This quasi-experimental cohort study uses data from the Danish population register of adult immigrants arriving from 1986 to 1998 and health outcomes from the inpatient clinic register, outpatient clinic register, and prescription drug register to assess the association between disadvantaged neighborhoods and cardiovascular disease risk among refugees.
Key Points
Question
Is there an association of neighborhood socioeconomic disadvantage with the development of cardiovascular risk factors, myocardial infarction, and stroke among refugees?
Findings
In this quasi-experimental cohort study, 49 305 refugees who were assigned to more disadvantaged neighborhoods across Denmark were at increased risk of developing hypertension, hyperlipidemia, diabetes, and myocardial infarction over subsequent decades. No associations were found for stroke.
Meaning
Neighborhood characteristics may be associated with long-term cardiovascular risk among refugees.
Abstract
Importance
Refugees are among the most disadvantaged individuals in society, and they often have elevated risks of cardiovascular risk factors and events. Evidence is limited regarding factors that may worsen cardiovascular health among this vulnerable group.
Objective
To test the hypothesis that refugee placement in socioeconomically disadvantaged neighborhoods is associated with increased cardiovascular risk.
Design, Setting, and Participants
The study population of this quasi-experimental, registry-based cohort study included 49 305 adults 18 years and older who came to Denmark as refugees from other countries during the years of Denmark’s refugee dispersal policy from 1986 to 1998. Refugees were dispersed to neighborhoods with varying degrees of socioeconomic disadvantage in an arbitrary manner conditional on observed characteristics. The association of neighborhood disadvantage on arrival with several cardiovascular outcomes in subsequent decades was evaluated using regression models that adjusted for individual, family, and municipal characteristics. Health outcomes were abstracted from the inpatient register, outpatient specialty clinic register, and prescription drug register through 2016. Data analysis was conducted from May 2018 to July 2019.
Exposures
A composite index of neighborhood disadvantage was constructed using 8 neighborhood-level socioeconomic characteristics derived from Danish population register data.
Main Outcomes and Measures
Primary study outcomes included hypertension, hyperlipidemia, type 2 diabetes, myocardial infarction, and stroke. Before data analysis commenced, it was hypothesized that higher levels of neighborhood disadvantage were associated with an increased risk of cardiovascular risk factors and events.
Results
A total of 49 305 participants were included (median [interquartile range] age, 30.5 [24.9-39.8] years; 43.3% women). Participant region of origin included 6318 from Africa (12.8%), 7253 from Asia (14.7%), 3446 from Eastern Europe (7.0%), 5416 from Iraq (11.0%), 6206 from Iran (12.6%), 5558 from Palestine (via Lebanon, Israel, Occupied Palestinian Territories; 11.3%), and 15 108 from Yugoslavia (30.6%). Adjusted models revealed an association between placement in disadvantaged neighborhoods and increased risk of hypertension (0.71 [95% CI, 0.30-1.13] percentage points per unit of disadvantage index; P < .01), hyperlipidemia (0.44 [95% CI, 0.06-0.83] percentage points; P = .01), diabetes (0.45 [95% CI, 0.09-0.81] percentage points; P = .01), and myocardial infarction (0.14 [95% CI, 0.03-0.25] percentage points; P = .01). No association was found for stroke. Individuals who arrived in Denmark before age 35 years had an increased risk of hyperlipidemia (1.16 [95% CI, 0.41-1.92] percentage points; P < .01), and there were no differences by sex.
Conclusions and Relevance
In this quasi-experimental cohort study, neighborhood disadvantage was associated with increased cardiovascular risk in a relatively young population of refugees. Neighborhood characteristics may be an important consideration when refugees are placed by resettlement agencies and host countries. Future work should examine additional health outcomes as well as potential mediating pathways to target future interventions (eg, neighborhood ease of walking, employment opportunities).
Introduction
Refugees are among the most vulnerable individuals in society, often surviving violence, war, and other trauma before relocating to an unfamiliar host country.1,2 Although some immigrants have better health than native-born citizens,3 refugees are uniquely at risk due to the often involuntary and sudden nature of their displacement and the adversity faced in their home countries.4,5 In many countries, population-level studies of refugee health are notoriously difficult to conduct due to data constraints. For example, the United States collects minimal data on refugees only during the 90 days after their arrival.6 Most literature is therefore limited to a few small cross-sectional studies of refugees from a single country or region or to the few refugees who happen to be interviewed in national surveys.5,7,8,9
A few studies have demonstrated that rates of cardiovascular disease (CVD) and related risk factors among some refugees are increased compared with those of native-born populations.10,11,12,13,14 In the general population, CVD is more common among individuals of lower socioeconomic status and is associated with chronic stress,15,16,17 making it a particularly relevant outcome among refugees.
Previous studies have investigated factors associated with health among refugees, although most focused on mental health as an outcome and on individual risk factors, such as sex or exposure to violence.18 Fewer studies focused on neighborhood factors,18 which theory suggests are key determinants of immigrant health.19 For example, socioeconomically disadvantaged neighborhoods often have limited walkability or availability of nutritious food, thereby affecting health behaviors associated with CVD.20,21,22 Alternatively, reduced employment opportunities or greater neighborhood crime rates may increase stress, which in turn is associated with increased CVD.23,24,25,26,27 Neighborhood socioeconomic characteristics may be particularly salient for refugees, who often have limited control over their placement and limited financial means.
This study took advantage of a unique natural experiment in which refugees to Denmark were assigned to neighborhoods with different levels of socioeconomic disadvantage.28 From 1986 to 1998, the Danish government dispersed tens of thousands of incoming refugees across the country in an arbitrary fashion, conditional on observed characteristics, to avoid overcrowding in major cities.27,28,29,30,31 We employed unique population-level data spanning 3 decades from Denmark’s population and health registers. We tested the hypothesis that neighborhood socioeconomic disadvantage is associated with increased risk of CVD risk factors, myocardial infarction, and stroke across the life course among resettled refugees.
Methods
Ethics Approval
This quasi-experimental, registry-based cohort study was approved by the Danish Data Protection Agency (record number 2015-57). Registry-based studies do not require ethical board approval in Denmark,32 and this study did not include any personally identifiable information on study participants. As a result, participant consent was not obtained.
Data
The cohort was created by linking several Danish national registers.33 Sociodemographic data were drawn from administrative registers of the total population (January 1, 1986, to December 31, 2016), whereas outcomes were ascertained from inpatient (January 1, 1986, to December 31, 2016), outpatient specialty clinic (January 1, 1994, to December 31, 2016), and prescription drug (January 1, 1995, to December 31, 2016) registers.34,35,36 Danish registers do not include diagnostic information on primary care encounters. The registers include 8.1 million individuals cumulatively during the study period. Data analysis was conducted from May 2018 to July 2019. This study followed the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) reporting guideline.
Study Population
The term immigrants refers to foreign-born individuals, whereas refugees are a unique subset of immigrants fleeing persecution and entitled to specific protections under international law. The study population included adult immigrants (18 years and older) arriving in Denmark from refugee-sending countries during the 1986 to 1998 period, which represents the years of the government dispersal policy (N = 49 305; eFigure 1 in the Supplement). We excluded individuals reuniting with family in Denmark, because they were not subject to the dispersal policy.
Danish Dispersal Policy
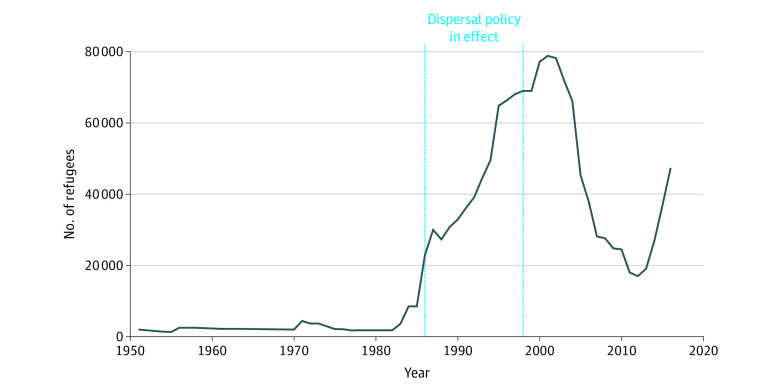
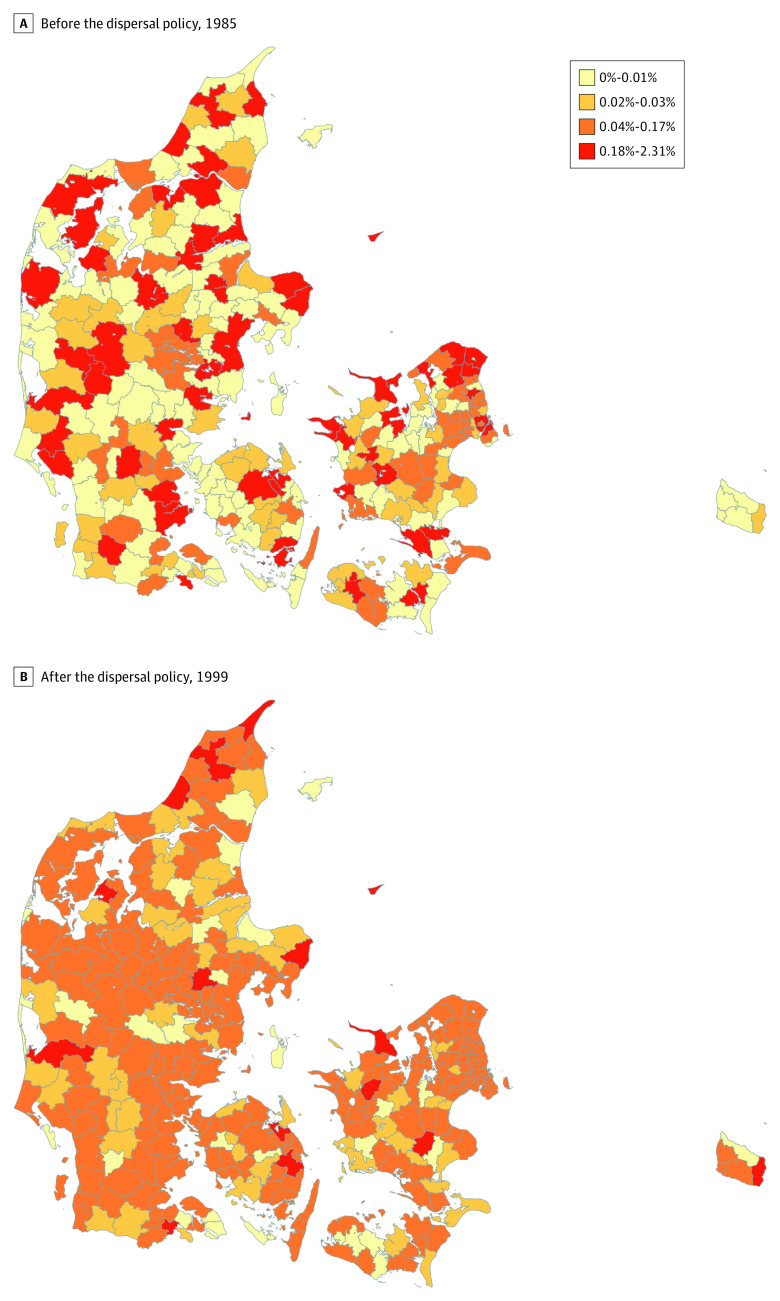
We leveraged a unique natural experiment in which incoming refugees were assigned to neighborhoods with varying levels of disadvantage throughout the country. Denmark implemented this refugee dispersal policy from 1986 to 1998.28 Because of the surge in arrivals to Denmark during this period (Figure 1), the policy’s goal was to ease labor market conditions in heavily settled areas and to promote better integration of refugees. As a result of the policy, refugees were spread more evenly across the country (Figure 2).
Figure 1. Refugees to Denmark by Year.
Source: Authors’ calculations using data from the United Nations High Commissioner for Refugees (http://popstats.unhcr.org).
Figure 2. Percentage of Immigrants From Countries Sending Refugees to Denmark by Municipality.
Percentage of immigrants shown in the year before (A) and the year after (B) the dispersal policy was in effect (1985 vs 1999).
Source: Authors’ calculations using data from Statistics Denmark.
Refugee placement officers only had knowledge of the following characteristics that were available on refugees’ applications: sex, birthdate, marital status, family size, and nationality.28 Officers otherwise had no direct interaction with families. Therefore, any possible confounding would have arisen only from observed characteristics in the refugees' applications, reducing the chances of confounding by unmeasured factors (ie, guaranteeing conditional exchangeability).37,38 Thus, initial neighborhood assignment within a municipality was arbitrary, conditional on these demographic characteristics. These characteristics are available in the register data, and we adjusted for them during data analysis. Studies have identified greater geographic dispersal of refugees during the policy period (as in Figure 2), no evidence of sorting by ethnic group, and covariate balance by neighborhood type.27,28,29,30 It is therefore unlikely that unobserved factors influenced neighborhood assignment. As a result, this study attempts to address the challenges of selective migration present in existing studies on neighborhood outcomes.
Although register data do not include information on the neighborhood to which refugees were assigned, official reports document that more than 90% of incoming refugees agreed to placement in their assigned municipality, indicating strong adherence to the placement program.28 Those who refused placement were responsible for finding their own place of residence, which may have resulted in some residual bias in our estimates. Nevertheless, this represents a high level of compliance relative to the only prior relevant assignment study to our knowledge, the US Moving to Opportunity experiment, in which only half of participants adhered to their assignment.39 As refugees reuniting with family were not subject to the dispersal policy, we excluded these individuals using family structure information available in the registers. For the remaining refugees, we assumed that the observed neighborhood of residence on arrival was the neighborhood to which refugees were assigned. For those who moved within 1 year of arrival, we assumed that the first place of residence was temporary housing—similar to prior work based on how the policy was implemented28,29—and instead used the second place of residence as the assigned neighborhood.
After assignment to an initial residence, the government offered language and training courses and social welfare support lasting approximately 18 months. There were no relocation restrictions if a family later decided to move, and receipt of welfare was not conditional on remaining in the assigned residence. Therefore, our study design is akin to a randomized encouragement design in which participants are randomly encouraged to be exposed to a given neighborhood.40 The approach provides a lower bound on the health outcomes associated with neighborhood disadvantage. The design is similar to that used for the Moving to Opportunity experiment.39 Later relocations represent mediating pathways through which disadvantage in the initially assigned neighborhood may be associated with later cardiovascular health.
Variables
Exposure
For each individual, the primary exposure was a measure of socioeconomic disadvantage in the initial neighborhood assigned on arrival to Denmark. We created a composite disadvantage index for each neighborhood by year, using principal component analysis to combine 8 neighborhood-level sociodemographic variables examined in prior research that represent different theoretical constructs capturing disadvantage: median income, family poverty, income inequality, unemployment rate, crime rate, foreign-born, welfare participation, and education.41,42 Additional details are available in the eAppendix and eTables 1 and 2 in the Supplement.
Small geographic units were used to define neighborhoods, as these align better than larger areas with residents’ definitions of neighborhoods.43 Using larger areas can also mask neighborhood effects.44 The Danish census bureau has geocoded all individuals to historically meaningful neighborhoods known as parishes. Parishes are nested within the larger geographic unit of municipality and each contain a mean of approximately 2000 individuals. During the study period, there were 2159 parishes nested within 271 municipalities, and they have been used previously to define neighborhoods.45,46
Outcomes
We examined hypertension, hyperlipidemia, type 2 diabetes, myocardial infarction (MI), and stroke, which represent 3 CVD risk factors and 2 clinical end points that have been plausibly linked to neighborhood disadvantage previously.47,48,49,50,51,52,53,54 For MI and stroke, individuals were considered to have these diagnoses if they were assigned relevant International Classification of Diseases, Eighth Revision (ICD-8) and International Statistical Classification of Diseases and Related Health Problems, Tenth Revision (ICD-10) codes, based on physician discharge diagnoses in inpatient settings. For hypertension, hyperlipidemia, and diabetes, we used ICD-8 and ICD-10 codes from outpatient specialty clinics and inpatient settings, as well as Anatomic Therapeutic Chemical medication codes from prescriptions of relevant medications (eg, statins for hyperlipidemia). To capture incident rather than prevalent cases, we excluded diagnoses within 2 years after arriving in Denmark.55,56 We also extracted the date on which diagnoses were first identified, which we used in Cox models.
Covariates
We adjusted for the characteristics available to placement officers who implemented the dispersal policy: sex, age and age-squared, marital status, family size, and region of origin. We included indicator variables for year of arrival to adjust for secular trends. Finally, we included indicator variables (ie, fixed effects) for municipality, which accounted for all time-invariant characteristics of municipalities. This allowed us to estimate associations with neighborhood disadvantage based on the difference in outcomes for refugees placed in the same municipality who were assigned to a high- vs low-disadvantage neighborhood.
Statistical Analysis
Primary Analysis
We first examined characteristics of individuals in the study population, splitting the neighborhood disadvantage index at the median (for the purposes of this descriptive analysis only) and comparing individuals assigned to high- vs low-disadvantage neighborhoods. We also compared the prevalence of each outcome among the refugee population with the prevalence among an age- and sex-matched population of native-born Danes.
Next, we regressed each outcome on the continuous measure of neighborhood disadvantage. In primary analyses, these were linear regressions, and we confirmed a linear association between the disadvantage index and each outcome through a graphical spline analysis. The models were first unadjusted and then adjusted for the covariates listed previously. All tests were 2-sided, and P < .05 was considered statistically significant; 95% CIs indicated precision of effect estimates. Robust SEs were clustered by municipality to account for correlated observations.
Secondary Analyses
Linear models do not consider the date of diagnosis and therefore do not capture the time to event, which may be important for these outcomes. To account for this possible bias, we next used Cox models to estimate the association of neighborhood disadvantage with time-to-diagnosis for each outcome. These models were first unadjusted and then adjusted for the covariates mentioned previously. They incorporated shared frailty at the municipality level to account for correlated observations. See the eAppendix in the Supplement for additional details.
Finally, we assessed whether associations differed by sex and by age on arrival, as men and women may experience neighborhood disadvantage differently, and individuals exposed at younger ages experience longer exposure to a neighborhood after arrival.57 We carried out an analysis in which we included an interaction term between neighborhood disadvantage and sex and another with an interaction term between neighborhood disadvantage and age younger than 35 years on arrival.
Results
Cohort Characteristics
A total of 49 305 participants were analyzed (median [interquartile range] age, 30.5 [24.9-39.8] years; 43.3% women) (Table). More than half (28 629 [58.1%]) were married, and approximately one-fifth had completed secondary education (14.4%) or more (5.8%). Participant region of origin included 6318 from Africa (12.8%), 7253 from Asia (14.7%), 3446 from Eastern Europe (7.0%), 5416 from Iraq (11.0%), 6206 from Iran (12.6%), 5558 from Palestine (via Lebanon, Israel, Occupied Palestinian Territories; 11.3%), and 15 108 from Yugoslavia (30.6%). Characteristics were roughly balanced across high- and low-disadvantage neighborhoods, except for the characteristics that were available to placement officers and may have influenced neighborhood assignment (eg, region of origin) and those correlated with such characteristics (eg, educational attainment). The median follow-up time was 16.0 (interquartile range, 3.7-20.3) years.
Table. Sociodemographic characteristics of Refugees Arriving in Denmark During 1986-1998, by Neighborhood Disadvantage Level on Arrival.
| Characteristica | Low-disadvantage neighborhood (n = 24 656) | High-disadvantage neighborhood (n = 24 649) | Total (N = 49 305) | |||
|---|---|---|---|---|---|---|
| % | Median (IQR) | % | Median (IQR) | % | Median (IQR) | |
| Women | 42.3 | NA | 44.3 | NA | 43.3 | NA |
| Age, y | NA | 29.9 (24.6-38.8) | NA | 31.3 (25.2-40.7) | NA | 30.5 (24.9-39.8) |
| Married | 54.9 | NA | 61.2 | NA | 58.1 | NA |
| Educational level | ||||||
| No education | 26.8 | 24.8 | 25.8 | |||
| Primary education | 51.5 | 56.4 | 53.9 | |||
| Secondary education | 15.2 | 13.6 | 14.4 | |||
| Higher education | 6.4 | 5.2 | 5.8 | |||
| Family size, No. of people | NA | 2 (1-3) | NA | 2 (1-4) | NA | 2 (1-4) |
| Region of origin | ||||||
| Africa | 13.9 | NA | 11.7 | NA | 12.8 | NA |
| Asia | 12.8 | 16.6 | 14.7 | |||
| Eastern Europe | 8.5 | 5.5 | 7.0 | |||
| Iraq | 13.9 | 8.1 | 11.0 | |||
| Iran | 15.0 | 10.2 | 12.6 | |||
| Palestineb | 13.7 | 8.8 | 11.3 | |||
| Yugoslavia | 22.1 | 39.2 | 30.6 | |||
| Follow-up, y | NA | 14.5 (3.3-21.1) | NA | 17.1 (4.1-20.1) | NA | 16.0 (3.7-20.3) |
| Health outcomes | ||||||
| Hypertension | 36.5 | NA | 37.8 | NA | 37.2 | NA |
| Hyperlipidemia | 23.3 | 27.1 | 25.2 | |||
| Diabetes | 15.6 | 16.4 | 16.0 | |||
| Myocardial infarction | 3.2 | 3.4 | 3.3 | |||
| Stroke | 2.7 | 2.8 | 2.8 | |||
Abbreviations: IQR, indicates interquartile range; NA, not applicable.
Study population includes all adult immigrants (aged 18 years and older) who arrived in Denmark from countries sending refugees during the period 1986-1998. Diagnoses were extracted from register data using medication and physician diagnosis codes. A composite index of socioeconomic disadvantage was created for each neighborhood by year, using principal component analysis to combine 8 neighborhood-level sociodemographic variables (eTable 1 in the Supplement). For the purposes of producing these descriptive characteristics only, the neighborhood disadvantage index was split at the median to compare refugees assigned to low- vs high-disadvantage neighborhoods.
The designation Palestine includes individuals arriving from Lebanon, Israel, or the Occupied Palestinian Territories.
During the follow-up period, 37.2% of refugees were diagnosed with hypertension, 25.2% with hyperlipidemia, 16.0% with diabetes, 3.3% with MI, and 2.8% with stroke. Rates of all conditions except stroke were higher among the refugee population compared with a population of native-born Danes matched by age and sex (hypertension, 37.2% vs 35.3%; hyperlipidemia, 25.2% vs 18.7%; diabetes, 16.0% vs 7.1%; MI, 3.3% vs 2.7%; stroke 2.8% vs 3.6%) (eTable 3 in the Supplement).
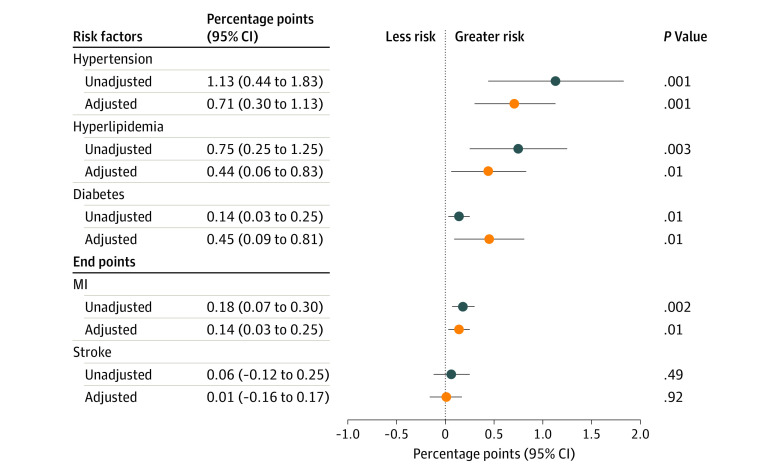
Association of Neighborhood Disadvantage With Cardiovascular Risk Factors and Events
In unadjusted models (Figure 3), greater neighborhood disadvantage was associated with a greater risk of hypertension (1.13 [95% CI, 0.44-1.83] percentage points per unit of deprivation index; P = .001), hyperlipidemia (0.75 [95% CI, 0.25-1.25] percentage points; P = .003), diabetes (0.14 [95% CI, 0.03-0.25] percentage points; P = .01), and MI (0.18 [95% CI, 0.07-0.30] percentage points; P = .002) but had no association with stroke.
Figure 3. Association of Neighborhood Disadvantage With Cardiovascular Outcomes, N = 49 305.
The study population includes all adult immigrants (aged 18 years and older) who arrived in Denmark from countries sending refugees from 1986 to 1998. Diagnoses were extracted from register data using medication and physician diagnosis codes. A continuous variable representing a composite index of socioeconomic disadvantage was created for each neighborhood by year using principal component analysis to combine 8 neighborhood-level sociodemographic variables (eTable 1 in the Supplement). Analyses involved multivariable linear regressions, with covariates including family size, sex, marital status, region of origin, year of arrival, and fixed effects for municipality. Coefficients represent the change in risk (in percentage points) per unit of the disadvantage index, with 95% CIs in parentheses for both risk factors and end points. MI indicates myocardial infarction.
In adjusted models, greater neighborhood disadvantage was associated with increased risk of hypertension (0.71 [95% CI, 0.30-1.13] percentage points; P < .01), hyperlipidemia (0.44 [95% CI, 0.06-0.83] percentage points; P = .01), diabetes (0.45 [95% CI, 0.09-0.81] percentage points; P = .01), and MI (0.14 [95% CI, 0.03-0.25] percentage points; P = .01), but not with stroke.
In Cox models, greater neighborhood disadvantage was associated with increased risk of diabetes (adjusted hazard ratio, 1.03; 95% CI, 1.01-1.06; P = .04) (eFigure 2 in the Supplement). However, we were unable to rule out the null hypothesis of no association for other outcomes.
Subgroup Analyses
Differences in the association between neighborhood disadvantage and each outcome were similar for men and women (eTable 4 in the Supplement). Increased neighborhood disadvantage was associated with a greater likelihood of hyperlipidemia among refugees who arrived before age 35 years compared with those who arrived at older ages (1.16 [95% CI, 0.41-1.92] percentage points; P < .01) (eTable 4 in the Supplement). For other outcomes, there were no differences in the association of neighborhood disadvantage among those who arrived in Denmark at younger or older ages.
Discussion
This quasi-experimental cohort study leveraged a unique natural experiment and rich Danish register data to provide among the first rigorous estimates of the association of neighborhood disadvantage with cardiovascular risk factors, MI, and stroke among refugees. Study results suggest that refugees who were assigned to more disadvantaged neighborhoods were more likely to develop hypertension, hyperlipidemia, diabetes, and MI in subsequent decades. Effect sizes were small, representing a 2% increase from baseline rates for each condition; although not necessarily clinically meaningful, these rates signify more meaningful outcomes when considering changes in distribution at a population level.58 We found no association of neighborhood disadvantage with risk of stroke, although results suggest that younger individuals were more likely than older individuals to develop hyperlipidemia in association with living in a more disadvantaged neighborhood.
Our findings are consistent with prior evidence from numerous observational studies that suggest that neighborhood characteristics are associated with CVD and its risk factors.47,48,49,50,51,59,60,61,62,63 Although many previous studies were limited by potential reverse association or confounding due to possible selection of unhealthy individuals (ie, those with higher CVD risk at baseline) into more disadvantaged neighborhoods, our use of a natural experiment reduced these sources of bias. One prior study that took advantage of a similar natural experiment in Sweden found that assignment to a more disadvantaged neighborhood was associated with higher rates of diabetes among refugees in later decades of life.53 This finding strengthens the argument that neighborhood socioeconomic circumstances matter for CVD risk.
Numerous mechanisms may underlie our findings. For example, disadvantaged neighborhoods may constrain employment and economic opportunities, thereby reducing income and the ability to purchase nutritious food.61 In addition, more disadvantaged neighborhoods often have more restricted food environments and walkability, thereby affecting health behaviors related to CVD.20,21,22 These neighborhoods also may have poorer access to primary care and other health care resources, resulting in lower-quality prevention and treatment of health conditions. Notably, health care access in Denmark is more equitably available nationwide relative to the United States.64,65,66 In addition, reduced income and greater neighborhood crime may increase chronic stress levels, which have been associated with increased rates of CVD.23,24,25,26 However, 1 prior study found that neighborhood disadvantage was not associated with refugee mental health in the context of a similar refugee dispersal policy in Sweden.67
Our results also suggest that, for hyperlipidemia, these pathways are more salient for refugees who arrive at younger ages. This is consistent with the literature on sensitive periods earlier in life that might constitute windows in which social exposures are particularly important.57,68 Future studies are needed to identify additional individual- and neighborhood-level characteristics that may place individuals at greater risk.
Previous work also has demonstrated that neighborhood disadvantage is associated with an increased risk of stroke,48,69,70,71 which we did not confirm in this study. Although it is possible that prior studies suffered from confounding and that there is, in fact, no effect of neighborhood disadvantage on this outcome, our study population may have been too young and this outcome too uncommon to replicate previous findings.
Limitations
Our study has several limitations. First, the study population included only refugees to Denmark, so the results may not generalize to refugees in other settings or to nonrefugees. Also, our study is unique due to the presence of the dispersal policy that created a natural experiment, and the outcomes of neighborhood disadvantage may differ when individuals self-select their place of residence. In addition, the dispersal policy that we examined was implemented during the 1986 to 1998 period, and the role of neighborhood disadvantage may differ based on other contemporaneous factors, such as economic conditions. Future studies should seek to identify more recent natural experiments. Additionally, the Danish register data include information on neighborhood of residence rather than neighborhood assigned. Although official reports document adherence of over 90% to the dispersal policy, there may nevertheless be some bias in resulting estimates. One limitation of Cox models is possible differential left-truncation bias, as various registers were established at different times. If differences in start date are associated with levels of neighborhood disadvantage and dates of diagnosis, Cox models could be biased. Finally, our study does not elucidate the specific socioeconomic aspects of neighborhoods that may underlie our findings, because we used a composite measure of neighborhood disadvantage. Future studies could examine how different aspects of neighborhoods—eg, unemployment, crime, walkability—may interact in order to develop targeted community interventions.
Conclusions
Given the surge in refugee migration to high-income countries in recent years,72 evidence is needed to inform governmental policies to optimize the economic and health trajectories of this vulnerable group. Such evidence can inform the development of tools to guide placement of refugees by host countries. Available tools currently do not include neighborhood-level characteristics.73
The findings of this quasi-experimental, registry-based cohort study suggest that neighborhoods where refugees are placed may have an association with risk of several CVD outcomes. Future studies should examine whether results are stronger after additional years of follow-up and aging of the cohort and should include additional outcomes. Additional studies could assess whether other subgroups (eg, those defined by region of origin or psychological resiliency) are particularly susceptible to neighborhood circumstances.
eAppendix. Supplemental Methods
eFigure 1. Study Flowchart
eFigure 2. Effect of Neighborhood Disadvantage on Cardiovascular Outcomes, Cox Models
eFigure 3. Effect of Neighborhood Disadvantage on Cardiovascular Outcomes, Using Alternative Neighborhood Deprivation Index
eTable 1. Characteristics Included in Neighborhood Disadvantage Index
eTable 2. Principal Component Analysis: Eigenvalues and Proportion of Variance Explained
eTable 3. Prevalence of Outcomes in Refugee Population Compared With Population of Native-Born Danes Matched on Age and Sex
eTable 4. Effect of Neighborhood Disadvantage on Cardiovascular Outcomes, by Sex and Age of Arrival in Denmark
eReferences
References
- 1.Sangalang CC, Vang C. Intergenerational trauma in refugee families: a systematic review. J Immigr Minor Health. 2017;19(3):745-754. doi: 10.1007/s10903-016-0499-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Shishehgar S, Gholizadeh L, DiGiacomo M, Green A, Davidson PM. Health and socio-cultural experiences of refugee women: an integrative review. J Immigr Minor Health. 2017;19(4):959-973. doi: 10.1007/s10903-016-0379-1 [DOI] [PubMed] [Google Scholar]
- 3.Markides KS, Rote S. Immigrant health paradox In: Scott RA, Kosslyn SM, eds. Emerging Trends in the Social and Behavioral Sciences. John Wiley & Sons; 2015. doi: 10.1002/9781118900772.etrds0174 [DOI] [Google Scholar]
- 4.Inhorn MC, Serour GI. Islam, medicine, and Arab-Muslim refugee health in America after 9/11. Lancet. 2011;378(9794):935-943. doi: 10.1016/S0140-6736(11)61041-6 [DOI] [PubMed] [Google Scholar]
- 5.Connor P. Explaining the refugee gap: economic outcomes of refugees versus other immigrants. J Refug Stud. 2010;23(3):377-397. doi: 10.1093/jrs/feq025 [DOI] [Google Scholar]
- 6.Sikorski N. Understanding the Algorithm Meant to Help Refugees Get Jobs Fast. News Deeply; 2018. [Google Scholar]
- 7.Ellis BH, MacDonald HZ, Lincoln AK, Cabral HJ. Mental health of Somali adolescent refugees: the role of trauma, stress, and perceived discrimination. J Consult Clin Psychol. 2008;76(2):184-193. doi: 10.1037/0022-006X.76.2.184 [DOI] [PubMed] [Google Scholar]
- 8.Fox PG, Cowell JM, Montgomery AC. Southeast Asian refugee children: violence experience and depression. Int J Psychiatr Nurs Res. 1999;5(2):589-600. [PubMed] [Google Scholar]
- 9.Geltman PL, Grant-Knight W, Mehta SD, et al. The “lost boys of Sudan”: functional and behavioral health of unaccompanied refugee minors re-settled in the United States. Arch Pediatr Adolesc Med. 2005;159(6):585-591. doi: 10.1001/archpedi.159.6.585 [DOI] [PubMed] [Google Scholar]
- 10.Marshall GN, Schell TL, Wong EC, et al. Diabetes and cardiovascular disease risk in Cambodian refugees. J Immigr Minor Health. 2016;18(1):110-117. doi: 10.1007/s10903-014-0142-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Barnes DM, Harrison C, Heneghan R. Health risk and promotion behaviors in refugee populations. J Health Care Poor Underserved. 2004;15(3):347-356. doi: 10.1353/hpu.2004.0034 [DOI] [PubMed] [Google Scholar]
- 12.Kinzie JD, Riley C, McFarland B, et al. High prevalence rates of diabetes and hypertension among refugee psychiatric patients. J Nerv Ment Dis. 2008;196(2):108-112. doi: 10.1097/NMD.0b013e318162aa51 [DOI] [PubMed] [Google Scholar]
- 13.DesMeules M, Gold J, McDermott S, et al. Disparities in mortality patterns among Canadian immigrants and refugees, 1980-1998: results of a national cohort study. J Immigr Health. 2005;7(4):221-232. doi: 10.1007/s10903-005-5118-y [DOI] [PubMed] [Google Scholar]
- 14.Bo A, Zinckernagel L, Krasnik A, Petersen JH, Norredam M. Coronary heart disease incidence among non-Western immigrants compared to Danish-born people: effect of country of birth, migrant status, and income. Eur J Prev Cardiol. 2015;22(10):1281-1289. doi: 10.1177/2047487314551538 [DOI] [PubMed] [Google Scholar]
- 15.Dimsdale JE. Psychological stress and cardiovascular disease. J Am Coll Cardiol. 2008;51(13):1237-1246. doi: 10.1016/j.jacc.2007.12.024 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Clark AM, DesMeules M, Luo W, Duncan AS, Wielgosz A. Socioeconomic status and cardiovascular disease: risks and implications for care. Nat Rev Cardiol. 2009;6(11):712-722. doi: 10.1038/nrcardio.2009.163 [DOI] [PubMed] [Google Scholar]
- 17.Hamad R, Penko J, Kazi DS, et al. Association of low socioeconomic status with premature coronary heart disease in US adults. JAMA Cardiol. Published online May 27, 2020. doi: 10.1001/jamacardio.2020.1458 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Fazel M, Reed RV, Panter-Brick C, Stein A. Mental health of displaced and refugee children resettled in high-income countries: risk and protective factors. Lancet. 2012;379(9812):266-282. doi: 10.1016/S0140-6736(11)60051-2 [DOI] [PubMed] [Google Scholar]
- 19.Edberg M, Cleary S, Vyas A. A trajectory model for understanding and assessing health disparities in immigrant/refugee communities. J Immigr Minor Health. 2011;13(3):576-584. doi: 10.1007/s10903-010-9337-5 [DOI] [PubMed] [Google Scholar]
- 20.Rundle A, Neckerman KM, Freeman L, et al. Neighborhood food environment and walkability predict obesity in New York City. Environ Health Perspect. 2009;117(3):442-447. doi: 10.1289/ehp.11590 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Sundquist K, Eriksson U, Kawakami N, Skog L, Ohlsson H, Arvidsson D. Neighborhood walkability, physical activity, and walking behavior: the Swedish Neighborhood and Physical Activity (SNAP) study. Soc Sci Med. 2011;72(8):1266-1273. doi: 10.1016/j.socscimed.2011.03.004 [DOI] [PubMed] [Google Scholar]
- 22.Sundquist K, Eriksson U, Mezuk B, Ohlsson H. Neighborhood walkability, deprivation and incidence of type 2 diabetes: a population-based study on 512,061 Swedish adults. Health Place. 2015;31:24-30. doi: 10.1016/j.healthplace.2014.10.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Boardman JD, Finch BK, Ellison CG, Williams DR, Jackson JS. Neighborhood disadvantage, stress, and drug use among adults. J Health Soc Behav. 2001;42(2):151-165. doi: 10.2307/3090175 [DOI] [PubMed] [Google Scholar]
- 24.Giurgescu C, Misra DP, Sealy-Jefferson S, et al. The impact of neighborhood quality, perceived stress, and social support on depressive symptoms during pregnancy in African American women. Soc Sci Med. 2015;130(0):172-180. doi: 10.1016/j.socscimed.2015.02.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Hill TD, Angel RJ. Neighborhood disorder, psychological distress, and heavy drinking. Soc Sci Med. 2005;61(5):965-975. doi: 10.1016/j.socscimed.2004.12.027 [DOI] [PubMed] [Google Scholar]
- 26.Kasarda JD. Inner-city concentrated poverty and neighborhood distress: 1970 to 1990. Hous Policy Debate. 1993;4(3):253-302. doi: 10.1080/10511482.1993.9521135 [DOI] [Google Scholar]
- 27.Damm AP, Dustmann C. Does growing up in a high crime neighborhood affect youth criminal behavior? Am Econ Rev. 2014;104(6):1806-1832. doi: 10.1257/aer.104.6.1806 [DOI] [Google Scholar]
- 28.Damm AP. The Danish Dispersal Policy on Refugee Immigrants 1986-1998: A Natural Experiment? Aarhus School of Business, Department of Economics; 2005. [Google Scholar]
- 29.Damm AP. Determinants of recent immigrants’ location choices: quasi-experimental evidence. J Popul Econ. 2009;22(1):145-174. doi: 10.1007/s00148-007-0148-5 [DOI] [Google Scholar]
- 30.Damm AP. Ethnic enclaves and immigrant labor market outcomes: quasi-experimental evidence. J Labor Econ. 2009;27(2):281-314. doi: 10.1086/599336 [DOI] [Google Scholar]
- 31.Damm AP, Rosholm M. Employment effects of spatial dispersal of refugees. Rev Econ Househ. 2010;8(1):105-146. doi: 10.1007/s11150-009-9067-4 [DOI] [Google Scholar]
- 32.Ludvigsson JF, Håberg SE, Knudsen GP, et al. Ethical aspects of registry-based research in the Nordic countries. Clin Epidemiol. 2015;7:491-508. doi: 10.2147/CLEP.S90589 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Schmidt M, Schmidt SAJ, Adelborg K, et al. The Danish health care system and epidemiological research: from health care contacts to database records. Clin Epidemiol. 2019;11:563-591. doi: 10.2147/CLEP.S179083 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Pottegård A, Schmidt SAJ, Wallach-Kildemoes H, Sørensen HT, Hallas J, Schmidt M. Data resource profile: the Danish national prescription registry. Int J Epidemiol. 2017;46(3):798-798f. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Schmidt M, Schmidt SAJ, Sandegaard JL, Ehrenstein V, Pedersen L, Sørensen HT. The Danish National Patient Registry: a review of content, data quality, and research potential. Clin Epidemiol. 2015;7:449-490. doi: 10.2147/CLEP.S91125 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Thygesen LC, Ersbøll AK. Danish population-based registers for public health and health-related welfare research: introduction to the supplement. Scand J Public Health. 2011;39(7 suppl):8-10. doi: 10.1177/1403494811409654 [DOI] [PubMed] [Google Scholar]
- 37.Hernán MA, Hernández-Díaz S, Robins JM. A structural approach to selection bias. Epidemiology. 2004;15(5):615-625. doi: 10.1097/01.ede.0000135174.63482.43 [DOI] [PubMed] [Google Scholar]
- 38.Greenland S, Robins JM. Identifiability, exchangeability and confounding revisited. Epidemiol Perspect Innov. 2009;6(1):4. doi: 10.1186/1742-5573-6-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Ludwig J, Duncan GJ, Gennetian LA, et al. Long-term neighborhood effects on low-income families: evidence from Moving to Opportunity. Am Econ Rev. 2013;103(3):226-231. doi: 10.1257/aer.103.3.226 [DOI] [Google Scholar]
- 40.Hirano K, Imbens GW, Rubin DB, Zhou X-H. Assessing the effect of an influenza vaccine in an encouragement design. Biostatistics. 2000;1(1):69-88. doi: 10.1093/biostatistics/1.1.69 [DOI] [PubMed] [Google Scholar]
- 41.Messer LC, Laraia BA, Kaufman JS, et al. The development of a standardized neighborhood deprivation index. J Urban Health. 2006;83(6):1041-1062. doi: 10.1007/s11524-006-9094-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Havard S, Deguen S, Bodin J, Louis K, Laurent O, Bard D. A small-area index of socioeconomic deprivation to capture health inequalities in France. Soc Sci Med. 2008;67(12):2007-2016. doi: 10.1016/j.socscimed.2008.09.031 [DOI] [PubMed] [Google Scholar]
- 43.Huie SAB. The concept of neighborhood in health and mortality research. Sociol Spectr. 2001;21(3):341-358. doi: 10.1080/027321701300202028 [DOI] [Google Scholar]
- 44.Meijer M, Röhl J, Bloomfield K, Grittner U. Do neighborhoods affect individual mortality? a systematic review and meta-analysis of multilevel studies. Soc Sci Med. 2012;74(8):1204-1212. doi: 10.1016/j.socscimed.2011.11.034 [DOI] [PubMed] [Google Scholar]
- 45.Meijer M, Engholm G, Grittner U, Bloomfield K. A socioeconomic deprivation index for small areas in Denmark. Scand J Public Health. 2013;41(6):560-569. doi: 10.1177/1403494813483937 [DOI] [PubMed] [Google Scholar]
- 46.Meijer M, Kejs AM, Stock C, Bloomfield K, Ejstrud B, Schlattmann P. Population density, socioeconomic environment and all-cause mortality: a multilevel survival analysis of 2.7 million individuals in Denmark. Health Place. 2012;18(2):391-399. doi: 10.1016/j.healthplace.2011.12.001 [DOI] [PubMed] [Google Scholar]
- 47.Buys DR, Howard VJ, McClure LA, et al. Association between neighborhood disadvantage and hypertension prevalence, awareness, treatment, and control in older adults: results from the University of Alabama at Birmingham Study of Aging. Am J Public Health. 2015;105(6):1181-1188. doi: 10.2105/AJPH.2014.302048 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Carlsson AC, Li X, Holzmann MJ, et al. Neighborhood socioeconomic status at the age of 40 years and ischemic stroke before the age of 50 years: a nationwide cohort study from Sweden. Int J Stroke. 2017;12(8):815-826. doi: 10.1177/1747493017702663 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Cubbin C, Sundquist K, Ahlén H, Johansson S-E, Winkleby MA, Sundquist J. Neighborhood deprivation and cardiovascular disease risk factors: protective and harmful effects. Scand J Public Health. 2006;34(3):228-237. doi: 10.1080/14034940500327935 [DOI] [PubMed] [Google Scholar]
- 50.Halonen JI, Stenholm S, Pentti J, et al. Childhood psychosocial adversity and adult neighborhood disadvantage as predictors of cardiovascular disease: a cohort study. Circulation. 2015;132(5):371-379. doi: 10.1161/CIRCULATIONAHA.115.015392 [DOI] [PubMed] [Google Scholar]
- 51.Kaiser P, Diez Roux AV, Mujahid M, et al. Neighborhood environments and incident hypertension in the multi-ethnic study of atherosclerosis. Am J Epidemiol. 2016;183(11):988-997. doi: 10.1093/aje/kwv296 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Kershaw KN, Diez Roux AV, Burgard SA, Lisabeth LD, Mujahid MS, Schulz AJ. Metropolitan-level racial residential segregation and black-white disparities in hypertension. Am J Epidemiol. 2011;174(5):537-545. doi: 10.1093/aje/kwr116 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.White JS, Hamad R, Li X, et al. Long-term effects of neighbourhood deprivation on diabetes risk: quasi-experimental evidence from a refugee dispersal policy in Sweden. Lancet Diabetes Endocrinol. 2016;4(6):517-524. doi: 10.1016/S2213-8587(16)30009-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Kershaw KN, Osypuk TL, Do DP, De Chavez PJ, Diez Roux AV. Neighborhood-level racial/ethnic residential segregation and incident cardiovascular disease: the multi-ethnic study of atherosclerosis. Circulation. 2015;131(2):141-148. doi: 10.1161/CIRCULATIONAHA.114.011345 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Hamad R, Modrek S, Kubo J, Goldstein BA, Cullen MR. Using “big data” to capture overall health status: properties and predictive value of a claims-based health risk score. PLoS One. 2015;10(5):e0126054. doi: 10.1371/journal.pone.0126054 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Scherrer JF, Virgo KS, Zeringue A, et al. Depression increases risk of incident myocardial infarction among Veterans Administration patients with rheumatoid arthritis. Gen Hosp Psychiatry. 2009;31(4):353-359. doi: 10.1016/j.genhosppsych.2009.04.001 [DOI] [PubMed] [Google Scholar]
- 57.Chetty R, Hendren N, Katz LF. The effects of exposure to better neighborhoods on children: new evidence from the moving to opportunity experiment. Am Econ Rev. 2016;106(4):855-902. doi: 10.1257/aer.20150572 [DOI] [PubMed] [Google Scholar]
- 58.Guyatt GH, Osoba D, Wu AW, Wyrwich KW, Norman GR; Clinical Significance Consensus Meeting Group . Methods to explain the clinical significance of health status measures. Mayo Clin Proc. 2002;77(4):371-383. doi: 10.4065/77.4.371 [DOI] [PubMed] [Google Scholar]
- 59.Diez Roux AV, Merkin SS, Arnett D, et al. Neighborhood of residence and incidence of coronary heart disease. N Engl J Med. 2001;345(2):99-106. doi: 10.1056/NEJM200107123450205 [DOI] [PubMed] [Google Scholar]
- 60.Diez-Roux AV, Nieto FJ, Muntaner C, et al. Neighborhood environments and coronary heart disease: a multilevel analysis. Am J Epidemiol. 1997;146(1):48-63. doi: 10.1093/oxfordjournals.aje.a009191 [DOI] [PubMed] [Google Scholar]
- 61.Sundquist K, Theobald H, Yang M, Li X, Johansson S-E, Sundquist J. Neighborhood violent crime and unemployment increase the risk of coronary heart disease: a multilevel study in an urban setting. Soc Sci Med. 2006;62(8):2061-2071. doi: 10.1016/j.socscimed.2005.08.051 [DOI] [PubMed] [Google Scholar]
- 62.Sundquist K, Winkleby M, Ahlén H, Johansson S-E. Neighborhood socioeconomic environment and incidence of coronary heart disease: a follow-up study of 25,319 women and men in Sweden. Am J Epidemiol. 2004;159(7):655-662. doi: 10.1093/aje/kwh096 [DOI] [PubMed] [Google Scholar]
- 63.Starks MA, Schmicker RH, Peterson ED, et al. ; Resuscitation Outcomes Consortium (ROC) . Association of neighborhood demographics with out-of-hospital cardiac arrest treatment and outcomes: where you live may matter. JAMA Cardiol. 2017;2(10):1110-1118. doi: 10.1001/jamacardio.2017.2671 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Documét PI, Sharma RK. Latinos’ health care access: financial and cultural barriers. J Immigr Health. 2004;6(1):5-13. doi: 10.1023/B:JOIH.0000014638.87569.2e [DOI] [PubMed] [Google Scholar]
- 65.Kirby JB, Kaneda T. Neighborhood socioeconomic disadvantage and access to health care. J Health Soc Behav. 2005;46(1):15-31. doi: 10.1177/002214650504600103 [DOI] [PubMed] [Google Scholar]
- 66.Zuvekas SH, Taliaferro GS. Pathways to access: health insurance, the health care delivery system, and racial/ethnic disparities, 1996-1999. Health Aff (Millwood). 2003;22(2):139-153. doi: 10.1377/hlthaff.22.2.139 [DOI] [PubMed] [Google Scholar]
- 67.Raphael E, White J, Li X, et al. Neighborhood deprivation and mental health among immigrants to Sweden. Epidemiology. 2020;31(3):e25-e27. doi: 10.1097/EDE.0000000000001160 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Ben-Shlomo Y, Kuh D. A life course approach to chronic disease epidemiology: conceptual models, empirical challenges and interdisciplinary perspectives. Int J Epidemiol. 2002;31(2):285-293. doi: 10.1093/ije/31.2.285 [DOI] [PubMed] [Google Scholar]
- 69.Menec VH, Shooshtari S, Nowicki S, Fournier S. Does the relationship between neighborhood socioeconomic status and health outcomes persist into very old age? a population-based study. J Aging Health. 2010;22(1):27-47. doi: 10.1177/0898264309349029 [DOI] [PubMed] [Google Scholar]
- 70.Hamano T, Kawakami N, Li X, Sundquist K. Neighbourhood environment and stroke: a follow-up study in Sweden. PLoS One. 2013;8(2):e56680. doi: 10.1371/journal.pone.0056680 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Howard VJ, McClure LA, Kleindorfer DO, et al. Neighborhood socioeconomic index and stroke incidence in a national cohort of blacks and whites. Neurology. 2016;87(22):2340-2347. doi: 10.1212/WNL.0000000000003299 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Organisation for Economic Co-operation and Development International Migration Outlook. OECD Publishing; 2018. [Google Scholar]
- 73.Bansak K, Ferwerda J, Hainmueller J, et al. Improving refugee integration through data-driven algorithmic assignment. Science. 2018;359(6373):325-329. doi: 10.1126/science.aao4408 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eAppendix. Supplemental Methods
eFigure 1. Study Flowchart
eFigure 2. Effect of Neighborhood Disadvantage on Cardiovascular Outcomes, Cox Models
eFigure 3. Effect of Neighborhood Disadvantage on Cardiovascular Outcomes, Using Alternative Neighborhood Deprivation Index
eTable 1. Characteristics Included in Neighborhood Disadvantage Index
eTable 2. Principal Component Analysis: Eigenvalues and Proportion of Variance Explained
eTable 3. Prevalence of Outcomes in Refugee Population Compared With Population of Native-Born Danes Matched on Age and Sex
eTable 4. Effect of Neighborhood Disadvantage on Cardiovascular Outcomes, by Sex and Age of Arrival in Denmark
eReferences