ABSTRACT
The double burden of malnutrition (DBM) is characterized by the coexistence of underweight and overweight individuals in a population. The objective of this study was to assess the level of DBM, as well as its main determinants, in women in South and Southeast Asia. We searched scientific literature databases, including PubMed, EMBASE, CINAHL, and Google Scholar; gray literature; and reference lists from primary research published between 1969 and September 30, 2017. In total, 128 studies met our inclusion criteria, representing data of ∼5 million women >15 y of age from South and Southeast Asia. The findings show that prevalence rates of underweight and overweight varied by study from 7.0% to 61.0% and 1.0% to 64.0%, respectively. For the total study period, the pooled prevalence of underweight and overweight was 28% (95% CI: 25%, 31%) and 17% (95% CI: 15%, 19%) in South Asia, respectively, and 20% (95% CI: 15%, 26%) and 20% (95% CI: 15%, 24%) in Southeast Asia, respectively. In both regions, underweight was more prevalent in rural areas, among women of the youngest age group (15–19 y), and among those in the poorest wealth quintile. In contrast, overweight was higher in urban areas, among women of older age, and among those in the wealthiest households. This study also found that prevalence of overweight has recently exceeded that for underweight in this population.
Keywords: underweight, overweight, double burden, Southeast Asia, trends
Introduction
While overweight and obesity have been recognized as major public health problems in most developed countries, until recently, the focus in many low- to middle-income countries (LMICs) has been on undernutrition. However, current evidence points to a double burden of malnutrition in LMICs resulting from the coexistence of underweight and overweight individuals in a given population (1–6). This double burden is thought to have arisen due to the nutritional transition experienced by these countries, along with a rapid change in food production, dietary habits, and physical activity (7).
Both underweight and overweight have multifaceted consequences for individuals in terms of longevity and disability as well as placing an economic burden on societies and health-care systems (8, 9). A continued focus on undernutrition, at the expense of tackling overweight and obesity, or the development of public health approaches to counter just one of them could be damaging.
Recent evidence shows that countries in South Asia, such as India, Bangladesh, and Nepal, are currently suffering such a double burden of malnutrition (10–14). India alone is home to one-third of the global population of malnourished children, while at the same time almost 50% of adults living in urban areas are overweight or obese (15). With other countries in the region experiencing in recent decades rapid nutritional, demographic, and socioeconomic transitions, this burden is set to rise (16–18), resulting in significant impacts on social and economic development. A study in the Asia-Pacific region estimated that the economic burden of underweight ranged from 2.5% to 3.8% of a country's gross domestic product, while overweight accounted for as much as 9.9% of a country's total health-care expenditure (19).
Although in recent times, underweight in women has been one of the most prominent public health issues in South and Southeast Asia, overweight remains a relatively low priority. While it is known that undernutrition in women is associated with adverse pregnancy outcomes, including maternal mortality, delivery complications, preterm birth, and intrauterine growth retardation (20), maternal overweight/obesity is also known to lead to several adverse maternal and fetal complications during pregnancy, delivery, and postpartum (21). This is alarming as studies suggest that both undernutrition and overnutrition are significant public health concerns in this region with women a high-risk population for both (22–26).
Although many studies have reported on country-specific prevalence of underweight and overweight among women in South and South East Asia, none have systematically analyzed data to understand which demographic groups are at greater risk. Understanding the within-country burden of malnutrition, along with associated determinants, is important to inform the development of interventions to meet the Sustainable Development Goals target of improving women's nutrition by 2030. To develop and implement effective policies and interventions to counter this double burden, we must understand the patterning of underweight and overweight within these countries and throughout the region.
In this study, we aimed to systematically review estimates of the double burden of malnutrition among women living in South and Southeast Asia, as well as identifying the major determinants of both conditions in this population.
Methods
We followed the Meta-analyses Of Observational Studies in Epidemiology (MOOSE) guidelines to identify studies reporting estimates on the prevalence of underweight and overweight in women according to BMI, conducted in countries of South Asia (Afganistan, Bangladesh, Bhutan, India, Nepal, and Pakistan) and Southeast Asia (Cambodia, Indonesia, Laos, Malaysia, Maldives, Mayanmar, Philippines, Sri Lanka, Thailand, Timor-leste, and Vietnam). Underweight and overweight in individual studies were defined according to WHO and Asia-specific cutoff points.
Search strategy
We used the PICOS criteria to define the research question (Table 1) (7). Studies eligible for inclusion met the folowing criteria: primary or secondary data, published in the English language, conducted in humans, and studies that provide an estimate of prevalence of underweight and/or overweight for women. Editorial and methodological articles or studies with no reported prevalence of either were excluded. Country-specific national survey reports were also eligible for inclusion.
TABLE 1.
PICOS criteria for inclusion and exclusion of studies
| Parameter | Inclusion criteria | Exclusion criteria |
|---|---|---|
| Population | Women who were age ≥15 y | Males |
| Intervention/exposure | Collection of data on weight and sociodemographic factors | Lack of data on weight and/or sociodemographic factors |
| Comparator | Nutritional status of women | Lack of data on nutritional status |
| Outcome | Prevalence of nutritional status | No reported prevalence measure |
| Study design | Observational study | Editorial |
| Cross-sectional study | Methodological article | |
| Cohort study |
Our search included studies published from January 1, 1969, to December 31, 2017. We used a number of different search engines: PubMed, EMBASE, CINAHL, Google Scholar, and Google. We also searched the gray literature in the Demography and Health Survey (DHS) database, WHO regional databases, and Global Burden of Diseases database. The keywords used in the search were women, female, mother, underweight, chronic energy deficiency, overweight, obesity, body mass index, BMI, South Asia, South East Asia, and the names of each of the individual countries.
Data extraction and quality assessment
Data extraction was carried out by 2 independent reviewers following a piloted version of the Cochrane Effective Practice and Organization of Care Group guidelines (27). They completed a standard data extraction form, summarizing the study design and other relevant data for each article, including country name, sample size, survey year, and geographic location (Supplemental Table 1). Where articles did not report survey year, publication year was listed. The main outcomes were prevalence of underweight, overweight/obese, and mean BMI score.
We adapted the modified Newcastle Ottawa Scale for assessing the quality of the study, as recommended by the Cochrane Collaboration (28). Four criteria were used to score studies as high quality (4 points), moderate quality (2–3 points), and poor quality (0–1 points). Criteria included target population a close representation of the national population (yes = 1, no = 0), sufficient sample size (yes = 1, no = 0), random sampling (yes = 1, no = 0), and ascertainment of BMI measure (yes = 1, no = 0). The cutoff for a sufficient sample size was set at 500 participants (29) (Supplemental Table 2).
Data analysis
All meta-analyses were performed using MetaXL version 1.4 (EpiGear International Pty Ltd). We calculated pooled prevalence of underweight and overweight for 4-y intervals: 2000 and earlier, 2001–2005, 2006–2010, and 2011–2017 for South Asia and Southeast Asia separately. In addition, using nationally representative survey data, we assessed pooled prevalence of underweight and overweight by age, education, place of residence (urban/rural), and wealth index for separate countries. Analyses for these factors used country-specific DHS data only, as these are sampled to be representative of the national population.
Results
Study characteristics and quality
Our literature search yielded 32,149 records. After exclusion of duplicates and review of titles and abstracts, 912 articles were included for further evaluation; of these, full texts could not be found for 481 articles. The full text of the remaining 431 articles was examined and a total of 303 articles were excluded after abstract screening. We included 128 articles (6, 14, 15, 17, 30–152) in the final synthesis (Figure 1). These articles covered 18 countries from South Asia and Southeast Asia, presenting data for 4,974,717 individuals. Of these 128 articles, 52 reported prevalence of both underweight and overweight among women, 60 studies reported prevalence of just 1 condition, and 16 articles reported mean BMI only. Ninety-two percent of studies were community based and 8% institute based (Supplemental Table 1). Most studies were cross-sectional in nature, with 3 cohort studies. In total, 112 articles were included in the meta-analysis (Figure 1). Seventy-one of the 112 (64%) studies included in the meta-analysis were graded as high quality, with 6 (5%) graded as low quality (Supplemental Table 2).
FIGURE 1.
Flow diagram showing data extraction process of the study.
Estimation of prevalence rates
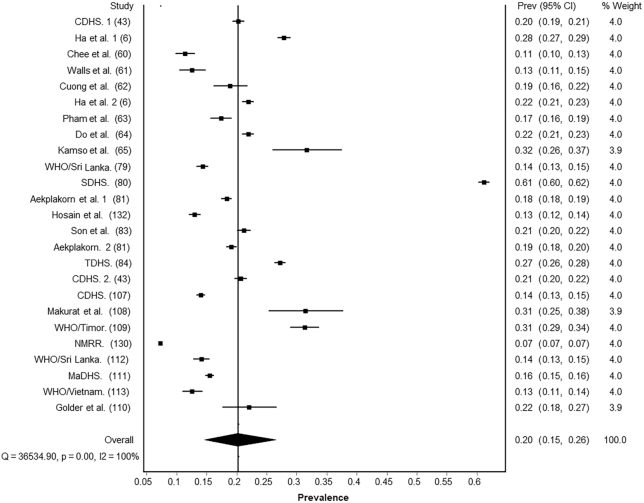
Prevalence rates varied widely across studies, from 7.0% to 61.0% for underweight and 1.0% to 64.0% for overweight. The pooled prevalence of underweight and overweight in South Asia for all studies was 28% (95% CI: 25%, 31%) and 17% (95% CI: 15%, 19%) respectively (Figures 2 and 3). In Southeast Asia, pooled prevalence was 20% (95% CI: 15%, 26%) for underweight and 20% (95% CI: 15%, 24%) for overweight (Figures 4 and 5).
FIGURE 2.
Pooled prevalence of underweight among women in South Asia.
FIGURE 3.

Pooled prevalence of overweight among women in South Asia.
FIGURE 4.
Pooled prevalence of underweight among women in Southeast Asia.
FIGURE 5.
Pooled prevalence of overweight among women in Southeast Asia.
Prevalence rates by year of study
To investigate underweight and overweight prevalence over time, we arranged outcomes by time of study in 4 aggregated intervals: 1) 2000 and earlier, 2) 2001–2005, 3) 2006–2010, and 4) 2011–2017.
2000 and earlier
We included 22 studies from South Asia from 2000 and earlier in our analysis, with 12 of these studies presenting findings for underweight (30–41) and 10 for overweight (30, 31, 33–39, 42). The pooled estimate of underweight was 43% (95% CI: 37%, 48%), whereas for overweight it was 9% (95% CI: 5%, 12%) (Supplemental Figures 1–16). Of the 12 studies presenting underweight prevalence, 8 studies came from India, 3 from Bangladesh, and 1 from Nepal. Of the 10 studies presenting overweight prevalence, 8 were from India and 2 from Bangladesh.
We identified 2 studies (6, 43) reporting underweight from 2000 and earlier in Southeast Asia, resulting in a pooled estimate of 24% (95% CI: 17%, 32%). Five studies (6, 43–45) reported overweight prevalence in the region, with a pooled estimate of 4% (95% CI: 1%, 8%). These five studies came from 3 countries, with Vietnam providing 55.5% of the sample population for meta-analysis, Indonesia 32%, and Cambodia 17.5%.
2001–2005
Ten studies from between 2001 and 2005 presented both prevalence of underweight and overweight in South Asia, and 3 studies presented prevalence of underweight only and 3 overweight only. Pooled estimates were 24% (95% CI: 21%, 28%) for underweight and 14% (95% CI: 11%, 16%) for overweight. Of the 13 studies (14, 46–57) that presented underweight prevalence, 6 came from Bangladesh, 5 from Nepal, and 2 from India. Of the 13 studies (14, 42, 47, 48, 50–52, 54–59) that presented overweight prevalence, 6 came from Bangladesh, 5 from Nepal, and 2 from India (Supplemental Figures 1–16).
Seven studies presented prevalence on underweight (6, 60–65) for Southeast Asia over the same period and 12 on overweight (6, 44, 59–68). Pooled estimates were 19% (95% CI: 16%, 22%) and 25% (95% CI: 13%, 39%) for underweight and overweight, respectively. Studies from Vietnam provided 92.3% of the sample population for underweight meta-analysis and Indonesia 75% of the sample for overweight.
2006–2010
We identified 8 studies from South Asia that presented findings for underweight between 2006 and 2010 (69–76). These resulted in a pooled estimate of 24% (95% CI: 17%, 32%). The studies came from 4 countries, with India providing 86% of the sample population. We identified 10 studies for the same period in this region that presented findings for overweight (15, 69, 70, 72–78), resulting in a pooled estimate of 19% (95% CI: 14%, 24%). Of these 10 studies, 4 came from India, 4 from Bangladesh, and 1 each from Nepal and Bhutan (Supplemental Figures 1–16).
Over the same time period, we identified 8 studies (43, 79–84) for underweight and 9 studies (17, 43, 79–84) for overweight in Southeast Asia. Polled estimates of underweight and overweight were 23% (95% CI: 13%, 35%) and 25% (95% CI: 11%, 42%), respectively.
2011–2017
For the most recent interval, we identified 17 studies (34, 85–99, 141) for underweight in South Asia with a pooled estimate of 22% (95% CI: 17%, 27%). These studies came from 5 countries, with Bangladesh providing 35.7%, India 25.1%, Nepal 23.1%, Afghanistan 11.4%, and Pakistan 4.5% of the sample population. We also identified 23 studies (34, 85–88, 90–97, 99–106, 136, 141) for overweight in the region with a pooled estimate of 23% (95% CI: 19%, 28%). Of these 23 studies, 7 were from Bangladesh (sample n = 36,204), 6 from India (n = 27,631), 5 from Nepal (n = 22,789), 3 from Pakistan (n = 8592), and 1 each from Bhutan (n = 1748) and Afghanistan (n = 11,124).
Eight studies were identified for a pooled estimate of underweight 17% (95% CI: 12%, 23%) in Southeast Asia (107–113, 143). These studies came from 7 countries: Cambodia, Timor, Malaysia, Sri Lanka, Myanmar, Vietnam, and Maldives. We also identified 11 studies (82, 107–109, 111–115) for overweight, with a pooled estimate of 18% (95% CI: 10%, 27%). These studies came from 9 countries, with Malaysia alone providing 89.8% of the sample for meta-analysis (Supplemental Figures 1–16).
Age-specific prevalence
We identified 9 nationally representative DHS studies in South Asia (47, 49, 70, 71, 91, 99, 101, 106, 122) and 6 for Southeast Asia (42, 80, 81, 86, 114, 116) for use in age-specific prevalence analysis.
Of these 9 studies in South Asia, 3 were conducted between 2001 and 2005, 2 from 2006 to 2010, and 4 from 2011 to 2017. These studies came from Bangladesh (n = 4), Nepal (n = 3), India (n = 1), and Pakistan (n = 1). Age-stratified pooled prevalence (PP) of overweight in South Asia in the older age groups (40–49 y) was almost 6 times higher than in younger ones (15–19 y) (3.5% compared with 18.1%). For underweight, there was little difference by age group (PP 15–19 y = 30%; PP 40–49 y = 29.1%) (Figure 2). Of the 6 studies for Southeast Asia, 1 was conducted during 2000 or earlier, 1 between 2001 and 2005, 2 from 2006 to 2010, and 2 from 2011 to 2017. Age-specific pooled prevalence of overweight was 10 times higher in the older age groups than the younger ones (15–19 y = 5.5%; 40–49 y = 56.7%), and underweight was higher in the younger age groups (PP 15–19 y = 28.1%; PP 40–49 y = 18.5%) (Figure 6).
FIGURE 6.
Age-specific prevalence of underweight among women in selected countries of South Asia (A) and Southeast Asia (B).
Urban-rural differences
In South Asia, pooled estimates for underweight, from the 12 nationally representative studies that included measures or urbanicity (34–36, 47, 49, 70, 71, 91, 99, 101, 106, 122), were 16.4% (95% CI: 12%, 25%) for urban areas and 26.7% (95% CI: 22%, 30%) for rural areas (Figure 4). Of these 12 studies, 3 were conducted during 2000 or earlier, 3 between 2001 and 2005, 2 from 2006 to 2010, 4 between 2011 and 2017. Pooled estimates from the 9 studies reporting overweight found overweight prevalence was more than twice as high in urban (24.1%; 95% CI: 19%, 27%) compared with rural areas (10.1%; 95% CI: 7%, 19%).
In Southeast Asia, pooled estimates by urban and rural classifications came from 7 studies (80, 81, 86, 114, 116, 123, 124), with 1 between 2001 and 2005, 2 from 2006 to 2010, and 2 from 2011 to 2017. The pooled prevalence of underweight was higher in rural areas (18.1%; 95% CI: 16%, 22%) than in urban areas (14.1%; 95% CI: 11%, 17%) in Southeast Asia, with overweight higher in urban areas (20.1%; 95% CI: 17%, 25%) than in rural areas (14.6%; 95% CI: 12%, 19%) (Figure 7).
FIGURE 7.
Urban- and rural-specific prevalence of overweight among women in selected countries of South Asia (A) and Southeast Asia (B).
Education and double burden of malnutrition
We identified 10 nationally representative studies that included measures of educational level from South Asia (35, 36, 49, 70, 71, 91, 99, 101, 106, 122) and 7 from Southeast Asia (80, 81, 86, 114, 116, 123, 124). The pooled prevalence of underweight was almost 2 times higher for South Asians with no education (35.2%; 95% CI: 25%, 39%) compared with those who had secondary and higher education (20.8%; 95% CI: 15%, 28%). For overweight, a higher pooled prevalence was found in those who had secondary and higher education (19.2%; 95% CI: 15%, 26%) than those with no education (9.7%; 95% CI: 7%, 17%).
In Southeast Asia, a similar pooled prevalence of underweight was found in those with no education (17.9%; 95% CI: 11%, 29%) and those who had secondary and higher education (17.4%; 95% CI: 19%, 28%). A higher prevalence of overweight was observed among those who had secondary and higher education compared with those with no education in Southeast Asia (Figure 8).
FIGURE 8.
Prevalence of underweight and overweight among women in South Asia (A) and Southeast Asia (B) by educational status.
Socioeconomic differences
Eight nationally representative studies from South Asia (47, 49, 70, 71, 91, 99, 101, 122) and 6 studies from Southeast Asia (81, 86, 114, 116, 123, 124) included prevalence of underweight and/or overweight according to socioeconomic status (SES). Of these 8 studies from South Asia, 2 were conducted between 2001 and 2005, 2 from 2006 to 2010, and 4 from 2011 to 2017. Of the 6 studies from Southeast Asia, 1 was conducted between 2001 and 2005, 1 from 2006 to 2010, and 4 from 2011 to 2017. Pooled prevalence of underweight in South Asia was more than 3 times higher in the poorest households (36.0%; 95% CI: 29%, 42%) than the richest households (11.7%; 95% CI: 8%, 21%). Those living in poorer households in Southeast Asia also had a higher pooled prevalence of overweight (17.3%; 95% CI: 15%, 25%) than those living in richer households (9.7%; 95% CI: 7%, 11%). Pooled prevalence of overweight was 6 times higher among the richest households (27.0%; 95% CI: 25%, 30%) than the poorest households (4.5%; 95% CI: 3%, 9%) in South Asia and 2 times higher in Southeast Asia (20.3%; 95% CI: 27%, 26% compared with 10.9%; 95% CI: 8%, 13%) (Figure 9).
FIGURE 9.
Prevalence of underweight and overweight among women in South Asia (A) and Southeast Asia (B) by wealth index.
Discussion
To our knowledge, this is the first systematic evaluation of the scientific literature on the double burden of underweight and overweight among women in South and Southeast Asia. In this study, we followed a systematic and comprehensive approach to identify studies on both underweight and overweight following MOOSE guidelines and a registered protocol (CRD42017079694). Within the study, we also investigated associations in prevalence with important determinants, including age, urbanicity, and SES. The pooled analysis from this study found that the prevalence of overweight has increased dramatically in both regions since before 2000. Despite the observed decreases in the prevalence of underweight over the same period, current prevalence of underweight in both regions remains worryingly high. However, findings from this study suggest that the prevalence of overweight among women in these regions now exceeds underweight, with this shift occurring in 2011–2017 (i.e., the most recent time period examined). We also found that while overweight was associated with older age groups, underweight is more prevalent among younger women. Those living in urban areas were more likely to be overweight, while those from rural areas had a greater risk of underweight. Lower SES was also associated with a greater prevalence of underweight and a lower prevalence of overweight.
In agreement with previous studies (107, 110, 116, 117), the present study demonstrates a higher prevalence of overweight or obesity in older women. Some have suggested that this finding can partially be explained by weight gain during pregnancy, with women often unable to get back to their prepregnancy weight (118). Studies have also reported that women living in urban areas, or those from wealthier households, are at a lower risk of underweight but at a greater risk of becoming overweight (119, 120). These reports are supported by the present study, with work also suggesting that urbanization is associated with a more sedentary lifestyle, resulting from decreased use of active transport and less physical active supporting environments (121–123). The associations of underweight and overweight with socioeconomic factors also agree with earlier work (119, 120), including a study using DHS data from 36 countries that demonstrated that wealth is a key determinant of overweight in LMICs (125). The findings presented here agree with other studies that older women (117, 127), those of a higher SES (128), and those living in urban areas (12, 14, 125, 126) are more likely to be obese. Similarly, younger women of lower SES and those living in rural areas are more likely to be underweight (119, 120, 124).
Our finding that, over time, there has been some decrease in underweight in these regions, along with corresponding increases in overweight, may have occurred due to substantial socioeconomic development within these countries. A recent study using DHS in 36 LMICs reported similar findings (131), with a number of others linking economic development to increases in the intake of processed food (126); the consumption of energy-dense foods, including fats and high-calorie drinks; and concurrent reductions in physical activity (132). Despite these decreases, this study also found that underweight remains a significant problem in South and Southeast Asia, with inequalities in both conditions between population subgroups.
Although policy makers and national development agencies working in these regions must recognize that overweight is now an increasing trend, the persistence of underweight means that policies and public health approaches must be developed and implemented that consider the double duty of underweight and overweight together. The determinants of these conditions should be explored further such that interventions could be targeted that consider the distribution of these conditions within countries. In addition, heterogeneity between studies, including a scarcity of data from rural regions, should encourage countries to develop extensive national surveillance programs using measured BMI and consistent underweight and overweight reference standards.
While in this study we assessed risk of publication bias using well-established criteria, the results presented need to be interpreted in light of some limitations. First, although most of the studies included in this review were graded as moderate to high quality, many were cross-sectional in nature and followed a survey-based approach. In addition, findings of this study were extremely heterogeneous in nature, not only in study design and data collection but also in outcome. As with all systematic reviews, there is the potential for publication bias in the identified studies, with some not initially designed to report on the prevalence of underweight and overweight. The reference standards for determining underweight and overweight were not consistent between all studies. In addition, although we attempted to estimate prevalence by determinants such as age, urbanicity, and SES, not all studies presented prevalence stratified by these factors. Moreover, information on certain groups, such as ethnicity, was not available in enough studies to be included in subgroup analysis.
Conclusions
We found a decline in the prevalence of underweight and an increase in the prevalence of overweight among women in South Asia and Southeast Asia over the study period. We also identified a number of determinants of both conditions that included age, urbanicity, education, and wealth. Future research should investigate within-country driving forces behind the increasing rates of overweight and explain the inequalities in both conditions. Policy approaches should be developed to counter the double burden of malnutrition, with integrated interventions to combat both overweight and undernutrition.
Supplementary Material
Acknowledgments
The authors’ responsibilities were as follows—TB and AM: developed the study concept and undertook reviews of published studies; RJSM and NT: contributed to study design; TB: wrote the first draft; RJSM, NT, SKD, AM: critically reviewed the drafts; and all authors: participated in the data analysis and discussion, and read and approved the final manuscript.
Notes
There were no external funding sources for this study.
Author disclosures: The authors report no conflicts of interest.
Supplemental Tables 1 and 2 and Supplemental Figures 1–16 are available from the “Supplementary data” link in the online posting of the article and from the same link in the online table of contents at https://academic.oup.com/advances/.
Abbreviations used: DBM, double burden of malnutrition; DHS, Demography and Health Survey; LMIC, low- to middle-income country; MOOSE, Meta-analyses Of Observational Studies in Epidemiology; PP, pooled prevalence; SES, socioeconomic status.
References
- 1. Popkin BM, Adair LS, Ng SW. Global nutrition transition and the pandemic of obesity in developing countries. Nutr Rev. 2012;70:3–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Kapoor S, Anand K. Nutritional transition: a public health challenge in developing countries. J Epidemiol Community Health. 2002;56:804–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Popkin BM. The nutrition transition in low‐income countries: an emerging crisis. Nutr Rev. 1994;52:285–98. [DOI] [PubMed] [Google Scholar]
- 4. Ke-You G, Da-Wei F. The magnitude and trends of under- and over-nutrition in Asian countries. Biomed Environ Sci. 2001;14:53–60. [PubMed] [Google Scholar]
- 5. Corsi DJ, Finlay JE, Subramanian S. Global burden of double malnutrition: has anyone seen it?. PLoS One. 2011;6:e25120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Ha DT, Feskens EJ, Deurenberg P, Mai LB, Khan NC, Kok FJ. Nationwide shifts in the double burden of overweight and underweight in Vietnamese adults in 2000 and 2005: two national nutrition surveys. BMC Public Health. 2011;11:62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Hoque ME, Long KZ, Niessen LW, Mamun AA. Rapid shift toward overweight from double burden of underweight and overweight among Bangladeshi women: a systematic review and pooled analysis. Nutr Rev. 2015;73:438–47. [DOI] [PubMed] [Google Scholar]
- 8. Black RE, Victora CG, Walker SP, Bhutta ZA, Christian P, de Onis M, Ezzati M, Grantham-McGregor S, Katz J, Martorell R et al.. Maternal and child undernutrition and overweight in low-income and middle-income countries. Lancet. 2013;382:427–51. [DOI] [PubMed] [Google Scholar]
- 9. Bloom DE, Cafiero E, Jané-Llopis E, Abrahams-Gessel S, Bloom LR, Fathima S, Feigl AB, Gaziano T, Hamandi A, Pandya A et al.. The Global Economic Burden of Noncommunicable Diseases. [Internet] Cambridge (MA): Program on the Global Demography of Aging at Harvard University; 2012; Jan [cited 2019 Jan 28]. Available from: https://ideas.repec.org/p/gdm/wpaper/8712.html. [Google Scholar]
- 10. Shukla H, Gupta P, Mehta H, Hébert JR. Descriptive epidemiology of body mass index of an urban adult population in western India. J Epidemiol Community Health. 2002;56:876–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Popkin BM. Nutrition in transition: the changing global nutrition challenge. Asia Pac J Clin Nutr. 2001; 10:(Suppl):S13–8. [PubMed] [Google Scholar]
- 12. Subramanian SV, Perkins JM, Khan KT. Do burdens of underweight and overweight coexist among lower socioeconomic groups in India?. Asia Pac J Clin Nutr. 2009;90:369–76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Balarajan Y, Villamor E. Nationally representative surveys show recent increases in the prevalence of overweight and obesity among women of reproductive age in Bangladesh, Nepal, and India. J Nutr. 2009;139:2139–44. [DOI] [PubMed] [Google Scholar]
- 14. Shafique S, Akhter N, Stallkamp G, de Pee S, Panagides D, Bloem MW.. Trends of under- and overweight among rural and urban poor women indicate the double burden of malnutrition in Bangladesh. Int J Epidemiol. 2007;36:449–57. [DOI] [PubMed] [Google Scholar]
- 15. Gupta R, Sharma KK, Gupta A, Agrawal A, Mohan I, Gupta VP, Khedar RS, Guptha S. Persistent high prevalence of cardiovascular risk factors in the urban middle class in India: Jaipur Heart Watch-5. J Assoc Physicians India. 2012;60:11–16. [PubMed] [Google Scholar]
- 16. Khan SH, Talukder SH.. Nutrition transition in Bangladesh: is the country ready for this double burden. Obes Rev. 2013;14:126–33. [DOI] [PubMed] [Google Scholar]
- 17. Jayawardena R, Byrne NM, Soares MJ, Katulanda P, Hills AP. The obesity epidemic in Sri Lanka revisited. Asia Pac J Public Health. 2015;27:NP1298–9. [DOI] [PubMed] [Google Scholar]
- 18. Wu Y. Overweight and obesity in China: the once lean giant has a weight problem that is increasing rapidly. BMJ. 2006;333:362–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Hoque ME, Mannan M, Long KZ, Mamun AA. Economic burden of underweight and overweight among adults in the Asia‐Pacific region: a systematic review. Trop Med Int Health. 2016;21:458–69. [DOI] [PubMed] [Google Scholar]
- 20. NCD Risk Factor Collaboration (NCD-RisC). Worldwide trends in body-mass index, underweight, overweight, and obesity from 1975 to 2016: a pooled analysis of 2416 population-based measurement studies in 128·9 million children, adolescents, and adults. Lancet. 2017;390:2627–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Van Lieshout R, Taylor V, Boyle M. Pre‐pregnancy and pregnancy obesity and neurodevelopmental outcomes in offspring: a systematic review. Obes Rev. 2011;12:e548–59. [DOI] [PubMed] [Google Scholar]
- 22. Popkin BM. The nutrition transition: an overview of world patterns of change. Nutr Rev. 2004;62:S140–3. [DOI] [PubMed] [Google Scholar]
- 23. Kennedy G, Nantel G, Shetty P. The Double Burden of Malnutrition: Case Studies from Six Developing Countries. [Internet] Rome (Italy): Nutrition Planning, Assessment and Evaluation Service, Food and Agriculture Organization of the United Nations; 2006; [cited 2018 Mar 8]. Available from: http://www.fao.org/docrep/009/a0442e/a0442e00.htm. [Google Scholar]
- 24. Monteiro CA, Conde WL, Popkin BM. Is obesity replacing or adding to undernutrition? Evidence from different social classes in Brazil. Public Health Nutr. 2002;5:105–12. [DOI] [PubMed] [Google Scholar]
- 25. Monteiro CA, Moura EC, Conde WL, Popkin BM. Socioeconomic status and obesity in adult populations of developing countries: a review. Bull World Health Organ. 2004;82:940–6. [PMC free article] [PubMed] [Google Scholar]
- 26. Popkin BM. The nutrition transition and obesity in the developing world. J Nutr. 2001;131:871S–3S. [DOI] [PubMed] [Google Scholar]
- 27. Cochrane Effective Practice and Organisation of Care Group. Data Collection Checklist. [Internet] London (UK): Cochrane; 2015; [cited 2018 Mar 31]. Available from: http://epoc.cochrane.org/sites/ epoc.cochrane.org/fi les/uploads/datacollectionchecklist.pdf. [Google Scholar]
- 28. Higgins JPT, Deeks JJ, Altman DG. Special topics in statistics. In: Higgins JPT, Green S, eds. Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 (updated March 2011). [Internet] West Sussex, England: The Cochrane Collaboration; 2011. Available from: www.handbook.cochrane.org. [Google Scholar]
- 29. Saquib N, Saquib J, Ahmed T, Khanam MA, Cullen MR. Cardiovascular diseases and type 2 diabetes in Bangladesh: a systematic review and meta-analysis of studies between 1995 and 2010. BMC Public Health. 2012;12:434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. National Institute of Population Research and Training (NIPORT). Bangladesh Demographic and Health Survey 1996–1997. [Internet] Dhaka (Bangladesh): National Institute of Population Research and Training (NIPORT); 1997; [cited 2018 Mar 31]. Available from: https://dhsprogram.com/publications/publication-fr88-dhs-final-reports.cfm. [Google Scholar]
- 31. National Institute of Population Research and Training (NIPORT). Bangladesh Demographic and Health Survey 1999–2000. [Internet] Dhaka (Bangladesh): National Institute of Population Research and Training (NIPORT); 2001; [cited 2018 Mar 31]. Available from: https://dhsprogram.com/publications/publication-fr119-dhs-final-reports.cfm. [Google Scholar]
- 32. Ahmed F, Mahmuda I, Sattar A, Akhtaruzzaman M. Anaemia and vitamin A deficiency in poor urban pregnant women of Bangladesh. Asia Pac J Clin Nutr. 2003;12:460–6. [PubMed] [Google Scholar]
- 33. Samuel PAB, Raghupathy P, Richard J, Fall CH. Socio-economic status and cardiovascular risk factors in rural and urban areas of Vellore, Tamilnadu, South India. Int J Epidemiol. 2012;41:1315–27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Meshram II, Balakrishna N, Sreeramakrishna K, Rao KM, Kumar RH, Arlappa N, Manohar G, Reddy ChG, Ravindranath M, Kumar SS et al.. Trends in nutritional status and nutrient intakes and correlates of overweight/obesity among rural adult women (≥18–60 years) in India: National Nutrition Monitoring Bureau (NNMB) national surveys. Public Health Nutr. 2016;19:767–76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. National Nutrition Monitoring Bureau, National Institute of Nutrition, Indian Council of Medical Research. Nutritional Status of Rural Population (1991–1992). [Internet] Hyderabad (India): National Nutrition Monitoring Bureau, National Institute of Nutrition, Indian Council of Medical Research; 1993; [cited 2018 Mar 31]. Available from: http://nnmbindia.org/NNMB-PDF%20FILES/Report_for_the_year91-1992.pdf. [Google Scholar]
- 36. National Nutrition Monitoring Bureau, National Institute of Nutrition, Indian Council of Medical Research. Nutritional Status of Rural Population (1994–1995). [Internet] Hyderabad (India): National Nutrition Monitoring Bureau, National Institute of Nutrition, Indian Council of Medical Research; 1996; [cited 2018 Mar 31]. Available from: http://nnmbindia.org/NNMB-PDF%20FILES/Report_Of_The_NNBB_NCAER94-95.pdf. [Google Scholar]
- 37. National Nutrition Monitoring Bureau, National Institute of Nutrition, Indian Council of Medical Research. Nutritional Status of Rural Population (1996–1997). [Internet] Hyderabad (India): National Nutrition Monitoring Bureau, National Institute of Nutrition, Indian Council of Medical Research; 1998; [cited 2018 Mar 31]. Available from: http://nnmbindia.org/NNMB-PDF%20FILES/Report_OF_2nd%20Repeat_Survey-96-97.pdf. [Google Scholar]
- 38. National Nutrition Monitoring Bureau, National Institute of Nutrition, Indian Council of Medical Research. Nutritional Status of Rural Population (1998–1999). [Internet] Hyderabad (India): National Nutrition Monitoring Bureau, National Institute of Nutrition, Indian Council of Medical Research; 2000; [cited 2018 Mar 31]. Available from: http://nnmbindia.org/NNMB-PDF%20FILES/Report-%20for%20the%20year%201998-99.pdf. [Google Scholar]
- 39. International Institute for Population Sciences. Mumbai, India: National Family Health Survey India (1992–1993). [Internet] International Institute for Population Sciences; 2017; [cited 2018 Mar 31]. Available from: https://dhsprogram.com/pubs/pdf/FRIND1/FRIND1.pdf. [Google Scholar]
- 40. Rao KM, Balakrishna N, Laxmaiah A, Venkaiah K, Brahmam GN. Diet and nutritional status of adolescent tribal population in nine states of India. Asia Pac J Clin Nutr. 2006; 15:64–71. [PubMed] [Google Scholar]
- 41. Family Health Division, Department of Health Services Ministry of Health. Family Health Survey Nepal 1996. [Internet] Kathmandu (Nepal): Family Health Division, Department of Health Services Ministry of Health; 1997; [cited 2018 Mar 31]. Available from: https://dhsprogram.com/publications/publication-fr78-dhs-final-reports.cfm. [Google Scholar]
- 42. Misra A, Pandey RM, Rama Devi J, Sharma R, Vikram NK, Khanna N. High prevalence of diabetes, obesity and dyslipidaemia in urban slum population in northern India. Int J Obes Relat Metab Disord. 2001;25(11):1722. [DOI] [PubMed] [Google Scholar]
- 43. Ministry of Health and Ministry of Planning. Cambodia Demographic and Health Survey 2000. [Internet] Phnom Penh (Cambodia): Ministry of Health and Ministry of Planning; 2001; [cited 2018 Mar 31]. Available from: https://dhsprogram.com/pubs/pdf/FR124/FR124.pdf. [Google Scholar]
- 44. Nguyen MD, Beresford SA, Drewnowski A. Trends in overweight by socio-economic status in Vietnam: 1992 to 2002. Public Health Nutr. 2007;10:115–21. [DOI] [PubMed] [Google Scholar]
- 45. Ministry of Health Malaysia. National Health and Morbidity Survey 1996 [Internet]. Kualalampur (Malaysia): Ministry of Health Malaysia [cited 2018 Mar 31]. Available from: https://www.nmrr.gov.my/ fwbPage.jsp?fwbPageId = NMRR_UserInstruction. [Google Scholar]
- 46. Chandyo RK, Ulak M, Sommerfelt H, Schneede J, Ueland PM, Strand TA. Nutritional intake and status of cobalamin and folate among non-pregnant women of reproductive age in Bhaktapur, Nepal. Nutrients. 2016;8(6):375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. National Nutrition Monitoring Bureau, National Institute of Nutrition, Indian Council of Medical Research. Nutritional Status of Rural Population (2001–2010) [Internet]. Hyderabad (India): National Nutrition Monitoring Bureau, National Institute of Nutrition, Indian Council of Medical Research; 2011; [cited 2018 Mar 31]. Available from: http://nnmbindia.org/NNMB-PDF%20FILES/Report_Of_The_NNBB_NCAER94-95.pdf. [Google Scholar]
- 48. Family Health Division, Department of Health Services, Ministry of Health. Nepal Demographic and Health Survey 2001 [Internet]. Kathmandu (Nepal): Family Health Division; 2002. Available from: https://dhsprogram.com/pubs/pdf/fr132/fr132.pdf. [Google Scholar]
- 49. Lindstrom E, Hossain MB, Lonnerdal B, Raqib R, El Arifeen S, Ekstrom EC. Prevalence of anemia and micronutrient deficiencies in early pregnancy in rural Bangladesh, the MINIMat trial. Acta Obstet Gynecol Scand. 2011;90:47–56. [DOI] [PubMed] [Google Scholar]
- 50. World Health Organization. Behavioural risk factors of non-communicable diseases in Bangladesh [Internet]. Dhaka (Bangladesh): World Health Organization [cited 2018 Mar 31]. Available from: http://www.who.int/ncds/ surveillance/steps/BangladeshSTEPSReport. pdf. [Google Scholar]
- 51. Ministry of Health and Population Nutrition. Nepal non communicable diseases risk factors: STEPS Survey Nepal 2003 [Internet]. Kathmandu (Nepal): Ministry of Health and Population Nutrition; 2004; [cited 2018 Mar 31]. Available from: https://www.who.int/ncds/surveillance/steps/NepalSTEPSReport2003Kathmandu.pdf. [Google Scholar]
- 52. Ministry of Health and Population Nutrition. Nepal non communicable diseases risk factors: STEPS Survey Nepal 2005 [Internet]. Kathmandu (Nepal): Ministry of Health and Population Nutrition; 2006; [cited 2018 Mar 31]. Available from: https://www.who.int/ncds/surveillance/steps/NepalSTEPSReport2005_3districts.pdf. [Google Scholar]
- 53. Alam N, Roy S, Ahmed T, Ahmed AM. Nutritional status, dietary intake, and relevant knowledge of adolescent girls in rural Bangladesh. J Health Popul Nutr. 2010;28:86–94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. National Institute of Population Research and Training (NIPORT). Bangladesh Demographic and Health Survey 2004 [Internet]. Dhaka (Bangladesh): National Institute of Population Research and Training (NIPORT); 2006; [cited 2018 Mar 31]. Available from: https://dhsprogram.com/publications/publication-fr165-dhs-final-reports.cfm. [Google Scholar]
- 55. National Nutrition Monitoring Bureau, National Institute of Nutrition, Indian Council of Medical Research. Nutritional Status of Rural Population (2004–05) [Internet]. Hyderabad (India): National Nutrition Monitoring Bureau, National Institute of Nutrition, Indian Council of Medical Research; 2006; [cited 2018 Mar 31]. Available from: http://nnmbindia.org/NNMB-PDF%20FILES/Report_Of_The_NNBB_NCAER94-95.pdf. [Google Scholar]
- 56. Bangladesh Bureau of Statistics and UNICEF. Child and mother nutrition survey of Bangladesh 2005 [Internet]. Dhaka (Bangladesh): UNICEF; 2007; [cited 2018 Mar 31]. Available from: http://www.unicef.org/bangladesh/Child_and_Mother_Nutriti on_Survey.pdf. [Google Scholar]
- 57. Ministry of Health and Population Nutrition. Nepal non communicable diseases risk factors: STEPS Survey Nepal 2007 [Internet]. Kathmandu (Nepal): Ministry of Health and Population Nutrition; 2008; [cited 2018 Mar 31]. Available from: https://www.who.int/ncds/surveillance/steps/Nepal_2007_STEPS_Report.pdf. [Google Scholar]
- 58. Fall CH, Sachdev HS, Osmond C, Lakshmy R, Biswas SD, Prabhakaran D, Tandon N, Ramji S, Reddy KS, Barker DJ et al.. Adult metabolic syndrome and impaired glucose tolerance are associated with different patterns of BMI gain during infancy: Data from the New Delhi Birth Cohort. Diabetes Care. 2008;31:2349–56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Oddo VM, Rah JH, Semba RD, Sun K, Akhter N, Sari M, de Pee S, Moench-Pfanner R, Bloem M, Kraemer K. Predictors of maternal and child double burden of malnutrition in rural Indonesia and Bangladesh. Am J Clin Nutr. 2012;95:951–8. [DOI] [PubMed] [Google Scholar]
- 60. Chee HL, Kandiah M, Khalid M, Shamsuddin K, Jamaluddin J, Nordin NA, Shuib R, Osman I. Body mass index and factors related to overweight among women workers in electronic factories in Peninsular Malaysia. Asia Pac J Clin Nutr. 2004;13:248–54. [PubMed] [Google Scholar]
- 61. Walls HL, Peeters A, Son PT, Quang NN, Hoai NT, Loi do D, Viet NL, Khai PG, Reid CM. Prevalence of underweight, overweight and obesity in urban Hanoi, Vietnam. Asia Pac J Clin Nutr. 2009;18:234–9. [PubMed] [Google Scholar]
- 62. Cuong TQ, Dibley MJ, Bowe S, Hanh TT, Loan TT. Obesity in adults: an emerging problem in urban areas of Ho Chi Minh City, Vietnam. Eur J Clin Nutr. 2007;61:673–81. [DOI] [PubMed] [Google Scholar]
- 63. Pham NM, Eggleston K. Diabetes prevalence and risk factors among Vietnamese adults: findings from community-based screening programs. Diabetes Care. 2015;38:e77–78. [DOI] [PubMed] [Google Scholar]
- 64. Do HT, Geleijnse JM, Le MB, Kok FJ, Feskens EJ. National prevalence and associated risk factors of hypertension and prehypertension among Vietnamese adults. Am J Hypertens. 2015;28(1):89–97. [DOI] [PubMed] [Google Scholar]
- 65. Kamso S, Purwantyastuti P, Rumawas YSP, Lukito W. Nutritional status of hyperlipidemics elderly in Indonesia according to body mass index (study in four Indonesian big cities). Med J Indonesia. 2005;14:97–100. [Google Scholar]
- 66. World Health Organization. NCD risk factors in Indonesia 2006 [Internet]. Jakarta (Indonesia): World Health Organization; 2006; [cited 2018 Mar 31]. Available from: http://www.who.int/ncds/surveillance/steps/indonesia/en/. [Google Scholar]
- 67. World Health Organization. NCD risk factors in Indonesia 2003 [Internet]. Jakarta (Indonesia): World Health Organization; 2003 [cited 2018 Mar 31]. Available from: http://www.who.int/ncds/surveillance/steps/indonesia/en/. [Google Scholar]
- 68. World Health Organization. Integrated community based intervention on Major NCDS in Depok municipality [Internet]. Jakarta (Indonesia): World Health Organization; 2003; [cited 2018 Mar 31]. Available from: http://www.who.int/ncds/surveillance/steps/indonesia/en/. [Google Scholar]
- 69. Family Health Division, Department of Health Services, Ministry of Health. Nepal Demographic and Health Survey 1996 [Internet]. Kathmandu (Nepal): Family Health Division; 1997[cited 2018 Mar 31]. Available from: https://dhsprogram.com/publications/publication-FR78-DHS-Final-Reports.cfm. [Google Scholar]
- 70. International Institute for Population Sciences. National Family Health Survey (NFHS-3) India [Internet]. Hyderabad (India): International Institute for Population Sciences; 2007; [cited 2018 Mar 31]. Available from: https://dhsprogram.com/pubs/pdf/FRIND3/FRIND3-Vol1AndVol2.pdf. [Google Scholar]
- 71. Prashant K, Shaw C.. Nutritional status of adolescent girls from an urban slum area in South India. Indian J Pediatr. 2009;76(5):501–4. [DOI] [PubMed] [Google Scholar]
- 72. Royal Government of Bhutan Ministry of Health. Report on 2007 steps survey for risk factors and prevalence of no communicable diseases in Thimphu [Internet]. Thimphu (Bhutan): Royal Government of Bhutan Ministry of Health; 2009; [cited 2018 Mar 31]. Available from: http://www.who.int/chp/steps/2007NCDreport.pdf. [Google Scholar]
- 73. National Institute of Population Research and Training (NIPORT). Bangladesh Demographic and Health Survey 2007 [Internet]. Dhaka (Bangladesh): National Institute of Population Research and Training (NIPORT); 2009; [cited 2018 Mar 31]. Available from: https://dhsprogram.com/publications/publication-fr207-dhs-final-reports.cfm. [Google Scholar]
- 74. National Nutrition Monitoring Bureau, National Institute of Nutrition, Indian Council of Medical Research. Nutritional Status of Rural Population (2007–08) [Internet]. Hyderabad (India): National Nutrition Monitoring Bureau, National Institute of Nutrition, Indian Council of Medical Research; 2009; [cited 2018 Mar 31]. Available from: http://nnmbindia.org/NNMB-PDF%20FILES/Report_Of_The_NNBB_NCAER94-95.pdf. [Google Scholar]
- 75. Alam DS, Talukder SH, Chowdhury MA, Siddiquee AT, Ahmed S, Pervin S, Khan S, Hasan K, Koehlmoos TL, Niessen LW. Overweight and abdominal obesity as determinants of undiagnosed diabetes and pre-diabetes in Bangladesh. BMC Obes. 2016;3:19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76. Daniel CR, Prabhakaran D, Kapur K, Graubard BI, Devasenapathy N, Ramakrishnan L, George PS, Shetty H, Ferrucci LM, Yurgalevitch S et al.. A cross-sectional investigation of regional patterns of diet and cardio-metabolic risk in India. Nutr J. 2011;10:12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77. Bhowmik B, Munir SB, Diep LM, Siddiquee T, Habib SH, Samad MA, Azad Khan AK, Hussain A. Anthropometric indicators of obesity for identifying cardiometabolic risk factors in a rural Bangladeshi population. J Diabetes Investig. 2013;4:361–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78. World Health Organization. Non-Communicable Disease Risk Factor Survey Bangladesh 2010 [Internet]. Dhaka (Bangladesh): World Health Organization; 2011; [cited 2018 Mar 31]. Available from: http://www.who.int/ncds/surveillance/steps/2010_STEPS_Report_Bangladesh.pdf. [Google Scholar]
- 79. World Health Organization. National Non-Communicable Diseases Risk Factor Survey [Internet]. Colombo (Sri Lanka): World Health Organization; 2006; [cited 2018 Mar 31]. Available from: http://www.who.int/ncds/surveillance/steps/ 2006_STEPS_Survey_SriLanka.pdf. [Google Scholar]
- 80. Department of Census and Statistics. Sri Lanka Demographic and Health Survey 2006–07 [Internet]. Colombo (Sri Lanka): Department of Census and Statistics; 2008; [cited 2018 Mar 31]. Available from: http://www.statistics.gov.lk/social/DHS%20200607%20FinalReport.pdf. [Google Scholar]
- 81. Aekplakorn W, Chariyalertsak S, Kessomboon P, Sangthong R, Inthawong R, Putwatana P, Taneepanichskul S; Thai National Health Examination Survey IV Study Group. Prevalence and management of diabetes and metabolic risk factors in Thai adults: the Thai National Health Examination Survey IV, 2009. Diabetes Care. 2011;34:1980–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82. Hussain MA, Mamun AA, Reid C, Huxley RR. Prevalence, awareness, treatment and control of hypertension in Indonesian adults aged ≥ 40 years: findings from the Indonesia Family Life Survey (IFLS). PLoS One. 2016;11:e0160922. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83. Son PT, Quang NN, Viet NL, Khai PG, Wall S, Weinehall L, Bonita R, Byass P. Prevalence, awareness, treatment and control of hypertension in Vietnam: results from a national survey. J Hum Hypertens. 2012;26:268–80. [DOI] [PubMed] [Google Scholar]
- 84. National Statistics Directorate, Ministry of Finance Democratic Republic of Timor-Leste. Timor-Leste Demographic and Health Survey 2009 [Internet]. Dili (Timor-Leste): National Statistics Directorate; 2010; [cited 2018 Mar 31]. Available from: https://dhsprogram.com/pubs/pdf/FR235/FR235.pdf. [Google Scholar]
- 85. Venkaiah K, Brahmam G, Vijayaraghavan K. Application of factor analysis to identify dietary patterns and use of factor scores to study their relationship with nutritional status of adult rural populations. J Health Popul Nutr. 2011;29:327–38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86. National Institute of Population Research and Training (NIPORT). Bangladesh Demographic and Health Survey 2011 [Internet]. Dhaka (Bangladesh): National Institute of Population Research and Training (NIPORT); 2013; [cited 2018 Mar 31]. Available from: https://dhsprogram.com/publications/publication-fr265-dhs-final-reports.cfm. [Google Scholar]
- 87. Population Division Ministry of Health and Population, Government of Nepal. Nepal Demographic and Health Survey 2011 [Internet]. Kathmandu (Nepal): Population Division Ministry of Health and Population; 2012; [cited 2018 Mar 31]. Available from: https://dhsprogram.com/pubs/pdf/fr257/fr257%5B13april2012%5D.pdf. [Google Scholar]
- 88. Bhandari S, Sayami JT, Thapa P, Sayami M, Kandel BP, Banjara MR. Dietary intake patterns and nutritional status of women of reproductive age in Nepal: findings from a health survey. Arch Public Health. 2016;74:2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89. Sekhri T, Kanwar RS, Wilfred R, Chugh P, Chhillar M, Aggarwal R, Sharma YK, Sethi J, Sundriyal J, Bhadra K et al.. Prevalence of risk factors for coronary artery disease in an urban Indian population. BMJ Open. 2014;4:e005346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90. Arora GP, Thaman RG, Prasad RB, Almgren P, Brøns C, Groop LC, Vaag AA. Prevalence and risk factors of gestational diabetes in Punjab, North India: results from a population screening program. Eur J Endocrinol. 2015;173:257–67. [DOI] [PubMed] [Google Scholar]
- 91. UNICEF. National Nutrition Survey Afghanistan [Internet]. Kabul (Afghanistan): UNICEF; 2013; [cited 2018 Mar 31]. Available from: https://www.humanitarianresponse.info/sites/www.humanitarianresponse.info/files/assessments/Report%20NNS%20Afghanistan%202013%20%28July%2026-14%29.pdf. [Google Scholar]
- 92. Karmacharya BM, Koju RP, LoGerfo JP, Chan KC, Mokdad AH, Shrestha A, Sotoodehnia N, Fitzpatrick AL. Awareness, treatment and control of hypertension in Nepal: findings from the Dhulikhel Heart Study. Heart Asia. 2017;9:1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93. Ministry of Health and Population Nutrition. Nepal non communicable diseases risk factors: STEPS Survey Nepal 2013 [Internet]. Kathmandu (Nepal): Ministry of Health and Population Nutrition; 2014; [cited 2018 Mar 31]. Available from: http://www.searo.who.int/nepal/mediacentre/non_communicable_diseases_risk_factors_steps_survey_nepal_2013 pdf. [Google Scholar]
- 94. National Institute of Population Studies. Pakistan Demographic and Health Survey 2012–13 [Internet]. Islamabad (Pakistan): National Institute of Population Studies; 2014; [cited 2018 Mar 31]. Available from: https://dhsprogram.com/pubs/pdf/fr290/fr290.pdf. [Google Scholar]
- 95. Fatema K, Natasha K, Ali L. Cardiovascular risk factors among Bangladeshi ready-made garment workers. J Public Health Africa. 2014;5;373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96. National Institute of Population Research and Training (NIPORT). Bangladesh Demographic and Health Survey 2014 [Internet]. Dhaka (Bangladesh): National Institute of Population Research and Training (NIPORT); 2016; [cited 2018 Mar 31]. Available from: https://dhsprogram.com/publications/publication-fr311-dhs-final-reports.cfm. [Google Scholar]
- 97. Little M, Humphries S, Patel K, Dewey C. Factors associated with BMI, underweight, overweight, and obesity among adults in a population of rural south India: A crosssectional study. BMC Obes. 2016;3:12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98. Nguyen PH, Sanghvi T, Tran LM, Afsana K, Mahmud Z, Aktar B, Haque R, Menon P. The nutrition and health risks faced by pregnant adolescents: Insights from a cross-sectional study in Bangladesh. PLoS One. 2017;12:e0178878. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99. Divya G, Hemamalini M, Dhanalakshmi A. Prevalence of obesity among nursing students in SRM college of nursing, SRM university, Kattankulathur, Kancheepuram district. Asian J Pharm Med Res. 2017;10:238–40. [Google Scholar]
- 100. Sawant A, Mankeshwar R, Shah S, Raghavan R, Dhongde G, Raje H, D'souza S, Subramanium A, Dhairyawan P, Todur S et al.. Prevalence of metabolic syndrome in urban India. Cholesterol. 2011;2011:7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101. Aryal KK, Mehata S, Neupane S, Vaidya A, Dhimal M, Dhakal P, Rana S, Bhusal CL, Lohani GR, Paulin FH et al.. The burden and determinants of non communicable diseases risk factors in Nepal: findings from a nationwide STEPS survey. PLoS One. 2015;10:e0134834. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102. Zaman MM, Yoshiike N, Rouf MA, Syeed MH, Khan MR, Haque S, Mahtab H, Tanaka H. Cardiovascular risk factors: distribution and prevalence in a rural population of Bangladesh. J Cardiovasc Risk. 2001;8:103–8. [DOI] [PubMed] [Google Scholar]
- 103. Pakistan Health Research Council. Non-Communicable Diseases Risk Factors Survey—Pakistan [Internet]. Islamabad (Pakistan): Pakistan Health Research Council; 2014; [cited 2018 Mar 31]. Available from: http://www.who.int/entity/chp/steps/2014_Pakistan_STEPS_Report.pdf?ua = 1. [Google Scholar]
- 104. World Health Organization. National survey for noncommunicable disease risk factors and mental health using approach in Bhutan—2014 [Internet]. Thimpu (Bhutan): World Health Organization; 2014; [cited 2018 Mar 31]. Available from: http:// www.who.int/ncds/ surveillance/steps/ Bhutan_2014_STEPS_Report. pdf. [Google Scholar]
- 105. Thakur JS, Jeet G, Pal A, Singh S, Singh A, Deepti SS, Lal M, Gupta S, Prasad R, Jain S et al.. Profile of risk factors for non-communicable diseases in Punjab, Northern India: results of a state-wide STEPS survey. PLoS One. 2016;11:e0157705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106. Rawal LB, Biswas T, Khandker NN, Saha SR, Bidat Chowdhury MM, Khan ANS, Chowdhury EH, Renzaho A. Non-communicable disease (NCD) risk factors and diabetes among adults living in slum areas of Dhaka, Bangladesh. PLoS One. 2017;12(10):e0184967. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107. Ministry of Planning and Ministry of Health. Cambodia Demographic and Health Survey 2014 [Internet]. Phnom Penh (Cambodia): Ministry of Planning and Ministry of Health; 2015; [cited 2018 Mar 31]. Available from: https://dhsprogram.com/pubs/pdf/FR312/FR312.pdf. [Google Scholar]
- 108. Makurat J, Friedrich H, Kuong K, Wieringa FT, Chamnan C, Krawinkel MB. Nutritional and micronutrient status of female workers in a garment factory in Cambodia. Nutrients. 2016;8:694. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109. World Health Organization. National survey for noncommunicable disease risk factors and injuries using WHO STEPS approach in Timor-Leste—2014 [Internet]. Dili (Timor-Leste): World Health Organization; 2014; [cited 2018 Mar 31]. Available from: http://www.who.int/ncds/surveillance/steps/Timor-Leste_2014_STEPS_Report.pdf. [Google Scholar]
- 110. Golder AM, Erhardt JG, Scherbaum V, Saeed M, Biesalski HK, Fürst P. Dietary intake and nutritional status of women and pre-school children in the Republic of the Maldives. Public Health Nutr. 2001;4:773–80. [DOI] [PubMed] [Google Scholar]
- 111. Ministry of Health and Sports. Myanmar Demographic and Health Survey 2015–16 [Internet]. Nay Pyi Taw (Myanmar): Ministry of Health and Sports; 2017; [cited 2018 Mar 31]. Available from: https://dhsprogram.com/pubs/pdf/FR324/FR324.pdf. [Google Scholar]
- 112. World Health Organization. Non Communicable Disease Risk Factor Survey Sri Lanka 2015 [Internet]. Colombo (Sri Lanka): World Health Organization; 2015; [cited 2018 Mar 31]. Available from: http://www.who.int/ncds/surveillance/steps/STEPS-report-2015-Sri-Lanka.pdf. [Google Scholar]
- 113. Ministry of Health. National survey on the risk factors of non-communicable diseases (STEPS) Viet Nam, 2015 [Internet]. Hanoi (Vietnam): Ministry of Health; 2016 [cited 2018 Mar 31]. Available from: http://www.who.int/ncds/surveillance/steps/VietNam_2015_STEPS_Report.pdf. [Google Scholar]
- 114. Loh KW, Rani F, Chan TC, Loh HY, Ng CW, Moy FM. The association between risk factors and hypertension in Perak, Malaysia. Med J Malaysia. 2013;68:291–6. [PubMed] [Google Scholar]
- 115. Aekplakorn W, Kessomboon P, Sangthong R, Chariyalertsak S, Putwatana P, Inthawong R, Nitiyanant W, Taneepanichskul S; NHES IV Study Group. Urban and rural variation in clustering of metabolic syndrome components in the Thai population: results from the fourth National Health Examination Survey 2009. BMC Public Health. 2011;11:854. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116. Cervantes VG, López-Espinoza A, Moreno AG, Canedo CL, Miramontes EH, Housni FE, del Toro HB, Castillo MG, Reyes-Castillo Z. Effect of the number of interruptions in the pattern of sedentary behavior on energy expenditure. Rev Mex Trastor Aliment. 2016;7:46–55. [Google Scholar]
- 117. Ertem M, Bahceci M, Tuzcu A, Saka G, Ozturk U, Gokalp D. The association between high parity and obesity in women living in South-eastern Turkey. Eat Weight Disord. 2008;13:e4–e7. [DOI] [PubMed] [Google Scholar]
- 118. Sidik SM, Rampal L. The prevalence and factors associated with obesity among adult women in Selangor, Malaysia. Asia Pac Fam Med. 2009;8(1):2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119. Heliövaara M, Aromaa A. Parity and obesity. J Epidemiol Community Health. 1981;35:197–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120. Sakurai T, Iimuro S, Araki A, Umegaki H, Ohashi Y, Yokono K, Ito H. Age-associated increase in abdominal obesity and insulin resistance, and usefulness of AHA/NHLBI definition of metabolic syndrome for predicting cardiovascular disease in Japanese elderly with type 2 diabetes mellitus. Gerontology. 2010;56:141–9. [DOI] [PubMed] [Google Scholar]
- 121. Mamun AA, Kinarivala M, O'Callaghan MJ, Williams GM, Najman JM, Callaway LK. Associations of excess weight gain during pregnancy with long-term maternal overweight and obesity: evidence from 21 y postpartum follow-up. Am J Clin Nutr. 2010;91:1336–41. [DOI] [PubMed] [Google Scholar]
- 122. Mendez MA, Monteiro CA, Popkin BM. Overweight exceeds underweight among women in most developing countries. Am J Clin Nutr. 2005;81:714–21. [DOI] [PubMed] [Google Scholar]
- 123. Subramanian S, Perkins JM, Özaltin E, Davey Smith G. Weight of nations: a socioeconomic analysis of women in low-to middle-income countries. Am J Clin Nutr. 2010;93:413–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124. Hasan MT, Soares Magalhaes RJ, Williams GM, Mamun AA. The role of maternal education in the 15‐year trajectory of malnutrition in children under 5 years of age in Bangladesh. Matern Child Nutr. 2016;12:929–39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125. Kotian MS, Kumar G, Kotian SS. Prevalence and determinants of overweight and obesity among adolescent school children of South Karnataka, India. Indian J Community Med. 2010;35:176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126. Balarajan Y, Villamor E.. Nationally representative surveys show recent increases in the prevalence of overweight and obesity among women of reproductive age in Bangladesh, Nepal, and India. J Nutr. 2009;139:2139–44. [DOI] [PubMed] [Google Scholar]
- 127. Golder AM, Erhardt JG, Scherbaum V, Saeed M, Biesalski HK, Fürst P. Dietary intake and nutritional status of women and pre-school children in the Republic of the Maldives. Public Health Nutr. 2001;4:773–80. [DOI] [PubMed] [Google Scholar]
- 128. Goyal RK, Shah VN, Saboo BD, Phatak SR, Shah NN, Gohel MC, Raval PB, Patel SS. Prevalence of overweight and obesity in Indian adolescent school going children: its relationship with socioeconomic status and associated lifestyle factors. J Assoc Phy India. 2010;58:151–8. [PubMed] [Google Scholar]
- 129. Hosegood V, Campbell OM. Body mass index, height, weight, arm circumference, and mortality in rural Bangladeshi women: a 19-y longitudinal study. Am J Clin Nutr. 2003;77:341–7. [DOI] [PubMed] [Google Scholar]
- 130. Zaman MM, Yoshiike N, Rouf MA, Syeed MH, Khan MR, Haque S, Mahtab H, Tanaka H. Cardiovascular risk factors: distribution and prevalence in a rural population of Bangladesh. J Cardiovasc Risk. 2001;8:103–8. [DOI] [PubMed] [Google Scholar]
- 131. Sayeed MA, Mahtab H, Khanam PA, Begum R, Banu A, Azad Khan AK. Diabetes and hypertension in pregnancy in a rural community of Bangladesh: a population-based study. Diabet Med. 2005;22:1267–71. [DOI] [PubMed] [Google Scholar]
- 132. Hosain GM, Chatterjee N, Begum A, Saha SC. Factors associated with low birthweight in rural Bangladesh. J Trop Pediatr. 2006;52:87–91. [DOI] [PubMed] [Google Scholar]
- 133. Nahar S, Mascie-Taylor CGN, Begum HA. Maternal anthropometry as a predictor of birth weight. Public Health Nutr. 2007;10:965–70. [DOI] [PubMed] [Google Scholar]
- 134. Islam MZ, Akhtaruzzaman M, Lamberg-Allardt C. Nutritional status of women in Bangladesh: comparison of energy intake and nutritional status of a low income rural group with a high income urban group. Asia Pac J Clin Nutr. 2004;13:61–8. [PubMed] [Google Scholar]
- 135. Hussain A, Rahim MA, Azad Khan AK, Ali SM, Vaaler S. Type 2 diabetes in rural and urban population: diverse prevalence and associated risk factors in Bangladesh. Diabet Med. 2005;22:931–6. [DOI] [PubMed] [Google Scholar]
- 136. Yeasmin R, Choudhury S, Parveen S, Nahar N, Begum K, Akhter F. Assessment of overweight, obesity and metabolic variables among students of a private medical college in Dhaka city. J Med Sci. 2015;14:53–8. [Google Scholar]
- 137. Bansal SK, Saxena V, Kandpal SD, Gray WK, Walker RW, Goel D. The prevalence of hypertension and hypertension risk factors in a rural Indian community: A prospective door-to-door study. J Cardiovasc Dis Res. 2012;3:117–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138. Das M, Pal S, Ghosh A. Association of metabolic syndrome with obesity measures, metabolic profiles, and intake of dietary fatty acids in people of Asian Indian origin. J Cardiovasc Dis Res. 2010;1:130–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139. Bondevik GT, Ulstein M, Lie RT, Rana G, Kvale G. The prevalence of anemia in pregnant Nepali women-a study in Kathmandu. Acta Obstet Gynecol Scand. 2000;79:341–9. [PubMed] [Google Scholar]
- 140. Bogati A, Manandhar R, Sharma D, Baidhya SG, Prajapati D, Baniya S, Bista N, Khanal S, Ranabhat S. Prevalence of cardiovascular risk factors among the residents of urban community of Kathmandu municipality. Nepalese Heart J. 2017;14:3–7. [Google Scholar]
- 141. Amin F, Fatima SS, Islam N, Gilani AH. Prevalence of obesity and overweight, its clinical markers and associated factors in a high risk South-Asian population. BMC Obes. 2015;2:16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142. Sekiyama M, Jiang HW, Gunawan B, Dewanti L, Honda R, Shimizu-Furusawa H, Abdoellah OS, Watanabe C. Double burden of malnutrition in rural West Java: household-level analysis for father-child and mother-child pairs and the association with dietary intake. Nutrients. 2015;7:8376–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143. Ghee LK. A review of adult obesity research in Malaysia. Med J Malaysia. 2016;71:7. [PubMed] [Google Scholar]
- 144. Cheah WL, Hazmi H, Chia HQ, Tindin E, Zafri NAA, Shah SHM. Hypertension and its association with anthropometric indexes among pre-university students. Int J Adolesc Med Health. 2016;28:373–9. [DOI] [PubMed] [Google Scholar]
- 145. Chin KY, Low NY, Dewiputri WI, Ima-Nirwanaa S. Factors associated with bone health in Malaysian middle-aged and elderly women assessed via quantitative ultrasound. Int J Environ Res Public Health. 2017;14:E736. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146. Pinidiyapathirage MJ, Kasturiratne A, Ranawaka UK, Gunasekara D, Wijekoon N, Medagoda K, Perera S, Takeuchi F, Kato N, Warnakulasuriya T et al.. The burden of diabetes mellitus and impaired fasting glucose in an urban population of Sri Lanka. Diabet Med. 2013;30:326–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147. Wijesuriya M, Gulliford M, Charlton J, Vasantharaja L, Viberti G, Gnudi L, Karalliedde J. High prevalence of cardio-metabolic risk factors in a young urban Sri-Lankan population. PLoS One. 2012;7:e31309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148. Son PT, Quang NN, Viet NL, Khai PG, Wall S, Weinehall L, Bonita R, Byass P. Prevalence, awareness, treatment and control of hypertension in Vietnam-results from a national survey. J Hum Hypertens. 2012;26:268–80. [DOI] [PubMed] [Google Scholar]
- 149. Ota E, Haruna M, Suzuki M, Anh DD, Tho le H, Tam NT, Thiem VD, Anh NT, Isozaki M, Shibuya K et al.. Maternal body mass index and gestational weight gain and their association with perinatal outcomes in Viet Nam. Bull World Health Organ. 2011;89:127–36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150. Binh TQ, Phuong PT, Nhung BT, Tung DD. Metabolic syndrome among a middle-aged population in the red river delta region of Vietnam. BMC endocrine disorders. 2014;14:77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151. Bui TV, Blizzard CL, Luong KN, Truong Nle V, Tran BQ, Otahal P, Srikanth V, Nelson MR, Au TB, Ha ST et al.. Physical activity in Vietnam: estimates and measurement issues. PLoS One. 2015;10:e0140941. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152. Nakamori M, Ninh NX, Isomura H, Yoshiike N, Hien VT, Nhug BT, Nhien NV, Nakano T, Khan NC, Yamamoto S. Nutritional status of lactating mothers and their breast milk concentration of iron, zinc and copper in rural Vietnam. J Nutr Sci Vitaminol (Tokyo). 2009;55:338–45. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.