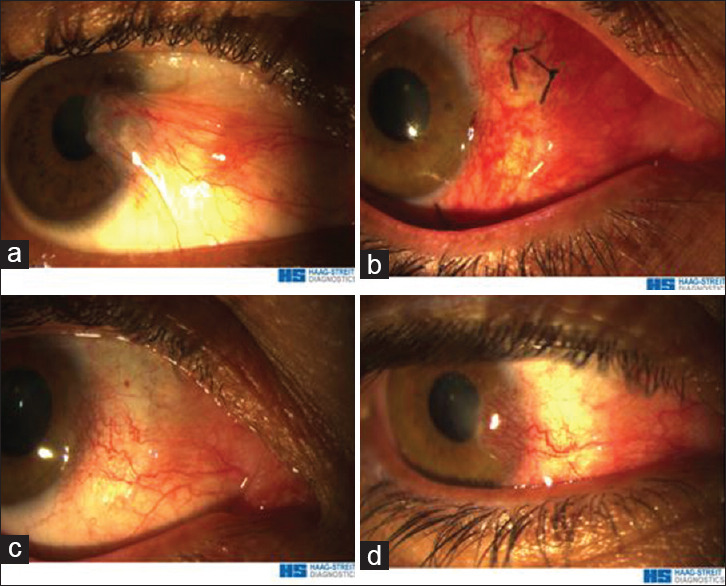
Recurrence of lesion after pterygium surgery in a patient of silk group (a) before, (b) 2 weeks after operation, (c) 1 month after operation, and (d) 6 months' postoperation
There was no significant statistical correlation between recurrence rate and grade of the primary pterygium lesion in both the nylon and silk groups (P = 0.576 and 0.2432; respectively). Similarly, there was no significant statistical correlation between recurrence and the length of the pterygium lesion in either of nylon and silk groups (P = 0.192 and 0.271; respectively). Moreover, there was no significant statistical correlation between recurrence and the width of the pterygium lesion in either groups (P = 0.562 and 0.512; respectively). Among patients with recurrence, three patients did not use topical medication regimen correctly, 2 patients had a history of recurrence in fellow eye after previous pterygium surgery and 2 patients had a history of recurrence in their first degree relatives. Nevertheless, there were no significant statistical correlation between the recurrence and history of recurrence in the fellow eye (P = 0.241) and having positive family history of recurrence (P = 0.412).
At 2 weeks' postoperation, significantly greater number of nylon sutures (mean 4.1, range 3–7) remained on the autograft compared with silk sutures (mean 0.9, range 0–4) (P = 0.021). Some of the nylon sutures were buried and could not be removed at day 14. All silk sutures were successfully removed at day 14.
There was no significant difference in graft edema between the two groups neither in the first postoperative day nor in the first postoperative week. Graft edema was occurred in 12% of patients in nylon group and in 16% of silk group, both of which resolved after 2 weeks. Lost graft was not occurred in any patient in this study.
Graft dehiscence were noted in 9 (18%) of all patients (4 in the nylon group versus 5 in the silk group); however, there was no significant statistical correlation between recurrence and premature suture loosening and graft dehiscence (P = 1 in the nylon group and P = 0.548 in the silk group).
Three of all patients developed pyogenic granuloma at the site of excised pterygium, two of them were in the nylon group that treated medically, one of them was in the silk group that was treated surgically.
Discussion
Recurrence remains the main complication of the pterygium surgery in spite of various surgical procedures that have been described and tested in the management of pterygium. Several studies have demonstrated that pterygium excision followed by conjunctival autograft technique is a safe and effective procedure for pterygium removal. According to previous studies, the rate of recurrence with this method is estimated between 2% and 39%.[4,5,6,7,8] Well anchoring of autograft is an essential part of a successful pterygium surgery with conjunctival autograft). Various suture materials and techniques including absorbable and nonabsorbable sutures of different diameters are employed to secure the autograft. Sutures are placed either interrupted or continuously, with knots left exposed or buried. Although many reports have assessed the technical modifications and recurrence rates of conjunctival autograft for pterygium surgery, few have compared the use of different suture materials in terms of postoperative patient discomfort. In a randomized, controlled study, comparing polyglactin, and nylon sutures for securing conjunctival autograft, they found that polyglactin sutures resulted in more tarsal conjunctival papillary reaction at day 1 and more graft hyperemia at week 1 postoperatively.[9] In this trial, we did not find any difference in graft hyperemia and graft edema, and both of these outcomes were resolved during first 2 postoperation weeks.
Varssano et al.[13] evaluated the efficacy of pterygium excision and conjunctival autograft using either 10-0 nylon or 8-0 to10-0 polyglactin sutures for conjunctival autograft suturing. It was noted that superficial corneal vessels without concurrent fibrosis developed in 58.8% of eyes sutured with nylon, whereas none was seen in the polyglactin group. Such an association was not showed in another study by Wong et al.,[9] with only two eyes in each group showing fine superficial corneal vessels. Silk and nylon sutures are the most commonly used materials for securing conjunctival autografts. The aim of our study was to compare the clinical results of silk versus nylon sutures for conjunctival autograft suturing in pterygium surgery. So far, no studies have compared the outcomes of using silk and nylon suture in securing conjunctival autograft. Overall, the procedure of pterygium surgery with conjunctival autograft showed good results. BCVA (logMAR BCVA) was improved after the operation while the mean astigmatism of patients was reduced from 2.39 preoperatively to 1.18 postoperatively.
The recurrence of pterygium was the main compared outcome measure to be compared in the present study. According to the grading system introduced by Prabhasawat et al., for definition of recurrence of the pterygium lesions three patients in the nylon group and four in the silk group were noted to have pterygium recurrence at month 6. Among them, two patients developed Grade 3 (conjunctival) and five patients Grade 4 (corneal) recurrence. When we defined recurrence as any vascular or fibrovascular tissue >1.5 mm on the cornea, five patients were noted to have pterygium recurrence at month 6, two patients in nylon group (%4) and three patients in silk group (%6) (P = 0.802). As our results demonstrated recurrence of pterygium was not associated with type of suture material; nylon and silk sutures showed a similar recurrence rate. Similarly, no significant difference in graft edema was observed between the two groups; graft edema was occurred in 12% of patients in nylon group and in 16% of silk group and after 2 weeks graft edema resolved in both groups.
Regarding the patient discomfort, despite a significant decrease in the mean VAS discomfort score from week 1 to week 2 in both the groups, there was no significant difference between two groups in patient discomfort scores. At 2 weeks' postoperation, significantly more nylon sutures remained on the autograft compared with silk.
Our results showed that significantly greater number of nylon sutures remained on the autograft at week 2 (mean: 4.1 vs. 0.9) compared with silk sutures. Although silk sutures were successfully removed at day 14, some of the nylon sutures were buried and could not be removed at day 14. Nylon suture removal may be more time-consuming and cause greater discomfort to the patient. Stitches that were buried and could not be removed may eventually become exposed and patients would require additional visits for suture removal.
As our results demonstrated in both nylon and silk groups there was no significant correlation between recurrence and grade of the primary pterygium lesion, the length or the width of the pterygium. In addition no significant correlation was found between the recurrence and history of recurrence in the fellow eye (P = 0.208) or having positive family history of recurrence (P = 0.588). No significant association between recurrence of pterygium and younger age (younger than 40 years), and thicker suture material (silk 8-0 versus nylon 10-0) were found.
Because of having multiple slots and more rough surface that may connect to and grow local infectious agents it is usually thought that nonmonofilament sutures like silk sutures have a more infectious rate.[14] No infection was occurred in the present study. Despite similar rates of recurrence and similar scores of postoperative discomfort in the two groups during the first 2 postoperative weeks, each suture material confers its own advantages. In the surgeon's experience, nylon sutures allowed for easier intraoperative handling and knotting. However, the removal of nylon stitches, especially those that are buried, is more difficult. The choice of suture material would depend on the surgeon's preference, availability, cost, and the patient's cooperation in suture removal.
Conclusion
Both silk and nylon are effective suture materials for autograft suturing in pterygium surgery with similar postoperative discomfort and recurrence rate. Signifcantly greater number of nylon sutures remains buried on the autograft and could not be removed easily.
Further researches seem necessary to further clarify advantages and disadvantages of silk and nylon sutures for securing conjunctival autograft in pterygium surgery.
Financial support and sponsorship
This study was funded by the Shiraz University of Medical Sciences and registered at the Iranian Registry of Clinical Trials (trial ID IRCT2016100230080N1).
Conflicts of interest
There are no conflicts of interest.
Acknowledgment
The present article was extracted from the thesis written by Mostafa Abuali which was under the supervision of Dr. Hossein Jamali and was financially supported by Shiraz University of Medical Sciences grants No. 9194.
References
- 1.Ghanavati SZ, Shousha MA, Betancurt C, Perez VL. Combined conjunctival autograft and overlay amniotic membrane transplantation; a novel surgical treatment for pterygium. J Ophthalmic Vis Res. 2014;9:399–403. doi: 10.4103/2008-322X.143386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Cameron ME. Histology of pterygium: An electron microscopic study. Br J Ophthalmol. 1983;67:604–8. doi: 10.1136/bjo.67.9.604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Fotouhi A, Hashemi H, Khabazkhoob M, Mohammad K. Prevalence and risk factors of pterygium and pinguecula: The Tehran Eye Study. Eye (Lond) 2009;23:1125–9. doi: 10.1038/eye.2008.200. [DOI] [PubMed] [Google Scholar]
- 4.Kenyon KR, Wagoner MD, Hettinger ME. Conjunctival autograft transplantation for advanced and recurrent pterygium. Ophthalmology. 1985;92:1461–70. doi: 10.1016/s0161-6420(85)33831-9. [DOI] [PubMed] [Google Scholar]
- 5.Lewallen S. A randomized trial of conjunctival autografting for pterygium in the tropics. Ophthalmology. 1989;96:1612–4. doi: 10.1016/s0161-6420(89)32667-4. [DOI] [PubMed] [Google Scholar]
- 6.Chen PP, Ariyasu RG, Kaza V, LaBree LD, McDonnell PJ. A randomized trial comparing mitomycin C and conjunctival autograft after excision of primary pterygium. Am J Ophthalmol. 1995;120:151–60. doi: 10.1016/s0002-9394(14)72602-9. [DOI] [PubMed] [Google Scholar]
- 7.Prabhasawat P, Barton K, Burkett G, Tseng SC. Comparison of conjunctival autografts, amniotic membrane grafts, and primary closure for pterygium excision. Ophthalmology. 1997;104:974–85. doi: 10.1016/s0161-6420(97)30197-3. [DOI] [PubMed] [Google Scholar]
- 8.Tan DT, Chee SP, Dear KB, Lim AS. Effect of pterygium morphology on pterygium recurrence in a controlled trial comparing conjunctival autografting with bare sclera excision. Arch Ophthalmol. 1997;115:1235–40. doi: 10.1001/archopht.1997.01100160405001. [DOI] [PubMed] [Google Scholar]
- 9.Wong VW, Rao SK, Lam DS. Polyglactin sutures versus nylon sutures for suturing of conjunctival autograft in pterygium surgery: A randomized, controlled trial. Acta Ophthalmol Scand. 2007;85:658–61. doi: 10.1111/j.1600-0420.2007.00904.x. [DOI] [PubMed] [Google Scholar]
- 10.Salthouse TN, Matlaga BF, Wykoff MH. Comparative tissue response to six suture materials in rabbit cornea, sclera, and ocular muscle. Am J Ophthalmol. 1977;84:224–33. doi: 10.1016/0002-9394(77)90856-x. [DOI] [PubMed] [Google Scholar]
- 11.Elwan SA. Comparison between sutureless and glue free versus sutured limbal conjunctival autograft in primary pterygium surgery. Saudi J Ophthalmol. 2014;28:292–8. doi: 10.1016/j.sjopt.2014.03.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Janson BJ, Sikder S. Surgical management of pterygium. Ocul Surf. 2014;12:112–9. doi: 10.1016/j.jtos.2014.01.001. [DOI] [PubMed] [Google Scholar]
- 13.Varssano D, Michaeli-Cohen A, Loewenstein A. Excision of pterygium and conjunctival autograft. Isr Med Assoc J. 2002;4:1097–100. [PubMed] [Google Scholar]
- 14.Kudur MH, Pai SB, Sripathi H, Prabhu S. Sutures and suturing techniques in skin closure. Indian J Dermatol Venereol Leprol. 2009;75:425–34. doi: 10.4103/0378-6323.53155. [DOI] [PubMed] [Google Scholar]


