ABSTRACT
Food environment research is increasingly gaining prominence in low- and middle-income countries (LMICs). However, in the absence of a systematic review of the literature, little is known about the emerging body of evidence from these settings. This systematic scoping review aims to address this gap. A systematic search of 6 databases was conducted in December 2017 and retrieved 920 records. In total, 70 peer-reviewed articles met the eligibility criteria and were included. Collectively, articles spanned 22 LMICs, including upper-middle-income countries (n = 49, 70%) and lower-middle-income countries (n = 18, 26%). No articles included low-income countries. Articles featured quantitative (n = 45, 64%), qualitative (n = 17, 24%), and mixed-method designs (n = 11, 8%). Studies analyzed the food environment at national, community, school, and household scales. Twenty-three articles (55%) assessed associations between food environment exposures and outcomes of interest, including diets (n = 14), nutrition status (n = 13), and health (n = 1). Food availability was associated with dietary outcomes at the community and school scales across multiple LMICs, although associations varied by vendor type. Evidence regarding associations between the food environment and nutrition and health outcomes was inconclusive. The paucity of evidence from high-quality studies is a severe limitation, highlighting the critical need for improved study designs and standardized methods and metrics. Future food environment research must address low-income and lower-middle-income countries, and include the full spectrum of dietary, nutrition, and health outcomes. Improving the quality of food environment research will be critical to the design of feasible, appropriate, and effective interventions to improve public health nutrition in LMICs.
Keywords: food environment, nutrition environment, obesogenic environment, food desert, low- and middle-income countries, double burden of malnutrition, food and nutrition security, diets, nutrition, health
Introduction
Food environment research is gaining prominence in low- and middle-income countries (LMICs) at the start of the UN Decade of Action on Nutrition 2016–2025 (1). Policymakers seeking to tackle global food and nutrition security and the double burden of malnutrition are increasingly turning their attention to the role that food environments play in shaping diets, nutrition, and health in these settings (2–4).
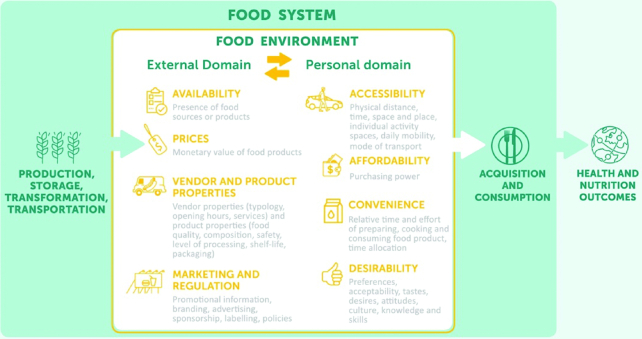
Food environments have been described as the interface where people interact with the wider food system to acquire and consume foods (5, 6). Recent conceptual work has sought to define external and personal food environment domains applicable to global settings (5) (Figure 1). The external domain features exogenous dimensions such as food availability, prices, vendor and product properties, and marketing and regulation, whereas the personal domain consists of individual-level dimensions, including food accessibility, affordability, convenience, and desirability. Improved knowledge and understanding of the interactions between these domains and dimensions are needed to address the double burden of malnutrition in LMICs, characterized by persistent undernutrition amongst women and children, as well as the increasing prevalence of overweight, obesity, and nutrition-related chronic diseases (NRCDs).
FIGURE 1.
Conceptual framework. The conceptual framework depicts the food environment as the interface within the wider food system where people interact with food sources to acquire and consume foods. The external domain features exogenous dimensions such as food availability, prices, vendor and product properties, and marketing, and regulation, whereas the personal domain consists of dimensions relative to individuals, including food accessibility, affordability, convenience, and desirability. Complex interactions between these domains and dimensions shape food acquisition and consumption. (Reproduced from reference (5) with permission from Elsevier.)
Food environment research has developed over recent decades within high-income countries (HICs) in response to the high prevalence of overweight, obesity, and NRCDs. Several systematic reviews have documented research methods and measures from HICs, as well as findings related to diet and nutrition outcomes (7–12). However, in the absence of a systematic review of the literature from LMICs, little is known about the state of science and the emerging body of evidence from these settings. This is a significant research gap given the fundamental differences between HICs and LMICs with regard to food systems, food environments, food acquisition and consumption practices, and public health nutrition challenges. This systematic scoping review aims to fill this gap by addressing 5 questions in relation to the literature from LMICs: 1) Where has food environment research been undertaken? 2) How have food environments been conceptualized? 3) Which key domains and dimensions of food environments have been studied? 4) Which study designs, methods, and measures have been implemented? 5) What are the key findings regarding associations between food environment exposure and dietary, nutrition, and health outcomes? The synthesis of knowledge from this review is intended to mobilize a rigorous research agenda and inform evidence-based practice in LMICs, contributing towards Sustainable Development Goal (SDG) targets to end hunger (SDG Target 2.1) and all forms of malnutrition (SDG Target 2.2) (13).
Methods
Systematic scoping review
We undertook a systematic scoping review. This type of systematic review is recognized as a salient approach when synthesizing knowledge from a diverse body of literature that has yet to be reviewed (14, 15). We followed the Preferred Reporting Items for Systematic Reviews and Meta-Analyses—Extension for Scoping Reviews (PRISMA-ScR) checklist and guidelines to ensure a robust and replicable process (15). The protocol is available upon request from the corresponding author.
Data collection
Search strategy
We conducted a systematic search of the following 6 electronic databases for articles published between January 2000 and December 2017: Medline, Embase, Global Health, EconLit, Web of Science, and Scopus. Search terms included: “food environment,” “nutrition environment,” “obesogenic environment,” “food deserts,” and “food swamps.” These terms were informed by a priori knowledge and were intended to capture the breadth of the nomenclature used in food environment research. Our search strategy featured the search terms in conjunction with the 140 LMICs as defined by the World Bank for the year 2017 (16). The search strategy for Scopus is provided as an example (Supplemental Methods 1). No restrictions were set with regard to publication language. Scoping of results from an initial search with no date restrictions determined January 2000 to be an appropriate cut-off year, as no potentially relevant articles were identified prior to this date.
Inclusion criteria
Original peer-reviewed published articles were considered for inclusion if they met the following criteria: 1) included ≥1 of the search terms; 2) included ≥1 LMIC; and 3) described or assessed the food environment or its associations with diets, nutrition status, or health outcomes.
Exclusion criteria
Articles were excluded if they fulfilled the following criteria: 1) did not primarily assess the food environment or any of the key concepts; 2) did not feature ≥1 LMIC; 3) were not original peer-reviewed research articles; or 4) did not contain sufficient evidence from a LMIC.
Data screening
All records were screened independently by 2 of the authors according to the eligibility criteria. Title and abstract screening was followed by the retrieval and screening of full-text articles. The screening protocol was piloted on 6 articles to ensure consistency. Interrater agreement was high. Any disagreements were resolved through discussion between screening authors. Two articles in Spanish were screened by an additional reviewer fluent in the language.
Data charting
Data charting was completed by 2 authors with a focus on study design, key concepts, food environment domains and dimensions (Figure 1), and any exposure, confounding, and outcome variables. Methods were categorized as either geospatial or observational (5). The data charting form was piloted on a random sample of 10 articles and refined following consultation with a third reviewer.
Quality assessment
Articles testing for associations between food environment exposure and dietary, nutrition or health outcomes were subjected to a quality assessment by 2 authors with the use of the National Heart Lung and Blood Institute checklists (17) or the Mixed-Methods Appraisal Tool (18) as appropriate. Observational notes were also taken with a focus on rigor when controlling for confounding. Quality was rated good, fair, or poor. Any discrepancies between reviewers were resolved through discussion.
Results
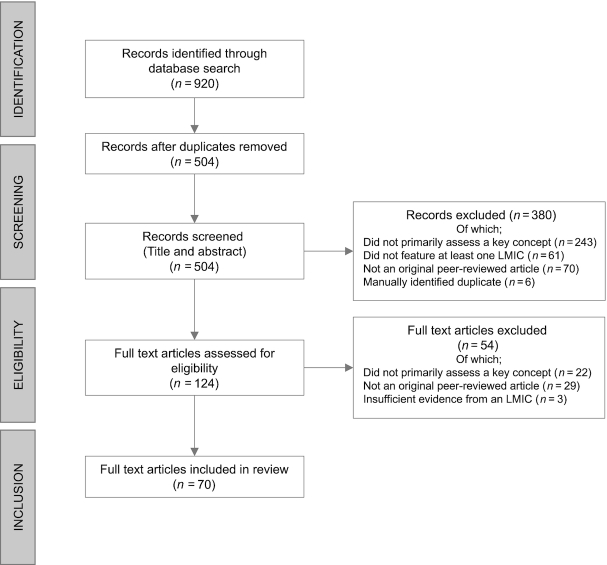
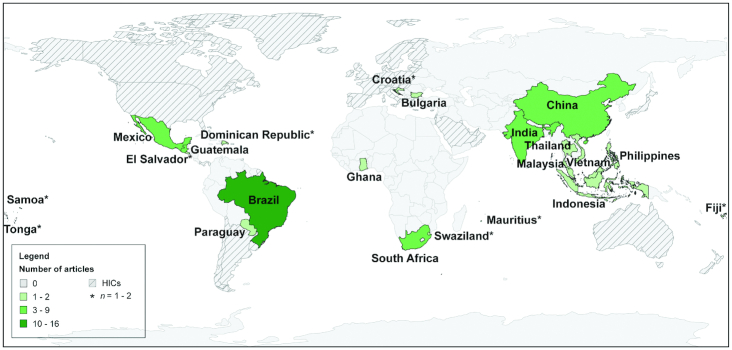
In total, 70 articles were included (Figure 2). An overview of key study characteristics is provided (Supplemental Table 1). Articles were published from 2009 to 2017, with the number of publications increasing per annum (Figure 3).
FIGURE 2.
Search tree.
FIGURE 3.
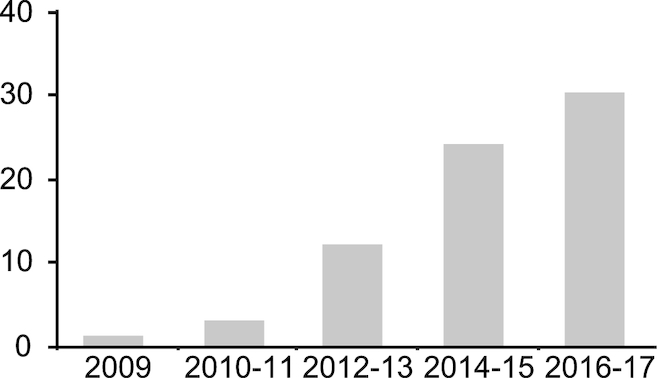
Publication year of included articles.
Where has food environment research been undertaken in LMICs?
The included studies spanned 22 LMICs. Forty-nine studies (70%) featured upper-middle-income countries, and 18 (26%) included lower-middle income countries. No studies were located in low-income countries. Three studies (4%) featured multiple countries from different income-level quartiles, 2 of which drew comparisons between upper-middle-income countries and HICs (19, 20), whilst 1 compared a lower-middle-income country with an HIC (21).
At the regional scale, Latin America and the Caribbean had the highest number of publications (n = 31), followed by East Asia and Pacific (n = 17), Sub-Saharan Africa (n = 11), South Asia (n = 6), and Europe and Central Asia (n = 3). Although Sub-Saharan Africa ranked third, South Africa dominated the continent with only 4 studies from elsewhere in the region. At the national scale, only 6 LMICs featured >2 studies: Brazil (n = 16), China (n = 9), Mexico (n = 8), South Africa (n = 7), India (n = 6), and Guatemala (n = 5) (Figure 4).
FIGURE 4.
The geographic distribution of included articles across LMICs.
How have food environments been conceptualized in LMICs?
Sixty studies used a single key concept from our search terms or derivatives thereof, including “food environment” (n = 48), “obesogenic environment” (n = 6), “food desert” (n = 4), and “nutrition environment” (n = 2). Ten studies used various combinations of these key concepts. “Food swamp” was the only search term not used as a single stand-alone concept. Only 26 articles (37%) defined the key concept or concepts used to frame the study. Of these, the majority (n = 21) cited existing definitions, whilst 5 provided their own definition.
Which key domains and dimensions of food environments have been studied in LMICs?
The external food environment domain featured prominently, including dimensions of availability (n = 63), vendor and product properties (n = 27), prices (n = 25), and marketing and regulation (n = 20). The personal food environment domain has been addressed to a lesser extent through dimensions of accessibility (n = 26), desirability (n = 21), convenience (n = 15), and affordability (n = 14). Most studies (63%) included multiple food environment dimensions. However, only around half (n = 33, 47%) addressed dimensions from both the external and personal food environment domains. Of these, one-third (n = 11, 33%) focused exclusively on availability in combination with accessibility, the 2 most commonly studied dimensions from each respective domain. Although the external and personal food environment domains have broadly been included, few articles analyzed interactions between dimensions, either within or across domains.
Which study designs, methods, and measures have been implemented in LMICs?
Quantitative articles
Forty-five articles (64%) used quantitative methods in isolation, either to describe or analyze the food environment, or test for associations with outcomes of interest. Amongst these articles, the vast majority (n = 39, 87%) featured cross-sectional study designs, whereas 3 used longitudinal data from the China Health Survey dataset (22–24), 2 used experimental designs (25, 26), and 1 implemented a modeling design (27). Quantitative articles featured a range of measurement methods, including market-based measures (n = 24), stakeholder-based measures (n = 17), and geographic information systems–based measures (n = 16) (Supplemental Table 2). The majority (n = 32) utilized 1 of these measurement methods in isolation, whereas 11 articles included 2 approaches, and 1 article included all 3. Four articles primarily focused on the adaptation and application of quantitative market-based survey tools from HICs (28–31).
Qualitative articles
Seventeen articles (24%) used qualitative stakeholder-based methods to investigate food environments. The majority (n = 10) featured a single method, such as semi-structured interviews (32–37), in-depth interviews (38), focus group discussions (21), and stakeholder workshops or dialog (39, 40). Seven articles used multiple qualitative methods (41–47).
Mixed method articles
Eight articles (11%) featured mixed methods. Measurement methods included stakeholder-based methods (n = 7), market-based methods (n = 6), and geographic information systems–based methods (n = 3). The majority of mixed-method articles combined ≥2 of these approaches (48–53). Mixed-method studies used similar methods and measures to those presented above.
Characterizing and analyzing food environments in LMICs
National scale
Three articles addressed the influence of national scale policies on LMIC food environments. In Vietnam, significant increases in the availability of sugar-sweetened beverages (SSBs) were found following foreign direct investment and trade liberalization policies when compared with a control case, the Philippines (54). Qualitative articles garnered stakeholder perspectives on national scale policies in Thailand (34), and in the Pacific island states of Fiji and Tonga (39). Common themes included the need to modify the availability, accessibility, prices, and quality and marketing of healthy and unhealthy foods.
Community scale
A number of articles characterized the availability of food sources and products at the community scale (45, 52, 53, 55–60). Evidence suggests that small- and medium-sized market-based vendors dominate across a number of LMIC settings (52, 58–60). Distinctions between formal and informal market-based vendors were identified. For example, in Cape Town, South Africa, a structural disconnect was found between the strategies of formal supermarkets and the needs of the poor, whereas informal vendors provided sources of cheaper, lower-quality foods available on credit (53). Nonmarket-based food sources were also found to be important in some settings. Examples include own production in Salvadorian communities vulnerable to food insecurity (45), and wild food harvesting in Brazilian rainforest cities (59).
Three articles from diverse settings found positive associations between levels of urbanization and the availability of market-based food vendors, such as fast-food restaurants, full-service restaurants, and supermarkets (23, 31, 60). Three articles applied a food desert perspective (49, 59, 61). In Brazil, food deserts characterized by insufficient availability and accessibility of healthy foods, particularly fruits and vegetables, were found to be widespread amongst urban communities (59). In Mexico, food swamps, rather than food deserts, typified by the inundation of unhealthy foods and drinks, were identified amongst low- and middle-income communities. In contrast, food oases were identified amongst high-income communities with limited availability of less-healthy options (49).
A number of qualitative and mixed-method articles from a range of communities described complex and contradictory perceptions and experiences of food environments. Common themes included the increasing availability and acceptance of cheap, convenient, tasty, and desirable ready-made “modern” foods, coupled with economic constraints limiting opportunities for healthier alternatives (32, 33, 45, 51). Multifaceted barriers to healthier diets were also identified in 2 studies of cross-border migrants in Cape Town, South Africa, and included an unfamiliar dependency on market-based food sources, discourse around inferior, unnatural, and unvaried food, and the fear of xenophobic violence restricting travel outside of local neighborhoods (46, 47).
School scale
Quantitative evidence from multiple settings consistently found school food environments to be saturated with vendors selling unhealthy foods and beverages (62–68). The targeted marketing of SSBs to children was also evident (62, 64). Qualitative assessments supported the notion of readily available, affordable, and desirable unhealthy foods and beverages, whereas healthier options were found to be limited in many school settings (35, 36, 42, 43). Qualitative evidence from India also raised additional concerns around misleading marketing messages, food safety, and the importance of peer influence in school canteens (35, 36), as well as the role of food prestige placed upon non-traditional, foods from roadside vendors, restaurants, and small grocery stalls around schools (41).
School policies were found to be highly contested amongst a wide array of actors (36, 40, 43). For example, qualitative evidence from Mexico revealed divergent stakeholder perspectives on proposed policies to regulate the sale of unhealthy foods in schools, with consolidated support amongst academics, health professionals, citizens, and parents juxtaposed against food industry concerns surrounding a negative public image, loss of income, and reduced employment opportunities (40).
Household scale
Evidence from multiple LMICs highlights a range of issues faced at the household scale, such as the role of traditional family structures and complex eating patterns in Brazil (19, 69), the perceived low efficacy of low-income mothers to provide their children with nutritious foods in Jakarta, Indonesia (38), and the targeted television marketing and promotion of unhealthy foods to children during school holidays in Malaysia (70).
Assessing associations between food environment exposures and diet, nutrition, and health outcomes in LMICs
Amongst the 42 quantitative and mixed-method articles, 23 (55%) sought to assess associations between food environment exposure and diet, nutrition, and health outcomes (Supplemental Table 3). Common food environment exposures included availability (vendor counts or densities) (n = 13), accessibility (distance to vendors or travel time) (n = 4), perceived availability (n = 2), food vendor choice (frequency of visits) (n = 2), and multicomponent indicators (n = 2) (20, 71). The majority of these analytical articles (n = 18, 78%) focused on a single type of outcome in isolation, whereas comparatively few (n = 5, 22%) included multiple types of outcomes. Overall, most analytical articles (n = 16, 70%) identified ≥1 significant association between food environment exposures and outcomes of interest. A synthesis of results related to dietary and nutrition outcomes is provided below. Only 1 study featured health outcomes in the form of doctor-diagnosed diseases (e.g., hypertension); however, no significant associations were found and the results are not reported in the text (72). On the whole, the quality of evidence from studies examining associations between food environment exposure and dietary, nutrition, and health outcomes was low, with 2 articles rated good (22, 73), 5 rated fair (25, 74–77), and 16 rated poor (20, 24, 26, 71, 72, 78–88) (Supplemental Tables 4 and 5). We therefore encourage the reader to exercise caution when interpreting results.
Dietary outcomes
Fourteen articles included dietary outcomes. The majority of these articles (n = 11, 79%) reported ≥1 significant association between food environment exposure and dietary outcome. Most articles (n = 10) framed dietary outcomes in terms of the consumption of multiple food groups, although a few (n = 3) focused on a singular food group, and 1 featured dietary intake of kilocalories and macronutrients. Dietary diversity was used as a measure of dietary quality in 1 article (26).
Community scale
Cross-sectional evidence from multiple settings found the neighborhood availability of food vendors to be significantly associated with dietary consumption, although associations varied with vendor typology (22, 73, 87). Perceptions of food availability were also found to be significantly and positively associated with food acquisition and dietary outcomes amongst diverse Brazilian populations (76, 85). However, perceptions of other dimensions, such as proximity to vendors, food quality, or variety, were not found to be associated with fruit and vegetable intake amongst pregnant women in Ribeirão Preto City, Brazil (77).
School scale
Evidence from 2 randomzed controlled trials indicates the potential for supportive school food environments to improve adolescent diets. A school-based intervention in Mexico designed to improve the school food environment by reducing the availability of energy-dense foods and SSBs reported statistically significant reductions in the intake of non-recommended foods and beverages (25). In South Africa, a school-based intervention designed to increase the availability of healthier food options, provide nutrition education, and form school policies produced no significant effects on dietary diversity or the intake of fat and sugar between 2009 and 2011, although minor improvements in dietary diversity and restricted intake of sugar were reported (26). Cross-sectional evidence from Brazil found the availability of vendors selling unhealthy foods in and around schools to be significantly and positively associated with the regular intake of these foods amongst adolescents (83). In Guatemala, common correlates of SSB consumption included school type (public or private), sedentary behavior, frequency of purchasing lunch from school cafeterias, and frequency of purchasing snacks from vending machines (74). Cross-sectional evidence also highlighted the importance of other dimensions amongst adolescents, such as accessibility, with travel time to and from school found to be significantly and positively associated with purchasing food at or near schools in Ghana (75).
Nutrition outcomes
Thirteen articles included nutrition outcomes. Of these, 6 (46%) found ≥1 significant association between food environment indicators and nutrition outcomes. BMI was used as the primary nutrition outcome amongst these articles, calculated with either measured (n = 9) or self-reported (n = 4) height and weight.
Community scale
Cross-sectional evidence from multiple settings identified significant associations between the availability (measured as density) of food vendors and BMI, although vendor type was found to have variable associations (86, 88). For example, a significant positive relationship was found between convenience stores and BMI in Ghana as hypothesized, whilst a significant negative relationship was found between out-of-home foods and BMI, the opposite to what was expected (86).
School scale
Evidence from a school-based randomized controlled trial in Mexico seeking to reduce the availability of energy-dense foods and SSBs found significant changes in BMI across intervention groups, although not always in the anticipated direction. Schools featuring a basic level of intervention (reliant on existing school resources) displayed increases in BMI, whereas plus-level intervention schools (provided with additional funding) and control schools showed reductions in BMI (25). Cross-sectional evidence from multiple settings also produced mixed findings. In Mexico, the availability of mobile vendors in and around schools was found to be significantly and positively associated with children's BMI, although significantly higher numbers of retail food sources around public schools produced no statistical difference on children's BMI when compared to private schools (84). A multinational study featuring Bulgarian schools (amongst others) found significant positive associations between the healthiness of the nutrition environments and the highest BMI-for-age z scores, contrary to the hypothesized expectation (20).
Discussion
The 70 articles included in this systematic scoping review constitute the rapidly emerging yet nascent body of food environment research from LMICs. Evidence from low-quality studies show that food availability is associated with dietary outcomes at both the community and school scales across multiple LMICs, although associations were found to vary by vendor type. Evidence regarding associations between food environment exposure and nutrition status is inconclusive at present, whilst evidence related to health outcomes is almost nonexistent.
The focus on outcomes related to overweight and obesity revealed in this review reflects a number of factors, including the increasing recognition of the nutrition transition that is underway across LMICs (89), the high proportion of upper-middle-income countries studied to date, many of which are arguably a considerable way along this trajectory (4), and also the development and adaptation of food environment research from HIC settings where these outcomes have typically taken precedence. However, the absence of attention to undernutrition is a striking omission within the literature. Food environment research in LMICs must seek to tackle the full spectrum of pressing public health nutrition challenges at hand (2–6), including undernutrition, overweight, obesity, and NRCDs. Research is urgently needed in lower-middle and low-income countries to track rapidly transitioning food environments and diets, and to identify the main pathways between food insecurity and multiple forms of malnutrition in these settings (90).
The lack of standardized food environment instruments and indicators identified in this review is broadly consistent with systematic reviews of the literature from HICs (7–11). Standardized instruments and indicators are needed to profile food environments across diverse LMIC settings and provide robust assessments of the influence of the food environment on transitioning diets, nutrition, and health. Deeper integration is needed between concepts, instruments, and indicators to improve the alignment between food environment exposures and outcomes of interest. The need to complement standardized dietary assessment instruments with ultraprocessed foods and out-of-home foods is increasingly being recognized (91), and such developments would benefit food environment research by harmonizing with data collection on the availability of these items.
The primary focus allocated to the external food environment domain and dimensions found in this review mirrors findings from HICs (7, 92). Although the personal food environment domain has featured less prominently, it has nevertheless received notable attention in LMICs. This is likely due to the increasing recognition of the need to understand lesser-studied dimensions such as affordability, desirability, and convenience (92, 93), the use of qualitative methods adept at capturing perceptions and experiences of such dimensions in understudied settings, and also the role that these dimensions play in food acquisition and consumption practices in LMICs. Going forward, food environment research must strive to improve understanding of the socio-ecological processes that shape food acquisition, diets, nutrition, and health (5). Establishing which dimensions are of particular importance across diverse LMIC settings and populations will be key. Mixed-methods studies are currently underutilized yet offer the opportunity for more comprehensive, multiscalar and nuanced assessments of food environments.
The paucity of evidence from high-quality analytical studies testing for associations between food environment exposures and dietary, nutrition, and health outcomes is a severe constraint at present. The current limited evidence base should not be interpreted as to diminish the importance of food environment exposure on diet, nutrition, and health outcomes in LMICs, but rather to emphasize the need to improve theoretical concepts, study designs, methods, and metrics to better capture, assess, and understand the socio-ecological interactions taking place. Similar calls have previously been made amongst several reviews from HICs (7, 9–11, 92). Recommendations for future food environment research in LMICs are provided in Box 1.
Recommendations for food environment research in LMICs
Research should seek to harmonize theoretical concepts with empirical research.
Low-income countries and lower-middle-income countries should be considered a priority given the current paucity of studies from these settings and the pressing public health nutrition challenges at hand.
Research should address the double burden of malnutrition, including undernutrition, overweight, obesity, and NRCDs.
The development, testing and validation of standardized instruments and metrics to profile food environments should be prioritized to track transitioning diets across diverse settings in LMICs.
Rigorous mixed-methods designs should be implemented to provide comprehensive assessments of external and personal food environment domains and dimensions.
Research should apply robust longitudinal and experimental designs at multiple scales to assess the impact of interventions on diets, nutrition status, and health outcomes in LMICs.
Strengths and Limitations
This systematic scoping review is the first to focus exclusively on food environment research from LMICs. The strengths of this review include the use of the PRISMA-ScR guidelines to ensure a robust and replicable process, the use of 6 electronic databases to capture the breadth and depth of peer-reviewed publications, the inclusion of quantitative, qualitative, and mixed-methods articles, the use of the conceptual framework to guide the reporting and analysis, and the quality assessment of analytical articles. We acknowledge a number of limitations. First, in order to maintain the feasibility of this systematic scoping review we focused on the established food environment terminology. However, we recognize that there is a wealth of relevant research from wide-ranging disciplines that may not necessarily apply this nomenclature. For example, we acknowledge the following studies that address food environment dimensions in LMICs without referring to the wider construct (94, 95). Second, we conducted this systematic scoping review in adherence to the PRISMA-ScR guidelines with the aim of providing a comprehensive synthesis of the diverse food environment literature emerging from LMICs. The ability to synthesize disparate literature is a key strength of systematic scoping reviews. However, the inclusion of such a broad range of articles also limits the scope for the kinds of fine-grained analysis that other systematic review styles with a narrower aperture provide. Third, although we did not set any restrictions regarding publication language, our search terms were written in English, potentially excluding articles written in other languages. Fourth, our focus on peer-reviewed empirical articles excluded any potentially relevant gray-literature publications.
Conclusions
This systematic scoping review reveals the rapidly emerging body of food environment literature from LMICs. The included articles predominantly feature upper-middle-income countries and outcomes related to overweight and obesity. Going forward, food environment research must address low-income and lower-middle-income countries as a priority, and seek to include the full spectrum of diets, nutritional status, and health outcomes. The paucity of evidence from high-quality analytical studies indicates the urgent need to improve study designs, methods, and metrics to better capture external and personal food environment domains and dimensions. Improving the quality of food environment research will be critical to the design of feasible, appropriate, and effective interventions to improve public health nutrition in LMICs.
Supplementary Material
ACKNOWLEDGEMENTS
We thank Lauren Blake for her contributions to the screening of manuscripts written in Spanish. We also thank Helen Harris-Fry for her critical contributions to the quality assessment process. The authors’ responsibilities were as follows—CT: conceived the paper, conducted the systematic search and screening, conducted data charting, analysis, and quality assessment, led the writing process, and finalized the manuscript for submission; S Kalamatianou: conducted the systematic search, screening, data charting, and provided critical feedback on the manuscript; AD, BK, S Kinra: provided critical feedback on the manuscript; S Kadiyala: conducted quality assessments and provided critical feedback on the initial paper concept, the data charting, and the manuscript throughout the writing process; and all authors: read and approved the final manuscript.
Notes
This research is funded by the Innovative Methods and Metrics for Agriculture and Nutrition Actions (IMMANA) program, funded with UK aid from the UK Government (grant 6682), the Leverhulme Centre for Integrated Research on Agriculture and Health, and the Department of Epidemiology and Population Health Studentship 2015, London School of Hygiene and Tropical Medicine, United Kingdom.
Author disclosures: CT, SK, AD, BK, S Kinra, and S Kadiyala, no conflicts of interest.
Supplemental Methods 1 and Supplemental Tables 1–5 are available from the “Supplementary data” link in the online posting of the article and from the same link in the online table of contents at https://academic.oup.com/advances/.
Abbreviations used: HIC, high-income country; LMIC, low- and middle-income country; NRCD, nutrition-related chronic disease; PRISMA-ScR, Preferred Reporting Items for Systematic Reviews and Meta-Analyses—Extension for Scoping Reviews; SDG, Sustainable Development Goal; SSB, sugar-sweetened beverage.
References
- 1. United Nations General Assembly. United Nations Decade of Action on Nutrition (2016–2025), GA Res 70/259, UN GAOR, 70th Session, Suppl 49, UN Doc A/RES/70/259. United Nations General Assembly; 2016. [Google Scholar]
- 2. Development Initiatives. Global nutrition report 2017: nourishing the SDGs. Bristol: Development Initiatives; 2017. [Google Scholar]
- 3. Global Panel on Agriculture and Food Systems for Nutrition. Improving nutrition through enhanced food environments. Policy Brief. London: Global Panel on Agriculture and Food Systems for Nutrition; 2017. [Google Scholar]
- 4. High Level Panel of Experts on Food Security and Nutrition. Nutrition and food systems. A report by the High Level Panel of Experts on Food Security and Nutrition of the Committee on World Food Security. Rome; 2017. [Google Scholar]
- 5. Turner C, Aggarwal A, Walls H, Herforth A, Drewnowski A, Coates J, Kalamatianou S, Kadiyala S. Concepts and critical perspectives for food environment research: a global framework with implications for action in low- and middle-income countries. Global Food Security. 2018;18:93–101. [Google Scholar]
- 6. Food and Agriculture Organization of the United Nations. Influencing food environments for healthy diets. Rome: FAO; 2016. [Google Scholar]
- 7. Caspi CE, Sorensen G, Subramanian SV, Kawachi I. The local food environment and diet: a systematic review. Health Place. 2012;18(5):1172–87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Cetateanu A, Jones A.. How can GPS technology help us better understand exposure to the food environment? A systematic review. SSM Popul Health. 2016;2:196–205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Engler-Stringer R, Le H, Gerrard A, Muhajarine N. The community and consumer food environment and children's diet: a systematic review. BMC Public Health. 2014;14:522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Gamba RJ, Schuchter J, Rutt C, Seto EY. Measuring the food environment and its effects on obesity in the United States: a systematic review of methods and results. J Community Health. 2015;40(3):464–75. [DOI] [PubMed] [Google Scholar]
- 11. Gustafson A, Hankins S, Jilcott S. Measures of the consumer food store environment: a systematic review of the evidence 2000–2011. J Community Health. 2012;37(4):897–911. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Lytle LA, Sokol RL.. Measures of the food environment: a systematic review of the field, 2007–2015. Health Place. 2017;44:18–34. [DOI] [PubMed] [Google Scholar]
- 13. United Nations General Assembly, Transforming Our World: the 2030 agenda for sustainable development, GA Res 70/1, UN GAOR, 70th Session, Suppl 49, UN Doc A/RES/70/1, United Nations General Assembly, 2015. [Google Scholar]
- 14. Peters MD, Godfrey CM, Khalil H, McInerney P, Parker D, Soares CB. Guidance for conducting systematic scoping reviews. Int J Evid Based Healthc. 2015;13(3):141–6. [DOI] [PubMed] [Google Scholar]
- 15. Tricco AC, Lillie E, Zarin W, O'Brien KK, Colquhoun H, Levac D, Moher D, Peters MDJ, Horsley T, Weeks L et al.. PRISMA Extension for Scoping Reviews (PRISMA-ScR): checklist and explanation. Ann Intern Med. 2018;169(7):467–73. [DOI] [PubMed] [Google Scholar]
- 16. World Bank. World Bank country and lending groups[Internet]. 2017. [cited 2017 Dec 1]. Available from: https://datahelpdesk.worldbank.org/knowledgebase/articles/906519-world-bank-country-and-lending-groups. [Google Scholar]
- 17. National Heart Lung and Blood Institute. Quality assessment tool for observational cohort and cross-sectional studies: US Department of Health and Human Services. [Internet] 2018; [accessed 2018 Apr 13]. Available from: https://www.nhlbi.nih.gov/health-topics/study-quality-assessment-tools. [Google Scholar]
- 18. Pluye P, Robert E, Cargo M, Bartlett G, O'Cathain A, Griffiths F, Boardman F, Gagnon MP, Rousseau MC. Proposal: a mixed methods appraisal tool for systematic mixed studies reviews. [Internet] 2011; [accessed 2018 Apr 13]. Available from: http://mixedmethodsappraisaltoolpublic.pbworks.com.
- 19. Estima CCP, Bruening M, Hannan PJ, Alvarenga MS, Leal GVS, Philippi ST, Neumark-Sztainer D. A cross-cultural comparison of eating behaviors and home food environmental factors in adolescents from Sao Paulo (Brazil) and Saint Paul-Minneapolis (US). J Nutr Educ Behav. 2014;46(5):370–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Wijnhoven TMA, van Raaij JMA, Sjoberg A, Eldin N, Yngve A, Kunesova M, Starc G, Rito AI, Duleva V, Hassapidou M et al.. WHO European Childhood Obesity Surveillance Initiative: school nutrition environment and body mass index in primary schools. Int J Environ Res Public Health. 2014;11(11):11261–85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Fuster M, Colón-Ramos U.. Changing places, changing plates? A binational comparison of barriers and facilitators to healthful eating among Central American communities. J Immigr Minor Healt. 2017;20(3):705–10. [DOI] [PubMed] [Google Scholar]
- 22. Wang R, Shi L.. Access to food outlets and children's nutritional intake in urban China: a difference-in-difference analysis. Ital J Pediatr. 2012;38:30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Wu Y, Xue H, Wang HJ, Su C, Du SF, Wang YF. The impact of urbanization on the community food environment in China. Asia Pac J Clin Nutr. 2017;26(3):504–13. [DOI] [PubMed] [Google Scholar]
- 24. Zhang J, Xue H, Cheng X, Wang ZH, Zhai FY, Wang YF, Wang HJ. Influence of proximities to food establishments on body mass index among children in China. Asia Pac J Clin Nutr. 2016;25(1):134–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Safdie M, Jennings-Aburto N, Lévesque L, Janssen I, Campirano-Núñez F, López-Olmedo N, Aburto T, Rivera JA. Impact of a school-based intervention program on obesity risk factors in Mexican children. Salud Publica Mex. 2013;55(Suppl 3):S374–87. [DOI] [PubMed] [Google Scholar]
- 26. Steyn NP, de Villiers A, Gwebushe N, Draper CE, Hill J, de Waal M, Dalais L, Abrahams Z, Lombard C, Lambert EV. Did HealthKick, a randomised controlled trial primary school nutrition intervention improve dietary quality of children in low-income settings in South Africa?. BMC Public Health. 2015;15:948. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Su SL, Li ZK, Xu MY, Cai ZL, Weng M. A geo-big data approach to intra-urban food deserts: transit-varying accessibility, social inequalities, and implications for urban planning. Habitat Int. 2017;64:22–40. [Google Scholar]
- 28. Duran AC, Lock K, Latorre MRDO, Jaime PC. Evaluating the use of in-store measures in retail food stores and restaurants in Brazil. Rev Saude Publica. 2015;49:2–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Kanter R, Alvey J, Fuentes D. A novel mobile phone application to assess nutrition environment measures in low- and middle-income countries. Food Nutr Bull. 2014;35(3):296–300. [DOI] [PubMed] [Google Scholar]
- 30. Martins PA, Cremm EC, Leite FHM, Maron LR, Scagliusi FB, Oliveira MA. Validation of an adapted version of the Nutrition Environment Measurement Tool for Stores (NEMS-S) in an urban area of Brazil. J Nutr Educ Behav. 2013;45(6):785–92. [DOI] [PubMed] [Google Scholar]
- 31. Hua JN, Seto E, Li Y, Wang MC. Development and evaluation of a food environment survey in three urban environments of Kunming, China. BMC Public Health. 2014;14:235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Hardin J, Kwauk CT.. Producing markets, producing people: local food, financial prosperity and health in Samoa. Food, Culture and Society. 2015;18(3):519–39. [Google Scholar]
- 33. Kimoto R, Ronquillo D, Caamaño MC, Martinez G, Schubert L, Rosado JL, Garcia O, Long KZ. Food, eating and body image in the lives of low socioeconomic status rural Mexican women living in Queretaro State, Mexico. Health Place. 2013;25:34–42. [DOI] [PubMed] [Google Scholar]
- 34. Phulkerd S, Vandevijvere S, Lawrence M, Tangcharoensathien V, Sacks G. Level of implementation of best practice policies for creating healthy food environments: assessment by state and non-state actors in Thailand. Public Health Nutr. 2017;20(3):381–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Rathi N, Riddell L, Worsley A. What influences urban Indian secondary school students' food consumption?—A qualitative study. Appetite. 2016;105:790–7. [DOI] [PubMed] [Google Scholar]
- 36. Rathi N, Riddell L, Worsley A. Food environment and policies in private schools in Kolkata, India. Health Promot Int. 2017;32(2):340–50. [DOI] [PubMed] [Google Scholar]
- 37. Veeck A, Yu FG, Yu H, Veeck G, Gentry JW. Influences on food choices of urban Chinese teenagers. Young Consumers. 2014;15(4):296–311. [Google Scholar]
- 38. Kolopaking R, Bardosono S, Fahmida U. Maternal self-efficacy in the home food environment: a qualitative study among low-income mothers of nutritionally at-risk children in an urban area of Jakarta, Indonesia. J Nutr Educ Behav. 2011;43(3):180–8. [DOI] [PubMed] [Google Scholar]
- 39. Snowdon W, Lawrence M, Schultz J, Vivili P, Swinburn B. Evidence-informed process to identify policies that will promote a healthy food environment in the Pacific Islands. Public Health Nutr. 2010;13(6):886–92. [DOI] [PubMed] [Google Scholar]
- 40. Monterrosa EC, Campirano F, Tolentino Mayo L, Frongillo EA, Hernandez Cordero S, Kaufer-Horwitz M, Rivera JA. Stakeholder perspectives on national policy for regulating the school food environment in Mexico. Health Policy Plan. 2015;30(1):28–38. [DOI] [PubMed] [Google Scholar]
- 41. Maxfield A, Patil S, Cunningham SA. Globalization and food prestige among Indian adolescents. Ecol Food Nutr. 2016;55(4):341–64. [DOI] [PubMed] [Google Scholar]
- 42. Pehlke EL, Letona P, Hurley K, Gittelsohn J. Guatemalan school food environment: impact on schoolchildren's risk of both undernutrition and overweight/obesity. Health Promot Int. 2016;31(3):542–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Pehlke EL, Letona P, Ramirez-Zea M, Gittelsohn J. Healthy casetas: a potential strategy to improve the food environment in low-income schools to reduce obesity in children in Guatemala City. Ecol Food Nutr. 2016;55(3):324–38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Smit W, de Lannoy A, Dover RVH, Lambert EV, Levitt N, Watson V. Making unhealthy places: the built environment and non-communicable diseases in Khayelitsha, Cape Town. Health Place. 2016;39:196–203. [DOI] [PubMed] [Google Scholar]
- 45. Fuster M, Messer E, Houser RF, Deman H, de Fulladolsa PP, Bermudez OI. Local notions of healthy eating and national dietary guidelines: a comparison in vulnerable Salvadoran communities. Food Foodways. 2013;21(4):288–314. [Google Scholar]
- 46. Hunter-Adams J. Exploring perceptions of the food environment amongst Congolese, Somalis and Zimbabweans living in Cape Town. Int Migr. 2017;55(4):78–87. [Google Scholar]
- 47. Hunter-Adams J, Rother HA.. Pregnant in a foreign city: a qualitative analysis of diet and nutrition for cross-border migrant women in Cape Town, South Africa. Appetite. 2016;103:403–10. [DOI] [PubMed] [Google Scholar]
- 48. Barr S. Using mixed methods to describe a spatially dynamic food environment in rural Dominican Republic. Hum Ecol. 2017;45(6):845–51. [Google Scholar]
- 49. Bridle-Fitzpatrick S. Food deserts or food swamps? A mixed-methods study of local food environments in a Mexican city. Soc Sci Med. 2015;142:202–13. [DOI] [PubMed] [Google Scholar]
- 50. Chaudhari LS, Begay RC, Schulz LO. Fifteen years of change in the food environment in a rural Mexican community: the Maycoba project. Rural Remote Health. 2013;13(3):2404. [PubMed] [Google Scholar]
- 51. Finzer LE, Ajay VS, Ali MK, Shivashankar R, Goenka S, Sharma P, Pillai DS, Khandelwal S, Tandon N, Reddy KS et al.. Fruit and vegetable purchasing patterns and preferences in South Delhi. Ecol Food Nutr. 2013;52(1):1–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Gupta V, Downs SM, Ghosh-Jerath S, Lock K, Singh A. Unhealthy fat in street and snack foods in low-socioeconomic settings in India: a case study of the food environments of rural villages and an urban slum. J Nutr Educ Behav. 2016;48(4):269–79.e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Peyton S, Moseley W, Battersby J. Implications of supermarket expansion on urban food security in Cape Town, South Africa. Afr Geogr Rev. 2015;34(1):36–54. [Google Scholar]
- 54. Schram A, Labonte R, Baker P, Friel S, Reeves A, Stuckler D. The role of trade and investment liberalization in the sugar-sweetened carbonated beverages market: a natural experiment contrasting Vietnam and the Philippines. Global Health. 2015;11:41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Castro-Sánchez AE, Aparicio-Moreno CE, Ramos-Peña EG. The study of food environments as a strategy of social sustainability in the Mexican Northeast. Int J Sustain Policy Prac. 2014;9(3):57–74. [Google Scholar]
- 56. Duran AC, Roux AVD, Latorre M, Jaime PC. Neighborhood socioeconomic characteristics and differences in the availability of healthy food stores and restaurants in Sao Paulo, Brazil. Health Place. 2013;23:39–47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Ivanova L, Trifonova J, Terziyska I. Study on some factors for healthy nutrition environment in restaurants in southwestern Bulgaria. Tourism and Hospitality Management. 2012;18(2):259–66. [Google Scholar]
- 58. Costa BVD, Oliveira CD, Lopes AC. Food environment of fruits and vegetables in the territory of the Health Academy Program. Cad Saude Publica. 2015;31:159–69. [DOI] [PubMed] [Google Scholar]
- 59. Davies G, Frausin G, Parry L. Are there food deserts in rainforest cities?. Ann Am Assoc Geogr. 2017;107(4):794–811. [Google Scholar]
- 60. Liao CX, Tan YY, Wu CQ, Wang SF, Yu CQ, Cao WH, Gao WJ, Lv J, Li LM. City level of income and urbanization and availability of food stores and food service places in China. PLoS One. 2016;11(3):e0148745. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Cerovečki IG, Grünhagen M.. “Food deserts” in urban districts: evidence from a transitional market and implications for macromarketing. J Macromarketing. 2016;36(3):337–53. [Google Scholar]
- 62. Chacon V, Letona P, Villamor E, Barnoya J. Snack food advertising in stores around public schools in Guatemala. Crit Public Health. 2015;25(3):291–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. Faber M, Laurie S, Maduna M, Magudulela T, Muehlhoff E. Is the school food environment conducive to healthy eating in poorly resourced South African schools?. Public Health Nutr. 2014;17(6):1214–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. Moodley G, Christofides N, Norris SA, Achia T, Hofman KJ. Obesogenic environments: access to and advertising of sugar-sweetened beverages in Soweto, South Africa, 2013. Prev Chronic Dis. 2015;12:140559. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65. Soltero EG, Ortiz Hernandez L, Jauregui E, Levesque L, Taylor JLY, Barquera S, Lee RE. Characterization of the school neighborhood food environment in three Mexican cities. Ecol Food Nutr. 2017;56(2):139–51. [DOI] [PubMed] [Google Scholar]
- 66. Chan Sun M, Lalsing Y, Subratty AH. Primary school food environment in Mauritius. Nutr Food Sci. 2009;39(3):251–9. [Google Scholar]
- 67. Pulz IS, Martins PA, Feldman C, Veiros MB. Are campus food environments healthy? A novel perspective for qualitatively evaluating the nutritional quality of food sold at foodservice facilities at a Brazilian university. Perspect Public Health. 2017;137(2):122–35. [DOI] [PubMed] [Google Scholar]
- 68. Wojcicki JM, Elwan D.. Primary school nutrition and tuck shops in Hhoho, Swaziland. J Child Nutr Manage. [Internet] 2014, 38(1); [Accessed 2019 Feb 13]. Available from: https://schoolnutrition.org/5--News-and-Publications/4--The-Journal-of-Child-Nutrition-and-Management/Spring-2014/Volume-38,-Issue-1,-Spring-2014---Wojcicki,-Elwan/). [Google Scholar]
- 69. Soares ALG, de Franca GVA, Goncalves H. Household food availability in Pelotas, Brazil: an approach to assess the obesogenic environment. Rev Nutr. 2014;27(2):193–203. [Google Scholar]
- 70. Ng SH, Kelly B, Se CH, Chinna K, Sameeha MJ, Krishnasamy S, Ismail MN, Karupaiah T. Obesogenic television food advertising to children in Malaysia: sociocultural variations. Global Health Action. 2015;8(1):1–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71. Gartin M. Food deserts and nutritional risk in Paraguay. Am J Hum Biol. 2012;24(3):296–301. [DOI] [PubMed] [Google Scholar]
- 72. Kelly M, Seubsman SA, Banwell C, Dixon J, Sleigh A. Thailand's food retail transition: supermarket and fresh market effects on diet quality and health. Br Food J. 2014;116(7):1180–93. [Google Scholar]
- 73. Duran AC, De Almeida SL, Latorre MDRD, Jaime PC. The role of the local retail food environment in fruit, vegetable and sugar-sweetened beverage consumption in Brazil. Public Health Nutr. 2016;19(6):1093–102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74. Godin KM, Chacon V, Barnoya J, Leatherdale ST. The school environment and sugar-sweetened beverage consumption among Guatemalan adolescents. Public Health Nutr. 2017;20(16):2980–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75. Fernandes M, Folson G, Aurino E, Gelli A. A free lunch or a walk back home? The school food environment and dietary behaviours among children and adolescents in Ghana. Food Security. 2017;9(5):1073–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76. Vedovato GM, Trude ACB, Kharmats AY, Martins PA. Degree of food processing of household acquisition patterns in a Brazilian urban area is related to food buying preferences and perceived food environment. Appetite. 2015;87:296–302. [DOI] [PubMed] [Google Scholar]
- 77. Zuccolotto DCC, Barbieri P, Sartorelli DS. Food environment and family support in relation to fruit and vegetable intake in pregnant women. Arch Latinoam Nutr. 2015;65(4):216–24. [Google Scholar]
- 78. Anggraini R, Februhartanty J, Bardosono S, Khusun H, Worsley A. Food store choice among urban slum women is associated with consumption of energy-dense food. Asia Pac J Public Health. 2016;28(5):458–68. [DOI] [PubMed] [Google Scholar]
- 79. Mendes LL, Nogueira H, Padez C, Ferrao M, Velasquez-Melendez G. Individual and environmental factors associated for overweight in urban population of Brazil. BMC Public Health. 2013;13:988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80. Patel O, Shahulhameed S, Shivashankar R, Tayyab M, Rahman A, Prabhakaran D, Tandon N, Jaacks LM. Association between full service and fast food restaurant density, dietary intake and overweight/obesity among adults in Delhi, India. BMC Public Health. 2017;18(1):36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81. Velasquez-Melendez G, Mendes LL, Padez CMP. Built environment and social environment: associations with overweight and obesity in a sample of Brazilian adults. Cad Saude Publica. 2013;29(10):1988–96. [DOI] [PubMed] [Google Scholar]
- 82. Zhang XY, van der Lans I, Dagevos H. Impacts of fast food and the food retail environment on overweight and obesity in China: a multilevel latent class cluster approach. Public Health Nutr. 2012;15(1):88–96. [DOI] [PubMed] [Google Scholar]
- 83. Azeredo CM, de Rezende LF, Canella DS, Claro RM, Peres MF, Luiz Odo C, Franca-Junior I, Kinra S, Hawkesworth S, Levy RB. Food environments in schools and in the immediate vicinity are associated with unhealthy food consumption among Brazilian adolescents. Prev Med. 2016;88:73–9. [DOI] [PubMed] [Google Scholar]
- 84. Barrera LH, Rothenberg SJ, Barquera S, Cifuentes E. The toxic food environment around elementary schools and childhood obesity in Mexican cities. Am J Prev Med. 2016;51(2):264–70. [DOI] [PubMed] [Google Scholar]
- 85. Chor D, Cardoso LO, Nobre AA, Griep RH, Fonseca MDM, Giatti L, Bensenor I, Molina MDB, Aquino EML, Diez-Roux A et al.. Association between perceived neighbourhood characteristics, physical activity and diet quality: results of the Brazilian Longitudinal Study of Adult Health (ELSA-Brasil). BMC Public Health. 2016;16:751. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86. Dake FAA, Thompson AL, Ng SW, Agyei-Mensah S, Codjoe SNA. The local food environment and body mass index among the urban poor in Accra, Ghana. J Urban Health. 2016;93(3):438–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87. Jaime PC, Duran AC, Sarti FM, Lock K. Investigating environmental determinants of diet, physical activity, and overweight among adults in Sao Paulo, Brazil. J Urban Health. 2011;88(3):567–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88. Zhou M, Tan SK, Tao YH, Lu YZ, Zhang Z, Zhang L, Yan DP. Neighborhood socioeconomics, food environment and land use determinants of public health: isolating the relative importance for essential policy insights. Land Use Policy. 2017;68:246–53. [Google Scholar]
- 89. Popkin BM. Nutrition transition and the global diabetes epidemic. Curr Diab Rep. 2015;15(9):64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90. Food and Agriculture Organization of the United Nations. The state of food security and nutrition in the world 2018: building climate resilience for food security and nutrition. Rome: FAO; 2018. [Google Scholar]
- 91. Walls HL, Johnston D, Mazalale J, Chirwa EW. Why we are still failing to measure the nutrition transition. BMJ Glob Health. 2018;3(1):e000657. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92. Penney TL, Almiron-Roig E, Shearer C, McIsaac JL, Kirk SFL. Modifying the food environment for childhood obesity prevention: challenges and opportunities. Proc Nutr Soc. 2014;73(2):226–36. [DOI] [PubMed] [Google Scholar]
- 93. Lytle LA. Measuring the food environment: state of the science. Am J Prev Med. 2009;36(4 Suppl):S134–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94. Miller V, Yusuf S, Chow CK, Dehghan M, Corsi DJ, Lock K, Popkin B, Rangarajan S, Khatib R, Lear SA et al.. Availability, affordability, and consumption of fruits and vegetables in 18 countries across income levels: findings from the Prospective Urban Rural Epidemiology (PURE) study. Lancet Glob Health. 2016;4(10):e695–703. [DOI] [PubMed] [Google Scholar]
- 95. Yim A, Humphries D, Abuova G. Food, alcohol and cigarette availability and consumption in Almaty, Kazakstan: results and appraisal of a rapid assessment. Public Health Nutr. 2003;6(8):791–800. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.