Abstract
The novel 2019 coronavirus disease (COVID-19), resulting from severe acute respiratory syndrome coronarvirus-2 (SARS-CoV-2) infection, typically leads to respiratory failure in severe cases; however, cardiovascular injury is reported to contribute to a substantial proportion of COVID-19 deaths. Preexisting cardiovascular disease (CVD) is among the most common risk factors for hospitalization and death in COVID-19 patients, and the pathogenic mechanisms of COVID-19 disease progression itself may promote the development of cardiovascular injury, increasing risk of in-hospital death. Sex differences in COVID-19 are becoming more apparent as mounting data indicate that males seem to be disproportionately at risk of severe COVID-19 outcome due to preexisting CVD and COVID-19-related cardiovascular injury. In this review, we will provide a basic science perspective on current clinical observations in this rapidly evolving field and discuss the interplay sex differences, preexisting CVD and COVID-19-related cardiac injury.
Keywords: Sex differences, Cardiovascular, COVID-19, ACE2, Arrhythmia, Thrombosis
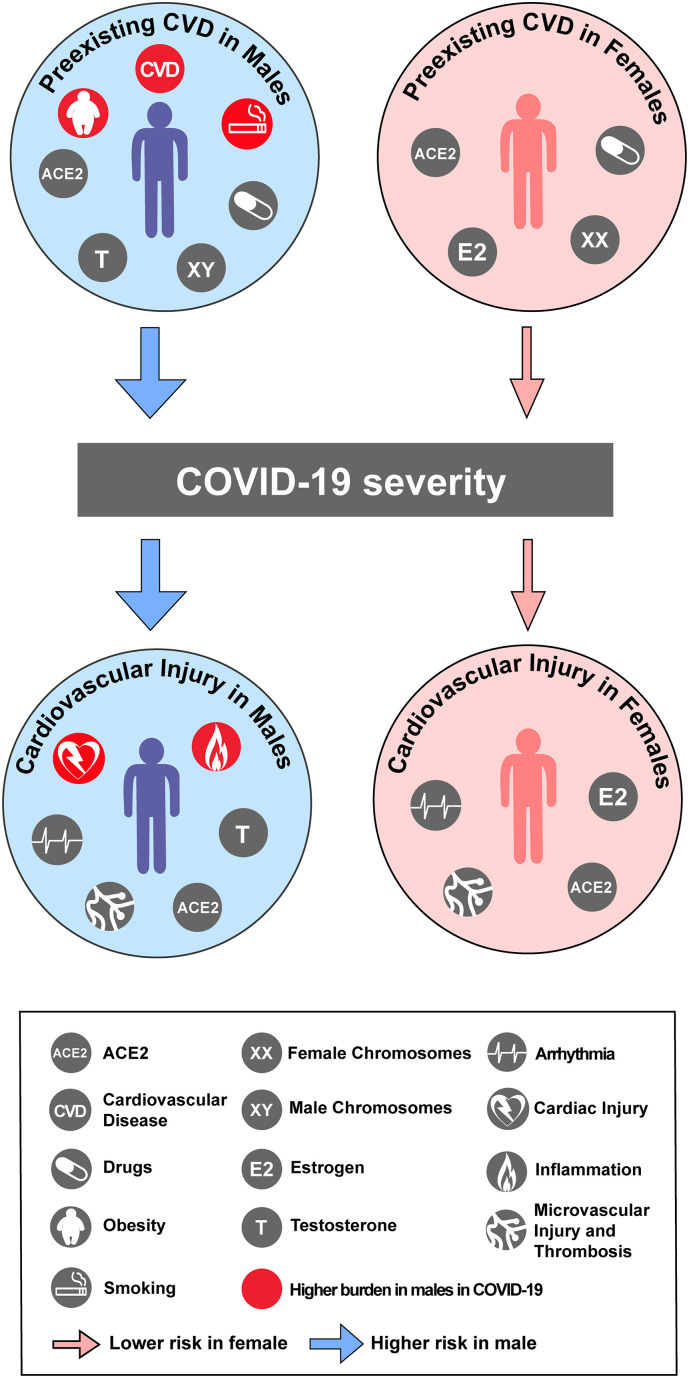
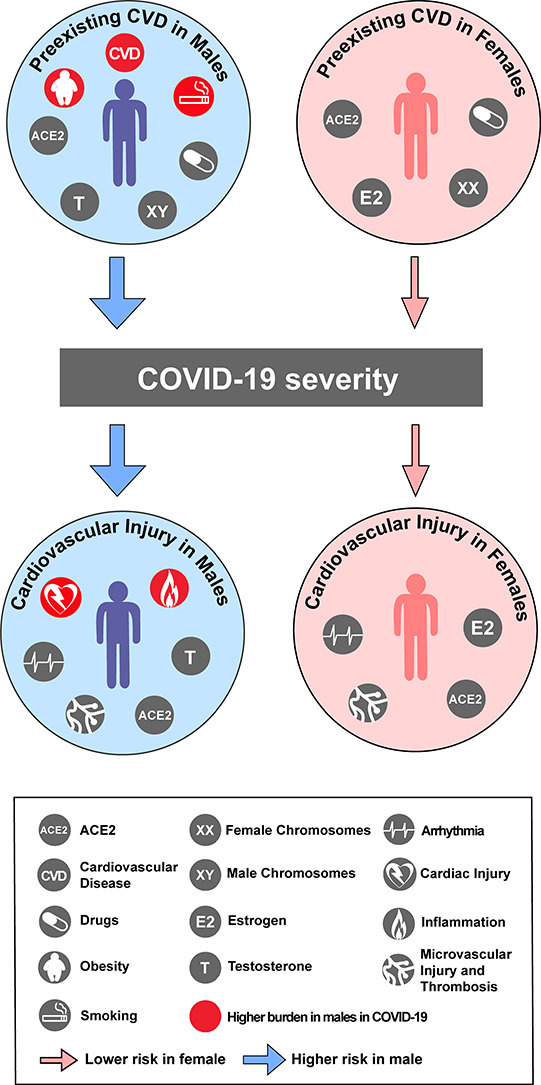
Graphical abstract
Highlights
-
•
Cardiovascular complications are prominent in COVID-19.
-
•
Preexisting cardiovascular disease is a risk factor for COVID-19 severity.
-
•
Cardiovascular disease, smoking and obesity burden more male COVID-19 patients
-
•
Cardiac injury and systemic inflammation are pronounced in male COVID-19 patients.
-
•
No sex disparities were observed in arrhythmia and thrombosis in COVID-19 patients.
1. Introduction
The novel 2019 coronavirus disease (COVID-19) results from severe acute respiratory syndrome coronarvirus-2 (SARS-CoV-2) infection and typically afflicts the lungs, with severe cases leading to acute respiratory distress syndrome [1]. Although the respiratory system is the major organ system affected by SARS-CoV-2, cardiovascular complications should not be overlooked by healthcare workers and basic scientists. In particular, acute myocardial injury, cardiac arrhythmias and microvascular dysfunction and thrombosis are reported to contribute to a large proportion of COVID-19 deaths [[2], [3], [4], [5], [6], [7]].
Patients with pre-existing cardiovascular disease (CVD) do not appear to be more prone to SARS-CoV-2 infection since the prevalence of CVD in COVID-19 cases is consistent with the high prevalence in the general population [5,6,8,9]. However, pre-existing CVD is among the most common risk factors associated with hospitalizations, elevated cardiac injury biomarkers and death of COVID-19 patients [4,10,11]. As such, it is plausible that pre-existing CVD may exacerbate the course of disease and mortality in COVID-19 patients by promoting cardiovascular injury including myocardial damage, arrhythmias and microvascular dysfunction and thrombosis. Additionally, the pathogenic mechanisms of COVID-19 disease progression itself may be associated with the development of cardiovascular injury, which increases the risk of in-hospital death [12,13].
While there is a robust body of evidence elucidating sex differences in CVD, sex disparities in COVID-19 are becoming more apparent as well [14]. Interestingly, mounting data also indicate that individuals with higher risk of severe COVID-19 outcome due to preexisting CVD and COVID-19-related cardiovascular injury include a disproportionate number of males. In this review, we will discuss sex differences in the interplay between preexisting CVD, COVID-19 severity, and COVID-19-related cardiac injury by providing a basic science perspective based on the current literature in this rapidly evolving field.
2. Sex differences in preexisting cardiovascular disease, risk factors and COVID-19
As the clinical data surrounding COVID-19 infection and mortality rates continues to become more robust, a staggering trend is becoming apparent: COVID-19 positive males suffer worse disease progression and have a higher rate of mortality than females despite having a similar rate of infection [15]. The first published study investigating sex differences in the COVID-19 cases in China reports that men are more likely to experience serious illness and are 2.4 times more likely to die from COVID-19 while the average age of mortality and rate of infection remains the same for both sexes [15,16].
Sex differences in COVID-19 result from a complicated interplay between biological and societal influences, including preexisting CVD (Fig. 1 ). Hypertension and history of CVD, both already known to increase COVID-19 severity and mortality [17], display strong sex differences with males exhibiting a higher prevalence of disease compared to age-matched women, prior to menopausal years [18,19]. On the other hand, women experience relatively worse outcomes of ischemic heart disease compared with men [20]. In HF, the overall lifetime risk is similar between men and women, there are marked sex differences in the variations of this condition, with males being predisposed to HF with reduced ejection fraction (HFrEF) and females to HF with preserved ejection fraction (HFpEF) [21]. In cardiac arrhythmias, the age-adjusted incidence of atrial fibrillation and Brugada syndrome is lower in women compared with that in men, whereas atrioventricular reentry tachycardia and cardiac events in long QT syndrome are more prevalent in adult females compared to males [22]. Lastly, male sex is an independent risk factor for various thrombotic events such as myocardial infarction, venous thromboembolism and thrombotic stroke [23]. In this section, we highlight sex differences in preexisting CVD and how they may contribute to the striking sex differences found in COVID-19 mortality.
Fig. 1.
Factors underlying preexisting CVD, risk of COVID-19 severity, and COVID-19 related cardiovascular injury in males and females. Preexisting CVD is modulated by sex chromosomes and hormones, ACE2 expression, drug interactions, obesity and smoking, which may predispose males and females differently to COVID-19 severity. CVD, obesity and smoking are risk factors with a higher burden in male vs. female COVID-19 patients (shown with red icons in males). COVID-19 pathogenic mechanisms also contribute to cardiovascular injury. Males exhibit higher burden of cardiac injury than females, while no sex disparities in arrhythmia and microvascular injury and thrombosis have been reported thus far. COVID-19-induced cardiovascular injury is thought to be modulated by sex hormones, ACE2 expression and systemic inflammation, with the latter being more pronounced in males. Altogether, these factors may explain why male COVID-19 patients seem to be at higher risk for severe disease progression and cardiovascular injury compared to females. Red icons reflect sex differences in factors observed in COVID-19 patients, gray icons reflect factors wherein no sex difference has been found in COVID-19 patients or is yet unknown. (For interpretation of the references to colour in this figure legend, the reader is referred to the web version of this article.)
2.1. Sex hormones and chromosomes in CVD
Males exhibit increased risk of CVD compared to age-matched women, prior to menopausal years [18,19]. These data indicate that individuals more at risk of severe COVID-19 outcome due to pre-existing CVD include a disproportionate number of males.
The increased prevalence of CVD in males is multifactorial and well-studied with biological variables including sex hormones and their receptors as well as sex chromosomes. As detailed in a previous review from our group, the protective effects of estrogen have been well documented over the past few decades and may help explain why females of premenopausal age have lower incidence of CVD when compared to males [24,25]. Exerting its effects through both genomic and non-genomic pathways, estrogen has been shown to ward off CVD through its effects on vasculature, cardiomyocytes and cardiac fibroblasts to promote vasodilation, angiogenesis, and cardiomyocyte survival while reducing cardiac fibrosis and oxidative stress [24]. More recently, the role of sex chromosomes has been implicated in the sex differences found in CVD as well [26]. Sex chromosomes, which differ between males (XY) and females (XX), can impart sex differences in disease through altered expression of genes encoded by the X and Y chromosomes [27]. Strikingly, studies that examined the effects of sex chromosome complement (XX or XY) in the absence of sex hormones reveal that XX chromosome complement increases the risk of developing CV complications including hypertension, atherosclerosis and ischemic injury [26,[28], [29], [30]]. A handful of genes encoded by the X chromosome that escape inactivation on the second X chromosome in females are implicated as females have elevated expression of these genes compared to male, many of which are epigenetic modifiers. Taken together, premenopausal females seem to be protected against CVD when compared to males; however, with reduced levels of estrogen, post-menopausal women have an elevated risk of CVD complications. This increased risk could potentially prime older females with COVID-19 for more severe cardiac outcome, although more data is needed to parse apart the influence of menopause on COVID-19-related CVD complications.
2.2. ACE2 in CVD and COVID-19
Angiotensin-converting enzyme 2 (ACE2) is the functional receptor for SARS coronaviruses including the novel SARS-CoV-2 that causes COVID-19 [31,32]. ACE-2, a carboxypeptidase transmembrane protein expressed in various cell types, regulates the activity of the renin-angiotensin system (RAS) by hydrolyzing angiotensin I (AngI) into Ang 1–9 and angiotensin II (AngII) into Ang 1–7 [33]. While ACE2 is homologous to ACE, the enzyme that converts AngI to the vasoconstrictive, pro-inflammatory, pro-hypertrophic and pro-fibrotic AngII, ACE2 counterbalances the detrimental effects of ACE [34]. ACE2 confers cardioprotection by enhancing vasodilation and preventing cardiac hypertrophy, fibrosis and oxidative stress [34]. ACE2-deficient mice exhibit elevated AngII levels, increased cardiac hypertrophy and fibrosis, and severe diastolic and systolic dysfunction, which is rescued by recombinant human ACE2 therapy [35,36].
While animal models and analysis of human hearts at the whole tissue level do not provide conclusive results regarding the directionality of cardiac ACE2 expression in CVD [[37], [38], [39], [40]], CVD does augment ACE2 expression in cardiomyocytes. ACE2 expression is increased in cardiomyocytes of patients suffering from dilated and hypertrophic cardiomyopathy, aortic stenosis and HFrEF compared to control donor hearts [37,41,42]. Interestingly, cardiac pericytes, fibroblasts and vascular smooth muscle cells from these patients exhibited lower ACE2 expression compared to control donor hearts [37,41]. Altered cardiac ACE2 expression profiles in CVD have been proposed as a mechanism underlying the more severe course of disease in COVID-19 patients with pre-existing CVD, since elevated cardiac ACE2 could mediate SARS-CoV-2 infection.
2.3. Sex differences in ACE2
ACE2 is encoded by the X chromosome and is located in a region of the X chromosome that escapes X-inactivation in females [43]. Since females have two copies of the X chromosome compared to one copy in males, most X-escapee genes are found to have higher expression in females [44,45]. ACE2, however, displays an uncharacteristically heterogeneous pattern across various tissues exhibiting increased mRNA expression in certain male tissues [44]. It is hypothesized that gene-hormone interactions accounts for this uncharacteristic pattern of expression as ACE2 activity has been demonstrated to be sex hormone dependent [46,47].
In the left ventricle (LV), hypertensive male rats (both spontaneously hypertensive and mRen2 strains) experience higher levels of ACE2 activity and hypertrophy when compared to females [48,49]. Gonadectomy in males resulted in decreased ACE2 expression and reduced cardiac hypertrophy, whereas ovariectomy in females resulted in increased LV ACE2 activity and cardiac hypertrophy coupled with reduced hemodynamic function of the heart [49]. In contrast, studies using normotensive Lewis rats and MF1 mice did not demonstrate sexually dimorphic cardiac ACE2 activity [48,50]. These studies, however, demonstrated that estrogen altered the expression and activity of ACE2 in other tissues including plasma, adipose tissue, and kidneys, while the effect of estrogen was varied. A study investigating the role of sex chromosomes in ACE2 activity revealed that while estrogen influenced ACE2 activity in the kidney of MF1 mice, sex chromosomes complement (XX or XY) had no effect [50].
While ACE2 is encoded by the X chromosome, more highly expressed in certain male tissues than female tissues, and is influenced by estrogen, it is still unclear whether sexual dimorphisms in ACE2 directly contribute to the sex differences seen in COVID-19 severity and mortality (Fig. 1. Even so, testing the use of short-term exogenous estrogen treatment as a therapy for COVID-19 patients is now underway in a Phase II clinical trial that includes both sexes (ID: NCT04359329) [51].
2.4. Sex differences, drugs and ACE2 in COVID-19
Since AngII plays a central role in CVD pathophysiology, drugs that inhibit the activity of ACE (ACEi) or block AngII receptors (ARBs) are commonly prescribed as a first-line treatment. Sex differences exist in the cardiovascular efficacy and outcome of ARB and ACEi use, indicating differences in drug absorption, distribution, metabolism, and excretion between males and females [[52], [53], [54]]. Various ACEi and ARB have been shown to enhance expression and activity of cardiac ACE2 in experimental animal models [55,56]. More recently, single-cell RNA sequencing (scRNAseq) revealed that hypertrophic cardiomyopathy patients taking ACEi trended towards elevated ACE2 expression in cardiomyocytes, fibroblasts, pericytes, and vascular smooth muscle cells [37]. Similarly, cardiomyocytes from ACEi-treated aortic stenosis and HFrEF patients exhibited enhanced ACE2 levels and unfavorable ACE/ACE2 ratios [41]. Since ACE2 is the main receptor of SARS-CoV-2, these studies led to initial concerns of enhanced susceptibility of SARS-CoV-2 infection; however, there is currently no proof that this outweighs their protective role in modulating RAS activity [41,57]. In two recent studies, including a large observational study of 8910 COVID-19 patients, no association was found between the use of ACEi and ARB and increased likelihood of a positive SARS-CoV-2 test nor with increased risk of COVID-19 complications when corrected for sex, among others (Fig. 1) [58]. As such, effects of sex-specific efficacy of ARB and ACEi on COVID-19 progression and outcome seem unlikely.
2.5. Sex differences in obesity
Obesity is a major risk factor for developing CVD and emerging evidence shows that obesity is also risk factor of developing severe COVID-19 outcome and mortality [[59], [60], [61], [62], [63], [64]]. Sex differences in obesity are well established (Fig. 1) [65]. Obesity prevalence is significantly associated with sex and pathophysiological mechanisms of obesity are modulated by both sex hormones and chromosomes [65,66]. Whether sex differences exist in the prevalence of obesity in COVID-19 patients is thus far not fully elucidated, but allude to higher prevalence of obese male COVID-19 patients than female. A study of 200 COVID-19 patients in New York City found no difference in proportion of males and females when COVID-19 patients were stratified by BMI [60]. However, studies of 383 Chinese and 92 Italian COVID-19 patients reported that the proportion of men was significantly higher in the overweight and obese BMI groups [61,63].
Interestingly, it is hypothesized that RAS dysregulation may link obesity to COVID-19 [67]. In line with this notion, an experimental mouse study reported that sex hormones contribute to tissue-specific ACE2 expression in the development of obesity-induced hypertension [47]. Here, high-fat diet fed females did not develop obesity-hypertension or elevated Ang 1–7 levels while males did. This effect was abolished upon ovariectomy and estrogen increased ACE2 levels. Considering the central role ACE2 and dysregulated RAS are thought to play in COVID-19, ACE2 may link sex differences, obesity, CVD and COVID-19.
2.6. Sex differences in smoking
In addition to biological factors, societal factors, including smoking, may also contribute to the sex differences present in COVID-19 (Fig. 1) [68]. Reports from 2015 reveal 52.1% of Chinese males smoke compared to just 2.7% of females [69]. Sex differences in smoking prevalence also exist in other populations, although to a much lesser degree (Italy: 26% Males, 17.2% Females [70]; United States: 17.5% Males: 13.5% Females [71]). According to a meta-analysis, history of smoking is one of the most prevalent preexisting factors associated with patients hospitalized for COVID-19 infection [17]. Studies show smoking is also a risk factor for the development of chronic obstructive pulmonary disease, hypertension, and CVD [72], which are comorbidities positively associated with COVID-19 hospitalizations [17]. Single-cell RNAseq studies recently revealed an upregulation of the SARS-CoV-2 receptor, ACE2, in the lungs of smokers compared to never-smokers, which could influence the risk and severity of COVID-19 in smokers [73]. Taken together, the sex differences found among the smoking population may contribute to the sex differences in COVID-19 hospitalizations and morbidity. Smoking, which is largely more common in male populations, is associated with COVID hospitalization, can lead to cardio-pulmonary comorbidities, and upregulates the expression of ACE2 within the lung.
3. Sex differences in COVID-19-related cardiovascular injury
Cardiovascular injury in COVID-19 is mainly observed in the form of acute cardiac injury, microvascular injury and thrombosis. Various pathophysiological mechanisms may contribute to the development COVID-19-related cardiovascular injury including direct cardiotropic and endothelial viral infection, secondary systemic toxicity of the hyperinflammatory state, cardiovascular stress due to SARS-CoV-2-induced respiratory failure, or a combination of all three factors [74,75]. Sex disparities underlie some of these factors leading to COVID-19-related cardiovascular injury.
3.1. Sex differences in clinical cardiac injury in COVID-19
Cardiac involvement is a prominent feature in COVID-19 pathophysiology. Acute myocardial damage in COVID-19 patients may be inferred from elevated circulating biomarkers, electrocardiographic changes, and imaging studies revealing features of impaired cardiac function [76]. Acute cardiac injury, based on circulating biomarkers, is more frequent in severe compared to non-severe COVID-19 cases [10,77,78] and circulating biomarker concentration is associated with disease severity and fatality [10,[78], [79], [80]]. Altogether, up to 36% of COVID-19 patients were reported to suffer from acute cardiac injury based on elevated cardiac biomarkers [6,10,77,80].
While data is still emerging, some sex disparities seem to exist in COVID-19-related cardiac injury. A study of 112 Chinese COVID-19 patients has shown a trend towards more men being diagnosed with possible myocarditis than women [11]. Similarly, two studies of Chinese COVID-19 patients showed that women account for more of the mild cases which also exhibited lower levels of troponin I, creatine kinase–myocardial band fraction, myoglobin, and N-terminal B-type brain natriuretic peptide [79,81]. In a study of 1557 COVID-19-positive individuals in New Haven, more males presented with abnormally elevated troponin T [16]. A larger study of 2736 COVID-19 patients in New York City, however, reported no significant sex differences when COVID-19 patients were stratified by troponin T levels [80]. In a study of 1557 COVID-19-positive individuals in New Haven, more males presented with abnormally elevated troponin T than females [16]. Interestingly, in this patient population, a model of combined risk factors including, age, hypertension and body mass index, showed that prostatic disease increased the odds of COVID-19 patients having elevated troponin T levels, independently of the other risk factors [16]. Together these data indicate that individuals more at risk of severe COVID-19 progression and outcome due to cardiac injury may include a disproportionate number of males (Fig. 1).
3.2. Sex differences in clinical cardiac arrhythmia in COVID-19
The clinical burden of cardiac arrhythmias in COVID-19 patients is becoming increasingly clear. Various forms of cardiac atrial and ventricular rhythm disorders have been reported in COVID-19 patients including atrial fibrillation, sinus tachycardia and bradycardia, complete conduction block and cardiac arrest [82]. Arrhythmia may associate with sudden cardiac death, which is a pathologic outcome also observed in COVID-19 patients [[83], [84], [85]]. Arrhythmia in COVID-19 patients is associated with myocardial injury and is thought to reflect the severity of illness [81,86,87]. Indeed, ICU admission is associated with arrhythmia, with up to 44% of COVID-19 patients in the ICU suffering from arrhythmia [5,88]. While the association of arrhythmias and in-hospital mortality in COVID-19 patients is inconclusive, it has been reported that the prevalence of arrhythmia is 60% in fatal COVID-19 cases [89].
Sex differences exist in cardiac electrophysiological characteristics as female sex is a known risk factor for drug-induced QT prolongation and torsade des pointes arrhythmia [90]. Whether sex differences exist in arrhythmia in COVID-19 patients remains under-reported. Since arrhythmia is associated with myocardial damage and elevated cardiac biomarkers are more prevalent in male COVID-19 patients, it is plausible that arrhythmia may also be more prevalent in male COVID-19 patients. However, a Chinese study of 234 COVID-19 patients shows no differences between the proportion of male and female COVID-19 patients with or without arrhythmia [86]. Future studies will be imperative to shed light on sex disparities in arrhythmia occurrence in COVID-19 patients (Fig. 1).
3.3. Sex differences in clinical microvascular injury and thrombosis in COVID-19
Mounting reports on microvascular dysfunction and thrombosis in COVID-19 patients suggest that endothelial dysfunction and coagulation imbalances may contribute to COVID-19 pathophysiology. Elevated levels of fibrinogen and D-dimer levels have been reported in COVID-19 patients, indicating elevated clot formation and fibrinolysis [91]. Elevated D-dimers were found to be associated with poor prognosis and increased risk of death [4,92]. Histology on post-mortem lungs and skin from COVID-19 patients revealed thrombogenic vasculopathy [93,94]. Moreover, thromboembolisms have been observed in several organs in COVID-19 patients [[95], [96], [97]]. Overall, 20–30% of COVID-19 patients in the ICU have been reported to suffer from thrombosis and major thromboembolic sequelae [7].
While data on sex differences in microvascular injury and thrombosis in COVID-19 is still sparse, sex disparities do not seem to be observed (Fig. 1). A study of 248 Chinese COVID-19 patients shows that there is no significant difference in proportion of male and females in normal and high D-dimer groups [98]. Accordingly, a meta-analysis reported that elevated D-dimer in severe COVID-19 cases and non-survivors do not seem to associate with sex [99]. Interestingly however, an Italian study of 100 COVID-19 patients reported that fibrinogen levels in female COVID-19 patients were significantly higher compared to female controls, while this increase was not significant in males [100].
3.4. Sex differences in SARS-CoV-2 cardiotropic infection
Cardiac samples from patients who succumbed to the previous SARS coronavirus in 2003 provides insight into the cardiotropic potential of coronaviruses. SARS-CoV, which also binds to the ACE2 receptor, was detected in 35% of hearts [101] and present in cardiomyocytes that displayed vacuolar degeneration, atrophy and cytoplasmic lysis [102]. While SARS-CoV-2 has been detected in hearts of COVID-19 patients, no reports yet have shown conclusive evidence of direct SARS-CoV-2 infection in non-inflammatory myocardial cells in COVID-19 patients [[103], [104], [105], [106]]. Several cell cardiac cell types express ACE2, including cardiomyocytes [107]. Recently, it was demonstrated that SARS-CoV-2 was able to infect human inducible pluripotent stem cell-derived cardiomyocytes in vitro, suggesting the potential for SARS-CoV-2 cardiotropic potential [108].
While data on sex differences in cardiotropic SARS-CoV-2 is yet unavailable, sex disparities do exist in the epidemiology and pathophysiology of viral myocarditis induced by various viruses, and this may also be the case for SARS-CoV-2 [[109], [110], [111]]. Expression of the SARS-CoV-2 receptor ACE2 is regulated by sex hormones in opposite directions in male and female mice [49]. A recent study reported that androgen signaling may regulate ACE2 expression and subsequent SARS-CoV-2 infection in human cardiac cells since treatment with the 5 alpha reductase inhibitor dutasteride and androgen receptor modulator spironolactone augmented ACE2 levels and internalization of SARS-CoV-2 recombinant spike receptor binding domain in human embryonic stem cell-derived cardiac cells [16]. As such, sex hormones may underlie possible sex differences in cardiotropic SARS-CoV-2 infection by regulating ACE2 expression.
3.5. Sex differences in endothelial dysfunction
Microvascular injury and thrombosis in COVID-19 are thought to be caused by endothelial dysfunction since activated and injured endothelial cells recruit inflammatory cells and activate the coagulation cascade [112]. Histology on post-mortem from COVID-19 patients revealed that SARS-CoV-2 is able to directly infect endothelial cells concomitant with endothelialitis and apoptosis in several organs [113]. Accordingly, SARS-CoV-2 was shown to be able to directly infect human blood vessel organoids in vitro [114].
Sex differences in endothelial dysfunction are well-established [115]. For instance, estrogen promotes proper endothelial cell function by enhancing endothelial nitric oxide synthase (eNOS) expression while testosterone has opposite effects [24]. A hallmark of endothelial dysfunction is dampened eNOS expression with NO deficiency [116]. Decreased NO levels in injured endothelial cells contribute to thrombus formation [112]. Recently it was proposed that eNOS deficiency could be a pathophysiological mechanism in COVID-19 [116]. As such, sex hormones may affect endothelial dysfunction in COVID-19. However, also in the absence of sex hormones, sex differences exist in barrier integrity and survival between male XY and female XX microvascular endothelial cells [117,118]. Although sex-differences in COVID-19-related microvascular injury and thrombosis in the clinic do not seem apparent thus far (Fig. 1), it is plausible that sex-differences play a pathophysiological role in COVID-19 endothelial dysfunction.
3.6. Sex differences in soluble ACE2
Upon binding to ACE2 on the cell surface, SARS-CoV-2 is endocytosed leading to downregulated ACE2 cell surface expression [119]. As such, the protective effects of ACE2 are likely blunted. Loss of membrane-bound ACE2 is hypothesized to be a critical step in the cardiac injury pathology in COVID-19. This notion is supported by experimental animal models wherein ACE2-deficient mice exhibit hypertrophy, fibrosis, HF and enhanced inflammation [35,36,120]. Autopsy material from the SARS epidemic revealed SARS-CoV infection in 35% of cardiac specimens concomitant with decreased membrane ACE2 levels, cardiac hypertrophy, inflammation, and fibrosis [120], indicating that loss of membrane-bound ACE2 indeed may be a pathogenic mechanism in SARS-CoV-induced cardiac injury. Similarly, ACE2 expression and activation in endothelial protects against endothelial dysfunction in atherosclerosis, hypertension and thrombosis [[121], [122], [123]]. It has been shown that ACE2 is released into the circulation which advances several CVD pathologies, and levels of soluble ACE2 in plasma correlate with worsened disease severity and prognosis in HF patients [34,124]. To date, no reports are available on levels of cardiac membrane-bound ACE2 or circulating levels of soluble ACE2 in COVID-19 patients. However, it seems that men, who are at increased risk of more severe COVID-19 progression, present with higher soluble ACE2 levels than women as was observed in both healthy subjects and two independent cohorts of HF patients [125,126].
3.7. Sex differences in systemic inflammation in COVID-19
SARS-CoV-2 infection is characterized by a robust cascade of inflammatory and immune events. In the early stages of infection, COVID-19 patients present progressive lymphocytopenia; however, patients were reported to eventually develop elevated white blood cell and neutrophil counts [2,5,127]. In the hyperinflammatory phase, driven by the host immune response, inflammatory markers become elevated and secondary organ damage may occur in what is deemed the cytokine storm. Systemic cytokine elevation is known to be cardiotoxic with the potential to induce profound myocardial injury, as reported in patients treated with chimeric antigen receptor T-cells who develop cytokine release syndrome [76,128,129]. Furthermore, cytokine storms may directly mediate ventricular electrical remodeling and significant QT interval prolongation, predisposing for ventricular arrhythmias [130]. Additionally, proinflammatory cytokines are known to promote coagulation and thrombosis by enhancing expression of tissue factor on endothelial cells, activating coagulation factors and inhibiting fibrinolysis, as is observed in severe cases of sepsis [131].
While the rate of SARS-CoV-2 infection seems to be similar between males and females [15], the ability to mount an immune response to protect against COVID-19 may contribute to sex differences seen in COVID-19 mortality and cardiac injury. Through a combination of sex biasing factors, females have a greater ability to detect virial infection and generally experience a more robust response to viral infection which could contribute to their protection against COVID-19 when compared to males [[132], [133], [134], [135]]. Both sex hormones and sex chromosomes influence sex differences in immunity [134,136]. Sex hormones have been shown to bind to receptors on immune cell surfaces to alter their gene expression and activity [134]. Additionally, the X chromosome encodes a high density of immune-related genes and microRNAs which, despite inactivation of the second X chromosome in females, remain overly expressed in females compared to males, contributing to the heightened immune response in females [[136], [137], [138]]. The male-specific Y chromosome, which encodes substantially less genes than its X chromosome counterpart, has also been found to influence immune function as Y chromosome genes are expressed in various immune cell types and have been shown to alter immune function [139,140].
Notably, similar sex differences were also observed in the previous coronaviruses SARS and Middle East respiratory syndrome (MERS). In both SARS and MERS outbreaks, males had higher mortality rates than females [15,141,142]. Mouse studies investigating SARS, which also infects the airways and lungs through the ACE2 receptor, revealed that infected male and female mice had a unique immune signature compared to males, and estrogen protected against SARS severity partially through mediating this immune response [141]. While the data is still sparse, reports show a sex-specific immune signature may be present in SARS-CoV-2 infection as well (Fig. 1). One study found male COVID-19 patients exhibit elevated circulating white blood cells and neutrophils when compared to female patients [15]. Another study revealed male COVID-19 patients exhibit a lower lymphocyte count and elevated levels of IL-10, TNF-α, and CRP compared to females [143]. It remains to be elucidated to which extent the sex differences observed in systemic inflammation in COVID-19 patients translate to differences in inflammation-induced cardiac injury, arrhythmia and microvascular dysfunction and thrombosis.
3.8. Sex differences in COVID-19 drug-induced cardiac arrhythmia
Arrhythmias in COVID-19 patients may result from biological factors in the pathophysiology of COVID-19 or may be induced by drugs used for treating COVID-19 [144]. While the clinical efficacy of these drugs is still relatively unknown, the antimalarial drugs chloroquine and hydroxychloroquine were shown to have antiviral properties against SARS-CoV-2 in vitro by increasing endosomal pH and interfering with ACE2 glycosylation [145,146]. Administration of chloroquine and hydroxychloroquine with or without adjunctive azithromycin has been reported to significantly prolong the QT interval in COVID-19 patients [[147], [148], [149], [150], [151]]. The risk of developing torsade des pointes ventricular arrhythmia and arrhythmic death in COVID-19 patients treated with hydroxychloroquine/chloroquine/azithromycin however does not seem to increase [[147], [148], [149], [150], [151], [152]].
Interestingly, an in silico modeling study using mathematical models of ion currents from human ventricular cardiomyocytes and clinically therapeutic drug doses has shown that females with preexisting cardiovascular disease may especially be susceptible to antimalarial drug-induced QT prolongation compared to males with cardiovascular disease or healthy individuals of either sex [153]. Indeed, sex differences in cardiovascular drug responses have been reported and female sex is a known risk factor for drug-induced QT prolongation and torsade des pointes which may be caused by female sex hormones affecting cardiomyocyte ion currents [90,154]. However, thus far no sex differences have been reported inthe prevalence of QT interval prolongation in COVID-19 patients treated with hydroxychloroquine/chloroquine with or without azithromycin (Fig. 1) [147,148,150].
4. Concluding remarks
Preexisting CVD and cardiovascular injury seem to be a prominent feature of COVID-19 severity and outcome. Research in the COVID-19 field is rapidly evolving; however, the thus-far observed sex disparities already emphasize the need to understand the pathophysiological role of sex hormones and chromosomes in COVID-19 disease progression and COVID-19-related cardiovascular injury. Clinically, studies show that males with preexisting CVD are particularly prone to more severe COVID-19 disease and COVID-19-related cardiovascular injury. As such, sex hormone and chromosome COVID-19 interactions will be a promising field of study to elucidate novel protective mechanisms and therapies for the treatment of COVID-19. Additionally, sex differences in ACE2 expression, inflammation and drug absorption, metabolism and tolerance make it imperative to study sex-specific disparities within COVID-19 treatment efficacy [155,156]. Considering that sex differences in cardiovascular drug responses have been reported, sex differences will be of special interest for treating COVID-19-related cardiovascular injury [154,157,158]. Lastly, cardiac abnormalities including myocarditis, fibrosis, edema and left and right ventricular dysfunction have been reported in recovered COVID-19 patients [[159], [160], [161]]. Although as of yet no sex differences were found in recovered COVID-19 patients, it has been reported previously that males and females exhibit different functional outcome and long-term mortality after myocarditis, cardiac arrest and thrombotic events [109,159,162,163]. Longitudinal follow-up studies will therefore be imperative to gain more insight into the long-term cardiovascular effects and recovery in male and female COVID-19 patients.
Disclosures
None.
Acknowledgments
M.E. is supported by National Institutes of Health R01HL131182 and R01HL147586.
References
- 1.Xu Z., Shi L., Wang Y., Zhang J., Huang L., Zhang C. Pathological findings of COVID-19 associated with acute respiratory distress syndrome. Lancet Respir. Med. 2020;8:420–422. doi: 10.1016/S2213-2600(20)30076-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Huang C., Wang Y., Li X., Ren L., Zhao J., Hu Y. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395:497–506. doi: 10.1016/S0140-6736(20)30183-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Chen N., Zhou M., Dong X., Qu J., Gong F., Han Y. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study. Lancet. 2020;395:507–513. doi: 10.1016/S0140-6736(20)30211-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Zhou F., Yu T., Du R., Fan G., Liu Y., Liu Z. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet. 2020;395:1054–1062. doi: 10.1016/S0140-6736(20)30566-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Wang D., Hu B., Hu C., Zhu F., Liu X., Zhang J. Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus–infected pneumonia in Wuhan, China. JAMA. 2020;323:1061–1069. doi: 10.1001/jama.2020.1585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Aggarwal S., Garcia-Telles N., Aggarwal G., Lavie C., Lippi G., Henry B.M. Clinical features, laboratory characteristics, and outcomes of patients hospitalized with coronavirus disease 2019 (COVID-19): early report from the United States. Diagnosis. 2020;7:91–96. doi: 10.1515/dx-2020-0046. [DOI] [PubMed] [Google Scholar]
- 7.Iba T., Levy J.H., Levi M., Thachil J. Coagulopathy in COVID-19. J. Thromb. Haemost. 2020 doi: 10.1111/jth.14975. n.d.;n/a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Shen Chengxing, Junbo Ge. Epidemic of cardiovascular disease in China. Circulation. 2018;138:342–344. doi: 10.1161/CIRCULATIONAHA.118.033484. [DOI] [PubMed] [Google Scholar]
- 9.Wang Z., Chen Z., Zhang L., Wang X., Hao G., Zhang Z. Status of hypertension in China: results from the China hypertension survey, 2012–2015. Circulation. 2018;137:2344–2356. doi: 10.1161/CIRCULATIONAHA.117.032380. [DOI] [PubMed] [Google Scholar]
- 10.Li J.-W., Han T.-W., Woodward M., Anderson C.S., Zhou H., Chen Y.-D. The impact of 2019 novel coronavirus on heart injury: A systemic review and Meta-analysis. Prog. Cardiovasc. Dis. 2020 doi: 10.1016/j.pcad.2020.04.008. S0033–0620(20)30080–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Deng Q., Hu B., Zhang Y., Wang H., Zhou X., Hu W. Suspected myocardial injury in patients with COVID-19: Evidence from front-line clinical observation in Wuhan, China. Int. J. Cardiol. 2020 doi: 10.1016/j.ijcard.2020.03.087. S0167–5273(20)31115–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Shi S., Qin M., Shen B., Cai Y., Liu T., Yang F. Association of Cardiac Injury with Mortality in hospitalized patients with COVID-19 in Wuhan, China. JAMA Cardiol. 2020 doi: 10.1001/jamacardio.2020.0950. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Shi S., Qin M., Cai Y., Liu T., Shen B., Yang F. Characteristics and clinical significance of myocardial injury in patients with severe coronavirus disease 2019. Eur. Heart J. 2020 doi: 10.1093/eurheartj/ehaa408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Gebhard C., Regitz-Zagrosek V., Neuhauser H.K., Morgan R., Klein S.L. Impact of sex and gender on COVID-19 outcomes in Europe. Biol. Sex Differ. 2020;11:29. doi: 10.1186/s13293-020-00304-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Jin J.-M., Bai P., He W., Wu F., Liu X.-F., Han D.-M. Gender differences in patients with COVID-19: focus on severity and mortality. Front. Public Health. 2020;8 doi: 10.3389/fpubh.2020.00152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ghazizadeh Z., Majd H., Richter M., Samuel R., Zekavat S.M., Asgharian H. Androgen regulates SARS-CoV-2 receptor levels and is associated with severe COVID-19 symptoms in men. BioRxiv. 2020 doi: 10.1101/2020.05.12.091082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Emami A., Javanmardi F., Pirbonyeh N., Akbari A. Prevalence of underlying diseases in hospitalized patients with COVID-19: a systematic review and meta-analysis. Arch. Acad. Emerg. Med. 2020;8 [PMC free article] [PubMed] [Google Scholar]
- 18.Sandberg K., Ji H. Sex differences in primary hypertension. Biol. Sex Differ. 2012;3:7. doi: 10.1186/2042-6410-3-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Wake R., Yoshiyama M. Gender differences in ischemic heart disease. Recent Pat. Cardiovasc. Drug Discov. 2009;4:234–240. doi: 10.2174/157489009789152249. [DOI] [PubMed] [Google Scholar]
- 20.Aggarwal Niti R., Patel Hena N., Mehta Laxmi S., Sanghani Rupa M., Lundberg Gina P., Lewis Sandra J. Sex differences in ischemic heart disease. Circulation. 2018;11 doi: 10.1161/CIRCOUTCOMES.117.004437. [DOI] [PubMed] [Google Scholar]
- 21.Lam C.S.P., Arnott C., Beale A.L., Chandramouli C., Hilfiker-Kleiner D., Kaye D.M. Sex differences in heart failure. Eur. Heart J. 2019;40:3859–3868. doi: 10.1093/eurheartj/ehz835. [DOI] [PubMed] [Google Scholar]
- 22.Ashkan Ehdaie, Eugenio Cingolani, Michael Shehata, Wang Xunzhang, Curtis Anne B., Chugh Sumeet S. Sex differences in cardiac arrhythmias. Circ. Arrhythm. Electrophysiol. 2018;11 doi: 10.1161/CIRCEP.117.005680. e005680. [DOI] [PubMed] [Google Scholar]
- 23.Wong J.H., Dukes J., Levy R.E., Sos B., Mason S.E., Fong T.S. Sex differences in thrombosis in mice are mediated by sex-specific growth hormone secretion patterns. J. Clin. Invest. 2008;118:2969–2978. doi: 10.1172/JCI34957. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Iorga A., Cunningham C.M., Moazeni S., Ruffenach G., Umar S., Eghbali M. The protective role of estrogen and estrogen receptors in cardiovascular disease and the controversial use of estrogen therapy. Biol. Sex Differ. 2017;8:33. doi: 10.1186/s13293-017-0152-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Mozaffarian D., Benjamin E.J., Go A.S., Arnett D.K., Blaha M.J., Cushman M. Executive summary: heart disease and stroke statistics-2014;2016 update. Circulation. 2016;133:447–454. doi: 10.1161/CIR.0000000000000366. [DOI] [PubMed] [Google Scholar]
- 26.Arnold A.P., Cassis L.A., Eghbali M., Reue K., Sandberg K. Sex hormones and sex chromosomes cause sex differences in the development of cardiovascular diseases. Arterioscler. Thromb. Vasc. Biol. 2017 doi: 10.1161/ATVBAHA.116.307301. ATVBAHA.116.307301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Snell D.M., Turner J.M.A. Sex chromosome effects on male–female differences in mammals. Curr. Biol. 2018;28:R1313–R1324. doi: 10.1016/j.cub.2018.09.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Arnold A.P., Reue K., Eghbali M., Vilain E., Chen X., Ghahramani N. The importance of having two X chromosomes. Philos. Trans. R Soc. Lond., B, Biol. Sci. 2016;371 doi: 10.1098/rstb.2015.0113. 20150113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.AlSiraj Y., Chen X., Thatcher S.E., Temel R.E., Cai L., Blalock E. XX sex chromosome complement promotes atherosclerosis in mice. Nat. Commun. 2019;10 doi: 10.1038/s41467-019-10462-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Li J., Chen X., McClusky R., Ruiz-Sundstrom M., Itoh Y., Umar S. The number of X chromosomes influences protection from cardiac ischaemia/reperfusion injury in mice: one X is better than two. Cardiovasc. Res. 2014;102:375–384. doi: 10.1093/cvr/cvu064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Li W., Moore M.J., Vasilieva N., Sui J., Wong S.K., Berne M.A. Angiotensin-converting enzyme 2 is a functional receptor for the SARS coronavirus. Nature. 2003;426:450–454. doi: 10.1038/nature02145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Yan R., Zhang Y., Li Y., Xia L., Guo Y., Zhou Q. Structural basis for the recognition of SARS-CoV-2 by full-length human ACE2. Science. 2020;367:1444. doi: 10.1126/science.abb2762. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Rice G.I., Thomas D.A., Grant P.J., Turner A.J., Hooper N.M. Evaluation of angiotensin-converting enzyme (ACE), its homologue ACE2 and neprilysin in angiotensin peptide metabolism. Biochem. J. 2004;383:45–51. doi: 10.1042/BJ20040634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Patel V.B., Zhong J.-C., Grant M.B., Oudit G.Y. Role of the ACE2/angiotensin 1-7 Axis of the renin-angiotensin system in heart failure. Circ. Res. 2016;118:1313–1326. doi: 10.1161/CIRCRESAHA.116.307708. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.JiuChang Zhong, Ratnadeep Basu, Guo Danny. Chow Fung L., Byrns Simon, Schuster Manfred, et al. angiotensin-converting enzyme 2 suppresses pathological hypertrophy, myocardial fibrosis, and cardiac dysfunction. Circulation. 2010;122:717–728. doi: 10.1161/CIRCULATIONAHA.110.955369. [DOI] [PubMed] [Google Scholar]
- 36.Crackower M.A., Sarao R., Oudit G.Y., Yagil C., Kozieradzki I., Scanga S.E. Angiotensin-converting enzyme 2 is an essential regulator of heart function. Nature. 2002;417:822–828. doi: 10.1038/nature00786. [DOI] [PubMed] [Google Scholar]
- 37.Tucker N.R., Chaffin M., Bedi K.C., Papangeli I., Akkad A.-D., Arduini A. Myocyte specific upregulation of ACE2 in cardiovascular disease: implications for SARS-CoV-2 mediated myocarditis. MedRxiv. 2020 doi: 10.1101/2020.04.09.20059204. 2020.04.09.20059204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Zisman Lawrence S., Keller Rebecca S., Barbara Weaver, Lin Qishan, Robert Speth, Bristow Michael R. Increased angiotensin-(1–7)–forming activity in failing human heart ventricles. Circulation. 2003;108:1707–1712. doi: 10.1161/01.CIR.0000094734.67990.99. [DOI] [PubMed] [Google Scholar]
- 39.Yang J., Feng X., Zhou Q., Cheng W., Shang C., Han P. Pathological Ace2-to-ace enzyme switch in the stressed heart is transcriptionally controlled by the endothelial Brg1-FoxM1 complex. Proc. Natl. Acad. Sci. U. S. A. 2016;113:E5628–E5635. doi: 10.1073/pnas.1525078113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Burrell L.M., Risvanis J., Kubota E., Dean R.G., MacDonald P.S., Lu S. Myocardial infarction increases ACE2 expression in rat and humans. Eur. Heart J. 2005;26:369–375. doi: 10.1093/eurheartj/ehi114. [DOI] [PubMed] [Google Scholar]
- 41.Nicin L., Abplanalp W.T., Mellentin H., Kattih B., Tombor L., John D. Cell type-specific expression of the putative SARS-CoV-2 receptor ACE2 in human hearts. Eur. Heart J. 2020 doi: 10.1093/eurheartj/ehaa311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Guo J., Wei X., Li Q., Li L., Yang Z., Shi Y. Single-cell RNA analysis on ACE2 expression provides insights into SARS-CoV-2 potential entry into the bloodstream and heart injury. J. Cell. Physiol. 2020 doi: 10.1002/jcp.29802. n.d.;n/a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.A Human Homolog of Angiotensin-converting Enzyme. https://www.jbc.org/content/275/43/33238.short n.d.
- 44.Tukiainen T., Villani A.-C., Yen A., Rivas M.A., Marshall J.L., Satija R. Landscape of X chromosome inactivation across human tissues. Nature. 2017;550:244–248. doi: 10.1038/nature24265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Cunningham C.M., Eghbali M. An introduction to epigenetics in cardiovascular development, disease, and sexualization. Adv. Exp. Med. Biol. 2018;1065:31–47. doi: 10.1007/978-3-319-77932-4_2. [DOI] [PubMed] [Google Scholar]
- 46.Ji H., Menini S., Zheng W., Pesce C., Wu X., Sandberg K. Role of angiotensin-converting enzyme 2 and angiotensin(1-7) in 17beta-oestradiol regulation of renal pathology in renal wrap hypertension in rats. Exp. Physiol. 2008;93:648–657. doi: 10.1113/expphysiol.2007.041392. [DOI] [PubMed] [Google Scholar]
- 47.Gupte M., Thatcher S.E., Boustany-Kari C.M., Shoemaker R., Yiannikouris F., Zhang X. Angiotensin converting enzyme 2 contributes to sex differences in the development of obesity hypertension in C57BL/6 mice. Arterioscler. Thromb. Vasc. Biol. 2012;32:1392–1399. doi: 10.1161/ATVBAHA.112.248559. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Pendergrass K.D., Pirro N.T., Westwood B.M., Ferrario C.M., Brosnihan K.B., Chappell M.C. Sex differences in circulating and renal angiotensins of hypertensive mRen.Lewis but not normotensive Lewis rats. Am. J. Physiol. Heart Circ. Physiol. 2008;295:H10–H20. doi: 10.1152/ajpheart.01277.2007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Dalpiaz P.L.M., Lamas A.Z., Caliman I.F., Ribeiro R.F., Abreu G.R., Moyses M.R. Sex hormones promote opposite effects on ACE and ACE2 activity, hypertrophy and cardiac contractility in spontaneously hypertensive rats. PLoS One. 2015;10 doi: 10.1371/journal.pone.0127515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Liu J., Ji H., Zheng W., Wu X., Zhu J.J., Arnold A.P. Sex differences in renal angiotensin converting enzyme 2 (ACE2) activity are 17β-oestradiol-dependent and sex chromosome-independent. Biol. Sex Differ. 2010;1:6. doi: 10.1186/2042-6410-1-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Yoshida H., Rosano G., Shimizu M., Mochizuki S., Yoshimura M. Gender differences in the effects of angiotensin receptor blockers on cardiovascular disease. Curr. Pharm. Des. 2011;17:1090–1094. doi: 10.2174/138161211795656909. [DOI] [PubMed] [Google Scholar]
- 52.Hudson M., Rahme E., Behlouli H., Sheppard R., Pilote L. Sex differences in the effectiveness of angiotensin receptor blockers and angiotensin converting enzyme inhibitors in patients with congestive heart failure — a population study. Eur. J. Heart Fail. 2007;9:602–609. doi: 10.1016/j.ejheart.2007.02.001. [DOI] [PubMed] [Google Scholar]
- 53.Santema B.T., Ouwerkerk W., Tromp J., Sama I.E., Ravera A., Regitz-Zagrosek V. Identifying optimal doses of heart failure medications in men compared with women: a prospective, observational, cohort study. Lancet. 2019;394:1254–1263. doi: 10.1016/S0140-6736(19)31792-1. [DOI] [PubMed] [Google Scholar]
- 54.Whitley H.P., Lindsey W. Sex-based differences in drug activity. AFP. 2009;80:1254–1258. [PubMed] [Google Scholar]
- 55.Ferrario Carlos M. Jessup Jewell, Chappell mark C., Averill David B., Brosnihan K. Bridget, Tallant E. Ann, et al. effect of angiotensin-converting enzyme inhibition and angiotensin II receptor blockers on cardiac angiotensin-converting enzyme 2. Circulation. 2005;111:2605–2610. doi: 10.1161/CIRCULATIONAHA.104.510461. [DOI] [PubMed] [Google Scholar]
- 56.Paz Ocaranza María, Ivan Godoy, Jalil Jorge E., Manuel Varas, Patricia Collantes, Melissa Pinto. Enalapril Attenuates Downregulation of Angiotensin-Converting Enzyme 2 in the Late Phase of Ventricular Dysfunction in Myocardial Infarcted Rat. Hypertension. 2006;48:572–578. doi: 10.1161/01.HYP.0000237862.94083.45. [DOI] [PubMed] [Google Scholar]
- 57.Vaduganathan M., Vardeny O., Michel T., McMurray J.J.V., Pfeffer M.A., Solomon S.D. Renin–angiotensin–aldosterone system inhibitors in patients with Covid-19. N. Engl. J. Med. 2020;382:1653–1659. doi: 10.1056/NEJMsr2005760. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Reynolds H.R., Adhikari S., Pulgarin C., Troxel A.B., Iturrate E., Johnson S.B. Renin–angiotensin–aldosterone system inhibitors and risk of Covid-19. N. Engl. J. Med. 2020 doi: 10.1056/NEJMoa2008975. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Caussy C., Pattou F., Wallet F., Simon C., Chalopin S., Telliam C. Prevalence of obesity among adult inpatients with COVID-19 in France. Lancet Diabetes Endocrinol. 2020;8:562–564. doi: 10.1016/S2213-8587(20)30160-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Palaiodimos L., Kokkinidis D.G., Li W., Karamanis D., Ognibene J., Arora S. Severe obesity, increasing age and male sex are independently associated with worse in-hospital outcomes, and higher in-hospital mortality, in a cohort of patients with COVID-19 in the Bronx, New York. Metabolism. 2020;108:154262. doi: 10.1016/j.metabol.2020.154262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Cai Q., Chen F., Wang T., Luo F., Liu X., Wu Q. Obesity and COVID-19 severity in a designated Hospital in Shenzhen, China. Diabetes Care. 2020;43:1392–1398. doi: 10.2337/dc20-0576. [DOI] [PubMed] [Google Scholar]
- 62.Suleyman G., Fadel R.A., Malette K.M., Hammond C., Abdulla H., Entz A. Clinical characteristics and morbidity associated with coronavirus disease 2019 in a series of patients in metropolitan Detroit. JAMA Netw. Open. 2020;3 doi: 10.1001/jamanetworkopen.2020.12270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Busetto L., Bettini S., Fabris R., Serra R., Dal Pra’ C., Maffei P. Obesity and COVID-19: an Italian snapshot. Obesity (Silver Spring) 2020 doi: 10.1002/oby.22918. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Hubert H.B., Feinleib M., McNamara P.M., Castelli W.P. Obesity as an independent risk factor for cardiovascular disease: a 26-year follow-up of participants in the Framingham heart study. Circulation. 1983;67:968–977. doi: 10.1161/01.CIR.67.5.968. [DOI] [PubMed] [Google Scholar]
- 65.Zore T., Palafox M., Reue K. Sex differences in obesity, lipid metabolism, and inflammation—a role for the sex chromosomes? Mol. Metab. 2018;15:35–44. doi: 10.1016/j.molmet.2018.04.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Lee A., Cardel M., Donahoo W.T. Social and environmental factors influencing obesity. In: Feingold K.R., Anawalt B., Boyce A., Chrousos G., Dungan K., Grossman A., editors. Endotext. MDText.com, Inc.; South Dartmouth (MA): 2000. [Google Scholar]
- 67.Akoumianakis I., Filippatos T. The renin-angiotensin-aldosterone system as a link between obesity and coronavirus disease 2019 severity. Obes. Rev. 2020 doi: 10.1111/obr.13077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Cai H. Sex difference and smoking predisposition in patients with COVID-19. Lancet Respir. Med. 2020;8 doi: 10.1016/S2213-2600(20)30117-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Nan Y., Xi Z., Yang Y., Wang L.L., Tu M.W., Wang J.J. The 2015 China adult tobacco survey: exposure to second-hand smoke among adults aged 15 and above and their support to policy on banning smoking in public places. Zhonghua Liu Xing Bing Xue Za Zhi. 2016;37:810–815. doi: 10.3760/cma.j.issn.0254-6450.2016.06.014. [DOI] [PubMed] [Google Scholar]
- 70.Lugo A., Zuccaro P., Pacifici R., Gorini G., Colombo P., La Vecchia C. Smoking in Italy in 2015-2016: prevalence, trends, roll-your-own cigarettes, and attitudes towards incoming regulations. Tumori. 2017;103:353–359. doi: 10.5301/tj.5000644. [DOI] [PubMed] [Google Scholar]
- 71.Jamal A., Phillips E., Gentzke A.S., Homa D.M., Babb S.D., King B.A. Current cigarette smoking among adults — United States, 2016. MMWR Morb. Mortal. Wkly Rep. 2018;67:53–59. doi: 10.15585/mmwr.mm6702a1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Prevention (US) C for DC and, Promotion (US) NC for CDP and H, Health (US) O on S and. Cardiovascular Diseases . 2010. Centers for Disease Control and Prevention (US) [Google Scholar]
- 73.Single-Cell RNA Expression Profiling of ACE2, the Putative Receptor of Wuhan 2019-nCov | bioRxiv. 2020. n.d. (accessed May 7, 2020) [DOI] [Google Scholar]
- 74.Akbarshakh Akhmerov, Eduardo Marbán. COVID-19 and the heart. Circ. Res. 2020;126:1443–1455. doi: 10.1161/CIRCRESAHA.120.317055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Colling M.E., Kanthi Y. COVID-19-associated coagulopathy: An exploration of mechanisms. Vasc. Med. 2020 doi: 10.1177/1358863X20932640. 1358863X20932640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Hendren Nicholas S., Drazner Mark H., Biykem Bozkurt, Cooper L.T., Jr. Description and proposed management of the acute COVID-19 cardiovascular syndrome. Circulation. 2020;0 doi: 10.1161/CIRCULATIONAHA.120.047349. n.d. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Lippi G., Lavie C.J., Sanchis-Gomar F. Cardiac troponin I in patients with coronavirus disease 2019 (COVID-19): Evidence from a meta-analysis. Prog. Cardiovasc. Dis. 2020 doi: 10.1016/j.pcad.2020.03.001. (S0033–0620(20)30055–4) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Toraih E.A., Elshazli R.M., Hussein M.H., Elgaml A., Amin M.N., El-Mowafy M. Association of cardiac biomarkers and comorbidities with increased mortality, severity, and cardiac injury in COVID-19 patients: A meta-regression and Decision tree analysis. J. Med. Virol. 2020 doi: 10.1002/jmv.26166. n.d.;n/a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Han H., Xie L., Liu R., Yang J., Liu F., Wu K. Analysis of heart injury laboratory parameters in 273 COVID-19 patients in one hospital in Wuhan, China. J. Med. Virol. 2020 doi: 10.1002/jmv.25809. n/a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Lala A., Johnson K.W., Januzzi J.L., Russak A.J., Paranjpe I., Richter F. Prevalence and impact of myocardial injury in patients hospitalized with COVID-19 infection. J. Am. Coll. Cardiol. 2020 doi: 10.1016/j.jacc.2020.06.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Guo T., Fan Y., Chen M., Wu X., Zhang L., He T. Cardiovascular Implications of Fatal Outcomes of Patients With Coronavirus Disease 2019 (COVID-19) JAMA Cardiol. 2020 doi: 10.1001/jamacardio.2020.1017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Gopinathannair R., Merchant F.M., Lakkireddy D.R., Etheridge S.P., Feigofsky S., Han J.K. COVID-19 and cardiac arrhythmias: a global perspective on arrhythmia characteristics and management strategies. J. Interv. Card. Electrophysiol. 2020 doi: 10.1007/s10840-020-00789-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Beri A., Kotak K. Cardiac injury, arrhythmia, and sudden death in a COVID-19 patient. HeartRhythm Case Rep. 2020;6:367–369. doi: 10.1016/j.hrcr.2020.05.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Shirazi S., Mami S., Mohtadi N., Ghaysouri A., Tavan H., Nazari A. Sudden cardiac death in COVID-19 patients, a report of three cases. Futur. Cardiol. 2020 doi: 10.2217/fca-2020-0082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Victor Waldmann, Xavier Jouven, Kumar Narayanan, Olivier Piot, Chugh Sumeet S., Albert Christine M. Association between atrial fibrillation and sudden cardiac death. Circ. Res. 2020;127:301–309. doi: 10.1161/CIRCRESAHA.120.316756. [DOI] [PubMed] [Google Scholar]
- 86.Liu Q., Chen H., Zeng Q. Clinical characteristics of COVID-19 patients with complication of cardiac arrhythmia. J. Inf. Secur. 2020 doi: 10.1016/j.jinf.2020.07.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Kochi A.N., Tagliari A.P., Forleo G.B., Fassini G.M., Tondo C. Cardiac and arrhythmic complications in patients with COVID-19. J. Cardiovasc. Electrophysiol. 2020;31:1003–1008. doi: 10.1111/jce.14479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Bhatla A., Mayer M.M., Adusumalli S., Hyman M.C., Oh E., Tierney A. COVID-19 and cardiac arrhythmias. Heart Rhythm. 2020 doi: 10.1016/j.hrthm.2020.06.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Du Y., Tu L., Zhu P., Mu M., Wang R., Yang P. Clinical features of 85 fatal cases of COVID-19 from Wuhan. A retrospective observational study. Am. J. Respir. Crit. Care Med. 2020;201:1372–1379. doi: 10.1164/rccm.202003-0543OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Linde C., Bongiorni M.G., Birgersdotter-Green U., Curtis A.B., Deisenhofer I., Furokawa T. Sex differences in cardiac arrhythmia: a consensus document of the European Heart Rhythm Association, endorsed by the Heart Rhythm Society and Asia Pacific Heart Rhythm Society. Europace. 2018;20 doi: 10.1093/europace/euy067. 1565–1565ao. [DOI] [PubMed] [Google Scholar]
- 91.Levi M., Thachil J., Iba T., Levy J.H. Coagulation abnormalities and thrombosis in patients with COVID-19. Lancet Haematol. 2020;7:e438–e440. doi: 10.1016/S2352-3026(20)30145-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Tang N., Li D., Wang X., Sun Z. Abnormal coagulation parameters are associated with poor prognosis in patients with novel coronavirus pneumonia. J. Thromb. Haemost. 2020;18:844–847. doi: 10.1111/jth.14768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Magro C., Mulvey J.J., Berlin D., Nuovo G., Salvatore S., Harp J. Complement associated microvascular injury and thrombosis in the pathogenesis of severe COVID-19 infection: a report of five cases. Transl. Res. 2020;220:1–13. doi: 10.1016/j.trsl.2020.04.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Ackermann M., Verleden S.E., Kuehnel M., Haverich A., Welte T., Laenger F. Pulmonary vascular endothelialitis, thrombosis, and angiogenesis in Covid-19. N. Engl. J. Med. 2020;0 doi: 10.1056/NEJMoa2015432. null. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Chibane S., Gibeau G., Poulin F., Tessier P., Goulet M., Carrier M. Hyperacute multi-organ thromboembolic storm in COVID-19: a case report. J. Thromb. Thrombolysis. 2020:1–4. doi: 10.1007/s11239-020-02173-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Lorenzo C., Francesca B., Francesco P., Elena C., Luca S., Paolo S. Acute pulmonary embolism in COVID-19 related hypercoagulability. J. Thromb. Thrombolysis. 2020;50:223–226. doi: 10.1007/s11239-020-02160-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Middeldorp S., Coppens M., van Haaps T.F., Foppen M., Vlaar A.P., MCA Müller. Incidence of venous thromboembolism in hospitalized patients with COVID-19. J. Thromb. Haemost. 2020 doi: 10.1111/jth.14888. n.d.;n/a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.D-Dimer as a Biomarker for Disease Severity and Mortality in COVID-19 Patients: a Case Control Study. 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Shah S., Shah K., Patel S.B., Patel F.S., Osman M., Velagapudi P. Elevated D-dimer levels are associated with increased risk of mortality in COVID-19: a systematic review and meta-analysis. Cardiovasc. Med. 2020 doi: 10.1101/2020.04.29.20085407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Di Micco P., Russo V., Carannante N., Imparato M., Rodolfi S., Cardillo G. Clotting factors in COVID-19: epidemiological association and prognostic values in different clinical presentations in an Italian cohort. J. Clin. Med. 2020;9 doi: 10.3390/jcm9051371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Oudit G.Y., Kassiri Z., Patel M.P., Chappell M., Butany J., Backx P.H. Angiotensin II-mediated oxidative stress and inflammation mediate the age-dependent cardiomyopathy in ACE2 null mice. Cardiovasc. Res. 2007;75:29–39. doi: 10.1016/j.cardiores.2007.04.007. [DOI] [PubMed] [Google Scholar]
- 102.Zhou G., Zhao J., Wang S. Pathological study of impact of SARS coronavirus on heart and its conduction system in SARS patients. Med. J. Chin. People’s Liberation Army. 1982;0(01) (n.d) [Google Scholar]
- 103.Tavazzi G., Pellegrini C., Maurelli M., Belliato M., Sciutti F., Bottazzi A. Myocardial localization of coronavirus in COVID-19 cardiogenic shock. Eur. J. Heart Fail. 2020 doi: 10.1002/ejhf.1828. n/a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Escher F., Pietsch H., Aleshcheva G., Bock T., Baumeier C., Elsaesser A. Detection of viral SARS-CoV-2 genomes and histopathological changes in endomyocardial biopsies. ESC Heart Fail. 2020 doi: 10.1002/ehf2.12805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Yao X.H., Li T.Y., He Z.C., Ping Y.F., Liu H.W., Yu S.C. A pathological report of three COVID-19 cases by minimally invasive autopsies. Zhonghua Bing Li Xue Za Zhi. 2020;49 doi: 10.3760/cma.j.cn112151-20200312-00193. [DOI] [PubMed] [Google Scholar]
- 106.Wenzel P., Kopp S., Göbel S., Jansen T., Geyer M., Hahn F. Evidence of SARS-CoV-2 mRNA in endomyocardial biopsies of patients with clinically suspected myocarditis tested negative for COVID-19 in nasopharyngeal swab. Cardiovasc. Res. 2020 doi: 10.1093/cvr/cvaa160. n.d. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Chen L., Li X., Chen M., Feng Y., Xiong C. The ACE2 expression in human heart indicates new potential mechanism of heart injury among patients infected with SARS-CoV-2. Cardiovasc. Res. 2020;116:1097–1100. doi: 10.1093/cvr/cvaa078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Sharma A., Garcia G., Arumugaswami V., Svendsen C.N. Human iPSC-derived Cardiomyocytes are susceptible to SARS-CoV-2 infection. Cell Biol. 2020 doi: 10.1101/2020.04.21.051912. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Fairweather D., Cooper L.T., Blauwet L.A. Sex and gender differences in myocarditis and dilated cardiomyopathy. Curr. Probl. Cardiol. 2013;38:7–46. doi: 10.1016/j.cpcardiol.2012.07.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Carta K.G., Britto I.J.M., Meza Y., Morr I., Marques J., Flores V.F. Sex and gender differences in Zika myocarditis. J. Am. Coll. Cardiol. 2019;73:719. doi: 10.1016/S0735-1097(19)31327-0. [DOI] [Google Scholar]
- 111.Koenig A., Sateriale A., Budd R.C., Huber S.A., Buskiewicz I.A. The role of sex differences in autophagy in the heart during coxsackievirus B3 induced myocarditis. J. Cardiovasc. Transl. Res. 2014;7:182–191. doi: 10.1007/s12265-013-9525-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Teuwen L.-A., Geldhof V., Pasut A., Carmeliet P. COVID-19: the vasculature unleashed. Nat. Rev. Immunol. 2020:1–3. doi: 10.1038/s41577-020-0343-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Varga Z., Flammer A.J., Steiger P., Haberecker M., Andermatt R., Zinkernagel A.S. Endothelial cell infection and endotheliitis in COVID-19. Lancet. 2020;395:1417–1418. doi: 10.1016/S0140-6736(20)30937-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Monteil V., Kwon H., Prado P., Hagelkrüys A., Wimmer R.A., Stahl M. Inhibition of SARS-CoV-2 infections in engineered human tissues using clinical-grade soluble human ACE2. Cell. 2020 doi: 10.1016/j.cell.2020.04.004. S0092–8674(20)30399–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Stanhewicz A.E., Wenner M.M., Stachenfeld N.S. Sex differences in endothelial function important to vascular health and overall cardiovascular disease risk across the lifespan. Am. J. Phys. Heart Circ. Phys. 2018;315:H1569–H1588. doi: 10.1152/ajpheart.00396.2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Green S.J. Covid-19 accelerates endothelial dysfunction and nitric oxide deficiency. Microbes Infect. 2020;22:149–150. doi: 10.1016/j.micinf.2020.05.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Gupta Nandita C., Davis Catherine M., Nelson Jonathan W., Young Jennifer M., Alkayed Nabil J. Soluble Epoxide Hydrolase. Arterioscler. Thromb. Vasc. Biol. 2012;32:1936–1942. doi: 10.1161/ATVBAHA.112.251520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Wang J., Bingaman S., Huxley V.H. Intrinsic sex-specific differences in microvascular endothelial cell phosphodiesterases. Am. J. Phys. Heart Circ. Phys. 2010;298:H1146–H1154. doi: 10.1152/ajpheart.00252.2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Wang H., Yang P., Liu K., Guo F., Zhang Y., Zhang G. SARS coronavirus entry into host cells through a novel clathrin- and caveolae-independent endocytic pathway. Cell Res. 2008;18:290–301. doi: 10.1038/cr.2008.15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Oudit G.Y., Kassiri Z., Jiang C., Liu P.P., Poutanen S.M., Penninger J.M. SARS-coronavirus modulation of myocardial ACE2 expression and inflammation in patients with SARS. Eur. J. Clin. Investig. 2009;39:618–625. doi: 10.1111/j.1365-2362.2009.02153.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Fraga-Silva R.A., Costa-Fraga F.P., Murça T.M., Moraes P.L., Martins Lima A., Lautner R.Q. Angiotensin-converting enzyme 2 activation improves endothelial function. Hypertension. 2013;61:1233–1238. doi: 10.1161/HYPERTENSIONAHA.111.00627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Lovren F., Pan Y., Quan A., Teoh H., Wang G., Shukla P.C. Angiotensin converting enzyme-2 confers endothelial protection and attenuates atherosclerosis. Am. J. Phys. Heart Circ. Phys. 2008;295:H1377–H1384. doi: 10.1152/ajpheart.00331.2008. [DOI] [PubMed] [Google Scholar]
- 123.Fraga-Silva R.A., Sorg B.S., Wankhede M., Dedeugd C., Jun J.Y., Baker M.B. ACE2 activation promotes antithrombotic activity. Mol. Med. 2010;16:210–215. doi: 10.2119/molmed.2009.00160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Epelman S., Tang W.H.W., Chen S.Y., Van Lente F., Francis G.S., Sen S. Detection of soluble angiotensin-converting enzyme 2 in heart failure: insights into the endogenous counter-regulatory pathway of the renin-angiotensin-aldosterone system. J. Am. Coll. Cardiol. 2008;52:750–754. doi: 10.1016/j.jacc.2008.02.088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Swärd P., Edsfeldt A., Reepalu A., Jehpsson L., Rosengren B.E., Karlsson M.K. Age and sex differences in soluble ACE2 may give insights for COVID-19. Crit. Care. 2020;24 doi: 10.1186/s13054-020-02942-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Sama I.E., Ravera A., Santema B.T., van Goor H., ter Maaten J.M., Cleland J.G.F. Circulating plasma concentrations of angiotensin-converting enzyme 2 in men and women with heart failure and effects of renin–angiotensin–aldosterone inhibitors. Eur. Heart J. 2020;41:1810–1817. doi: 10.1093/eurheartj/ehaa373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Ruan Q., Yang K., Wang W., Jiang L., Song J. Clinical predictors of mortality due to COVID-19 based on an analysis of data of 150 patients from Wuhan, China. Intensive Care Med. 2020:1–3. doi: 10.1007/s00134-020-05991-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Shimabukuro-Vornhagen A., Gödel P., Subklewe M., Stemmler H.J., Schlößer H.A., Schlaak M. Cytokine release syndrome. J. Immunother. Cancer. 2018;6 doi: 10.1186/s40425-018-0343-9. 56–56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Alvi R.M., Frigault M.J., Fradley M.G., Jain M.D., Mahmood S.S., Awadalla M. Cardiovascular events among adults treated with chimeric antigen receptor T-cells (CAR-T) J. Am. Coll. Cardiol. 2019;74:3099–3108. doi: 10.1016/j.jacc.2019.10.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Lazzerini P.E., Acampa M., Laghi-Pasini F., Bertolozzi I., Finizola F., Vanni F. Cardiac arrest risk during acute infections: systemic inflammation directly prolongs QTc interval via cytokine-mediated effects on Potassium Channel expression. Circ. Arrhythm. Electrophysiol. 2020 doi: 10.1161/CIRCEP.120.008627. [DOI] [PubMed] [Google Scholar]
- 131.van der Poll T., de Jonge E., An Ten C.H. Madame Curie Bioscience Database [Internet] Landes Bioscience; Austin (TX): 2000-2013. Cytokines as Regulators of Coagulation.https://www.ncbi.nlm.nih.gov/books/NBK6207/ Available from: [Google Scholar]
- 132.Ghosh S., Klein R.S. Sex drives dimorphic immune responses to viral infections. J. Immunol. 2017;198:1782–1790. doi: 10.4049/jimmunol.1601166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Vom Steeg L.G., Klein S.L. SeXX matters in infectious disease pathogenesis. PLoS Pathog. 2016:12. doi: 10.1371/journal.ppat.1005374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Klein S.L., Jedlicka A., Pekosz A. The Xs and Y of immune responses to viral vaccines. Lancet Infect. Dis. 2010;10:338–349. doi: 10.1016/S1473-3099(10)70049-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Berghöfer B., Frommer T., Haley G., Fink L., Bein G., Hackstein H. TLR7 ligands induce higher IFN-alpha production in females. J. Immunol. 2006;177:2088–2096. doi: 10.4049/jimmunol.177.4.2088. [DOI] [PubMed] [Google Scholar]
- 136.Fischer J., Jung N., Robinson N., Lehmann C. Sex differences in immune responses to infectious diseases. Infection. 2015;43:399–403. doi: 10.1007/s15010-015-0791-9. [DOI] [PubMed] [Google Scholar]
- 137.Stamova B., Tian Y., Jickling G., Bushnell C., Zhan X., Liu D. The X-chromosome has a different pattern of gene expression in women compared with men with ischemic stroke. Stroke. 2012;43:326–334. doi: 10.1161/STROKEAHA.111.629337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Conti P., Younes A. Coronavirus COV-19/SARS-CoV-2 affects women less than men: clinical response to viral infection. J. Biol. Regul. Homeost. Agents. 2020;34 doi: 10.23812/Editorial-Conti-3. [DOI] [PubMed] [Google Scholar]
- 139.Meester I., Manilla-Muñoz E., León-Cachón R.B.R., Paniagua-Frausto G.A., Carrión-Alvarez D., Ruiz-Rodríguez C.O. SeXY chromosomes and the immune system: reflections after a comparative study. Biol. Sex Differ. 2020;11:3. doi: 10.1186/s13293-019-0278-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Spach K.M., Blake M., Bunn J.Y., McElvany B., Noubade R., Blankenhorn E.P. Cutting edge: the Y chromosome controls the age-dependent experimental allergic encephalomyelitis sexual dimorphism in SJL/J mice. J. Immunol. 2009;182:1789–1793. doi: 10.4049/jimmunol.0803200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Channappanavar R., Fett C., Mack M., Ten Eyck P.P., Meyerholz D.K., Perlman S. Sex-based differences in susceptibility to severe acute respiratory syndrome coronavirus infection. J. Immunol. 2017;198:4046–4053. doi: 10.4049/jimmunol.1601896. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Jansen A., Chiew M., Konings F., Lee C.-K., Ailan L. Sex matters – a preliminary analysis of Middle East respiratory syndrome in the Republic of Korea, 2015. Western Pac. Surveill. Response J. 2015;6:68–71. doi: 10.5365/WPSAR.2015.6.3.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Qin L., Li X., Shi J., Yu M., Wang K., Tao Y. Gendered effects on inflammation reaction and outcome of COVID-19 patients in Wuhan. J. Med. Virol. 2020 doi: 10.1002/jmv.26137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Enea Lazzerini Pietro, Mohamed Boutjdir, Leopoldo Capecchi Pier. COVID-19, arrhythmic risk, and inflammation. Circulation. 2020;142:7–9. doi: 10.1161/CIRCULATIONAHA.120.047293. [DOI] [PubMed] [Google Scholar]
- 145.Wang M., Cao R., Zhang L., Yang X., Liu J., Xu M. Remdesivir and chloroquine effectively inhibit the recently emerged novel coronavirus (2019-nCoV) in vitro. Cell Res. 2020;30:269–271. doi: 10.1038/s41422-020-0282-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Gordon C.J., Tchesnokov E.P., Woolner E., Perry J.K., Feng J.Y., Porter D.P. Remdesivir is a direct-acting antiviral that inhibits RNA-dependent RNA polymerase from severe acute respiratory syndrome coronavirus 2 with high potency. J. Biol. Chem. 2020 doi: 10.1074/jbc.RA120.013679. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.Chorin E., Wadhwani L., Magnani S., Dai M., Shulman E., Nadeau-Routhier C. QT interval prolongation and torsade de pointes in patients with COVID-19 treated with hydroxychloroquine/azithromycin. Heart Rhythm. 2020 doi: 10.1016/j.hrthm.2020.05.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.Saleh M., Gabriels J., Chang D., Soo Kim B., Mansoor A., Mahmood E. Effect of Chloroquine, Hydroxychloroquine, and azithromycin on the corrected QT interval in patients with SARS-CoV-2 infection. Circ. Arrhythm. Electrophysiol. 2020;13 doi: 10.1161/CIRCEP.120.008662. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.van den Broek M.P.H., Möhlmann J.E., Abeln B.G.S., Liebregts M., van Dijk V.F., van de Garde E.M.W. Chloroquine-induced QTc prolongation in COVID-19 patients. Neth. Hear. J. 2020 doi: 10.1007/s12471-020-01429-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Mercuro N.J., Yen C.F., Shim D.J., Maher T.R., McCoy C.M., Zimetbaum P.J. Risk of QT interval prolongation associated with use of Hydroxychloroquine with or without concomitant azithromycin among hospitalized patients testing positive for coronavirus disease 2019 (COVID-19) JAMA Cardiol. 2020 doi: 10.1001/jamacardio.2020.1834. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151.Chorin E., Dai M., Shulman E., Wadhwani L., Bar-Cohen R., Barbhaiya C. The QT interval in patients with COVID-19 treated with hydroxychloroquine and azithromycin. Nat. Med. 2020;26:808–809. doi: 10.1038/s41591-020-0888-2. [DOI] [PubMed] [Google Scholar]
- 152.Rosenberg E.S., Dufort E.M., Udo T., Wilberschied L.A., Kumar J., Tesoriero J. Association of Treatment with Hydroxychloroquine or azithromycin with in-hospital mortality in patients with COVID-19 in New York state. JAMA. 2020;323:2493–2502. doi: 10.1001/jama.2020.8630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153.Varshneya M., Irurzun-Arana I., Campana C., Dariolli R., Gutierrez A., Pullinger T.K. Investigational treatments for COVID-19 may increase ventricular arrhythmia risk through drug interactions. Pharmacol. Ther. 2020 doi: 10.1101/2020.05.21.20109397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Murphy E., Steenbergen C. Sex, drugs, and trial design: sex influences the heart and drug responses. J. Clin. Invest. 2014;124:2375–2377. doi: 10.1172/JCI76262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155.Lythgoe M.P., Middleton P. Ongoing clinical trials for the management of the COVID-19 pandemic. Trends Pharmacol. Sci. 2020 doi: 10.1016/j.tips.2020.03.006. S0165–6147(20)30070–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156.Bischof E., Wolfe J., Klein S.L. Clinical trials for COVID-19 should include sex as a variable. J. Clin. Investig. 2020 doi: 10.1172/JCI139306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157.Sasaki H., Nagayama T., Blanton R.M., Seo K., Zhang M., Zhu G. PDE5 inhibitor efficacy is estrogen dependent in female heart disease. J. Clin. Invest. 2014;124:2464–2471. doi: 10.1172/JCI70731. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158.Tamargo J., Rosano G., Walther T., Duarte J., Niessner A., Kaski J.C. Gender differences in the effects of cardiovascular drugs. Eur. Heart J. Cardiovasc. Pharmacother. 2017;3:163–182. doi: 10.1093/ehjcvp/pvw042. [DOI] [PubMed] [Google Scholar]
- 159.Huang L., Zhao P., Tang D., Zhu T., Han R., Zhan C. Cardiac involvement in recovered COVID-19 patients identified by magnetic resonance imaging. J. Am. Coll. Cardiol. Img. 2020 doi: 10.1016/j.jcmg.2020.05.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160.Sardari A., Tabarsi P., Borhany H., Mohiaddin R., Houshmand G. Myocarditis detected after COVID-19 recovery. Eur. Heart J. Cardiovasc. Imaging. 2020 doi: 10.1093/ehjci/jeaa166. n.d. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161.Puntmann V.O., Carerj M.L., Wieters I., Fahim M., Arendt C., Hoffmann J. Outcomes of cardiovascular magnetic resonance imaging in patients recently recovered from coronavirus disease 2019 (COVID-19) JAMA Cardiol. 2020 doi: 10.1001/jamacardio.2020.3557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 162.Nehme Z., Andrew E., Bernard S., Smith K. Sex differences in the quality-of-life and functional outcome of cardiac arrest survivors. Resuscitation. 2019;137:21–28. doi: 10.1016/j.resuscitation.2019.01.034. [DOI] [PubMed] [Google Scholar]
- 163.Warner Gargano Julia, Reeves Mathew J. Sex differences in stroke recovery and stroke-specific quality of life. Stroke. 2007;38:2541–2548. doi: 10.1161/STROKEAHA.107.485482. [DOI] [PubMed] [Google Scholar]