Abstract
Background
We studied the effect of age, baseline viral load, vaccination status, antiviral therapy, and emergence of drug resistance on viral shedding in children infected with influenza A or B virus.
Methods
Samples from children (aged ≤13 years) enrolled during the 7 years of the prospective Influenza Resistance Information Study were analyzed using polymerase chain reaction to determine the influenza virus (sub-)type, viral load, and resistance mutations. Disease severity was assessed; clinical symptoms were recorded. The association of age with viral load and viral clearance was examined by determining the area under the curve for viral RNA shedding using logistic regression and Kaplan-Meier analyses.
Results
A total of 2131 children infected with influenza (683, A/H1N1pdm09; 825, A/H3N2; 623, influenza B) were investigated. Age did not affect the mean baseline viral load. Children aged 1−5 years had prolonged viral RNA shedding (±1–2 days) compared with older children and up to 1.2-fold higher total viral burden. Besides, in older age (odds ratio [OR], 1.08; confidence interval [CI], 1.05–1.12), prior vaccination status (OR, 1.72; CI, 1.22–2.43) and antiviral treatment (OR, 1.74; CI, 1.43–2.12) increased the rate of viral clearance. Resistance mutations were detected in 49 children infected with influenza A virus (34, A/H1N1pdm09; 15, A/H3N2) treated with oseltamivir, most of whom were aged <5 years (n = 39).
Conclusions
Children aged 1−5 years had a higher total viral burden with prolonged virus shedding and had an increased risk of acquiring resistance mutations following antiviral treatment.
Clinical Trials Registration
Keywords: influenza, pediatrics, Influenza Resistance Information Study, viral load, resistance mutations
We demonstrate that children aged 1−5 years shed a 1.04- to 1.24-fold higher total quantity of influenza virus compared with older children associated with an increased risk of acquiring resistance mutations following antiviral treatment.
Children are more likely than adults to be infected with influenza virus during epidemics [1]. Annually, pediatric infections are associated with a high number of emergency room visits and hospitalizations [2–5]. This susceptibility of children to influenza virus infection largely results from the absence of preexisting acquired immunity [6, 7]. Thus, children can serve as a major reservoir for further prolongation of outbreaks in the community [8–10]. Although several studies report prolonged influenza virus replication in children compared with adults, this finding is not consistently reported and remains to be elucidated [1, 8–14].
To gain further insight into the drivers of pediatric viral replication and antiviral resistance, studies with sufficient numbers of patients are needed to compare kinetics between the different age strata. The Influenza Resistance Information Study (IRIS) provided a unique opportunity to capitalize on the knowledge of influenza viral kinetics and the incidence of antiviral resistance in children [15–17]. With more than 2000 children included, it was possible to analyze the effect of age, baseline viral load, antiviral usage, emergence of resistance, and vaccination status of children on viral shedding and clearance for influenza A (A/H1N1pdm09, A/H3N2) and influenza B viruses.
METHODS
Study Design
IRIS was a prospective, multicenter, nonrandomized study undertaken from 2008 to 2015. Study participants were enrolled from Europe, the United States, China (Hong Kong), Australia, and South Africa. The study was implemented in compliance with the principles of the Declaration of Helsinki and its amendments and in accordance with Good Clinical Practice. Written informed consent was obtained from all study participants and/or their legal guardians. Local ethics committees and institutional review boards approved the study protocol and amendments.
Inclusion Criteria and Clinical Assessment
A detailed description of the study procedures has been previously published [15, 17]. In brief, during the first 5 years of IRIS (December 2008 to March 2013), both adults and children aged ≥1 year were eligible for enrollment when positive for influenza virus by rapid test and/or upon display of influenza-like signs and symptoms within 48 hours (≤96 hours for hospitalized adults, no time limit for hospitalized children) [15]. Since resistance mutations were more prevalent in children during the first 5 years of the study, the inclusion criteria for the last 2 years of the study (March 2013 to September 2015) were modified to recruit only children aged ≤13 years on antiviral treatment. Clinical management, including prescription of antivirals, was at the discretion of the healthcare provider.
For clinical assessment, patients were evaluated on days 1 (study enrollment), 6, and 10. Influenza signs and symptoms were assessed by investigators at each center using a 4-point scale [15]. Temperature (oral or tympanic) and adverse events (AEs) were recorded daily on diary cards. In the last 2 years of the study, baseline and follow-up symptom assessments were conducted by the study physicians, but diary cards were not obtained.
Virological Assessment
Qualitative, quantitative, and mutation-specific real-time reverse transcriptase polymerase chain reaction (RT-PCR) was performed on collected nasal and throat swabs on days 1 (study enrollment), 3, 6, and 10 to determine the influenza virus (sub-)type, viral load, and resistance mutations in the neuraminidase (NA) gene (H275Y, R292K, E119V, R150K, D197N, N294S) [15, 17]. Viral RNA loads (RNA copies [log10/mL]) were determined by converting the cycle threshold value to viral particle counts (viral RNA copies), by processing electron microcopy–counted influenza A/Puerto Rico/8/34, and B/Lee/40 virus stocks (Advanced Biotechnologies Inc, Maryland) in parallel to the patient samples.
Statistical Analyses
Data from all children enrolled during the entire 7 years of IRIS were evaluated. Patients who received more than 1 NA inhibitor treatment or other antivirals were excluded. Children were stratified into age groups according to presumed immunity development [6, 7]: ≤6 months, 6 months−1 year, 1−3 years, 3−5 years, 5−10 years, and 10−13 years.
Continuous data, such as viral load, were summarized as means and standard deviations (SDs); medians and ranges were calculated/reported to 1 decimal point. Categorical data were summarized as frequency and percentage of the appropriate study population. The area under the curve (AUC) of the virus load was determined using the trapezoid rule. The Student t test was used to compare AUC values between age groups.
Logistic multivariable analyses were performed to explore the associations between duration of viral RNA detection and baseline viral load, age (years), antiviral treatment, virus subtype, influenza virus vaccination status during the previous 4 months, and emergence of resistance in the postbaseline samples. The dependent variable was “cleared” or “not cleared” depending on RNA detection on day 6. The associations of emergence of resistance mutations with baseline viral load, age (years), and influenza virus subtype were analyzed using a regression analysis. Results of the regression analyses are shown as odd ratios (ORs) and confidence intervals (CIs) with significance determined by χ 2 test.
Kaplan-Meier plots for time to nondetection of viral RNA by quantitative RT-PCR and for time to symptom resolution were generated for various age strata using the recorded symptoms diary cards of children aged ≥1 year. Data were censored at the date of the last available sample, if patients were lost to follow-up, if samples were inadequate, or if RNA was still detected at the final visit. Wilcoxon and log-rank tests were used to compare outcomes between the age groups and influenza virus (sub-)type.
RESULTS
Patient Characteristics and Demographics
A total of 2131 children aged ≤13 years tested positive for a single influenza virus (sub-)type by RT-PCR (see Supplementary Figure 1 for study flow chart). Baseline characteristics stratified by age are summarized in Table 1 and Supplementary Tables 1 and 2 [6]. Relatively few infants (aged <1 year) were included in IRIS and were positive for influenza virus (N = 23). A total of 683 children were infected with A/H1N1pdm09, 825 with A/H3N2, and 623 with influenza B virus. No infants aged 6 months−1 year had influenza B virus infection. Gender was distributed similarly across all age groups. The majority of children received antivirals (61%). Pulmonary (13.4%) and cardiovascular (0.8%) comorbidities were relatively uncommon, as was influenza vaccination coverage in the previous 4 months (8.3%).
Table 1.
Clinical Characteristics of Children With Laboratory-confirmed Influenza at Baseline
| Patients Characteristic | Age Group | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Total | <6 Months | 6 Months–1 Year | 1–3 Years | 3–5 Years | 5–10 Years | 10–13 Years | |||||||
| (N = 2131) | (n = 12) | (n = 11) | (n = 369) | (n = 473) | (n = 936) | (n = 330) | |||||||
| Virus (sub-)type | |||||||||||||
| A/H1N1pdm09 | 683 (32.1%) | 4 (33.3%) | 7 (63.6%) | 151 (40.9%) | 158 (33.4%) | 270 (28.8%) | 93 (28.2%) | ||||||
| A/H3N2 | 825 (38.7%) | 6 (50.0%) | 4 (36.4%) | 150 (40.7%) | 214 (45.2%) | 335 (35.8%) | 116 (35.2%) | ||||||
| Influenza B | 623 (29.2%) | 2 (16.7%) | 0 (0.0) | 68 (18.4%) | 101 (21.4%) | 331 (35.4%) | 121 (36.7%) | ||||||
| Country | |||||||||||||
| France | 396 (18.6%) | 0 (0.0) | 0 (0.0) | 60 (16.3%) | 88 (18.6%) | 186 (19.9%) | 62 (18.8%) | ||||||
| Germany | 41 (1.9%) | 0 (0.0) | 0 (0.0) | 4 (1.1%) | 15 (3.2%) | 15 (1.6%) | 7 (2.1%) | ||||||
| Norway | 3 (0.1%) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 1 (0.2%) | 2 (0.2%) | 0 (0.0) | ||||||
| Poland | 573 (26.9%) | 0 (0.0) | 0 (0.0) | 139 (37.7%) | 169 (35.7%) | 210 (22.4%) | 55 (16.7%) | ||||||
| United States | 695 (32.6%) | 12 (100%) | 10 (90.9%) | 88 (23.8%) | 111 (23.5%) | 336 (35.9%) | 138 (41.8%) | ||||||
| China (Hong Kong [Special Administrative Region of the People’s Republic of China]) | 369 (17.3%) | 0 (0.0) | 0 (0.0) | 61 (16.5%) | 76 (16.1%) | 170 (18.2%) | 62 (18.8%) | ||||||
| South Africa | 22 (1.0%) | 0 (0.0) | 1 (9.1%) | 6 (1.6%) | 5 (1.1%) | 8 (0.9%) | 2 (0.6%) | ||||||
| Australia | 32 (1.5%) | 0 (0.0) | 0 (0.0) | 11 (3.0) | 8 (1.7) | 9 (1.0) | 4 (1.2) | ||||||
| Gender | |||||||||||||
| Female | 1031 (48.4%) | 7 (58.3%) | 5 (45.5%) | 183 (49.6%) | 236 (49.9%) | 455 (48.6%) | 145 (43.9%) | ||||||
| Male | 1100 (51.6%) | 5 (41.7%) | 6 (54.5%) | 186 (50.4%) | 237 (50.1%) | 481 (51.4%) | 185 (56.1%) | ||||||
| Antiviral treatment | |||||||||||||
| No | 831 (39.0%) | 0 (0.0) | 0 (0.0) | 140 (37.9%) | 210 (44.4%) | 360 (38.5%) | 121 (36.7%) | ||||||
| Yes | 1300 (61.0%) | 12 (100%) | 11 (100%) | 229 (62.1%) | 263 (55.6%) | 576 (61.5%) | 209 (63.3%) | ||||||
| Febrilea | |||||||||||||
| No | 827 (38.8%) | 9 (75.0%) | 5 (45.5%) | 137 (37.1%) | 165 (34.9%) | 366 (39.1%) | 145 (43.9%) | ||||||
| Yes | 1303 (61.1%) | 3 (25.0%) | 6 (54.5%) | 232 (62.9%) | 308 (65.1%) | 570 (60.9%) | 184 (55.8%) | ||||||
| Cardiovascular disease | |||||||||||||
| No | 2115 (99.2%) | 12 (100%) | 11 (100%) | 365 (98.9%) | 468 (98.9%) | 931 (99.5%) | 328 (99.4%) | ||||||
| Yes | 16 (0.8%) | 0 (0.0) | 0 (0.0) | 4 (1.1%) | 5 (1.1%) | 5 (0.5%) | 2 (0.6%) | ||||||
| Pulmonary disease | |||||||||||||
| No | 1846 (86.6%) | 12 (100%) | 10 (90.9%) | 339 (91.9%) | 424 (89.6%) | 791 (84.5%) | 270 (81.8%) | ||||||
| Yes | 285 (13.4%) | 0 (0.0) | 1 (9.1%) | 30 (8.1%) | 49 (10.4%) | 145 (15.5%) | 60 (18.2%) | ||||||
| Vaccinated in previous 4 monthsb | |||||||||||||
| No | 1952 (91.6%) | 12 (100%) | 7 (63.6%) | 333 (90.2%) | 451 (95.3%) | 851 (90.9%) | 298 (90.3%) | ||||||
| Yes | 177 (8.3%) | 0 (0.0) | 4 (36.4%) | 35 (9.5%) | 22 (4.7%) | 85 (9.1%) | 31 (9.4%) | ||||||
| Time from symptom onset to study baseline, mean (standard deviation), days | 1.2 (0.77) | 1.6 (0.90) | 1.4 (0.67) | 1.1 (0.75%) | 1.2 (0.94) | 1.2 (0.70) | 1.2 (0.68) | ||||||
aTotal N = 2130, febrile status of 1 patient was not reported.
bTotal N = 2129, vaccination status of 3 patients was not reported.
Virological Kinetics
Baseline Viral RNA Load
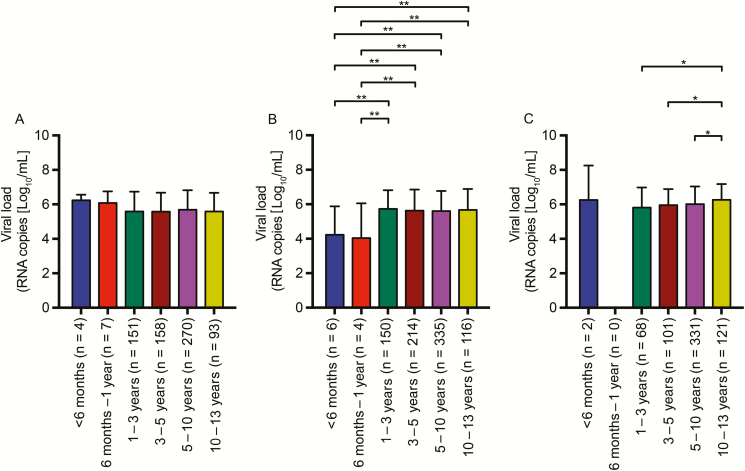
The mean viral RNA loads (RNA copies [log10/mL]) at the day of study enrollment (baseline) of all children infected with A/H1N1pdm09 and A/H3N2 virus were comparable, except in the small group of infants infected with A/H3N2 virus (Figure 1). Children aged 10−13 years (6.3 log10/mL) infected with influenza B virus had a significantly higher baseline viral load compared with children aged 1−10 years (range, 5.8–6.0 log10/mL; *.05 > P > .01).
Figure 1.
Baseline viral RNA load of children infected with A/H1N1pdm09, A/H3N2, and influenza B virus. The mean baseline viral RNA load of children infected with A/H1N1pdm09 (A), A/H3N2 (B), and influenza B virus (C) are depicted as mean ± standard deviation. Influenza B virus was not detected in infants aged 6 months−1 year. Asterisks represent significant P values (*.05 < P < .01 and **.01 > P > .001).
Viral RNA Clearance
The change in viral RNA load over time relative to the baseline viral load was calculated for all children in order to determine the rate of viral RNA clearance (Table 2). In most cases, children aged 10−13 years cleared viral RNA faster than younger children. For A/H1N1pdm09 virus, the higher rate of viral load reduction in older children was only significant at day 6. For A/H3N2 and influenza B virus, this effect remained significant until day 10 postbaseline.
Table 2.
Postbaseline Mean Viral Load (RNA Copies Log10/mL) Change from Baseline
| Influenza Virus (Sub)-Type | Time Postbaseline Enrollment (day) | Totala | Age Group | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| <6 Months | 6 Months–1 Year | 1–3 Years | 3–5 Years | 5–10 Years | 10–13 Years | |||||||||
| (N = 2131) | (n = 4) | (n = 7) | (n = 151) | (n = 158) | (n = 270) | (n = 93) | ||||||||
| A/H1N1pdm09 | 3 | 650 | −1.04 (1.37) | −1.00 (1.52) | −1.52 (1.80) | −1.50 (1.70) | −1.70 (1.75) | −2.08 (1.74) | ||||||
| 6* | 662 | −1.35 (1.58) | −3.12 (1.18) | −3.36 (2.25) | −3.48 (2.13) | −3.93 (1.95) | −4.18 (2.12) | |||||||
| 10 | 654 | −3.77 (1.70) | −5.74 (0.85) | −5.01 (1.66) | −4.85 (1.66) | −5.06 (1.50) | −5.07 (1.57) | |||||||
| A/H3N2 | 3** | 789 | −0.97 (2.42) | −1.32 (0.92) | −1.77 (1.79) | −1.59 (1.85) | −2.11 (1.77) | −2.18 (1.86) | ||||||
| 6*** | 792 | −3.49 (0.98) | −4.04 (2.01) | −3.11 (2.09) | −3.08 (2.09) | −3.97 (1.85) | −3.85 (2.07) | |||||||
| 10* | 785 | −3.97 (0.85) | −4.04 (2.01) | −5.21 (1.45) | −4.82 (1.69) | −5.10 (1.50) | −5.26 (1.46) | |||||||
| Influenza Bb | 3* | 601 | −0.93 (0.64) | … | −1.05 (1.53) | −1.23 (1.88) | −1.31 (1.85) | −1.83 (1.94) | ||||||
| 6** | 599 | −3.39 (1.07) | … | −3.25 (2.22) | −3.52 (2.14) | −3.43 (2.18) | −4.25 (1.94) | |||||||
| 10** | 592 | −6.25 (0.16) | … | −4.87 (1.89) | −5.20 (1.64) | −5.08 (1.80) | −5.76 (1.34) | |||||||
Data depicted are the mean viral load (RNA copies log10/mL) and in brackets, the standard deviation. Reduction in the virus RNA loads (RNA copies log10/mL) are shown as minus values. The highest reduction in mean viral RNA load relative to baseline of children infected with A/H1N1pdm09 virus, A/H3N2 virus, and influenza B virus are marked in bold.
aThe total N swabs collected at each time point.
bInfluenza B virus was not detected in infants aged 6 months–1 year.
*Asterisks depict the postbaseline sample day in which the analysis of variance within the age groups was significant (*.05 < P < .01, **.01 > P > .001, and ***P < .0001).
When corrected for the date of symptom onset, children aged 10−13 years infected with A/H1N1pdm09 and A/H3N2 cleared the virus faster than younger children if they were enrolled on the day that symptoms first occurred (n = 270; Supplementary Figure 2A). A/H3N2 virus–infected children aged 10–13 years showed a similar trend even if they were enrolled ≥3 days after symptom onset (Supplementary Figure 2D and 2E). At longer time periods between study enrollment and disease onset, the difference in viral RNA load reduction was no longer observed between the different age groups (Supplementary Figure 2B–2E).
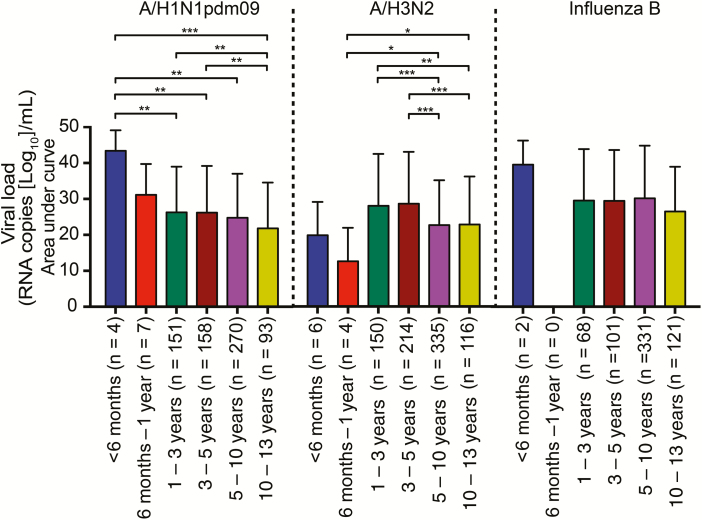
Total Quantified Viral RNA Load in Time
The mean AUC of the viral load was calculated over the course of infection (Figure 2). A/H1N1pdm09-infected infants (aged <1 year; 37.3 log10/mL*time) and young children (aged 1−5 years; 26.2 log10/mL*time) had significantly higher mean AUCs of 1.60- and 1.12-fold, respectively, than older children (aged >5 years; 23.3 log10/mL*time) (**.01 > P > .001 and ***P < .001). The same trend was observed for influenza B virus infection with a 1.37- and 1.04-fold larger total mean quantity of virus detected in infants (aged <6 months; 39.6 log10/mL*time) and young children (aged 1−5 years; 29.5 log10/mL*time), respectively, compared with older children (aged >5 years; 28.4 log10/mL*time). Infants (aged <1 year; 16.2 log10/mL*time) infected with A/H3N2 virus shed a smaller amount of virus than older children (*.05 > P > .01). The mean AUCs of A/H3N2 virus–infected children aged 1−5 years (28.3 log10/mL*time) were 1.24-fold higher compared with older children (22.8 log10/mL*time; **.01 > P > .001 and ***P < .001). When corrected for treatment status, these age-related effects on the total quantity of viral RNA load persisted (Supplementary Figure 3).
Figure 2.
Total viral RNA load of children infected with A/H1N1pdm09, A/H3N2, and influenza B virus. The total amount of viral RNA shedding in children infected with A/H1N1pdm09, A/H3N2, and influenza B virus was determined by calculating the area under the curve. Influenza B virus was not detected in infants aged 6 months−1 year. The bar graphs depict the mean ± standard deviation. Asterisks represent significant P values (*.05 < P < .01, **.01 > P > .001, ***P < .001).
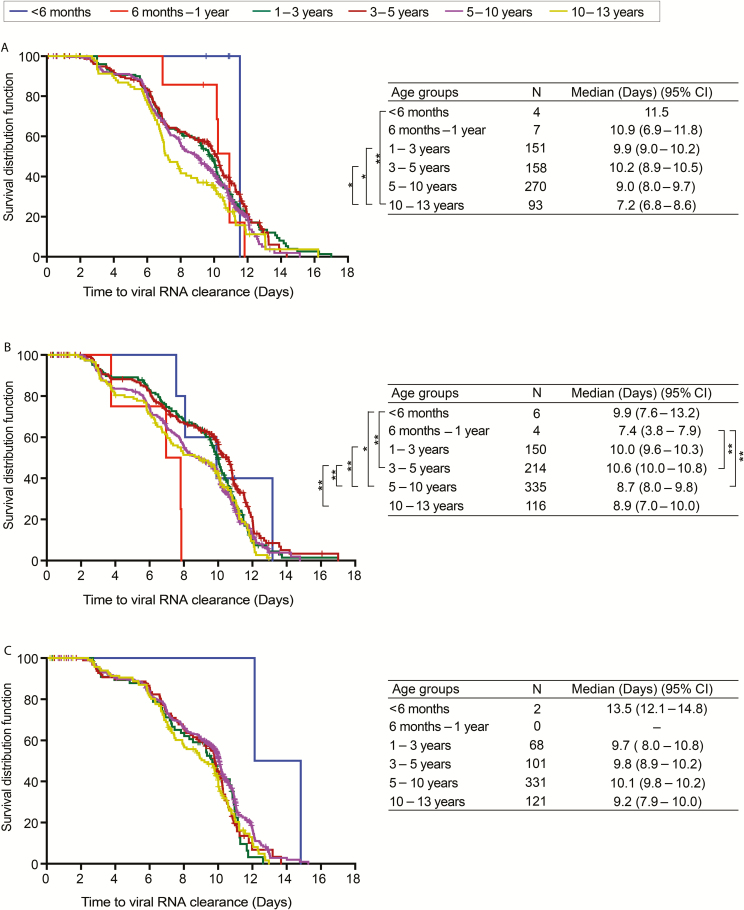
Time to Nondetection of Viral RNA
The median time to A/H1N1pdm09 virus RNA clearance was longest for young children (aged <5 years [N = 320]; median range, 9.9–11.5 days) compared with older children (aged >5 years [N = 363]; median range, 7.2–9.0 days; Figure 3A). Viral RNA clearance in A/H3N2 virus–infected older children (aged >5 years [N = 451]; median range, 8.7–8.9 days) was faster compared with younger children (aged 1−5 years [N = 364]; median range, 10.0–10.6 days). Infants (aged 6 months−1 year) cleared the A/H3N2 virus faster than all other children (Figure 3B). Older children infected with influenza B virus also tended to clear the virus faster than younger children; however, these differences were not statistically significant (Figure 3C).
Figure 3.
Kaplan-Meier plots for time to viral RNA clearance of children infected with H1N1pmd09 (A), A/H3N2 (B), and influenza B virus (C). Censored patients are illustrated as plus signs. The median time to viral RNA clearance in each age group is depicted next to the Kaplan-Meier plots. Influenza B virus was not detected in infants aged 6 months−1 year. Asterisks represent significant P values (*.05 < P < .01 and **.01 > P > .001). Abbreviation: CI, confidence interval.
Variables Associated With Viral RNA Clearance
Logistic regression analyses confirmed the relationship between duration of virus shedding and older age (OR, 1.08; CI, 1.05–1.12; P < .0001). Additionally, vaccination (OR, 1.72; CI, 1.22–2.43; P = .0017) and antiviral treatment (OR, 1.74; CI, 1.43–2.12; P < .0001) were associated with shorter duration of virus shedding. High baseline viral loads (OR, 0.57; CI, .52–.62; P < .0001) and the emergence of resistance mutations (OR, 0.05; CI, .01–.20; P < .0001) were independently associated with longer duration of virus shedding. Infection with A/H3N2 (OR, 0.71; CI, .57–.90; P = .01) or influenza B virus (OR, 0.78; CI, .61–.99; P = .01) decreased the odds of viral RNA clearance compared with infection with A/H1N1pdm09 virus.
Clinical Symptoms
Clinical signs were mild, and complications were relatively rare. A total of 185 (8.7%) patients reported AEs. Of these, 117 (9.0%) received antiviral therapy and 68 (8.2%) were untreated (Supplementary Tables 3 and 4). The incidence of AEs was the highest for young children (aged <5 years). Serious AEs were reported in 14 (0.7%) children, of whom 10 (0.8%) received oseltamivir treatment and 4 (0.5%) were untreated (Supplementary Tables 5 and 6). Two children were admitted to the intensive care unit (ICU), one 5-month-old infant and one 8-year-old child. Both were treated with oseltamivir and recovered.
The duration of symptoms of older children infected with A/H1N1pdm09 and A/H3N2 (aged >5 years; median range, 4–5 days) was shorter compared with younger children (aged <5 years; median range, 5–6 days; *.05 > P > .01 and **.01 > P > .001) (Supplementary Figure 4). This age-related difference in symptom duration was less pronounced when infected children were stratified according to their antiviral treatment status (Supplementary Figures 5 and 6). There was no significant observed difference in symptom resolution between the age groups of all children infected with influenza B virus (Supplementary Figures 4−6).
Emergence of Resistance
Neuraminidase inhibitor–associated resistance mutations were detected in the NA gene of the postbaseline samples in 49 oseltamivir-treated children (2.3%), including 34 (1.6%) A/H1N1pdm09 viruses with the H274Y mutation and 15 (0.7%) A/H3N2 viruses with the R292K mutation (Table 3). No resistance mutations were detected in influenza B viruses. The emergence of resistance mutations was equally distributed over the entire 7 years of IRIS (Table 4). The prevalence of resistance was higher in children aged <5 years (n = 39) compared with children aged >5 years (n = 10; Table 3). The children infected with viruses who acquired resistance mutations had a higher viral load at day 3 and/or day 6 compared with children infected with wild-type A/H1N1pdm09 and A/H3N2 virus (Supplementary Figures 7 and 8). This difference was not observed at day 10, since most children had cleared the virus.
Table 3.
Emergence of Resistance to Neuraminidase Inhibitors in Children With Laboratory-Confirmed A/H1N1pdm09 and A/H3N2 Influenza Virus at Baseline
| Influenza (Sub-)Type a | Age Group | |||||
|---|---|---|---|---|---|---|
| <6 Months | 6 Months–1 Year | 1–3 Years | 3–5 Years | 5–10 Years | 10–13 Years | |
| n = 10 | n = 11 | n = 301 | n = 372 | n = 605 | n = 209 | |
| A/H1N1pdm09 | 2/4 (50.0) | 2/7 (28.6) | 15/151 (9.9) | 9/158 (5.7) | 6/270 (2.2) | 0/93 (0.0) |
| A/H3N2 | 0/6 (0.0) |
0/4 (0.0) |
5/150 (3.3) | 6/214 (2.8) | 4/335 (1.2) | 0/116 (0.0) |
Data are the fraction of resistant (%).
aData from children infected with influenza B are not shown, because no resistance mutations were detected in these patients.
Table 4.
Emergence of Resistance Mutations Over the Influenza Resistance Information Study Yearsa
| Influenza Resistance Information Study Year | Total | Age Group | |||||
|---|---|---|---|---|---|---|---|
| <6 Months | 6 Months–1 Year | 1–3 Years | 3–5 Years | 5–10 Years | 10–13 Years | ||
| N = 1508 | n = 10 | n = 11 | n = 301 | n = 372 | n = 605 | n = 209 | |
| 2009 | 7/700 (1.0%) | 0 | 0 | 0/1 | 0/2 | 0/3 | 0/1 |
| 2009/2010 | 1/293 (0.3%) | 0 | 0 | 1/45 (2.2%) | 0/56 | 0/131 | 0/61 |
| 2010/2011 | 14/274 (5.1%) | 0 | 0 | 9/64 (14.1%) | 3/72 (4.2%) | 2/97 (2.1%) | 0/41 |
| 2011/2012 | 5/131 (3.8%) | 0 | 0 | 1/23 (4.4%) | 2/39 (5.1%) | 2/53 (3.8%) | 0/16 |
| 2012/2013 | 15/400 (3.8%) | 0 | 0 | 6/94 (6.4%) | 7/113 (6.2%) | 2/144 (1.4%) | 0/49 |
| 2013/2014 | 7/151 (4.7%) | 2/4 (50%) | 2/8 (25%) | 0/30 | 2/40 (5.0%) | 1/62 (1.6%) | 0/7 |
| 2014/2015 | 7/252 (2.8%) | 0/6 | 0/3 | 3/44 (6.8%) | 1/50 (2.0%) | 3/155 (2.6%) | 0/34 |
| All years combined | 49/1508 (3.3%) | 2/10 (20%) | 2/11 (18.2%) | 20/301 (6.6%) | 15/372 (4.0%) | 10/605 (1.7%) | 0/209 |
aData are the fraction of resistant (%), unless specified otherwise. Children infected with influenza B are excluded, because no resistance mutations were detected in these patients. The denominator for percentages is the total number of A/H1N1pdm09 and A/H3N2 patients by age group enrolled in the respective years. Children aged <1 year were not recruited during years 1 to 5 of Influenza Resistance Information Study.
Variables Associated With Emergence of Resistance
Logistic regression analyses demonstrated that older age was associated with reduced odds of acquiring resistance mutations (OR, 0.70; CI, .62–.81; P < .0001). A high baseline viral load was associated with the development of resistance mutations (OR, 1.50; P = .005). Influenza A/H3N2 virus was less likely to become resistant compared with A/H1N1pdm09 virus (OR, 0.38; P = .0016).
DISCUSSION
The viral load at baseline and the rate of viral clearance both contribute to the total viral RNA load in patients with influenza virus infection. The presented data demonstrate that, over the duration of their infection, children aged 1−5 years shed a 1.04- to 1.24-fold higher total quantity of influenza virus compared with older children. This higher total viral burden in young children was observed in both untreated and oseltamivir-treated children’s age groups.
Similar to previous data, no age-related differences were observed in the baseline viral load of infected children in this study (excluding infants aged <1 year infected with A/H3N2 virus), indicating that baseline viral load did not have a direct effect on the high total quantity of virus shedding detected in the upper respiratory tract of infected young children [13, 14]. The relatively low rate of viral RNA clearance observed in children aged 1−5 years may have led to their high viral burden, and it most likely resulted from their immature immune response and/or the absence of prior exposure to influenza A viruses [6]. In contrast to the data presented here, several studies reported no difference in viral burden between children of different age groups [12–14, 18]. However, those studies did not take the timing of symptom onset into account. The influenza virus load depends on the time when a sample is obtained in relation to disease onset [12, 19]. When corrected for the date of symptom onset, this study showed that viral RNA shedding was, in general, still prolonged in young children compared with older children. Ultimately, this age-related viral load difference was no longer observed for children who were included ≥2 days after symptom onset. Therefore, by not correcting for the date of disease onset, previous studies may have failed to detect differences between age groups [12–14, 18].
Surprisingly, compared with older children, infants infected with A/H3N2 virus had a low baseline viral load and cleared viral RNA faster, whereas the opposite was observed for A/H1N1pdm09 virus. Technical reasons for the observed low baseline viral load in these infants were ruled out first, since the same sampling and virological assays were used for all patients included in this study. Second, parents with sick infants tend to seek professional care earlier upon symptom onset compared with parents with older children [20]. This early sampling may have resulted in very low viral loads, since virus production has only just started. However, in this study, the time from symptom onset to study baseline in infants was either similar or higher than in older children. As infants were not included during the first 5 years of IRIS, only a small number of young children, primarily from the United States, were included in this study. This small sample size and the observed substantial variation in the detected viral loads makes it difficult to draw any solid conclusion from this group.
Age-related differences in the viral kinetics in children infected with influenza B virus were not as prominent as those observed in influenza A virus–infected children. According to available surveillance data to date, most influenza epidemics were dominated by influenza A virus infections [21, 22]. Correspondingly, due to the absence of preexisting immunity, influenza B virus infection might affect both young and older children equally [23].
Interestingly, despite the low observed vaccination coverage, in accordance with previous data, the present study showed that both vaccination and antiviral treatment reduced the duration of virus shedding [11, 24, 25]. In addition, antiviral treatment seemed to have a beneficial effect on symptom resolution. However, IRIS was a nonrandomized clinical study that was not designed to determine the efficacy of antiviral treatment. Therefore, no conclusions were drawn regarding oseltamivir usage with clinical symptoms. Previous studies have suggested that antiviral therapy is associated with the development of resistance mutations [11, 15, 26–28]. Similarly, in this study, only children infected with A/H1N1pdm09 and A/H3N2 who received oseltamivir treatment acquired resistance mutations. The prevalence of resistance in this study was highest in children aged <5 years and almost absent in older children, which may suggest that the protracted viral RNA shedding in young children allowed for the influenza viruses to evolve and acquire resistance mutations upon selective pressure of antiviral therapy. Similar to a previous study, emergence of resistant viruses did not affect symptom resolution in influenza A–infected children (data not shown) [16].
The emergence of resistance can also delay viral clearance [16]. This may be a contributing factor to prolonged shedding in young children prone to the developed antiviral resistance. However, when children who acquired antiviral resistance were excluded from the analysis, the probability of age to increase viral clearance remained the same (data not shown).
Young children are at higher risk of acquiring severe influenza [1, 4, 29]. In this study, serious complications were rare, with only 2 ICU admissions and influenza-related symptoms that lasted for approximately 1 week. Since antiviral therapy was at the discretion of the physician, it is not known whether the observed AEs were related to the antiviral usage or a reflection of the severity of influenza virus infection.
In conclusion, we showed that the baseline nasopharyngeal influenza virus loads were comparable among all age groups. However, over time, viral RNA shedding was protracted in young children (aged 1−5 years) compared with older children. This could explain why young children are more likely to develop antiviral resistance upon antiviral therapy and serve as spreaders of influenza virus in the community.
Supplementary Data
Supplementary materials are available at Clinical Infectious Diseases online. Consisting of data provided by the authors to benefit the reader, the posted materials are not copyedited and are the sole responsibility of the authors, so questions or comments should be addressed to the corresponding author.
Acknowledgements
The authors thank all parties involved in the influenza resistance information study, which includes the patients, investigators, steering committee members, and the clinical study management team at Roche and Micron research.
Notes
Data sharing. Qualified researchers may request access to individual patient level data through the clinical study data request platform (www.clinicalstudydatarequest.com). Further details on Roche’s criteria for eligible studies are available here (https://clinicalstudydatarequest.com/Study-Sponsors/Study-Sponsors-Roche.aspx). For further details on Roche’s Global Policy on the Sharing of Clinical Information and how to request access to related clinical study documents, see here (https://www.roche.com/research_and_development/who_we_are_how_we_work/clinical_trials/our_commitment_to_data_sharing.htm).
Disclaimer. The views expressed in this manuscript are not necessarily those of the Department of Health and Social Care (DHSC), England.
Financial support. This work was supported by F. Hoffmann-La Roche Ltd.
Potential conflicts of interest. R. R., R. A. M. F., and A. D. M. E. O. have received research funding from F. Hoffmann-La Roche Ltd. P. L. A. F. receives funding from PREPARE Europe (EU FP7 grant 378 602525) and Takeda and was an invited speaker at scientific meetings sponsored by GlaxoSmithKline and Shire. D. K. has received research funding from F. Hoffmann-La Roche Ltd and GlaxoSmithKline and honoraria from GlaxoSmithKline and Sanofi. J. S. N.-V.-T. is currently seconded to the DHSC. R. W. receives support from the National Institutes of Health (NIH) and is on the Gilead Science Board of Directors. A. D. M. E. O. reports personal fees from Hoffman La Roche and GlaxoSmithKline; is the founder, chief service officer, and minor shareholder of Viroclinics Biosciences BV and C202; and reports EU and Coalition for Epidemic Preparedness Innovations grants outside the submitted work. M. S. received consultancy fees for the Influenza Resistance Information Study project from Hoffmann-La Roche Ltd. A. M. reports consulting fees from F. Hoffmann-La Roche Ltd. R. A. M. F. reports grants from H2020 COMPARE and the NIH National Institute of Allergy and Infectious Diseases/Centers of Excellence for Influenza Research and Surveillance during the conduct of the study. B. C. reports employment with stock from Roche Products Ltd. C. A. B . reports speakers honoraria from ViiV outside the submitted work. All other authors report no potential conflicts. All authors have submitted the ICMJE Form for Disclosure of Potential Conflicts of Interest. Conflicts that the editors consider relevant to the content of the manuscript have been disclosed.
References
- 1. Fraaij PL, Heikkinen T. Seasonal influenza: the burden of disease in children. Vaccine 2011; 29:7524–8. [DOI] [PubMed] [Google Scholar]
- 2. Rahmqvist M, Gjessing K, Faresjö T. Influenza-related healthcare visits, hospital admissions, and direct medical costs for all children aged 2 to 17 years in a defined Swedish region, monitored for 7 years. Medicine (Baltimore) 2016; 95:e4599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Ang LW, Lim C, Lee VJ, et al. Influenza-associated hospitalizations, Singapore, 2004–2008 and 2010–2012. Emerg Infect Dis 2014; 20:1652–1660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Jules A, Grijalva CG, Zhu Y, et al. Influenza-related hospitalization and ED visits in children less than 5 years: 2000–2011. Pediatrics 2015; 135:e66–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Monto AS, Sullivan KM. Acute respiratory illness in the community. Frequency of illness and the agents involved. Epidemiol Infect 1993; 110:145–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Bodewes R, Fraaij PL, Osterhaus AD, Rimmelzwaan GF. Pediatric influenza vaccination: understanding the T-cell response. Expert Rev Vaccines 2012; 11:963–71. [DOI] [PubMed] [Google Scholar]
- 7. Olin A, Henckel E, Chen Y, et al. Stereotypic immune system development in newborn children. Cell 2018; 174:1277–1292 e14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Ng S, Lopez R, Kuan G, et al. The timeline of influenza virus shedding in children and adults in a household transmission study of influenza in Managua, Nicaragua. Pediatr Infect Dis J 2016; 35:583–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Sato M, Hosoya M, Kato K, Suzuki H. Viral shedding in children with influenza virus infections treated with neuraminidase inhibitors. Pediatr Infect Dis J 2005; 24:931–2. [DOI] [PubMed] [Google Scholar]
- 10. Coates BM, Staricha KL, Wiese KM, Ridge KM. Influenza A virus infection, innate immunity, and childhood. JAMA Pediatr 2015; 169:956–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Whitley RJ. The role of oseltamivir in the treatment and prevention of influenza in children. Expert Opin Drug Metab Toxicol 2007; 3:755–67. [DOI] [PubMed] [Google Scholar]
- 12. Fielding JE, Kelly HA, Mercer GN, Glass K. Systematic review of influenza A(H1N1)pdm09 virus shedding: duration is affected by severity, but not age. Influenza Other Respir Viruses 2014; 8:142–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Oshansky CM, Gartland AJ, Wong SS, et al. Mucosal immune responses predict clinical outcomes during influenza infection independently of age and viral load. Am J Respir Crit Care Med 2014; 189:449–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Li CC, Wang L, Eng HL, et al. Correlation of pandemic (H1N1) 2009 viral load with disease severity and prolonged viral shedding in children. Emerg Infect Dis 2010; 16:1265–1272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Whitley RJ, Boucher CA, Lina B, et al. Global assessment of resistance to neuraminidase inhibitors, 2008–2011: the Influenza Resistance Information Study (IRIS). Clin Infect Dis 2013; 56:1197–1205. [DOI] [PubMed] [Google Scholar]
- 16. Lina B, Boucher C, Osterhaus A, et al. Five years of monitoring for the emergence of oseltamivir resistance in patients with influenza A infections in the Influenza Resistance Information Study. Influenza Other Respir Viruses 2018; 12:267–78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. van der Vries E, Ip DK, Cowling BJ, et al. Outcomes and susceptibility to neuraminidase inhibitors in individuals infected with different influenza B lineages: the influenza resistance information study. J Infect Dis 2016; 213:183–90. [DOI] [PubMed] [Google Scholar]
- 18. Loeb M, Singh PK, Fox J, et al. Longitudinal study of influenza molecular viral shedding in Hutterite communities. J Infect Dis 2012; 206:1078–84. [DOI] [PubMed] [Google Scholar]
- 19. Launes C, Garcia-Garcia JJ, Jordan I, Selva L, Rello J, Munoz-Almagro C. Viral load at diagnosis and influenza A H1N1 (2009) disease severity in children. Influ Other Respir Viruses 2012; 6:e89–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Harrold J, Langevin M, Barrowman N, et al. ; Pediatric Emergency Research Canada Network Parental characteristics and perspectives pertaining to neonatal visits to the emergency department: a multicentre survey. CMAJ Open 2018; 6:E423–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Su S, Chaves SS, Perez A, et al. Comparing clinical characteristics between hospitalized adults with laboratory-confirmed influenza A and B virus infection. Clin Infect Dis 2014; 59:252–5. [DOI] [PubMed] [Google Scholar]
- 22. Tan J, Asthagiri Arunkumar G, Krammer F. Universal influenza virus vaccines and therapeutics: where do we stand with influenza B virus? Curr Opin Immunol 2018; 53:45–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Peltola V, Ziegler T, Ruuskanen O. Influenza A and B virus infections in children. Clin Infect Dis 2003; 36:299–305. [DOI] [PubMed] [Google Scholar]
- 24. COMMITTEE ON INFECTIOUS DISEASES. Recommendations for prevention and control of influenza in children, 2018–2019. Pediatrics 2018; 142:1–28. [DOI] [PubMed] [Google Scholar]
- 25. Malosh RE, Martin ET, Heikkinen T, Brooks WA, Whitley RJ, Monto AS. Efficacy and safety of oseltamivir in children: systematic review and individual patient data meta-analysis of randomized controlled trials. Clin Infect Dis 2018; 66:1492–500. [DOI] [PubMed] [Google Scholar]
- 26. Roosenhoff R, van der Vries E, van der Linden A, et al. Influenza A/H3N2 virus infection in immunocompromised ferrets and emergence of antiviral resistance. PLoS One 2018; 13:e0200849. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. van der Vries E, Stittelaar KJ, van Amerongen G, et al. Prolonged influenza virus shedding and emergence of antiviral resistance in immunocompromised patients and ferrets. PLoS Pathog 2013; 9:e1003343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Stephenson I, Democratis J, Lackenby A, et al. Neuraminidase inhibitor resistance after oseltamivir treatment of acute influenza A and B in children. Clin Infect Dis 2009; 48:389–96. [DOI] [PubMed] [Google Scholar]
- 29. Kondrich J, Rosenthal M. Influenza in children. Curr Opin Pediatr 2017; 29:297–302. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.