Abstract
After the outbreak of severe acute respiratory syndrome (SARS) in November 2002, coronaviruses (CoVs) received worldwide attention. On December 1, 2019, the first case of coronavirus disease 2019 (COVID-19), caused by a novel coronavirus (SARS-CoV-2), was reported in Wuhan, China, and CoVs returned to public view. On January 30, 2020, the World Health Organization (WHO) declared that the COVID-19 epidemic is a public health emergency of international concern (PHEIC), and on March 11, 2020, the WHO classified COVID-19 as a pandemic disease. As of July 31, 2020, COVID-19 has affected 216 countries and regions, with 17,064,064 confirmed cases and 668,073 deaths, and the number of new cases has been increasing daily. Additionally, on March 19, 2020, there were no new confirmed cases in China, providing hope and valuable experience for the international community. In this review, we systematically compare COVID-19 and SARS in terms of epidemiology, pathogenesis and clinical characteristics and discuss the current treatment approaches, scientific advancements and Chinese experience in fighting the epidemic to combat the novel coronavirus pandemic. We also discuss the lessons that we have learned from COVID-19 and SARS.
Keywords: Coronavirus disease 2019 (COVID-19), SARS-CoV-2, SARS, Pandemic, Chinese experience
Background
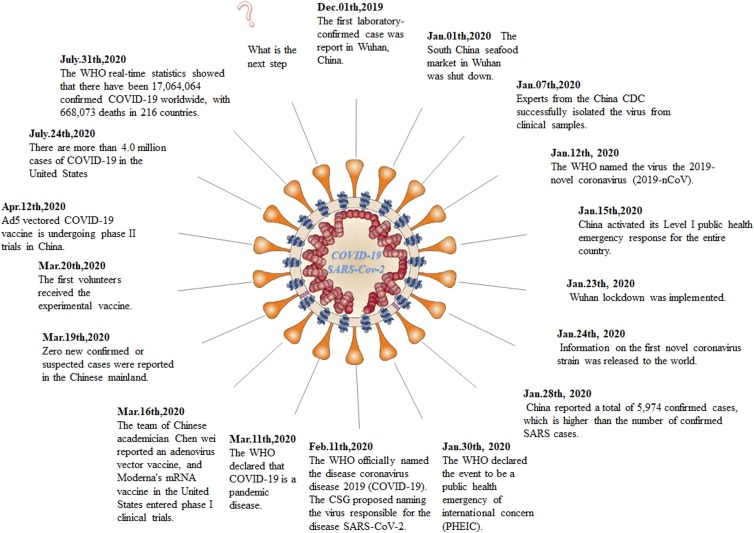
After the outbreak of severe acute respiratory syndrome (SARS) in November 2002 [1], coronaviruses (CoVs) received worldwide attention. After a lapse of 17 years and after the first report case of a coronavirus disease in Wuhan, China, on December 1, 2019 [2], pneumonia caused by a new coronavirus began spreading rapidly in China, with a similar trend globally. As the virus continued to spread, on March 11, 2020, the WHO declared that COVID-19 is a pandemic disease, making this the first time that a coronavirus infection has been regarded as a global pandemic, in contrast to SARS in 2002, which did not reach this level. As of July 31, 2020, 216 countries have been affected, with a global total of 17,064,064 confirmed cases and 668,073 deaths (WHO real-time statistics). The main timeline of the COVID-19 pandemic is shown in Fig. 1 . The outbreak has caused widespread fear and concern and threatens global health security.
Fig. 1.
Timeline of COVID-19 epidemic development before July 31, 2020.
The virus that causes COVID-19 named SARS-COV-2 [3], SARS-CoV-2 and SARS-CoV have highly similar gene sequences and behavior patterns. This paper summarizes the differences in the epidemiology, clinical manifestations, and treatment of SARS and COVID-19 during the two outbreaks, summarizes the lessons learned, and provides a comprehensive reference for the global epidemic prevention and treatment of COVID-19.
Epidemiology–origin, reservoirs and transmission
According to the WHO data, a total of 8442 cases of clinically diagnosed SARS were reported worldwide, with 919 deaths and 32 countries and regions affected. Most of the cases occurred in China, Canada and Singapore. Both outbreaks were first reported in China and resulted in a large number of infections. However, the COVID-19 has been more widespread and has spread faster than SARS, affecting populations around the globe [4].
There has been considerable discussion on the origin of the causative virus SARS-CoV-2 after the first reports of COVID-19 in Wuhan [5,6]. Rapid sequencing of the nearly 30,000-nucleotide SARS-CoV-2 genome was accomplished and announced worldwide on January 10, 2020, by Zhang's group and several others in China. CoV is an enveloped RNA virus that primarily causes respiratory and gastrointestinal infections [7]. Studies have shown that the nucleotide sequences of the SARS-CoV-2 and SARS-CoV genes are less than 80% identical [5]. However, the amino acid sequences of the seven conserved replicase domains in ORF1ab that are used for CoV species classification are 94.4% identical between SARS-CoV-2 and SARS-CoV, suggesting that the two viruses belong to the same species. Notably, studies have confirmed that SARS-CoV-2 uses the same cell entry receptor—angiotensin converting enzyme II (ACE2) - as SARS-CoV [4,8]. Wrapp et al. found that the binding affinity of SARS-CoV-2 to ACE2 was approximately 10–20 times that of SARS-CoV [9], which can provide one explanation for why SARS-CoV-2 has more human-to-human transmission than SARS-CoV. However, there is no clear evidence suggesting that SARS-CoV-2 has evolved from SARS-CoV.
To date, there is no evidence showing that SARS-CoV-2 originated in the seafood market. Recently, an article published in Nature Medicine on March 17 clearly showed that SARS-CoV-2 is not a laboratory construct or a purposefully manipulated virus. Several studies have shown that bats may be a potential reservoir for SARS-CoV-2 [10]. Sequencing of the viral genome showed 96.2% consistency across the whole genome sequences of bat CoV from Rhinolophus affinis and human SARS-CoV-2 [5], indicating that they may belong to the same ancestor; however, no bats were sold in the Wuhan seafood market [6]. In addition, protein sequence alignment and phylogenetic analysis showed that similar receptor residues were found in many species, which provided more possibilities for alternative intermediate hosts, such as pangolins or mink [11].
According to the research by the team of academician Zhong Nanshan, the incubation period of COVID-19 ranges from 0 to 24 days, with a median incubation period of 3 days. The population is generally susceptible to infection or infectious during the incubation period [12]. COVID-19 is highly contagious among humans, and older individuals and people with underlying diseases are especially affected. Based on the published data, the median patient age was 47–59 years in COVID-19 (similar to SARS and MERS), and 54.3−58.1% of patients were male in COVID-19 (the male-to-female ratio of 1:1.25 in SARS, and 1.82:1 in MERS) [1,8,12,13]. Some studies have reported that 1.2–2% of COVID-19 patients were children (6% in SARS and 2% in MERS) [[13], [14], [15], [16]]. According to the available data, children appear to be at lower risk for COVID-19 than adults and children are less symptomatic with less fatality, which is concordant to earlier epidemic outbreaks of SARS-CoV respectively [14,15]. On March 4, 2020, the national health commission issued the diagnosis and treatment program of COVID-19 pneumonia (trial seventh edition) [15], which indicated that transmission through respiratory droplets and close contact was the main transmission route of SARS-CoV-2. The virus can be spread by aerosol when an individual is exposed to a high concentration of aerosolized virus for a long time in a relatively closed environment. Since SARS-CoV-2 can be isolated from feces and urine, attention should be paid to aerosol or contact transmission from feces, urine or environmental pollution; other avenues of spread are not entirely clear [17]. A paper published in the Lancet argues that transmission through the conjunctiva of the eye cannot be ignored [18]. Other studies have suggested that there may be mother-to-child transmission (vertical transmission) [19]. In summary, to date, the transmission route of SARS-CoV-2 has not been completely clarified, and relevant protective measures and attention should not be reduced [20]. Regardless of the exact mechanisms by which SARS-CoV-2 was naturally selected, the ongoing surveillance of pneumonia in humans and other animals is clearly of utmost importance. According to a report published in Nature on March 20, 2020, 30%–60% of newly infected people have no symptoms or mild symptoms; however, their ability to spread the virus is not low, and covert coronavirus infections could be seeding new outbreaks. There is growing evidence that some infected people are highly contagious when their symptoms are mild or asymptomatic [21]. Understanding the proportion of cases of asymptomatic or mild illness is important for us to understand the cause of this particular pandemic, as indicated by Michael Osterholm, director of the center for infectious disease research and policy at the University of Minnesota [22].
Clinical characteristics and symptoms
SARS patients mainly present with fever and chills, accompanied by systemic and respiratory symptoms including mild fever and muscle pain. Severe respiratory failure and other organ dysfunction can occur during the incubation period from 1 to 16 days, commonly from 3 to 5 days. The onset is rapid, and the infectivity is strong, with fever as the first symptom. The course of the disease is 1–2 weeks. The prognosis of patients with headache, muscle soreness, general fatigue and diarrhea is related to the characteristics of the host (including age and sex) [23]. During hospitalization, the mean time from onset to severe respiratory distress was 9.8 to 3.0 days in 90.8% of SARS patients. Chest computed tomography (CT) shows ground-glass opacities with smooth interlobular septal thickening, sometimes with consolidation in a subpleural location [24,25].
SARS-CoV-2 infections generally exhibit milder symptoms than SARS-related infections. Zhong Nanshan's team and a number of studies [26,27] have shown that the main symptoms of COVID-19 patients are fever, cough and fatigue, and the infrequency of symptoms of the upper respiratory and gastrointestinal tracts suggests that the viral tropism of SARS-CoV-2 is different from that of SARS-CoV [28]. A study published in the New England Journal of Medicine (NEJM) on March 19 found that among COVID-19 patients, children have milder symptoms than adults, and it is not uncommon to see asymptomatic children [29]. The disease can be classified as mild, moderate, severe or critical according to whether there are clinical symptoms, whether there is pneumonia, the severity of the pneumonia, the presence of respiratory failure or shock, and whether there is other organ failure. The Beijing Center for Disease Control and Prevention suggests that the typical COVID-19 case exhibits a progressive disease course, and current clinical data show that most deaths occur among older patients. However, severe cases have been documented among young people with specific factors, especially those with chronic diseases, such as hypertension, diabetes, and cardiovascular disease; additionally, young people who have been using hormones or immunosuppressants for a long time and whose immune function is impaired are likely to have severe disease.
Laboratory examination showed that the white blood cell count in peripheral blood was normal or decreased, that the lymphocyte count was decreased, and that the degree of lymphocyte decline was correlated with disease severity [6]. In most patients, CRP and blood sedimentation were increased, and in some patients, liver enzymes, myoglobin, LDH, and D-dimer were increased. SARS-CoV-2 nucleic acids can be detected in a variety of specimens, including pharyngeal swabs, sputum, lower respiratory tract secretions, blood and feces [12]. RT-PCR and/or NGS methods have been used to detect SARS-CoV-2 nucleic acids in lower respiratory tract specimens (sputum or airway extracts) more accurately. By serological monitoring, positivity for the new coronavirus-specific IgM antibody is evident in most cases from 3 to 5 days after onset, and the titer of IgG antibody in the recovery stage is 4 times higher than that in the acute stage. Regarding pathological changes, the mucus and mucus accumulation in the airway are mainly caused by damage to the lungs and immune system. Other organs show mostly secondary damage due to different underlying diseases. Data from Zhong Nanshan's team showed that on admission, a ground-glass shadow was the most common radiological manifestation on chest CT (56.4%). Lymphocytopenia at admission affected for 83.2% of cases [12]. Radiological diagnostic sensitivity is limited, so findings should be verified by combining clinical symptoms and viral RNA detection. The first autopsy report of the COVID-19 in China indicated that the gross view of the lung had large amounts of airway viscous secretions, mainly caused by distal alveolar injury. Findings from a local histological study of COVID-19 cadaver biopsy samples published in Lancet Respiratory Medicine showed that the pathological features of COVID-19 were similar to those of SARS and MERS [30]. More systematic autopsy data and histopathological verification are needed for further study.
Treatment of COVID-19
At present, effective antiviral drugs against the pathogen are lacking, and the main treatments are isolation and symptomatic supportive treatment.
Supportive therapy
In general, the following strategies should be applied: bedrest and intense supportive treatment to ensure adequate heat; attention to water/electrolyte balance and maintenance of stability of the internal environment; and close monitoring of vital signs, namely, oxygen saturation. For patients with anoxic dyspnea in the acute phase, oxygen therapy should be given in time, and noninvasive or invasive ventilator support, which can best restore the patient's lung function, should be given when necessary.
On the basis of symptomatic treatment, we should also actively prevent and treat complications, treat basic diseases, prevent secondary infection and provide timely organ function support for severe and critical cases.
Respiratory support includes oxygen therapy; high-flow nasal catheter oxygen therapy or noninvasive mechanical ventilation; invasive mechanical ventilation; and salvage therapy. Salvage therapy is recommended for patients with severe Acute Respiratory Distress Syndrome (ARDS). Prone position ventilation should be performed for more than 12 h per day if there are adequate human resources. If conditions permit, extracorporeal membrane oxygenation (ECMO) should be considered as soon as possible.
Regarding circulation support, on the basis of full fluid resuscitation, we should also improve microcirculation, use vasoactive drugs, and perform hemodynamic monitoring if necessary.
In addition, intravenous infusion of gamma globulin may be considered for severe and critical pediatric cases. Severe or critical pregnancy cases should undergo termination of pregnancy, and cesarean section is the preferred delivery method. Patients often have anxiety and fear and should therefore undergo psychological counseling.
Drugs
Recently, based on the experiences of China and other countries worldwide in the fight against COVID-19, the WHO summarized and launched the four most promising COVID-19 treatment regimens: (1) remdesivir (2) chloroquine phosphate and hydroxychloroquine (3) lopinavir + ritonavir (4) lopinavir + ritonavir + interferon. The four treatment regimens will be widely and randomly tested in a number of countries and regions, and we hope to find an effective and safe treatment for COVID-19 as soon as possible.
Traditional Chinese medicine
COVID-19 is highly infectious and belongs to the category of traditional Chinese medicine (TCM) "epidemic" diseases, and "dampness, poison, stasis, closure and deficiency" are the characteristics of its pathogenesis [31]. TCM formulates treatment based on a symptom-based diagnosis, an approach that is increasingly emphasized in other disciplines [32].
TCM treatment is divided into observation periods and clinical treatment periods (confirmed cases), and the clinical treatment period is divided into mild, moderate, severe, critical and convalescent periods. Combined with clinical practice and integrated traditional and Western medicine, we screened out a batch of effective formulas represented by "three drugs and three parties" with obvious curative effects. These included jinhua qinggan granules, lianhuaqingwen (LH) capsules, xuebijing injection and qingfei paidu decoction, huashi baidu recipe, and xuanfei baidu recipe, among others.
The general prescription of qingfei paidu decoction is recommended in the clinical treatment period, and mild, moderate, severe, critical and convalescent have been described from three points of view: the clinical manifestation, recommended prescription, and dosage and method of administration. At the same time, the specific usage of Chinese patented drugs (including TCM injections) that are applicable to the severe and critical disease types was added to the scheme and followed the principle of dialectical adjustment from a small dosage. Blood-activating drugs such as xuebijing injection can improve microcirculation and effectively reduce the mortality of septic shock. Notably, patients with severe or critical disease such as systemic inflammatory response syndrome and/or multiorgan failure, can be treated with xuebijing injection.
According to the latest research by Zhong Nanshan's team, LH significantly inhibits SARS-CoV-2 replication, affects viral morphology and has anti-inflammatory activity in vitro [33]. These findings indicate that LH protects against viral attack, making LH treatment a novel strategy for controlling COVID-19.
The differences and similarities between SARS and COVID-19 are summarized in Table 1 .
Table 1.
Comparison of SARS and COVID-19.
| Items | SARS | COVID-19 |
|---|---|---|
| Pathogen | SARS-CoV | SARS-CoV-2 |
| Primary host | Bats | Bats (possible) |
| Intermediate host | Masked civet | Unknown |
| Reproduction number (R0) | 2–5 | 2–3 |
| Time to sequencing completion | Approximately 3 months | Approximately 3 weeks |
| Epidemiology | ||
| Propagation mode | Droplets or close contacts | Droplets or close contacts and high-density aerosols |
| Affected countries | 32 | >216 |
| Number of infected | 8422 | >17,064,064 |
| Number of deaths | 919 | >668,073 |
| Geographical distribution | Mainly in China, Canada, Singapore, and Vietnam | Global |
| Epidemic prevention | Community lockdown only | Community, city, even national lockdown |
| Vaccine | No FDA-approved vaccine. | The first group of volunteers has completed a phase I clinical trial to inject the vaccine. |
| Clinical characteristics | ||
| Latency | 3−5 days on average | 3−7 days on average |
| Susceptible population | Young adults | All people, especially older individuals and people with underlying diseases |
| Clinical type | Mild and severe | Mild, moderate, severe, critical and convalescent |
| Symptoms | Fever, cough, myalgia, dyspnea, and diarrhea | Main: Fever, dry cough, fatigue Rare: Upper respiratory symptoms, gastrointestinal symptoms |
| Pediatric infections | Similar to adults | Milder than adults, with some asymptomatic cases |
| Laboratory findings | Leukopenia, lymphopenia, thrombocytopenia, mild abnormal liver function, elevated CRP. Some patients show electrolyte disorder with hyponatremia/hypokalemia or coagulopathy and prolonged clotting time (APTT). D-dimer levels can be increased. | The total white blood cell count in peripheral blood is normal or decreased, and the lymphocyte count is decreased. CRP and blood sedimentation are increased. In most patients, the liver enzymes, myoglobin, LDH, and D-dimer levels are increased. |
| Pathological findings | ||
| Main targets of viral attack | Lungs, immunological organs, and systemic small vessels | Lungs |
| Pathological findings of lungs | Fibrosis and consolidation | Exudative inflammation. Mucus and mucus accumulation in the airway. |
| Imaging features | ||
| CT | Ground-glass opacities with smooth interlobular septal thickening, sometimes with consolidation in a subpleural location. | Ground-glass opacities (most common), bilateral patchy shadows, local patchy shadows, interstitial abnormalities. |
| Diagnostic methods | RT-PCR, rRT-PCR, RT-LAMP, rRT-LAMP, Coronavirus testing kits | SARS-CoV-2 nucleic acid testing kits (fluorescent PCR method) and the SARS-CoV-2 nucleic acid sequencing system |
| Treatment | ||
| General treatment | Supportive therapy and antiviral drugs. | Supportive therapy and antiviral drugs. |
| Severe treatment | Corticosteroid therapy, antiviral agents, anti-infection agents, mechanical ventilation. | On the basis of symptomatic treatment, preventing complications and secondary infections, treating underlying diseases, and providing respiratory and circulatory support including ventilator and ECMO use. |
| TCM treatment | Used domestically. TCM treatment led to a significant reduction in mortality, a shortened duration of fever, symptom relief, reductions in chest radiograph abnormalities, and reductions in secondary fungal infections among patients receiving glucocorticoids. |
Used internationally. TCM treatment plays a significant role in reducing mortality, suppressing progression to severe disease, and curing patients with moderate or mild symptoms. |
| Prognosis | ||
| Mortality rate | 11% | Lower than that of SARS |
SARS: Severe acute respiratory syndrome; COVID-19: Coronavirus disease 2019; CRP: C-reactive protein; APTT: Activated partial thromboplastin time; LDH: Lactate dehydrogenase; RT-PCR: Reverse transcription polymerase chain reaction; RT-LAMP: Reverse transcription Loop-MediatedIsothermal Amplification; PCR: Polymerase chain reaction; ECMO: Extracorporeal Membrane Oxygenation; TCM: Traditional Chinese medicine.
Lessons
On March 11, the WHO declared the outbreak of COVID-19 to be a "pandemic" and on July 31, 2020, the global epidemic had spread to 216 countries and regions. Among these countries, the United States has confirmed a total of 4,388,566 cases, both Brazil and India had more than 1,600,000 confirmed patients and the epidemic is in a period of rapid growth. Additionally, on March 19, the Chinese mainland, including Hubei Province, reported zero new confirmed or suspected cases, and the new confirmed cases was lower than 10 everyday now. During the outbreak, China acted quickly; an epidemiological investigation was carried out on December 29. On January 1, the South China seafood market in Wuhan was closed. On January 23, the Wuhan lockdown was implemented. On January 25, the CPC central committee set up a leading group to address the epidemic. Digital media was used to monitor and report the epidemic situation in real time [34]. The government formulated epidemic prevention policies (strict restrictions on travel and public gatherings; closure of public places; implementation of strict temperature monitoring across the country; correct use of masks; suspension of work and school; personal monitoring at home, etc.), and people throughout the country actively cooperated.
In an interview on March 18, the WHO representative in China, Dr. Colliers, said that China has shown the world that the trajectory of the epidemic can be changed. Typically, an epidemic grows exponentially, peaks, and then gradually begins to decline after all susceptible people have been infected or become ill. But that has not occurred in China. The epidemiological curve in China is irregular, the epidemic has been snuffed out in its growth phase, and the transmission of the virus has been blocked, as is clearly shown by both the collected data and the observed social reality. The national emergency response appears to have delayed the growth and limited the size of the COVID-19 epidemic in China, averting hundreds of thousands of cases by 19 February (day 50) [35]. Chinese experience shows that not all infectious diseases need to manifest as large outbreaks that overwhelm health systems. Every country can learn from this experience and apply the obtained knowledge on its own terms.
-
(1)
Early detection: Viral detection reagents play an important role in this process. Early in the outbreak, a community in the heart of the Italian epidemic conducted an experiment in controlling the epidemic and was able to stop the rise in cases (all residents were tested repeatedly for the virus, regardless of whether they had symptoms). After the infection is confirmed, strict quarantine measures are imposed on contacts. This highlights the importance of detecting and isolating carriers of the virus. Various measures should be taken to strengthen the effective control of the source of infection.
-
(2)
Early diagnosis: Integrated medical thinking is required because viruses involve the respiratory system, oral cavity, digestive tract, eyes, skin, genital tract, and central nervous system.
-
(3)
Early quarantine: The population is generally susceptible, regardless of race, with slightly more males than females affected, with more older patients and fewer pediatric cases.
-
(4)
Early treatment: Importance should be attached to the use of TCM. In response to this new epidemic, TCM has demonstrated its ability to treat acute and critical diseases, showing that its clinical efficacy is not inferior to that of Western medicine and highlighting the characteristics and advantages of TCM. The role of TCM is also reflected in the whole process of fighting against the epidemic, including prevention, treatment and rehabilitation.
TCM plays an important role in preventing the progression of mild or moderate disease to severe or critical disease. In the treatment of severe and critical cases, TCM also plays a very important role, especially in reducing high fever, promoting exudation and absorption, improving oxygenation levels, and reducing pulmonary fibrosis. The use of both Chinese and Western medicine has effectively reduced the death rate.
It is undeniable that both Chinese and Western medicine have their own limitations, but in the fight against the COVID-19 epidemic, with the implementation of integrated traditional and Western medicine clinical treatment programs, the advantages of traditional and Western medicine can be complementary. Through continuous optimization and improvement of integrated TCM and Western medicine diagnosis and treatment programs and screening of clinically effective TCM and Western medicine, the cure rate of COVID-19 has steadily improved. The treatment of the epidemic fully reflects the importance of the use of both TCM and Western medicine.
-
(5)
Professor Zhong Nanshan noted that SARS-CoV-2 infection does not provide immunity from one infection for life and cannot be solved by immunity.
A paper published in the NEJM indicated that China's aggressive response may have delayed the global spread of the current outbreak and bought time for its control [36]. However, anti-Chinese hostility has been a recurrent problem, both with SARS in 2002 and COVID-19 today [36]. The WHO stresses that the origin of the novel coronavirus is still uncertain and opposes the association of viruses with specific countries and regions and the associated stigmatization.
At present, COVID-19 is spreading in many parts of the world, and it is essential that the international community works together to fight the epidemic. China has taken the lead in building a community of shared futures to fight the epidemic: China has provided anti-epidemic material assistance to 82 other countries and international organizations, including Japan, Korea, Italia, France and Serbia. More importantly, China is willing to share its experience with the rest of the world. China has recently sent anti-epidemic teams to Iran, Iraq and Italy. Although the development of therapeutics and vaccines for the treatment of COVID-19 is still in its early stage, there has been some significant progress in the research area from complete genome sequencing of SARS-CoV-2 to the beginning of clinical trials with COVID-19 vaccines [37]. As Dr. Aylward, the foreign team leader of the China-WHO joint investigation team on COVID-19 said that China's approach to fighting the epidemic can be replicated, and other countries do not have to start from scratch with Chinese experience [38]. WHO Director-General Tedros Adhanom Ghebreyesus said that the first trial of the COVID-19 vaccine has begun, and the first volunteers have received the experimental vaccine, which is an unprecedented scientific triumph. Academician Chen Wei's team found that the Ad5 vectored COVID-19 vaccine is tolerable and immunogenic in healthy adults, and ongoing phase 2 trial in China (NCT04341389) will provide more information on the safety and immunogenicity [39]. The last enemy of the humanity is the virus, that's what my mentor told me, Walter Ian Lipkin said. The observation of zero new COVID-19 cases in Wuhan is a source of hope for the world, and we hope that all countries will work together to build a community of shared experiences in the fight against COVID-19 and that the world will quickly overcome this pandemic [40].
The lessons we have learned from the SARS and COVID-19 epidemics are summarized in Table 2 .
Table 2.
Lessons learned from SARS and COVID-19.
| SARS | COVID-19 | |
|---|---|---|
| Lesson 1 | Enhanced monitoring of wildlife sources. | Closing wildlife markets, forbidding wildlife trade, and prohibiting wildlife consumption as food. |
| Lesson 2 | Unrestricted sharing of information. Travel restrictions partly. |
International cooperation. Unrestricted, accurate, timely and effective information dissemination. Travel restrictions; Community, city, and even national lockdown. Increased viral transmission due to human mobility and quick and convenient public transportation. |
| Lesson 3 | Building up an epidemic reporting system network. | Rapid responses: National and local government measures; Rapid mobilization of healthcare personnel to treat patients; Developing guidelines to control viral transmission; Cloud computing and big data to control the epidemic. |
| Lesson 4 | Reducing viral transmission: Isolation of suspect cases; Regular disinfection; Wearing of masks and washing of hands. |
Rigorous infection control: Aggressive quarantine; Regular disinfection; Wearing masks correctly; Effective hand washing; Minimal social contact. |
| Lesson 5 | The importance of rapid testing and isolation. | Early testing, early reporting, early isolation, early diagnosis, early treatment. Although CT examination is important for identifying suspected cases, it does not replace accurate diagnosis with nucleic acid testing kits. |
| Lesson 6 | Urgent construction of a temporary hospital. | Reassignment of medical facilities: Flexible use of public facilities for temporary hospitals. Differentiated patient admittance: Existing hospitals for patients with severe or critical disease; Mobile, field, or temporary medical facilities for patients with mild or moderate disease. |
| Lesson 7 | Corticosteroids was used to treat patients with severe disease. | Integral medicine: Multidisciplinary and multiorgan treatment. Critical care medicine is crucial for patients with severe or critical disease. Oxygen supplementation and mechanical ventilation are key to treatment of patients with severe or critical disease. |
| Lesson 8 | TCM was effective in treating SARS and reduced complications due to corticosteroid use. Building a number of TCM hospitals nationwide and developing TCM. |
Defining the importance of TCM and reintegrated treatment with TCM and Western medicine. TCM was effective in decreasing mortality, suppressing progression to severe disease, and curing mild or moderate cases. Shaping a protocol to use a batch of effective TCM formulas. |
| Lesson 9 | There is no FDA-approved vaccine for SARS. | Accelerating the development of vaccines. |
| Lesson 10 | Virus has no borders. Viral infection occurs regardless of socioeconomic status. Human life is not simply a number. Medical personnel are the backbone fighting against COVID-19 and SARS by saving patients' lives and providing recommendations for epidemic control. |
|
SARS: Severe acute respiratory syndrome; COVID-19: Coronavirus disease 2019; CT: Computed tomography; TCM: Traditional Chinese medicine; FDA: Food and Drug Administration.
Conclusion
SARS-CoV-2 poses a threat to public health because it is highly infectious, has a high incidence of susceptibility and can cause serious illness or death. A total of 668,073 people in 216 countries have died from COVID-19. The emergence of SARS-CoV and SARS-CoV-2 suggests that coronaviruses will pose a lasting threat to humans and that the current epidemic will eventually be brought under control. The collective memory of SARS and SARS-CoV-2 may gradually fade, but we must not forget the lessons learned from the SARS and current SARS-CoV-2 outbreaks. More accurate and effective drugs and vaccines need to be studied. At the same time, nations worldwide need to work together to fight COVID-19 to shorten hospital stays and reduce the consumption of healthcare resources, and we must prepare for the next epidemic.
Funding
This work was supported by the National Natural Scientific Foundation of China (81870767 & 81570978), the Project of Jiangsu Provincial Medical Youth Talent (QNRC2016118), the Key Project of Science and Technology Department of Jiangsu Province (BL2014018), and the Nanjing Medical Science and Technique Development Foundation (ZKX17033).
Competing interests
None declared.
Ethical approval
Not required.
Authors' contributions
Qin Liu initiated this Personal View and wrote the first draft. Kaiyuan Xu assisted with the literature search and figures. Xiang Wang and Wenmei Wang reviewed and edited the manuscript. All authors read and approved the final manuscript.
References
- 1.Zhong N.S., Zheng B.J., Li Y.M., Poon L.L.M., Xie Z.H., Chan K.H., et al. Epidemiology and cause of severe acute respiratory syndrome (SARS) in Guangdong, People’s Republic of China, in February, 2003. Lancet. 2003;362(9393):1353–1358. doi: 10.1016/S0140-6736(03)14630-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Huang C., Wang Y., Li X., Ren L., Zhao J., Hu Y., et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395(10223):497–506. doi: 10.1016/S0140-6736(20)30183-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Cohen J., Kupferschmidt K. Labs scramble to produce new coronavirus diagnostics. Science. 2020;367(6479):727. doi: 10.1126/science.367.6479.727. [DOI] [PubMed] [Google Scholar]
- 4.Petrosillo N., Viceconte G., Ergonul O., Ippolito G., Petersen E. COVID-19, SARS and MERS: are they closely related? Clin Microbiol Infect. 2020;26(6):729–734. doi: 10.1016/j.cmi.2020.03.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Zhou P., Yang X.L., Wang X.G., Hu B., Zhang L., Zhang W., et al. A pneumonia outbreak associated with a new coronavirus of probable bat origin. Nature. 2020;579(7798):270–273. doi: 10.1038/s41586-020-2012-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Wu F., Zhao S., Yu B., Chen Y.M., Wang W., Song Z.G., et al. A new coronavirus associated with human respiratory disease in China. Nature. 2020;579(7798):265–269. doi: 10.1038/s41586-020-2008-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wu A., Peng Y., Huang B., Ding X., Wang X., Niu P., et al. Genome composition and divergence of the novel coronavirus (2019-nCoV) originating in China. Cell Host Microbe. 2020;27(3):325–328. doi: 10.1016/j.chom.2020.02.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Xu J., Zhao S., Teng T., Abdalla A.E., Zhu W., Xie L., et al. Systematic comparison of two animal-to-human transmitted human coronaviruses: SARS-CoV-2 and SARS-CoV. Viruses. 2020;12(2):244. doi: 10.3390/v12020244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Wrapp D., Wang N., Corbett K.S., Goldsmith J.A., Hsieh C.L., Abiona O., et al. Cryo-EM structure of the 2019-nCoV spike in the prefusion conformation. Science. 2020;367(6483):1260–1263. doi: 10.1126/science.abb2507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Paraskevis D., Kostaki E.G., Magiorkinis G., Panayiotakopoulos G., Sourvinos G., Tsiodras S. Full-genome evolutionary analysis of the novel corona virus (2019-nCoV) rejects the hypothesis of emergence as a result of a recent recombination event. Infect Genet Evol. 2020;79:104212. doi: 10.1016/j.meegid.2020.104212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Liu Z., Xiao X., Wei X., Li J., Yang J., Tan H., et al. Composition and divergence of coronavirus spike proteins and host ACE2 receptors predict potential intermediate hosts of SARS-CoV-2. J Med Virol. 2020;92(6):595–601. doi: 10.1002/jmv.25726. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Guan W.J., Ni Z.Y., Hu Y., Liang W.H., Ou C.Q., He J.X., et al. Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med. 2020;382(18):1708–1720. doi: 10.1056/NEJMoa2002032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Azhar E.I., Hui D.S.C., Memish Z.A., Drosten C., Zumla A. The middle east respiratory syndrome (MERS) Infect Dis Clin North Am. 2019;33(4):891–905. doi: 10.1016/j.idc.2019.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Rehman S., Majeed T., Azam Ansari M., Ali U., Sabit H., Al-Suhaimi E.A. Current scenario of COVID-19 in pediatric age group and physiology of immune and Thymus response. Saudi J Biol Sci. 2020 doi: 10.1016/j.sjbs.2020.05.024. [published online ahead of print, 2020 May 15] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Zhou M.Y., Xie X.L., Peng Y.G., Wu M.J., Deng X.Z., Wu Y., et al. From SARS to COVID-19: what we have learned about children infected with COVID-19. Int J Infect Dis. 2020;96:710–714. doi: 10.1016/j.ijid.2020.04.090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Zhong N.S., Wong G.W.K. Epidemiology of severe acute respiratory syndrome (SARS): adults and children. Paediatr Respir Rev. 2004;5(4):270–274. doi: 10.1016/j.prrv.2004.07.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Li Q., Guan X., Wu P., Wang X., Zhou L., Tong Y., et al. Early transmission dynamics in Wuhan, China, of novel coronavirus-infected pneumonia. N Engl J Med. 2020;382(13):1199–1207. doi: 10.1056/NEJMoa2001316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Nation Health Commission of the People’s Republic of China . 2020. Notice on the Issuance of COVID-19 Protocol (Trial Seventh Edition)http://www.nhc.gov.cn/yzygj/s7653p/202003/46c9294a7dfe4cef80dc7f5912eb1989.shtml February 19, (in Chinese) [Google Scholar]
- 19.Lu C.W., Liu X.F., Jia Z.F. 2019-nCoV transmission through the ocular surface must not be ignored. Lancet. 2020;395(10224):e39. doi: 10.1016/S0140-6736(20)30313-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Rothan H.A., Byrareddy S.N. The epidemiology and pathogenesis of coronavirus disease (COVID-19) outbreak. J Autoimmun. 2020;109:102433. doi: 10.1016/j.jaut.2020.102433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Chen H., Guo J., Wang C., Luo F., Yu X., Zhang W., et al. Clinical characteristics and intrauterine vertical transmission potential of COVID-19 infection in nine pregnant women: a retrospective review of medical records. Lancet. 2020;395(10226):809–815. doi: 10.1016/S0140-6736(20)30360-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Qiu J. Covert coronavirus infections could be seeding new outbreaks. Nature. 2020 doi: 10.1038/d41586-020-00822-x. published online Mar 20. [DOI] [PubMed] [Google Scholar]
- 23.Mizumoto K., Kagaya K., Zarebski A., Chowell G. Estimating the asymptomatic proportion of coronavirus disease 2019 (COVID-19) cases on board the Diamond Princess cruise ship, Yokohama, Japan, 2020. Eurosurveillance. 2020;25(10):2000180. doi: 10.1101/2020.03.05.20030502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Wang J.T., Sheng W.H., Fang C.T., Chen Y.C., Wang J.L., Yu C.J., et al. Clinical manifestations, laboratory findings, and treatment outcomes of SARS patients. Emerg Infect Dis. 2004;10(5):818–824. doi: 10.3201/eid1005.030640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Goh J.S., Tsou I.Y., Kaw G.J. Severe acute respiratory syndrome (SARS): imaging findings during the acute and recovery phases of disease. J Thorac Imaging. 2003;18(3):195–199. doi: 10.1097/00005382-200307000-00010. [DOI] [PubMed] [Google Scholar]
- 26.Guan W.J., Liang W.H., Zhao Y., Liang H.R., Chen Z.S., Li Y.M., et al. Comorbidity and its impact on 1590 patients with COVID-19 in China: a nationwide analysis. Eur Respir J. 2020;55(5):2000547. doi: 10.1183/13993003.00547-2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Chen N., Zhou M., Dong X., Qu J., Gong F., Han Y., et al. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study. Lancet. 2020;395(10223):507–513. doi: 10.1016/S0140-6736(20)30211-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Lee N., Hui D., Wu A., Chan P., Cameron P., Joynt G.M., et al. A major outbreak of severe acute respiratory syndrome in Hong Kong. N Engl J Med. 2003;348(20):1986–1994. doi: 10.1056/NEJMoa030685. [DOI] [PubMed] [Google Scholar]
- 29.Lu X., Zhang L., Du H., Zhang J., Li Y.Y., Qu J., et al. SARS-CoV-2 infection in children. N Engl J Med. 2020;382(17):1663–1665. doi: 10.1056/NEJMc2005073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Xu Z., Shi L., Wang Y., Zhang J., Huang L., Zhang C., et al. Pathological findings of COVID-19 associated with acute respiratory distress syndrome. Lancet Respir Med. 2020;8(4):420–422. doi: 10.1016/s2213-2600(20)30076-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Yang D.W., Wang Y.P., Zhang H.M., Zhang Y., Zhang Y.G., Guo Y., et al. Thoughts on the etiology and pathogenesis of COVID-19 in Traditional Chinese medicine. J Tradit Chin Med. 2020 http://kns.cnki.net/kcms/detail/11.2166.R.20200217.0906.002.html published online Feb 17 (in Chinese) [Google Scholar]
- 32.Idborg H. Symptom-based stratification of autoimmune diseases. Lancet Rheumatol. 2019;1:e76–e77. doi: 10.1016/S2665-9913(19)30047-5. [DOI] [PubMed] [Google Scholar]
- 33.Li R.F., Hou Y.L., Huang J.C., Pan W.Q., Ma Q.H., Shi Y.X., et al. Lianhuaqingwen exerts anti-viral and anti-inflammatory activity against novel coronavirus (SARS-CoV-2) Pharmacol Res. 2020;156:104761. doi: 10.1016/j.phrs.2020.104761. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Li C., Chen L.J., Chen X., Zhang M., Pang C.P., Chen H. Retrospective analysis of the possibility of predicting the COVID-19 outbreak from Internet searches and social media data, China, 2020. Eurosurveillance. 2020;25(10):2000199. doi: 10.2807/1560-7917.ES.2020.25.10.2000199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Tian H., Liu Y., Li Y., Wu C.H., Chen B., Kraemer M.U.G., et al. An investigation of transmission control measures during the first 50 days of the COVID-19 epidemic in China. Science. 2020;368(6491):638–642. doi: 10.1126/science.abb6105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Jones D.S. History in a crisis - lessons for Covid-19. N Engl J Med. 2020;382(18):1681–1683. doi: 10.1056/NEJMp2004361. [DOI] [PubMed] [Google Scholar]
- 37.Ahn D.G., Shin H.J., Kim M.H., Lee S., Kim H.S., Myoung J., et al. Current status of epidemiology, diagnosis, therapeutics, and vaccines for novel coronavirus disease 2019 (COVID-19) J Microbiol Biotechnol. 2020;30(3):313–324. doi: 10.4014/jmb.2003.03011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Li H., Chen X., Huang H. The novel coronavirus outbreak: what can be learned from China in public reporting? Glob Health Res Policy. 2020;5:9. doi: 10.1186/s41256-020-00140-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Zhu F.C., Li Y.H., Guan X.H., Hou L.H., Wang W.J., Li J.X., et al. Safety, tolerability, and immunogenicity of a recombinant adenovirus type-5 vectored COVID-19 vaccine: a dose-escalation, open-label, non-randomised, first-in-human trial. Lancet. 2020;395(10240):1845–1854. doi: 10.1016/S0140-6736(20)31208-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.The Lancet COVID-19: learning from experience. Lancet. 2020;395(10229):1011. doi: 10.1016/S0140-6736(20)30686-3. [DOI] [PMC free article] [PubMed] [Google Scholar]