Abstract
Cardiovascular disease (CVD) disparities are shaped by differences in risk factors across racial and ethnic groups. Housing remains an important social determinant of health (SDH). The objective of this statement is to review and summarize research that has examined the associations of housing status with cardiovascular (CV) health and overall health. PubMed/Medline, Centers for Disease Control and Prevention, US Census data, Cochrane Library reviews and the annual Heart Disease and Stroke Statistics report from the American Heart Association were used to identify empirical research studies that examined associations of housing with CV health and overall well-being. Health is impacted by four prominent dimensions of housing: 1) stability, 2) quality and safety, 3) affordability and accessibility, and 4) neighborhood environment. Vulnerable and underserved populations are adversely affected by housing insecurity and homelessness, at risk for lower quality and unsafe housing conditions, confront structural barriers that limit access to affordable housing, and at risk for living in areas with substandard built-environment features that are linked to CVD. Research linking select pathways to CV health is relatively strong, but there remain research gaps in other housing pathways and CV health. Efforts to eliminate CVD disparities have recently emphasized the importance of SDH. Housing is a prominent social determinant of CV health and well-being, and should be considered when evaluating prevention efforts to reduce and eliminate racial/ethnic and socioeconomic disparities.
Keywords: Housing, cardiovascular health, cardiovascular disease, social determinants of health, health disparities, racial disparities
INTRODUCTION
Cardiovascular disease (CVD) disparities are shaped by differences in risk factors across racial/ethnic and socioeconomic groups. Disparities have been largely noted by differences in risk factors for CVD (hypertension, diabetes, obesity, cholesterol), cardiovascular (CV) incidence and mortality.1 Recently, more attention has focused on the social determinants of CV risk and outcomes.2 Vulnerable and underserved populations (i.e., Blacks) report greater levels of psychosocial stress, which is associated with racial disparities in risk factors such as hypertension and obesity.3 Where one lives remains an important social determinant of health (SDH) as well. Studies have primarily examined the associations of residential environments with CVD risk.4 However, the conditions of housing (i.e., stability, quality, affordability) are also important contributors to existing health inequities.5
The SDH conceptual framework emphasizes how social structures impact population health through a myriad of social, economic, political, psychosocial and behavioral interactions.6 Structural mechanisms (i.e., socioeconomic and political context and social class divisions) generate social hierarchies that influence intermediary determinants of health (i.e., behaviors, psychosocial factors and material circumstances) that ultimately affect health inequity and well-being. This statement focuses on the segment of the SDH framework that addresses pathways between living/housing conditions and CV health.7 Although outside of the scope of this review, we recognize that racial and socioeconomic disadvantages are shaped by upstream social structures that impact economic resources available to purchase housing status, which ultimately may affect downstream CV health and well-being.
This statement considers four major pathways connecting housing and CV health: 1. housing stability, 2. housing quality and safety, 3. housing affordability and accessibility, and 4. neighborhood physical and social environment. Based on previous work on housing and health,8–11 Taylor (2018) summarized their health impact and implications for SDH (Figure 1).12 The objective of this statement is to review and summarize research that has examined the pathways linking housing to CV health and overall health. The following approach was used to identify empirical studies that examined housing and CV health and well-being: 1) utilized PubMed/Medline, Centers for Disease Control and Prevention, US Census data, Cochrane Library reviews databases and the annual Heart Disease and Stroke Statistics report from the American Heart Association; 2) performed key word searches on residential stability, quality and safety, affordability and accessibility, neighborhood environment, CVD, CV and overall health; and 3) limited search to studies that were published in the last twenty years. An understanding of these dimensions of housing is important for purposes of reducing and ultimately eliminating health inequities that plague vulnerable and underserved populations.
Figure 1. Four Pathways Connecting Housing and Health.
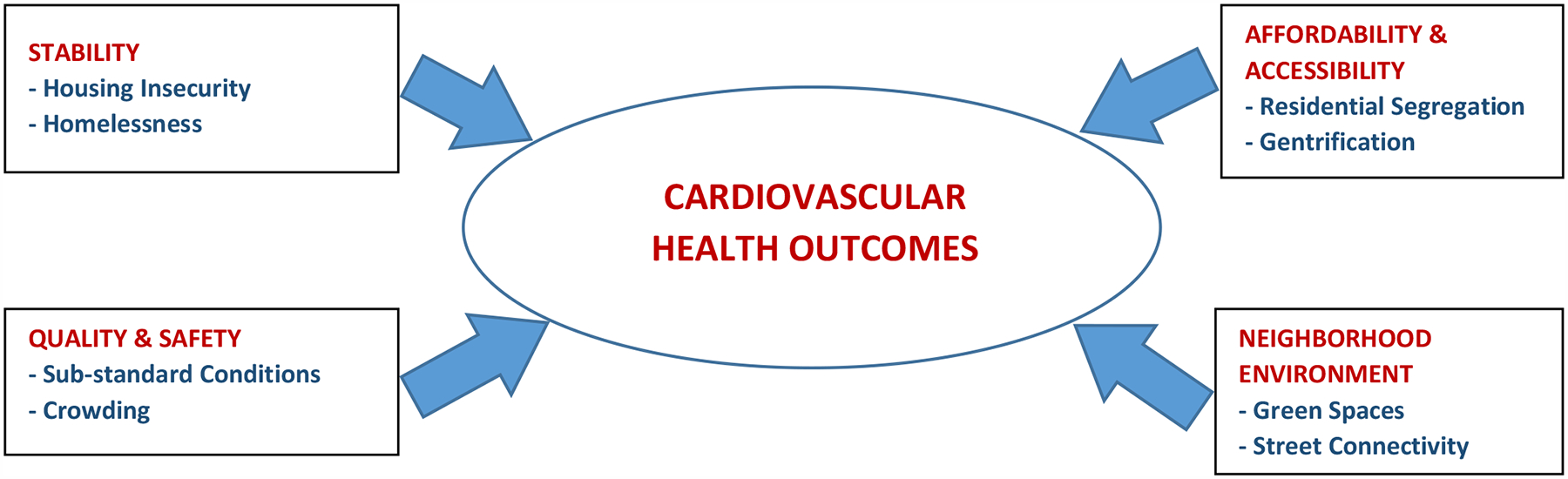
Note: Adapted with permission from Taylor.12 Adapted from the work of Braveman et al.,8 Gibson et al.,9 Maqbool et al.,10 and Sandel et al.11
HOUSING STABILITY
Indicators of housing instability, such as homelessness and housing insecurity, are associated with poor physical and mental health outcomes. Homelessness is defined by the U.S. Department of Housing and Urban Development as not having the resources to obtain permanent housing. Categories of homelessness include frequent moves in a short period of time (e.g., serial renters), temporary shelter in a hotel, with friends (couching surfing), or in a shelter and unsheltered situations (e.g., on the street).13, 14 National data on homelessness report that 7% of people without permanent housing live in rural areas,15 which has health implications for urban vs. rural homelessness.
Epidemiologic data suggest that adults who are homeless experience 60–70% higher rates of CV events compared to the general population.16, 17 Regarding CV risk factors, data on homeless populations are mixed. Some studies have observed a similar prevalence of hypertension between homeless and non-homeless adults,16 while others have observed higher rates of hypertension among homeless adults.17 The prevalence of diabetes appears to be similar to that of the general population. In contrast, prevalent cigarette smoking among homeless adults is high, where between 70% and 80% of the population reported current smoking.16 Few studies have examined CVD risk assessments and homelessness.
Additionally, non-traditional factors may contribute to an increased risk for CVD among certain subgroups of homeless individuals. Some studies have observed a higher prevalence of human immunodeficiency virus (HIV), which may contribute to an elevated risk for CVD among some subgroups of homeless adults. An estimated 25% of homeless adults report recent cocaine use, which is associated with an increased risk for CV events including myocardial infarction.16 Rates of mental illness are estimated to be at 25% of the homeless population,16 which may be an additional factor contributing to fragmented CVD care in this population.
Homeless adults may experience a higher CVD mortality due to the inadequacy of CV risk factor diagnosis and treatment.16 Similarly, timely diagnosis of CVD may be difficult in this population due to barriers to care, need for testing sometimes over several days, medication initiation and adherence and access to healthy foods. Issues of fragmented care and stigmatization in traditional healthcare settings may also contribute to inadequate treatment for CV risk factors and CVD management. However, data on the management of primary and secondary prevention of CVD is not well studied.
For those who confront housing insecurity (e.g., high housing cost relative to income), the prevalence of CV risk factors may be higher than those with more secure housing. Housing security has been generally based on self-reported difficulty paying for rent or mortgage. The 2015 Behavioral Risk Factor Surveillance System (BRFSS) found those with self-reported CVD were more likely to be housing insecure than those who did not have CVD.18 Authors posited that developing CVD led to housing insecurity, but as this study is cross-sectional, the direction of this relationship is not clear. A study of Hawaii BRFSS participants found housing insecurity was associated with CVD and diabetes in Native Hawaiian and other Pacific Islanders, but not among Whites or Asians.19 In addition, a study of residents of the Philadelphia metropolitan area did not find a significant association between housing insecurity and self-reported heart disease, but they did find housing insecure participants were more likely to have hypertension.20
Housing security was unrelated to emergency department visits (for any reason) in the Philadelphia study,20 but a study of participants of the National Survey of American Families found that those who are housing insecure have more emergency department visits and hospitalizations.21 Two national studies found housing insecure participants were less likely to have a usual source of care,21, 22 and studies in Philadelphia and Washington State found housing insecure participants were less likely to seek medical care or prescription medications due to cost.20 A review reported that those at risk for home eviction were more likely to have negative health outcomes, including depression, poor self-reported health, and elevated blood pressure.23 Among 711 low-income adults with diabetes, housing instability (adults lacking a usual place to stay) was inversely associated with self-efficacy for diabetes self-care.24
Several barriers to CV care may be particularly prevalent among the homeless or those with housing insecurity. Competing stressors include the need to obtain nightly shelter, food, and clothing. Suboptimal sleep is likely to be common among the homeless. Given recent evidence for the association of poor sleep with CV risk, this may be an important modifiable factor for this population.25 Barriers to obtaining regular care, lack of insurance and barriers to obtaining medications and storing medications may be more prevalent among the homeless population. Housing instability was associated with postponing medical care and medications, increased use of the emergency department, and a higher rate of hospitalizations.26 Housing instability was also inversely associated with access to a usual source of healthcare. Lastly, prediction tools such as the pooled risk equation may not adequately represent the homeless population, given the lack of non-traditional risk factors incorporated into such risk prediction tools. In addition to reducing knowledge gaps related to the epidemiology of CV risk factors and CVD among homeless or housing insecure adults throughout the U.S., data on tailored medical management of primary and secondary CVD are required to improve CV healthcare in these populations. Finally, since 2015 data suggest that rental options are limited in rural areas,27 which has health implications for housing insecurity between urban vs. rural poor residents, more research is needed that examine these area differences in hosing stability.
Overall, our measures of instability considered the negative CV health consequences of homelessness and insecurity. Housing instability describes conditions that stem from involuntary moves. Conversely, voluntary moves are characterized by residential mobility which may yield positive or negative health consequences (peace of mind or anxiety of a new environment, respectively). We have demonstrated that housing instability is chronic and less likely to have a positive impact on health.
HOUSING QUALITY AND SAFETY
Poor housing quality has been associated with numerous physical and mental health conditions.28 In addition, residential crowding has also been associated with poor health outcomes among both children and adults, but little is known of the impact of poor housing quality on CV health. Features of housing quality such as structural deterioration, presence of mold and pests, lead, insufficient heating/cooling and poor air quality (tobacco smoke) have been associated with mental health, behaviors as well as other physical health conditions.29 In addition to the health impact, poor housing quality can also lead to an unsafe environment. Dilapidated and deteriorated housing can lead to increased risk of falls and injuries; non-working smoke detectors or faulty electrical systems can lead to power outages and fires, increasing the risk of injury and even death.30 Low-income housing, including public housing, is often of poorer quality as physical residences may be older, in need of repairs and service maintenance, which often is not conducted on a consistent basis. Renovations and modifications to housing can improve certain features of the housing environment and consequently influence health outcomes. Housing options in rural areas are often poorer quality than in urban areas, where a substantial proportion of rural homes have inadequate heating or plumbing systems, leaks, or pests.31 This level of substandard housing likely affects the health of rural residents.
Housing quality factors have been shown to impact a number of health outcomes among both children and adults. However, little is known about the impact of housing quality and safety on CV health. Extensive literature has shown that air pollutants, specifically particulate matter and elemental carbon, are associated with CVD and mortality.32 These pollutants can be found in indoor residential environments as a result of using biomass, wood and kerosene stoves, having tighter building construction, and poor air ventilation systems.33 In addition, second-hand smoke exposure is highly prevalent among residents in multi-unit housing and public housing, and secondhand tobacco smoke can migrate through shared ventilation systems, unsealed cracks, and door spaces, leading to adverse health outcomes.34 Although many low-income families turn to ‘doubling up’ and overcrowding as a cost-saving coping strategy, this too may contribute to adverse health outcomes among both children and adults.
It is plausible that poor housing quality impacts CV health as a result of cardiotoxic pollutants found in indoor air, environmental smoke and volatile organic compounds (VOCs). Additionally, poor housing quality has been shown to impact mental health, which in turn is associated with CV health in both children and adults. The adverse psychological consequences of poor housing quality have been partly attributed to: 1) stress about substandard living conditions, 2) poor control over the conditions of one’s home due to the inability to pay for upgrades, or 3) because of housing tenure status as a renter (or both).35
Those who live in older housing as well as people who live in public or low-income housing are more likely to have CVD. For example, NHANES participants who reside in older housing (> 20 years old) are more likely to self-report having had a stroke or heart failure and to have higher environmental contaminant concentrations as measured in blood and urine compared to those who reside in newer housing.36 In the Affordable Housing as an Obesity Mediating Environment (AHOME) study, Bronx, NY public housing residents were more likely to self-report a heart attack or stroke and to have higher measured blood pressure compared to section 8 housing residents as well as those who qualify but do not receive housing assistance.37 There is a need to further examine how housing conditions may affect cardio-metabolic risk factors that contribute to the development of CVD.
Recently, several studies have evaluated the impact of interventions and/or remediation to evaluate the potential benefit of improving housing conditions. A 2013 systematic review of studies focusing on warmth and energy efficiency interventions, for example, concluded that investing in better thermal comfort can improve general health, respiratory health, and mental health.38 Improving housing thermal quality by reducing mold, dampness and producing a comfortable temperature have been shown to reduce systolic and diastolic blood pressure.39 Other home interventions targeting the improvement of air quality have been shown to reduce residential exposure to indoor air pollutants; however, whether the improvements on air quality affect CV health is largely unknown.
Overall, there is limited literature that examines factors that relate to housing quality and safety and cardiometabolic risk factors or CVD. Understanding how the impact of housing quality on mental health, respiratory health as well as developmental and cognitive outcomes extend to affecting CV health would be of utmost importance to address housing quality as a social determinant of CV health.
HOUSING AFFORDABILITY AND ACCESSIBILITY
Several structural factors, including residential segregation, gentrification, and the recent foreclosure crisis, impact CV health by limiting access to affordable, high-quality housing. Racial residential segregation, or the systematic separation of racial and ethnic groups, may also influence CVD risk and serve as a root cause of health disparities in CVD. The occurrence of a higher proportion of one racial/ethnic group within neighborhoods is not inherently problematic as studies have shown that predominately minority urban neighborhoods are more likely to have more social support and cohesion, and access to some culturally specific resources and services.40 However, this may be offset by limited economic resources and access to jobs and high-quality schools, poorer access to health enriching resources, and exposure to toxic stressors.41
The majority of the literature on residential segregation and CVD has focused on Blacks and Hispanics. Among Blacks, many but not all studies, have shown that exposure to segregation is associated with CVD risk factor prevalence.42 However, longitudinal analyses in this area remain sparse. Higher levels of residential segregation were associated with incident CVD in Black adults,43 and with obesity among Black women but not Black men.44 Another study found that reductions in exposure to segregation over a 25-year follow-up period were associated with reductions in systolic blood pressure among Black adults. Moreover, research suggests that Black-White disparities in CVD risk are less pronounced in more integrated communities.45 Findings among Hispanics are more mixed, likely due to differences in background country, nativity, and length of time in the US.42 Few studies have examined the impact of segregation on other racial/ethnic groups.
Gentrification is the process of revitalizing a deteriorating neighborhood through an influx of middle-class or affluent people. This process typically leads to the displacement of earlier, often poorer residents. Existing studies of gentrification and health have largely focused on its impact on self-rated health and mental health. A national cross-sectional study of older adults found that economically vulnerable participants had better self-rated health than their counterparts living in low-income neighborhoods; there was no difference in self-rated health between economically vulnerable participants living in gentrifying neighborhoods vs. moderate-to-high income neighborhoods.46
Two studies used data from a cross-sectional community survey in the Philadelphia metropolitan area. One study found that participants living in gentrifying neighborhoods, characterized by an increase in White residents and declines in non-Whites, were significantly more likely to report above-average self-rated stress levels than those living in neighborhoods that were not gentrifying.47 The other found that Black participants living in gentrifying neighborhoods reported worse self-rated health than their Black counterparts living in neighborhoods that were not gentrifying.48 A cross-sectional study using data from the California Health Interview Survey reported similar findings.49 This suggests living in a gentrifying neighborhood may be worse for the health of vulnerable and underserved populations.
The foreclosure crisis has had a substantial impact on housing accessibility.50 At the beginning of this decade, foreclosure rates peaked with approximately 3 million homes at risk for foreclosure in a single year. The foreclosure crisis was initiated by a deregulated mortgage market and an increase in subprime mortgages. Subprime mortgages were problematic because loans often surpassed property values, federal financing supported creditors rather than lenders, and creditors were incentivized for subprime mortgages.50 The foreclosure crisis exploited vulnerable and underserved populations by targeting them with subprime loans.50, 51
Multiple studies have observed an association between foreclosures and poor health. In the Massachusetts Framingham cohort, every additional foreclosure within 100 meters of a participant was associated with a 1.7 mm Hg rise in systolic blood pressure.52 Residential areas at higher risk for foreclosure had higher proportions of hypertension and hypercholesterolemia than locations at lower risk for foreclosure in the Hispanic Community Health Study/Study of Latinos.53 In a study of four Western states, foreclosures were disproportionately associated with higher rates of myocardial infarctions and strokes among middle-aged Blacks compared to other ethnic groups.54 The foreclosure crisis is also linked to worse adherence, increases in urgent elective visits, and worse psychological health.55 A consequence of property foreclosures includes being evicted, which is likely to be experienced by vulnerable and underserved populations. Most studies on evictions and health examined mental health (stress, depression) followed by physical health conditions (hypertension, obesity), and also reported that the threat of eviction (particularly during the subprime crisis) had a detrimental effect on psychological well-being.23
Providing equitable housing opportunities may improve CV health.10 Providing affordable housing has been associated with reduced Medicaid expenditures in one state.12 Multiple interventions such as low-income housing tax credit and inclusionary zoning require further study to address the potential impact on CV health.12
NEIGHBORHOOD PHYSICAL AND SOCIAL ENVIRONMENT
Another important dimension of housing is a consideration of the broader neighborhood context in which individuals and homes exist. Neighborhood environments have emerged as strong predictors of CV health and well-being.2, 56 The most robust evidence linking neighborhood environments to CVD risk and outcomes is with neighborhood socioeconomic disadvantage. Studies have consistently shown that individuals residing in economically distressed neighborhoods (e.g., high % poverty and unemployment) have a higher incidence of CVD risk factors (e.g., obesity, diabetes, and hypertension),57 CVD events [coronary heart disease (CHD), stroke],4 and CVD mortality.58
More recently, there has been a shift in focus to the investigation of how specific features of neighborhood built/physical and social environments impact CVD. Neighborhood built/physical environment captures indicators of the design and physical attributes of a neighborhood (e.g., residential density, street connectivity, traffic density), and the availability of health-promoting or impeding resources (e.g., healthy food stores, recreational facilities).59 Systematic reviews have identified extensive research documenting associations between built environment indicators and cardio-metabolic factors.60 The density of healthy and unhealthy food retail, walkability, and other urban design features that define obesogenic environments, have been consistently associated with not only diet, physical activity, and BMI/obesity, but also blood pressure, diabetes, and metabolic syndrome. Fewer studies have linked these features to hard CVD outcomes, and among these studies, associations between traffic-related exposures and incident CHD have been documented.61 There is also research to suggest that greenness or level of vegetative presence in a neighborhood may be protective for CV health as recent studies have shown that higher levels of neighborhood greenness are associated with a lower incidence of type 2 diabetes, acute myocardial infarction, ischemic heart disease, and heart failure.62
The social environment, including the social processes, conditions, and relationships within a neighborhood, may also affect CVD.59 One study found that lower police-reported crime and higher overall neighborhood safety are associated with a lower incidence of obesity (along with average BMI over time).63 Studies have also shown that neighborhood social cohesion is protective against incident diabetes and stroke mortality.64, 65
Given the strong evidence from observational studies on the link between neighborhood socioeconomic, built/physical, and social environments and CVD, there is a need for evaluation of interventions, programs, and policies designed to improve health to determine if those improvements also improve CV outcomes. There has only been one randomized trial, The Moving to Opportunities Study, to investigate the long-term benefits of moving people out of disadvantaged neighborhoods and showed some improvements for cardio-metabolic outcomes.66 Other quasi-experimental studies that have focused on evaluating improvements in the food environment and walkability of the neighborhood have found modest to no effects on diet, physical activity, and obesity.67, 68 More research is needed to better understand the levers of neighborhood change, and which levers are most important for improving CV health.
CONCLUSIONS
Housing is a major social determinant of CV health and well-being. This statement summarized research that highlighted important pathways by which dimensions of housing affect CV health and general well-being. This statement also showed there are gaps in the scientific literature on housing and health and showed areas that need further exploration (Table 1). Studies have primarily examined the associations of residential economic environments with CVD risk and general health. However, few studies have examined the extent to which important dimensions of housing (stability, quality and safety, affordability and accessibility, and neighborhood social and built environment) contribute to CV health or increased CV risk that shape inequities among racial/ethnic and socioeconomic groups. This domain of SDH emphasizes the interplay of structural, social, economic, and psychosocial factors and their impact on the association of housing with health.
Table 1.
Research Gaps and Recommendations for Housing and Health
| Housing construct | Research gaps or recommendations |
|---|---|
| Stability |
|
| Quality and Safety |
|
| Affordability and Accessibility |
|
| Neighborhood environment |
|
| All |
|
This area of research informs us of the importance of each pathway in addressing health inequities. We have shown that people who experience housing instability have poorer physical and mental health outcomes than those who do not. Regarding the quality and safety pathway, we have shown that numerous physical housing qualities are related to poor health. In the affordability and accessibility pathway, we have shown that families who experience foreclosures and other structural barriers limiting access to affordable housing have poorer CV and self-rated health. Finally, for the neighborhood environment pathway, we reported that favorable built environment resources are protective of CVD and correlated with favorable health outcomes. Although each of the four pathways is presented as mutually exclusive factors that independently affect CV health and well-being, we acknowledge that these four pathways may potentially overlap, and thus, have a combined impact that negatively affects CV health and well-being. We also acknowledge that housing factors may also overlap with other SDH and have a synergistic impact on health. Future work that examines the CV health effects that derive from the overlap and synergistic effects between dimensions of housing and between housing and other SDH is warranted.
Table 1 displays specific research gaps and recommendations that should be considered in the area of housing and health. For example, there is a need for intervention and prevention efforts that consider each housing construct but also efforts that consider combined features of each construct that will help to improve CV health inequities. Moreover, novel methods should be developed that capture areas of housing that have not been considered in research on housing as a SDH. A final recommendation is that there is a need for research to focus on rural housing and health, as well as urban housing and health.
Although the majority of research we reviewed on housing and CV health and well-being focuses on urban areas, these issues plague many rural places as well. Housing tends to cost less in rural communities, but poverty rates are higher and more persistent, and access to mortgage credit is more limited, leaving many families struggling to pay for housing.27 In addition, although improvements have been made in recent decades, rural low-income families often live in substandard conditions, homes with rodent problems, leaking roofs, and inadequate plumbing and heating.69 As with urban families, these factors increase risk of homelessness in low-income rural families.15 Given this brief snapshot of rural housing-health findings, it is clear that more comparative studies are needed that consider the CV health implications of housing for urban and rural residents (Table 1). A more comprehensive review of the CV health implications of living in rural areas is outlined by Harrington et al. in the recently published AHA presidential advisory on rural health.70
This statement has demonstrated that housing is an important SDH. While the theoretical framework for this statement focuses on the segment of the SDH conceptual model that addresses the pathway between housing conditions and CV health, we recognize that housing conditions may be a direct driver of CV health and well-being, as well as intermediate in the pathway between upstream social and economic disadvantages and downstream CV health outcomes. Efforts to reduce and eliminate health disparities may want to promote and consider multi-level housing interventions, particularly for vulnerable and underserved populations. Efforts should also be made to consider prevention efforts that promote optimal housing conditions that in turn contribute to ideal CV health outcomes. An understanding of these and other dimensions of housing is important for purposes of key stakeholders (healthcare, community development corporations, private businesses, government) to formulate partnerships that would help to improve housing conditions in the U.S., which will reduce and ultimately eliminate health inequities in housing. Finally, engaging in public policy through voting and advocacy, community networking, and population education will be integral in stabilizing the housing crisis.
REFERENCES
- 1.Carnethon MR, Pu J, Howard G, Albert MA, Anderson CAM, Bertoni AG, Mujahid MS, Palaniappan L, Taylor HA Jr., Willis M, Yancy CW, American Heart Association Council on E, Prevention, Council on Cardiovascular Disease in the Y, Council on C, Stroke N, Council on Clinical C, Council on Functional G, Translational B and Stroke C. Cardiovascular Health in African Americans: A Scientific Statement From the American Heart Association. Circulation. 2017;136:e393–e423. [DOI] [PubMed] [Google Scholar]
- 2.Havranek EP, Mujahid MS, Barr DA, Blair IV, Cohen MS, Cruz-Flores S, Davey-Smith G, Dennison-Himmelfarb CR, Lauer MS, Lockwood DW, Rosal M, Yancy CW, American Heart Association Council on Quality of C, Outcomes Research CoE, Prevention CoC, Stroke Nursing CoL, Cardiometabolic H and Stroke C. Social Determinants of Risk and Outcomes for Cardiovascular Disease: A Scientific Statement From the American Heart Association. Circulation. 2015;132:873–98. [DOI] [PubMed] [Google Scholar]
- 3.Ford CD, Sims M, Higginbotham JC, Crowther MR, Wyatt SB, Musani SK, Payne TJ, Fox ER and Parton JM. Psychosocial Factors Are Associated With Blood Pressure Progression Among African Americans in the Jackson Heart Study. American Journal of Hypertension. 2016;29:913–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Diez Roux AV, Merkin SS, Arnett D, Chambless L, Massing M, Nieto FJ, Sorlie P, Szklo M, Tyroler HA and Watson RL. Neighborhood of residence and incidence of coronary heart disease. New England Journal of Medicine. 2001;345:99–106. [DOI] [PubMed] [Google Scholar]
- 5.Shaw M. Housing and public health. Annual Review of Public Health. 2004;25:397–418. [DOI] [PubMed] [Google Scholar]
- 6.Irwin A, Valentine N, Brown C, Loewenson R, Solar O, Brown H, Koller T and Vega J. The commission on social determinants of health: tackling the social roots of health inequities. PLoS Medicine. 2006;3:e106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Braveman P, Egerter S and Williams DR. The social determinants of health: coming of age. Annual Review of Public Health. 2011;32:381–98. [DOI] [PubMed] [Google Scholar]
- 8.Braveman P, Dekker M, Egerter S, Sadegh-Nobari T and Pollack C. How does housing affect health? 2011:Web page: https://www.rwjf.org/en/library/research/2011/05/housing-and-health.html.
- 9.Gibson M, Petticrew M, Bambra C, Sowden AJ, Wright KE and Whitehead M. Housing and health inequalities: a synthesis of systematic reviews of interventions aimed at different pathways linking housing and health. Health & place. 2011;17:175–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Maqbool N, Viveiros J and Ault M. The Impacts of Affordable Housing on Health: A Research Summary. 2015.
- 11.Sandel M, Sheward R, Ettinger de Cuba S, Coleman SM, Frank DA, Chilton M, Black M, Heeren T, Pasquariello J, Casey P, Ochoa E and Cutts D. Unstable Housing and Caregiver and Child Health in Renter Families. Pediatrics. 2018;141. [DOI] [PubMed] [Google Scholar]
- 12.Taylor LA. Housing And Health: An Overview Of The Literature. Health Affairs Health Policy Brief. 2018. [Google Scholar]
- 13.Clifford B, Wilson A and Harris P. Homelessness, health and the policy process: A literature review. Health Policy. 2019;123:1125–1132. [DOI] [PubMed] [Google Scholar]
- 14.Defintion of Homelessness. Homeless Emergency Assistance and Rapid Transition to Housing Act of 2009. 2009:Web page: https://www.hudexchange.info/homelessness-assistance/hearth-act/.
- 15.National Alliance to End Homelessness. Rural Homelessness. 2010:Web page: https://endhomelessness.org/resource/rural-homelessness/.
- 16.Baggett TP, Liauw SS and Hwang SW. Cardiovascular Disease and Homelessness. Journal of the American College of Cardiology. 2018;71:2585–2597. [DOI] [PubMed] [Google Scholar]
- 17.Nayyar D and Hwang SW. Cardiovascular Health Issues in Inner City Populations. The Canadian Journal of Cardiology. 2015;31:1130–8. [DOI] [PubMed] [Google Scholar]
- 18.Charkhchi P, Fazeli Dehkordy S and Carlos RC. Housing and Food Insecurity, Care Access, and Health Status Among the Chronically Ill: An Analysis of the Behavioral Risk Factor Surveillance System. Journal of General Internal Medicine. 2018;33:644–650. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Stupplebeen DA. Housing and Food Insecurity and Chronic Disease Among Three Racial Groups in Hawai’i. Preventing Chronic Disease. 2019;16:E13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Pollack CE, Griffin BA and Lynch J. Housing Affordability and Health Among Homeowners and Renters. American Journal of Preventive Medicine. 2010;39:515–521. [DOI] [PubMed] [Google Scholar]
- 21.Kushel MB, Gupta R, Gee L and Haas JS. Housing instability and food insecurity as barriers to health care among low-income Americans. Journal of General Internal Medicine. 2006;21:71–77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Martin P, Liaw W, Bazemore A, Jetty A, Petterson S and Kushel M. Adults with Housing Insecurity Have Worse Access to Primary and Preventive Care. The Journal of the American Board of Family Medicine. 2019;32:521–530. [DOI] [PubMed] [Google Scholar]
- 23.Vasquez-Vera H, Palencia L, Magna I, Mena C, Neira J and Borrell C. The threat of home eviction and its effects on health through the equity lens: A systematic review. Social Science & Medicine. 2017;175:199–208. [DOI] [PubMed] [Google Scholar]
- 24.Vijayaraghavan M, Jacobs EA, Seligman H and Fernandez A. The association between housing instability, food insecurity, and diabetes self-efficacy in low-income adults. Journal of Health Care for the Poor and Underserved. 2011;22:1279–91. [DOI] [PubMed] [Google Scholar]
- 25.Dominguez F, Fuster V, Fernandez-Alvira JM, Fernandez-Friera L, Lopez-Melgar B, Blanco-Rojo R, Fernandez-Ortiz A, Garcia-Pavia P, Sanz J, Mendiguren JM, Ibanez B, Bueno H, Lara-Pezzi E and Ordovas JM. Association of Sleep Duration and Quality With Subclinical Atherosclerosis. Journal of the American College of Cardiology. 2019;73:134–144. [DOI] [PubMed] [Google Scholar]
- 26.Kushel MB, Gupta R, Gee L and Haas JS. Housing instability and food insecurity as barriers to health care among low-income Americans. Journal of General Internal Medicine. 2006;21:71–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Housing, Assistance and Council. Taking Stock: Rural People, Poverty, and Housing in the 21st Century; 2012.
- 28.Evans GW. Child development and the physical environment. Annual Review of Psychology. 2006;57:423–51. [DOI] [PubMed] [Google Scholar]
- 29.Shaw M. Housing and public health. Annual Review of Public Health. 2004;25:397–418. [DOI] [PubMed] [Google Scholar]
- 30.World Health Organization: Housing and Health Guidelines. 2018.
- 31.National Rural Housing Coalition. Barriers to Affordable Rural Housing. 2018:Web page: http://ruralhousingcoalition.org/overcoming-barriers-to-affordable-rural-housing/.
- 32.Rajagopalan S, Al-Kindi SG and Brook RD. Air Pollution and Cardiovascular Disease: JACC State-of-the-Art Review. Journal of the American College of Cardiology. 2018;72:2054–2070. [DOI] [PubMed] [Google Scholar]
- 33.Rossner A, Jordan CE, Wake C and Soto-Garcia L. Monitoring of carbon monoxide in residences with bulk wood pellet storage in the Northeast United States. Journal of the Air & Waste Management Association. 2017;67:1066–1079. [DOI] [PubMed] [Google Scholar]
- 34.Young W, Karp S, Bialick P, Liverance C, Seder A, Berg E and Karp L. Health, Secondhand Smoke Exposure, and Smoking Behavior Impacts of No-Smoking Policies in Public Housing, Colorado, 2014–2015. Preventing Chronic Disease. 2016;13:E148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Suglia SF, Duarte CS and Sandel MT. Housing quality, housing instability, and maternal mental health. Journal of urban health : bulletin of the New York Academy of Medicine. 2011;88:1105–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Shiue I Indoor mildew odour in old housing was associated with adult allergic symptoms, asthma, chronic bronchitis, vision, sleep and self-rated health: USA NHANES, 2005–2006. Environmental Science and Pollution Research International. 2015;22:14234–40. [DOI] [PubMed] [Google Scholar]
- 37.Chambers EC and Rosenbaum E. Cardiovascular health outcomes of Latinos in the Affordable Housing as an Obesity Mediating Environment (AHOME) study: a study of rental assistance use. Journal of Urban Health. 2014;91:489–98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Thomson H, Thomas S, Sellstrom E and Petticrew M. Housing improvements for health and associated socio-economic outcomes. The Cochrane Database of Systematic Reviews. 2013;2:CD008657. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Lloyd EL, McCormack C, McKeever M and Syme M. The effect of improving the thermal quality of cold housing on blood pressure and general health: a research note. Journal of Epidemiology and Community Health. 2008;62:793–7. [DOI] [PubMed] [Google Scholar]
- 40.Kramer MR and Hogue CR. Is Segregation Bad for Your Health? Epidemiologic Reviews. 2009;31:178–194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Williams DR and Collins C. Racial residential segregation: a fundamental cause of racial disparities in health. Public health reports. 2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Kershaw KN and Albrecht SS. Racial/ethnic residential segregation and cardiovascular disease risk. Current cardiovascular risk reports. 2015;9:10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Kershaw KN, Osypuk TL, Do DP, De Chavez PJ and Diez Roux AV. Neighborhood-level racial/ethnic residential segregation and incident cardiovascular disease: the multi-ethnic study of atherosclerosis. Circulation. 2015;131:141–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Pool LR, Carnethon MR, Goff DC, Gordon-Larsen P, Robinson WR and Kershaw KN. Longitudinal associations of neighborhood-level racial residential segregation with obesity among blacks. Epidemiology. 2018;29:207–214. [DOI] [PubMed] [Google Scholar]
- 45.LaVeist T, Pollack K, Thorpe R Jr, Fesahazion R and Gaskin D. Place, not race: disparities dissipate in southwest Baltimore when blacks and whites live under similar conditions. Health affairs. 2011;30:1880–1887. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Smith RJ, Lehning AJ and Kim K. Aging in place in gentrifying neighborhoods: Implications for physical and mental health. The Gerontologist. 2017;58:26–35. [DOI] [PubMed] [Google Scholar]
- 47.Gibbons J Are gentrifying neighborhoods more stressful? A multilevel analysis of self-rated stress. SSM - population health. 2019;7:100358–100358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Gibbons J and Barton MS. The Association of Minority Self-Rated Health with Black versus White Gentrification. Journal of urban health : bulletin of the New York Academy of Medicine. 2016;93:909–922. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Izenberg JM, Mujahid MS and Yen IH. Health in changing neighborhoods: A study of the relationship between gentrification and self-rated health in the state of California. Health & place. 2018;52:188–195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Crump J, Newman K, Belsky ES, Ashton P, Kaplan DH, Hammel DJ and Wyly E. Cities Destroyed (Again) For Cash: Forum on the U.S. Foreclosure Crisis. Urban Geography. 2008;29:745–784. [Google Scholar]
- 51.Rugh JS and Massey DS. Racial Segregation and the American Foreclosure Crisis. American Sociological Review. 2010;75:629–651. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Arcaya M, Glymour MM, Chakrabarti P, Christakis NA, Kawachi I and Subramanian SV. Effects of proximate foreclosed properties on individuals’ systolic blood pressure in Massachusetts, 1987 to 2008. Circulation. 2014;129:2262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Chambers EC, Hanna DB, Hua S, Duncan DT, Camacho-Rivera M, Zenk SN, McCurley JL, Perreira K, Gellman MD and Gallo LC. Relationship between area mortgage foreclosures, homeownership, and cardiovascular disease risk factors: The Hispanic Community Health Study/Study of Latinos. BMC Public Health. 2019;19:77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Currie J and Tekin E. Is There a Link between Foreclosure and Health? American Economic Journal: Economic Policy. 2015;7:63–94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Vásquez-Vera H, Palència L, Magna I, Mena C, Neira J and Borrell C. The threat of home eviction and its effects on health through the equity lens: A systematic review. Social Science & Medicine. 2017;175:199–208. [DOI] [PubMed] [Google Scholar]
- 56.Diez Roux AV, Mujahid MS, Hirsch JA, Moore K and Moore LV. The Impact of Neighborhoods on CV Risk. Global Heart. 2016;11:353–363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Claudel SE, Adu-Brimpong J, Banks A, Ayers C, Albert MA, Das SR, de Lemos JA, Leonard T, Neeland IJ and Rivers JP. Association between neighborhood-level socioeconomic deprivation and incident hypertension: A longitudinal analysis of data from the Dallas heart study. American heart journal. 2018;204:109–118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Xiao Q, Berrigan D, Powell-Wiley TM and Matthews CE. Ten-Year Change in Neighborhood Socioeconomic Deprivation and Rates of Total, Cardiovascular Disease, and Cancer Mortality in Older US Adults. American Journal of Epidemiology. 2018;187:2642–2650. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Diez Roux AV. Residential environments and cardiovascular risk. Journal of Urban Health. 2003;80:569–89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Malambo P, Kengne AP, De Villiers A, Lambert EV and Puoane T. Built environment, selected risk factors and major cardiovascular disease outcomes: a systematic review. PloS one. 2016;11:e0166846. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Kan H, Heiss G, Rose KM, Whitsel EA, Lurmann F and London SJ. Prospective analysis of traffic exposure as a risk factor for incident coronary heart disease: the Atherosclerosis Risk in Communities (ARIC) study. Environmental health perspectives. 2008;116:1463–1468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Wang K, Lombard J, Rundek T, Dong C, Gutierrez CM, Byrne MM, Toro M, Nardi MI, Kardys J and Yi L. Relationship of neighborhood greenness to heart disease in 249 405 US Medicare beneficiaries. Journal of the American Heart Association. 2019;8:e010258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Powell-Wiley TM, Moore K, Allen N, Block R, Evenson KR, Mujahid M and Diez Roux AV. Associations of neighborhood crime and safety and with changes in body mass index and waist circumference: the Multi-Ethnic Study of Atherosclerosis. American Journal of Epidemiology. 2017;186:280–288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Gebreab SY, Hickson DA, Sims M, Wyatt SB, Davis SK, Correa A and Diez-Roux AV. Neighborhood social and physical environments and type 2 diabetes mellitus in African Americans: The Jackson Heart Study. Health & place. 2017;43:128–137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Clark CJ, Guo H, Lunos S, Aggarwal NT, Beck T, Evans DA, Mendes de Leon C and Everson-Rose SA. Neighborhood cohesion is associated with reduced risk of stroke mortality. Stroke. 2011;42:1212–1217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Ludwig J, Sanbonmatsu L, Gennetian L, Adam E, Duncan GJ, Katz LF, Kessler RC, Kling JR, Lindau ST and Whitaker RC. Neighborhoods, obesity, and diabetes—a randomized social experiment. New England Journal of Medicine. 2011;365:1509–1519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Dubowitz T, Ghosh-Dastidar M, Cohen DA, Beckman R, Steiner ED, Hunter GP, Flórez KR, Huang C, Vaughan CA and Sloan JC. Diet and perceptions change with supermarket introduction in a food desert, but not because of supermarket use. Health Affairs. 2015;34:1858–1868. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Rachele JN, Kavanagh AM, Brown WJ, Healy AM and Turrell G. Neighborhood disadvantage and body mass index: A study of residential relocation. American Journal of Epidemiology. 2018;187:1696–1703. [DOI] [PubMed] [Google Scholar]
- 69.Barriers to Affordable Housing. National Rural Housing Coalition. 2018:Web page: http://ruralhousingcoalition.org/overcoming-barriers-to-affordable-rural-housing/.
- 70.Harrington RA, Califf RM, Balamurugan A, Brown N, Benjamin RM, Braund WE, Hipp J, Konig M, Sanchez E and Joynt Maddox KE. Call to Action: Rural Health: A Presidential Advisory From the American Heart Association and American Stroke Association. Circulation. 2020;141:e615–e644. [DOI] [PubMed] [Google Scholar]


