Abstract
A top priority for the Veteran’s Healthcare Administration is improving access to high-quality mental healthcare. Mobile and telemental healthcare are a vital component of increasing access for veterans. The Veteran’s Healthcare Administration is making efforts to further broaden how veterans receive their care through VA Video Connect, which allows veterans to connect with their provider from their residence or workplace. In this mixed-methods study, successes and challenges associated with the rapid implementation of VA Video Connect telemental health appointments are examined through (1) administrative data and (2) qualitative interviews at one medical center. Within 1 year of the telehealth initiative, the number of providers experienced with telemental health increased from 15% to 85%, and telehealth appointments increased from 5376 to 14,210. Provider reported barriers included administrative challenges and concerns regarding care. Having an implementation model of telehealth champions and a team of experienced mental health providers allowed for rapid adoption of telehealth. Utilizing a similar model in other settings will further enable more veterans with depression and anxiety to have access to evidence-based psychotherapy, regardless of location or national crisis. With the dramatic increase in both training for providers as well as veteran use of telemental healthcare during the COVID-19 pandemic response, future research should aim to better understand which teams were able to switch to telehealth easily versus those which struggled, along with examining system-wide and provider-level factors that facilitated continued use of telehealth after social distancing requirements related to COVID-19 were relaxed.
Electronic supplementary material
The online version of this article (10.1007/s41347-020-00161-8) contains supplementary material, which is available to authorized users.
Keywords: Access to care, Mental health, Technology, Telehealth, Veteran
The demand for flexible mental health service delivery came to the forefront for healthcare industries across the globe this year as a result of COVID-19. Current projections estimate there could be as many as 1 billion telehealth appointments conducted by the end of 2020, compared with the original pre-COVID-19 projected estimates of 36 million virtual visits for 2020 (Coombs 2020). More than 50 healthcare systems in the USA have existing programs capable of incorporating various telehealth technologies to maintain care (Hollander and Carr 2020) and were able to adapt to the increased demands for virtual care. This includes the Veterans Health Administration (VHA), which has been providing telehealth and telemental health for more than two decades, and currently stands as the largest healthcare agency in the USA providing telehealth care (Godleski et al. 2012).
VHA began testing and implementing telehealth on a national scale in 2003, first through a hub-and-spoke model of telehealth by which veterans received specialized care at their local outpatient clinics while their providers were located at the main hospitals. This model then expanded to include providing care to the location of preference, including non-VA locations such as a veteran’s residence through the VHA “Anywhere to Anywhere” initiative. Gradually and then through a more targeted expansion initiative, VHA sets objectives to ensure that by the end of FY 2021, 100% of providers serving in outpatient Mental Health and Primary Care service lines nationwide would be both capable and experienced with providing care through VHA’s telehealth platform, VA Video Connect (VVC; i.e., have completed a telehealth-into-the-home encounter with a veteran; Department of Veteran’s Affairs 2018b). VVC allows veterans and providers to participate in video visits on any computer, tablet (personally owned or VA-issued), or mobile device with an internet connection. This initiative, along with other work through the Office of Connected Care and the Office of Rural Health, led to over 1,000,000 telehealth appointments conducted in the VHA in FY2019 (Office of Public and Intergovernment Affairs 2019). Coinciding with an increased emphasis on telemental health delivery, in 2006 VHA prioritized increasing its mental health workforce and training initiatives, and in implementing and disseminating more wide-scale use of 16 evidence-based psychotherapies (EBP; Department of Veteran’s Affairs 2008, 2012); see Rosen et al. (2016) for a review of EBPs within VHA, with particular emphasis on expanding the availability of EBPs for anxiety disorders and depression (Karlin et al. 2010).
A recent review examining six decades of clinical outcome research found strong evidence for the safety and effectiveness of delivering EBPs via telemental health for anxiety and depression across multiple care settings, including VHA (Tuerk et al. 2018). In addition to efficacy data, surveys of veterans receiving care through VA telehealth to a non-VA location yielded high levels of patient satisfaction (88%; Department of Veteran’s Affairs 2018a) and was found to be cost-effective compared to in-person care (Jacobs et al. 2019). Though treatment delivered via telehealth may be effective and patients appear to be satisfied with this treatment format, provider buy-in and support are also necessary for both successful adoption and sustained use. Currently, although the VHA has set national VVC training benchmarks for its providers, how each facility is working to achieve these goals has been left up to the discretion of clinical directors and team members at each location.
The aims of this project are to (1) describe how VVC was implemented locally with particular consideration for the unique challenges of EBP delivery via telemental health and VVC platforms, (2) report on the outcome of this work via (a) VA administrative data and (b) qualitative interviews with the providers, and (3) present recommendations for future telemental health service delivery.
Method
Administrative Data
Administrative data were gathered from the VHA Support Service Center (VSSC) dashboards, which allow for real-time tracking of VA mental health encounters. We used the VVC modifier codes (179) to assess the increase in VVC use during each quarter from January 2018 to April 2020.
Qualitative Data
The study team conducted qualitative interviews with mental health providers (psychologists and social workers) about their satisfaction with providing treatment via VVC. Our thematic interview followed a structured interview guide which consisted of open-ended questions. The primary author sent emails to mental health providers with experience using VVC inviting them to voluntarily participate in the interview about VVC (approximately 32 providers at the time of recruitment), and eight gave informed consent via procedures approved by the IRB and R&D committees of the primary author’s respective university and VA affiliates, respectively. The thematic interviews were all individual, conducted by authors USM and KK either in person or virtually with Skype video, lasted approximately 30 min, were audiotaped, and transcribed. Transcriptions were then deductively coded and analyzed by the primary author using rapid turn-around qualitative analysis procedures (Hamilton 2013). In addition, qualitative data from 72 VVC sessions from April 2019 to November 2019 were gathered. Providers in the posttraumatic stress disorder (PTSD) Clinical Team (PCT) clinic, a clinic which provided approximately 60% VVC appointments, 40% in-person appointments, alerted the primary author to any session issues they encountered, which were then coded as (1) type of issue: technical, etiquette-related, or “other,” (2) percentage of the total treatment session was impacted by the issue, and (3) subjective rating of provider satisfaction ranging from 0 (poor session, unable to complete any treatment) to 5 (perfect session, any issues did not impact treatment).
Implementation of VVC
In order to rapidly implement VVC through the mental health service line at our local VA, the Ralph H. Johnson VAMC, a champion model of implementation was utilized (Hendy and Barlow 2012). Supervisors and service chiefs from each of the mental health service departments selected one staff member from each team who would serve as a VVC Champion. This individual was in charge of assisting other team members with completing the requirements necessary to conduct a telehealth appointment via VVC. Selected VVC Champions included a mixture of providers heavily experienced with VVC as well as some who had never conducted a VVC appointment and required training themselves. This group then developed best practice guidelines to be disseminated across the service line. Monthly VVC Champion calls were also set up to help with the distribution of guidelines, answer questions, and to review completion status reports from each department.
For each provider in a clinic, the VVC champion assisted with mandatory training of policy and procedures (including use of e911 in case of an emergency, which routes 911 calls to the appropriate local emergency responder), enrollment into the VVC system, procurement of equipment (e.g., webcam, working microphone), and completion of a systems check (e.g., test calls, quality check of audio and visual issues) prior to assisting providers with selection criteria for determining appropriateness of treatment delivered via VVC. Initial criteria for exclusion from VVC care included high-risk veterans (e.g., those with active psychotic symptoms or a recent suicidal gesture/attempt) as well as those facing logistical barriers (e.g., those with no internet or cell phone capability, those who lacked privacy in their home or other personal settings, or those likely to experience multiple distractions that could interfere with the encounter). The VVC champion remained a first line resource for providers and was available to address any questions or concerns that a provider had before their initial session while also offering providers basic troubleshooting tips for technical problems. Providers were encouraged to contact the VHA telehealth help desk if they experienced technical issues that could not be resolved independently or with a brief VVC champion intervention. These VVC champions also were able to more rapidly respond and assist with the clinic wide use of VVC in response to COVID-19 pandemic.
Results
Systematic Increase of VVC Prior to COVID-19
When the VVC expansion initiative was announced across the VHA in June of 2018, the Ralph H. Johnson VAMC employed 188 mental health providers who worked in outpatient clinics and therefore were targeted to complete the training as part of the VVC expansion initiative. At the outset, 28 of these providers (15%) were already VVC-trained due in part to the hospital’s position as a telemental health hub-affiliated site, and pre-existing adoption of VVC across the service line. The training team spent the early part of the 2019 fiscal year (FY19; October through December of 2018) preparing to launch the initiative internally, with the launch occurring in January of 2019, and a majority of providers having completed the training and initial encounter by of March 2019 (Table 1). Over that year, the increasing number of providers trained in VVC coincided with an increasing number of completed VVC encounters (Fig. 1).
Table 1.
Provider completion data over 1 year of the VVC expansion initiative
| MH total provider count | Count of MH providers with CVT to home | Change from prior quarter | % MH providers with CVT to home | |
|---|---|---|---|---|
| VVC expansion objectives released nationwide June 8, 2018 (VHA Notice 2018-25). | ||||
| FY18 Q4 (Jul–Sep) | 188 | 28 | . | 14.89% |
| FY19 Q1 (Oct–Dec) | 184 | 32 | + 4 | 17.39% |
| VVC implementation training and dissemination completed facility-wide at RHJ starting January 2019. | ||||
| FY19 Q2 (Jan–Mar) | 199 | 146 | +114 | 73.37% |
| FY19 Q3 (Apr–May) | 204 | 173 | +27 | 84.80% |
Note. MH = mental health, CVT = clinical video telehealth, FY = fiscal year, RHJ = Ralph H. Johnson
Fig. 1.
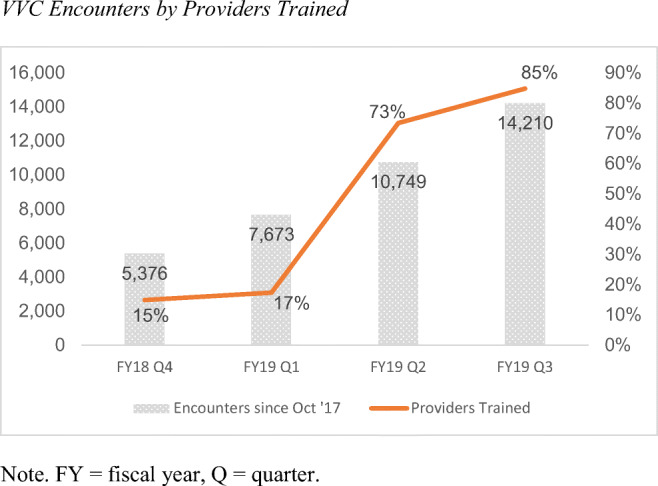
VVC encounters by providers trained. Note. FY, fiscal year; Q, quarter
Provider Experience
Specific VVC Session Issues
During a six-month window, providers in the PCT were asked to alert the primary author if they encountered an issue during a VVC session and to record the nature of the difficulty. Out of a total 1225 sessions conducted over 6 months, 72 sessions (6%) were flagged as having issues, with 95% of them categorized as technical issues and 11% categorized as “etiquette” issues, such as veterans answering sessions while driving, with children present, veterans drinking alcohol/smoking during sessions, etc. For the sessions with technical issues, 53% of the technical issues were related to signal issues, 32% were related to the VVC network being “down,” and 17% of technical issues were related to veteran user error. Providers rated the quality of these sessions as an average of 2.2 out of 5, with 40% of the session spent not conducting therapy. Lastly, for sessions with technical issues, the National Telehealth Helpdesk was contacted 25% of the time.
Qualitative Interviews
In addition to session data, the primary author conducted qualitative interviews with providers in the same PCT as well as the evidence-based telemental health clinic to assess provider views of the barriers and facilitators of VVC. The percentage of social workers and psychologists that participated in the interviews reflects the distribution in the clinics. Based on preliminary data, the primary concerns providers expressed were related to (1) emergency procedures (e.g., not being able to send rescue or timely for suicidal patients), (2) being asked to treat veterans via VVC who they considered to be “too high risk” or unstable for telehealth services (e.g., actively suicidal, severe alcohol use disorders, actively psychotic), (3) concerns that some veterans were not respecting therapeutic boundaries (e.g., trying to engage in treatment sessions while driving), (4) concerns related to time lost attending to technical issues rather than devoted to delivering EBPs, and (5) difficulty in delivering measurement-based care (see Table 2).
Table 2.
Qualitative interview themes and direct quotation examples
| Theme | Direct quotation |
|---|---|
| Emergency procedures | “My ability to rest my head on my pillow at night is compromised in a crisis on VVC more so than in person. Even talking about it right now is… you know primarily I just want to be sure everybody is safe. In those situations, I think being in the clinic is a better environment. At least I feel like you have more control than you do....” |
| Concerns about high-risk status | “There are some people I describe it as I want to smell, especially if someone reports a lot of substance abuse. It’s more challenging just to be able to tell if someone is using during the session through video.” |
| Therapeutic boundaries | “When they treat it like they are facetiming a friend…and driving.” |
| Technology interference | “I’d say its when things go down whether it’s the scheduling system or Wi-Fi, sometimes these places are pretty remote.” |
| Measurement-based care limitations | “But if there was some app where they could give assessments, you could assign them, and they could just sign on and complete them and they would flip over to you that would be amazing. Because I spend a lot of time verbally giving assessments or doing clinical reminders.” |
Integration of Results
Taken together, these data suggest that the primary reported concerns with VVC that providers expressed were those that occurred with the least frequency during clinical practice (as reflected in veterans’ electronic session notes). It is important to note that asking providers to alert the primary author to issues was another demand for their limited time, so it is likely that all of the sessions with issues were not fully captured using these methods. Despite this limitation, these data suggest that over 90% of VVC appointments were conducted smoothly. While providers reported concerns related to veterans not taking the appointments seriously, less than 5% of the issues reported during actual VVC sessions were related to veteran etiquette issues (e.g., answering the appointment while driving, not wearing clothing), and there were no instances of providers encountering problems accessing emergency services if and when necessary. Rather, the most common issues reported during VVC service delivery were technical in nature, and with appropriate training and regular use of VVC, providers rarely experienced technical issues requiring them to contact the telehealth support line to resolve. Additional issues related to providing EBPs with fidelity to the model (e.g., timely or time-efficient exchange of therapy materials, measurement of weekly outcomes), and suggestions to address these concerns are outlined below.
Impact of COVID-19 on the Expanded Use of VVC Within VA
In order to meet the enormous healthcare challenge COVID-19 created, the VHA rapidly increased the number of outpatient appointments conducted via VVC so veterans remained connected and engaged in their care while reducing exposure risk, limiting travel, and maintaining social distancing guidelines. At the Ralph H. Johnson VA Medical Center in Charleston, South Carolina, 2034 mental health appointments were conducted via VVC in March 2020 as compared to 1429 appointments in January of 2020, representing a 42% increase in VVC sessions in a 3 month period of time. Nationally, the VHA saw a 70% increase in mental health treatment provided via VVC, from 20,000 VVC appointments conducted in February 2020 to 34,000 conducted in March 2020 (Department of Veteran’s Affairs 2020b).
Discussion
The use of VVC within VHA has expanded within recent years to include an ever increasing number of veterans rather than being limited to those living in rural areas and/or those facing other significant logistical barriers prohibiting in-person care. However, use of VVC to successfully expand telemental health services which allows for expanded access to EBPs for anxiety and depression, depends on how providers and patients adapt to telehealth technology and how well they are able to integrate it into routine care (Morgan et al. 2008; Richardson et al. 2009). The Ralph H. Johnson VAMC is on the forefront of developing policies and procedures in this arena to meet the increasing demand for VVC and to ensure that care delivered through VVC is both effective and embraced by both veterans and providers. The need for such policies and procedures is even more apparent in light of recent COVID-19 containment guidelines.
Lessons Learned
Administrative, institutional, and clinical complexities inherent in this ambitious initiative were evident, and while it may be challenging for some providers to sustain their use of VVC in the future, there are a number of factors that have increased the uptake of VVC within our facility. Below we will outline some of the challenges we encountered, as well as potential strategies for improving the implementation and ease of VVC both locally and nationally.
First, a VVC-specific clinic had to be developed electronically for each individual provider to ensure that the clinical encounter would be coded or billed correctly. Support staff estimated that this required approximately 20 min per provider due in part to the multiple electronic systems used administratively throughout VHA; it is anticipated that future planned improvements with VHA electronic systems (i.e., the Cerner system) may help to address this barrier. Second, and most commonly cited as a barrier to service delivery by clinic VVC champions, were difficulties scheduling VVC appointments within or around providers’ existing in-person clinics. While this inconvenience was considered relatively inconsequential for completing a single VVC encounter, it has been a more substantial barrier for providers who want to offer VVC to veterans on an as-needed basis but who cannot sustain a daily or weekly VVC clinic. Third, providers’ available time to complete VVC training was limited; with demanding caseloads, many providers faced the tension between learning a new treatment modality while having that effort siphon time from managing their existing caseloads. The fourth challenge is perhaps the most important with regard to the long-term growth and success of the VHA’s telemental health initiative program. The effort to train all mental health providers at the Ralph H. Johnson VAMC in VVC was undertaken largely by program champions who volunteered their time while still attending to all pre-existing clinical and administrative duties. As telehealth programs grow within VHA nationwide, it will be important for national leaders and other key stakeholders to support efforts to expand the infrastructure for these programs, specifically by allocating staff and provider positions and/or allocation of effort/working hours and resources to telehealth at a rate that coincides with anticipated or desired growth.
The strategy of identifying and training clinic-specific program champions was highly effective at the Ralph H. Johnson VAMC for increasing collaboration and communication among clinicians that facilitated rapid expansion of telehealth. This VVC Champion model influenced an April memo sent across VA which has been adopted by VHA’s Office of Mental Health and Suicide Prevention to establish a facility-level telemental health champion (Department of Veteran’s Affairs 2020a). It is important that sites also consider other available models for both facilitating ongoing expansion efforts related to VVC as well as future VHA innovation and dissemination efforts. For example, the Quality Enhancement Research Initiative (QUERI) for Team-Based Behavioral Health with the Central Arkansas Veterans Healthcare System developed a manual which provides evidence-based guidance to leaders on implementation facilitation, “a multi-faceted process of enabling and supporting individuals, groups and organizations in their efforts to adopt and incorporate clinical innovations into routine practices” (Ritchie et al. 2017). This approach provides guidance not only for facilitating learning and progress within VHA, but also for facilitating this clinical innovation virtually (i.e., with limited or no in-person contact between leaders/facilitators and providers and staff), sustaining these innovations over time, and evaluating fidelity and correcting program drift over time.
Large-scale telehealth initiatives led by government-funded organizations in other nations are engaged in similar efforts to facilitate growth through effective implementation. In the UK, the Delivering Assisted Living Lifestyles at Scale (dallas) relied on normalization process theory (NPT) to understand challenges and successes within a nationwide initiative to develop and disseminate a range of digital resources for promoting national public health (Lennon et al. 2017). NPT specifically focuses on how groups and individuals adopt and sustain new technologies and practical innovations, and provides a framework for identify contextual barriers (e.g., policy or governmental, commercial, organizational, technical) that may interfere with these processes (Weiner et al. 2009); such theory may be applicable to implementation efforts with an organization as broad, complex, and diverse as VHA.
It is important to note the limitations of this project. First, this project focused primarily on providers in the PCT and EBP clinics as they were conducting the bulk of the telehealth appointments during this period of time; as such, the reported provider concerns here may not generalize to non-EBP providers overall. Further, the psychiatrists in this clinic did not express interest in participating in the interviews, resulting in only social workers and psychologists being interviewed, limiting our knowledge about the unique aspects of providing psychiatric care via VVC. The findings presented here are also from a national healthcare system with established telehealth infrastructure; while we believe this is a helpful model to use, it likely does not reflect all telemental healthcare experiences outside of the VHA. In addition, the data presented here reflect administrative data and provider interviews, which means that we do not have sociodemographic information of the veterans seen via VVC.
Future Directions
The COVID-19 pandemic had the unintended consequence of highlighting and accelerating telehealth treatment within VHA and other healthcare networks. With this rapid growth of telehealth comes the opportunity to understand what barriers to care existed, as well as highlighted the importance of better understanding how telehealth care can be sustained. Successful adoption of telehealth will be necessary in order for the delivery of EBPs with high fidelity.
Delivery of EBPs via VVC and Measurement-Based Care
Telehealth implementation initially increases administrative burden on providers as described above, even without consideration of EBP-specific factors (e.g., exchange of EBP self-assessments, worksheets, and psychoeducation materials). These additional considerations may influence provider decisions regarding whether or how rigorously they will maintain fidelity to EBPs delivered through telehealth (i.e., fidelity adherence to the protocol, administering weekly self-report measures to track patient progress; Tuerk et al. 2018). VHA began the Measurement-Based Care in Mental Health Initiative in 2016 in order to use repeated patient-reported outcomes to enhance mental health care and measure treatment response. Recent data from the initial stage of the measurement-based care (MBC) initiative within VHA suggests that the most common barrier to implementing MBC, even for in-person care, remains technological given that there is not an efficient way to integrate patient outcomes into patient records or to track clinical outcomes across sessions (Resnick and Hoff 2019). This difficulty becomes even more pronounced when delivering telehealth because implementing MBC can add substantial time to each session (e.g., a patient has to read self-report ratings to their provider, assessment cannot be integrated quickly into patient chart). More work needs to be done to find ways to improve the ease of delivery and ability to seamlessly exchange therapy related materials between providers and veterans rather than lose this valuable data at expense of using telehealth. Promising efforts include expanded mobile health efforts to complement EBPs within VHA (e.g., Mood Coach, PE coach) that have self-report measures imbedded within the applications. Other recent efforts have also included the ability for veterans to email providers these data. This is an important move toward the ultimate and needed goal of real-time exchange of EBP data into medical charts directly, which would alleviate some of the extra time-burden that currently exists burden providers and veterans.
Delivery Models—Specialty Care Versus a Tool for All to Use
It remains unclear if it is better to have all providers be “telehealth generalists” or if telehealth should be a speciality. During the COVID-19 pandemic, providers who were previously trained to provide care via telehealth were better equipped to provide care with minimal interruptions. Future studies should examine which providers/teams were able to continue to provide care and which providers/teams faced more significant barriers in the uptake of telehealth service delivery.
Take a Note from the Dissemination and Implementation Programs in the VHA
The efforts to continue to disseminate and implement the use of VVC for mental health treatment are similar to those efforts to roll out PTSD treatment VA wide beginning in 2008 and the suicide prevention program. Following the exponential increase in telehealth use, the future priorities of this initiative have undergone a large shift from a focus on uptake to one of sustainability. In addition to our own local strategic efforts, programs such as the National Center for PTSD and the Rocky Mountain MIRECC for suicide prevention provide useful roadmaps that telehealth could implement.
Electronic Supplementary Material
(DOCX 20 kb)
Author Contributions
Conception and design: USM, ALG; provision of study materials or patients: USM, AB; collection and assembly of data: USM, SC; data analysis and interpretation: USM, SC; manuscript writing: all authors; final approval of manuscript: all authors.
Funding Information
VISN 7 Research Development Award, Myers (PI); Research to Impact for Veterans–Telehealth Research Collaborative, VA Health Services Research and Development (RIVR 19-471), Grubaugh (PI).
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- Coombs, B. (2020). Telehealth visits are booming as doctors and patients embrace distancing amid the coronavirus crisis. CNBC. Retrieved from https://www.cnbc.com/2020/04/03/telehealth-visits-could-top-1-billion-in-2020-amid-the-coronavirus-crisis.html.
- Department of Veteran’s Affairs. (2008). Uniform mental health services in VA medical centers and clinics. Washington, DC.
- Department of Veteran’s Affairs. (2012). Local implementation of evidence-based psychotherapies for mental and behavioral health conditions. Washington, DC.
- Department of Veteran’s Affairs. (2018a). Fact sheet: Telemental Health in the Department of Veterans Affairs. Retrieved from http://vaww.infoshare.va.gov/sites/telehealth/docs/Forms/factsheets.aspx.
- Department of Veteran’s Affairs. (2018b). VA MISSION Act of 2018. Washington, DC.
- Department of Veteran’s Affairs. (2020a). Bolstering National Telemental Health Champions Community of Practice. Washington, DC.
- Department of Veteran’s Affairs. (2020b). A virtual mental health care use on the rise amid COVID-19 [Press release]. Retrieved from https://www.va.gov/opa/pressrel/pressrelease.cfm?id=5418.
- Godleski L, Darkins A, Peters J. Outcomes of 98,609 US Department of Veterans Affairs patients enrolled in telemental health services, 2006–2010. Psychiatric Services. 2012;63(4):383–385. doi: 10.1176/appi.ps.201100206. [DOI] [PubMed] [Google Scholar]
- Hamilton, A. (2013). Qualitative methods in rapid turn-around health services research. VA HSR&D Cyberseminar: Spotlight on Women’s Health.
- Hendy J, Barlow J. The role of the organizational champion in achieving health system change. Social Science and Medicine. 2012;74(3):348–355. doi: 10.1016/j.socscimed.2011.02.009. [DOI] [PubMed] [Google Scholar]
- Hollander JE, Carr BG. Virtually perfect? Telemedicine for COVID-19. New England Journal of Medicine. 2020;382(18):1679–1681. doi: 10.1056/NEJMp2003539. [DOI] [PubMed] [Google Scholar]
- Jacobs, J. C., Hu, J., Slightam, C., Gregory, A., & Zulman, D. M. (2019). Virtual savings: patient-reported time and money savings from a VA National Telehealth Tablet Initiative. Telemedicine and e-Health. [DOI] [PubMed]
- Karlin BE, Ruzek JI, Chard KM, Eftekhari A, Monson CM, Hembree EA, Resick PA, Foa EB. Dissemination of evidence-based psychological treatments for posttraumatic stress disorder in the Veterans Health Administration. Journal of Traumatic Stress. 2010;23:663–673. doi: 10.1002/jts.20588. [DOI] [PubMed] [Google Scholar]
- Lennon, M. R., Bouamrane, M.-M., Devlin, A. M., O’Connor, S., O’Donnell, C., Chetty, U., . . . Finch, T. (2017). Readiness for delivering digital health at scale: Lessons from a longitudinal qualitative evaluation of a national digital health innovation program in the United Kingdom. Journal of Medical Internet Research, 19(2), e42. [DOI] [PMC free article] [PubMed]
- Morgan RD, Patrick AR, Magaletta PR. Does the use of telemental health alter the treatment experience? Inmates’ perceptions of telemental health versus face-to-face treatment modalities. Journal of Consulting and Clinical Psychology. 2008;76(1):158–162. doi: 10.1037/0022-006X.76.1.158. [DOI] [PubMed] [Google Scholar]
- Office of Public and Intergovernment Affairs. (2019). VA exceeds 1 million video telehealth visits in FY2018: One-year achievement represents a 19% increase over previous year [Press release]. Retrieved from https://www.va.gov/opa/pressrel/pressrelease.cfm?id=5196.
- Resnick, S. G., & Hoff, R. A. (2019). Observations from the national implementation of Measurement Based Care in Mental Health in the Department of Veterans Affairs. Psychological Services. [DOI] [PubMed]
- Richardson LK, Christopher Frueh B, Grubaugh AL, Egede L, Elhai JD. Current directions in videoconferencing tele-mental health research. Clinical Psychology: Science and Practice. 2009;16(3):323–338. doi: 10.1111/j.1468-2850.2009.01170.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ritchie, M., Dollar, K., Miller, C., Oliver, K., Smith, J., Lindsay, J., & Kirchner, J. (2017). Using implementation facilitation to improve care in the Veterans Health Administration (version 2). Veterans Health Administration, Quality Enhancement Research Initiative (QUERI) for Team-Based Behavioral Health.
- Rosen, C., Matthieu, M., Stirman, S. W., Cook, J., Landes, S., Bernardy, N., . . . Finley, E. (2016). A review of studies on the system-wide implementation of evidence-based psychotherapies for posttraumatic stress disorder in the Veterans Health Administration. Administration and Policy in Mental Health and Mental Health Services Research, 43(6), 957–977. [DOI] [PubMed]
- Tuerk PW, Keller SM, Acierno R. Treatment for anxiety and depression via clinical videoconferencing: Evidence base and barriers to expanded access in practice. Focus. 2018;16(4):363–369. doi: 10.1176/appi.focus.20180027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weiner BJ, Lewis MA, Linnan LA. Using organization theory to understand the determinants of effective implementation of worksite health promotion programs. Health Education Research. 2009;24(2):292–305. doi: 10.1093/her/cyn019. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(DOCX 20 kb)


