Abstract
Purpose:
To assess the association between children’s sleep quality and life satisfaction; and to evaluate the underlying mechanisms of this relationship.
Methods:
Three pediatric cohorts in the National Institutes of Health (NIH) Environmental influences on Child Health (ECHO) Research Program administered Patient Reported Outcome Measurement Information System (PROMIS®) parent-proxy measures to caregivers (n=1111) who reported on their 5–9-year-old children’s (n=1251) sleep quality, psychological stress, general health, and life satisfaction; extant sociodemographic data was harmonized across cohorts. Bootstrapped path modeling of individual patient data meta-analysis was used to determine whether and to what extent stress and general health mediate the relationship between children’s sleep quality and life satisfaction.
Results:
Nonparametric bootstrapped path analyses with 1000 replications suggested children’s sleep quality was associated with lower levels of stress and better general health, which, in turn, predicted higher levels of life satisfaction. Family environmental factors (i.e., income and maternal mental health) moderated these relationships.
Conclusion:
Children who sleep well have happier lives than those with more disturbed sleep. Given the modifiable nature of children’s sleep quality, this study offers evidence to inform future interventional studies on specific mechanisms to improve children’s well-being.
Keywords: ECHO, life satisfaction, positive health, sleep quality, well-being
Sleep quality, or the adequacy of and satisfaction with sleep [1], is a core component of sleep health. The National Sleep Foundation recently operationalized sleep quality via sleep continuity indicators, including sleep latency and efficiency, awakening after sleep onset, and frequency of nighttime awakenings >5 minutes [2]. Recently deemed a national priority in the United States [3, 4], sleep quality is a critical contributor to general health and well-being across the lifespan, with broad public health significance. More than a third of U.S. 6- to 9-year-olds have inadequate sleep according to their parents – up from 23% in 2003 – and inadequate sleep increases in adolescence to nearly half of U.S. teenagers [5]. For children and youth, consequences of poor sleep quality span physical, mental, and social health outcomes [6–11]. Although the direction of associations has not been definitively established, epidemiological findings from prospective longitudinal studies indicate that poor sleep quality early in life predicts health issues later in life as well, including emotional and behavioral problems and substance use in adolescence and adulthood, as well as worse health-related quality of life (HRQoL) [12–14].
Prior research emphasizes poor sleep quality and associations with health problems, illness, and impairment. Whether better sleep quality promotes positive health (well-being), particularly in childhood, remains a gap in the literature. Studies with adults suggest sleep is a crucial health asset that enables optimal functioning, including better general health and HRQoL as well as well-being, including positive affect, life satisfaction, and purpose in life [15, 16]. The limited research in pediatric populations focuses on older children and adolescents, and suggests sleep characteristics that underpin sleep quality (i.e., longer sleep duration, earlier bedtimes, non-disrupted sleep) are associated with higher life satisfaction and HRQoL [17–19]. Less is known about whether such associations are present earlier in childhood.
This dearth of research may be due to limitations in reliable and valid measures for this age group. Several existing instruments [20–23] have contributed to the burgeoning knowledge on the importance of well-being – and life satisfaction in particular – as both an outcome and predictor of positive physical, mental, and social functioning (see [24–26] for reviews); however, such measures have limited content validity because they were developed without input from children and families and did not undergo cognitive testing to ensure comprehensibility and developmental appropriateness [27]. The recently developed National Institutes of Health’s (NIH) Patient-Reported Outcomes Measurement Information System (PROMIS®) parent proxy measures now make it possible to evaluate this relationship [28, 29]. Using these U.S. population-based norm reference measures, the current study examines whether and how sleep quality influences children’s well-being. In particular, we focus on children’s life satisfaction – defined an individual’s assessment of his/her life as good and satisfying [24] – as an indicator of well-being because of its strong positive relationship with a myriad of favorable youth developmental outcomes and its ability to mitigate the negative effects of stressful life events and poor parenting styles [24, 25, 30].
Using combined cross-sectional parent-report data from three pediatric cohorts, we examined whether 5 to 9 year-old children’s sleep quality is associated with their life satisfaction, and the underlying mechanisms of this relationship. Based on previous research with adolescents and adults, we propose a model (Figure 1) where 1) poor sleep quality is positively associated with psychological stress (path a; [9, 31]) and negatively associated with general health (path b; [1, 10, 32]); 2) stress is negatively associated with general health (path c; [31, 33]) and life satisfaction (path d; [27, 33]); and 3) general health is positively associated with life satisfaction (path e; [33]). We also examined whether poor sleep quality has a direct negative relationship (i.e., unmediated) with life satisfaction (path f; [15, 16]).
Figure 1.
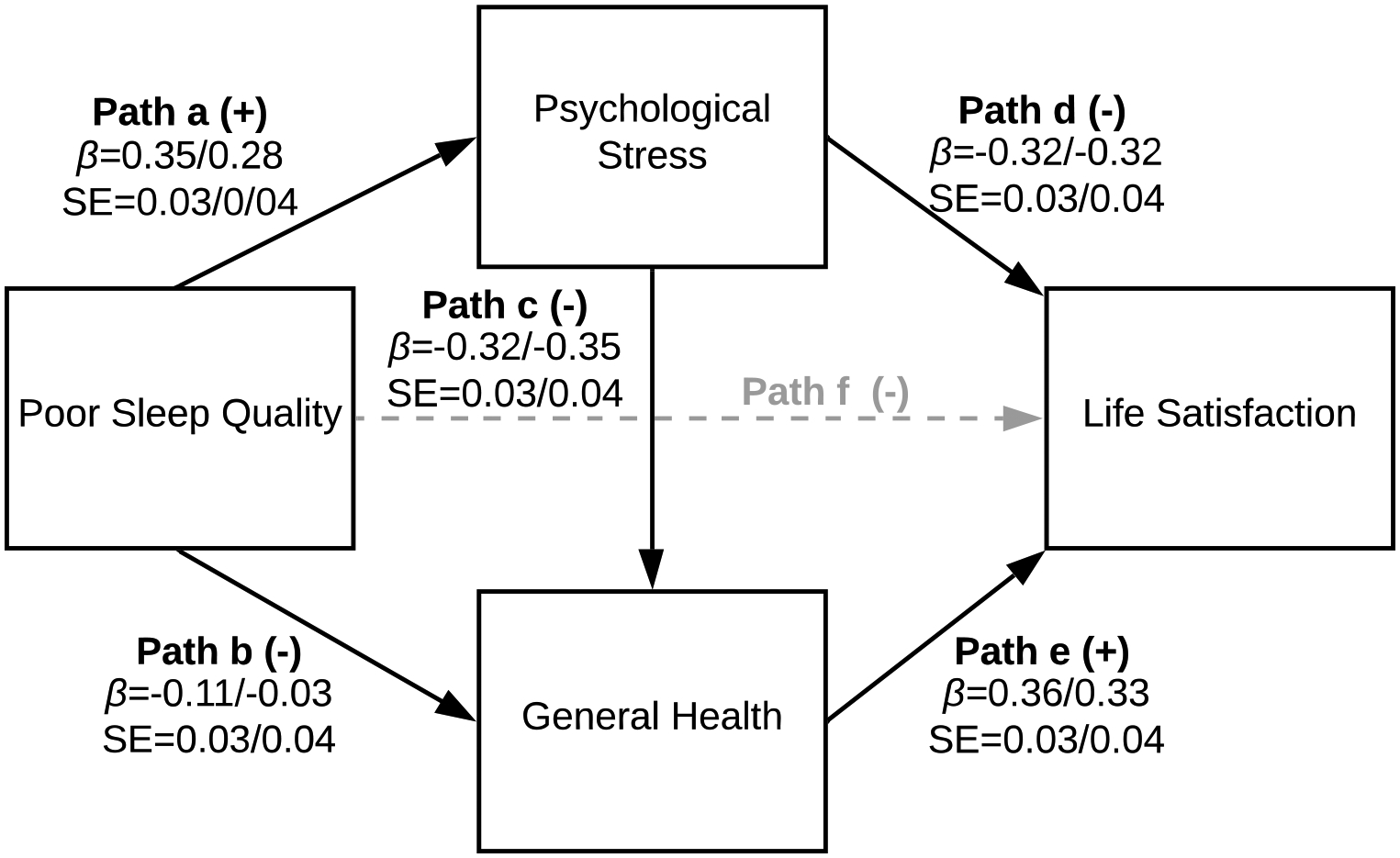
Hypothesized path model and path intercepts () and standards errors (SE) (Model 1 – full sample/Model 2 – subsample). Paths a, b, and c control for child age, sex, race, Hispanic origin, annual family income, and maternal mental health problems. Paths d and e control for annual family income and maternal mental health problems. Path f was not significant in either model and did not change model fit; thus, path f was dropped from the final models.
Methods.
This study draws on data collected for the National Institutes of Health (NIH) Environmental influences on Child Health (ECHO) Research Program (see [34] for overview) as part of the Positive Health Volunteer Pilot Study. Between March and December 2017, investigators from 3 ECHO cohorts administered PROMIS Parent-Proxy Sleep Disturbance [32], Life Satisfaction [27], Global Health [28], and Psychological Stress Experiences [29] measures to caregivers who completed these surveys about their children. We did not impose specific inclusion and exclusion criteria on the basis of sleep quality or disorders. Cohorts also shared previously-collected data pertaining to child and family sociodemographics. The institutional review board at each cohort’s home institution approved data collection and sharing, and the lead Institutional Review Board approved de-identified sharing of data for secondary data analyses under protocol #STU00203654.
A total of 1111 caregivers completed all 4 PROMIS measures for 1251 children ages 5 to 9 years (mean: 6.5, Standard Deviation [SD]: 1.3). Participants primarily resided in the Midwest (77%), with 13% in the South, 8% in the Northeast, 2% in the West (based on region designation by the U.S. Census Bureau). Approximately half of children were male (53%), 79% were white, and 10% were Hispanic. Children came from diverse income levels, including 21% from households making ≤$20,000/year (see Table 1 for complete demographic information).
Table 1.
Descriptive comparisons between the good/average and poor sleep quality subsamples.a
| Good/Average Sleep Quality | Poor Sleep Quality | p | Full Sample | |
|---|---|---|---|---|
| Number of children | 537 | 714 | - | 1252 |
| Number of caregivers | 460 | 651 | - | 1111 |
| Age (years), mean (SD) | 6.5 (1.2) | 6.5 (1.3) | 0.92 | 6.5 (1.3) |
| range | 5.0–9.0 | 5.0–9.0 | 5.0–9.0 | |
| Sex (male = 1), % | 55% | 51% | 0.11 | 53% |
| Race, % | 0.07 | |||
| White | 79% | 78% | - | 79% |
| African American | 7% | 5% | - | 6% |
| Other race | 14% | 17% | - | 16% |
| Hispanic origin, % | 13% | 8% | <0.01 | 10% |
| Annual family income, % | - | |||
| ≤$20,000 | 19% | 23% | 0.06 | 21% |
| $20–40,000 | 18% | 19% | - | 18% |
| $40–60,000 | 34% | 35% | - | 34% |
| ≥$60,000 | 30% | 23% | - | 26% |
| Single parent, % | 13% | 9% | 0.05 | 11% |
| Maternal mental health, % | 27% | 33% | 0.02 | 30% |
| Sleep Disturbance, mean (SD)b | 42.3 (2.1) | 56.8(6.3) | <0.001 | 50.6 (8.7) |
| range | 41.4–49.3 | 49.6–79.4 | - | 41.4–79.4 |
| Psychological Stress, mean (SD)b | 45.8(7.1) | 50.7(8.3) | <0.001 | 48.6 (8.2) |
| range | 39.6–67.3 | 39.6–73.5 | - | 39.6–73.5 |
| General health, mean (SD)b | 54.3 (8.2) | 51.6(8.1) | <0.001 | 52.7(8.3) |
| range | 29.4–66.1 | 27.6–66.1 | - | 27.6–66.1 |
| Life satisfaction, mean (SD)b | 54.5 (6.7) | 51.8(7.5) | <0.001 | 53.0(7.3) |
| range | 34.3–59.2 | 30.9–59.2 | - | 30.9–59.2 |
-, not applicable.
The cutpoint for “good/average” and “poor” sleep quality was based on the PROMIS Pediatric Parent-Proxy Sleep Disturbance nationally normed scores, where “good/average” represented children at or below the 50th percentile and “poor” represented children above the 50th percentile.
Sleep disturbance, general health, stress, and life satisfaction were assessed with the PROMIS Pediatric Parent-Proxy instruments, which are scored on the PROMIS T-metric (mean = 50, SD = 10). Norm-referenced percentile ranks were derived from nationally representative samples through calibration and centering, such that the 50th percentile represents an average PROMIS T-score of 49.3 (range: 41.4–80.3) for sleep (lower scores reflect better sleep quality); 49.9 (range: 14.7–66.1) for general health (higher scores reflect better health); 55.3 (range: 20.2–59.2) for life satisfaction (higher scores reflect higher life satisfaction); and 46.2 (range: 39.6–82.8) for stress (lower scores reflect lower stress).
Measurements.
Sleep Quality
Sleep Quality was evaluated using the 4-item PROMIS Parent-Proxy Sleep Disturbance Short Form 4a (α=0.79) [32], which evaluates sleep onset, continuity, and satisfaction in the past 7 days on a 5-point Likert scale anchored by never and always. A lower score reflects better sleep quality.
Stress
Stress was evaluated with the 4-item PROMIS Parent-Proxy Psychological Stress Experiences Short Form 4a (α=0.79) [29], which assesses perceptions of feeling overwhelmed and unable to manage general life stress in the past 7 days on a 5-point Likert scale from never to always. A lower score reflects lower stress.
General Health
General Health was measured with the 7-item PROMIS Parent-Proxy Global Health 7 (α=0.78) [28], which provides a global measure of physical, mental, and social health and well-being. The instrument includes 4 omnibus items (e.g., “In general, would you say your child’s health is…”) measured without a specific timeframe on a 5-point Likert scale from excellent to poor and 3 social-emotional items (e.g., “How often does your child have fun with friends?”) measured on a 5-point Likert scale from always to never. A higher score reflects better general health.
Life Satisfaction
Life Satisfaction was assessed with the 4-item PROMIS Parent-Proxy Life Satisfaction Short Form 4a (α=0.87) [27], which assesses overall satisfaction with life in the past 4 weeks on a 5-point Likert scale anchored by not at all and very much. A higher score reflects higher life satisfaction.
We scored PROMIS measures using the standard PROMIS scoring procedures to produce PROMIS T-scores with mean=0 and SD=1. A score of 50 represents the average sleep, general health, life satisfaction, and psychological stress for children based on national samples used for calibration and norming. See [35] for overview of PROMIS scoring and measurement development methods and [27–29, 32] for reliability and validity of measures used in this study.
Sociodemographics
Sociodemographics included child age in years (continuous from 5 to 9), sex (male=1), race, (White, reference; African American; “other race,” representing all other categories with sample sizes too small for individual evaluation), and Hispanic origin (Hispanic=1); annual family income (≤$20,000, reference; $20–40,000; $40–60,000; ≥$60,000); and maternal mental health problems (yes=1), representing whether the mother ever had a mental health problem (e.g., depression, anxiety).
Statistical Analysis.
We used individual patient data meta-analysis by combining child-level data from all three cohorts (validity of and rationale for selecting this approach for this dataset is discussed elsewhere [33]). We conducted bivariate descriptive analyses (i.e., Pearson’s correlations and Analysis of Variance [ANOVA]) to examine associations between PROMIS scores and sociodemographic variables (see Table 2; Supplementary Table 1). We used standard intervals established in the literature to evaluate the strength of correlations (r = 0, no correlation; r = below +/−0.10, low; r = +/−0.30, moderate; r ≥ +/−0.50, large; r = 1, perfect correlation) [36]. Due to floor effects of the sleep quality measure, we conducted Pearson’s chi-square and ANOVAs to evaluate observed differences between children above (“poor” sleep quality) and below (“good” sleep quality) the 50th percentile of nationally normed scores on the PROMIS Parent-Proxy Sleep Disturbance measure (Table 1).
Table 2.
Correlation matrix.
| Sleep | General Health | Life Satisfaction | Stress | Age | |
|---|---|---|---|---|---|
| Sleep | - | ||||
| General health | −0.19** | - | |||
| Life Satisfaction | −0.24** | 0.4** | - | ||
| Stress | 0.38** | −0.47** | −0.32** | - | |
| Age | 0.01 | −0.13** | 0.01 | 0.13** | - |
p<0.01.
To examine the relationship between children’s sleep quality and life satisfaction, we used path modeling with nonparametric bootstrapped standard errors using 1000 replications and normal-based 95% confidence intervals (CI) to account for non-normal distributions of endogenous variables and ensure stability and replicability of model results [37–39]. We controlled for child demographic variables in paths from sleep to stress (path a, Figure 1) and general health (paths b and c, Figure 1) but not for life satisfaction based on extant research showing they exert little influence on this outcome [24–26], particularly for younger children. We also controlled for maternal mental health and annual family income in all paths as these are known environmental factors that contribute to the primary variables of interest [40, 41]. Observations with missing values were omitted from the analysis using case-wise deletion (n=54). Bivariate analyses revealed omitted cases had lower stress F(1249)=8.65; p<0.01and higher life satisfaction F(1249)=6.80; p=0.01, such that models may slightly underestimate relationships (see Supplementary Table 2 for comparisons). However, given the missing cases represent a small proportion of the overall sample, excluding them likely does not strongly influence the final results.
We assessed model fit with x2 significance (p>0.05 suggests good fit) and the ratio of x2 to degrees of freedom (df; values <5 indicate good fit) [42]. Given the susceptibility of x2 metrics to large sample sizes, we examined additional goodness-of-fit indices: Root Mean Square Error of Approximation (RMSEA) <0.06; Comparative Fit Index (CFI) and Tucker-Lewis Index (TLI) >0.95; and Standardized Root Mean Squared Residual (SRMR) <0.08 [42]. We also examined modification indices to determine if model adjustments should be made. Additionally, we tested a model with a direct path from sleep quality to life satisfaction, and replicated the hypothesized models for the subsample of children with poor sleep quality to confirm it accurately characterized this subset of children. See Table 3 for model results, Figure 1 for summarized path coefficients, and Supplementary Table 3 for standardized direct, indirect, and total effects of sleep quality, stress, general health, and life satisfaction.
Table 3.
Path analysis results evaluating whether children’s general health and stress mediate the relationship between sleep quality and life satisfaction for the full sample and subsample of children with above average sleep distance.
| Model 1 - Full Sample | Model 2 - Subsample | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| SE | 95% CI | p-value | SE | 95% CI | p-value | |||||
| LL | UL | LL | UL | |||||||
| Sleep disturbance → Stress | 0.35 | 0.03 | 0.29 | 0.4 | <0.01 | 0.28 | 0.04 | 0.2 | 0.35 | <0.01 |
| Covariates → Stress | ||||||||||
| Age (in years) | 0.08 | 0.03 | 0.02 | 0.13 | <0.01 | 0.08 | 0.03 | 0.01 | 0.15 | 0.02 |
| Sex | ||||||||||
| Female | Ref | Ref | ||||||||
| Male | −0.02 | 0.03 | −0.07 | 0.03 | 0.53 | −0.02 | 0.04 | −0.09 | 0.05 | 0.64 |
| Race | ||||||||||
| White | Ref | Ref | ||||||||
| Black/African American | −0.09 | 0.03 | −0.14 | −0.04 | <0.01 | −0.1 | 0.04 | −0.17 | −0.03 | <0.01 |
| Other race | −0.01 | 0.03 | −0.07 | 0.05 | 0.67 | −0.01 | 0.04 | −0.09 | 0.08 | 0.87 |
| Hispanic origin | ||||||||||
| Non-Hispanic | Ref | Ref | ||||||||
| Hispanic | −0.08 | 0.03 | −0.13 | −0.02 | <0.01 | −0.09 | 0.04 | −0.17 | −0.01 | 0.03 |
| Annual household income | ||||||||||
| $20,000 | Ref | Ref | ||||||||
| $20–40,000 | −0.02 | 0.03 | −0.08 | 0.05 | 0.58 | −0.01 | 0.04 | −0.1 | 0.07 | 0.76 |
| $40–60,000 | −0.03 | 0.04 | −0.1 | 0.05 | 0.45 | −0.09 | 0.05 | −0.18 | 0.01 | 0.08 |
| $60,000 | −0.1 | 0.04 | −0.17 | −0.03 | <0.01 | −0.11 | 0.05 | −0.2 | −0.02 | 0.02 |
| Maternal mental health | ||||||||||
| No problems | Ref | Ref | ||||||||
| Problems | 0.14 | 0.03 | 0.09 | 0.19 | <0.01 | 0.12 | 0.04 | 0.05 | 0.19 | <0.01 |
| Sleep disturbance → General health | −0.11 | 0.03 | −0.16 | −0.05 | <0.01 | −0.03 | 0.04 | −0.1 | 0.04 | <0.01 |
| Stress → General health | −0.32 | 0.03 | −0.38 | −0.27 | <0.01 | −0.35 | 0.04 | −0.42 | −0.28 | 0.36 |
| Covariates → General health | ||||||||||
| Age (in years) | 0.01 | 0.03 | −0.04 | 0.06 | 0.69 | 0 | 0.03 | −0.07 | 0.06 | 0.96 |
| Sex | ||||||||||
| Female | Ref | Ref | ||||||||
| Male | −0.07 | 0.03 | −0.12 | −0.02 | 0.01 | −0.07 | 0.03 | −0.14 | 0 | 0.04 |
| Race | ||||||||||
| White | Ref | Ref | ||||||||
| Black/African American | −0.11 | 0.03 | −0.17 | −0.05 | <0.01 | −0.13 | 0.04 | −0.2 | −0.05 | <0.01 |
| Other race | 0.07 | 0.03 | 0.01 | 0.13 | 0.02 | 0.07 | 0.04 | −0.01 | 0.14 | 0.09 |
| Hispanic origin | ||||||||||
| Non-Hispanic | Ref | Ref | ||||||||
| Hispanic | −0.12 | 0.03 | −0.18 | −0.07 | <0.01 | −0.06 | 0.04 | −0.14 | 0.01 | 0.09 |
| Annual household income | ||||||||||
| $20,000 | Ref | Ref | ||||||||
| $20–40,000 | 0.05 | 0.03 | −0.02 | 0.12 | 0.14 | 0.12 | 0.04 | 0.03 | 0.2 | <0.01 |
| $40–60,000 | 0.14 | 0.04 | 0.07 | 0.21 | <0.01 | 0.2 | 0.05 | 0.11 | 0.29 | <0.01 |
| $60,000 | 0.17 | 0.04 | 0.1 | 0.25 | <0.01 | 0.24 | 0.05 | 0.14 | 0.33 | <0.01 |
| Maternal mental health | ||||||||||
| No problems | Ref | Ref | ||||||||
| Problems | −0.01 | 0.03 | −0.07 | 0.04 | 0.68 | 0 | 0.04 | −0.07 | 0.08 | 0.89 |
| Stress → Life satisfaction | −0.32 | 0.03 | −0.38 | −0.26 | <0.01 | −0.32 | 0.04 | −0.39 | −0.24 | <0.01 |
| General health → Life satisfaction | 0.36 | 0.03 | 0.3 | 0.41 | <0.01 | 0.33 | 0.04 | 0.26 | 0.41 | <0.01 |
| Covariates → Life satisfaction | ||||||||||
| Annual household income | ||||||||||
| $20,000 | Ref | Ref | ||||||||
| $20–40,000 | 0.03 | 0.03 | −0.03 | 0.1 | 0.23 | 0.04 | 0.04 | −0.04 | 0.12 | 0.32 |
| $40–60,000 | 0.02 | 0.03 | −0.04 | 0.08 | 0.55 | 0.02 | 0.04 | −0.06 | 0.11 | 0.57 |
| $60,000 | 0.08 | 0.03 | 0.02 | 0.15 | <0.01 | 0.12 | 0.04 | 0.04 | 0.2 | <0.01 |
| Maternal mental health | ||||||||||
| No problems | Ref | Ref | ||||||||
| Problems | 0 | 0.02 | −0.05 | 0.05 | 0.97 | −0.02 | 0.03 | −0.09 | 0.04 | 0.51 |
| Stress error variance | 0.81 | 0.02 | 0.77 | 0.85 | - | 0.87 | 0.02 | 0.82 | 0.92 | - |
| General health error variance | 0.81 | 0.02 | 0.77 | 0.85 | - | 0.8 | 0.03 | 0.75 | 0.86 | - |
| Life satisfaction error variance | 0.67 | 0.02 | 0.62 | 0.72 | - | 0.68 | 0.03 | 0.62 | 0.74 | - |
-, not applicable.
Abbreviations: SE, Standard Error; 95% CI, 95% Confidence Interval; LL, Lower limit; UL, Upper limit; Ref, reference category.
Note. Results reflect bootstrapped standard errors and normal-based confidence intervals.
Results.
Bivariate analyses.
We summarize results from Pearson correlations (Table 2) and ANOVAs (Supplementary Table 1) below by the main exogenous and endogenous variables in the path models. All statistically significant values were at the p<0.01 level, unless otherwise noted.
Sleep quality
Sleep quality was significantly moderately correlated with life satisfaction (r=−0.24), general health (r=−0.19), and stress (r=0.38), income category F(3)=4.57, and maternal mental health F(1)=9.27, all in the hypothesized directions. Sleep quality was not significantly associated with child age, race, gender, or Hispanic origin. See Table 2 and Supplementary Table 1 for complete results.
General health
General health was significantly moderately correlated with stress (r=−0.32), income F(3)=16.14, and maternal mental health F(1)=10.63, all in the hypothesized directions. Additionally, girls, White and “other race” children, and non-Hispanic children had better general health compared to boys F(1)=4.01; p=0.05, African Americans F(3)=5.17, and non-Hispanic children F(1)=13.87, respectively. General health was not associated with child age. See Table 2 and Supplementary Table 1 for complete results.
Life satisfaction
Life satisfaction was significantly moderately correlated with general health (r=0.4), stress (r=−0.47), income F(3)=10.65, maternal mental health F(1)=10.97, and child age (r=−0.13), all in the hypothesized directions. Additionally, life satisfaction was associated with child race, F(2)=3.30; p=0.04, with African American children having higher life satisfaction compared to White and “other” race children. Alternatively, children’s life satisfaction was not significantly associated with child sex or Hispanic origin. See Table 2 and Supplementary Table 1 for complete results.
Stress
Stress was significantly moderately associated with income F(3)=5.75 and highly correlated with maternal mental health F(1)=43.05, both in the hypothesized directions. Additionally, younger children, African American children, and Hispanic children had lower stress compared to older children (r=−0.13), White and “other” race children F(3)=9.72, and non-Hispanic children F(1)=13.01. Stress was not associated with child sex. See Table 2 and Supplementary Table 1 for complete results.
Full sample analyses.
Results showed children’s sleep quality predicted psychological stress and general health in the hypothesized directions, with excellent model fit (x2(6)=14.03, x2/df=2.34, p=0.03, CFI=0.99, TLI=0.96, RMSEA=0.03, SRMR=0.01; Table 3). Children with poor sleep quality had higher levels of psychological stress (path a) and worse health (path b), as reported by their caregivers. Stress had a negative association with general health (path c) and life satisfaction (path d); in turn, general health positively predicted children’s life satisfaction (path e; see Figure 1). Additionally, the total indirect effect of poor sleep quality on life satisfaction via stress and general health was significant, as was the indirect effect of stress on life satisfaction via general health (Supplementary Table 3). We also tested whether adding a direct path from sleep quality to life satisfaction improved model fit using the likelihood ratio test (LRT), but this additional path did not significantly change model fit (Δdf=1, Δx 2=0.10, p=0.75) and was thus dropped from the model.
Subsample analyses.
Results from secondary analyses with the subsample of children with poor sleep quality (n = 695) confirmed that the original hypothesized model appropriately fit the observed data (x2(6)=10.53, x2/df=1.76, p=0.10, CFI=0.99, TLI=0.95, RMSEA=0.03, SRMR=0.01; Table 3; Figure 1). The path from sleep quality to general health was not significant (path b). Additionally, the total indirect effect of poor sleep quality on life satisfaction via stress and general health was significant, as was the indirect of stress on life satisfaction via general health (Supplementary Table 3). Using the LRT, we examined whether adding a direct path from sleep quality to life satisfaction improved model fit, but the path was not statistically significant (95% CI[0.0, 0.12]), nor did it change model fit (Δdf=1, Δx2 =3.39, p=0.07); therefore, we dropped it from the model and retained the same model as the full sample.
Discussion.
While extant literature primarily focuses on the negative impacts of poor sleep, results from this study add to an emerging body of work examining associations of sleep quality on children’s positive well-being. As numerous studies have established positive relationships between life satisfaction and children’s positive affect, self-esteem, self-confidence, and resiliency [20, 24–26], as well as long-term implications of positive well-being on adult health outcomes [14], the importance of understanding how modifiable factors such as sleep quality directly or indirectly influence children’s well-being cannot be understated.
Findings from the current study suggest better quality sleep is associated with higher life satisfaction via lower psychological stress and better general health; such results remained stable for the subsample of children with poor sleep quality, suggesting the underlying mechanisms by which sleep quality influences well-being are robust across the normal-abnormal sleep quality spectrum. These findings reflect and extend prior theoretical and empirical evidence from adolescent and adult literature [19, 31, 43] to younger children.
Whereas much of the extant literature focuses on stress as a predictor of sleep and sleep as a predictor of general health, we examined stress as a potential mediator of children’s sleep quality and life satisfaction based on studies with adult populations [43, 44]. Conceptualizing poor sleep as a neurobiologic and physiologic stressor that, in turn, increases stress and decreases overall health and well-being, we found a stronger relationship between sleep and psychological stress compared to sleep and general health. This finding is consistent with previous research that identified associations between poor sleep quality and stress dysregulation [6] and elevated blood pressure [7] – an indicator of physiological stress. Further, stress mediated associations between sleep quality and life satisfaction and general health, suggesting that improving sleep quality could lead to improvements in children’s life satisfaction as well as general health via decreasing stress. This is an important message for caregivers, who may understand that adequate sleep and low stress are important for school performance and mood, but may be unaware of the role of sleep quality in possibly decreasing stress and, in turn, enhancing children’s life satisfaction.
Given that children’s stress is among the top health concerns for U.S. parents [45], educating families and communities on sleep’s impact on stress, among other developmental outcomes, could be one path to boosting children’s health and well-being. As [31] noted, however, sleep quality is critical to address above and beyond stress. Such education programs would require concrete strategies for overcoming barriers to high quality sleep at the child, caregiver, and community levels. For example, not having a TV in the bedroom or engaging with digital media in the hour before bedtime are associated with better sleep quality in children [46, 47]. Having a consistent bedtime routine, including reading before bedtime and going to bed before 9pm, and not consuming caffeine are also associated with better sleep quality [47]. Clinicians may be particularly suitable to promote such strategies, as parents are more likely to seek out parenting advice from pediatricians than any other non-familial source [48]. Alternatively, adjusting school start times to accommodate bus schedules has led to decreases in sleep duration and detrimental ramifications on student academic performance and behavior [17], such that broader public policy changes may be required to adequately address children’s sleep quality.
Published data from intervention and education programs have primarily targeted infancy [49], the preschool years [50], and adolescents [51], with less work focused on middle childhood. Additionally, the research literature overwhelmingly focuses on sleep duration as the primary indicator of sleep health, with less attention given to other sleep characteristics that contribute to sleep quality. Further, to date, little-to-no policy-related research (e.g., school start times, homework policies, napping schedules) that may impact the sleep health of 5- to 9-year-olds is available. One study did assess the effects of advancing school start times in school-age children and found increases in behavioral problems, as well as in-school removals, suspensions, and expulsions [52]. Thus, there remain critical gaps in data needed to support making policy recommendations affecting sleep and life satisfaction in young school-age children.
The current study has several limitations that should be considered when interpreting results. First, the data were not nationally representative, such that findings may not generalize to the broader U.S. population. While results for child race were significant, the sample was not representative for a detailed subgroup analysis by race. Additionally, we did not have data on sleep duration (i.e., how many hours of sleep, on average, children got each night), but focused specifically on sleep quality given the lack of prior work on this component of sleep health and suggestions that sleep quality is a unique and equally important contributor to health outcomes than duration [53]. Data came from parental reports of children’s sleep quality, stress, general health, and life satisfaction, versus child self-report. While associations between parent and child reports are low to moderate [54], using parent proxy reports is a common and necessary strategy, particularly for younger children who unable to provide reliable self-reports [35]. Most person-reported outcome measurement tools begin at age 8 for child self-report, and those that obtain self-reports from younger children often require interviewer-administered surveys or qualitative interviews; such methods are not feasible for population health research endeavors. Alternatively, PROMIS parent-proxy instruments are particularly useful for large-scale epidemiological studies such as ECHO, where balancing brief and efficient assessments with scientific rigor are of utmost importance.
Second, the data were cross-sectional, limiting the ability to establish the directionality of the relationship between sleep quality, stress, general health, and life satisfaction. For example, it is plausible that higher stress may lead to poorer sleep and worse health, which in turn could decrease life satisfaction. Most likely, associations between sleep quality and stress are bidirectional in nature during childhood. The current study, however, is a first step in establishing whether sleep quality and life satisfaction are related and identifying potential mediators. Future longitudinal studies are required to determine how and when the associations identified emerge during childhood.
Third, the PROMIS measure aligns with the core sleep quality indicators put forth by the National Sleep Foundation [2], but only includes 1 positively framed item along with 3 negatively framed items. The negative framing is not unique to the PROMIS instrument, as other instruments for children’s sleep health also focus on poor sleep quality [55, 56]. Such an emphasis is consistent with the broader healthcare focus on alleviating suffering.
Finally, this study examined one component of well-being (i.e., life satisfaction), and associations may differ with other components of this multidimensional construct (e.g., positive affect and purpose in life). Given the interrelatedness of such constructs, we expect similar relationships with sleep quality during childhood, but future work can build upon the foundation provided here to examine such associations.
Conclusions.
Overall, this study provides novel insight into associations between sleep quality and children’s life satisfaction, as well as the underlying mechanisms of this relationship. Given the reality that many children who experience disease or illness continue to grow emotionally, cognitively, and behaviorally, and lead fulfilling and satisfying lives [33], the current focus on negative outcomes resulting from poor sleep quality may devalue individuals’ lived experience. Alternatively, adopting a positive health perspective and defining health as more than the absence of disease shifts the focus to processes that promote positive growth and development; this perspective moves beyond traditional healthcare models that seek to treat problems by, instead, placing positive well-being at the center of care.
Supplementary Material
Acknowledgements
The authors wish to thank our ECHO colleagues, the medical, nursing and program staff, as well as the children and families participating in the ECHO cohorts. We also acknowledge the contributions of the following ECHO program collaborators:
Duke Clinical Research Institute (Coordinating Center), Durham, NC: Benjamin, DK, Smith PB, Newby KL, Bristow, H
Medical University of South Carolina, Charleston, SC: Vena JE, Wapner R
National Institutes of Health (ECHO Program Office), Bethesda, MD: Blaisdell, C
Northwestern University (Person Reported Outcomes (PRO) Core), Evanston, IL: Gershon R, Cella D
University of Oregon, Eugene, OR: Leve LD
Funding Source: Research reported in this publication was supported by the Environmental influences on Child Health Outcomes (ECHO) program, Office of The Director, National Institutes of Health, under Award Numbers U2COD023375 (Coordinating Center), U24OD023319 with co-funding from the Office of Behavioral and Social Sciences Research (OBSSR; Person Reported Outcomes Core, Blackwell & Forrest), UG3/UH3OD023313 (LeBourgeois & Hartstein); UG3/UH3OD023279 (Elliott), UG3/UH3OD023389 (Ganiban), UG3OD023316 (Hunt), and UG3/UH3OD023253 (Camargo). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Abbreviations:
- ANOVA
Analysis of Variance
- CFI
Comparative Fit Index
- CI
confidence interval
- ECHO
Environmental influences on Child Health Outcomes
- HRQoL
Health-Related Quality of Life
- LRT
Likelihood Ratio Test
- NIH
National Institutes of Health
- PROMIS
Patient-Reported Outcomes Measurement Information System
- RMSEA
Root Mean Square Error of Approximation
- SD
Standard Deviation
- SRMR
Standardized Root Mean Squared Residual
- TLI
Tucker-Lewis Index
Footnotes
Publisher's Disclaimer: This Author Accepted Manuscript is a PDF file of an unedited peer-reviewed manuscript that has been accepted for publication but has not been copyedited or corrected. The official version of record that is published in the journal is kept up to date and so may therefore differ from this version.
Financial Disclosure: The authors have no financial relationships relevant to this article to disclose.
Conflict of Interest: The authors have no conflicts of interest relevant to this article to disclose.
References
- 1.Buysse DJ, Sleep health: can we define it? Does it matter? Sleep, 2014. 37(1): p. 9–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ohayon M, et al. , National Sleep Foundation’s sleep quality recommendations: first report. 2017. 3(1): p. 6–19. [DOI] [PubMed] [Google Scholar]
- 3.US Department of Health and Human Services. 2020 Topics & Objectives: Sleep Health. 2014: Washington, DC;. [Google Scholar]
- 4.US Department of Health and Human Services. Secretary’s Advisory Committee on National Health Promotion and Disease Prevention Objectives for 2030 Report #7: Assessment and Recommendations for Proposed Objectives for Healthy People 2030. 2019: Washington, DC;. [Google Scholar]
- 5.Hawkins SS and Takeuchi DT, Social determinants of inadequate sleep in US children and adolescents. Public Health. 138: p. 119–126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hatzinger M, et al. , Electroencephalographic sleep profiles and hypothalamic-pituitary-adrenocortical (HPA)-activity in kindergarten children: early indication of poor sleep quality associated with increased cortisol secretion. J Psychiatr Res, 2008. 42(7): p. 532–43. [DOI] [PubMed] [Google Scholar]
- 7.Javaheri S, et al. , Sleep quality and elevated blood pressure in adolescents. Circulation, 2008. 118(10): p. 1034–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Van Cauter E and Knutson KL, Sleep and the epidemic of obesity in children and adults. Eur J Endocrinol, 2008. 159 Suppl 1: p. S59–66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Gregory AM and Sadeh A, Sleep, emotional and behavioral difficulties in children and adolescents. Sleep Medicine Reviews, 2012. 16(2): p. 129–136. [DOI] [PubMed] [Google Scholar]
- 10.Beebe DW, Cognitive, behavioral, and functional consequences of inadequate sleep in children and adolescents. Pediatr Clin North Am, 2011. 58(3): p. 649–65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Matricciani L, et al. , Children’s sleep and health: A meta-review. Sleep medicine reviews, 2019. 46: p. 136–150. [DOI] [PubMed] [Google Scholar]
- 12.Wong MM, et al. , Sleep Problems in Early Childhood and Early Onset of Alcohol and Other Drug Use in Adolescence. Alcoholism: Clinical & Experimental Research, 2004. 28(4): p. 578–587. [DOI] [PubMed] [Google Scholar]
- 13.Reidy BL, et al. , Prospective associations between chronic youth sleep problems and young adult health. Sleep Health, 2016. 2(1): p. 69–74. [DOI] [PubMed] [Google Scholar]
- 14.Richards M and Huppert FA, Do positive children become positive adults? Evidence from a longitudinal birth cohort study. J Posit Psychol, 2011. 6(1): p. 75–87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Steptoe A, et al. , Positive affect, psychological well-being, and good sleep. J Psychosom Res, 2008. 64(4): p. 409–15. [DOI] [PubMed] [Google Scholar]
- 16.Strine TW and Chapman D.P.J.S.m., Associations of frequent sleep insufficiency with health-related quality of life and health behaviors. 2005. 6(1): p. 23–27. [DOI] [PubMed] [Google Scholar]
- 17.Perkinson-Gloor N, Lemola S, and Grob A, Sleep duration, positive attitude toward life, and academic achievement: the role of daytime tiredness, behavioral persistence, and school start times. J Adolesc, 2013. 36(2): p. 311–8. [DOI] [PubMed] [Google Scholar]
- 18.Roberts RE, Roberts CR, and Duong HT, Sleepless in adolescence: prospective data on sleep deprivation, health and functioning. J Adolesc, 2009. 32(5): p. 1045–57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Magee CA, Robinson L, and Keane C, Sleep quality subtypes predict health-related quality of life in children. Sleep Med, 2017. 35: p. 67–73. [DOI] [PubMed] [Google Scholar]
- 20.Huebner ES, Initial Development of the Student’s Life Satisfaction Scale. School Psychology International, 1991. 12: p. 231–240. [Google Scholar]
- 21.Huebner ES, Preliminary development and validation of a multidimensional life satisfaction scale for children. Psychological Assessment, 1994. 6(2): p. 149–158. [Google Scholar]
- 22.Bevans KB, Riley AW, and Forrest CB, Development of the healthy pathways child-report scales. Quality of Life Research, 2010. 19(8): p. 1195–1214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Bevans KB, Riley AW, and Forrest CB, Development of the healthy pathways parent-report scales. Quality of Life Research, 2012. 21(10): p. 1755–1770. [DOI] [PubMed] [Google Scholar]
- 24.Proctor CL, Linley PA, and Maltby J, Youth life satisfaction: A review of the literature. Journal of Happiness Studies, 2009. 10: p. 583–630. [Google Scholar]
- 25.Huebner ES, et al. , Life satisfaction in children and youth: Empirical foundations and implications for school psychologists. Psychology in the Schools, 2004. 41(1): p. 81–93. [Google Scholar]
- 26.Gilman R and Huebner S, A review of life satisfaction research with children and adolescents. Sch Psych Q, 2003. 18: p. 192–205. [Google Scholar]
- 27.Forrest CB, et al. , Development and psychometric evaluation of the PROMIS® Pediatric Life Satisfaction item banks, child-report, and parent-proxy editions. Qual Life Res, 2018. 27(1): p. 217–234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Forrest CB, et al. , Development of the PROMIS® pediatric global health (PGH-7) measure. Qual Life Res, 2014. 23(4): p. 1221–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Bevans KB, et al. , Psychometric Evaluation of the PROMIS® Pediatric Psychological and Physical Stress Experiences Measures. J Pediatr Psychol, 2018. 43(6): p. 678–692. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Suldo SM and Huebner ES, Does life satisfaction moderate the effects of stressful life events on psychopathological behavior during adolescence? School Psychology Quarterly, 2004. 19(2): p. 93–105. [Google Scholar]
- 31.Benham G, Sleep: an important factor in stress-health models. Stress and Health, 2010. 26(3): p. 204–214. [Google Scholar]
- 32.Forrest CB, et al. , Development and validation of the PROMIS® Pediatric Sleep Disturbance and Sleep-Related Impairment item banks. Sleep, 2018. 41(6). [DOI] [PubMed] [Google Scholar]
- 33.Blackwell CK, et al. , for the ECHO Consortium. General health and life satisfaction in children with chronic illness. Pediatrics, 2019. 143(6): p. e20182988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Gillman MW and Blaisdell CJ, Environmental influences on child health outcomes, a research program of the National Institutes of Health. Current opinion in pediatrics, 2018. 30(2): p. 260–2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Forrest CB, et al. , Commentary: the patient-reported outcome measurement information system (PROMIS®) for children and youth: application to pediatric psychology. 2012. 37(6): p. 614–621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Cohen J, Statistical power analysis for the behavioral sciences. 2nd ed. 1988, Hillsdale, NJ: Erlbaum. [Google Scholar]
- 37.Kline RB, Principles and practice of structural equation modeling. 4th ed. 2016, New York, NY: Guilford Publications. [Google Scholar]
- 38.Yung YF and Bentler PM, Bootstrapping techniques in analysis of mean and covariance structures, in Advanced structural equation modeling: Issues and techniques, Marcoulides GA and Schumacker RE, Editors. 1996, Lawrence Erlbaum Associates, Inc.: New York, NY: p. 195–226. [Google Scholar]
- 39.Fan X, Using commonly available software for bootstrapping in both substantive and measurement analyses. Educational and Psychological Measurement, 2003. 63(1): p. 24–50. [Google Scholar]
- 40.Gitterman BA, et al. , Poverty and child health in the United States. 2016. 137(4): p. peds. 2016–0339. [DOI] [PubMed] [Google Scholar]
- 41.Bannink R, Pearce A, and Hope S, Family income and young adolescents’ perceived social position: Associations with self-esteem and life satisfaction in the UK Millennium Cohort Study. Archives Disease Childhood, 2016. 101(10): p. 917–921 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Hu L.t. and Bentler PM, Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Structural Equation Modeling: A Multidisciplinary Journal, 1999. 6(1): p. 1–55. [Google Scholar]
- 43.McEwen BS, Sleep deprivation as a neurobiologic and physiologic stressor: allostasis and allostatic load. Metabolism, 2006. 55: p. S20–S23. [DOI] [PubMed] [Google Scholar]
- 44.Barber LK and Munz DC, Consistent-sufficient sleep predicts improvements in self-regulatory performance and psychological strain. Stress and Health, 2011. 27(4): p. 314–324. [Google Scholar]
- 45.Mott CS Children’s Hospital National Poll on Children’s Health. 2017.
- 46.Hale L, et al. , Youth screen media habits and sleep: sleep-friendly screen behavior recommendations for clinicians, Educators, and Parents. Child and Adolescent Psychiatric Clinics, 2018. 27(2): p. 229–245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Mindell JA, M. L, Carskadon MA, Chervin RD., Developmental aspects of sleep hygiene: findings from the 2004 National Sleep Foundation Sleep in America Poll. Sleep medicine, 2009. 10(7): p. 771–779. [DOI] [PubMed] [Google Scholar]
- 48.Wartella EA, et al. , Parenting in the Age of Digital Technology: A National Survey. 2013, Center on Media and Human Development, School of Communication, Northwestern University: Evanston, IL. [Google Scholar]
- 49.Taylor B, et al. , Prevention of Overweight in Infancy (POI. nz) study: a randomised controlled trial of sleep, food and activity interventions for preventing overweight from birth. BMC Public Health, 2011. 11(1). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Garrison M and Christakis D, The impact of a healthy media use intervention on sleep in preschool children. Pediatrics, 2012. 130(2): p. 492–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Bowers J and Moyer A, Effects of school start time on students’ sleep duration, daytime sleepiness, and attendance: a meta-analysis. Sleep health, 2017. 3(6): p. 423–31. [DOI] [PubMed] [Google Scholar]
- 52.Keller P, et al. , Earlier school start times are associated with higher rates of behavioral problems in elementary schools. Sleep health, 2017. 3(2): p. 113–8. [DOI] [PubMed] [Google Scholar]
- 53.Bin YS, Is sleep quality more important than sleep duration for public health? SLEEP, 2016. 39(9): p. 1629–1630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Upton P, Lawford J, and Eiser C.J.Q.o.l.r., Parent–child agreement across child health-related quality of life instruments: a review of the literature. 2008. 17(6): p. 895. [DOI] [PubMed] [Google Scholar]
- 55.McGreavey J, et al. , The Tayside children’s sleep questionnaire: a simple tool to evaluate sleep problems in young children. 2005. 31(5): p. 539–544. [DOI] [PubMed] [Google Scholar]
- 56.Bruni O, et al. , The Sleep Disturbance Scale for Children (SDSC) Construct ion and validation of an instrument to evaluate sleep disturbances in childhood and adolescence. 1996. 5(4): p. 251–261. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


