Abstract
The severe acute respiratory syndrome corona virus 2, responsible for the worldwide COVID-19 pandemic, has caused unprecedented changes to society as we know it. The effects have been particularly palpable in the practice of medicine. The field of otolaryngology has not been spared. We have had to significantly alter the way we provide care to patients, changes that are likely to become a new norm for the foreseeable future. This article highlights some of the changes as they apply to otology/neurotology. Although this is written from the perspective of an academic physician, it is also applicable to private practice colleagues.
Keywords: Mastoidectomy, Middle ear, Skull base surgery, Neurotology, Infectious disease, COVID-19, SARS-CoV-2
Key points
-
•
The use of traditional facemasks impairs communication with hard-of-hearing and deaf patients because it restricts lip reading ability. Implementing transparent windows is a strategy to help mitigate this problem.
-
•
Preoperative screening for COVID-19 guides providers and staff in the use of adequate personal protective equipment and may potentially delay surgical intervention in positive patients, a practice driven by reports of poor perioperative prognosis.
-
•
Respirators are used during most otologic and neurotologic procedures; the need for routine controlled air-purifying respirator and powered air-purifying respirator use is uncommon.
-
•
Alterations to standard microscope draping to mitigate spread of pulverized bone splatter during mastoid drilling should be considered, given the unknown risk posed by aerosolized particles from the middle ear and mastoid.
-
•
Telehealth is an option for otologic and neurotologic patients. Examples are patients with cochlear implants, tinnitus/hyperacusis management, as well as atypical migraine and some vestibular patients. Neurotologic consultations are also feasible, such as treatment planning and surveillance of vestibular schwannoma.
History
At the time of this entry, the number of worldwide Coronavirus Disease-19 (COVID-19) cases surpassed 10 million; 2.6 million claimed by the United States. Those numbers are startling, and although many countries are seeing a stabilization or even decline in cases, the United States is currently facing a surge, with no end in sight. Our hopes are heavy on the development of a safe and effective vaccine.
The field of otolaryngology has been at the forefront in creating novel ways to deliver care due to our command of the upper aerodigestive tract. Scientific endeavors were jump-started by discovery of high viral loads in the nasopharynx.1 , 2 We have had to alter how to examine patients, from deciphering what is adequate personal protective equipment (PPE), to the way rooms are ventilated and equipment disinfected, to how we manage patient workflow to provide proper screening and implement social distancing parameters within the clinics. We have also had to develop new preoperative and intraoperative protocols, including alterations to well-established operating room (OR) setups. The changes have been topics of much discussion and approached differently depending on the nature of the facility, each taking into account the availability of reliable COVID-19 polymerase chain reaction (PCR) testing, adequate PPE, and staff resources. Not surprisingly, these factors can be vastly different when considering, for example, a large tertiary medical center versus small independent outpatient surgical facility. The wide spectrum thus prompts protocols that reflect internal resources unique to each facility.
Although those who routinely manage the upper digestive tract endured the most drastic changes to their practice, otologists and neurotologists have not been spared. At the height of the pandemic, when much was unknown and reliable viral testing was unavailable and PPE sparse, we faced a startling stop in outpatient and surgical care. What was deemed “elective” was suspended, and only urgent and essential care provided. Many dove into telehealth visits, albeit knowing that lack of an adequate microscopic examination or audiometric and vestibular testing limited diagnosis and treatment options. As time passed, however, we faced the uncharted territory of triaging patient care. When would it be safe to offer stapedectomies? Tympanoplasties or cochlear implants? Could that draining chronic ear wait a few weeks, or a month or 2? What about vestibular schwannoma surgery or repair of cerebrospinal fluid (CSF) leaks? We flocked to online professional forums and sought guidance from national societies and international colleagues, many with weeks or months of experience behind them, all with the intent to gather a collective voice.
Patients were understandably conflicted as well, anxious at the thought of going into facilities with COVID-19–positive inpatients. Elderly individuals and those with comorbid conditions were in a precarious situation, left weighing the benefit of getting a much-awaited cochlear implant for example, with the risk of nosocomial infection. It was not until there was reliable testing for severe acute respiratory syndrome corona virus 2 (SARS-CoV-2), a steady supply of PPE, and predictable inpatient hospital resource capacity that we phased back into the OR and clinics.
During this time, we saw a surge of society consensus statements and recommendations or guidelines that were difficult to implement because of the variability in loco-regional virus burden and health care capacity between states and even counties. Ultimately, many of those statements or recommendations found themselves quickly outdated as information about the virus evolved. Given the rapid evolution of the pandemic, at the time of this entry, the published data were too scarce to implement robust evidence-based protocols. This is particularly true for the otology/neurotology practice. In the following text, I review some of the changes to the practice of otology and neurotology in the United States, in the context of the COVID-19 pandemic.
Background
Otology and neurotology as subspecialties are unique in that we manage a wide spectrum of acuity. From elective procedures like stapedectomy, ossiculoplasty, tympanoplasty or cochlear implants, to more ominous conditions like extratemporal complications of chronic ear disease or temporal bone malignancies. On the neurotology side, we manage cerebellopontine angle (CPA) lesions, some that present as small tumors, whereas others are large enough to pose imminent brainstem compression. Similarly, with CSF leaks, some present with a chronic history of relatively asymptomatic CSF otorrhea, whereas others are acutely ill with meningitis. Some conditions clearly need to be managed urgently, because the risk of delaying care outweighs the COVID-19 exposure risk, whereas others can be delayed without affecting the overall prognosis.
There are many considerations when counseling the surgical patient, but the reality is many of the procedures we routinely provide can be postponed for weeks and even months. Although we cannot postpone a large CPA tumor with obstructive hydrocephalus or a coalescent mastoiditis with extratemporal extension, we can certainly delay an adult cochlear implant or stapedectomy. The same wide spectrum that makes the subspecialty interesting, challenges us when prioritizing care, particularly when presented with months’ worth of surgical backlog, restricted OR availability, and limited hospital resources. Each practitioner, therefore, must juggle unique challenges. What may be a barrier to someone practicing in South Dakota, may not be problematic in California because of the loco-regional variability in case density and health care resources. Similar hurdles can be experienced by private practice colleagues that cannot access resources available to their academic counterparts in the same city. As a result, it would be inappropriate to provide detailed or blanket statements on how the practice has changed collectively, but change has occurred in some way for all. In addition to this, the peer-reviewed literature is nearly nonexistent as it relates to our subspecialty. With that in mind, the following discussion is largely based on exchanges with colleagues via professional forums and communications from national and international societies.
Discussion
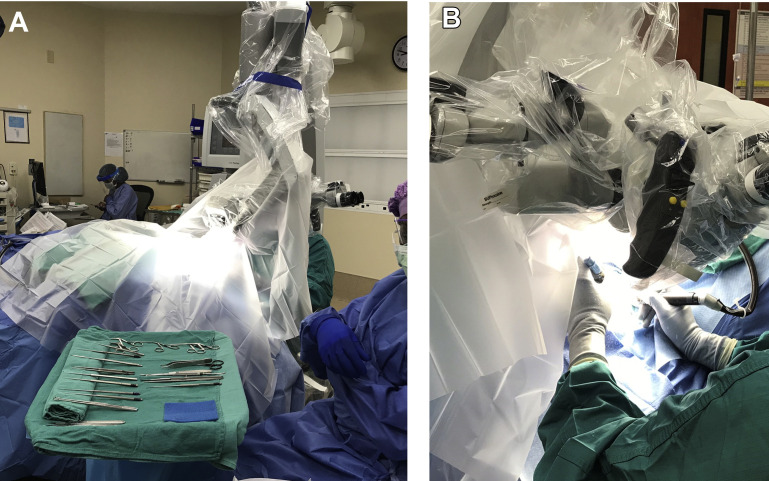
Early reports of heightened infection risk to health care workers from aerosolization of viral particles produced by high-speed drills, most notably during endonasal sinus or skull base surgery, raised the question of whether similar phenomenon was applicable to middle ear and mastoid surgery.3 Although there have been reports of corona viruses found in middle ear specimens, there have been no data specific to SARS-CoV-2 thus far.4 , 5 Given the lack of data for SARS-CoV-2, many opted for precaution and instituted alterations to the clinic and OR setup to minimize spread of aerosolized middle ear and mastoid contents. Examples of changes include the integration of filters into clinic suctions, improved ventilation in clinic rooms, and novel draping in the OR, such as the use of tentlike coverage over microscopes to capture or limit droplet splatter during mastoid drilling (Fig. 1 ). Special anesthesia protocols for intubation were procured and the use of intraoperative respirators implemented. N95 masks with or without face shields and eye protection became the most common PPE used. Other respirators were either in scarce availability or were too cumbersome to use under a microscope, most notably as experienced with controlled air-purifying respirators (CAPRs) and powered air-purifying respirators (PAPRs). Ultimately, the specifics of PPE are usually left up to the surgeon and surgical team, a decision influenced by the facility’s resources, surgeon’s preference, nature of surgical intervention, and the COVID status of the patient.6 In general, it is safe to say that although N95s have been used extensively, the role of CAPR and PAPR is limited for routine otologic and neurotologic procedures, but may be necessary on patients who are positive for COVID-19.
Fig. 1.
(A, B) Microscope drape limiting splatter during mastoid drilling.
Another change to standard operating procedures has been the implementation of preoperative COVID-19 testing for all patients undergoing surgery. The most common screening method is PCR testing from nasopharyngeal swab. The results help guide PPE requirements and also enable the surgeon to postpone procedures when possible for those found to be COVID-19 positive, a decision guided by published reports of poor perioperative prognosis in infected patients.7 , 8
Another change has been the implementation of face masks for all patient encounters. We have learned that consistent mask use, whether it be in the workplace or beyond, is critical in containing the spread of disease. This necessary practice has proven quite problematic by restricting ease of communication for patients who are hard of hearing because it eliminates the ability to lip read.9 Due to the large volume of hard-of-hearing and deaf patients in an otolaryngology practice, the use of face masks with transparent windows is optimal. Although this may be a necessity for the otolaryngology or audiology provider, it is unlikely to be implemented by the rest of the medical community, as it is difficult to procure such masks.
Finally, the use of telehealth underwent significant expansion during the pandemic, particularly when shelter-in-place orders went into effect. Some institutions have been more aggressive than others with implementing these services, and although it may not be a viable option for all otologic or neurotologic patients, it has proven beneficial in specific circumstances. Examples of good telehealth candidates include cochlear implant follow-ups, tinnitus or hyperacusis counseling, and vestibular patients, such as those with established Meniere disease and lack of middle ear pathology. Telehealth neurotologic consultations for management of CPA lesions, already implemented pre-COVID by several institutions, is another example of a suitable telehealth candidate.
Summary
The COVID-19 pandemic has required otologists and neurotologists to implement several changes into our practices. Due to the unforeseeable timeline in controlling the global pandemic, most of those changes are bound to be left in place for the foreseeable future. As more information on SARS-CoV-2 becomes available, we will need to continuously evaluate current practices to keep up with the changing face of this pandemic.
Acknowledgments
Disclosure
The author has nothing to disclose.
References
- 1.Hou Y.J., Okuda K., Edwards C.E. SARS-CoV-2 reverse genetics reveals a variable infection gradient in the respiratory tract. Cell. 2020;182(2):429–446.e14. doi: 10.1016/j.cell.2020.05.042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Zou L., Ruan F., Huang M. SARS-CoV-2 viral load in upper respiratory specimens of infected patients. N Engl J Med. 2020;382:1177–1179. doi: 10.1056/NEJMc2001737. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Patel Z.M., Fernandez-Miranda J., Hwang P.H. Letter: Precautions for endoscopic transnasal skull base surgery during the COVID-19 pandemic. Neurosurgery. 2020;87(1):E66–E67. doi: 10.1093/neuros/nyaa125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Pitkaranta A., Jero J., Arruda E. Polymerase chain reaction-based detection of rhinovirus, respiratory syncytial virus, and coronavirus in otitis media with effusion. J Pediatr. 1998;133:390–394. doi: 10.1016/S0022-3476(98)70276-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Pitkaranta A., Virolainen A., Jero J. Detection of rhinovirus, respiratory syncytial virus, and coronavirus infections in acute otitis media by reverse transcriptase polymerase chain reaction. Pediatrics. 1998;102:291–295. doi: 10.1542/peds.102.2.291. [DOI] [PubMed] [Google Scholar]
- 6.Howard B.E. High-risk aerosol-generating procedures in COVID-19: respiratory protective equipment considerations. Otolaryngol Head Neck Surg. 2020;163(1):98–103. doi: 10.1177/0194599820927335. [DOI] [PubMed] [Google Scholar]
- 7.Aminian A., Safari S., Razeghian-Jahromi A. COVID-19 outbreak and surgical practice: unexpected fatality in perioperative period. Ann Surg. 2020;272:e27–e29. doi: 10.1097/SLA.0000000000003925. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lei S., Jiang F., Su W. Clinical characteristics and outcomes of patients undergoing surgeries during the incubation period of COVID-19 infection. EClinicalMedicine. 2020;21:100331. doi: 10.1016/j.eclinm.2020.100331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Eby T.L., Arteaga A.A., Spankovich C. Otologic and Audiologic Considerations for COVID-19. Otolaryngol Head Neck Surg. 2020;163(1):110–111. doi: 10.1177/0194599820928989. [DOI] [PubMed] [Google Scholar]