Abstract
PURPOSE:
Although Taiwan was one of the first countries to develop coronavirus disease 2019 (COVID-19), with effective antiepidemic measures, Taiwan has effectively controlled the spread of the disease. The purpose of this article is to provide useful safety strategies for ophthalmologists in daily practice during the COVID-19 pandemic.
MATERIALS AND METHODS:
Infection control strategies in the hospital and Department of Ophthalmology, Chang Gung Memorial Hospital, Linkou, are discussed.
RESULTS:
Ophthalmologists are at high risk of contracting COVID-19 infection, as they have close contact with patients during ocular examinations, and are also facing high patient volume in outpatient clinics as well as emergency consultations. Furthermore, ocular symptoms, such as conjunctivitis, may be the presenting signs of COVID-19 infection. We provide our strategies, which include hospital's gate control with triage station, patient volume control, proper personal protective equipment, and consultation with telemedicine technology, to decrease the risk of cross-infection between medical staffs and patients.
CONCLUSION:
To achieve the goal of preventing viral spread and maximizing patient and medical staffs' safety, besides providing proper protective equipment, it is also crucial for staffs and patients to strictly follow antiepidemic measures. We hope that our experience can help ophthalmologists and health-care workers to have a safer working environment when facing COVID-19 pandemic.
Keywords: Coronavirus, coronavirus disease 2019, ophthalmology, Taiwan
Introduction
Coronavirus disease 2019 (COVID-19), which is caused by severe acute respiratory syndrome-coronavirus 2 (SARS-CoV-2), is rapidly causing major threats to global health and economic systems. As of April 25, 2020, according to the World Health Organization, there were 2,626,321 confirmed cases and 181,938 deaths caused by COVID-19.[1] According to the data released by Taiwan Centers for Disease Control (CDC), until April 25, 2020, there were 429 cases and 6 deaths in Taiwan, which were mostly imported with a few local cases – A situation under relatively good control compared to the rest of the world.[2]
SARS-CoV-2 is highly contagious. Sources of transmission include discharge or direct contact with droplets and fomites that contain virus particles through the mouth, nose, or eyes.[3,4,5] The mean incubation period was 5–7 days, although the longest incubation period could be up to 24 days in some cases.[6] Symptoms of the infection include fever, cough, shortness of breath, diarrhea, and myalgia. Other less common symptoms include loss of taste or smell, headache, and fatigue. According to previous studies, ocular manifestations such as conjunctival chemosis, hyperemia, epiphora, and secretion were reported.[7,8] There are no effective treatments found so far.
Ophthalmologists are at high risk of contracting the aforementioned infection, as they have close contact with patients during ocular examinations, and are also facing high patient volume in both the outpatient clinics and emergency consultations. Prolonged stay in the clinic for the completions of multiple ocular examinations also increases risks of transmission. Moreover, SARS-CoV had been isolated from tear samples of patients in the previous outbreak, which may indicate the possibility of direct transmission through the tears of COVID-19 patients.[9,10] In rare cases, conjunctivitis may be the first presenting symptoms of COVID-19 infection, rendering ophthalmologists among the first health-care providers to evaluate suspected cases.[10,11]
Although Taiwan was initially considered to be one of the countries most affected by COVID-19 in the world, due to the lessons learned from the SARS epidemic years ago, the early adoption of preventive measures taken by the Taiwan government and health authorities has effectively controlled the spread of disease. Facing this epidemic, Taiwan's medical institutions actively mobilized and clearly divided the responsibilities. Since the proper protection with careful precautions is mandatory to minimize the risks of COVID-19 infection, we would like to share our experience from the perspectives of a tertiary referral medical center in Taiwan.
Hospital Policy
Chang Gung Memorial Hospital (CGMH, Linkou Branch) is a major medical center located in Northern Taiwan. CGMH in Linkou presently provides the largest number of beds (around 3800) in our nation. With over 9500 employees and over 1000 attending staffs, the hospital takes charge of almost 4 million outpatients annually, two hundred thousand patients in the emergency department, and handles close to one hundred thousand patients that have sought surgery. The hospital has inpatient isolation facilities and is responsible for treating COVID-19 patients, especially severe cases.
Since late January 2020, our hospital has implemented gate control policies and triage stations were set at each entrance of the hospital. Entrances other than the main gate in a building are closed to facilitate access control. All visitors were screened by infra-red thermometers and were requested to put on masks before entering our hospital [Figure 1a]. Febrile patients will be referred to the emergency department or specialized infectious clinic for further evaluation. An isolated temporary fever screening station was set up just outside of the emergency room, which was equipped with portable X-ray and laboratory machines. Besides, surveillance for Travel history to epidemic areas, Occupation, Contact of a suspected or confirmed case, Cluster of cases (TOCC) was also carried out at the entrance and triage station. To avoid an indirect contact, patients and accompanying family were checked by their national health insurance card at the entrance before entering the hospital. A policy to terminate the visitation of hospitalized patients was also announced in early February. Social distancing for at least 1.5-m indoors was also implemented in waiting rooms and the cafeteria in concordance to Taiwan CDC's policy. The registration counters in outpatient clinics and examination rooms were shifted to automated machines to prevent frequent contact between medical staffs and patients [Figure 1b]. At the entrance of elevators, hand disinfection gel or solution-dispensing device was set up. If person-to-person contact cannot be avoided, such as in the reception, cashier, and pharmacy, a plastic protection shield was installed over the counter to prevent spreading of aerosol [Figure 1c]. Our hospital had also set up a counter outside the hospital for the people with the need of chronic prescription so that they do not need to enter the hospital to get their prescription.
Figure 1.

Examples of measures taken by hospital. (a) Triage stations equipped with infra-red thermometers; medical staffs are equipped with facial masks, surgical mask, and protective clothing. (b) Automated registration machine; marks on the floor are designed for social distancing reminder. (c) Plastic protection shield is installed over the counter to prevent spreading of aerosol
With respect to medical staff training and health monitoring, all our staffs were required to undergo a series of online infection control training programs. In addition, all clinical staffs were asked to measure and to register their body temperatures daily before attending work through specialized mobile software. If symptoms such as fever, myalgia, sore throat, cough, diarrhea, or vomiting were noted, the related staffs would be mandated to report and be referred to special infectious clinic for further evaluation. Since March 2020, medical staffs with recent overseas traveling history were banned from attending conferences to reduce the risks of transmission of COVID-19. CGMH also provided dormitory rooms for medical staffs requiring quarantine during this critical period.
Outpatient Clinic Setting
The Department of Ophthalmology in CGMH is one of the largest and busiest ophthalmologic referral centers in Taiwan. It provides general and urgent eye care services, as well as subspecialty services for cornea, glaucoma, oculoplastic and orbital surgery, retinal and vitreous diseases, pediatric ocular disorders, cataract, and neuro-ophthalmic diseases. The daily average outpatient volume and ocular examinations were 450 and 500, respectively. High patient volume coupled with crowded space is a challenge for preventing transmission of COVID-19. To avoid such scenario, we apply the following strategies:
Reduction of patient volume
Patients who are febrile or have respiratory symptoms are asked to reschedule their eye clinic appointments and seek health advice for their respiratory symptoms first. Patients with nonurgent ocular conditions or examinations will also be rescheduled and postponed to at least 1 month later.
Segregating patients and medical staffs
Nurses and optometrists were assigned to fixed clinic or examination room to avoid rotation between different rooms, thus preventing possible cross-infection in outpatient clinics. In order to avoid patients gathering in examination rooms and clinics, only one patient is allowed to enter the room at one time. If a patient has any mobility issue, only one caregiver can come along with the patient. Patients are instructed to adhere to social distancing for at least 1.5 m with their masks on in the waiting area and also reduce chatting while waiting [Figure 2a].
Figure 2.
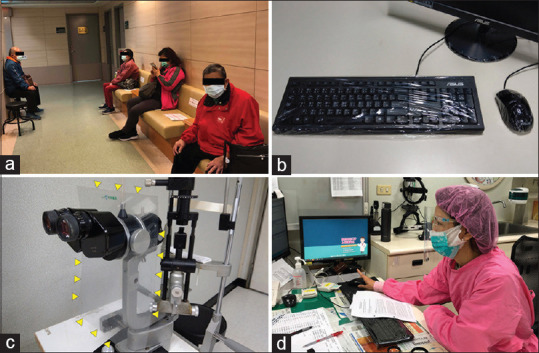
Procedures taken by ophthalmology department. (a) Each seat departed at least 1.5 m at the waiting area in our clinic. (b) Keyboard and mouse were covered with disposable plastic wrap. (c) Slit lamp was installed with plastic protective shields (yellow arrowheads). (d) Medical staff was equipped with facial mask, surgical mask, gown, surgical cap, and protective eye goggle
Environmental sanitation
A recent study showed that SARS-CoV-2 virus can survive up to 24 h on cardboards and up to 2–3 days on plastic and stainless steel surfaces.[3] Therefore, it is crucial to perform frequent and appropriate sanitation of the environment.[12] We use disposable plastic wrap to enwrap all keyboards and mousses, while also changing them twice a day to prevent contamination on the surface [Figure 2b]. Frequent cleaning of desks, chairs, as well as the handle of examination equipment (such as joystick of slit lamp and handle of direct ophthalmoscope) with 75% alcohol are also applied. The clinic is disinfected with diluted household bleach (0.1% sodium hypochlorite) by the end of the day.
Protective equipment
As COVID-19 is capable of aerosol transmission, protection from droplets is, therefore, very important.[13] All slit lamps in our clinics were installed with plastic protective shields [Figure 2c]. These shields could block or reduce droplets in either direction. They were also disinfected with 75% alcohol after every clinic session. The use of personal protective equipment (PPE) could further reduce the risk of exposure to aerosolized droplets. Surgical masks, protective eyewear, facial masks, and protective clothing were provided to all doctors, nurses, and optometrists [Figure 2d]. According to different procedures and examinations, we have proposed different prevention strategies, as shown in Table 1. Doctors managing high-risk patients will have to perform examinations wearing additional PPE including gloves, cap, and N95 mask in a negative pressure room. All medical staffs are recommended to change into medical gowns upon arrival to the hospital, thus preventing possible viral contamination on personal garments.
Table 1.
Suggestions of prevention management in different scenario
| Scenario | Prevention management | |
|---|---|---|
| Low risk | History taking (at >1 m distance) at clinic or bedside | Surgical mask, gown, surgical cap |
| Median risk | Slit-lamp examination, gonioscopy, ultrasonography, laser treatment of anterior chamber or posterior segment | Surgical mask, gown, surgical cap, glasses, gloves, face shield |
| High risk | Ophthalmic surgeries and intervention for suspected or confirmed cases Managing cases with travel history to epidemic regions of COVID-19 |
N95 mask, surgical gown, surgical cap, glasses, gloves, face shield, protective cover roll, environment with negative pressure or good ventilation |
COVID-19: Coronavirus disease 2019
Hand hygiene
It is particularly important for both medical staffs and patients to practice proper steps of handwashing. Povidone-iodine scrub, alcohol-contained solution, and soap are provided in all clinic and examination rooms. After entering the clinic, patients were asked to disinfect their hands with 75% alcohol before seeing the doctor. All medical staffs are required to wash their hands after every patient encounter.
Examination equipment
To prevent possible cross-infection using the same equipment for multiple patients, disposable tools will be considered a priority. For example, tonometers such as Icare (Icare Finland Oy, Helsinki, Finland) or Tonopen (Reichert Technologies, Depew, NY) will be applied with single-use, disposable tips. For the items that are autoclavable, such as lid speculums used for the retinopathy of prematurity (ROP) screening, they were autoclaved before use. We have also prepared multiple sets of examination equipment to account for the large patient volume expected.
Inpatient Ward Setting
To prevent possible cross-infection between outpatient visitors and inpatients, we limit only one accompanying person for each inward patient and prohibit visitors other than accompanying person to patients. We also check inpatients in the examination rooms established in the ward. Attending staffs and resident doctors were divided into two groups, through which each group will take care of inpatients in rotation. The roster will be alternated every 2 weeks to minimize contagion risk. The nurses in the ward all wear waterproof gown, rubber glove, N95 mask, surgical cap, and face shield [Figure 3].
Figure 3.

The nurse in the ward wears water-proof gown, rubber glove, N95 mask, surgical cap, and face shield
Besides, we have practiced controlled movement and usage of the duty rooms in our wards. All personnel using the duty room will be required to register in order to prevent crowded conditions and to monitor contact.
Consultations
To prevent transmission of COVID-19, inpatient consultations from other specialties were carried out in a designated room instead of the regular clinic. Consultations from our emergency department were screened initially by an online telemedicine program [Figure 4]. If the consultations were not considered urgent, medications would be prescribed first after teleconference consultation, and a patient would be educated on the necessary precautions in subsequent care. If immediate attention was indicated, a designated ophthalmologist will visit the emergency department and examine patients in an isolated, specialized consultation room while donning a standard full PPE.
Figure 4.
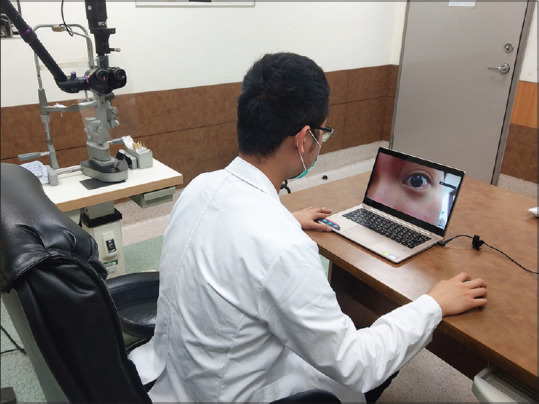
Telemedicine online program for emergency consultation
Operation Room Setting
All patients checking in at our nursing station will receive detailed TOCC background confirmation and will have their body temperature measured. Febrile patients will be referred to screening stations in the emergency department for further evaluation. High-risk patients scheduled for elective surgeries (such as cataract surgery and cosmetic eyelid surgery) will be recommended to postpone the operation for at least 1 month. If emergent surgery was indicated in high-risk patients, the patients need to obtain additional X-ray examinations to screen for possible pneumonia. Compared to endotracheal intubation, due to reduced risk of aerosol-generating conditions, local anesthesia is preferred for the high-risk patients. If general anesthesia was inevitable, designated infection and anesthesia specialist will be consulted first. Operation will be performed in an isolated operation room with all staffs equipped with disposable surgical gowns, N95 masks, and protective eye goggles.
The dining area for medical staffs in the operation room was also equipped with plastic protective shields between seats, therefore lessening the spread of aerosol during meal intake [Figure 5]. All staffs were banned from chatting during meals.
Figure 5.

Dining area of operative room equipped with plastic protective shields
Department Meetings
With respect to the trend of teleconference, we have promoted utilizing teleconferences for morning meetings and grand rounds. The results have been largely effective as the attendance and participation of these meetings were encouraging.
The outlines of our strategies facing COVID-19 in different locations are summarized in Table 2. With these measures implemented, we did not have any positive cases in our department yet.
Table 2.
Outline of strategies in different locations
| Location | Key strategies |
|---|---|
| Hospital’s gate | Infra-red thermometers screening |
| TOCC information gathering; travel history revealed from the National Insurance Card | |
| Identifying high-risk patients and referring them to ER | |
| Setting up a special fever screening station equipped with X-ray and laboratory machine outside ER | |
| Automatic hand sanitizer dispensers equipped for visitors | |
| Outpatient clinic | Detail history taking, identify high-risk patients |
| Reduction of patient volume | |
| Segregating patients and medical staffs | |
| Environmental sanitation | |
| Protective equipment: PPE and slit lamp’s shield | |
| Hand hygiene | |
| Use disposable tools or tips as possible | |
| Social distancing | |
| Inpatient ward | Prohibition of bringing inpatient to clinics for ocular examinations |
| Rotation of task force taking care of inpatients, alternating every 2 weeks | |
| Call room registration | |
| Limit to one accompanying person for each inward patient | |
| Prohibit visitors other than accompanying person to patients | |
| Consultation | Designating an isolated room for inpatient consultation or examining high-risk patients |
| Online telemedicine program for emergency department’s consultation | |
| Operating room | Detailed history taking to identify high-risk patients |
| Body temperature measured and chest X-ray taken for high-risk and positive TOCC patients | |
| Postponement of nonurgent operations | |
| Avoiding general anesthesia, if inevitable, consult infection and anesthesia specialist | |
| Proper PPE during operation | |
| Plastic protective shields between seats in dining area |
ER: Emergency room, PPE: Personal protective equipment, TOCC: Travel history to epidemic areas, Occupation, Contact of a suspected or Confirmed case, cluster of cases
Discussion
COVID-19, which was first identified in December 2019 in Wuhan, China, has since spread globally and has caused major impacts on the health-care system and global economies. The responsible virus, SARS-CoV-2, is highly contagious, whereby previous study indicates that person-to-person transmission will happen at a large scale in familial clusters.[5] Although still controversial, the transmission of COVID-19 is believed to occur through droplets or by direct contact with secretions from infected patients.[14] In this article, we have shared our experiences to curb the spread of COVID-19. With these measures, we are fortunate that to date, we have not encountered any positive cases. It is important to know that each chain of antipandemic, including country, society, and our workplace, plays a pivotal role in controlling the spread of this terrifying disease. Hospital or ophthalmology department alone could not achieve success without the corresponding procedures taken in the country.
In 2003, Taiwan experienced a series of challenges from SARS, which was also caused by coronavirus (SARS-CoV), with a record of 668 probable cases and 181 deaths between March 14 and July 30, 2003.[15] The most serious outbreak of SARS in Taiwan was cluster nosocomial infection which took place in the Municipal Hoping Hospital in Taipei, and 137 probable cases and 26 deaths were recorded. The current fatality rate of COVID-19 seems to be less (3.4%)[16] than SARS (9.5%) and Middle East respiratory syndrome (34.4%).[17] However, the extent of infection in COVID-19 is over 100 times than that of SARS.[18,19] Therefore, it is vital to have comprehensive managements when facing COVID-19 pandemic.
On the heels of previous lessons learned from SARS, Taiwan CDC quickly formed a response team on January 2, 2020, and had classified COVID-19 as a Type 5 notifiable communicable disease to enhance disease surveillance in order to prepare for a possible pandemic.[20] Multiple prevention strategies were also implemented, including border control, home isolation and quarantine, nosocomial infection control, and increasing stockpiles of masks and PPEs. These strategies helped in providing adequate protective equipment for all medical workers, thus ameliorating fear of shortages and preserving morale in tackling the pandemic. The rapid response helps Taiwan to rein in epidemics and avoid further lockdown.
For ophthalmologists facing the COVID-19 pandemic, multiple suggestions were proposed in different areas around the world too.[12,21,22,23] All of them suggest the use of proper PPE, hand hygiene, environmental control, and patient volume control. Regarding the patient volume control, the Royal College of Ophthalmologists in UK has suggested that for diabetic macular edema, retinal vein occlusion or uveitis cases to defer review in clinic by 4 months.[24] In Italy, one of the most serious epidemic areas of COVID-19, a study group has proposed a risk assessment tool for ophthalmologists to reduce all nonurgent elective activities in order to free up staff and ward beds for confirmed cases.[23] All these suggestions were for the purpose of postponement of nonurgent conditions or surgeries. The American Academy of Ophthalmology also suggested that before entering the waiting room of clinic, patients should be asked about fever and respiratory symptoms or whether they had any contact history with confirmed cases in the past 2–14 days.[25] In our department, we contacted elective patients to reschedule their appointment. Using detailed TOCC screening and body temperature measurement during gate triage before patients' clinical appointment, and upon entering the nursing station in the operation room, we could identify patients with suspected infection and refer them to our special screening center for further management.
So far, there is no effective treatment for COVID-19 infection. Some therapies, such as hydroxychloroquine, have been tried. It may reduce viral load but without seeing significant clinical effects yet.[26] Its use in COVID-19 infection remains uncertain. It should be noted that there is macular toxicity related after its long-term use, and ophthalmologists play an important role in determining the detrimental side effect caused by overdose in these patients.
Telemedicine refers to the use of telecommunication and information technologies in order to provide remote clinical health care, which previously had different usages in eye diseases, such as diabetic retinopathy or ROP.[27,28,29,30] In the current COVID-19 pandemic, telemedicine may be very useful to prevent contact between medical staffs and high-risk cases. Our hospital proposed a strategy using telemedicine technology at the emergency department before seeing the patients personally. Doctors could make history taking and have a brief inspection of patients' external eye before deciding if the patients need further detailed examination. Using this way, patients could receive appropriate evaluations and managements, and person contact could also be reduced.
Conclusion
To achieve the goal of preventing viral spread while maximizing patient's and medical staffs' safety, it is crucial to provide proper protective procedures and strictly adhered by staffs and patients. We hope that our experience could help ophthalmologists and health-care workers in safer and better eye care in COVID-19 pandemic.
Financial support and sponsorship
Nil.
Conflicts of interest
The authors declare that there are no conflicts of interests of this paper.
References
- 1.Coronavirus disease 2019 (COVID-19) Situation Report – 95 (2020) World Health Organization; [Last accessed on 2020 Apr 25]. Available from: https://wwwwhoint/docs/default-source/coronaviruse/situation-reports/20200424-sitrep-95-covid-19pdfsfvrsn=e8065831_4 . [Google Scholar]
- 2.Taiwan Central Epidemic Command Center (CECC) press release on Apr. 25. [Last accessed on 2020 Apr 25]. Available from: https://www.cdc.gov.tw/En/Bulletin/Detail/liSRaimbPJQO7RQH2tSHYg?typeid=158 .
- 3.van Doremalen N, Bushmaker T, Morris DH, Holbrook MG, Gamble A, Williamson BN, et al. Aerosol and surface stability of SARS-CoV-2 as compared with SARS-CoV-1. N Engl J Med. 2020;382:1564–7. doi: 10.1056/NEJMc2004973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Li JO, Lam DS, Chen Y, Ting DS. Novel coronavirus disease 2019 (COVID-19): The importance of recognising possible early ocular manifestation and using protective eyewear. Br J Ophthalmol. 2020;104:297–8. doi: 10.1136/bjophthalmol-2020-315994. [DOI] [PubMed] [Google Scholar]
- 5.Chan JF, Yuan S, Kok KH, To KK, Chu H, Yang J, et al. A familial cluster of pneumonia associated with the 2019 novel coronavirus indicating person-to-person transmission: A study of a family cluster. Lancet. 2020;395:514–23. doi: 10.1016/S0140-6736(20)30154-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Guan WJ, Ni ZY, Hu Y, Liang WH, Ou CQ, He JX, et al. Clinical characteristics of coronavirus disease 2019 in China? N Engl J Med. 2020 Feb 28; doi: 10.1056/NEJMoa2002032. Published online. doi: 10.1056/NEJMoa2002032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Chen L, Liu M, Zhang Z, Qiao K, Huang T, Chen M, et al. Ocular manifestations of a hospitalised patient with confirmed 2019 novel coronavirus disease? Br J Ophthalmol. 2020 doi: 10.1136/bjophthalmol-2020-316304. Published Online: 07 April 2020. doi: 10.1136/bjophthalmol-2020-316304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wu P, Duan F, Luo C, Liu Q, Qu X, Liang L, et al. characteristics of ocular findings of patients with coronavirus disease 2019 (COVID-19) in Hubei province, China? JAMA Ophthalmol. 2020 doi: 10.1001/jamaophthalmol.2020.1291. Published online: 31 March 31. doi:10.1001/jamaophthalmol.2020.1291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Loon SC, Teoh SC, Oon LL, Se-Thoe SY, Ling AE, Leo YS, et al. The severe acute respiratory syndrome coronavirus in tears. Br J Ophthalmol. 2004;88:861–3. doi: 10.1136/bjo.2003.035931. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Xia J, Tong J, Liu M, Shen Y, Guo D. Evaluation of coronavirus in tears and conjunctival secretions of patients with SARS-CoV-2 infection. J Med Virol. 2020;92:589–94. doi: 10.1002/jmv.25725. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Liang L, Wu P. There may be virus in conjunctival secretion of patients with COVID-19. Acta Ophthalmol. 2020;98:223. doi: 10.1111/aos.14413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Zhang MC, Xie HT, Xu KK, Cao Y. Suggestions for disinfection of ophthalmic examination equipment and protection of ophthalmologist against 2019 novel coronavirus infection. Zhonghua Yan Ke Za Zhi. 2020;56:E001. doi: 10.3760/cma.j.issn.0412-4081.2020.0001. [DOI] [PubMed] [Google Scholar]
- 13.Huang C, Wang Y, Li X, Ren L, Zhao J, Hu Y, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395:497–506. doi: 10.1016/S0140-6736(20)30183-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Wang J, Du G. COVID-19 may transmit through aerosol? Ir J Med Sci. 2020 doi: 10.1007/s11845-020-02218-2. Published online: 24 March. doi: 10.1007/s11845-020-02218-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Chen KT, Twu SJ, Chang HL, Wu YC, Chen CT, Lin TH, et al. SARS in Taiwan: An overview and lessons learned. Int J Infect Dis. 2005;9:77–85. doi: 10.1016/j.ijid.2004.04.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.WHO Director-General's Opening Remarks at the Media Briefing on COVID-19; 2020. [Last accessed on 2020 Apr 13]. Available from: https://wwwwhoint/dg/speeches/detail/who-director-general-s-opening-remarks-at-the- media-briefing-on-covid-19---3-march-2020 .
- 17.Munster VJ, Koopmans M, van Doremalen N, van Riel D, de Wit E. A novel coronavirus emerging in China – Key questions for impact assessment. N Engl J Med. 2020;382:692–4. doi: 10.1056/NEJMp2000929. [DOI] [PubMed] [Google Scholar]
- 18.Huang; YMYHTWAPXW. ACE2 Shedding and Furin Abundance in Target Organs may Influence the Efficiency of SARS-CoV-2 Entry. 2020. [Last accessed on 2020 Apr 14]. Available from: http://wwwchinaxivorg/abs/20200200082 .
- 19.Coronavirus disease 2019 (COVID-19) Situation Report – 84 (2020) World Health Organization; [Last acessed 2020 Apr 14]. Available from: https://wwwwhoint/docs/default-source/coronaviruse/situation-reports/20200413-sitrep-84-covid-19pdfsfvrsn=44f511ab_2 . [Google Scholar]
- 20.Wang CJ, Ng CY, Brook RH. Response to COVID-19 in Taiwan: Big data analytics, new technology, and proactive testing. JAMA. 2020;323:1341–2. doi: 10.1001/jama.2020.3151. [DOI] [PubMed] [Google Scholar]
- 21.Lai TH, Tang EW, Chau SKY, Fung KS, Li KK. Stepping up infection control measures in ophthalmology during the novel coronavirus outbreak: An experience from Hong Kong. Graefes Arch Clin Exp Ophthalmol. 2020;258:1049–55. doi: 10.1007/s00417-020-04641-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Minocha A, Sim SY, Than J, Vakros G. Survey of ophthalmology practitioners in A&E on current COVID-19 guidance at three Major. UK Eye Hospitals Eye (Lond) 2020. Published online: 7 Apr 2020. Available from: https://doiorg/101038/s41433-020-0857-5 . [DOI] [PMC free article] [PubMed]
- 23.Romano MR, Montericcio A, Montalbano C, Raimondi R, Allegrini D, Ricciardelli G, et al. Facing COVID-19 in ophthalmology department? Curr Eye Res. 2020 doi: 10.1080/02713683.2020.1752737. Published online: 23 Apr. doi: 10.1080/02713683.2020.1752737. [DOI] [PubMed] [Google Scholar]
- 24.Medical Retinal Management Plans during COVID-19, Royal College of Ophthalmologists (RCOphth) [Last accessed on 2020 Mar 30]. Available from: https://www.rcophth.ac.uk/wp-content/uploads/2020/03/Medical-Retinal-Management-Plan-during-COVID-19-UPDATED-300320-1-3.pdf .
- 25.Important coronavirus updates for ophthalmologists, American Academy of Ophthalmology. [Last accessed on 2020 Apr 12]. Available from: https://www.aao.org/headline/alert-important-coronavirus-context .
- 26.Gautret P, Lagier JC, Parola P, Hoang VT, Meddeb L, Mailhe M, et al. Hydroxychloroquine and azithromycin as a treatment of COVID-19: Results of an open-label non-randomized clinical trial. Int J Antimicrob Agents. 2020 doi: 10.1016/j.ijantimicag.2020.105949. Published online 20 March. doi: 101016/jijantimicag2020105949. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Cuadros J, Bresnick G. EyePACS: An adaptable telemedicine system for diabetic retinopathy screening. J Diabetes Sci Technol. 2009;3:509–16. doi: 10.1177/193229680900300315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Tozer K, Woodward MA, Newman-Casey PA. Telemedicine and diabetic retinopathy: Review of published screening programs. J Endocrinol Diabetes. 2015;2:1–10. doi: 10.15226/2374-6890/2/4/00131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Daniel E, Quinn GE, Hildebrand PL, Ells A, Hubbard GB, 3rd, Capone A, Jr, et al. Validated system for centralized grading of retinopathy of prematurity: Telemedicine approaches to evaluating acute-phase retinopathy of prematurity (e-ROP) study. JAMA Ophthalmol. 2015;133:675–82. doi: 10.1001/jamaophthalmol.2015.0460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Richter GM, Williams SL, Starren J, Flynn JT, Chiang MF. Telemedicine for retinopathy of prematurity diagnosis: Evaluation and challenges. Surv Ophthalmol. 2009;54:671–85. doi: 10.1016/j.survophthal.2009.02.020. [DOI] [PMC free article] [PubMed] [Google Scholar]


