Abstract
Many diseases and conditions affect a relatively localized area of the body. They can be treated either by direct deposition of drug in the target area, or by giving the drug systemically. Here we review nanoparticle-based approaches to achieving both. We highlight advantages and disadvantages that nanoscale solutions have for locally administered therapies, with emphasis on the former. We discuss strategies to enable systemically delivered nanoparticles to deliver their payloads at specific locations in the body, including triggering (local and remote) and targeting.
Keywords: drug delivery, nanosystems, local administration, systemic administration, local effects
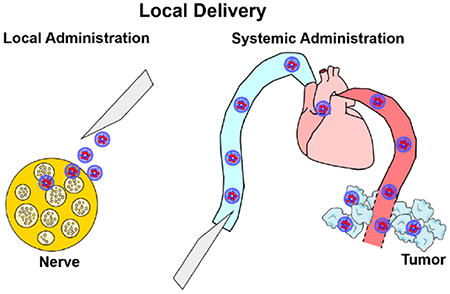
Graphical Abstract
1. Introduction
Drug delivery technologies can be categorized according to the method of administration (i.e. how they are introduced into the body) and the intended site of action.[1] Both of these can be local or systemic (Figure 1).[1–4] This review addresses the use of nanoparticles for local effect, administered either locally or systemically. Please note that administration is not the same as delivery; the former denotes how an agent is introduced into the body, the latter can also relate to where in the body the agent ends up. As we will see, a systemically-administered targeted nanoparticle can deliver drugs to a given site in the body, where the drug will have localized effect.
Figure 1.
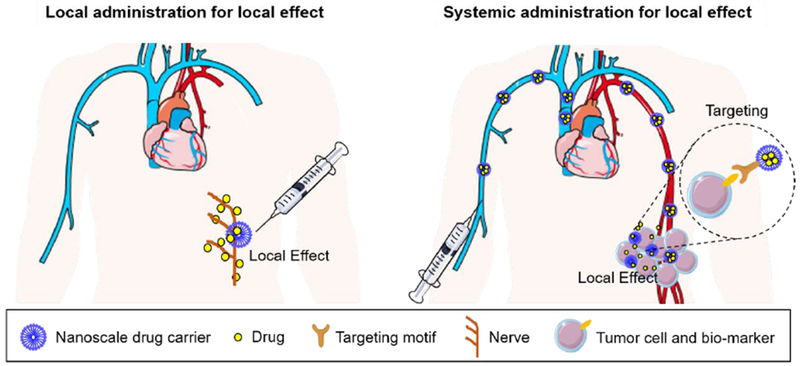
Administration and effects of nanoscale drug delivery systems (DDSs). Schematic illustration showing drug delivery system being administered locally for a local or systemic effect, or administered systemically but targeted to have a local effect.
Systemic effect is usually achieved after intravenous or oral administration of drugs: the drug is distributed throughout the body, even if the target is a relatively small part of the body. For example, one might take acetaminophen by mouth for a headache, or amoxicillin by mouth for middle ear infections, or intravenous propranolol for an abnormal cardiac rhythm. In all those cases, the drug is distributed throughout the body in order to achieve a therapeutic concentration at the intended target site. The presence of high drug concentrations at off-target sites leads to side effects (liver toxicity, diarrhea, and bronchospasm respectively in the examples in the preceding sentence). It is partly the avoidance of those side effects that makes local administration or delivery for local effect appealing.
With local drug action, the pharmacologic effects (both desirable and undesirable) are ideally restricted to a relatively localized part of the body: a specific nerve, an extremity, a particular organ, etc. Often such localization is not perfect but rather achieves an improvement in the proportion of the drug dose in the target tissue. The major advantages of localized drug action are that efficacy can be improved and perhaps drug access to off-target sites can be reduced, minimizing toxicity. In this way, the therapeutic ratio can be improved (Figure 2a), allowing either safer treatment for the same effect, or dose escalation (better effect) with the same toxicity.
Figure 2.
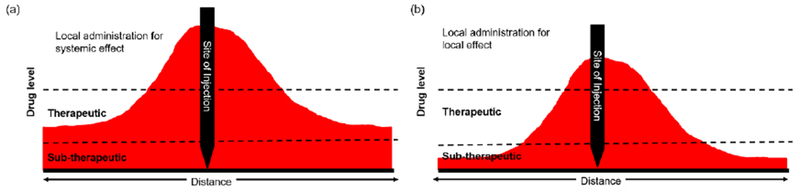
Drug levels after local administration for systemic effect or local effect. (a) Drug level needed for systemic effect. (b) Drug level for local effect.
Local effect can be achieved by direct local administration of the DDS at the desired site of action: by injection or implantation, by inhalation, topically, etc. Systemic effect can also be achieved by local administration. In both cases, the drug or drug depot is placed in contact with the total body water. However, with local administration for systemic effect, the dose given is sufficient to spread throughout the body at therapeutic concentrations (Figure 2a); examples would be subcutaneous growth hormone, free or encapsulated. With local administration for local effect, the dose is only sufficient for local effect (Figure 2b); examples include peripheral nerve blocks with local anesthetics, free or encapsulated. For locally administered DDS, which are usually depot systems, one often wants the DDS to contain as much drug as possible, and release the drugs for as long as possible to reduce the need for repeated administration. These design considerations argue against the use of nanoparticles, which generally have worse loading efficiencies,[5–7] tend to leave the site of injection more rapidly,[8] and degrade and release drug more rapidly.[9] There are however, situations where the nanoscale is advantageous even for local administration. For example, because of their small size, nanoparticles are better able to penetrate a variety of tissues.[10–12] Their greater surface area-to-volume ratio also enhances surface binding.[13] (The volume of a sphere is proportional to the third power of the radius (V = 4/3πr3), while the surface area (SA) is proportional to the second power (SA = 4πr2). The surface area-to volume ratio is therefore inversely proportional to the radius.) Targeting or binding functions can be further enhanced by surface modification with ligands or cell penetrating peptides (CPP).[14–18]
Local effect can also be achieved after systemic (intravenous) administration. This usually entails achieving means of causing drug delivery systems in the bloodstream to accumulate in a particular location. Methods of administration of drug delivery systems, and their intended site of delivery and action are summarized in Table 1.
Table 1.
Methods of administration of drug delivery systems, and their intended site of delivery and action. The shaded boxes are the subject of this review.
| Method of administration | |||
|---|---|---|---|
| Local | Systemic | ||
| Intended site of drug delivery (and action) | Local |
Concept. DDS applied at particular site to affect adjacent structures. Example. Nanoparticles deposited next to nerve, to penetrate that nerve |
Concept. DDS applied into systemic circulation but targeted to affect a specific site. Example. Intravenous nanoparticles photo-targeted to bind in the eye. |
| Systemic |
Concept. DDS applied at an accessible location, with drugs intended to affect remote locations. Example. Subcutaneous microparticles containing growth hormone. |
Concept. DDS applied into systemic circulation, to affect the entirely of the body. Example. Intravenous nanoparticles containing an antifungal agent. |
|
Here, the use of small – usually nanoscale (less than 400 nm) – particles is mandated by the need to avoid causing emboli [19] in the blood stream and to take advantage of size-dependent phenomena, [20] such as altered blood vessel permeability in some organs and disease states.[21,22]
2. Local administration of nanoparticles for local effect
As discussed above, larger particles have many properties that one would find advantageous in localized drug delivery. However there are circumstances where nanoscale particles might be advantageous.
2.1. Enhancing tissue penetration
There are many biological barriers preventing drugs from getting to their intended sites of action.[23] These barriers may be obvious physical entities, such as skin, or may be more poorly defined, such as the connective tissue around a nerve and/or the various sheaths that surround it (per-, epi-, and endoneurium), and/or the lipid-rich Schwann cells around some axon types. Barriers in other tissues (such as the stratum corneum in skin, mucus in intestines and lungs, the blood-brain barrier, etc.) only allow drugs with fairly specific physicochemical properties to cross.[24–33]
DDSs also can have difficulty crossing barriers, although nanoscale DDSs may have less difficulty than do larger (micron-scale) systems. For example, 15 nm gold nanoparticles (AuNPs) penetrated the stratum corneum better than did 102 nm and 198 nm AuNPs, and after crossing it, the smaller nanoparticles reached deeper into skin.[34] The shape and surface characteristics of nanoparticles can also influence tissue penetration.[35,36] For example, more gold nanorods (~20 nm width, 2.8 ± 0.5 aspect ratio) penetrated into skin than did spherical AuNPs (~15 nm);[35] colloidal AuNPs modified with cell-penetrating peptides (CPPs) accumulated in skin to a greater degree than did than polyethylene glycol (PEG)-functionalized AuNPs, and they were able to penetrate more deeply.[35] Negatively charged AuNPs penetrated skin more readily than did neutrally and positively charged AuNPs of the same size (~15 nm).[36]
The impact of smaller size within the nanoscale is seen in some other tissues. In local anesthesia, drugs are deposited outside of nerve bundles and then diffuse inward, where they have their pharmacological effects. This diffusion can be particularly difficult for very hydrophilic compounds.[37,38] A variety of approaches have been developed to increase that flux, including the use of chemical permeation enhancers and ultrasound. Hollow silica nanoparticles smaller than 70 nm in diameter (Figure 3a) can also penetrate nerve (Figure 3b,c); larger cannot.[39] Such particles loaded with the local anesthetic tetrodotoxin and injected at the sciatic nerve in rats increased the frequency of successful nerve blocks and significantly prolonged the duration of local anesthesia duration compared to free drug.
Figure 3.

Penetration of hollow silica nanoparticles (HSN) can penetrate. (a) TEM image of ~30 nm HSN. (b,c) HSN distribution in the sciatic nerve tissue after 4 h injection. The HSN were fluorescently labeled with fluorescein (green). The scale bars is 200 μm. Adapted from [39], copyright from American Chemical Society, 2018.
Mucus is a viscoelastic gel layer that typically protects surfaces of the gastrointestinal tract, lung airways, and other mucosal tissues.[40] Particles targeted to these tissues can be trapped and removed by mucus,[40,41] thereby limiting their effectiveness. Nanoformulations ~200 nm in diameter achieved higher mucus distribution and tissue penetration than did micron-scale formulations; budesonide-loaded nanoformulations provided enhanced drug delivery in a murine model of inflammatory bowel disease (IBD).[42] As in skin, particle morphology could have an effect: cylindrical nanoparticles had superior transport in mucus compared with nanospheres with the same chemical composition and surface charge.[43]
2.2. Improved binding to surfaces
Prolonged local retention of DDS is important for sustained local release and prolonged local effect. Microparticles usually are retained in tissues longer than are nanosized particles, e.g. after injection.[44,45] However, in some circumstances, tissue retention may be primarily dictated by particle binding to tissue. In those cases, nanoparticles may have an advantage because of their higher surface area to volume ratio.
One example of this is seen with intravenous regional anesthesia (IVRA, also known as the Bier block), which is commonly used to anesthetize extremities for surgery.[46–48] Here local anesthetics are infused into an extremity that is isolated from the circulation by a tourniquet. Attempts to improve the efficacy and duration of IVRA by infusing nanoformulations showed that smaller particles were more effective than larger ones, and better than free drug.[13] Specifically, 15 nm micellar bupivacaine infused into the veins of an isolated rat tail provided regional anesthesia that lasted twice as long as that from a larger dose of free bupivacaine. 100 nm liposomes with similar release kinetics did not provide any local anesthesia. It was hypothesized that the longer anesthesia from small particles was related to better binding to cells (Figure 4a) and blood vessels (Figure 4b,c), presumably from the better surface area to volume ratio.
Figure 4.
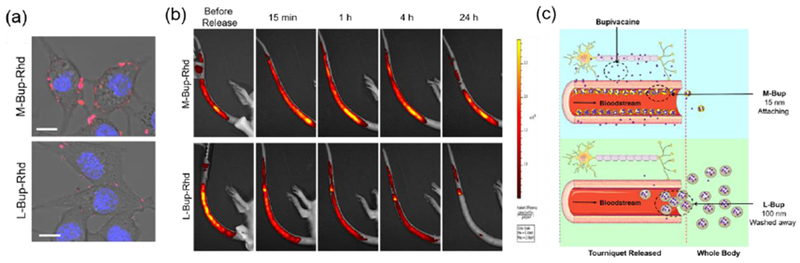
Comparison of binding by smaller micelles (M-Bup-Rhd, 15 nm) and larger liposomes (L-Bup-Rhd, 100 nm), both containing bupivacaine (Bup) and the fluorophore rhodamine (Rhd). (a) Confocal laser scanning microscopy of cells incubated with M-Bup-Rhd or L-Bup-Rhd. Red, rhodamine (Rhd); blue, nuclei (Hoechst33342). Scale bar = 25 μm. (b) Time course of fluorescence in the tail after intravenous regional anesthesia with M-Bup-Rhd or L-Bup-Rhd. (c) Proposed actions of nanoformulations. Adapted from [13] with permission, copyright from American Chemical Society, 2019.
Nanoparticle binding can be enhanced by using specific ligands to molecules present on the surfaces of interest.[14–18] For example, a nanoscale liposomal eye drop formulation provided prolonged topical local anesthesia due to immobilization on the corneal surface by binding to glycans via succinyl-concanavalin moieties on the liposomal surface.[49] Topical local anesthesia from these targeted liposomes was much longer than that from free drugs or untargeted liposomal formulations.
2.3. Nanosized materials to trigger drug release from larger DDSs
In recent years there has been interest in drug delivery systems where the patient (or health care providers) can change the rate of drug release in response to changing patient needs.[3] One such approach uses the fact that gold nanostructures of particular dimensions will heat up when exposed to near-infrared (NIR) light of certain wavelengths, by surface plasmon resonance.[50,51] The heat produced by this process elicits drug release from a thermosensitive device.
In one example, gold nanorods were attached to the lipid bilayers of liposomes loaded with the local anesthetic tetrodotoxin and the adjuvantic compound dexmedetomidine (Figure 5a).[52] Irradiation with NIR light (808 nm, continuous wave) lead to rapid release of drug. When injected at the sciatic nerve, these particles caused an initial nerve block. Once that wore off, nerve block could be induced again for a few days by irradiating the site of injection with NIR light. The intensity and duration of local anesthesia could be adjusted by modulating the intensity and/or duration of irradiation, allowing repeatable and adjustable on-demand local anesthesia (Figure 5b). Gold nanorods have also been incorporated into chlorhexidine microspheres coated with a multilayer polyelectrolyte capsule;[53] the gold nanorods produced heat in response to NIR irradiation, which dissolved the microparticles and burst the capsule, releasing chlorhexidine.
Figure 5.
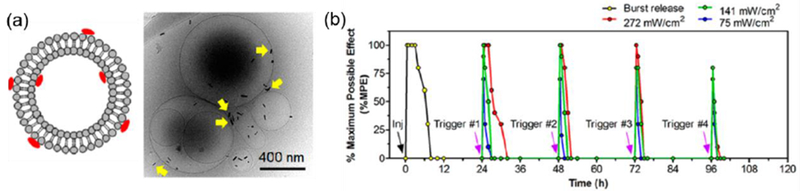
Repeated light-triggered on-demand local anesthesia with liposomes containing tetrodotoxin and dexmedetomidine and decorated with gold nanorods, (a) Scheme and cryoelectromicrograph of liposomes. Arrows indicated gold nanorods, (b) Time course of local anesthesia (y-axis) after injection of liposomes, followed by irradiation of the injection site (purple arrows) one to four days later. Adapted from [52] with permission, copyright from American Chemical Society 2016.
2.4. Strategies for enhancing local penetration and retention of nanoparticles
Many strategies have been proposed to enhance the penetration of locally-applied nanoparticles. These have included chemical penetration enhancers (CPEs),[54] microneedles,[55] and externally applied ultrasound or electric fields.[56,57]
Many classes of compounds have been proposed as CPEs, including small hydrophobic and hydrophilic compounds, surfactants, lipids and organic solvents,[54,58,59] which have usually been used to increase the penetration of small molecule drugs into skin, but have also been used in other tissues such as nerve.[23,38] They can also increase penetration of nanoparticles, depending on the latter’s properties. Pretreating skin with dimethyl sulfoxide (DMSO) enhanced the penetration of hydrophilic (citrate stabilized) gold colloid but reduced the penetration of hydrophobic (cetrimide-coated) gold nanoparticles, as a result of aggregation in the top layers of the stratum corneum.[61]
Microneedle technology is an effective minimally invasive method for delivery because it can help drugs or DDSs to directly cross the stratum corneum.[59,60–62] Polymer-based microneedle platforms have been used to deliver peptide/DNA nanoparticles loaded with DNA into tissues.[60] Dissolving microneedle arrays have been used to deliver antigen-carrier poly-D,L-lactide-co-glycolide (PGLA) nanoparticles to dendritic cell networks within the skin, [61] which increased antigen immunogenicity and significantly improved treatment of murine melanoma.
Ultrasound treatment in the presence of microbubbles can enhance the penetration of nanosized fluorescent particles into MCF-7 breast cancer spheroids,[63] with the penetration of smaller (20 nm and 40 nm) particles being increase more than that of larger (100 nm) ones. Pre-treatment of skin with ultrasound and sodium lauryl sulfate enhanced transdermal penetration by quantum dots by 500-1300%.[64] Iontophoresis has also been used to enhance the penetration of 100 nm PLGA nanoparticles loaded with indomethacin and coumarin-6 into skin.[65]
3. Systemic administration for local effect
In some diseases, direct local administration is difficult, usually because of anatomical difficulty of access, or because the precise anatomical location of the target tissue is not known. Therefore, local effect must be achieved by systemic administration so that the drugs may reach the diseased tissues through the circulation. Since systemic administration potentially exposes the entire body to drugs, it becomes important to enhance the drugs’ accumulation at the desired target location. Thus, the proportion of drug at off-target sites is decreased, and the therapeutic index is improved.[66,67] Systemic administration usually entails intravenous injection, which usually requires the DDSs to be nanoscale to avoid embolic phenomena. The circulation half-life of small molecule drugs can be prolonged after nanoencapsulation,[68] especially if the surface of the DDSs is modified with special techniques, such as PEGylation or cell membrane coating.[68–71]
Ideally, DDS administered systemically for local effect would have the following characteristics:[3] 1) they would not release drugs while traveling through the circulation, i.e. until they reach their destination; 2) they would preferentially accumulate at the lesion site and 3) they would preferentially release drugs there. However, although thousands of nanoparticle types have been reported, made from a wide range of materials (polymers, liposomes, inorganic materials, small molecular assemblies, proteins, etc.),[72–75] it is uncommon for them to fully meet those three criteria. Nevertheless, efforts persist to enhance the local accumulation of nanoparticles, or the local release of drugs, using cues inherent to the target tissues or provided by external energy sources.
3.1. Strategies for local delivery via systemic administration
3.1.1. Targeting
One approach seeks to increase the accumulation of nanoparticles in a particular tissue, often referred to as “targeting”. Targeting is often categorized as passive and active (we have argued that that nomenclature is flawed).[3]
3.1.1.1. Passive targeting
In passive targeting, the targetable characteristics of the disease sites are their pH, [76–78] the permeability of their vasculature, [79–81] the presence of enzymes,[82,83] etc. (These tissue properties also are the drivers of intrinsic [or passive] triggers, §3.1.2.1.) Targeting is achieved by particle properties such as size, shape, or material type.[84–86]
An example of passive targeting is seen in the accumulation of nanoparticles in tumors, commonly referred to as enhanced permeation and retention (EPR).[79–81] This phenomenon is ascribed to a more permeable vasculature and defective lymphatics. The improved performance of nanoformulations - such as doxorubicin liposomes and albumin paclitaxel,[87,88] - compared to free drugs is attributed to the EPR effect. For example, nanoparticles formed by co-assembly of a photosensitizer (chlorine e6) and Dox (70 nm) (Figure 6a) had improved accumulation compared to free chlorine e6 (Figure 6b) in tumors, due to EPR.[89]
Figure 6.
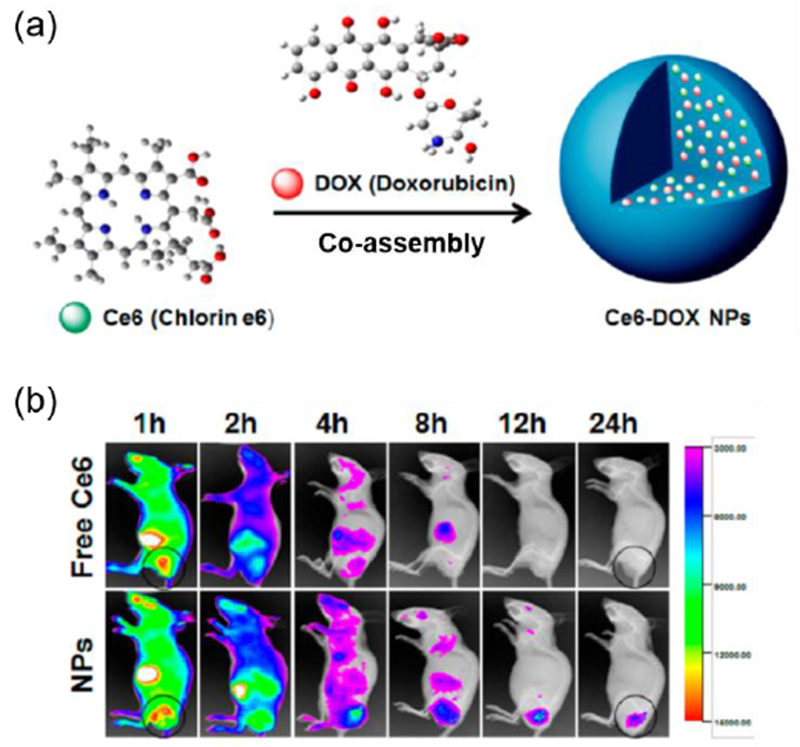
Accumulation in tumors of nanoparticles formed by assembly of a photosensitizer (chlorine e6) and doxorubicin, (a) Schematic representation of nanoparticles, (b) In vivo fluorescence images of mice after administration of free chlorine e6 solution or the nanoparticles. Nanoparticles accumulated at the tumor site because of the EPR effect. The black circled area indicates tumor tissue. Adapted from [89] with permission, copyright from American Chemical Society 2016.
A study of accumulation in tumors of gold nanoparticles with different sizes and shapes demonstrated that 55 × 60 nm nanospheres accumulated more in tumors than did 80 × 180 nm and 80 × 320 nm gold nanorods.[84] A clear demonstration of the effect of size was seen with docetaxel-containing ~100 nm nanoparticles composed of modified spiropyran, which accumulated in tumors by the EPR effect. When irradiated with 365 nm light, these nanoparticles would shrink to ~50 nm, enhancing tissue penetration and drug release.[90]
Phenomena analogous to EPR can lead to nanoparticle accumulation in other tissues and diseases, such as in myocardial ischemia,[91–93] inflammation and choroidal neovascularization.[94–96] Size and surface modification can influence the accumulation of particles in the injured heart.[91–93] For example, PEG-modified polystyrene nanoparticles with core diameters between 20 nm and 2 μm accumulated more readily in the myocardium after ischemia-reperfusion injury in mice than did larger particles.[92] This accumulation occurred only in the injured myocardium.[97]
3.1.1.2. Active targeting
In many diseases, there is overexpression of specific molecules in the diseased tissue. Modifying nanoparticle surfaces with ligands that bind those molecules can enhance nanoparticle accumulation in diseased tissues after systemic administration. This form of targeting is sometime called ‘active’.[98–100]
One example of active targeting involves targeting integrinαvβ3 with the peptide sequence Arg-Gly-Asp (RGD).[101–103] RGD peptides have been widely used to modify the surfaces of various nanoparticles for cancer targeting because of the overexpression of integrinαvβ3 on tumor cells and tumor angiogenic endothelial cells. For example, gold nanorods modified with RGD exhibited much higher tumor targeting than particles modified with the amino acid sequence RAD (which has no targeting function), so that they could deliver chemotherapeutic drugs to tumors. Similarly, RGD-modified exosomes achieved more accumulation in tumors than did non-modified ones.[104]
With growing understanding of cancer biology, more cellular and noncellular components of the tumor microenvironment have been investigated as potential targets, such as cancer-associated fibroblasts (CAFs), tumor-associated macrophages (TAMs), and the extracellular matrix (ECM).[105–108] For example, nanoparticles coated with an antibody against fibroblast activation protein-α (FAP-α a CAF marker) achieved tumor targeting, with an efficiency much higher than with a non-targeting IgG molecule.[106]
Injured areas of organs may undergo structural changes that encourage nanoparticle accumulation, and may also overexpress biomarkers which can be used for nanoparticle targeting. For example, myocardial ischemia and/or myocardial infarction may cause blood vessels to become more permeable, so that nanoparticles may accumulate in the injured area perhaps by a process analogous to EPR.[109] Moreover, the angiotensin II type 1 receptor is overexpressed in the injured area; targeting can be improved by decorating the surface of nanoparticles with a ligand to that receptor.[91]
Some proteins with cage or hollow structures can encapsulate drugs, and some of these proteins exhibit targeting effects. For example, apo-ferritin constructed from heavy (H) chain subunits can target the transferrin receptor, which is overexpressed on tumors. This targeting ability enabled doxorubicin-loaded H-ferritin (12 nm in size) to specifically deliver doxorubicin to tumors.[110] In a separate example, GroEL (a 10 nm protein) contains a hollow into which drugs can be loaded. It also has a specific affinity for a tumor-cell-specific structural protein, plectin, which allows GroEL loaded with drugs to be delivered to tumors.[111]
3.1.1.3. Intracellular targeting
Localization of drug delivery - whether by local or systemic administration - has been taken down to the subcellular level, targeting specific cell compartments (such as mitochondria, endoplasmic reticulum, Golgi apparatus and nucleus); there is now a substantial literature on this matter.[112–114] In this context, localization of drug delivery is not intended in quite the same sense as in the rest of this article, in that the localization could, in theory, occur in every cell in the body. Here we provide two examples of such.
Many diseases are related to gene overexpression and mutation.[115–117] Delivering gene therapy agents into target cells has been demonstrated as a potential strategy for modulating gene expression to suppress disease.[115–117] Naked RNA agents have difficulty reaching diseased sites via the bloodstream (due to their short circulation time and lability to degradation by RNases), and in entering cells (due to their negative charge).[115] To be taken up by cells, it is generally important for carriers to be < 200 nm in size unless they can be taken up by phagocytosis.[118,119] Many nanoscale gene delivery systems have been developed and have been reviewed elsewhere.[115–117]
Other diseases are related to mitochondrial dysfunction, such as cancer, neurodegenerative and neuromuscular diseases, obesity, and diabetes.[120–122] In cancer treatment, mitochondria can be therapeutic targets, because disrupting the cellular energy supply can kill tumor cells or reverse the drug resistance of tumor cells.[123–125] To approach the mitochondria, nanoparticles need to have the capability to escape from lysosomal/endosomal compartments, and should bear mitochondria targeting motifs (such as triphenylphosphonium compounds or specific peptides) to achieve targeted delivery.[126]
3.1.2. Triggered drug delivery
Another way to achieve local delivery of drugs from systemically administered nanoparticles is to induce the particles to release their payload more rapidly at a specified location, a process referred to as “triggering”.[127,128] Nanoparticle targeting (i.e. accumulation) can also be triggered, as we shall discuss. The triggering stimuli can be intrinsic to the local environment of the disease site (e.g. local pH) and/or external (e.g. external energy sources such as light and ultrasound).
3.1.2.1. Intrinsic triggers
Intrinsic triggering relies on special properties of the diseased environment, either extracellular or intracellular, such as the weakly acidic environment (pH6.5-7.0) of solid tumors, [76,77,129] the overexpression of multiple proteases in tumors and sites of inflammation, [82,83,130] and the acidic pH in lysosomes (pH4-5).[131–133] Intrinsic triggers are often termed “passive” stimuli. “Smart” materials can be designed that will undergo drug delivery events in response to those stimuli in particular diseased environments.
The mild acidity (pH 6.6-7.0) of the microenvironment of solid tumors, [76] has been widely used as a trigger for drug delivery events.[77,129] Designing materials that would respond rapidly to modest changes in pH has been challenging. Polymer based nanoparticles have been developed that respond to tumor pH by changing surface charge from negative to positive to enhance cell uptake, or by disassembling to release drugs.[77,129] Nanoparticles were formed at physiological pH (7.4) by self-assembly of an amphiphilic molecule composed of 3-diethylaminopropyl isothiocyanate (DEAP) (which is hydrophobic at pH 7.4) conjugated to a hydrophilic tumor-targeting peptide (hydrophilic). When the nanoparticles, loaded with doxorubicin, accumulated at the tumor site (pH6.6-7.0), the DEAP was protonated and became hydrophilic, resulting in nanoparticle disassembly and doxorubicin release.[134] In another example, dextran (Dex) was conjugated with doxorubicin (DOX) via a pH-sensitive imine bond, and the resulting prodrug (Dex-DOX) with amphiphilic properties self-assembled into nanoparticles. The Dex-DOX nanoparticles maintained integrity at neutral pH but disintegrated at the more acidic pH of the lysosome, so that the DOX could be released to kill tumor cells.[135]
Enzymes or other molecules with specific chemical properties (such as the reductive agent glutathione) are often overexpressed in diseased tissues, and are therefore used as triggers for cargo release.[136–138] Micelles encapsulating doxorubicin have been formed from a polymer composed of poly(ethylene glycol) (PEG) conjugated to poly(ε-caprolactone) (PCL) by disulfide bonds (-S-S-). Once the micelles entered the cytoplasm of tumor cells, the disulfide bonds would be cleaved by the overexpressed glutathione, allowing doxorubicin to be released.[139] Nanoassemblies have been developed from amphiphilic peptides that are cleaved by fibroblast activation protein-α (FAP-α), a protease specifically expressed on the surface of CAFs, allowing drug release.[140] This release disrupted the tumor stromal barrier and enhanced local drug accumulation. In another example, an amphiphilic peptide that could be cleaved by matrix metalloproteinase-2 (MMP-2) was inserted into the lipid membrane of liposomes.[141] The liposomes, loaded with the anti-fibrosis drug pirfenidone (PFD), would release PFD when in the MMP-2-rich environment of the pancreatic tumors site. This anti-fibrosis formulation reduced multiple components of the extracellular matrix (such as collagen I, laminin) by suppressing the activity of stromal cells and thus increasing the penetration of gemcitabine into tumor tissue.[141]
Tissue hypoxia is a salient feature of some diseases, including rheumatoid arthritis, ischemic stroke, and solid tumors.[142–144] Consequently, hypoxia has been investigated as a trigger for stimulus-responsive DDSs. In hypoxia-responsive systems, drugs are attached to nanocarriers by electron acceptor moieties, such as nitroimidazoles, nitrobenzyl alcohols and azo groups. Drug release occurs when these electron acceptor moieties are cleaved or change polarity when they accept electrons. For example, nanoparticles were formed by self-assembly of a hydrophobically modified 2-nitroimidazole derivative (electron acceptor) conjugated to the backbone of carboxymethyl dextran.[143] In hypoxic environments, the 2-nitroimidazole accepted electrons and converted to 2-aminoimidazole, decreasing the affinity between doxorubicin and the nanoparticles, which accelerated the rate of drug release.[143]
3.1.2.2. External triggers:
Nanoparticles can also be made responsive to external stimuli such as light, ultrasound, electrical and magnetic fields.[145–147] After systemic administration of the nanoparticles, application of the stimulus at a particular anatomical location leads to a localized drug delivery event.
Many external stimuli have been used a triggers, including light, microwave, ultrasound, and others, as has been described and reviewed elsewhere.[3,128,148–151] Here, we will use light as an example, since it has been has been the most commonly studied external trigger. Photo-triggering can be achieved by a variety of mechanisms including photocleavage reactions, photoisomerization, upconversion, photodynamic reactions and photothermal effects.[95,152–155] The pros and cons of light as a stimulus, and of the various wavelengths that can be used, has been reviewed elsewhere.[3,128]
Light, and other external stimuli, can trigger drug release from nanoparticles, or trigger nanoparticle targeting by eliciting the deployment of targeting ligands or other means.
3.1.2.2.1. External triggering of drug release
External stimuli can be used to trigger release of drugs from nanosystems. For example, a nanoformulation that encapsulated both siRNA and upconversion nanoparticles was created from a cationic conjugated polyelectrolyte brush (CCPEB) containing UV light-cleavable bonds. Irradiation with 980 nm light excited the upconversion nanoparticles to generate UV light, which cleaved the UV-cleavable bonds, so that the cationic side-chain of CCPEB became zwitterionic, accelerating siRNA release.[156] Triggered drug release can be also achieved with other stimuli, such as ultrasound and magnetic fields.[3,148–151]
3.1.2.2.2. External triggering of nanoparticle targeting
An early example of photo-triggered targeting was seen in 300 nm polystyrene particles whose surfaces were decorated with a peptide ligand with the amino acid sequence YIGSR, which binds to β1-integrin, which is found throughout the body. Binding of nanoparticles to cells was inhibited by covalently binding a nitrobenzyl group to the YIGSR.[152] Upon irradiation of the particles with ultraviolet light, the nitrobenzyl moieties were cleaved, allowing the YIGSR to become active, and permitting nanoparticle binding to cells. An interesting benefit of this approach is that it allows anatomically precise targeting in the absence of a ligand specific to the target tissue. A potential challenge is that one may need to know where the target is.
This approach has been used to target tumors and as well as non-cancerous conditions.[153,95] As an example of the latter, nanoparticles were developed to target lesions of choroidal neovascularization (CNV) in the posterior segment of the eye – an anatomical location difficult to reach except by intravitreal injection (Figure 7a).[95] The nanoparticles were decorated with cell-penetrating peptides (CPPs) which were inactivated (“caged”) by covalent modification with a coumarin-like molecule. Irradiation of the retina through the pupil led to cleavage of the coumarin-like molecule (Figure 7b), which allowed nanoparticle binding within the CNV lesions in the choroid (Figure 7c). The resulting delivery of doxorubicin was therapeutically effective (Figure 7d). Note that the success of approaches of this kind may depend on the concurrent presence of a second mechanism for nanoparticle accumulation, such as EPR.
Figure 7.
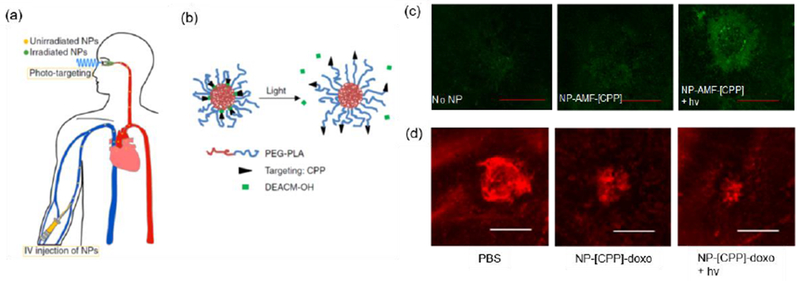
Treatment of choroidal neovascularization (CNV) by photo-triggered targeting of systemically-administered nanoparticles. (a) Scheme of administration and light-triggered targeting. (b) Scheme of light-triggering of nanoparticle targeting. Irradiation removes the caging groups from the targeting motifs, which also allows them to come to the surface of the nanoparticles. (c) Targeting efficiency evaluation by confocal laser scanning microscoscopy. Accumulation of nanoparticles labeled with the fluorescent dye AMF (NP-AMF) in CNV lesions. NP-AMF-[CPP]: nanoparticles with caged cell penetrating peptide (CPP). NP-AMF-[CPP] + hv: such nanoparticles with photo-triggering. The scale bar = 100 μm. (d) Representative isolectin GS IB4-stained (red, indicating the vasculature) images of CNV lesions after treatment with doxorubicin (doxo)-containing formulations. NP-[CPP]-doxo: nanoparticles with caged CPP containing doxorubicin. Scale bar = 100 μm. Adapted from [95] with permission, copyright from Nature Publishing Group, 2019.
Note that it is possible for external stimuli to trigger both drug release and targeting. For example, irradiation of the spiropyran-docetaxel nanoparticles described in §3.1.1.1 caused both particle shrinkage – which increased accumulation in tumors – and drug release.[90]
3.2. Enhanced permeability of regional blood vessels and tissues
EPR can increase the accumulation of particles although the degree to which this occurs is variable (and debated) and can be variable within individual tumors and between tumor types.[157–160] The longer a drug delivery system stays in the circulation, the more likely it is to extravasate into the tumor through the EPR effect, but it can also extravasate into normal tissues albeit at a slower rate. Many investigators have therefore developed means of increasing blood flow and/or vascular permeability within target tissues, to enhance particle delivery and accumulation. For example, polymer-lipid-peptide nanoparticles have been used to deliver an antiplatelet antibody to tumors, where platelet depletion by the antibody would enhance the permeability of tumor blood vessels.[161] In another approach, mesoporous silica nanoparticles (112 × 205 nm) containing gemcitabine and coated with gold nanoshells were used to treat pancreatic tumors in mice. NIR laser irradiation induced tumor site-specific heating of the gold nanoshells by the photothermal effect. The heating enhanced local tumor blood flow and vascular permeability, which increased accumulation of nanocarriers, resulting in improved therapeutic efficacy.[162] Ultrasound-induced microbubble cavitation can cause enhanced permeability across biological barriers within tumors such as vessel walls, extracellular matrix (ECM) or cellular membranes,[163–166] allowing for enhanced penetration of nanoparticles into target tissues. For example, performing ultrasound at the tumor site after systemically administering PLGA-PEG nanoparticles loaded with microRNA together with microbubbles increased the depth of penetration of the nanoparticles 1.3- to 3-fold, which led to a 7.9-fold higher delivery of the microRNA.[164] In a separate report, high-intensity focused ultrasound loosened the structure of ECM in tumor tissues,[165,166] resulting in enhanced penetration and accumulation into tumors of extravasated paclitaxel-loaded thiolated human serum albumin nanoparticles conjugated onto microbubbles.[166] Ultrasound also caused the disruption of the microbubbles, leading to release of the nanoparticles.[166]
4. Perspectives and challenges of nanoscale DDSs for local delivery
As we have seen, local delivery using nanoparticles occurs by basically two broad methods: direct placement (e.g. injection at the intended site of use), or a targeted/triggered approach after systemic administration. There are many ways in which these can and are being improved.
Local delivery of DSS could be enhanced by advances in imaging (to precisely identify targets),[158,167–170] endoscopy (to identify and reach them),[171,172] and other technologies. For example, it is now the standard of care for injection of local anesthetics near nerves for peripheral nerve blockade to be performed under ultrasound guidance, to improve targeting and to avoid injuring tissues with the needle.[173,174] Theranostic nanoparticles, or nanoparticles for imaging, could also be helpful.[175–179] Systemic administration could delineate targets for either surgical resection,[180–184] radiation therapy,[185] or targeting with nanotherapies such as those described above. A special case of such approaches is nanoparticles that are injected locally or systemically so that they are taken up in a particular type of tissue (e.g. lymphatics, tumor).[179] During subsequent surgery, the location of the particles – and therefore of the specific tissue to be resected can be detected by irradiation of the surgical field.[186]
Improving methods of increasing nanoparticle accumulation at specific sites is the subject of a large body of literature. It has correctly been pointed out that the percentage of an injected dose of nanoparticles that actually reaches tumors (for example) is very small.[158] That is perhaps not surprising given that the target tissues are themselves very small, in comparison the potential volume of distribution of a systemically delivered material. Moreover, it could be argued that what really matters is not the absolute amount of nanoparticle reaching a diseased site but the fractional change in that amount due to targeting, which could in theory increase the therapeutic index. Strategies to improve targeting will therefore be important. One approach would be to increase the tissue depth at which targeting and triggering by external energy sources can be effective,[187,188] which may involve making drug delivery systems more sensitive to the stimuli, improving photosensitizers, making upconversion more effective, etc. With upconversion, the goal is to allow the nanoparticles in the target tissue to be reached by NIR light (which has greater tissue penetration than light of shorter wavelengths),[189] where it is converted in situ to light of shorter wavelength and higher energy. That upconverted light then has sufficient energy to cleave covalent bonds, etc., enabling drug delivery events. Targeting can also be improved by the discovery of more specific targeting receptors, and perhaps by combinations of targeting modalities.
Developing methods to enhance drug loading could also be beneficial, since achieving drug loading is often problematic with nanoscale DDSs, and since the mass of nanoparticle that reaches target sites is usually small. The use of synergistic drug combinations can serve a similar purpose,[190,191] allowing a smaller mass of delivered drug to have a greater effect.
Highlights:
Advantages and disadvantages of nanoscale drug delivery systems for local drug delivery.
Strategies for local nanoscale drug delivery by local and systemic administration.
Targeting and triggering of nanoscale drug delivery systems
Acknowledgements
Support for this work was provided by NIH R35 GM131728 (D.S.K.) and The Anesthesia Research Distinguished Trailblazer Award (to T.J.).
Biographies
Tianjiao Ji received his Ph.D. (2016) from the National Center for Nanoscience and Technology (NCNST) under the supervision of Prof. Guangjun Nie. He is currently a postdoctoral associate under the supervision of Prof. Daniel Kohane (Boston Children’s Hospital, Harvard Medical School). His research interests focus on the construction of functional peptide self-assemblies for drug delivery.
Daniel S. Kohane obtained his M.D. and a Ph.D. in Physiology from Boston University. He is a pediatrician, anesthesiologist, and pediatric intensive care physician. His laboratory at Boston Children’s Hospital at Harvard Medical School focuses on biomaterials, drug delivery, and nanoscience.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References:
- 1.Savjani KT, Gajjar AK, Savjani JK, ISRN Pharm. 2012 (2012) 195727. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Wen H, Jung H, Li X, AAPS J. 17 (2015) 1327–1340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Wang Y, Kohane DS, Nat. Rev. Mater 2 (2017) 17020. [Google Scholar]
- 4.Chen Q, Wang C, Zhang X, Chen G, Hu Q, Li H, Wang J, Wen D, Zhang Y, Lu Y, Yang G, Jiang C, Wang J, Dotti G, Gu Z, Nat. Nanotechnol 14 (2019) 89–97. [DOI] [PubMed] [Google Scholar]
- 5.Singh R, Lillard JW, Exp. Mol. Pathol 86 (2009) 215–223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ferrari M, Nat. Rev. Cancer 5 (2005) 161–171. [DOI] [PubMed] [Google Scholar]
- 7.Ogawara K, Yoshizawa Y, Un K, Araki T, Kimura T, Higaki K, Biol. Pharm. Bull 36 (2013) 698–702. [DOI] [PubMed] [Google Scholar]
- 8.Shipunova VO, Nikitin MP, Nikitin PI, Deyev SM, Nanoscale 8 (2016) 12764–12772. [DOI] [PubMed] [Google Scholar]
- 9.Rathor S, Bhatt DC, Aamir S, Singh SK, Kumar V, Pharm. Nanotechnol 5 (2017) 263–275. [DOI] [PubMed] [Google Scholar]
- 10.Buzea C, Pacheco II, Robbie K, Biointerphases 2 (2007) MR17–MR71. [DOI] [PubMed] [Google Scholar]
- 11.Rancan F, Gao Q, Graf C, Troppens S, Hadam S, Hackbarth S, Kembuan C, Blume-Peytavi U, Rühl E, Lademann J, Vogt A, ACS Nano 6 (2012) 6829–6842. [DOI] [PubMed] [Google Scholar]
- 12.Huang K, Ma H, Liu J, Huo S, Kumar A, Wei T, Zhang X, Jin S, Gan Y, Wang PC, He S, Zhang X, Liang XJ, ACS Nano 6 (2012) 4483–4493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Weldon C, Ji T, Nguyen MT, Rwei A, Wang W, Hao Y, Zhao C, Mehta M, Wang BY, Tsui J, Marini RP, Kohane DS, ACS Nano 13 (2019) 18–25. [DOI] [PubMed] [Google Scholar]
- 14.Verma A, Stellacci F, Small 6 (2010) 12–21. [DOI] [PubMed] [Google Scholar]
- 15.Black KC, Yi J, Rivera JG, Zelasko-Leon DC, Messersmith PB, Nanomedicine 8 (2013) 17–28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ruoslahti E, Adv. Mater 24 (2012) 3747–3756. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Boeneman K, Delehanty JB, Blanco-Canosa JB, Susumu K, Stewart MH, Oh E, Huston AL, Dawson G, Ingale S, Walters R, Domowicz M, Deschamps JR, Algar WR, Dimaggio S, Manono J, Spillmann CM, Thompson D, Jennings TL, Dawson PE, Medintz IL, ACS Nano 7 (2013) 3778–3796. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Guan X, Li C, Wang D, Sun W, Ga X, RSC Adv. 6 (2016) 9461–9464. [Google Scholar]
- 19.Kohane DS, Biotechnol. Bioeng 96 (2007) 203–209. [DOI] [PubMed] [Google Scholar]
- 20.Ilinskaya AN, Dobrovolskaia MA, Nanomedicine 8 (2013) 969–981. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Matsumoto Y, Nichols JW, Toh K, Nomoto T, Cabral H, Miura Y, Christie RJ, Yamada N, Ogura T, Kano MR, Matsumura Y, Nishiyama N, Yamasoba T, Bae YH, Kataoka K, Nat. Nanotechnol 11 (2016) 533–538. [DOI] [PubMed] [Google Scholar]
- 22.Hoshyar N, Gray S, Han H, Bao G, Nanomedicine 11 (2016) 673–692. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Yang R, Wei T, Goldberg H, Wang W, Cullion K, Kohane DS, Adv. Mater 29 (2017) 1606596. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Raju G, Katiyar N, Vadukumpully S, Shankarappa SA, J. Dermatol. Sci 89 (2018) 146–154. [DOI] [PubMed] [Google Scholar]
- 25.Labouta HI, el-Khordagui LK, Kraus T, Schneider M, Nanoscale 3 (2011) 4989–4999. [DOI] [PubMed] [Google Scholar]
- 26.Tang BC, Dawson M, Lai SK, Wang YY, Suk JS, Yang M, Zeitlin P, Boyle MP, Fu J, J. Hanes, Proc. Natl. Acad. Sci. USA 106 (2009) 19268–19273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Lai SK, Suk JS, Pace A, Wang YY, Yang M, Mert O, Chen J, Kim J, Hanes J, Biomaterials 32 (2011) 6285–6290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Lockman PR, Koziara JM, Mumper RJ, Allen DD, J. Drug Target 12 (2004) 635–641. [DOI] [PubMed] [Google Scholar]
- 29.Lockman PR, Mumper RJ, Khan MA, Allen DD, Drug Dev. Ind. Pharm 28 (2002) 1–13. [DOI] [PubMed] [Google Scholar]
- 30.Tsou YH, Zhang XQ, Zhu H, Syed S, Xu X, Small 13 (2017) 1701921. [DOI] [PubMed] [Google Scholar]
- 31.Wick P, Malek A, Manser P, Meili D, Maeder-Althaus X, Diener L, Diener PA, Zisch A, Krug HF, von Mandach U, Environ. Health Perspect. 118 (2010) 432–436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Chu M, Wu Q, Yang H, Yuan R, Hou S, Yang Y, Zou Y, Xu S, Xu K, Ji A, Sheng L, Small 6 (2010) 670–678. [DOI] [PubMed] [Google Scholar]
- 33.Taylor U, Tiedemann D, Rehbock C, Kues WA, Barcikowski S, Rath D, Beilstein J Nanotechnol. 6 (2015) 651–664. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Sonavane G, Tomoda K, Sano A, Ohshima H, Terada H, Makino K, Colloids Surf. B Biointerfaces 65 (2008) 1–10. [DOI] [PubMed] [Google Scholar]
- 35.Fernandes R, Smyth NR, Muskens OL, Nitti S, Heuer-Jungemann A, Ardern-Jones MR, Kanaras AG, Small 11 (2015) 713–721. [DOI] [PubMed] [Google Scholar]
- 36.Chen Y, Wu Y, Gao J, Zhang Z, Wang L, Chen X, Mi J, Yao Y, Guan D, Chen B, Dai J, ACS Appl. Mater. Interfaces 9 (2017) 5173–5180. [DOI] [PubMed] [Google Scholar]
- 37.Kohane DS, Yieh J, Lu NT, Langer R, Strichartz GR, Berde CB, Anesthesiology 89 (1998) 119–131. [DOI] [PubMed] [Google Scholar]
- 38.Simons EJ, Bellas E, Lawlor MW, Kohane DS, Mol. Pharm 6 (2009) 265–273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Liu Q, Santamaria CM, Wei T, Zhao C, Ji T, Yang T, Shomorony A, Wang BY, Kohane DS, Nano Lett. 18 (2018) 32–37. [DOI] [PubMed] [Google Scholar]
- 40.Lai SK, Wang YY, Hanes J, Adv. Drug Deliv. Rev 61 (2009) 158–171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Fang L, Wang L, Yao Y, Zhang J, Wu X, Li X, Wang H, Zhang X, Gong X, Chang J, Nanomedicine 13 (2017) 153–171. [DOI] [PubMed] [Google Scholar]
- 42.Date AA, Halpert G, Babu T, Ortiz J, Kanvinde P, Dimitrion P, Narayan J, Zierden H, Betageri K, Musmanno O, Wiegand H, Huang X, Gumber S, Hanes J, Ensign LM, Biomaterials 185 (2018) 97–105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Yu M, Wang J, Yang Y, Zhu C, Su Q, Guo S, Sun J, Gan Y, Shi X, Gao H, Nano Lett. 16 (2016) 7176–7182. [DOI] [PubMed] [Google Scholar]
- 44.Varde NK, Pack DW, Expert Opin. Biol. Ther 4 (2004) 35–51. [DOI] [PubMed] [Google Scholar]
- 45.Schlapp M, Friess W, J. Pharm. Sci 92 (2003) 2145–2151. [DOI] [PubMed] [Google Scholar]
- 46.Brown EM, McGriff JT, Malinowski RW, Can. J. Anaesth 36 (1989) 307–310. [DOI] [PubMed] [Google Scholar]
- 47.van Zundert A, Helmstadter A, Goerig M, Mortier E, Reg. Anesth. Pain Med 33 (2008) 483–489. [DOI] [PubMed] [Google Scholar]
- 48.Gupta B, Verma RK, Kumar S, Chaudhary G, Anesth. Essays Res 11 (2017) 62–66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Zhan C, Santamaria CM, Wang W, McAlvin JB, Kohane DS, Biomaterials 181 (2018) 372–377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Roszek B, Jong W.H.d., Geertsma RE, Nanotechnology in medical applications: state-of-the-art in materials and devices, Department of Pharmaceutical Affairs and Medical Technology of the Dutch Ministry of Health, Welfare and Sports, 2005. [Google Scholar]
- 51.Simovic S, Losic D and Vasilev K, Chem. Commun 46 (2010) 1317–1319. [DOI] [PubMed] [Google Scholar]
- 52.Feschet-Chassot E, Raspal V, Sibaud Y, Awitor OK, Bonnemoy F, Bonnet JL and Bohatier J, Thin Solid Films, 519 (2011) 2564–2568. [Google Scholar]
- 53.Bimbo LM, M”akil”a E, Laaksonen T, Lehto VP,Salonen J, Hirvonen J, Santos HA, Biomaterials 32 (2011. 2625–2633. [DOI] [PubMed] [Google Scholar]
- 54.Lee S, Hwang G, Kim TH, Kwon SJ, Kim JU, Koh K, Park B, Hong H, Yu KJ, Chae H, Jung Y, Lee J, Kim TI, ACS Nano. 12 (2018) 6756–6766. [DOI] [PubMed] [Google Scholar]
- 55.Sanchez-Gaytan BL, Qian Z, Hastings SP, Reca ML, Fakhraai Z, Park SJ, J. Phys. Chem. C 117 (2013) 8916–8923. [Google Scholar]
- 56.Huang X, Neretina S, El-Sayed MA, Adv. Mater 21 (2009) 4880–4910. [DOI] [PubMed] [Google Scholar]
- 57.Zhan C, Wang W, Santamaria C, Wang B, Rwei A, Timko BP, Kohane DS, Nano Lett. 17 (2017) 660–665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Luo D, Hasan MS, Shahid S, Khlebtsov BN, Cattell MJ, Sukhorukov GB, Langmuir 33 (2017) 7982–7993. [DOI] [PubMed] [Google Scholar]
- 59.Marepally S, Boakye CH, Shah PP, Etukala JR, Vemuri A, Singh M, PLoS One. 8 (2013) e82581. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Pierre MB, Rossetti FC, Curr. Drug Targets 15 (2014) 281–291. [DOI] [PubMed] [Google Scholar]
- 61.Polat BE, Hart D, Langer R, Blankschtein D, J. Control Release 152 (2011) 330–348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Rodzinski A, Guduru R, Liang P, Hadjikhani A, Stewart T, Stimphil E, Runowicz C, Cote R, Altman N, Datar R, Khizroev S, Sci. Rep 6 (2016) 20867. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Labouta HI, El-Khordagui LK, Schneider M, Skin Pharmacol. Physiol 25 (2012) 208–218. [DOI] [PubMed] [Google Scholar]
- 64.Pham QD, Bjorklund S, Engblom J, Topgaard D, Sparr E, J. Control Release 232 (2016) 175–187. [DOI] [PubMed] [Google Scholar]
- 65.Cole G, McCaffrey J, Ali AA, McBride JW, McCrudden CM, Vincente-Perez EM, Donnelly RF, McCarthy HO, Hum. Vaccin. Immunother 13 (2017) 50–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Zaric M, Lyubomska O, Poux C, Hanna ML, McCrudden MT, Malissen B, Ingram RJ, Power UF, Scott CJ, Donnelly RF, Kissenpfennig A, J. Invest. Dermatol 135 (2015) 425–434. [DOI] [PubMed] [Google Scholar]
- 67.Wang C, Ye Y, Hochu GM, Sadeghifar H, Gu Z, Nano Lett. 16 (2016) 2334–2340. [DOI] [PubMed] [Google Scholar]
- 68.Suk JS, Xu Q, Kim N, Hanes J, Ensign LM, Adv. Drug Deliv. Rev 99 (2016) 28–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Perry JL, Reuter KG, Kai MP, Herlihy KP, Jones SW, Luft JC, Napier M, Bear JE, DeSimone JM, Nano Lett. 12 (2012) 5304–5310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Hu CM, Zhang L, Aryal S, Cheung C, Fang RH, Zhang L, Proc. Natl. Acad. Sci. U S A 108 (2011) 10980–10985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Fang RH, Hu CM, Zhang L, Expert Opin. Biol. Ther 12 (2012) 385–389. [DOI] [PubMed] [Google Scholar]
- 72.Ulbrich K, Hola K, Subr V, Bakandritsos A, Tucek J, Zboril R, Chem. Rev 116 (2016) 5338–5431. [DOI] [PubMed] [Google Scholar]
- 73.Allen TM, Cullis PR, Adv. Drug Deliv. Rev 65 (2013) 36–48. [DOI] [PubMed] [Google Scholar]
- 74.Li Z, Barnes JC, Bosoy A, Stoddart JF, Zink JI, Chem. Soc. Rev 41 (2012) 2590–2605. [DOI] [PubMed] [Google Scholar]
- 75.Qin H, Ding Y, Mujeeb A, Zhao Y, Nie G, Mol. Pharm 92 (2017) 219–231. [DOI] [PubMed] [Google Scholar]
- 76.Shen S, Li HJ, Chen KG, Wang YC, Yang XZ, Lian ZX, Du JZ, Wang J, Nano Lett. 17 (2017) 3822–3829. [DOI] [PubMed] [Google Scholar]
- 77.Yang XZ, Du XJ, Liu Y, Zhu YH, Liu YZ, Li YP, Wang J, Adv. Mater 26 (2014) 931–936. [DOI] [PubMed] [Google Scholar]
- 78.Kanamala M, Wilson WR, Yang M, Palmer BD, Wu Z, Biomaterials 85 (2016) 152–167. [DOI] [PubMed] [Google Scholar]
- 79.Torchilin V, Adv. Drug Deliv. Rev 63 (2011) 131–135. [DOI] [PubMed] [Google Scholar]
- 80.Maeda H, Wu J, Sawa T, Matsumura Y, Hori K, J. Control. Release 65 (2000) 271–284. [DOI] [PubMed] [Google Scholar]
- 81.Fang J, Nakamura H, Maeda H, Adv. Drug Deliv. Rev 63 (2011) 136–151. [DOI] [PubMed] [Google Scholar]
- 82.de Groot FM, Damen EW, Scheeren HW, Curr. Med. Chem 8 (2001) 1093–1122. [DOI] [PubMed] [Google Scholar]
- 83.Cheng YJ, Luo GF, Zhu JY, Xu XD, Zeng X, Cheng DB, Li YM, Wu Y, Zhang XZ, Zhuo RX, He F, ACS Appl. Mater. Interfaces 7 (2015) 9078–9087. [DOI] [PubMed] [Google Scholar]
- 84.Perry JL, Reuter KG, Luft JC, Pecot CV, Zamboni W, DeSimone JM, Nano Lett. 17 (2017) 2879–2886. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Albanese A, Tang PS, Chan WCW, Annu. Rev. Biomed. Eng 14 (2012) 1–16. [DOI] [PubMed] [Google Scholar]
- 86.Devarajan PV, Jindal AB, Patil RR, Mulla F, Gaikwad RV, Samad A, J. Pharm. Sci 99 (2010) 2576–2581. [DOI] [PubMed] [Google Scholar]
- 87.Barenholz Y, J. Control Release 160 (2012) 117–134. [DOI] [PubMed] [Google Scholar]
- 88.Desai N, Trieu V, Yao Z, Louie L, Ci S, Yang A, Tao C, De T, Beals B, Dykes D, Noker P, Yao R, Labao E, Hawkins M, Soon-Shiong P, Clin. Cancer Res 12 (2006) 1317–1324. [DOI] [PubMed] [Google Scholar]
- 89.Zhang R, R. Xing R, Jiao T, Ma K, Chen C, Ma G, Yan X, ACS Appl. Mater. Interfaces 8 (2016) 13262–13269. [DOI] [PubMed] [Google Scholar]
- 90.Tong R, Chiang HH, Kohane DS, Proc. Natl. Acad. Sci. USA 110 (2013) 19048–19053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Dvir T, Bauer M, Schroeder A, Tsui JH, Anderson DG, Langer R, Liao R, Kohane DS, Nano Lett. 11 (2011) 4411–4414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Lundy DJ, Chen KH, Toh EK, Hsieh PC, Sci. Rep 6 (2016) 25613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Geelen T, Paulis LE, Coolen BF, Nicolay K, Strijkers GJ, Contrast Media Mol. Imaging 8 (2013) 117–126. [DOI] [PubMed] [Google Scholar]
- 94.Maeda H, Cancer Sci. 104 (2013) 779–789. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Wang Y, Liu C, Ji T, Mehta M, Wang W, Marino E, Chen J, Kohane DS, Nat. Commun 10 (2019) 804. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Ideta R, Yanagi Y, Tamaki Y, Tasaka F, Harada A, Kataoka K, FEBS Lett. 557 (2004) 21–25. [DOI] [PubMed] [Google Scholar]
- 97.Weis SM, Curr. Opin. Hematol 15 (2008) 243–249. [DOI] [PubMed] [Google Scholar]
- 98.Bertrand N, Wu J, Xu X, Kamaly N, Farokhzad OC, Adv. Drug Deliv. Rev 66 (2014) 2–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Lammers T, Kiessling F, Hennink WE, Storm G, J. Control Release 161 (2012) 175–187. [DOI] [PubMed] [Google Scholar]
- 100.Danhier F, Feron O, Preat V, J. Control. Release 148 (2010) 135–146. [DOI] [PubMed] [Google Scholar]
- 101.Zhang L, Su H, Cai J, Cheng D, Ma Y, Zhang J, Zhou C, Liu S, Shi H, Zhang Y, Zhang C, ACS Nano 10 (2016) 10404–10417. [DOI] [PubMed] [Google Scholar]
- 102.Xu XD, Cheng YJ, Wu J, Cheng H, Cheng SX, Zhuo RX, Zhang XZ, Biomaterials 76 (2016) 238–249. [DOI] [PubMed] [Google Scholar]
- 103.Gao J, Xie C, Zhang M, Wei X, Yan Z, Ren Y, Ying M, Lu W, Nanoscale 8 (2016) 7209–7216. [DOI] [PubMed] [Google Scholar]
- 104.Tian Y, Li S, Song J, Ji T, Zhu M, Anderson GJ, Wei J, Nie G, Biomaterials 35 (2014) 2383–2390. [DOI] [PubMed] [Google Scholar]
- 105.Bhowmick NA, Neilson EG, Moses HL, Nature 432 (2004) 332–337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Ji T, Ding Y, Zhao Y, Wang J, Qin H, Liu X, Lang J, Zhao R, Zhang Y, Shi J, Tao N, Qin Z, Nie G, Adv. Mater 27 (2015) 1865–1873. [DOI] [PubMed] [Google Scholar]
- 107.Alsaab HO, Sau S, Alzhrani RM, Cheriyan VT, Polin LA, Vaishampayan U, Rishi AK, Iyer AK, Biomaterials 183 (2018) 280–294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Kanapathipillai M, Mammoto A, Mammoto T, Kang JH, Jiang E, Ghosh K, Korin N, Gibbs A, Mannix R, Ingber DE, Nano Lett. 12 (2012) 3213–3217. [DOI] [PubMed] [Google Scholar]
- 109.Molavi B, Chen J, Mehta JL, Am. J. Physiol. Heart Circ. Physiol 291 (2006) H687–693. [DOI] [PubMed] [Google Scholar]
- 110.Liang M, Fan K, Zhou M, Duan D, Zheng J, Yang D, Feng J, Yan X, Proc. Natl..Acad. Sci. U S A 111 (2014) 14900–14905. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Yuan Y, Du C, Sun C, Zhu J, Wu S, Zhang Y, Ji T, Lei J, Yang Y, Gao N, Nie G, Nano Lett. 18 (2018) 921–928. [DOI] [PubMed] [Google Scholar]
- 112.Huang JG, Leshuk T, Gu FX, Nano Today 6 (2011) 478–492. [Google Scholar]
- 113.Shi M, Ho K, Keating A, Shoichet MS, Adv. Funct. Mater 19 (2009) 1689–1696. [Google Scholar]
- 114.Yameen B, Choi W, Vilos C, Swami A, Shi J, Farokhzad OC, J. Control Release 190 (2014) 485–499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Kaczmarek JC, Kowalski PS, Anderson DG, Genome Med. 9 (2017) 60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Guzman-Aranguez A, Loma P, Pintor J, Br. J. Pharmacol 170 (2013) 730–747. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Adijanto J, Naash MI, Eur. J. Pharm. Biopharm 95 (2015) 353–367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.dos Santos T, Varela J, Lynch I, Salvati A, Dawson KA, Small 7 (2011) 3341–3349. [DOI] [PubMed] [Google Scholar]
- 119.Zhu M, Nie G, Meng H, Xia T, Nel A, Zhao Y, Acc. Chem. Res 46 (2013) 622–631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Duchen MR, Mol. Aspects Med 25 (2004) 365–451. [DOI] [PubMed] [Google Scholar]
- 121.Cadonic C, Sabbir MG, Albensi BC, Mol. Neurobiol 53 (2016) 6078–6090. [DOI] [PubMed] [Google Scholar]
- 122.Rosca MG, Hoppel CL, Heart Failure Rev. 18 (2013) 607–622. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Fulda S, Galluzzi L, Kroemer G, Nat. Rev. Drug Discov 9 (2010) 447–464. [DOI] [PubMed] [Google Scholar]
- 124.Errico A, Nat. Rev. Clin. Oncol 11 (2014) 562. [DOI] [PubMed] [Google Scholar]
- 125.Lu P, Bruno BJ, Rabenau M, Lim CS, J. Controlled Release 240 (2016) 38–51. [DOI] [PubMed] [Google Scholar]
- 126.Zielonka J, Joseph J, Sikora A, Hardy M, Ouari O, Vasquez-Vivar J, Cheng G, Lopez M, Kalyanaraman B, Chem Rev. 117 (2017) 10043–10120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Kim CS, Duncan B, Creran B, Rotello VM, Nano Today 8 (2013) 439–447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Rwei AY, Wang W, Kohane DS, Nano Today 10 (2015) 451–467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Ji T, Zhao Y, Ding Y, Nie G, Adv. Mater 25 (2013) 3508–3525. [DOI] [PubMed] [Google Scholar]
- 130.Lanone S, Zheng T, Zhu Z, Liu W, Lee CG, Ma B, Chen Q, Homer RJ, Wang J, Rabach LA, Rabach ME, Shipley JM, Shapiro SD, Senior RM, Elias JA, J. Clin. Invest 110 (2002) 463–474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Hanahan D, Weinberg RA, Cell 144 (2011) 646–674. [DOI] [PubMed] [Google Scholar]
- 132.Newby AC, Physiol. Rev 85 (2005) 1–31. [DOI] [PubMed] [Google Scholar]
- 133.Mindell JA, Annu. Rev. Physiol 74 (2012) 69–86. [DOI] [PubMed] [Google Scholar]
- 134.Ding Y, Ji T, Zhao Y, Zhang Y, Zhao X, Zhao R, Lang J, Zhao X, Shi J, Sukumar S, Nie G, Mol. Cancer Ther 14 (2015) 2390–2400. [DOI] [PubMed] [Google Scholar]
- 135.Feng X, Li D, Han J, Zhuang X, Ding J, Mater. Sci. Eng. C Mater. Biol. Appl 76 (2017) 1121–1128. [DOI] [PubMed] [Google Scholar]
- 136.Zhang F, Ni Q, Jacobson O, Cheng S, Liao A, Wang Z, He Z, Yu G, Song J, Ma Y, Niu G, Zhang L, Zhu G, Chen X, Angew. Chem. Int. Ed 57 (2018) 7066–7070. [DOI] [PubMed] [Google Scholar]
- 137.Zhang M, Xu C, Wen L, Han MK, Xiao B, Zhou J, Zhang Y, Zhang Z, Viennois D, Merlin D, Cancer Res. 76 (2016) 7208–7218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Zhang C, Pan D, Li J, Hu J, Bains A, Guys N, Zhu H, Li X, Luo K, Gong Q, Gu Z, Acta Biomater. 55 (2017) 153–162. [DOI] [PubMed] [Google Scholar]
- 139.Zhu Y, Zhang J, Meng F, Deng C, Cheng R, Feijen J, Zhong Z, J. Control Release 233 (2016) 29–38. [DOI] [PubMed] [Google Scholar]
- 140.Ji T, Zhao Y, Ding Y, Wang J, Zhao R, Lang J, Qin H, Liu X, Shi J, Tao N, Qin Z, Nie G, Zhao YL, Angew. Chem. Int. Ed 55 (2016) 1050–1055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Ji T, Lang J, Wang J, Cai R, Zhang Y, Qi F, Zhang L, Zhao X, Wu W, Hao J, Qin Z, Zhao Y, Nie G, ACS Nano 11 (2017) 8668–8678. [DOI] [PubMed] [Google Scholar]
- 142.Qian C, Yu J, Chen Y, Hu Q, Xiao X, Sun W, Wang C, Feng P, Shen QD, Gu Z, Adv. Mater 28 (2016) 3313–3320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Thambi T, Deepagan VG, Yoon HY, Han HS, Kim SH, Son S, Jo DG, Ahn CH, Suh YD, Kim K, Kwon IC, Lee DS, Park JH, Biomaterials 35 (2014) 1735–1743.. [DOI] [PubMed] [Google Scholar]
- 144.Thambi T, Park JH, Lee DS, Chem. Commun 52 (2016) 8492–8500. [DOI] [PubMed] [Google Scholar]
- 145.Chen Q, Hu Q, Dukhovlinova E, Chen G, Ahn S, Wang C, Ogunnaike EA, Ligler FS, Dotti G, Gu Z, Adv. Mater. 31 (2019) e1900192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Goodman AM, Hogan NJ, Gottheim S, Li C, Clare SE, Halas NJ, ACS Nano 11 (2017) 171–179. [DOI] [PubMed] [Google Scholar]
- 147.Chertok B, David AE, Yang VC, Biomaterials 31 (2010) 6317–6324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.Qiao Y, Wan J, Zhou L, Ma W, Yang Y, Luo W, Yu Z, Wang H, Wiley Interdiscip. Rev. Nanomed. Nanobiotechnol. 11 (2019) e1527. [DOI] [PubMed] [Google Scholar]
- 149.Morey M, Pandit A, Adv. Drug Deliv. Rev 129 (2018) 169–193. [DOI] [PubMed] [Google Scholar]
- 150.Kang H, Hua S, Cho MH, Hong SH, Choi Y, Choi HS, Nano Today 23 (2018) 59–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151.Kim CS, Duncan B, Creran B, Rotello VM, Nano Today. 8 (2013) 439–447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.Dvir T, Banghart MR, Timko BP, Langer R, Kohane DS, Nano Lett. 10 (2010) 250–254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153.Wang W, Liu Q, Zhan C, Barhoumi A, Yang T, Wylie RG, Armstrong PA, Kohane DS, Nano Lett. 15 (2015) 6332–6338. [DOI] [PubMed] [Google Scholar]
- 154.Liu Q, Wang W, Zhan C, Yang T, Kohane DS, Nano Lett. 16 (2016) 4516–4520. [DOI] [PubMed] [Google Scholar]
- 155.Wang Y, Barhoumi A, Tong R, Wang W, Ji T, Deng X, Li L, Lyon SA, Reznor G, Zurakowski D, Kohane DS, Acta Biomater. 72 (2018) 287–294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156.Zhao H, Hu WB, Ma HH, Jiang RC, Tang YF, Ji Y, Lu XM, Hou B, Deng WX, Huang W, Fan QL, Adv. Funct. Mater 27 (2017) 1702592. [Google Scholar]
- 157.Matsumura Y, Maeda H, Cancer Res. 46 (1986) 6387–6392. [PubMed] [Google Scholar]
- 158.Wilhelm S, Tavares AJ, Dai Q, Ohta S, Audet J, Dvorak HF, Chan WCW, Nat. Rev. Mater 1 (2016) 16014. [Google Scholar]
- 159.Prabhakar U, Maeda H, Jain RK, Sevick-Muraca EM, Zamboni W, Farokhzad OC, Barry ST, Gabizon A, Grodzinski P, Blakey DC, Cancer Res. 73 (2013) 2412–2417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160.Danhier F, J. Control Release 244 (2016) 108–121. [DOI] [PubMed] [Google Scholar]
- 161.Li S, Zhang Y, Wang J, Zhao Y, Ji T, Zhao X, Ding Y, Zhao X, Zhao R, Li F, Yang X, Liu S, Liu Z, Lai J, Whittaker AK, Anderson GJ, Wei J, Nie G, Nat. Biomed. Eng 1 (2017) 667–679. [DOI] [PubMed] [Google Scholar]
- 162.Zhao R, Han X, Li Y, Wang H, Ji T, Zhao Y, Nie G, ACS Nano 11 (2017) 8103–8113. [DOI] [PubMed] [Google Scholar]
- 163.Postema M, Kotopoulis S, Delalande A, Gilja OH, Ultraschall. Med 33 (2012) 97–98. [Google Scholar]
- 164.Wang TY, Choe JW, Pu K, Devulapally R, Bachawal S, Machtaler S, Chowdhury SM, Luong R, Tian L, Khuri-Yakub B, Rao J, Paulmurugan R, Willmann JK, J. Control Release 203 (2015) 99–108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 165.Lee S, Han H, Koo H, Na JH, Yoon HY, Lee KE, Lee H, Kim H, Kwon IC, Kim K, J. Control. Release 263 (2017) 68–78. [DOI] [PubMed] [Google Scholar]
- 166.Han H, Lee H, Kim K, Kim H, J. Control Release 266 (2017) 75–86. [DOI] [PubMed] [Google Scholar]
- 167.Mou X, Ali Z, Li S, He N, J. Nanosci. Nanotechnol 15 (2015) 54–62. [DOI] [PubMed] [Google Scholar]
- 168.Huang J, Li Y, Orza A, Lu Q, Guo P, Wang L, Yang L, Mao H, Adv. Funct. Mater 26 (2016) 3818–3836. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 169.Nguyen KT, Zhao Y, Acc. Chem. Res 48 (2015) 3016–3025. [DOI] [PubMed] [Google Scholar]
- 170.Choi KY, Liu G, Lee S, Chen X, Nanoscale 4 (2012) 330–342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 171.Davis RM, Kiss B, Trivedi DR, Metzner TJ, Liao JC, Gambhir SS, ACS Nano 12 (2018) 9669–9679. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 172.Chen NT, Souris JS, Cheng SH, Chu CH, Wang YC, Konda V, Dougherty U, Bissonnette M, Mou CY, Chen CT, Lo LW, Nanomedicine 13 (2017) 1941–1952. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 173.Wadhwa A, Kandadai SK, Tongpresert S, Obal D, Gebhard RE, Anesthesiol. Res. Pract 2011 (2011) 262070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 174.Marhofer P, Greher M, Kapral S, Br. J. Anaesth 94 (2005) 7–17. [DOI] [PubMed] [Google Scholar]
- 175.Xie J, Lee S, Chen X, Adv. Drug Deliv. Rev 62 (2010) 1064–1079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 176.Liu J, Zheng X, Yan L, Zhou L, Tian G, Yin W, Wang L, Liu Y, Hu Z, Gu Z, Chen C, Zhao Y, ACS Nano 9 (2015) 696–707. [DOI] [PubMed] [Google Scholar]
- 177.Satterlee AB, Huang L, Theranostics 6 (2016) 918–929. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 178.Satpathy M, Wang L, Zielinski RJ, Qian W, Wang YA, Mohs AM, Kairdolf BA, Ji X, Capala J, Lipowska M, Nie S, Mao H, Yang L, Theranostics 9 (2019) 778–795. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 179.Yang B, Chen Y, Shi J, Adv. Mater 31 (2019) 1802896. [DOI] [PubMed] [Google Scholar]
- 180.Will O, Purkayastha S, Chan C, Athanasiou T, Darzi AW, Gedroyc W, Tekkis PP, Lancet Oncol. 7 (2006) 52–60. [DOI] [PubMed] [Google Scholar]
- 181.Zhao T, Huang G, Li Y, Yang S, Ramezani S, Lin Z, Wang Y, Ma X, Zeng Z, Luo M, de Boer E, Xie XJ, Thibodeaux J, Brekken RA, Sun X, Sumer BD, Gao J, Nat. Biomed. Eng 1 (2016) 0006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 182.Li CH, Kuo TR, Su HJ, Lai WY, Yang PC, Chen JS, Wang DY, Wu YC, Chen CC, Sci. Rep 5 (2015) 15675. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 183.Hu Z, Chi C, Liu M, Guo H, Zhang Z, Zeng C, Ye J, Wang J, Tian J, Yang W, Xu W, Nanomedicine 13 (2017) 1323–1331. [DOI] [PubMed] [Google Scholar]
- 184.Yang L, Sajja HK, Cao Z, Qian W, Bender L, Marcus AI, Lipowska M, Wood WC, Wang YA, Theranostics 4 (2013) 106–118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 185.Satterlee AB, Yuan H, Huang L, J. Control Release 217 (2015) 170–182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 186.Chen Q, Liang C, Wang X, He J, Li Y, Liu Z, Biomaterials 35 (2014) 9355–9362. [DOI] [PubMed] [Google Scholar]
- 187.Ho YJ, Chang YC, Yeh CK, Theranostics 6 (2016) 392–403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 188.Kong SD, Zhang W, Lee JH, Brammer K, Lal R, Karin M, Jin S, Nano Lett. 10 (2010) 5088–5092. [DOI] [PubMed] [Google Scholar]
- 189.Li F, Du Y, Liu J, Sun H, Wang J, Li R, Kim D, Hyeon T, Ling D, Adv. Mater 30 (2018) 1802808. [DOI] [PubMed] [Google Scholar]
- 190.Wang H, Zhao Y, Wu Y, Hu YL, Nan K, Nie G, Chen H, Biomaterials 32 (2011) 8281–8290. [DOI] [PubMed] [Google Scholar]
- 191.Ruan H, Hu Q, Wen D, Chen Q, Chen G, Lu Y, Wang J, Cheng H, Lu W, Z Gu, Adv. Mater 31 (2019) e1806957. [DOI] [PubMed] [Google Scholar]


