Abstract
Tumor of lacrimal sac invading into orbit has to be removed carefully to avoid injuring the eyeball, optic nerve, and extraocular muscles. Transnasal endoscopic-assisted tumor excision is a method to remove the tumor from the nasal cavity through the lacrimal sac to the orbit in one procedure. A 55-year-old female patient with thyroid carcinoma removed more than 10 years ago. She recently had a swollen submandibular lymph node enlargement, which was pathologically diagnosed as metastatic carcinoma. Follow-up investigation showed a tumor in the ipsilateral lacrimal sac with invasion into adjacent orbit and nasal cavity. The tumor was removed through image-guided surgery (IGS), navigation-assisted transnasal endoscopic-assisted excision. The tumor was removed as much as possible. The eyeball, extraocular muscles, and optic nerve were not injured in the surgery. Postoperative swelling was minimal with mild nasal hemorrhage. No ecchymosis and conjunctiva chemosis and eyelid swelling was noticed. Ocular motility was full without diplopia. Although exenteration and partial maxillectomy were suggested after pathological result showed a carcinoma of lacrimal sac, patient did not want these extensive surgery immediately. On patient request to reserve the eyeball function, navigation-assisted transnasal endoscopic excision is a safe and efficient method for the preliminary surgery. This case of orbital tumor excision using endoscope and IGS navigation system is the first case by Taiwan ophthalmologists.
Keywords: Endoscope, lacrimal sac carcinoma, navigation
Introduction
Tumor of lacrimal sac is rare and easily overlooked due to a more common disorder of idiopathic nasolacrimal duct obstruction or dacryocystitis.[1] When epiphora is treated by intubation without examining the lacrimal sac, delay of diagnosis may lead to a tumor invasion into the orbit. The tumor may grow extensively to surround the eyeball and optic nerve. Such tumors invading into orbit have to be removed carefully to avoid injuring the eyeball, optic nerve, and extraocular muscles, before pathological nature of the tumor is not known.
Compared to the common transconjunctival or transcutaneous approaches for excision of lacrimal sac tumor, transnasal endoscopic-assisted tumor excision is to remove the tumor from the nasal cavity, through the lacrimal sac to the orbit. If the tumor invades into the nasal cavity, such approach is a good option. Tumor excision approached from the nasal side has the risk of damaging the eyeball and extraocular muscles since the eyeball and the extraocular muscle is veiled by the tumor. During the procedure, the surgeons have difficulty deciding where to stop removing tumor and avoiding damaging the extraocular muscles, eyeball, and optic nerve.
Image-guided surgery (IGS) acts as a road map for surgeons to the safe access of an orbital and lacrimal sac tumor. This three-dimensional (3D) model of IGS, an animation of the patient's orbit, is registered to the actual position of the patient on the operating table.[2] The orbital surgeons can access to the orbital tumor simultaneously with live endoscopic images of the patient and computed tomography (CT) images taken of the patient presurgery. Surgeons continually are aware where the surgical instrument is during surgery. With IGS navigation, surgeons know where excision has to be terminated.
Case Report
A 55-year-old female with chronic epiphora came with a diagnosis of lacrimal sac tumor of the right eye, which was from an investigation of an enlarged ipsilateral submandibular lymph node with carcinoma metastasis of unknown origin. Positron emission tomography showed an involvement of ipsilateral right lacrimal sac and CT scan revealed a mass in the right lacrimal sac extending to the eyeball and the nasal cavity [Figure 1]. The tumor did not grow to the temporal side of the globe and the optic nerve. The patient had a past history of thyroid carcinoma.
Figure 1.

Orbital CT revealed a mass in the left lacrimal sac and surrounding the eyeball and extending into nasal cavity
She did not want extensive surgery such as an exenteration even if the frozen section of the specimen had revealed malignancy of the tumor. Instead, she insisted on a surgery with the least scar on her face and no facial disfiguration. In response to this request, transnasal endoscopic approach with assistance by IGS navigation (KARL STORZ, NAV1® OPTICAL system, Germany) was arranged for tumor excision to obtain specimen for pathological examination and safe maximal tumor removal. The eyeball was protected by a planned marking [Figure 2]. Excision instrument close to the area with navigation marking will be warmed with an alarm. The tumor in the nasal cavity to start with excision was marked as well [Figure 2]. The procedure was smooth. The eyeball, extraocular muscles, and optic nerve were not injured in the surgery. Mild nasal bleeding was noticed in the night after surgery. Postoperative swelling was minimal with mild nasal hemorrhage [Figure 3]. Neither conjunctiva chemosis nor eyelid swelling was noticed. Ocular motility was full without diplopia. The patient did not have oozing around periorbital region, chemosis, subconjunctival hemorrhage, or limitation of ocular motility. Vision is not affected. Pathological examination showed squamous cell carcinoma of lacrimal sac. Since the patient did not want exenteration and partial maxillectomy, she is referred to oncologist and radiologist for further management. She received further treatment of chemotherapy and radiotherapy. Follow-up CT [Figure 4] revealed recurrence of tumor 3 months after our primary excision.
Figure 2.

In an IGS preoperative planning, the border of eyeball was marked by a planed marking [Dots of circles]. Excision close to the marking line will be alarmed. The tumor in the nasal cavity to start with excision was marked as well [single circle].
Figure 3.
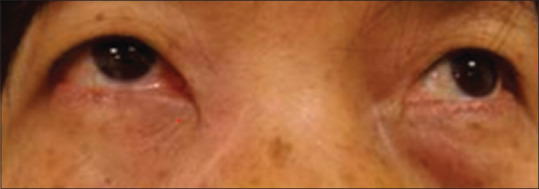
Patient's appearance in the first night after surgery. The eyeball, extraocular muscles and optic nerve was not injured in the surgery. Postoperative swelling was minimal with mild nasal hemorrhage
Figure 4.

Follow up CT scan of the patient revealed recurrence of tumor 3 months after primary excision
Discussion
Lacrimal sac/nasolacrimal duct tumors can be of either epithelial or nonepithelial origin. The majority are epithelial and malignant. These include mostly squamous cell carcinoma, transitional cell carcinoma, adenoid cystic carcinoma, and adenocarcinoma. The patient was a case of squamous carcinoma of lacrimal sac with submandibular lymph node metastasis. Before our surgery, the possible diagnosis is expected. On the basis of the malignant tumor from lacrimal sac invading nasolacrimal duct, en bloc excision with the frontal process of the maxilla, lateral nasal wall, lacrimal fossa, ethmoids, and anterior part of the medial orbital wall is suggested.[2] Intraoperative frozen section examination is a preferred adjuvant procedure. Postoperative, the radiotherapy is recommended. Nevertheless, the patient did not want extensive surgery to completely remove the tumor.
To meet the requirement of the patient, combination of navigation- and endoscope-assisted orbital surgery is a good option. The surgeon can see or “track” his instruments in relation to the patient's real anatomy and orientate them on the 3D animation shown on the computer screen. Thus, the patient can have maximal tumor removal without injuring the eyeball, extraocular muscles, and optic nerve.
In this case, we operated on the tumor as the patient requested for no facial scar or disfiguration. Nonetheless, a more complete surgery should include partial maxillectomy to remove the tumor within the nasolacrimal duct. Without removing the tumor within this bone-confined area, tumor can be expected to grow back soon after the surgery. Such result was shown in the follow-up CT scan 3 months after the diagnostic surgery.
The use of IGS for sinus surgery has a lower risk of major and total complications compared with non-IGS sinus surgery.[3,4] Orbital surgery is approached with endoscope and a surgical route identical to sinus surgery. Both endoscopic sinus surgery and orbital surgery share similar benefits from IGS. This case of orbital tumor excision using endoscope and IGS navigation system is the first case by Taiwan ophthalmologists. In the near future, IGS navigation could be a handy assistant to all orbital surgeons in Taiwan.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient has given her consent for her images and other clinical information to be reported in the journal. The patient understands that name and initials will not be published and due efforts will be made to conceal her identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
The authors declare that there are no conflicts of interests of this paper.
Acknowledgement
We appreciated Miss Min-Chia Wu for arrangement of endoscope and navigation equipments. We also appreciated Kenny for technical support of the navigation.
References
- 1.Alabiad CR, Weed DT, Walker TJ, Vivero R, Hobeika GA, Hatoum GF, et al. En bloc resection of lacrimal sac tumors and simultaneous orbital reconstruction: Surgical and functional outcomes. Ophthalmic Plast Reconstr Surg. 2014;30:459–67. doi: 10.1097/IOP.0000000000000134. [DOI] [PubMed] [Google Scholar]
- 2.Durairaj VD. Image guidance surgery – Is it useful to the orbital surgeon? Saudi J Ophthalmol. 2010;24:67–8. doi: 10.1016/j.sjopt.2010.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Dalgorf DM, Sacks R, Wormald PJ, Naidoo Y, Panizza B, Uren B, et al. Image-guided surgery influences perioperative morbidity from endoscopic sinus surgery: A systematic review and meta-analysis. Otolaryngol Head Neck Surg. 2013;149:17–29. doi: 10.1177/0194599813488519. [DOI] [PubMed] [Google Scholar]
- 4.Strauss G, Koulechov K, Röttger S, Bahner J, Trantakis C, Hofer M, et al. Evaluation of a navigation system for ENT with surgical efficiency criteria. Laryngoscope. 2006;116:564–72. doi: 10.1097/01.MLG.0000202091.34295.05. [DOI] [PubMed] [Google Scholar]


