Abstract
Background
Novel coronavirus pneumonia (COVID-19) is a global reminder of the need to attend to the mental health of patients and health professionals who are suddenly facing this public health crisis. In the last two decades, a number of medical pandemics have yielded insights on the mental health impact of these events. Based on these experiences and given the magnitude of the current pandemic, rates of mental health disorders are expected to increase. Mental health interventions are urgently needed to minimize the psychological sequelae and provide timely care to affected individuals.
Method
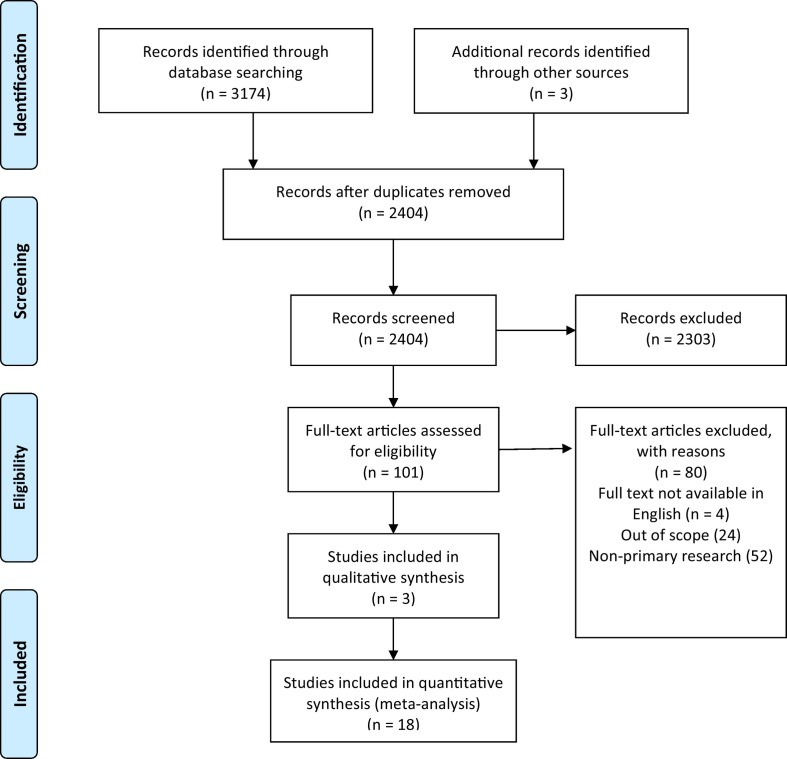
We conducted a rapid systematic review of mental health interventions during a medical pandemic, using three electronic databases. Of the 2404 articles identified, 21 primary research studies are included in this review.
Result
We categorized the findings from the research studies using the following questions: What kind of emotional reactions do medical pandemics trigger? Who is most at risk of experiencing mental health sequelae? What works to treat mental health sequelae (psychosocial interventions and implementation of existing or new training programs)? What do we need to consider when designing and implementing mental health interventions (cultural adaptations and mental health workforce)? What still needs to be known?
Conclusion
Various mental health interventions have been developed for medical pandemics, and research on their effectiveness is growing. We offer recommendations for future research based on the evidence for providing mental health interventions and supports to those most in need.
1. Background
Global medical pandemics such as severe acute respiratory syndrome (SARS), Ebola virus disease and, most recently, novel coronavirus pneumonia (COVID-19) have not only sparked widespread fear of infection, but also affect mental health among the general public and health professionals who provide patient care [1,2]. Most recently, COVID-19 has triggered anxiety, and measures to contain the virus have caused uncertainty, isolation, and economic despair, which take their toll on mental health. Health professionals who care for patients during these crises are vulnerable not only to infection, but also to psychological distress, as population morbidity and deaths, and demand for health services increase [3,4]. Unique stressors for health professionals include burnout [5] and moral injury [6], and are exacerbated by shortages of medical supplies and health services during a time of unprecedented need [7]. Yet despite the need for mental health supports for patients, the general public, and people working in health care, health professionals have received little or no training in providing mental health care during pandemics [8]. Health professionals are asking for reassurance that their organizations will support them, do everything possible to protect them, and provide medical and social support if they or their families become infected [9]. The general public is asking that the health care system be a source of support for maintaining and restoring mental health in the midst of a pandemic [10]. To date, there is little information to guide the development and implementation of mental health interventions to support health professionals, patients, and the general public during medical pandemics [11].
Research indicates that people who have been affected by medical pandemics as survivors, caregivers, orphans, or health professionals working with infected patients are more likely to experience psychological distress, sleep disorders, anxiety, and post-traumatic stress disorder (PTSD) [2,3,5,6,9]. These symptoms can progress to suicidal ideation, substance abuse, and significantly reduced quality of life. Yet it is still not clear how best to respond to mental health challenges during a medical pandemic [12]. Given the critical situation with COVID-19, evidence-based information on existing mental health interventions is urgently needed in order to develop and deliver effective mental health interventions for people in need. This rapid systematic review aims to provide an up-to-date and robust synthesis of the evidence by reporting on implementation, evaluation, and outcomes regarding mental health interventions during medical pandemics within the last two decades.
2. Methods
We used the Preferred Reporting Items for Systematic Reviews and Metal Analysis statement guidelines (PRISMA) to conduct our review and report on the evidence regarding mental health interventions during medical pandemics [13]. We proceeded with the data abstraction process and therefore were not able to register our a priori protocol on PROSPERO. However, we reviewed the already registered reviews of human studies relevant to COVID-19 to minimize the potential of duplicating efforts.
2.1. Information sources, study selection and review process
A comprehensive search strategy was developed with the assistance of a librarian (TR) and was used to identify articles in four electronic databases: Medline (including Epub ahead of print, in process, and other non-indexed citations); Embase; APA PsycInfo; and the Cumulative Index to Nursing & Allied Health Literature (CINAHL). The year range for the search was “2003 to present” to ensure that the SARS literature was included. No language limits were applied. The full Medline search strategy can be found in Supplementary Appendix 1. The searches used database-specific subject headings and keywords in natural language. Database searches were run on March 27, 2020, April 16, 2020, and July 31, 2020 to capture the most recent publications. Reference lists of identified and other relevant articles were hand-searched to capture other potential evidence. This was a rapid review with the aim of being both systematic and expedient; therefore, we did not search the grey literature.
Each identified primary research study was evaluated using PICO (Population, Intervention, Comparison, Outcome) as specified in the Joanna Briggs Institute methodology [14], and included the following:
-
(a)
Population: Studies examining adults, children, and adolescents who participated in a mental health intervention, or health professionals who were trained to provide mental health interventions during or after a medical pandemic.
-
(b)
Intervention: Studies that report any type of mental health interventions and/or training programs using the following criteria: (1) main focus is mental health-related intervention and/or the implementation of a mental health intervention; (2) intervention occurs during or after a major public health event (e.g. disease outbreak, viral pandemic). An intervention is defined as a service performed for, with, or on behalf of a person or populations with the purpose of assessing, improving, maintaining, promoting, or modifying health, functioning, or health condition [15]. Reasons for exclusion included (1) off topic (i.e. not focused on mental health or pandemic setting); (2) not about intervention (e.g. prevalence studies, disaster preparedness, economic loss); (3) health-related disasters unrelated to disease (e.g. mass violence, natural disasters); (4) health trends described as epidemics (e.g. obesity); (5) systematic reviews (although their references were hand-searched for potentially relevant citations); and (6) full text in language other than English.
-
(c)
Comparison: Other treatment interventions associated with normal or usual care.
-
(d)
Outcomes: Studies reporting on the development, effectiveness, and acceptability for mental health interventions designed to improve health functioning.
-
(e)
Types of studies: To determine effectiveness or report on the outcome of a mental health intervention, we included quantitative study designs (randomized controlled trials [RCTs]; quasi-RCTs; controlled before-after studies; case-control, cohort, and cross-sectional studies; surveys; system-level case studies; and pre-post studies). To understand how individuals perceived and experienced an intervention, we included qualitative study designs.
-
(f)
Language: No initial limits were placed on language, however, non-English language studies for which interpretation could not be obtained were excluded.
-
(g)
Country: No limits.
Search terms used to capture the pandemic concept included “pandemic,” “outbreak,” “quarantine,” “shelter in place,” and names of specific epidemic diseases, such as “COVID-19,” “SARS,” and “Ebola.”
Search terms for the mental health concept included subject headings for mental health services and text words such as “mental health,” “mental disorder,” “psychiatry,” “use disorder,” “trauma,” “stress,” and names of specific disorders, in close proximity to intervention terms such as “program,” “service,” and “treatment.”
A total of 2404 titles and abstracts were screened for relevance and possible inclusion. The librarian and the first author independently applied the exclusion criteria to the possible citations. In total, 101 articles were selected for full-text review.
The articles were independently assessed by two reviewers (first author and either second or third author). Disagreements regarding eligibility were resolved by discussion among the reviewers. Through this process, 21 primary research studies were selected for inclusion. The number of articles identified at each stage of the selections process is listed in Fig. 1 .
Fig. 1.
Flow diagram.
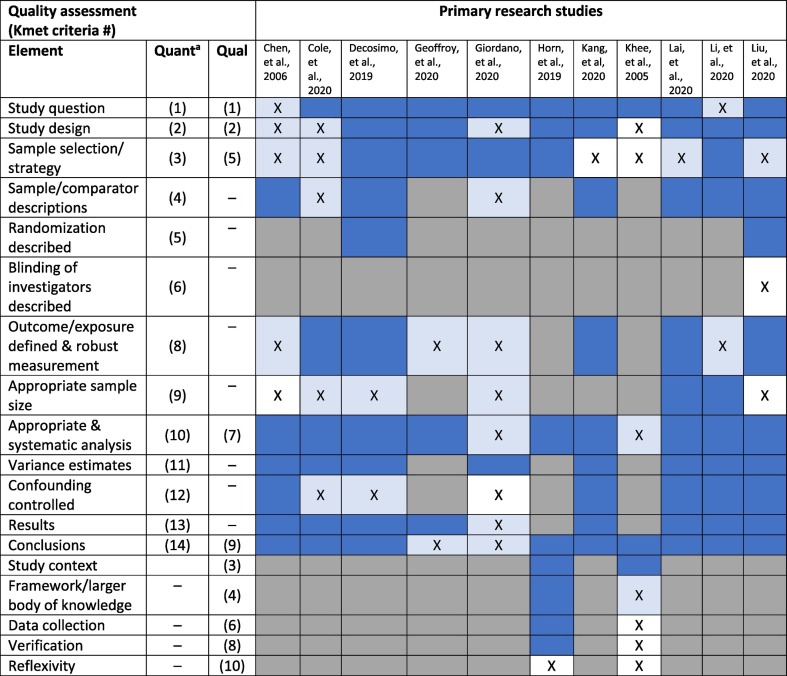
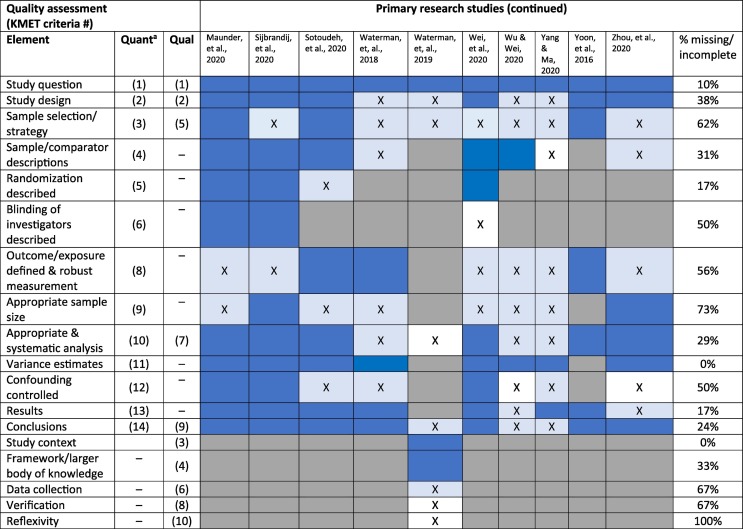
2.2. Methodological quality assessment
The methodological quality of the primary research studies was evaluated using the quantitative and qualitative criteria developed by Kmet and colleagues [16]. The following quality criteria were considered: question/objectives; study design; methods of participant selection; data collection; describing and reporting of random allocation and/or blinding; robust description of outcome measures; sample size; reporting of variance for the main results; controlling for confounding; and verification and reflexivity (for qualitative studies) [16].
We performed a reviewer calibration by having two reviewers (second and last authors) independently rate three studies (two studies at the beginning of the review process and a third study calibration check toward the end). The ratings were compared, discrepancies were identified, and the underlying reasons for disagreement were discussed and resolved. The remaining 18 studies were then rated by the second author. Of the 21 studies, 12 met the criteria for high-quality studies (Kmet score > 80%), with seven studies reaching the very high–quality threshold (Kmet score > 90%) [17]. Table 1 shows the quality ratings for each study, as well as the percentage of missing or incomplete information for each rating criterion.
Table 1.
Quality assessment summary table.
aQuantitative criterion 7 (blinding of participants) not feasible in reviewed studies and therefore not included in this table.
Medium blue = fully met criterion.
Pale blue with X = partially met criterion.
No color with X = missing element.
Grey = not applicable.
3. Results
We categorized the findings from the primary research studies using the following questions: What kind of emotional reactions do medical pandemics trigger? Who is most at risk of experiencing mental health sequelae? What works to treat mental health sequelae (psychosocial interventions and the implementation of existing or new training programs)? What do we need to consider when designing and implementing mental health interventions (cultural adaptations and mental health workforce)? What still needs to be known? The 21 primary research studies involved nine countries and covered five medical pandemics: MERS (n = 1), SARS (n = 2), influenza pandemics (n = 1), Ebola (n = 6), and COVID-19 (n = 11). Table 2 describes the characteristics of the primary research studies.
Table 2.
Characteristics of primary research articles.
| What are the mental health sequelae? | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| Study | Pandemic | Country | Design & type of sample | Assessment methods | Participants | Exposure | Psychosocial/mental health measures (outcomes) | Findings | Quality rating |
| Kang et al. [23] | COVID-19 | PRC | Cross-sectional Convenience sample |
Anonymous questionnaire and informed consent distributed to all workstations via Internet | 944 medical/nursing staff | Level of exposure to COVID-19 | GAD-7, IES-R, ISI, PHQ9 | Higher levels of measured outcomes among those with higher risks of exposure to COVID-19 | 90 |
| Lai et al. [24] | COVID-19 | PRC | Cross-sectional Stratified, 2-stage cluster sampling: hospitals randomly chosen within region, 1 randomly chosen unit from each hospital. All unit workers asked to participate (69% response rate) |
Anonymous survey (administration method not described); verbal consent; | 1257 healthcare workers from 34 hospitals | Level of exposure to COVID-19 | GAD-7, IES-R, ISI, PHQ9 | Higher levels of measured outcomes among those with higher risks of exposure to COVID-19 | 95 |
| Li et al. [37] | COVID-19 | PRC | Pre-post All ‘active’ bloggers on Chinese microblogging website: those averaging 50 posts/month during study period |
Blogging material retrieved from December 31, 2019 to January 26, 2020 | 17,865 bloggers | Official COVID19 announcement (January 20, 2020) | Online Ecological Recognition analysis of extracted blog content | Increase in negative emotions and concerns | 91 |
| Wu & Wei [26] | COVID-19 | PRC | Cross-sectional Stratified sample: 60 staff each from one designated and one non-designated COVID-19 hospital; recruitment methods and response rates within hospitals not reported |
On-line administration of questionnaires and self-rated scale/survey items | 120 front-line hospital staff | Self-reported exercise, level of exposure to COVID-19 | Self-reported prescribed exercise, SCL-90, SDS, SAS, PSQI, PCL-C | Poorer symptom scores and sleep quality among those with higher risk of exposure | 55 |
| Yang & Ma [38] | COVID-19 | PRC | Cross-sectional Nationally representative survey panels |
Surveys administered end of Dec 2019 and mid-Feb 2020 by data intelligence lab at major Chinese university (administration method not described) | 11,131 (pre) and 3000 (during) residents of the PRC | Public reporting of COVID-19 | Well-being measure (both surveys); COVID-related knowledge, sense of control (2nd survey) | Different mean well-being scores between two surveys; associations between well-being and knowledge/sense of control | 57 |
| What works to treat mental health sequelae? psychosocial interventions | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| Study | Pandemic | Country | Design & type of sample | Assessment methods | Participants | Intervention/support (components/details) | Psychosocial/mental health measures (outcomes) | Findings | Quality rating |
| Decosimo et al. [36] | Ebola | Liberia | Randomized clinical trial Cluster sampling: 40 communities randomly selected from list of ‘hot zone’ communities and then randomly assigned to 3- or 5-month condition; all children in those communities eligible; response rates within com-munities not reported |
Triangulation of pre- and post- PSS checklists based on interviews with children, their parents, and facilitator ratings; | 870 children (ages 3–18) | 3- vs. 5-month exposure to psychosocial intervention (Playing to Live program: administered by clinical team; integration of art, play, and yoga therapies and child life expertise to improve coping, communication, and under-standing in children dealing with trauma) | Pretested PSS scorecard | PSS reduction for both conditions | 91 |
| Giordano, et al. [28] | COVID-19 | Italy | Pre-post Convenience sample |
Self-rated tiredness, sadness, fear, and worry Assessed pre- and post- listening experience session via mobile phone |
34 clinical staff from coronavirus care hospital unit | 5-week receptive music therapy with guided imagery delivered by mobile phone 3 playlist modules (breathing, energy, serenity); week 1: Breathing playlist; Subsequent weeks: playlist modules customized by music therapist team |
MTC-Q1 (pre-post listening sessions) MTC-Q2 (end of study) |
Improvements on all assessed symptoms | 51 |
| Khee et al., [19] | SARS | Singapore | Qualitative Convenience sample |
Therapy session information (collection and analytic methods not reported; number of sessions per participant not reported) | 144 healthcare providers | Group therapy facilitated by psychology team (supportive therapy) | Analysis of therapy session content | Multiple themes on impact of SARS on providers | 40 |
| Liu et al. [32] | COVID-19 | PRC | Randomized clinical trial Inpatients on isolation ward with confirmed COVID-19; participants randomly assigned to intervention or control groups |
EMR records for historical and clinical data Pre- and post-intervention self-completed questionnaires |
51 inpatients with confirmed COVID-19 | 5-day progressive muscle relaxation training by research team, 30 min/day vs. TAU (‘Jacobson's relaxation techniques’: ‘progressive muscle relaxation’, ‘deep breathing’) | STAI, SRSS | Improvement in both outcomes compared to TAU | 81 |
| Sotoudeh et al. [34] | COVID-19 | Iran | Randomized clinical trial Inpatients with confirmed COVID-19 assigned to control or intervention group |
Self-reported ratings collected pre- and post-intervention | 30 inpatients with confirmed COVID-19 | 4-Session brief crisis intervention package delivered by PhD clinical psychologists (developed from scientific literature to address COVID-specific recommendations content: relaxation, tension reduction, adjustment, and responsibility skills; increasing resiliency) | DASS21, SCL-25, WHOQOL-BREF | Improvement on all outcome measures compared to controls | 92 |
| Waterman et al. [20] | Ebola | Sierra Leone | Stepped intervention with assessments at 4 time points Convenience samples: staff from all 6 Ebola Treatment Centres invited to attend
|
Ratings and scales (both self- and facilitator-completed) over 3-phase process:
|
Ebola clinic staff:
|
|
Wellbeing screen (designed for study); AUDIT-3, GAD-7, PCL-C, Perceived Stress Scale, PHQ9, ISI | Improvement on all outcome measures | 73 |
| Wei et al. [33] | COVID-19 | PRC | Prospective randomized controlled trial All confirmed COVID-19 patients on isolation ward screened for psychological distress; recruits meeting threshold randomly assigned to intervention or supportive care (control) group |
Outcome measures at baseline, mid-point (Week 1), and study end (Week 2) (administration methods not reported) | 26 inpatients with confirmed COVID-19 and moderate psychological distress scores | Internet-based self-help intervention (4 components: breath relaxation; mindfulness, ‘refuge’ skills, butterfly hug method) Administered daily at a fixed time via mobile phone audio Control group received daily supportive care |
17-HAMD, HAMA | Increasing improvement in depression and anxiety scores over 2-week study period compared to controls | 83 |
| Zhou et al. [35] | COVID-19 | PRC | Pre-post Convenience sample; inpatients with suspected COVID-19 in tertiary hospital quarantine wards |
Anxiety and depression scales and subscales pre-post (administration methods not reported) | 63 inpatients with suspected COVID-19 recruited; 30 (scoring higher than set threshold) provided with intervention | Mobile phone-based individual counseling with on-site nurse (two 10-minute consultations, twice daily, with nurse providing listening, information, emotional and material support, and positive dialogue) | HADS and HADS anxiety and depression subscales | Pre-post improvement on all scale and subscale measures | 77 |
| What works to treat mental health sequelae? Implementation of existing or new training programs/guidelines/system-level protocols? | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| Study | Pandemic | Country | Design & type of sample | Assessment methods | Participants | Intervention/support (components/details) | Psychosocial/mental health measures (outcomes) | Findings | Quality rating |
| Chen et al. [22] | SARS | Taiwan | Longitudinal (4 time points) Convenience sample: Volunteers from nursing staff of largest obligatory SARS hospital |
Self-reported questionnaires completed pre-care delivery, 2 weeks and 1 months after start of care, 1 month after, and 1 month post-return to normal hospital functioning | 116 nurses from designated SARS treatment hospital | SARS prevention program (program content based on WHO and CDC epidemic prevention information to develop hospital protocols and standards for space, staff, and environment) | SAS, SDS, PSQI | Improvement in anxiety and depressive symptoms from baseline to time 4; no improvement in sleep quality | 74 |
| Cole et al. [25] | Ebola | Sierra Leone | Pre-post Convenience sample: Phase 3 participants (see Waterman et al. [20]) |
Self-completed outcome measures (with facilitator assistance available) at 1-week pre-intervention and within 2 weeks post-intervention | 253 Ebola treatment clinic staff enrolled in Phase 3 | 8 CBT group sessions over 6 weeks focusing on depression and anxiety | GAD-7, PHQ9, WSAS | Improvements in anxiety, depression, and functional impairment scores; results tempered by respondents' reading ability, geographic location, and facilitator characteristics | 77 |
| Geoffroy et al. [31] | COVID-19 | France | Cross sectional Convenience sample; all hospital workers in regional group of 39 hospitals eligible |
Data collected at time of call to hotline (over 26 days) | 149 hotline calls | Hotline volunteers providing rapid assessment, crisis resolution, referrals to other services as needed | Date/time of call; sociodemographic, professional, and hospital department characteristic; psychiatric history and reason for call | Rapidly developed (3-day) hotline-based support program demonstrated accessibility, spread (many professions, many hospital departments); numbers of referrals reported | 89 |
| Horn et al. [29] | Ebola | Sierra Leone, Liberia | Qualitative Purposive sampling of Psychological First Aid (PFA) participants |
Semi-structured interviews covering PFA training delivery during Ebola crisis, program fidelity, reflections on implementation of training | 23 PFA trainees, 36 PFA trainers; 14 key informants | Psychosocial support (Psychological First Aid – PFA - based on adapted PFA guide and training developed by WHO for Ebola) | Themes and subthemes abstracted via coding scheme developed and trialed by research team | Quality of training was variable | 90 |
| Maunder et al. [27] | Influenza pandemics | Canada | Randomized single-blind controlled trial All employees and professional staff of one hospital eligible; Volunteers randomly assigned to short (7 sessions), medium (12 sessions), or long (17 sessions) psychological training courses; courses to be completed at several sittings as participant-determined pace |
Self-completed outcome measures at pre- and post-course | 158 Canadian hospital workers | 3 course-lengths of interactive, self-administered computer- assisted training to improve resilience (multiple learning modality approach: Knowledge-based modules; audio modules teaching relaxation skills; interactive reflexive modules; self-assessment; quizzes and games) | Confidence scale, Pandemic Self-Efficacy Scale, IIP-32, Ways of Coping Inventory | Improvement in all measures (improvement in coping limited those with low baseline use of coping); higher dropout rate for longest course duration Best results for medium-length course |
94 |
| Sijbrandij et al. [30] | Ebola | Sierra Leone | Cluster-randomized single-blind controlled trial Eligible Public Health Units randomized to training and control conditions; PFS-naïve primary health care workers within each condition were approached to participate |
Self-completed questionnaires and independent rater-scored items completed at baseline, 3-month post-assessment (i.e., post-training), and 6-months follow-up | 408 primary health care workers | 1-day training for Psychosocial support (Psychological First Aid – PFA-based on adapted PFA guide and training developed by WHO for Ebola) | Questionnaires for: PFA knowledge, scenario response, professional attitude, confidence; ProQOL-5 | Increased PFA knowledge at post-assessment and 6-month follow-up. Increased scenario response and professional attitude at 6-month follow-up No impact on confidence |
98 |
| Waterman, et al. [21] | Ebola | Sierra Leone | Qualitative Convenience sample: CBT group facilitators and staff delivering Phase 3 intervention (see by Waterman et al. [20]; Cole et al. [25]) |
Thematic analysis of individual interviews with open ended questions regarding barriers and enablers for implementing group CBT session | 9 CBT group facilitators, 1 project coordinator | (implementation of CBT training program) | Themes abstracted from Interviews | Implementation barriers and enablers | 45 |
| Yoon et al. [39] | MERS | South Korea | Case study (of system) Population served by provincial mental health services for MERS victims |
Secondary analysis of provincial administrative data | 6231 patients | Mental health service system for:
|
Numbers of patients assessed or served at various system levels | 20% of total had emotional problems;
|
100 |
17-HAMD = 17-item Hamilton Depression Scale.
AUDIT-3 = Alcohol Use Disorders Identification Test-C.
DASS21 = Depression, Anxiety, and Stress Scale.
GAD-7 = Generalized Anxiety Disorder (7 item scale).
HADS, HADS-D, HADS-A = Hospital Anxiety and Depression Scale; depression subscale, anxiety subscale.
HAMA = Hamilton Anxiety Scale.
IIP-32 = Inventory of Interpersonal Problems (32 item scale).
ISI = Insomnia Severity Index.
IES-R = Impact of Event Scale-Revised.
MTC-Q1, MTC-Q2 = MusicTeamCare-Q1, MusicTeamCare-Q2.
PCL-C = Post-Traumatic Stress Checklist - Civilian.
PHQ9 = Patient Health Questionnaire.
PRC = People's Republic of China.
ProQOL-5 = Professional Quality of Life Scale (5 items).
PSQI = Pittsburgh Sleep Quality Index.
PSS = psychosocial stress symptoms.
SARS = severe acute respiratory syndrome.
SAS = Self-rating Anxiety Scale (Zung).
SCL-25, SCL-90 = Symptom Checklist 25, Symptom Checklist 90.
SDS = Self-rating Depression Scale (Zung).
SRSS = Sleep State Self-Rating Scale.
STAI = Spielberger State-Trait Anxiety Scale (STAI).
TAU = treatment as usual.
WHOQOL-BREF = World Health Organization Quality of Life (abbreviated version).
3.1. What kind of emotional reactions do medical pandemics trigger?
All of the studies described the emotional stress that health professionals [[19], [20], [21], [22], [23], [24], [25], [26], [27], [28]], non-specialists working in health care [[29], [30], [31]], patients [[32], [33], [34], [35]], children [36], and members of the general public experience during a medical pandemic [37,38,39]. The first cases of a novel disease to emerge spark fear among health professionals and non-specialists working in health care because little or nothing is known about the disease or how it is transmitted [19,[22], [23], [24],37]. Added to this fear is a sense of helplessness and uncertainty when the number of cases rises and continues to grow [19]. As colleagues and patients succumb to the illness, health professionals experience profound grief and sorrow.
Medical pandemics elicit strong emotional reactions, but health professionals cannot refuse to provide care for infected patients. They feel vulnerable, afraid that they will bring the disease home to their families, that they may die, that they will continue to lose colleagues. Many factors contribute to the stress that health professionals feel: the overwhelming workload, shortage of personal protection equipment, constant media coverage, lack of specific treatments, and inadequate support [24]. Psychological impacts of pandemics such as Ebola on children and their families include extreme stress, loss, and trauma [36]. The one study published to date on the public's psychological reaction to COVID-19 found that although people are feeling more stress and anxiety, positive reactions such as having faith in the future and feeling blessed for what one has have also surfaced [37]. Faced with uncertainty, it is common for people to seek positive solutions and social and group solidarity to maintain a sense of purpose and cohesiveness [[19], [20], [21],25,37].
3.2. What are the mental health sequelae?
Of the five studies in our review that focused on the mental health sequelae of COVID-19, only one conducted a true pre- post-test to explore the impacts of medical pandemics on mental health in order to guide policy and interventions for affected populations [37]. The study used online ecological recognition, an approach based on machine-learning predictive models, to calculate word frequency and emotional and cognitive indicator scores from the postings of regular bloggers on a popular Chinese website. A paired sample t-test was used to examine differences in content before and after January 20, 2020, when COVID-19 was declared to be transmissible by humans. The authors found that negative reactions such as anxiety, depression, and indignation increased after the declaration, and positive experiences such as happiness and life satisfaction decreased. Another study also found cross-sectional associations between emotional well-being, an individual's knowledge about COVID-10, and their sense of control [38,39].
These findings for the general public were echoed in the remaining three COVID-19 studies, which examined the mental well-being of health professionals during medical pandemics [23,24,26]. Two studies assessed the mental health of medical staff working in Wuhan, in the Chinese province Hubei [23], and of health professionals treating patients exposed to COVID-19 in different regions of China [24]. Both studies found high rates of depression, anxiety, insomnia, and distress using the Patient Health Questionnaire, the Generalized Anxiety Disorder scale, the Insomnia Severity Index, and the Impact of Event Scale–Revised. For example, 70% of respondents reported psychological distress [24]. Psychological distress varied by gender (higher for women), health profession (higher for nurses), and level of exposure to COVID-19 (higher for those working in the epicenter of the pandemic) [23,24]. Higher rates of symptoms were also found in a third study that used a different set of assessment tools (Symptom Checklist 90, Self-rating Depression and Anxiety Scales, and Post-traumatic Stress Checklist–Civilian). The study also found poorer sleep quality (Pittsburgh Sleep Quality Index) among front-line staff who had higher risks of exposure to COVID-19 [26].
Some evidence suggests that delays in receiving mental health interventions result in higher rates of baseline negative psychological symptoms. For example, a study that examined the impact of a psychosocial support program for children in 40 Liberian communities identified as Ebola “hot zones” found that the two-month delay in receiving support may have exacerbated the distress that these children felt [36].
3.3. Who is most at risk of mental health sequelae?
Several studies identified specific populations that are more vulnerable during a medical pandemic and thus have a higher need for mental health interventions, which should be tailored to their specific needs. Among health professionals, women and nurses treating patients with COVID-19 warrant particular attention [23,24,26]. Study findings suggest that the relationship between levels of exposure to COVID-19 and levels of mental health symptoms mediates the kinds of support that health professionals prefer [23]. For example, physicians and nursing staff with higher levels of mental health problems showed more urgent desires to seek help from psychotherapists and psychiatrists while those with subthreshold or mild disturbances preferred to obtain services from medial sources [23]. Physicians and nursing staff who work at newly created or designated pandemic treatment hospitals at the epicenter of a crisis tend to be the hardest hit emotionally and mentally [22,24,28]. Children are another high-risk group. Given their low social status, dependence on caregivers, vulnerability to becoming orphaned during a medical pandemic, and the lack of child-oriented services, children require interventions that address their unique needs [36].
Our review also found that developing countries face challenges in coordinating efforts and ensuring the quality of training during a medical pandemic [29,30]. Although health professionals sometimes received support from other non-profit organizations, lack of coordination often meant that people received duplicate training from different organizations. Given the shortage of health professionals in developing countries, some non-specialist trainers became involved in providing education during a pandemic because they themselves needed psychological support, and delivering training was the only way they could learn to cope with the situation they were working in [29].
3.4. What works to treat mental health sequelae?
Sixteen studies on mental health interventions were grouped under two categories: psychosocial interventions (n = 8) and the implementation of existing or new training programs, guidelines, or system-level protocols (n = 8).
3.4.1. Psychosocial interventions
One qualitative study examined group therapy sessions for physicians and nurses who were providing care for SARS patients in Singapore [19]. The researchers did not measure the efficacy of the therapy, but used the information they gathered to explore the emotional impact on these health care providers. Two trends were identified: the first was the emergence of emotions such as fear, anger, and blame at the beginning of the outbreak. The second trend featured emotions such as grief, frustration, and loss as death tolls rose, including among colleagues. Overall, fear was the most common emotion. Lack of social support, created by the need for distancing, added to the stresses of providing care.
The second study evaluated the effectiveness of a complex three-phase training program for Ebola clinic staff, which was launched when the number of new Ebola cases in Sierra Leone was decreasing [20]. Phases 1 and 2 involved a well-being workshop and screen, and psychoeducation workshops. Trainees who scored above thresholds for well-being, anxiety, or depression were eligible to attend Phase 3, which involved a 6-week cognitive behavioral therapy (CBT) program delivered by colleagues. The study found some improvement in well-being, anxiety, and depression across all three phases. In Phase 3, CBT participants showed decreased anxiety, depression, PTSD, and stress symptoms, and improved sleep, sense of well-being, and relationships.
Two studies assessed mobile phone–delivered interventions—one for healthcare staff and one for patients. The first study examined the effectiveness of a music therapy intervention for staff working on a coronavirus unit in a hospital in Italy [28]. During the study, participants self-isolated in a hotel to minimize risk of infecting their families, and listened to playlists that focused on breathing, energy, and serenity. Playlists were customized for each participant based on their listening experience from the previous week. Participants reported their levels of tiredness, sadness, fear, and worry before and after listening to the customized playlists. The study found improvements in these symptoms, especially with the energy playlist, which showed significant changes in all four symptoms.
The second mobile-phone study focused on the impact of an individual consultation intervention on inpatients with suspected COVID-19 who were in quarantine wards in a tertiary hospital in Guangdong, China [35]. The intervention involved twice-daily 10-minute consultations with an onsite nurse who provided information and support. Participants were assessed using the Hospital Anxiety and Depression Scale before and at the end of the intervention and showed improvement in mood on the anxiety and depression subscales.
Four studies evaluated interventions using a randomized trial design. In the study that examined the impact of a psychosocial support program for Liberian children in Ebola “hot zones,” communities were randomly assigned to a 5-month or a 3-month arts-based program, and all children were eligible to participate [36]. Both groups showed significant decreases in stress, but there was no statistical difference between the two programs. In discussing why the longer program did not produce better results, the researchers noted that children in the shorter program started two months after those in the longer program and also had higher beginning levels of stress. They speculated that the two-month delay in receiving support may have exacerbated the distress that these children felt.
Three randomized controlled studies examined the efficacy of specific interventions aimed at reducing anxiety or depression symptoms in inpatients with COVID-19. One trial involved progressive muscle relaxation [32]. Compared with controls, participants in the five-day course showed significant improvement in anxiety and sleep, as measured by the Spielberger State-Trait Anxiety Scale and the Sleep State Self-Rating Scale. The second trial featured a four-session brief crisis intervention to improve resilience by building skills related to: adjustment skills, responsibility and factualism and spirituality [34]. The intervention group showed greater improvement on symptoms as measured by the Depression, Anxiety, and Stress Scale, SCL-25, and WHOQOL-BREF. In the third trial, which involved an Internet-based self-help intervention, participants showed reduced anxiety symptoms after one week, as assessed by the Hamilton Depression and Hamilton Anxiety scales and even further improvement by the second week [33]. The common thread in these three studies is the active and sustained involvement of patients in their own care.
3.4.2. Implementation of existing or new training programs, guidelines, and system-level protocols
Eight studies evaluated the implementation of existing or new training programs, guidelines, and system-level protocols. Four focused on the Ebola pandemic; two examined the SARS or influenza-related pandemics; one evaluated a psychosocial support system developed in response to COVID-19; and one used a system-level protocol developed for MERS as a case study.
The Ebola studies examined train-the-trainer programs [21,25,29,30]. Two also explored a CBT-based peer-to-peer training program [21,25]. One of the CBT-based studies of these involved qualitative interviews with clinical staff; the other assessed the impact of the intervention on clinical staff. Both studies identified implementation barriers and enablers. Among the barriers relevant to the setting (sub-Saharan Africa) were low literacy, cultural understanding of mental health problems, and lack of resources. Enablers included the novelty of the intervention and the opportunity for staff to create social networks. In one of these studies, there were no differences in baseline anxiety and depression symptoms between those holding roles with high versus low risk of exposure to infection [25]. The authors hypothesized that this finding could be due to factors such as better previous training for the high-risk group, which may have acted as a protective factor. The remaining two studies evaluated a psychological first aid program [29,30]. The first was a qualitative study that involved interviews with psychological first aid trainers, trainees, and administrators in Sierra Leone and Liberia [29]. Implementation relied on training non-specialists to deliver the intervention. The authors concluded that the quality of the train-the-trainer method varied and that the program content and short duration were better suited to people with more experience. The second study, conducted by members of the same research team, was a cluster-randomized controlled trial evaluating the psychological first aid training of primary care workers in Sierra Leone [30]. Compared with controls, trainees had improved scores for knowledge about psychological first aid–consistent psychosocial support, both shortly after training and 3 months later (i.e. 6-month post-baseline). Scenario responses (designed to assess whether participants could apply their knowledge in a practical situation), as well as professional attitudes (designed to assess participants' ability to be non-judgmental) also showed improvement for trainees, but only at the 6-month assessment. There was no statistical difference between trainees and controls on confidence levels. These results highlight the value of assessing the impact of training over time, possibly after trainees have a chance to apply what they have learned and to consolidate it with their post-training real-world activities.
The SARS and influenza-pandemic studies examined two very different aspects of dealing with pandemics. The first study examined the impact of a prevention plan on the mental health of nurses in the largest designated SARS hospital in Taiwan [22]. Anxiety, depression, and sleep quality were measured using the Zung Anxiety and Depression Self-Rating Scale and the Pittsburgh Sleep Quality Index. Nurses were assessed four times: before the program was implemented, 2 weeks and 4 weeks after implementation, and 3 months after the program concluded. Anxiety, depression, and sleep quality showed signs of improvement at 2 weeks, and mental health symptoms continued to decrease over time; however, sleep quality remained poor. The findings suggest that coping ability increases with perceived sense of control over stressful circumstances. The program provided an opportunity for nurses to learn more about SARS and about important prevention measures that buffer the negative impacts of work stress.
The second study assessed whether there was a dose-related response to three durations of a computer-assisted resilience training program for hospital workers [27]. The study assessed levels of confidence, pandemic self-efficacy, interpersonal problems (Inventory of Interpersonal Problems), and coping (Ways of Coping Inventory). Participants in the medium- and longer-length courses showed improvement across all measures, except coping where improvements were limited to participants who reported underusing coping strategies at baseline. The researchers concluded that, although the longer course was associated with improved outcomes, the findings need to be balanced against the higher dropout rate for this arm of the trial; therefore, they recommended considering the medium-length course as an effective option.
The need for a rapid response to support staff during COVID-19 was the focus of a French study [31]. In three days, researchers developed a psychosocial support program that was based on a hotline system. In that short time, they were able to gain support from official authorities; recruit and certify hotline responders (certified psychologists) and medical back-up (psychiatrists); create the hotline protocols and content; set up the hotlines; create an anonymized database; and advertise the program. Intended beneficiaries of the program were all staff in a regional group of 39 hospitals. Hotline responders provided rapid assessment, brief crisis resolution, and service referrals. Results supported the feasibility (149 calls within 26 days), spread (callers represented various professions and hospital departments), and utility (70% of callers were also referred to COVID-19 and other kinds of support).
Finally, a case study of a mental health service system protocol designed to address the needs of patients with MERS and their families in South Korea identified areas for improvement going forward [39]. The system was created for patients in quarantine and for families of MERS patients who had died or recovered. Administrative data collected on quarantined, recovered, and deceased patients were used to describe the flow of individuals through the designated protocols, which included physical and psychological monitoring and assessment by the provincial public health and community mental health centers. The study found that of the more than 6000 patients quarantined, 20% were identified as having emotional problems and 6% had emotional problems needing continual mental health care. Of this latter group, only 35% actually received the indicated care. In addition, having a national access point to provincial or local-level services was not effective, particularly for recovered patients or family members of deceased patients.
3.5. What do we need to consider when designing and implementing mental health interventions?
3.5.1. Cultural considerations
Two of the 21 studies identified in our study merely mentioned culture and the influence of environmental factors as limitations, without explaining how these factors influenced the implementation of mental health interventions for COVID-19 [32,34]. Only five studies, all from Liberia and focusing on the Ebola pandemic, discussed the importance of cultural adaptation to the local context in detail. The remaining 14 studies did not provide contextual or cultural factors related to the implementation of mental health interventions or training.
Two of the five studies described the challenges with implementing and sustaining a CBT intervention related to differing cultural conceptualizations of mental illness, low literacy levels, and competing priorities such as employment [21,25]. These studies describe adaptations to training materials to enhance cultural appropriateness. The interventions emphasized the importance of using or incorporating cultural rituals of healing that embody a community's belief system within mental health and psychosocial programming [36]. Mental health problems are often conceptualized in ways that differ from the Western biopsychosocial model; for example, they may be caused by witchcraft, evil spirits, or curses. Cultural differences in conceptualizing mental health can make it challenging for participants to understand novel approaches such as CBT that are the focus of many Western-based interventions or training programs [21]. Moreover, mental health screening and assessment tools such as the Patient Health Questionnaire and the Generalized Anxiety Disorder scale for measuring anxiety and depression were developed in the West and their reliability and validity have not been established in non-Western countries [25].
Literacy is another consideration. Because CBT typically involves written materials and homework, interventions need to be adapted for patients with low literacy. Validated adaptations of CBT materials for low-literacy populations in general are lacking [20], but one study that we identified adapted the intervention by including more diagrams and images to depict CBT concepts [25].
There are also cultural considerations in children's mental health. One study noted that the low status of children in some cultures may make the mental health of this population a low priority [36]. The authors relied on key partnerships with government ministries for ethical and cultural guidance on creating data collection instruments and collecting information in a culturally appropriate way [36]. Similarly, the authors of the study on psychological first aid interventions adapted the program's content to reflect the Liberian context during the Ebola outbreak [29,30]. The authors indicate that even when adaptations have been made, it is difficult to ensure the quality of training in delivering the intervention. The authors add that trainees are often expected to change their attitudes and beliefs, as well as learn new skills, and the effort involved in making these changes should not be underestimated [29].
One study noted that cultural adaptations alone may not be enough to increase the success of an intervention [20]. For example, in some countries, traditional healers command more respect than trained health professionals, which means that collaborating with them is important to deliver interventions that are effective and sustainable.
3.5.2. Mental health work force
The majority of studies describing mental health interventions or training in low-resource countries acknowledged a shortage of trained mental health professionals [21,25,29,32]. Although this might also be true in middle- and high-resource countries, none of the studies from China, Canada, France, or Iran provided information on the mental health work force. The one study from Italy indicated that newly recruited clinicians at designated COVID-19 hospitals had inadequate psychological training [28]. Another study from Liberia described the challenges of using a train-the-trainer model for psychological first aid training as a capacity-building response [29]. The authors describe how, in the country's economic climate, it was difficult to take people out of their current work environment to attend training. As a result, training sessions were shorter than would be ideal, which affected the quality of training. Because it was also difficult to find non-professionals who had education or training in mental health or psychological support, key ideas or approaches to the intervention were not always implemented as intended. Trainees who lacked adequate education in mental health were often unable to navigate the nuances of therapeutic encounters. Limited mental health knowledge and training time meant that training material could become diluted or misrepresented as successive groups of trainers provide the training.
3.6. What still needs to be known?
Several primary research studies discussed strengths and limitations to their work. Half of the studies noted recruitment bias, small sample size, and response bias as limitations to the generalizability of their findings [[22], [23], [24],26,33,[35], [36], [37]]. Collecting data, especially in hectic times at the epicenter of a medical pandemic can be challenging for data collectors [36]. Incomplete data sets and missing information were common. Future studies should consider ways to distinguish between pre-existing and new mental health symptoms [23], use larger sample sizes to verify results [23,28,34], and adopt study designs such as randomized prospective studies to better determine correlations and causation [23,27].
4. Discussion
Previous medical pandemics have led to policies, working group recommendations, protocols, and interventions that are helping to guide responses to the COVID-19 pandemic. However, it is surprising that few published evaluations of these interventions exist, particularly those arising from SARS.
The primary research articles that do exist provide reasonably strong evidence for several conclusions and recommendations that can provide direction for dealing with COVID-19. The mental health sequelae of pandemics are significant and should be addressed in a timely, sustained way. The psychological response of healthcare workers to medical pandemics is complicated. These pandemics are extraordinary historical events that dramatically change health care services and delivery. When little or nothing is known about highly infectious and unusual viruses, lack of knowledge about the mode of transmission and risk of exposure for medical workers creates a sense of helplessness and uncertainty that lead to a general state of fear. Sources of distress include feelings of vulnerability or loss of control and concerns about one's health and the health of one's family and others, and about the spread of the virus.
A range of mental health services and supports are needed to meet the unique needs of specific groups with different vulnerabilities and risks. Health professionals and other people exposed to COVID-19, including children, are high-needs, high-risk groups. Resources are also needed to support the mental health needs of the general public. This review found that non-psychiatric mental health supports can be effective in addressing mental health concerns during medical pandemics [26,28,32,33,[35], [36], [37]]. Providing opportunities to create social networks and establishing protocols for ensuring safety enhance well-being among health professionals and the general public. Particular attention needs to be paid to cultural considerations when designing and implementing mental health interventions and training. Training non-specialists when mental health professionals are scarce builds capacity and empowers communities to deliver mental health interventions. However, training non-specialists requires time. Without adequate investment, trainees will not be able to provide the emotional and practical support that people need during a pandemic.
The high quality of more than half of the primary research studies that were reviewed in our study provides encouraging support for these recommendations. However, the range of the quality ratings (40–100%) suggests a need for caution. The main reason for lower quality ratings was insufficient, or sometimes lacking, descriptions of two elements: 1) the sampling strategy, sample characteristics, or the underlying population; and 2) discussion or acknowledgment of the limitations of sample size, particularly in quantitative studies. Information gaps for these two criteria create uncertainty about how applicable the findings might be when generalizing to other settings or populations.
Overall, this review revealed that various mental health interventions have been developed for medical pandemics and that research on their effectiveness is growing. However, few studies distinguished between pre-existing mental health problems and those that are triggered by medical pandemics. Studies of the SARS outbreak suggest the need for training and support to bolster the resilience of healthcare professionals, particularly those with a history of mental health problems, in dealing with future pandemics [40,41]. Resilience training for psychologically healthy health professionals will support them not only during the unpredictability of a medical pandemic, but also during regular clinical practice [27,41,42]. Our review also found promise in interventions in which people were actively involved in their care over a sustained period [32,33]. When designing mental health interventions for health professionals, we also need to know more about protective factors that buffer the negative psychological impacts during and after a medical pandemic.42 This review showed some evidence for the importance of evaluating longer-term impacts of training because some impacts are not realized until several months after training [30].
Another area to explore is digital/social media interventions for mental health support [27,28,31,33,35]. The public health and health care measures used to address COVID-19 (e.g., physical distancing, isolation/quarantine), combined with the high levels of uncertainty and concern, create special stresses, especially on traditional and resource-intensive ways of providing care and support. Interventions that are synchronous (occur in real time) and asynchronous (occur online without real-time interaction) using digital and social media are an increasingly relevant focus for research. Developing and evaluating social media and digital health interventions are ways to extend and support existing interventions, as well as to involve patients and the general public more actively in their own care. The effectiveness of such interventions (both independently and in coordination with other programs), and the feasibility of developing and implementing them are rapidly growing concerns for future research.
4.1. Strengths and limitations of this systematic rapid review
There are limitations and strengths of this review. The search was limited to peer-reviewed publications written in English. Given the large amount of information from China, we would have included members of our team who could read Mandarin if that had been possible. Moreover, by focusing on peer-reviewed literature, we could not capture findings from the grey literature. Strengths of this review included a formal quality appraisal of the articles and a search process that ensured we were able to examine the most recently published articles possible.
4.2. Future research
There are positive signs that more is being done to address mental health during medical pandemics. Since the COVID-19 pandemic emerged, we found seven high-quality articles that focused on COVID-19 [23,24,[32], [33], [34], [35],37], of which two were randomized control trials of interventions [32,33]. In addition, as of August 11, 2020, a search on clinicaltrials.gov, using the terms “mental health interventions” and “COVID-19” for all countries, yielded 33 studies, of which eight focused on the mental health and well-being of health professionals and 25 focused on patients and the general public. We interpret these findings as showing global readiness to move toward study designs that better determine correlation and causation. There is a need for continued support and focus on evaluations in order to develop an even stronger evidence base for addressing future medical pandemics. This is the time to capitalize on the momentum for building a robust evidence base for COVID-19. Doing so will assist people in immediate need of mental health support and help to plan multi-pronged mitigation strategies for the future.
Funding
This research received no specific grant from any funding agency, commercial or not-for-profit sectors.
CRediT authorship contribution statement
Sophie Soklaridis contributed to the literature search, study design, figures, data collection, data analysis, data interpretation, and writing of the manuscript.
Elizabeth Lin contributed to the literature search, figures, study design, data collection, data analysis, quality assessment, data interpretation, and writing of the manuscript.
Yasmin Lalani contributed to data collection, data analysis, data interpretation, and writing of the manuscript.
Terri Rodak contributed to the literature search, study design, data collection, and writing of the manuscript.
Sanjeev Sockalingam contributed to the study design, figures, data interpretation, quality assessment, and writing of the manuscript.
Declaration of competing interest
None.
Acknowledgments
Acknowledgement
We would like to thank Hema Zbogar for her editorial support in preparing this manuscript.
Data availability
The data that support the findings of this study are available from the corresponding author, SS, upon reasonable request.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.genhosppsych.2020.08.007.
Appendix A. Supplementary data
Supplementary material 1
Supplementary material 2
References
- 1.Jalloh M.F., Li W., Bunnell R.E. Impact of Ebola experiences and risk perceptions on mental health in Sierra Leone, July 2015. BMJ Glob Health. 2018;3 doi: 10.1136/bmjgh-2017-000471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ho C.S., Chee C.Y., Ho R.C. Mental health strategies to combat the psychological impact of COVID-19 beyond paranoia and panic. Ann Acad Med Singapore. 2020;49:1–3. [PubMed] [Google Scholar]
- 3.Lu W., Wang H., Lin Y., Li L. Psychological status of medical workforce during the COVID-19 pandemic: a cross-sectional study. Psychiatry Res. 2020;288 doi: 10.1016/j.psychres.2020.112936. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Du J., Dong L., Wang T. Psychological symptoms among frontline healthcare workers during COVID-19 outbreak in Wuhan. Gen Hosp Psychiatry. April 3 2020 doi: 10.1016/j.genhosppsych.2020.03.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Fessell D., Cherniss C. Coronavirus disease 2019 (COVID-19) and beyond: micropractices for burnout prevention and emotional wellness. J Am Coll Radiol. March 24 2020 doi: 10.1016/j.jacr.2020.03.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Williamson V., Murphy D., Greenberg N. COVID-19 and experiences of moral injury in front-line key workers. Occup Med (Lond) Apr 2 2020 doi: 10.1093/occmed/kqaa052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Dewey C., Hingle S., Goelz E., Linzer M. Supporting clinicians during the COVID-19 pandemic. Ann Intern Med. March 20 2020 doi: 10.7326/M20-1033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Xiang Y.T., Yu X., Ungvari G.S., Correll C.U., Chiu H.F. Outcomes of SARS survivors in China: not only physical and psychiatric co-morbidities. East Asian Arch Psychiatry. 2014;24:37–38. [PubMed] [Google Scholar]
- 9.Shanafelt T., Ripp J., Trockel M. Understanding and addressing sources of anxiety among health care professionals during the COVID-19 pandemic. JAMA. April 07 2020 doi: 10.1001/jama.2020.5893. [DOI] [PubMed] [Google Scholar]
- 10.Yıldırım M., Arslan G. 2020. Exploring the associations between resilience, dispositional hope, subjective well-being, and psychological health among adults during early stage of COVID-19. [under review] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Maunder R., Hunter J., Vincent L. The immediate psychological and occupational impact of the 2003 SARS outbreak in a teaching hospital. CMAJ. 2003;168:1245–1251. [PMC free article] [PubMed] [Google Scholar]
- 12.Xiang Y.T., Yang Y., Li W. Timely mental health care for the 2019 novel coronavirus outbreak is urgently needed. Lancet Psychiatry. 2020;7:228–229. doi: 10.1016/S2215-0366(20)30046-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Moher D., Liberati A., Tetzlaff J., Altman D.G. Preferred reporting items for systematic reviews and metaanalyses: the PRISMA statement. Ann Intern Med. 2009;151:264–269. doi: 10.7326/0003-4819-151-4-200908180-00135. [DOI] [PubMed] [Google Scholar]
- 14.Aromataris E., Munn Z. Chapter 1: JBI systematic reviews. In: Aromataris E., Munn Z., editors. Joanna Briggs Institute reviewer’s manual. The Joanna Briggs Institute; 2017. https://reviewersmanual.joannabriggs.org/ Available from. [Google Scholar]
- 15.International Classification of Health Interventions—ICHI Beta 2017. https://mitel.dimi.uniud.it/ichi/ Available online.
- 16.Kmet L.M., Lee R.C., Cook L.S. Standard quality assessment criteria for evaluating primary research papers from a variety of fields. Feb. 1 2004. https://www.ihe.ca/publications/standard-quality-assessment-criteria-for-evaluating-primary-research-papers-from-a-variety-of-fields
- 17.Lee S.Y., Fisher J., Wand A.P.F. Developing delirium best practice: a systematic review of education interventions for healthcare professionals working in inpatient settings. Eur Geriatr Med. 2020;11:1–32. doi: 10.1007/s41999-019-00278-x. [DOI] [PubMed] [Google Scholar]
- 19.Khee K.S., Lee L.B., Chai O.T., Loong C.K., Ming C.W., Kheng T.H. The psychological impact of SARS on health care providers. Crit Care Shock. 2004;7:99–106. [Google Scholar]
- 20.Waterman S., Hunter E.C.M., Cole C.L., Evans L.J., Greenberg G.J., Beck A. Training peers to treat Ebola centre workers with anxiety and depression in Sierra Leone. Int J Soc Psychiatry. 2018;64:156–165. doi: 10.1177/0020764017752021. [DOI] [PubMed] [Google Scholar]
- 21.Waterman S., Cole C.L., Greenberg N., Rubin G.J., Beck A. A qualitative study assessing the feasibility of implanting a group cognitive-behavioural therapy-based intervention in Sierra Leone. BJPsych Int. 2019;16:31–34. doi: 10.1192/bji.2018.7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Chen R., Chou K.R., Huang Y.J., Wang T.S., Liu S.Y., Ho L.Y. Effects of a SARS prevention programme in Taiwan on nursing staff’s anxiety, depression and sleep quality: a longitudinal survey. Int J Nurs Stud. 2006;43:215–225. doi: 10.1016/j.ijnurstu.2005.03.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kang L., Ma S., Chen M. Impact on mental health and perceptions of psychological care among medical and nursing staff in Wuhan during the 2019 novel coronavirus disease outbreak: a cross-sectional study. Brain Behav Immun. 2020 doi: 10.1016/j.bbi.2020.03.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Lai J., Ma S., Wang Y. Factors associated with mental health outcomes among health care workers exposed to Coronavirus disease 2019. JAMA Netw Open. 2020;3 doi: 10.1001/jamanetworkopen.2020.3976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Cole C.L., Waterman S., Hunter E.C.M. Effectiveness of small group cognitive behavioural therapy for anxiety and depression in Ebola treatment centre staff in Sierra Leone. Int Rev Psychiatry. April 17 2020 doi: 10.1080/09540261.2020.1750800. [DOI] [PubMed] [Google Scholar]
- 26.Wu K., Wei X. Analysis of psychological and sleep status and exercise rehabilitation of front-line clinical staff in the fight against COVID-19 in China. Med Sci Monit Basic Res. 2020;26 doi: 10.12659/MSMBR.924085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Maunder R.G., Lancee W.J., Mae R. Computer-assisted resilience training to prepare healthcare workers for pandemic influenza: a randomized trial of the optimal dose of training. BMC Health Serv Res. 2010;10:72. doi: 10.1186/1472-6963-10-72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Giordano F., Scarlata E., Baroni M. Receptive music therapy to reduce stress and improve wellbeing in Italian clinical staff involved in COVID-19 pandemic: a preliminary study. Arts Psychother. 2020;70:1–5. doi: 10.1016/j.aip.2020.101688. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Horn R., O’May F., Esliker R. The myth of the 1-day training: the effectiveness of psychosocial support capacity-building during the Ebola outbreak in West Africa. Glob Ment Health (Camb) 2019;6:e5. doi: 10.1017/gmh.2019.2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Sijbrandij M., Horn R., Esliker R. The effect of psychological first aid training on knowledge and understanding about psychosocial support principles: a cluster-randomized controlled trial. Int J Environ Res Public Health. 2020;17(2) doi: 10.3390/ijerph17020484. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Geoffroy P.A., Le Goanvic V., Sabbach O. Psychological support system for hospital workers during thre Covid-19 outgreak: rapid design and implementationof the Covid-Psy hotline. Front Psych. 2020;11:11. doi: 10.3389/fpsyt.2020.00511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Liu K., Chen Y., Wu D., Lin R., Wang Z., Pan L. Effects of progressive muscle relaxation on anxiety and sleep quality in patients with COVID-19. Complement Ther Clin Pract. 2020;39 doi: 10.1016/j.ctcp.2020.101132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Wei N., Huang B., Lu S. Efficacy of internet-based integrated intervention on depression and anxiety symptoms in patients with COVID-19. J Zhejiang Univ Sci B. 2020;1581:1–5. doi: 10.1631/jzus.B2010013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Sotoudeh H.G., Alavi S.S., Akbari Z., Jannatifard F., Artounian V. The effect of brief crisis intervention package on improving quality of life and mental health in patients with COVID-19. Iran J Psychiatry. 2020;15:205–212. doi: 10.18502/ijps.v15i3.3812. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Zhou L., Xie R., Yang X., Zhang S., Li D., Zhang Y. Feasibility and preliminary results of effectiveness of social media-based intervention on the psychological well-being of suspected COVID-19 cases during quarantine. Can J Psychiatry. 2020:1–3. doi: 10.1177/0706743720932041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Decosimo C.A., Hanson J., Quinn M., Badu P., Smith E.G. Playing to live: outcome evaluation of a community-based psychosocial expressive arts program for children during the Liberian Ebola epidemic. Glob Ment Health (Camb) 2019;6:e5. doi: 10.1017/gmh.2019.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Li S., Wang Y., Xue J., Zhao N., Zhu T. The impact of COVID-19 epidemic declaration on psychological consequences: a study of active Weibo users. Int J Environ Res Public Health. 2020;17:2032. doi: 10.3390/ijerph17062032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Yang H, Ma J. How an epidemic outbreak impacts happiness: Factors that worsen (vs. protect) emotional well-being during the coronavirus pandemic. Psychiatry Res. 2020;289(113045) doi: 10.1016/j.psychres.2020.113045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Yoon M.K., Kim S.Y., Ko H.S., Lee M.Y. System effectiveness of detection, brief intervention and refer to treatment for the people with post-traumatic emotional distress by MERS: a case report of community-based proactive intervention in South Korea. Int J Ment Health Syst. 2016;10:51. doi: 10.1186/s13033-016-0083-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Lancee W.J., Maunder R.G., Goldbloom D.S. Prevalence of psychiatric disorders among Toronto hospital workers one to two years after the SARS outbreak. Psychiatr Serv. 2008;59:91–95. doi: 10.1176/ps.2008.59.1.91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Maunder R.G., Leszcz M., Savage D. Applying the lessons of SARS to pandemic influenza: an evidence-based approach to mitigating the stress experienced by healthcare workers. Can J Public Health. 2008;99:486–488. doi: 10.1007/BF03403782. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Wu P., Fang Y., Guan J. The psychological impact of the SARS epidemic on hospital employees in China: exposure, risk perception, and altruistic acceptance of risk. Can J Psychiatry. 2009;54:302–311. doi: 10.1177/070674370905400504. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary material 1
Supplementary material 2
Data Availability Statement
The data that support the findings of this study are available from the corresponding author, SS, upon reasonable request.