Abstract
Objectives
Mid-life adults have notably higher rates of alcohol and other substance misuse than older adults and maintain higher levels of use over time. Social isolation has been linked to higher risk use with increasing age. The purpose of this study is to examine the associations between social relationships, drinking, and misuse of sedative-tranquilizers.
Methods
The data for this study comes from the national Midlife in the United States study wave 2 (MIDUS 2) of adults (N = 3,378; 53.3% women) aged 40 and older. Past month alcohol use and past year sedative medication misuse were assessed with social support and strain. Multinomial logistic regressions evaluated the relationship of a) support and b) strain to use and co-use of alcohol and sedatives.
Results
Of the sample, 58.4% used alcohol only, 1.7% only misused sedatives, and 3.5% co-used alcohol/misused sedative-tranquilizers. Support from friends was associated with 1.18 increased risk of co-using compared to not using either substance. Source of strain was associated with co-use for middle-aged and older adults. Familial strain was associated with increased risk of co-using for middle-aged adults. Friend-related strain was associated increased risk of co-use for older adults.
Conclusion
Evidence suggests that older co-users may differ from those in midlife in terms of social risk factors. As the aging population increases, elucidating the potential mechanisms by which social factors impact concurrent alcohol use and sedative-tranquilizer medication misuse aid the development of targeted interventions and prevention programs in these groups.
Keywords: social support, social strain, alcohol use, prescription medication misuse
Introduction
Current mid-life adults (those aged 50–64) have notably higher rates of substance misuse than those aged 65 and older and, as they move into later life, they are more likely to consume alcohol than previous generations of older adults (Barry & Blow, 2016; Maree, Marcum, Saghafi, Weiner, & Karp, 2016; Schepis & McCabe, 2016). Adults aged 50 to 59 account for 83% of substance abuse treatment admissions among adults aged 50 years and older (Schepis & McCabe, 2016). Although alcohol and other substance use is not as high as among younger adults, alcohol is the most commonly abused substance in adults 50 and older. Sedative-tranquilizers (anxiolytic, sleep-promoting, and muscle relaxant medications) are some of the most commonly misused medications, including benzodiazepines (Bogunovic, 2012; Maust, Lin, Blow, 2019; Moore, Thomas, & Mattison, 2017; Wu & Blazer, 2011). While misuse declines among older age groups, nonmedical prescription drug use is growing among older adults and the misuse of tranquilizers has grown as much as for opioids, though the latter has received much more attention (Schepis & McCabe, 2016).
Concurrent use of alcohol and sedative-tranquilizers pose particular health risks, but less is known about such use among older adults. International studies suggest that upwards of 50% of older sedative or hypnotic users consume alcohol (Holton, Gallagher, Fahey, & Cousins, 2017; Ilomäki et al., 2013). Little research has examined risk factors for concurrent use among older adults, and how these risk factors may vary for middle-aged adults compared to those 65 or older. Apart from sociodemographic factors (e.g., being aged 70–79, higher social status, living in rural areas), one study of German older adults found that social factors were associated with concurrent use of alcohol and psychotropic medications (Du, Scheidt-Nave, & Knopf 2008). Specifically, for older adults, living alone or having a limited social network were associated with concurrent use of alcohol and psychotropic medications, though they did not examine this association by specific psychotropic class. Previous work has demonstrated associations between a variety of social factors and use of both alcohol and misuse of such medications, including loneliness, lower social support, quality of relationship with family, and less social interaction, which were associated with overall misuse of sedative and tranquilizers and greater alcohol use (Kuerbis et al., 2018; Moos, Brennan, Schutte, & Moos, 2010; Tseng et al., 2018). Further evidence suggests that interpersonal stress might be associated with misuse of controlled substances, such as benzodiazepines (Weaver, 2015). Given evidence that early-onset substance users may differ from late-onset users in terms of demographic characteristics and risk factors, understanding the shifts in mid- to late-life multiple or concurrent use of alcohol and prescription medications is of particular importance (Barry & Blow, 2016; Wu & Blazer, 2011).
Given previous research indicating a relationship between lack of social network or support and single use or misuse of alcohol and prescription sedative and tranquilizers, we hypothesized that a) social support would be negatively associated with co-use while b) social strain would be positively associated with co- use in a sample of a mid- to late-life adults. We also hypothesized that the associations would differ by source of support and strain (family vs. friends). Lastly, we explored whether these associations varied between middle-aged and older adults.
Methods
Sample
The present study uses cross-sectional data from the second wave of the National Survey of Midlife in the United States study (MIDUS-II; Brim, Ryff, Kessler, 2004; Ryff et al., 2017). MIDUS-II was designed to examine how behavioral, psychology, and social factors contributed to health and well-being in a sample of noninstitutionalized, English-Speaking adults. At Wave 2, 90.8% of the sample was located from Wave 1. Of those located, 82.8% were interviewed. The overall response rate for respondents who had completed both the phone and self-administered questionnaire at Time 1 was 79.7%. The present sample included 1,708 adults aged 40 and older (n = 867 women, n = 841 men) with complete data on outcome variables.
Measures
Outcomes
Alcohol use was examined with an item assessing quantity of typical alcohol consumption in the past month. Those who reported having zero drinks on average were considered ‘non-drinkers’ and those who reported one or more drinks were considered ‘drinkers.’
Prescription sedative or tranquilizer medication misuse over the past 12 months was assessed with two items. Misuse was defined as ‘use of medications on your own either without a doctor’s prescription, in larger amounts than prescribed, or for a longer period than prescribed.’ The two items included past year misuse of 1) ‘Sedatives, including either barbiturates or sleeping pills on your own (e.g. Seconal®, Halcion®, Methaqualone®)’ and 2) ‘Tranquilizers or “nerve pills” on your own (e.g. Librium®, Valium®, Ativan®, Xanax®).’ Response choices included Yes (1) or No (0). These items were combined to create a single dichotomous item such that 1 = Misused either sedatives and/or tranquilizers and 0 = did not misuse sedatives or tranquilizers.
Social relationships
Perceived social support and strain were assessed for two relationships: family members exclusive of a spouse/partner and friends.
Perceived social support consisted of four items for family and friend relationships each. Items examined how often participants could open up to and rely on their family members (excluding their spouse/partner) or friends (1 = not at all; 4 = a lot) (Schuster, Kessler, & Aseltine, 1990; Walen & Lachman, 2000). Items were averaged to create a composite score for family support and friend support, with higher scores indicating higher perceived support.
Perceived social strain consisted of four items for strain from family and friend relationships. These items included 1) ‘[Not including your spouse or partner], How often do members of your family/your friends make too many demands on you?’; 2) ‘How often do they criticize you?’; 3) ‘How often do they let you down when you are counting on them?’; and 4) ‘How often do they get on your nerves?’ Response choices for social strain items were on a 4-point Likert scale and ranged from Often (1) to Never (4). Items were recoded such that higher scores indicated higher relationship strain.
Covariates
Models included covariates controlling for age; educational attainment [0 = Less than high school, 1 = High school diploma or equivalent, 2 = Some college, but no degree, 3 = College degree (including associate degree, vocational degree, and 4-year college degree), and 4 = graduate education]; and number of chronic health conditions present in the past year (range 0 to 30 conditions; e.g., asthma, diabetes).
Analytic strategy
The majority of cases (about 98.0%) were complete. Missing data analyses determined that those who were missing on one dimension of a social relationship measure (e.g., social support from friends) were also missing data from the other (e.g., strain from friends). We used multiple imputation to address missing data in predictors with 10 imputed datasets. Univariate and bivariate analyses were conducted for measures of social relationships (i.e., support and strain) and substance use.
Next, two multinomial logistic regression models were conducted to determine whether social support and strain were associated with alcohol use and/or sedative-tranquilizer misuse. The first model regressed social support from friends and family onto alcohol use/sedative-tranquilizer misuse. For the second model, social strain from friends and family were regressed onto alcohol use/sedative-tranquilizer misuse. Lastly, we stratified by age to explore whether these associations varied between middle-aged (adults aged 40–64) and older adults (adults aged 65 and older). Thus, for each group, the two multinomial models examining the associations between 1) social support and concurrent use of alcohol and misuse of sedative-tranquilizers and 2) social strain support and concurrent use of alcohol and misuse of sedative-tranquilizers. For all models, age, education, and chronic health conditions were included as covariates.
Results
Descriptive statistics for substance use and social relationships are reported by age in Table 1. The mean age for the sample was 57.74 (SE = 0.19 years) with a little over half being women (53.3%) and about 91% being non-Hispanic/Latinx White. Most had completed at least a high school education or beyond (93%). Of the sample, 5.2% reported past-year misuse of prescription sedative-tranquilizer medications. 36.3% neither drank in the past month nor misused prescription sedative-tranquilizer medications in the past year; 58.7% of respondents only endorsed alcohol use. 1.7% endorsed sedative misuse without alcohol use, while 3.5% reported both sedative medication misuse and alcohol use. Concurrent users were more likely to be middle-aged (adults aged 40–64; 72.0%), women (63.6%), and to have a college degree or higher (44.9%). Of the concurrent users, 90.7% were moderate drinkers and 9.3% were heavy drinkers.
Table 1.
Sample characteristics and means for middle-aged and older adults (N = 3,378)
| Middle-aged adults (n = 2,412) | Older adults (n = 966) | |
|---|---|---|
| Mean (SE) or Percent (Freq.) | Mean (SE) or Percent (Freq.) | |
| Sociodemographics | ||
| Age (range 40 to 84 years) | 51.99 (0.14) | 72.10 (0.18) |
| Women (%) | 53.4 (1,289) | 52.8 (510) |
| Race/Ethnicity | ||
| Non-White (%) a,b | 9.5 (228) | 7.5 (72) |
| White/Caucasian (%) | 90.5 (2,184) | 92.5 (894) |
| Educational attainment c | ||
| Less than high school/GED (%) | 4.1 (98) | 10.0 (96) |
| High school diploma/GED (%) | 25.3 (609) | 30.8 (297) |
| Some college (%) | 21.4 (515) | 21.7 (209) |
| College and beyond (%) | 49.3 (1,189) | 37.6 (362) |
| Chronic health conditions (range 0–30 conditions) | 3.37 (0.05) | 3.12 (2.90) |
| Substance use (%) | ||
| No drinking or sedative misuse | 33.4 (806) | 43.6 (421) |
| Alcohol use only | 61.5 (1,483) | 50.8 (491) |
| Sedative-tranquilizer misuse only | 1.6 (38) | 2.2 (21) |
| Alcohol use and sedative misuse | 3.5 (85) | 3.4 (33) |
| Social support | ||
| Family (range 1–4) | 3.48 (0.01) | 3.62 (0.02) |
| Friends (range 1–4) | 3.27 (0.01) | 3.30 (0.02) |
| Social strain | ||
| Family (range 1–4) | 2.11 (0.01) | 1.86 (0.02) |
| Friends (1–4) | 1.88 (0.01) | 1.73 (0.02) |
Note.
Non-whites consisted of Latinx (n = 96); Black/African Americans (n = 121); Native Americans, Alaska Native Aleutian Islander (n = 40); Asian (n = 7); Native Hawaiian/Pacific
Islander (n = 3); and other (n = 35);
Missing = 9;
Missing = 3.
Social support and concurrent use
Overall, social support from friends, but not family members, was associated with both using alcohol and misusing sedative-tranquilizer medication, b = 0.17, p = .016. Specifically, those who perceived more support from friends had 1.18 increased risk of using both alcohol and misusing sedatives compared to not using either, 95% CI: [1.03–1.36]. There was no difference in this association between middle-aged and older adults.
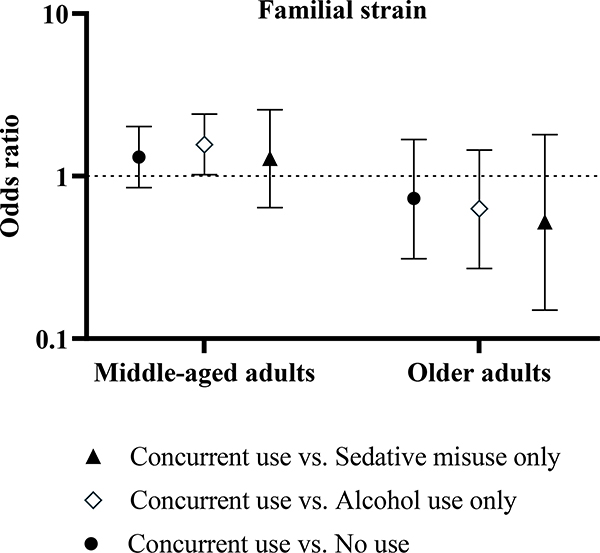
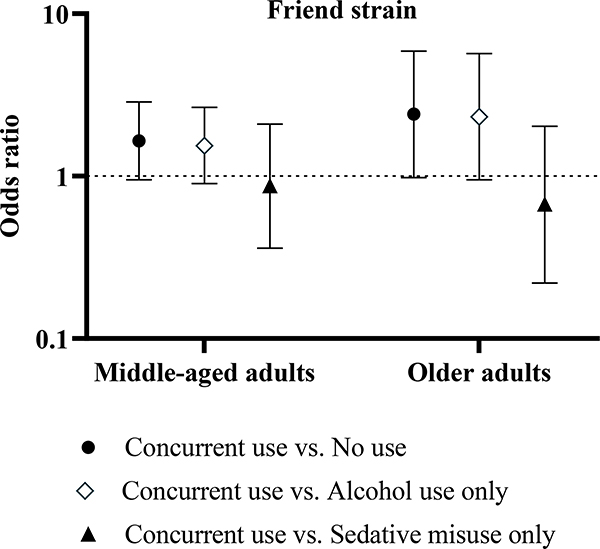
While social strain was generally not associated with concurrent use of alcohol and misuse of sedative and tranquilizers overall, this varied by age (see Figures 1 and 2). Among middle-aged adults, higher social strain related to family was associated with 1.56 increased risk of concurrently using alcohol and misusing prescription sedatives than to only using alcohol, b = 0.45, p = .042, 95% CI: [1.02–2.41]. Conversely, among adults 65 or older, higher perceived social strain related to friends was marginally associated with 2.41 increased risk of concurrently using alcohol and misusing prescription sedatives than not using alcohol or misusing sedatives, b = 0.88, p = .054, 95% CI: [0.98–5.88].
Figure 1.
Odds ratios from multinomial logistic regressions for familial social strain and concurrent alcohol use and misuse of sedative and tranquilizers by age group.
Figure 2.
Odds ratios from multinomial logistic regressions for familial social strain and concurrent alcohol use and misuse of sedative and tranquilizers by age group.
Discussion
The present study examined the association between social relationship quality and concurrent alcohol use and misuse of sedative-tranquilizer medications in adults aged 40 and older. Overall, roughly 5% of the sample misused sedative-tranquilizer medications in the past year. Additionally, more than half of the sample had only used alcohol, about 2% had only misused sedative-tranquilizers, and approximately 4% had used alcohol and misused sedative-tranquilizers. The current study also suggests that concurrent use may be differentially associated with specific social relationships and varied by age.
Overall, higher perceived social support from friends, but not family, was associated with increased risk of concurrently consuming alcohol and misusing sedatives compared to not using either. However, these associations didn’t differ between concurrent drinking and misuse of sedatives and single use of either alcohol or sedatives. These findings are counter to a previous study in which having a poor social network (having no or only one person available for emergencies) was associated with increased risk for use of sedative and tranquilizers as well as combined use of alcohol and psychotropic drugs among older Germans (Du, Scheidt-Nave, & Knopf, 2008). However, this particular study did not examine relationship type (i.e., family versus friends) nor use of specific psychotropic medication classes.
Previous research has found that among adults aged 50 and older, the main reasons for misusing benzodiazepines consisted of relaxation/relieving tension, to help with sleep, to get high, or to help with feelings or emotions (Maust, Lin, & Blow, 2019). Similarly, greater alcohol use has been linked to social engagement and relaxation but also loneliness and self-medication of anxiety or insomnia among in adults aged 55 and older (Immonen, Valvanne, & Pitkälä, 2011; Kelly, Olanrewaju, Cowan, Brayne, & Lafortune, 2018; Moos, Brennan, Schutte, & Moos, 2010). Thus, norms regarding drinking or misuse of sedative and tranquilizers to cope might play a role, particularly acceptability of these behaviors by friends. One study found no association between friends’ norms and drinking to cope motives among older adults (Wilson, Wray, & Turrisi, 2019); however, there remains a little to no literature on norms for alcohol and prescription medication misuse in middle- to later-life.
Alternatively, it may be that, as with alcohol and sedative misuse individually, those who misuse these medications and consume alcohol are do not find either alcohol or these medications alone to be adequate in addressing increases in anxiety or emotional stress (Weaver, 2015). More work is needed to better understand context and reasons for use and misuse of sedative-tranquilizer medications among those who also consume alcohol to clarify this association.
Lastly, social strain was not associated with concurrent alcohol use and misuse of sedatives. This association, however, differed for middle-aged and older adults. Among middle-aged adults, higher perceived family-related social strain was associated with increased risk of concurrently using alcohol with sedative misuse. Conversely, among older adults, higher friend-related social strain was marginally associated with co-use of these substances. These findings align with previous work suggesting that documented increases in emotional stress (e.g., dispute with family or friends) may lead to increased consumption of controlled substance medications due to heightened discomfort from anxiety symptoms (Weaver, 2015). That familial strain was a particular risk factor for middle-aged adults but not older adults may lie in possible differences in roles and, potentially, role strain. Middle adulthood is marked with shifts due to adult children leaving or returning to the home, retirement, and role re-negotiation (Almeida, Piazza, Stawski, & Klein, 2011). Conflict stemming from role strain arises when pressures from one role make it difficult to fulfill other role requirements and has been linked to increased use of alcohol but could, conceivably, be related to misuse of medications, such as benzodiazepines (e.g., Valium®) to reduce stress and sleep disturbances due to these issues (Allen, 2012; Blumenstein, Benyamini, Chetrit, Mizrahi, & Lerner-Geva, 2012; Frone, Russell, & Cooper, 1993; Wolff, Rospenda, & Richman, 2014). On the other hand, older adults, who have cultivated smaller but more meaningful social networks may be particularly affected by strain within their friendships. This may result in increased stress reactivity and, subsequently, substance use to alleviate it (Friedman, Karlamangla, Almeida, & Seeman, 2012; Peltier et al., 2019). Future research should examine other aspects of these different relationships (e.g., strength or closeness) to better understand how they may be related to substance use and misuse.
The present study is not without limitations. The data presented are cross-sectional, thus, direction of associations and causal inference cannot be made. Alcohol use and prescription sedative and tranquilizer misuse were self-reported, which may lead to skewed estimates of use due to social desirability or recall bias. The majority of the sample were non-Hispanic White, reducing generalizability to the general U.S. population of middle-aged and older adults. Similarly, sedative and tranquilizer misuse were slightly higher than previous studies, including from the National Study of Drug Use and Health that found that among adults aged 50 and older, between 0.2% and 1.4% misused tranquilizers compared to the present sample at 5.0% (Schepis & McCabe, 2016). However, in terms of concurrent use of alcohol and interactive medications, the present sample mirrors that of those found among older adults residing in Europe, North America, and Australia which found that between 34% and 54% of older sedative-tranquilizer users consume alcohol compared to the 61.0% of older adults in the present sample (Holton, Gallagher, Fahey, & Cousins, 2017; Ilomäki et al., 2013).
Despite these limitations, the present study identified important social factors associated with concurrent use of alcohol and misuse of prescription sedative-tranquilizer medications, which also varied by age. This study highlights the need for additional research to improve identification of mid- and late-life adults at risk for using alcohol with alcohol-interactive medications, such as sedative and tranquilizers, for intervention. Better understanding how social relationship quality in addition to received social support or network sizes is an important preliminary step to addressing these issues.
Acknowledgments
Funding
This work was supported by the National Institute of Mental Health (NIMH) [grant number T32 MH073553-11] at the National Institutes of Health (NIH). The NIMH played no role in manuscript writing, preparation, or interpretation of the results. The content is solely the responsibility of the author and does not necessarily represent the official views of the NIMH or the NIH.
References
- Allen TD (2013). The work–family role interface: A synthesis of the research from industrial and organizational psychology. In Weiner IB (Ed.), Handbook of Psychology (2nd ed., pp. 699–718). [Google Scholar]
- Almeida DM, Piazza JR, Stawski RS, & Klein LC (2011). The speedometer of life: Stress, health, and aging. In Schaie K. Warner & Willis SL. Handbook of the Psychology of Aging (7th ed., pp. 295–310). [Google Scholar]
- Barry KL, & Blow FC (2016). Drinking over the lifespan: Focus on older adults. Alcohol Research: Current Reviews, 38 (1), 115–120. [PMC free article] [PubMed] [Google Scholar]
- Blumstein T, Benyamini Y, Chetrit A, Mizrahi EH, & Lerner-Geva L (2012). Prevalence and correlates of psychotropic medication use among older adults in Israel: Cross-sectional and longitudinal findings from two cohorts a decade apart. Aging & Mental Health, 16 (5), 636–647. doi: 10.1080/13607863.2011.644262 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Breslow RA, Dong C, & White A (2015). Prevalence of alcohol-interactive prescription medication use among current drinkers: United States, 1999 to 2010. Alcoholism: Clinical and Experimental Research, 39(2), 371–379. doi: 10.1111/acer.12633 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Du Y, Scheidt-Nave C, & Knopf H (2008). Use of psychotropic drugs and alcohol among non-institutionalised elderly adults in Germany. Pharmacopsychiatry, 41 (6), 242–251. doi: 10.1055/s-0028-1083791 [DOI] [PubMed] [Google Scholar]
- Gregory Hobelmann J, Clark MR, Hobelmann JG, & Clark MR (2016). Benzodiazepines, alcohol, and stimulant use in combination with opioid use. In Staats PS & Silverman SM (Eds.), Controlled Substance Management in Chronic Pain: A Balanced Approach (pp. 75–86). doi: 10.1007/978-3-319-30964-4_6 [DOI] [Google Scholar]
- Holton AE, Gallagher P, Fahey T, & Cousins G (2017). Concurrent use of alcohol interactive medications and alcohol in older adults: A systematic review of prevalence and associated adverse outcomes. BMC Geriatrics, 17 (1), 148. doi: 10.1186/s12877-017-0532-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ilomäki J, Gnjidic D, Hilmer SN, Le Couteur DG, Naganathan V, Cumming RG, … Bell JS (2013). Psychotropic drug use and alcohol drinking in community-dwelling older Australian men: The CHAMP study. Drug and Alcohol Review, 32 (2), 218–222. doi: 10.1111/j.1465-3362.2012.00496.x [DOI] [PubMed] [Google Scholar]
- Immonen S, Valvanne J, & Pitkälä KH (2011). Older adults’ own reasoning for their alcohol consumption. International Journal of Geriatric Psychiatry, 26( 11), 1169–1176. doi: 10.1002/gps.2657 [DOI] [PubMed] [Google Scholar]
- Kelly S, Olanrewaju O, Cowan A, Brayne C, & Lafortune L (2018). Alcohol and older people: A systematic review of barriers, facilitators and context of drinking in older people and implications for intervention design. PLOS ONE, 13 (1), e0191189. doi: 10.1371/journal.pone.0191189 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kuerbis A, Treloar Padovano H, Shao S, Houser J, Muench FJ, & Morgenstern J (2018). Comparing daily drivers of problem drinking among older and younger adults: An electronic daily diary study using smartphones. Drug and Alcohol Dependence, 183 (017), 240–246. doi: 10.1016/j.drugalcdep.2017.11.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maree RD, Marcum ZA, Saghafi E, Weiner DK, & Karp JF (2016). A systematic review of opioid and benzodiazepine misuse in older adults. The American Journal of Geriatric Psychiatry, 24 (11), 949–963. doi: 10.1016/j.jagp.2016.06.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maust DT, Lin LA, & Blow FC (2019). Benzodiazepine use and misuse Among adults in the United States. Psychiatric Services, 70 (2), 97–106. doi: 10.1176/appi.ps.201800321 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moore TJ, & Mattison DR (2017). Adult utilization of psychiatric drugs and differences by sex, age, and race. JAMA Internal Medicine, 177 (2), 274–275. doi: 10.1001/jamainternmed.2016.7266 [DOI] [PubMed] [Google Scholar]
- Moos RH, Brennan PL, Schutte KK, & Moos BS (2010). Social and financial resources and high-risk alcohol consumption among older adults. Alcoholism: Clinical and Experimental Research, 34 (4), 646–654. doi: 10.1111/j.1530-0277.2009.01133.x [DOI] [PubMed] [Google Scholar]
- Qato DM, Manzoor BS, & Lee TA (2015). Drug-alcohol interactions in older U.S. adults. Journal of the American Geriatrics Society, 63(11), 2324–2331. doi: 10.1111/jgs.13787 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ryff C, Almeida DM, Ayanian J, Carr DS, Cleary PD, Coe C, … Williams D (2017). Midlife in the United States (MIDUS 2), 2004–2006. Ann Arbor, MI: Inter-university Consortium for Political and Social Research [distributor], 2017-11–20. doi: 10.3886/ICPSR04652.v7 [DOI] [Google Scholar]
- Ryff C, Carr DS, & Coe C (2006). MIDUS II, 2004–2006 Documentation of Psychosocial Constructs and Composite Variables. [Google Scholar]
- Schepis TS, & McCabe SE (2016). Trends in older adult nonmedical prescription drug use prevalence: Results from the 2002–2003 and 2012–2013 National Survey on Drug Use and Health. Addictive Behaviors, 60, 219–222. doi: 10.1016/j.addbeh.2016.04.020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schuster TL, Kessler RC, & Aseltine RH (1990). Supportive interactions, negative interactions, and depressed mood. American Journal of Community Psychology, 18(3), 423–438. doi: 10.1007/BF00938116 [DOI] [PubMed] [Google Scholar]
- Veldhuizen S, Wade TJ, & Cairney J (2009). Alcohol consumption among Canadians taking benzodiazepines and related drugs. Pharmacoepidemiology and Drug Safety, 18 (3), 203–210. doi: 10.1002/pds.1702 [DOI] [PubMed] [Google Scholar]
- Walen HR, & Lachman ME (2000). Social support and strain from partner, family, and friends: Costs and benefits for men and women in adulthood. Journal of Social and Personal Relationships, 17 (1), 5–30. doi: 10.1177/0265407500171001 [DOI] [Google Scholar]
- Weaver MF (2015). Prescription sedative misuse and abuse. The Yale Journal of Biology and Medicine, 88 (3), 247–256. [PMC free article] [PubMed] [Google Scholar]
- Wolff JM, Rospenda KM, & Richman JA (2014). Age differences in the longitudinal relationship between work-family conflict and alcohol use. Journal of Addiction, 2014, 1–10. doi: 10.1155/2014/354767 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu LT, & Blazer DG (2011). Illicit and nonmedical drug use among older adults: A review. Journal of Aging and Health, 23(3), 481–504. doi: 10.1177/0898264310386224 [DOI] [PMC free article] [PubMed] [Google Scholar]